0c40e2f2f9ea02aef54d6bb2994dad3e.ppt
- Количество слайдов: 33
Module 3 Evidence-Based Practice / Documentation An Introduction to Evidence-Based Practice & an Overview of Documentation Systems & the Nurse’s Responsibility for the Documentation of Patient Care
But First…Let’s Review Nursing Diagnosis You are making a home visit, your patient complains of trouble sleeping. Here is the assessment data you collect: Objective Data: Frequent yawning & closes eyes intermittently during interview. Subjective Data: “I’m not sleeping well. ” Reports feeling “very tired” & states, “I just don’t have the energy to do what I normally do each day. This is very bothersome to me… I feel like a real slug. ” Reports having out of town family staying at his home for several weeks. States the house guests have made it difficult to maintain his normal night-time routines.
You look at your NANDA Nursing Diagnosis list and see that there are 2 possible nursing problems related to sleep - SLEEP DEPRIVATION - DISTURBED SLEEP PATTERN In order for you to select the correct nursing diagnosis for this patient, you must verify that the - Definition of the problem reflects your patient’s condition …. . AND - Defining characteristics for the NANADA approved diagnosis are present per the data you have collected during your assessment
What are the Defining Characteristics of the Problem? SLEEP DEPRIVATION ◦ acute confusion, agitation, anxiety, apathy, combativeness, daytime drowsiness, decreased ability to function, fatigue, fleeting nystagmus, hallucinations, hand tremors, heightened sensitivity to pain, inability to concentrate, irritability, lethargy, listlessness, mailaise, perceptual disorders (i. e. , disturbed body sensation, delusions, feeling afloat), restlessness, slowed reaction, transient paranoia DISTURBED SLEEP PATTERN ◦ change in normal sleep pattern, reports not feeling well rested, dissatisfaction with sleep, decreased ability to function, reports being awakened, reports no difficulty falling asleep
ANALYZE / CLUSTER THE DATA WHAT IS THE CORRECT NURSING DIAGNOSIS FOR THIS PATIENT? DISTURBED SLEEP PATTERN
Based on your patient’s clinical presentation, what is an appropriate COMPLETE nursing diagnosis statement for this patient? Include the etiology (R/T part of the nursing diagnosis statement) and the patient’s signs & symptoms (AMB part of the nursing diagnosis statement).
Sample Nursing Diagnosis Statement Disturbed sleep pattern R/T lack of normal night-time routines secondary to house guests AMB patient states, “I’m not sleeping well” & reports feeling “very tired. ”
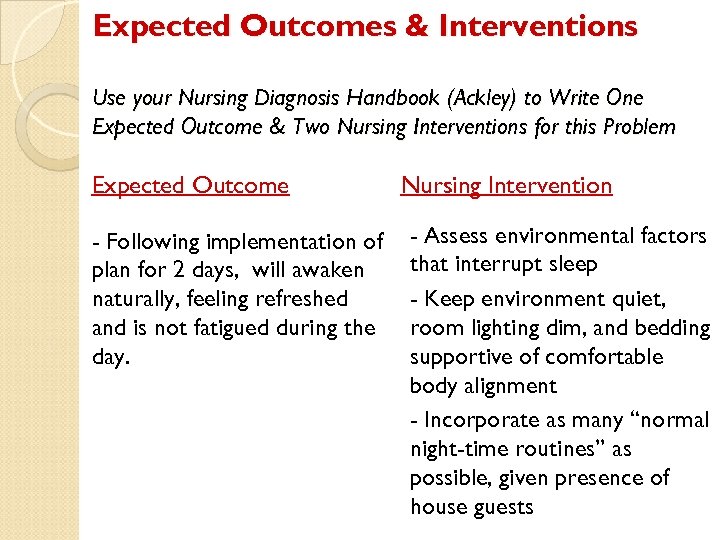
Expected Outcomes & Interventions Use your Nursing Diagnosis Handbook (Ackley) to Write One Expected Outcome & Two Nursing Interventions for this Problem Expected Outcome - Following implementation of plan for 2 days, will awaken naturally, feeling refreshed and is not fatigued during the day. Nursing Intervention - Assess environmental factors that interrupt sleep - Keep environment quiet, room lighting dim, and bedding supportive of comfortable body alignment - Incorporate as many “normal night-time routines” as possible, given presence of house guests
Refer to Evidence-Based Practice Paper/Presentation Assignment DEFINITION OF EVIDENCE-BASED PRACTICE: A problem solving approach to clinical decision making that incorporates a search for the best and latest evidence, clinical expertise, and assessment, and patient preference values within a context of caring. NUR 151 Evidence-Based Practice Assignment Online Tutoring
Occurrence reports are used to ‘write up’ nurses when they make mistakes. TRUE 2. FALSE 1.
Correct answer: 2 (False) They are used by the Risk Management department for quality improvement purposes.
Documentation of nursing care for home health patients requires ongoing assessment of need for skilled nursing care. TRUE 2. FALSE 1.
Correct answer: 1 (True) Also requires documentation of ‘homebound’ status
The nurse documents the following: “Selfadministered subcutaneous insulin injection, with no prompting. “ In Focus Charting, this statement would be preceded by which of the following letters? D 2. R 3. P 4. E 1.
Correct Answer: 2 In Focus Charting, the acronym used is “DAR”: Data, Action, Response. This statement describes how the client responded to the nursing intervention of teaching, so it is “R” for “Response. ”
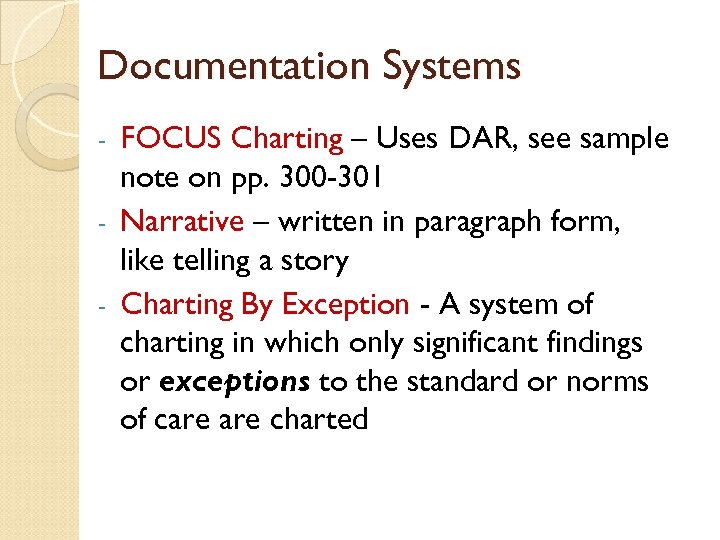
Documentation Systems FOCUS Charting – Uses DAR, see sample note on pp. 300 -301 - Narrative – written in paragraph form, like telling a story - Charting By Exception - A system of charting in which only significant findings or exceptions to the standard or norms of care charted -
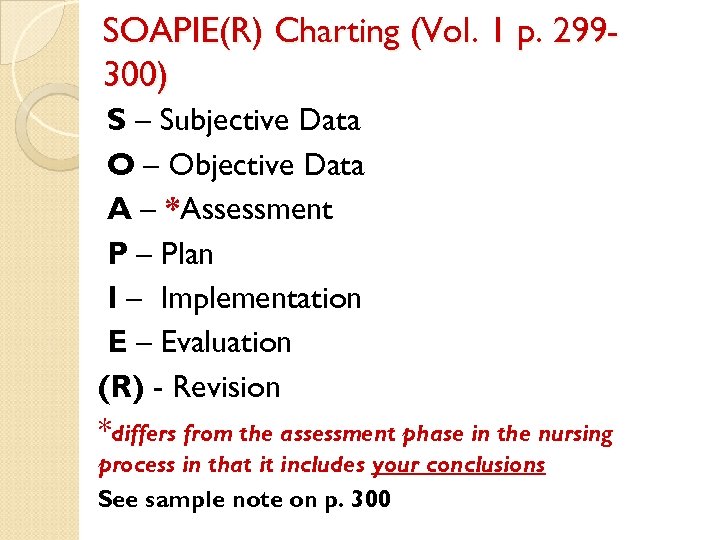
SOAPIE(R) Charting (Vol. 1 p. 299300) S – Subjective Data O – Objective Data A – *Assessment P – Plan I – Implementation E – Evaluation (R) - Revision *differs from the assessment phase in the nursing process in that it includes your conclusions See sample note on p. 300
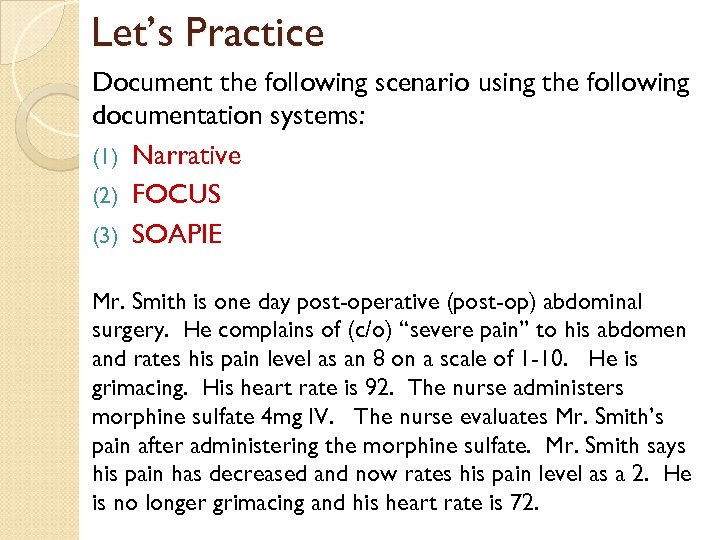
Let’s Practice Document the following scenario using the following documentation systems: (1) Narrative (2) FOCUS (3) SOAPIE Mr. Smith is one day post-operative (post-op) abdominal surgery. He complains of (c/o) “severe pain” to his abdomen and rates his pain level as an 8 on a scale of 1 -10. He is grimacing. His heart rate is 92. The nurse administers morphine sulfate 4 mg IV. The nurse evaluates Mr. Smith’s pain after administering the morphine sulfate. Mr. Smith says his pain has decreased and now rates his pain level as a 2. He is no longer grimacing and his heart rate is 72.
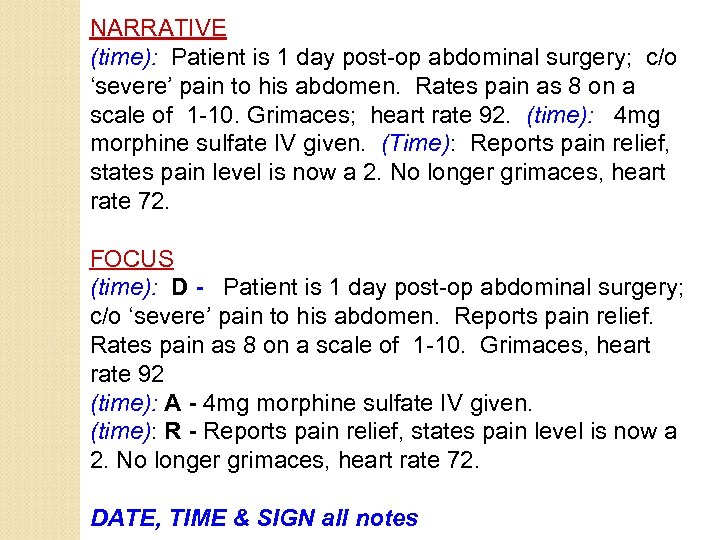
NARRATIVE (time): Patient is 1 day post-op abdominal surgery; c/o ‘severe’ pain to his abdomen. Rates pain as 8 on a scale of 1 -10. Grimaces; heart rate 92. (time): 4 mg morphine sulfate IV given. (Time): Reports pain relief, states pain level is now a 2. No longer grimaces, heart rate 72. FOCUS (time): D - Patient is 1 day post-op abdominal surgery; c/o ‘severe’ pain to his abdomen. Reports pain relief. Rates pain as 8 on a scale of 1 -10. Grimaces, heart rate 92 (time): A - 4 mg morphine sulfate IV given. (time): R - Reports pain relief, states pain level is now a 2. No longer grimaces, heart rate 72. DATE, TIME & SIGN all notes
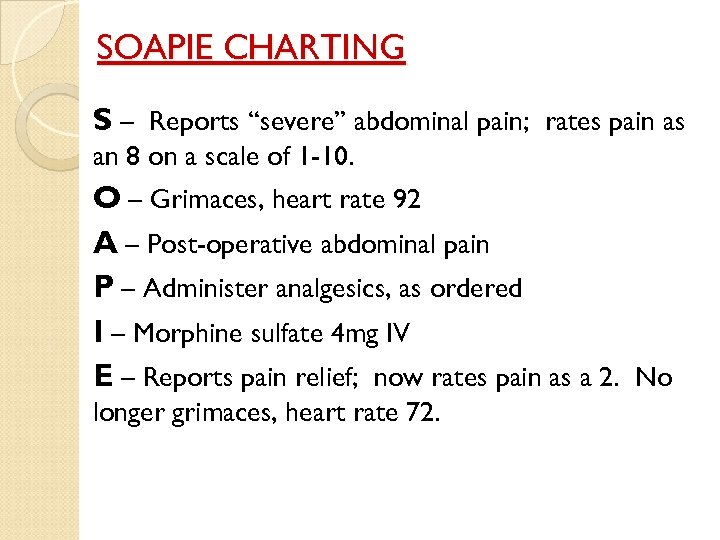
SOAPIE CHARTING S – Reports “severe” abdominal pain; rates pain as an 8 on a scale of 1 -10. O – Grimaces, heart rate 92 A – Post-operative abdominal pain P – Administer analgesics, as ordered I – Morphine sulfate 4 mg IV E – Reports pain relief; now rates pain as a 2. No longer grimaces, heart rate 72.
Common Charting Forms Refer to Fund. Vol 2, pp. 185 – 187 ◦ Intake & Output (I&O) ◦ Long-term care flow sheet ◦ Nursing assessment flow sheet Refer to Fund. Vol 1, p. 51 ◦ Graphic flow sheet – vital signs, I&O Refer to Fund. Vol 1, p. 521 ◦ Medication Administration Record (MAR) Electronic Medical Record - CERNER
Common Abbreviations Refer to Fund. Vol 2, pp. 183 -184 ◦ Each facility has a list of “approved abbreviations” for documentation “Do Not Use” list; refer to Fund. Vol 1, p. 299 (listed on next slide) ◦ More to be added to the list ◦ MUST KNOW!
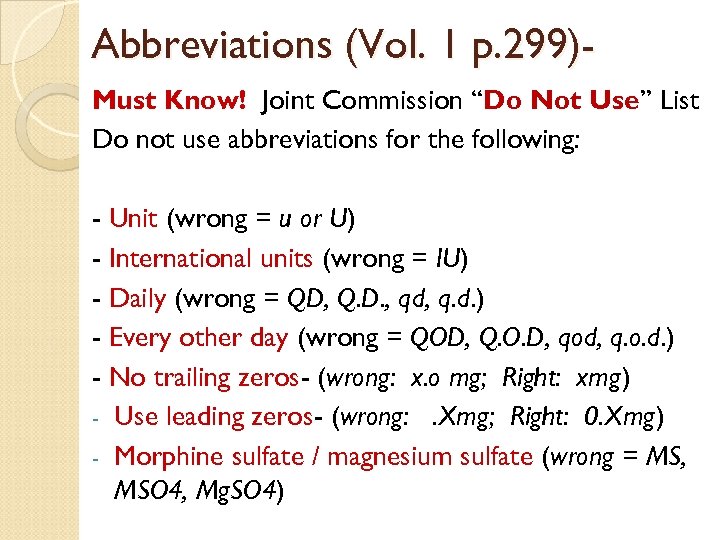
Abbreviations (Vol. 1 p. 299)Must Know! Joint Commission “Do Not Use” List Do not use abbreviations for the following: - Unit (wrong = u or U) - International units (wrong = IU) - Daily (wrong = QD, Q. D. , qd, q. d. ) - Every other day (wrong = QOD, Q. O. D, qod, q. o. d. ) - No trailing zeros- (wrong: x. o mg; Right: xmg) - Use leading zeros- (wrong: . Xmg; Right: 0. Xmg) - Morphine sulfate / magnesium sulfate (wrong = MS, MSO 4, Mg. SO 4)
It is routine practice for RN’s to take verbal and telephone orders. TRUE 2. FALSE 1.
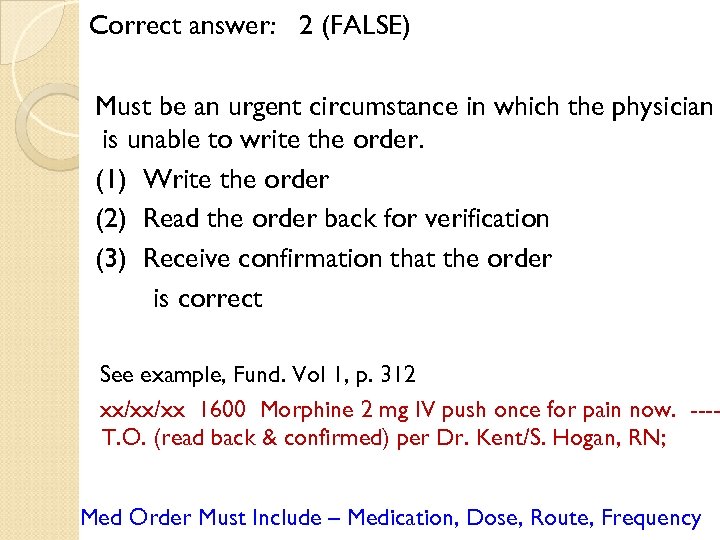
Correct answer: 2 (FALSE) Must be an urgent circumstance in which the physician is unable to write the order. (1) Write the order (2) Read the order back for verification (3) Receive confirmation that the order is correct See example, Fund. Vol 1, p. 312 xx/xx/xx 1600 Morphine 2 mg IV push once for pain now. ---T. O. (read back & confirmed) per Dr. Kent/S. Hogan, RN; Med Order Must Include – Medication, Dose, Route, Frequency
From a legal standpoint, if you didn’t chart it, you didn’t do it! TRUE 2. FALSE 1.
Correct answer: 1 (True) In court, your documentation is your primary defense. Also remember, the order is not legal until it is signed by the physician
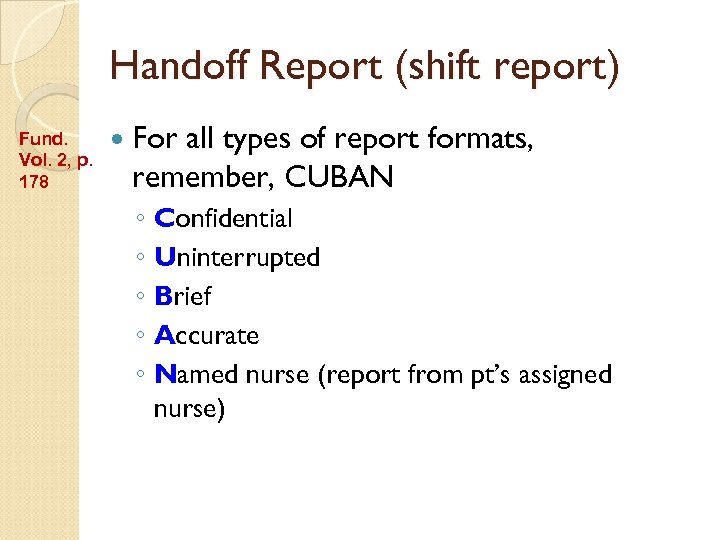
Handoff Report (shift report) Fund. Vol. 2, p. 178 For all types of report formats, remember, CUBAN ◦ Confidential ◦ Uninterrupted ◦ Brief ◦ Accurate ◦ Named nurse (report from pt’s assigned nurse)
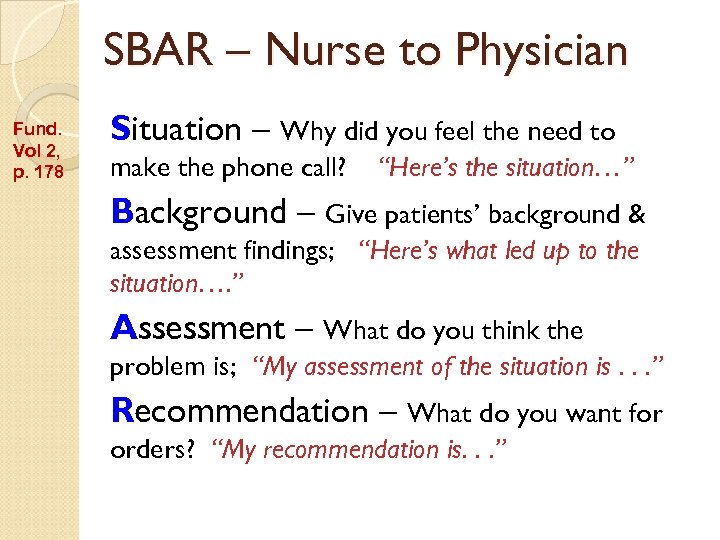
SBAR – Nurse to Physician Fund. Vol 2, p. 178 Situation – Why did you feel the need to make the phone call? “Here’s the situation…” Background – Give patients’ background & assessment findings; “Here’s what led up to the situation…. ” Assessment – What do you think the problem is; “My assessment of the situation is. . . ” Recommendation – What do you want for orders? “My recommendation is. . . ”
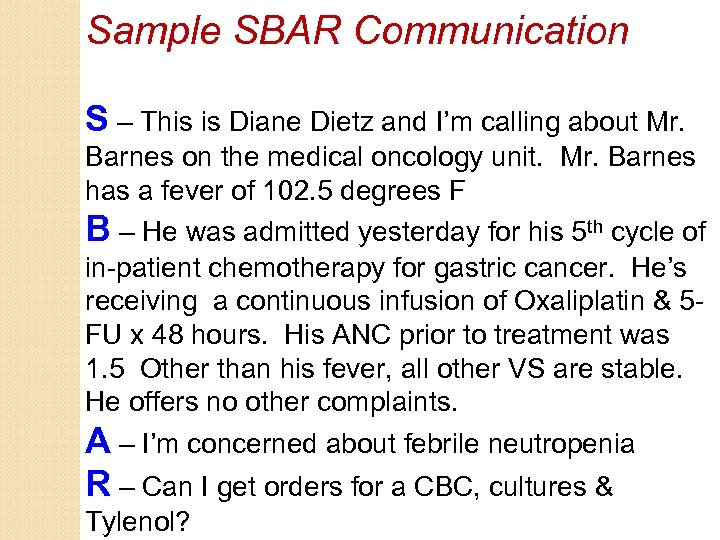
Sample SBAR Communication S – This is Diane Dietz and I’m calling about Mr. Barnes on the medical oncology unit. Mr. Barnes has a fever of 102. 5 degrees F B – He was admitted yesterday for his 5 th cycle of in-patient chemotherapy for gastric cancer. He’s receiving a continuous infusion of Oxaliplatin & 5 FU x 48 hours. His ANC prior to treatment was 1. 5 Other than his fever, all other VS are stable. He offers no other complaints. A – I’m concerned about febrile neutropenia R – Can I get orders for a CBC, cultures & Tylenol?
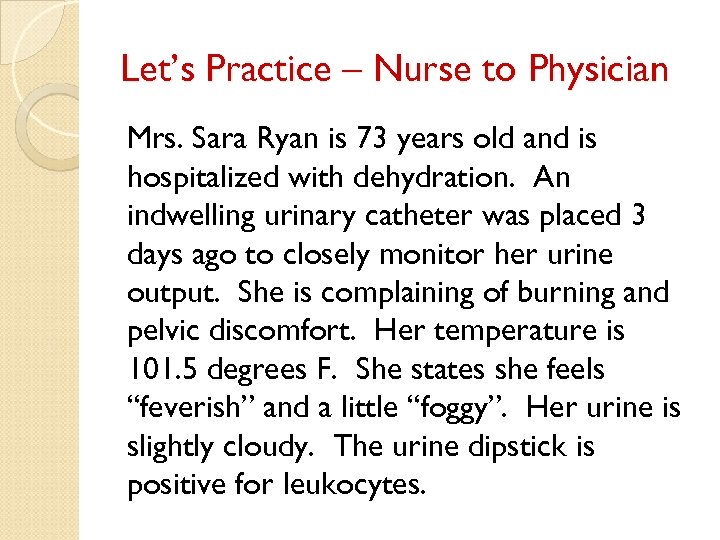
Let’s Practice – Nurse to Physician Mrs. Sara Ryan is 73 years old and is hospitalized with dehydration. An indwelling urinary catheter was placed 3 days ago to closely monitor her urine output. She is complaining of burning and pelvic discomfort. Her temperature is 101. 5 degrees F. She states she feels “feverish” and a little “foggy”. Her urine is slightly cloudy. The urine dipstick is positive for leukocytes.
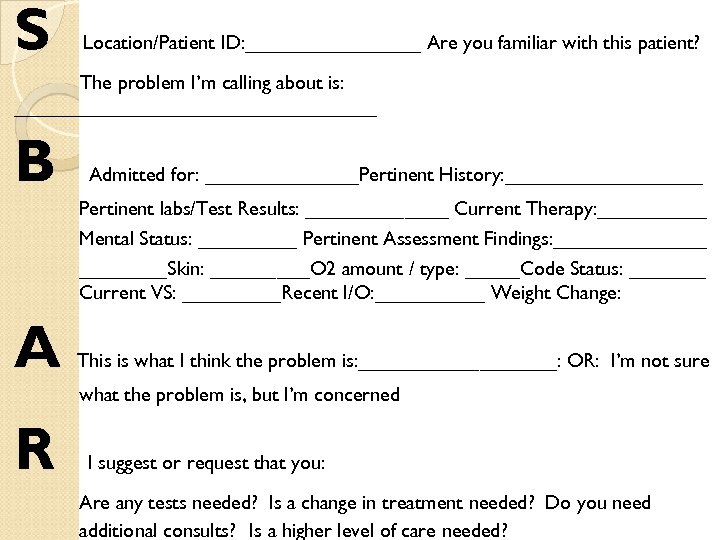
S Location/Patient ID: ________ Are you familiar with this patient? The problem I’m calling about is: _________________ B Admitted for: _______Pertinent History: _________ Pertinent labs/Test Results: _______ Current Therapy: _____ Mental Status: _____ Pertinent Assessment Findings: _______Skin: _____O 2 amount / type: _____Code Status: _______ Current VS: _____Recent I/O: _____ Weight Change: A This is what I think the problem is: _________: OR: I’m not sure what the problem is, but I’m concerned R I suggest or request that you: Are any tests needed? Is a change in treatment needed? Do you need additional consults? Is a higher level of care needed?
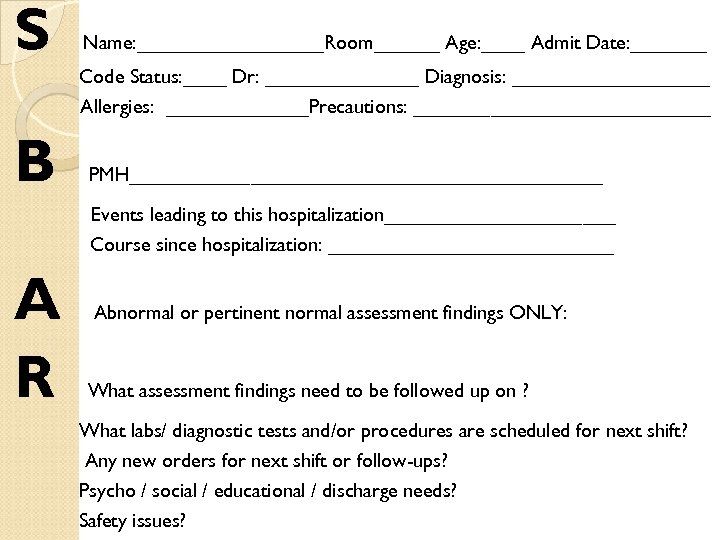
S Name: _________Room______ Age: ____ Admit Date: _______ Code Status: ____ Dr: _______ Diagnosis: _________ Allergies: _______Precautions: ______________ B PMH______________________ Events leading to this hospitalization___________ Course since hospitalization: _____________ A R Abnormal or pertinent normal assessment findings ONLY: What assessment findings need to be followed up on ? What labs/ diagnostic tests and/or procedures are scheduled for next shift? Any new orders for next shift or follow-ups? Psycho / social / educational / discharge needs? Safety issues?
0c40e2f2f9ea02aef54d6bb2994dad3e.ppt