ed354ce203203c5a77898518cb73d893.ppt
- Количество слайдов: 12

MIPS Basics
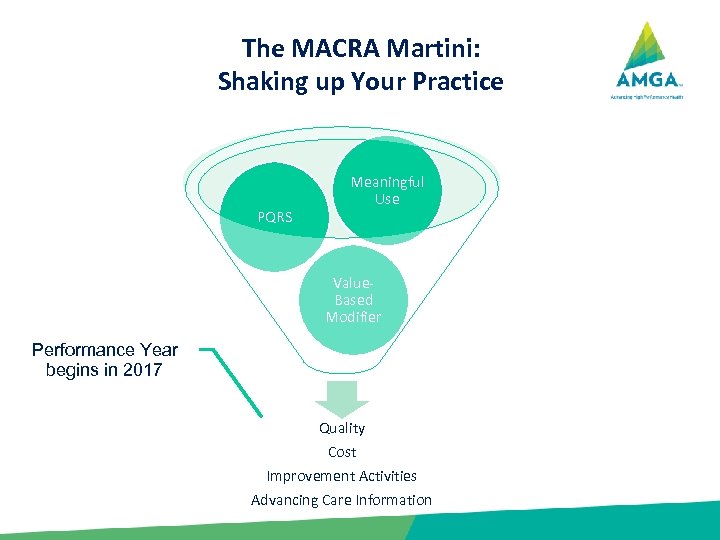
The MACRA Martini: Shaking up Your Practice PQRS Meaningful Use Value. Based Modifier Performance Year begins in 2017 Quality Cost Improvement Activities Advancing Care Information
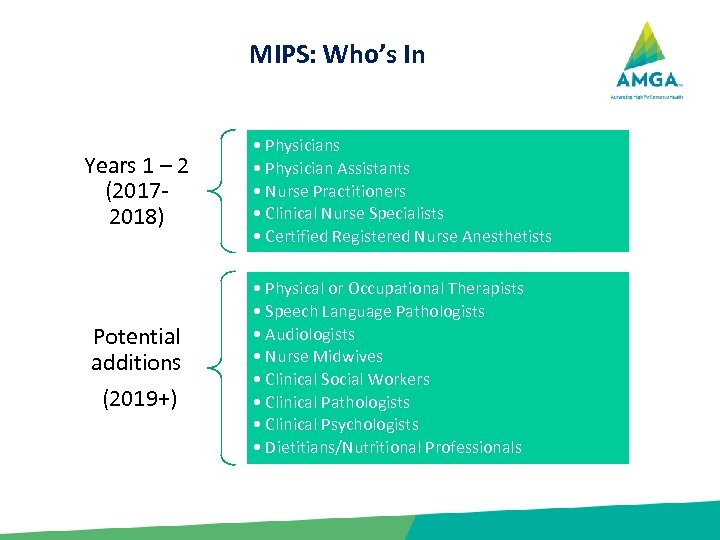
MIPS: Who’s In Years 1 – 2 (20172018) Potential additions (2019+) • Physicians • Physician Assistants • Nurse Practitioners • Clinical Nurse Specialists • Certified Registered Nurse Anesthetists • Physical or Occupational Therapists • Speech Language Pathologists • Audiologists • Nurse Midwives • Clinical Social Workers • Clinical Pathologists • Clinical Psychologists • Dietitians/Nutritional Professionals
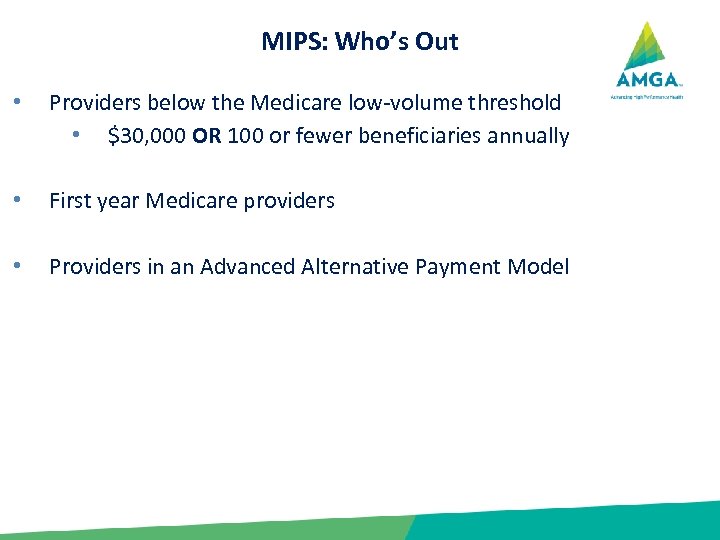
MIPS: Who’s Out • Providers below the Medicare low-volume threshold • $30, 000 OR 100 or fewer beneficiaries annually • First year Medicare providers • Providers in an Advanced Alternative Payment Model
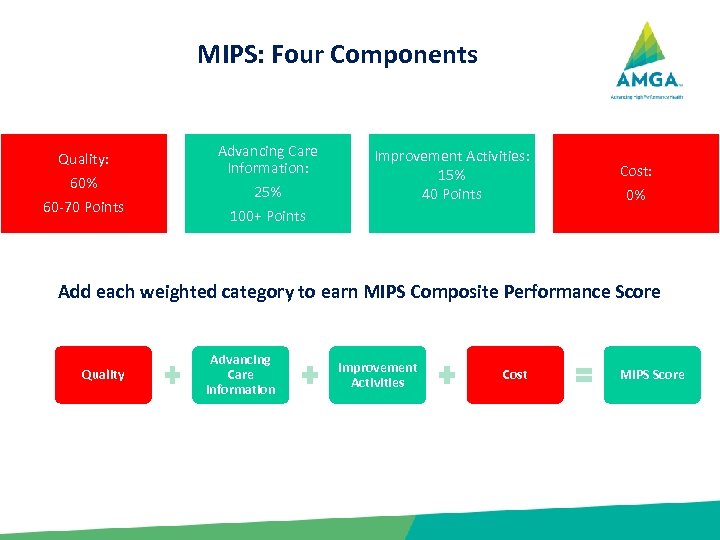
MIPS: Four Components Quality: 60% 60 -70 Points Advancing Care Information: 25% Improvement Activities: 15% 40 Points Cost: 0% 100+ Points Add each weighted category to earn MIPS Composite Performance Score Quality Advancing Care Information Improvement Activities Cost MIPS Score
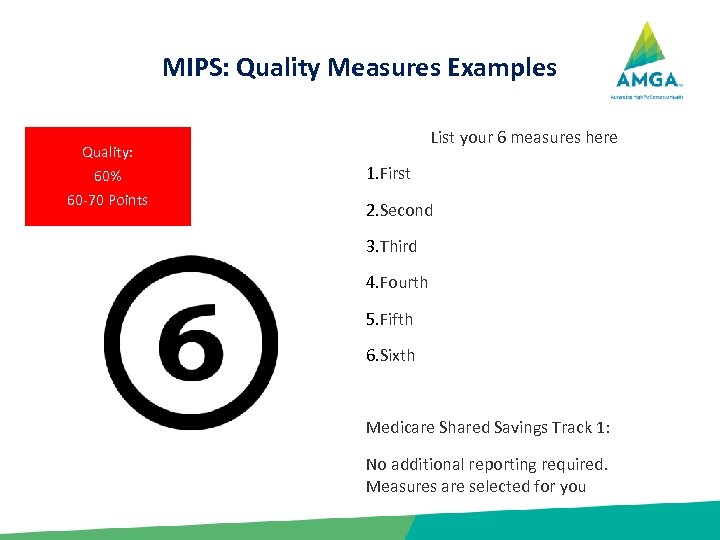
MIPS: Quality Measures Examples List your 6 measures here Quality: 60% 60 -70 Points 1. First 2. Second 3. Third 4. Fourth 5. Fifth 6. Sixth Medicare Shared Savings Track 1: No additional reporting required. Measures are selected for you

MIPS: Improvement Activities Reporting Improvement Activities: 15% 40 Points Our IA Activities 1. Categories 2. Expanded Care Access 3. Care Coordination 4. Population Management Beneficiary Engagement Patient Safety and Practice Assessment Achieving Health Equity Emergency Preparedness and Response Integrated Behavior and Mental Health
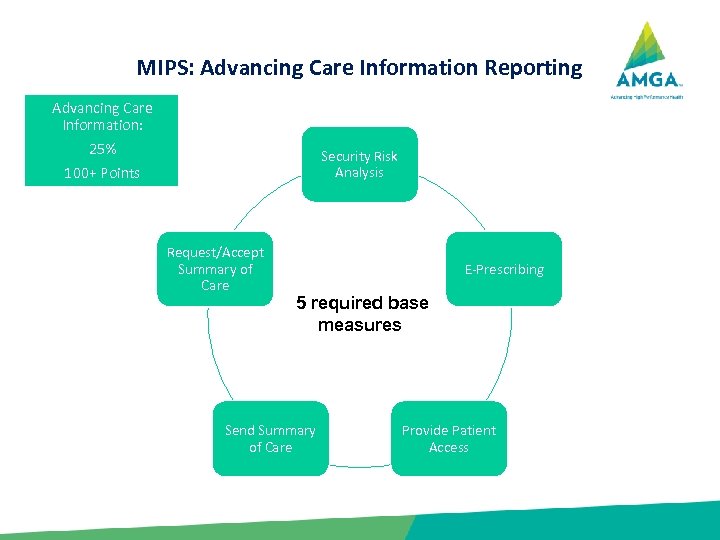
MIPS: Advancing Care Information Reporting Advancing Care Information: 25% Security Risk Analysis 100+ Points Request/Accept Summary of Care E-Prescribing 5 required base measures Send Summary of Care Provide Patient Access
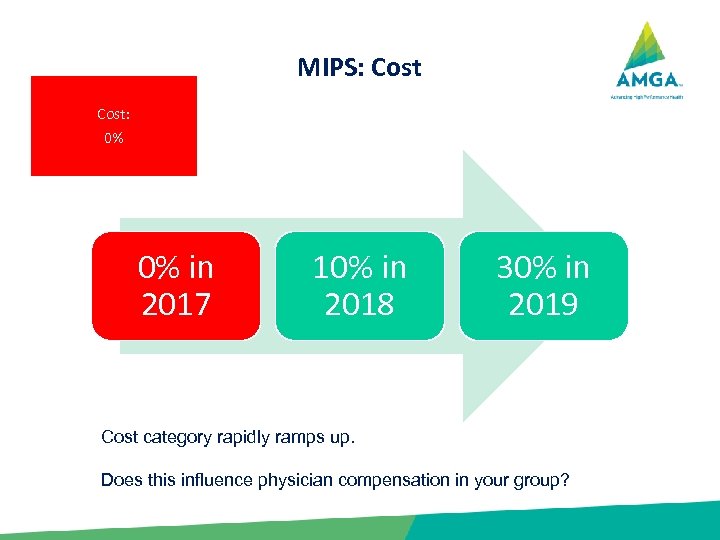
MIPS: Cost: 0% 0% in 2017 10% in 2018 30% in 2019 Cost category rapidly ramps up. Does this influence physician compensation in your group?
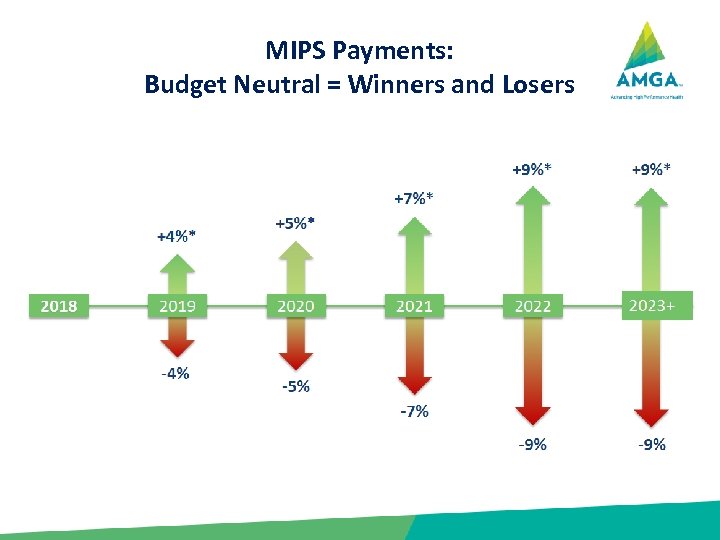
MIPS Payments: Budget Neutral = Winners and Losers
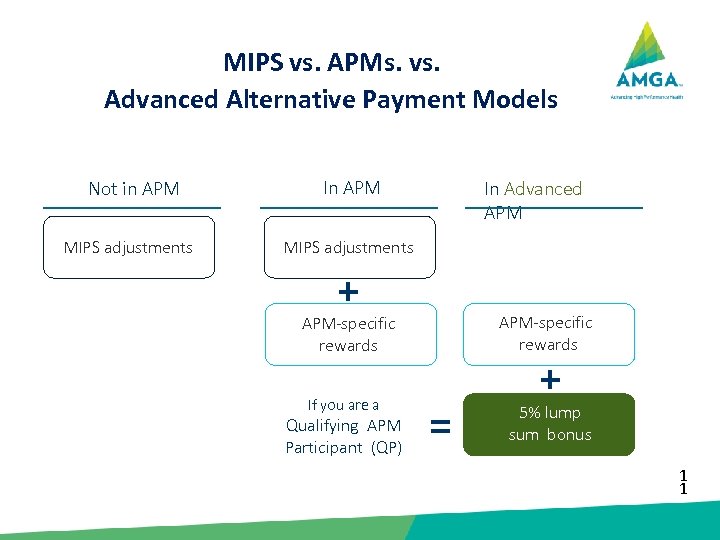
Quality Payment Program MIPS vs. APMs. vs. Advanced Alternative Payment Models Not in APM MIPS adjustments In APM In Advanced APM MIPS adjustments + APM-specific rewards If you are a Qualifying APM Participant (QP) = + 5% lump sum bonus 1 1
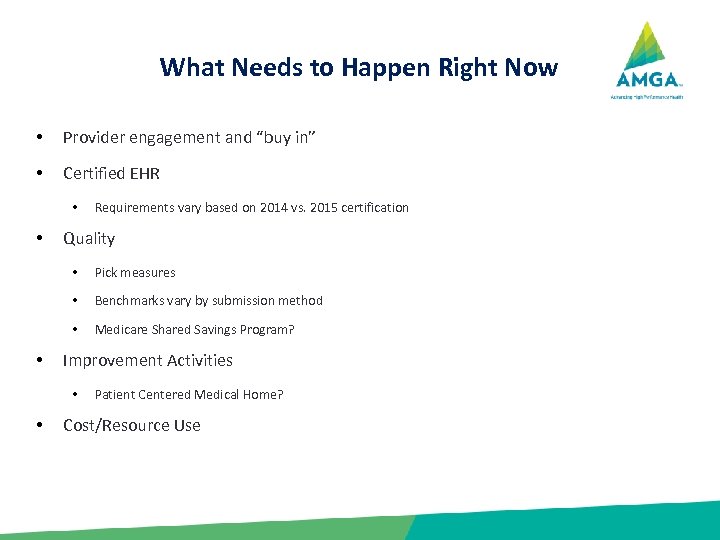
What Needs to Happen Right Now • Provider engagement and “buy in” • Certified EHR • • Requirements vary based on 2014 vs. 2015 certification Quality • • Benchmarks vary by submission method • • Pick measures Medicare Shared Savings Program? Improvement Activities • • Patient Centered Medical Home? Cost/Resource Use
ed354ce203203c5a77898518cb73d893.ppt