142b17a7488144e83c67af192648ce98.ppt
- Количество слайдов: 20

Modernising diagnostic medical microbiology services Professor Brian I. Duerden CBE, MD Emeritus Professor of Medical Microbiology, Cardiff University

Inspector of Microbiology - 2003 Champion & promote high quality clinical & public health microbiology – all labs in NHS contribute to surveillance – promote standards & quality – identify gaps in specialist & reference micro. – achieve adherence to SOPs – protocols to reduce the risk of loss/misuse – compliance with security and health & safety
Vision and Goal - 2004 An integrated and cohesive, quality assured microbiology and virology service to support clinical care of patients with infection and for health protection.
……. 2011 Microbiology and Virology service – Infection Service Health Protection – Public Health

Slow progress…. why? Pathology modernisation – 2005 visits and report highly variable but little concrete action – Carter review and pilots HPA establishment – Hiatus for public health microbiology 2003 -7 HCAI prominence – MRSA and C. difficile targets – Intense effort 30 years in the “backroom”
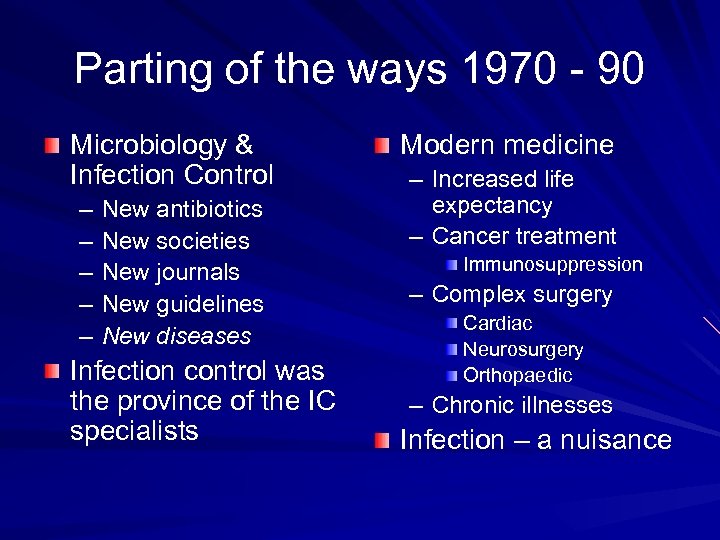
Parting of the ways 1970 - 90 Microbiology & Infection Control – – – New antibiotics New societies New journals New guidelines New diseases Infection control was the province of the IC specialists Modern medicine – Increased life expectancy – Cancer treatment Immunosuppression – Complex surgery Cardiac Neurosurgery Orthopaedic – Chronic illnesses Infection – a nuisance
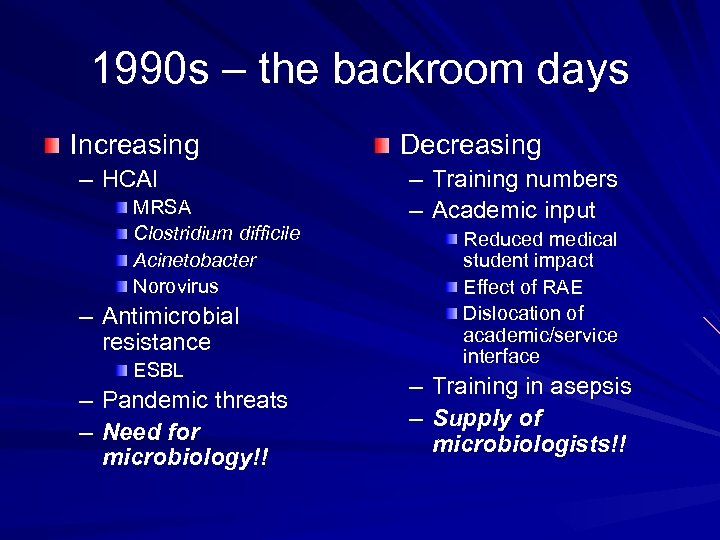
1990 s – the backroom days Increasing – HCAI MRSA Clostridium difficile Acinetobacter Norovirus – Antimicrobial resistance ESBL – – Pandemic threats Need for microbiology!! Decreasing – Training numbers – Academic input Reduced medical student impact Effect of RAE Dislocation of academic/service interface – Training in asepsis – Supply of microbiologists!!
BUT……. . …. we did not help ourselves

Perceived dogmas Laboratory focused – What about patient focus? Individual clinical pathology disciplines A lab in every main hospital/trust Transport too difficult – delays Lab headed by medical microbiologist – Medical microbiologists based in labs – Unwilling to have cover from a distance Daytime (8. 30 – 17. 30) service – On-call out of hours

Results Traditional methods Lack of investment in – new technology, IT Lack of specialisation Isolated services

Where do we go from here?

Coalition Government & NHS reorganisation Infection (prevention &control) is a priority Commissioning by GP Consortia – Need for support and guidance – Potential role for revised National Standards for Microbiology (standard methods) with Professional bodies’ ownership Public Health Service – – – Within DH National and local components Incorporates HPA functions (incl. labs) How will Public Health Microbiology be delivered?

Post-Carter developments Various models – same aims – Consolidation, centralisation – Enable technology development Automation - conventional tests; new technology Molecular, post-genomic – sequencing, micro-array, MALDITOF – – – Concentrate staff expertise Extended (24/7) working Cost effectiveness ………maintain the quality of patient care and public health support
Public Health responsibility HPA (Public Health England) – Public health, specialist, reference microbiology Clinical/diagnostic laboratories – NHS or commissioned Surveillance reporting Notifiable diseases Outbreak identification and support Standardised methods for infections of public health importance
Communicable diseases legislation 2010 Act – Notifiable diseases Requires all diagnostic laboratories to report isolates of pathogens with Public Health significance – Much longer list – In addition to medical practitioners reporting clinical cases – Expectation of accreditation and use of standard methods 2008 Code of Practice for HCAI – Requires microbiology support from an accredited laboratory

Technology developments Automation – Conventional tests – Molecular, post-genomic Which technologies – Next generation sequencing – Micro-arrays – MALDI-TOf – ? ? ? …we need a strategy for their use

UKCRC - TIRI Oxford – Application of sequencing to diagnostic and public health microbiology; eg, HCAIs Imperial – Changing the culture and embedding HCAI prevention & control in healthcare services – Linked to modern diagnostics for HCAI epidemiology St Georges – POC molecular testing and mobile communication modules for STI Cambridge – Sequencing developments for MRSA and web-based systems for analysing data generated remotely

POC testing Healthcare settings – ICU – MRSA screening in A&E etc …need to be integrated with laboratory service “High Street” settings – Increase accessibility for patients/clients – Professional oversight? Interpretation? Advice? – Links to patient record? – Risks loss of surveillance data for public health …Microbiologists need to be involved in pilot projects

Transforming medical specialist training Medical roles of infection specialists – Clinical patient care – Consultation/advice What investigations? Interpretation of results Antimicrobial treatment Epidemiology Infection prevention and control Common training pathway – Core infection training – Clinical care, diagnostic & public Health microbiology/virology , infection prevention & control
Challenges for the future Keep infection as a patient safety priority in healthcare It will never go away! Use modern technology to deliver a patient -focused service Do not repeat the mistakes of 1970 - 2000
142b17a7488144e83c67af192648ce98.ppt