3 мыш сокращение 2014-2015 англ.ppt
- Количество слайдов: 93
Ministry of Education of the Republic Kazakhstan KSMU KARAGANDA STATE MEDICAL UNIVERSITITY Department: Physiology Topic: « Muscles contraction » Compliers: c. b. s, Nuriya Mansurovna Kharissova KARAGANDA, 2014
Purpose: • to disassemble the basic concepts on a theme of lecture (kinds of muscles, properties of muscles, kinds of muscular reductions, neuromotor units and their classification, functional features of smooth muscles). • to disassemble the mechanism of carrying out of excitation on a muscular fibre, the mechanism of reduction and a relaxation of muscles, force of muscles their work and exhaustion).
Brief contents 1. 2. 3. 4. 5. Physiology of muscles. Kinds of muscular activity. Physiological properties of muscles. Impellent units and their classification. Types and modes of muscular contractions. Physiology of smooth and skeletal muscles. Features of their structure 6. The Modern theory of the mechanism of contraction and a relaxation of muscles. 7. Force of muscles and their work. The law of average loadings. 8. Fatigue of muscles and the whole organism.
Situational problem • Muscle of nerve-muscle preparation is subjected to indirect stimulation. • After a while the amplitude of the contractions began to diminish. • Does this mean that the muscle fatigue occurred? How is test this hypothesis?
Types of Skeletal Systems • Movement is a major characteristic of animals. This movement is a result of contraction of muscles. The skeleton helps transmit that movement. • Skeletons are either a fluid-filled body cavity, exoskeletons, or internal skeletons.
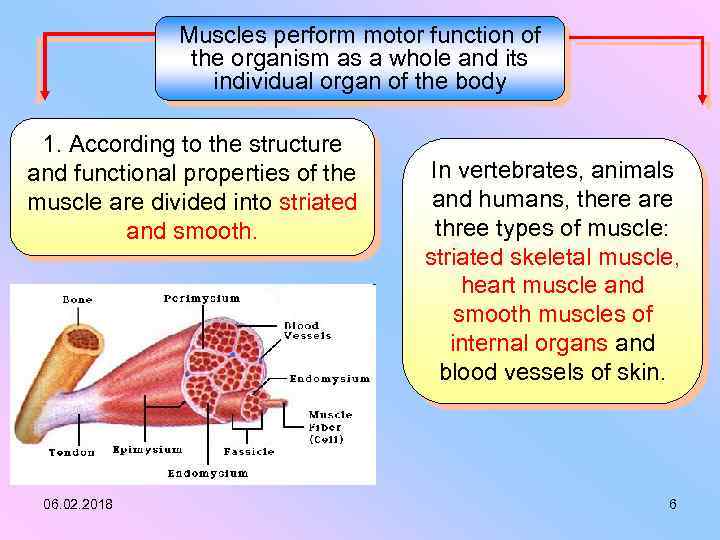
Muscles perform motor function of the organism as a whole and its individual organ of the body 1. According to the structure and functional properties of the muscle are divided into striated and smooth. 06. 02. 2018 In vertebrates, animals and humans, there are three types of muscle: striated skeletal muscle, heart muscle and smooth muscles of internal organs and blood vessels of skin. 6
Skeletal Muscle and Smooth Muscle • Skeletal Muscle are in association with bones forming the skeletal system. • The Skeletal Muscle form 40 to 50 % of body mass. • In human beings about 600 muscles are identified. • The muscles, which are in association with viscera are called Smooth Muscles or visceral Muscles.
Two types of smooth muscle: • 1 - visceral, or unitary, smooth muscle – found in the walls of hollow organs (e. g. , small blood vessels, digestive tract, urinary system, & reproductive system) – multiple fibers contract as a unit (because impulses travel easily across gap junctions from cell to cell) &, in some cases, are selfexcitable (generate spontaneous action potentials & contractions) • 2 - multiunit smooth muscle – consists of motor units that are activated by nervous stimulation – found in the walls of large blood vessels, in the eye (adusting the shape of the lens to permit accommodation & the size of the pupil to adjust the amount of light entering the eye), & at the base of hair follicle (the 'goose bump' muscles)
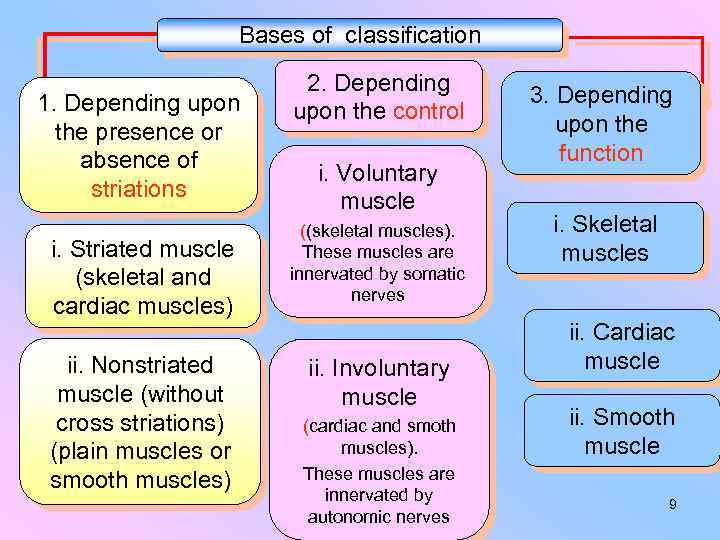
Bases of classification 1. Depending upon the presence or absence of striations i. Striated muscle (skeletal and cardiac muscles) ii. Nonstriated muscle (without cross striations) (plain muscles or smooth muscles) 06. 02. 2018 2. Depending upon the control i. Voluntary muscle ((skeletal muscles). These muscles are innervated by somatic nerves ii. Involuntary muscle (cardiac and smoth muscles). These muscles are innervated by autonomic nerves 3. Depending upon the function i. Skeletal muscles ii. Cardiac muscle ii. Smooth muscle 9
Functions of Muscles and Bones • The skeleton and muscles function together as the musculoskeletal system. • This system (often treated as two separate systems, the muscular, and skeletal) plays an important homeostatic role: allowing the animal to move to more favorable external conditions. • Certain cells in the bones produce immune cells as well as important cellular components of the blood. • Bone also helps regulate blood calcium levels, serving as a calcium sink. • Rapid muscular contraction is important in generating internal heat, another homeostatic function.
Functions of muscle: • motion • maintenance of posture • heat production
Electrical and chemical activity • Muscles have both electrical and chemical activity. • There is an electrical gradient across the muscle cell membrane: the outside is more positive than the inside. • Stimulus causes an instantaneous reversal of this polarity, causing the muscle to contract (the mechanical characteristic) producing a twitch or movement.
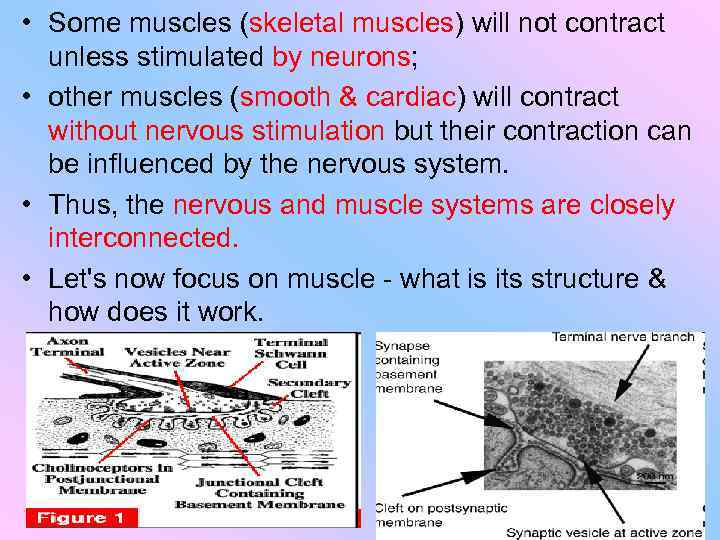
• Some muscles (skeletal muscles) will not contract unless stimulated by neurons; • other muscles (smooth & cardiac) will contract without nervous stimulation but their contraction can be influenced by the nervous system. • Thus, the nervous and muscle systems are closely interconnected. • Let's now focus on muscle - what is its structure & how does it work.
Characteristics of muscle: • excitability - responds to stimuli (e. g. , nervous impulses) • contractility - able to shorten in length • extensibility - stretches when pulled • elasticity - tends to return to original shape & length after contraction or extension
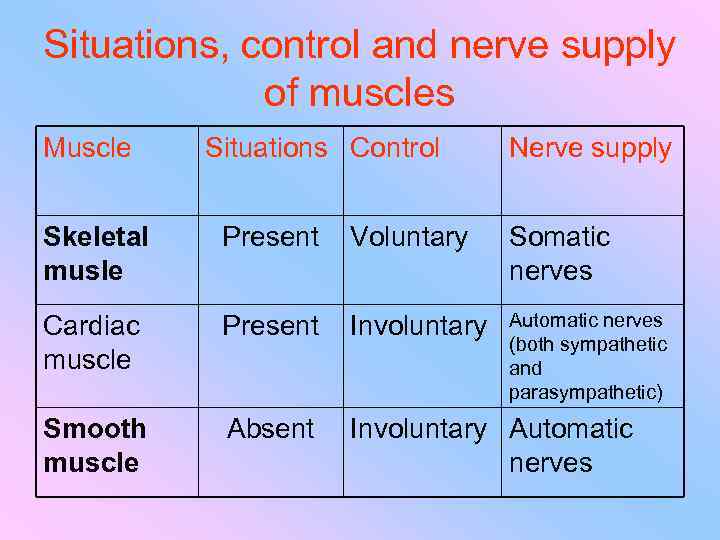
Situations, control and nerve supply of muscles Muscle Situations Control Nerve supply Skeletal musle Present Voluntary Somatic nerves Cardiac muscle Present Involuntary Automatic nerves (both sympathetic and parasympathetic) Smooth muscle Absent Involuntary Automatic nerves
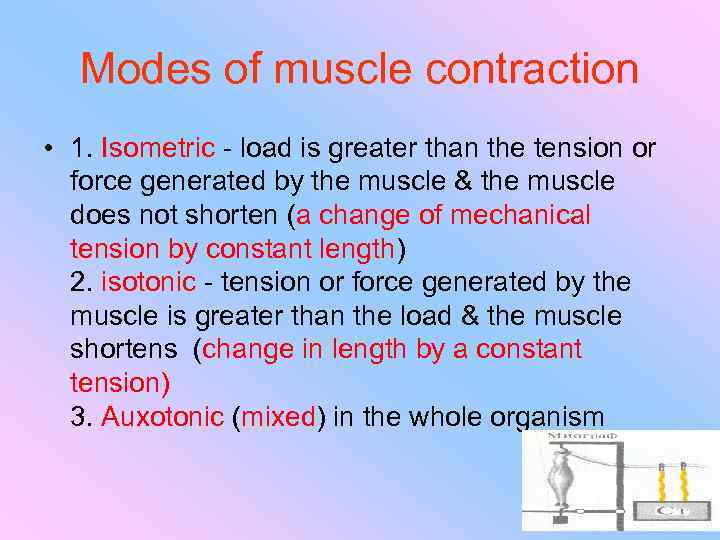
Modes of muscle contraction • 1. Isometric - load is greater than the tension or force generated by the muscle & the muscle does not shorten (a change of mechanical tension by constant length) 2. isotonic - tension or force generated by the muscle is greater than the load & the muscle shortens (change in length by a constant tension) 3. Auxotonic (mixed) in the whole organism
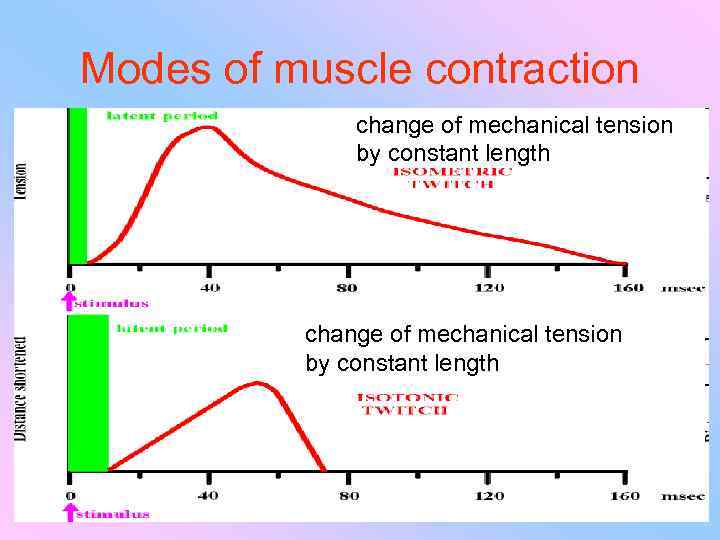
Modes of muscle contraction change of mechanical tension by constant length
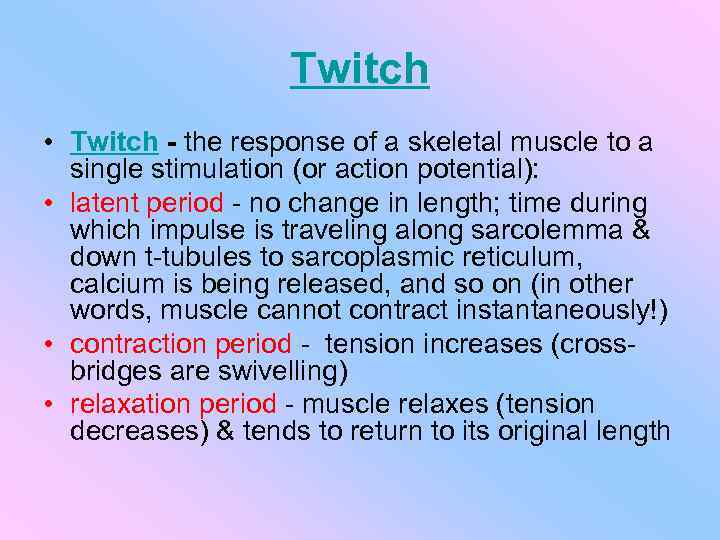
Twitch • Twitch - the response of a skeletal muscle to a single stimulation (or action potential): • latent period - no change in length; time during which impulse is traveling along sarcolemma & down t-tubules to sarcoplasmic reticulum, calcium is being released, and so on (in other words, muscle cannot contract instantaneously!) • contraction period - tension increases (crossbridges are swivelling) • relaxation period - muscle relaxes (tension decreases) & tends to return to its original length
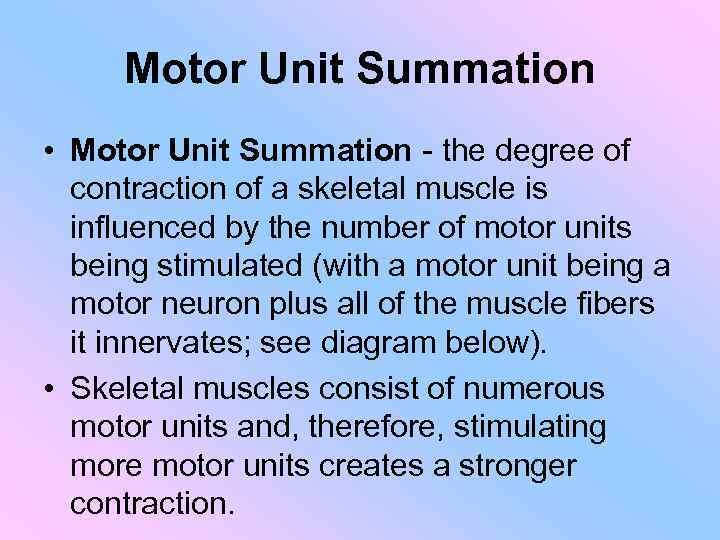
Motor Unit Summation • Motor Unit Summation - the degree of contraction of a skeletal muscle is influenced by the number of motor units being stimulated (with a motor unit being a motor neuron plus all of the muscle fibers it innervates; see diagram below). • Skeletal muscles consist of numerous motor units and, therefore, stimulating more motor units creates a stronger contraction.
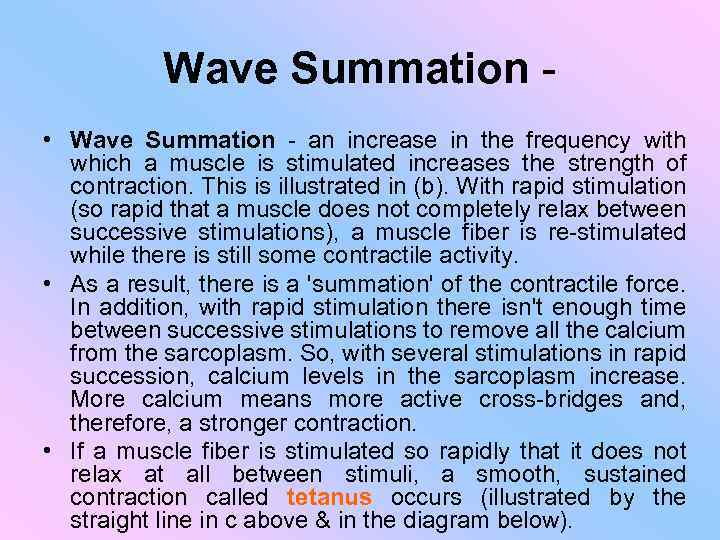
Wave Summation • Wave Summation - an increase in the frequency with which a muscle is stimulated increases the strength of contraction. This is illustrated in (b). With rapid stimulation (so rapid that a muscle does not completely relax between successive stimulations), a muscle fiber is re-stimulated while there is still some contractile activity. • As a result, there is a 'summation' of the contractile force. In addition, with rapid stimulation there isn't enough time between successive stimulations to remove all the calcium from the sarcoplasm. So, with several stimulations in rapid succession, calcium levels in the sarcoplasm increase. More calcium means more active cross-bridges and, therefore, a stronger contraction. • If a muscle fiber is stimulated so rapidly that it does not relax at all between stimuli, a smooth, sustained contraction called tetanus occurs (illustrated by the straight line in c above & in the diagram below).

tetanus
Types of smooth muscle contraction • 1. Basal tone (muscle of blood vessels) 2. Basal tone and phasic activity (uterus. 12 Reduction / min) For smooth muscle is characterized by single-reduction (contraction)
The reaction of muscle to passive stretching • In skeletal muscle - the more its strength, the higher the tension In smooth muscles - first tenson increases and then decreases almost to the source to perform the reservoir function (plasticity)
The strength of skeletal muscle depends on 1. number of excited motor units (DE) 2. Synchronicity of the DE 3. The frequency of action potentials 4. Initial sarcomere length (maxmal contraction in the average length of 2 -2. 5 m
The strength of smooth muscle depends on 1. Initial length of the sarcomeres 2. Synchronous excitation of smooth muscle cells (SMC) 3. Number of MMC 4. The values of the entrance of calcium ions into the MMC
Physiological properties and characteristics of smooth muscle • a) The plasticity - the ability to hold the assigned stretch length without much - any pronounced change in voltage. Due to the plasticity of smooth muscle is provided by the ability of hollow organs in a significant increase in their content, without a marked increase in pressure inside them (the stomach, bladder, etc. ). b) The Automatic - the ability to spontaneous automatic activity. However, regulated by the nerve plexus, which are in the walls of the smooth muscle organs.
Physiological properties and features of skeletal and smooth muscle: excitability, conductivity, contractility • c) The electrical activity (irritability). Upon excitation of smooth muscle in which there action potentials, and there is an automatic contraction of the muscle. The magnitude of the resting potential in smooth muscle with machine is 30 - 70 m. V. And in the non-automatic 60 - 70 m. V in skeletal muscle (-80 -90 m. V). The action potential in smooth muscle (-60 m. V) is slightly lower than in skeletal (-120 -135 m. V) Ionic mechanism of action potentials in a number of smooth muscle associated with the appearance of membrane permeability is not for Na and for Ca, barium and strontium
Physiological properties and features of skeletal and smooth muscle (con. ) • d) Conduct of excitation. Excitation in smooth muscle distributed in the form of local electric currents between the excited and energized portion of the cell membrane, from one fiber to another excitation is the Nexus. Velocity of conduction of excitation in smooth muscle (2 - 15 cm / s) than in skeletal (in the double-headed muscle 3. 55 m / s)
Physiological properties and features of skeletal and smooth muscle • e) contraction of smooth muscles. In the mechanism of reduction plays a major role of Ca ions. • In smooth muscle, unlike skeletal twitch may occur. Length of reach a few tens of seconds. In skeletal muscle - tetanic contraction (neurotransmitter - Acetylcholine) Y smooth - solitary reductions (plectrum - noradrenalin etc. )
Physiological properties and features of skeletal and smooth muscle • e) Regulation of smooth muscle. For the smooth muscles in the body adequate stimulus is a degree of tension (the more stretched, the greater the force is reduced), subject to the autonomic nervous system. Activities of skeletal muscle is regulated by motor neurons, which come from the nerve impulses of the pyramidal and extrapyramidal tract
• Skeletal muscles are organized into hundreds of motor units, each of which is a motor neuron and a group of muscle fibers. • A graded response to a circumstance will involve controlling the number of motor units. • While individual muscle units contract as a unit, the entire muscle can contract on a graded basis due to their organization into motor units.
Contraction of Nonmuscular Cells • Actin and myosin, whose interaction causes muscle contraction, occur in many other cells. Actin is attached to the inner surface of the plasma membrane. The interaction of cytoplasmic myosin and this actin causes contraction of the cell, such a the coordinated contractions of intestinal cells to absorb nutrients.
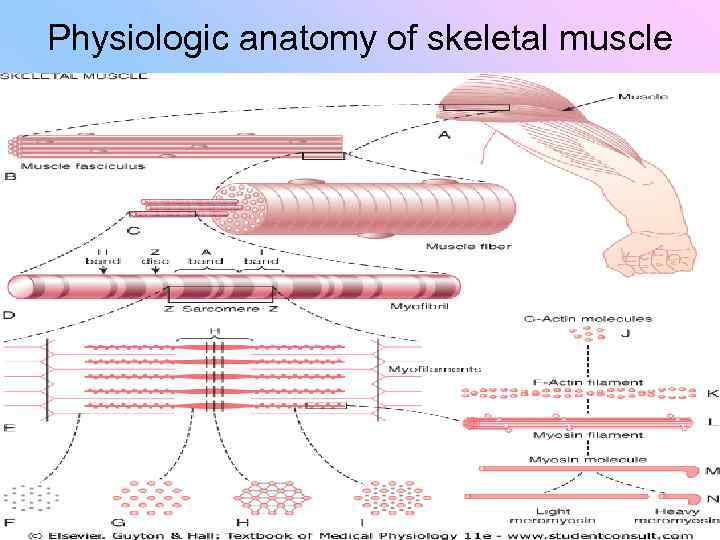
Skeletal Muscle Structure • Muscle fibers are multinucleated, with the nuclei located just under the plasma membrane. • Most of the cell is occupied by striated, thread - like myofibrils. • Within each myofibril there are dense Z lines. • A sarcomere (or muscle functional unit) extends from Z line to Z line. • Each sarcomere has thick and thin filaments. The thick filaments are made of myosin and occupy the center of each sarcomere. • Thin filaments are made of actin and anchor to the Z line.
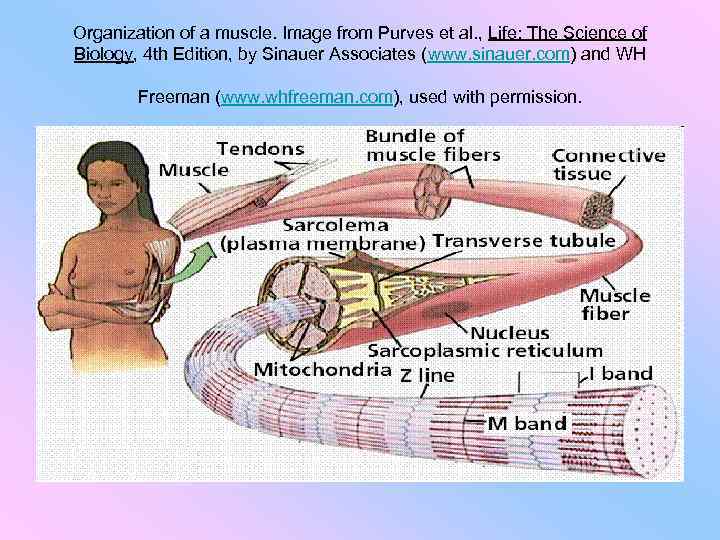
Organization of a muscle. Image from Purves et al. , Life: The Science of Biology, 4 th Edition, by Sinauer Associates (www. sinauer. com) and WH Freeman (www. whfreeman. com), used with permission.
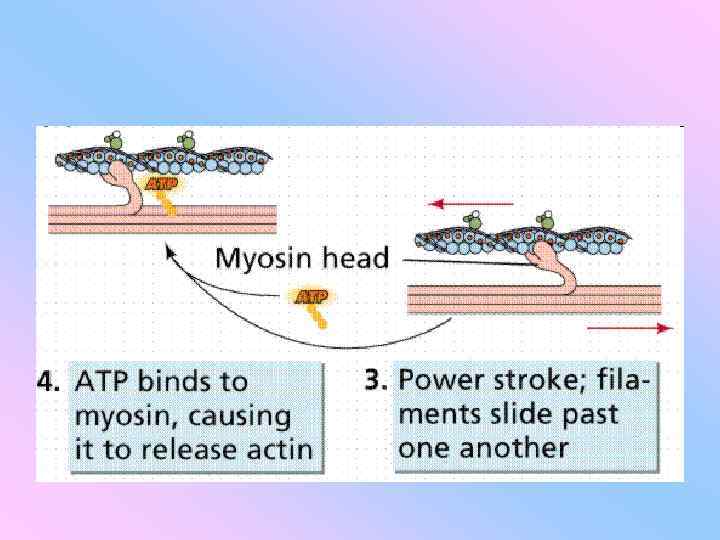
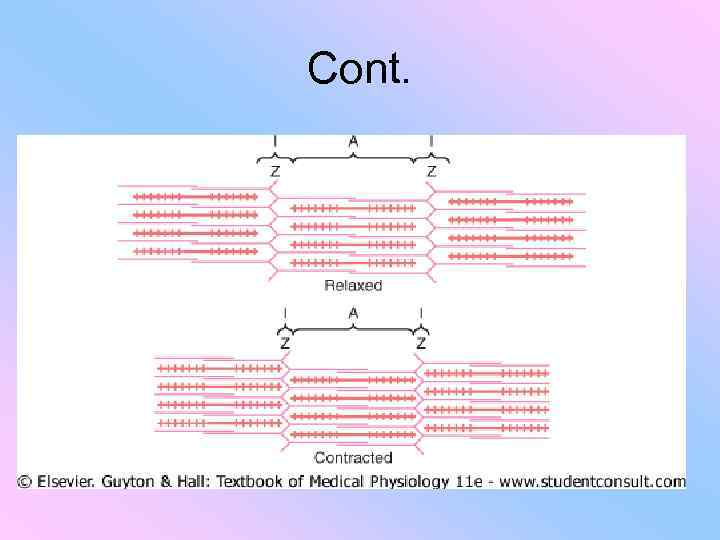
Muscles contract • Myosin heads attach to binding sites on the actin filaments. • The myosin heads swivel toward the center of the sarcomere, detach and then reattach to the nearest active site of the actin filament. • Each cycle of attachment, swiveling, and detachment shortens the sarcomere 1%. • Hundreds of such cycles occur each second during muscle contraction.
Muscles contract • Muscles contract by shortening each sarcomere. • The sliding filament model of muscle contraction has thin filaments on each side of the sarcomere sliding past each other until they meet in the middle. • Myosin filaments have club-shaped heads that project toward the actin filaments.
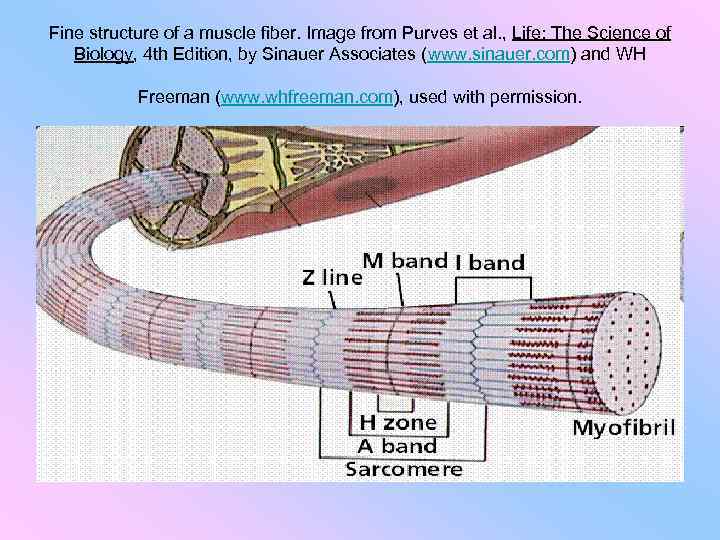
Fine structure of a muscle fiber. Image from Purves et al. , Life: The Science of Biology, 4 th Edition, by Sinauer Associates (www. sinauer. com) and WH Freeman (www. whfreeman. com), used with permission.
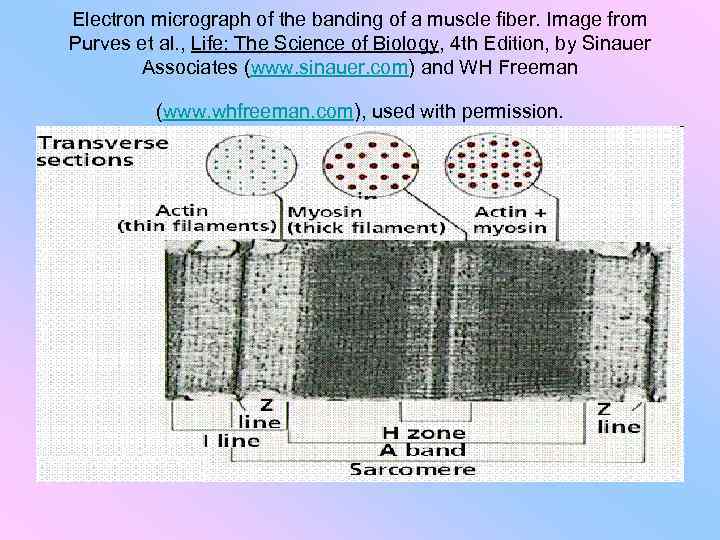
Electron micrograph of the banding of a muscle fiber. Image from Purves et al. , Life: The Science of Biology, 4 th Edition, by Sinauer Associates (www. sinauer. com) and WH Freeman (www. whfreeman. com), used with permission.
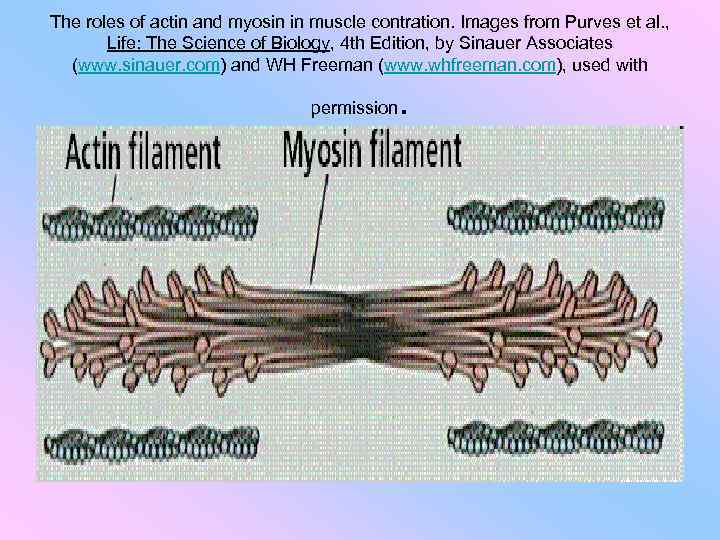
The roles of actin and myosin in muscle contration. Images from Purves et al. , Life: The Science of Biology, 4 th Edition, by Sinauer Associates (www. sinauer. com) and WH Freeman (www. whfreeman. com), used with permission .
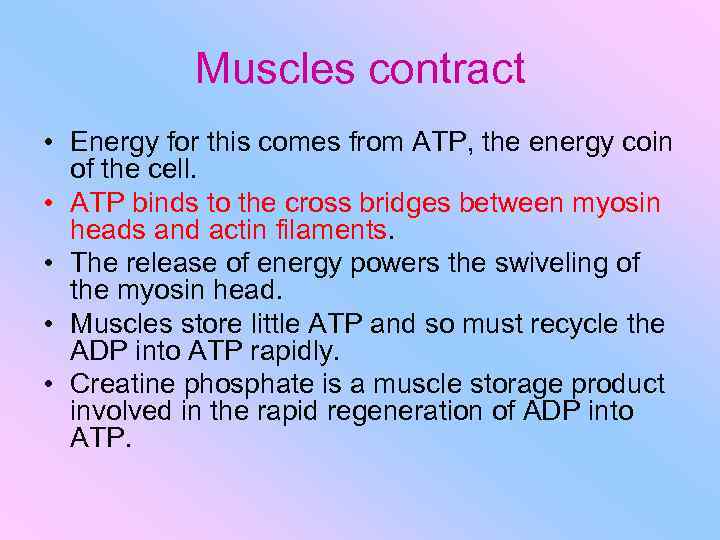
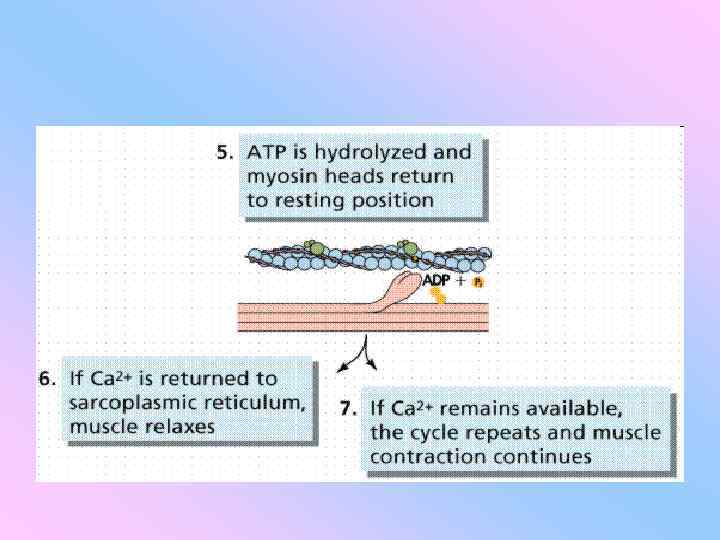
Muscles contract • Energy for this comes from ATP, the energy coin of the cell. • ATP binds to the cross bridges between myosin heads and actin filaments. • The release of energy powers the swiveling of the myosin head. • Muscles store little ATP and so must recycle the ADP into ATP rapidly. • Creatine phosphate is a muscle storage product involved in the rapid regeneration of ADP into ATP.
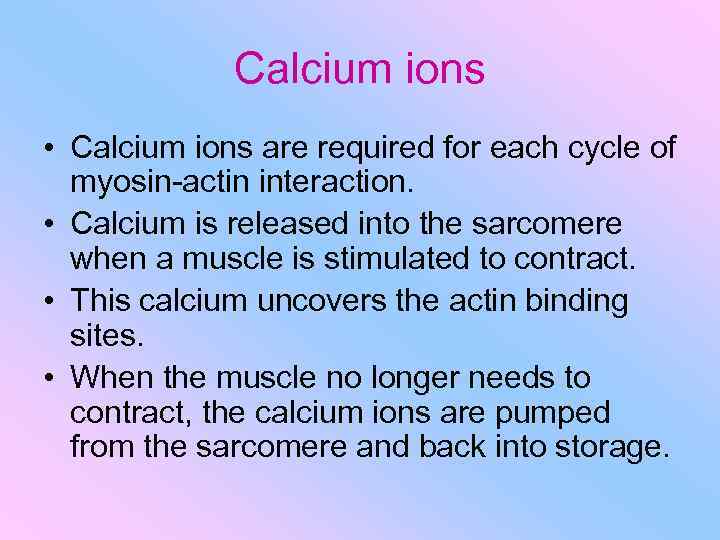
Calcium ions • Calcium ions are required for each cycle of myosin-actin interaction. • Calcium is released into the sarcomere when a muscle is stimulated to contract. • This calcium uncovers the actin binding sites. • When the muscle no longer needs to contract, the calcium ions are pumped from the sarcomere and back into storage.
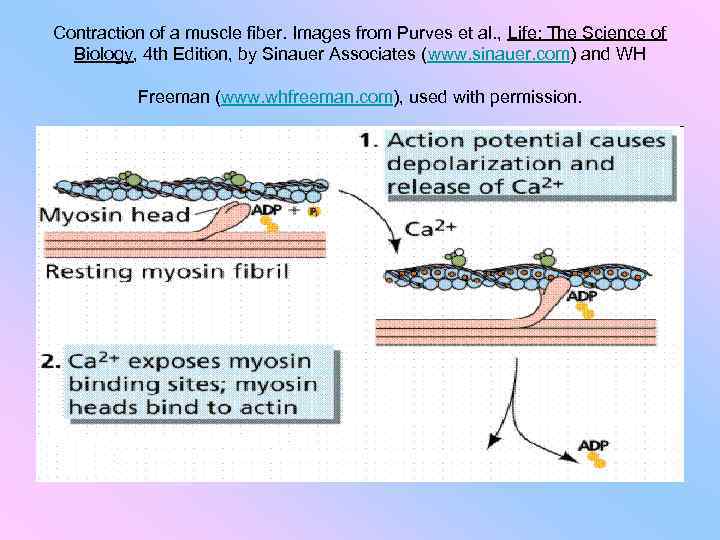
Contraction of a muscle fiber. Images from Purves et al. , Life: The Science of Biology, 4 th Edition, by Sinauer Associates (www. sinauer. com) and WH Freeman (www. whfreeman. com), used with permission.
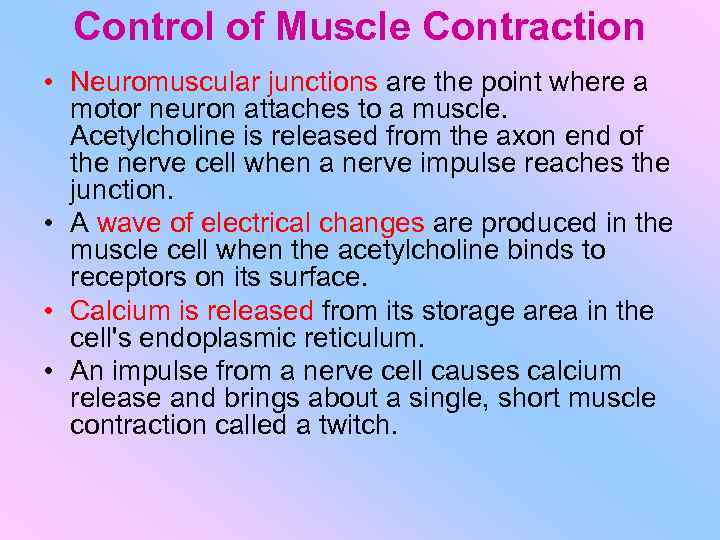
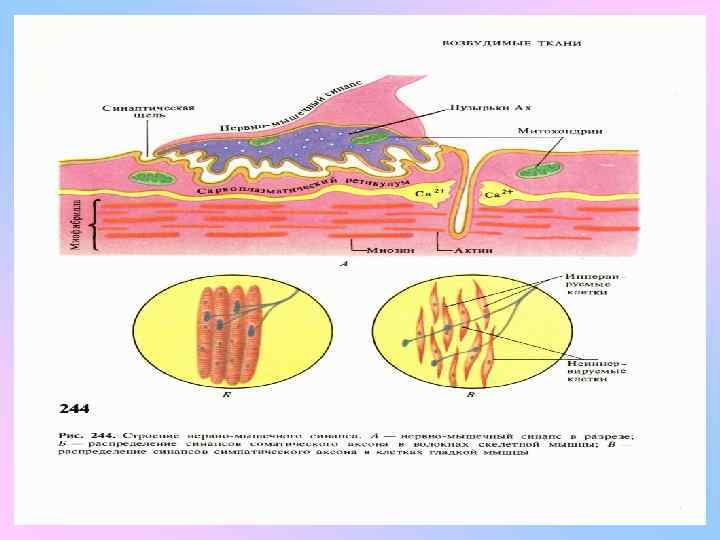
Control of Muscle Contraction • Neuromuscular junctions are the point where a motor neuron attaches to a muscle. Acetylcholine is released from the axon end of the nerve cell when a nerve impulse reaches the junction. • A wave of electrical changes are produced in the muscle cell when the acetylcholine binds to receptors on its surface. • Calcium is released from its storage area in the cell's endoplasmic reticulum. • An impulse from a nerve cell causes calcium release and brings about a single, short muscle contraction called a twitch.
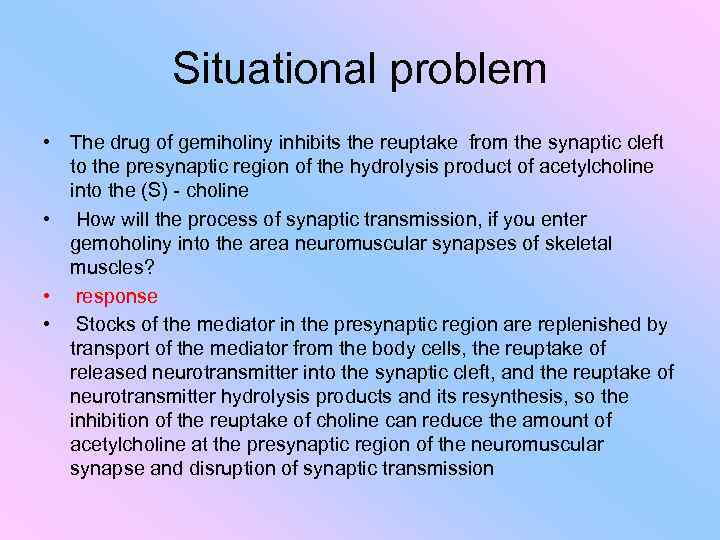
Situational problem • The drug of gemiholiny inhibits the reuptake from the synaptic cleft to the presynaptic region of the hydrolysis product of acetylcholine into the (S) - choline • How will the process of synaptic transmission, if you enter gemoholiny into the area neuromuscular synapses of skeletal muscles? • response • Stocks of the mediator in the presynaptic region are replenished by transport of the mediator from the body cells, the reuptake of released neurotransmitter into the synaptic cleft, and the reuptake of neurotransmitter hydrolysis products and its resynthesis, so the inhibition of the reuptake of choline can reduce the amount of acetylcholine at the presynaptic region of the neuromuscular synapse and disruption of synaptic transmission

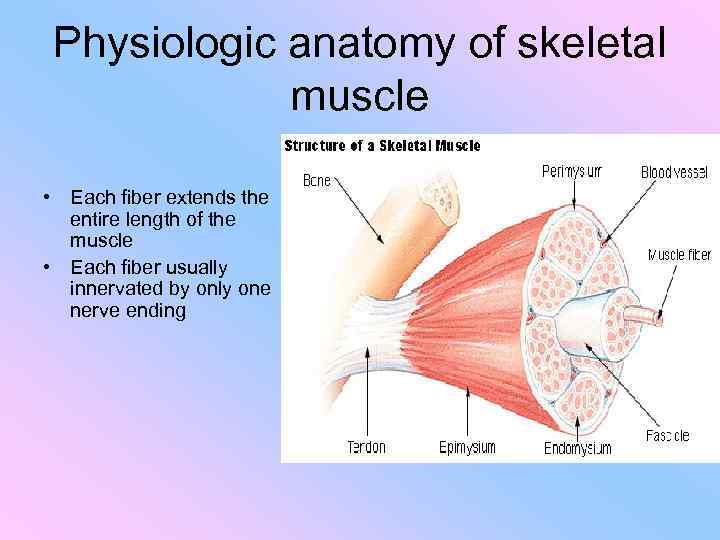
Physiologic anatomy of skeletal muscle • Each fiber extends the entire length of the muscle • Each fiber usually innervated by only one nerve ending
Physiologic anatomy of skeletal muscle
Cont.
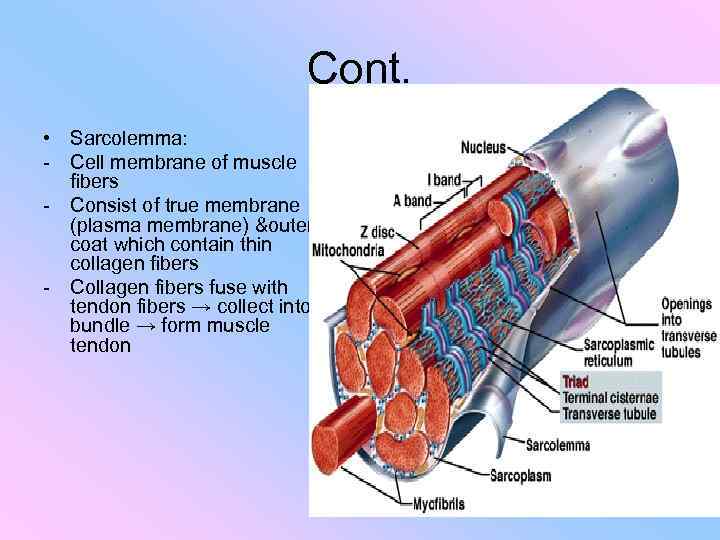
Cont. • Sarcolemma: - Cell membrane of muscle fibers - Consist of true membrane (plasma membrane) &outer coat which contain thin collagen fibers - Collagen fibers fuse with tendon fibers → collect into bundle → form muscle tendon
Cont. • Actin & myosin filaments are kept in place by protein called titin which is very springy • Sarcoplasm reticulum: - The ICF that fill the space between the myofibrils - Contain K, Mg, phosphate & protein enzymes - Contain mitochondria → supply ATP
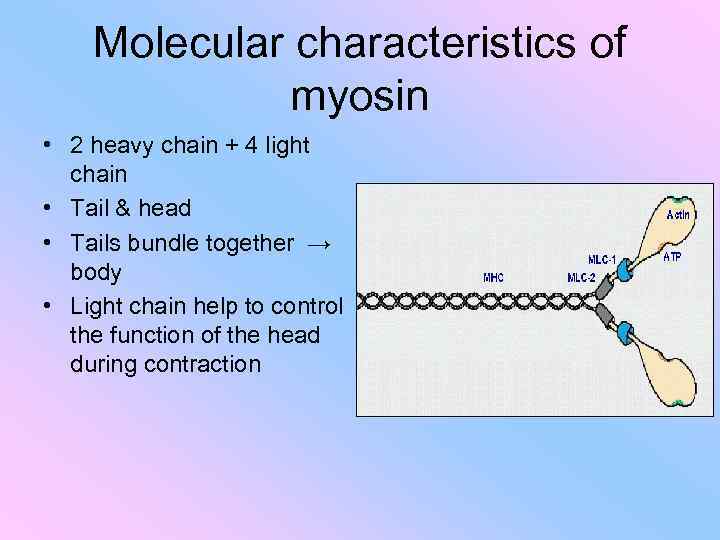
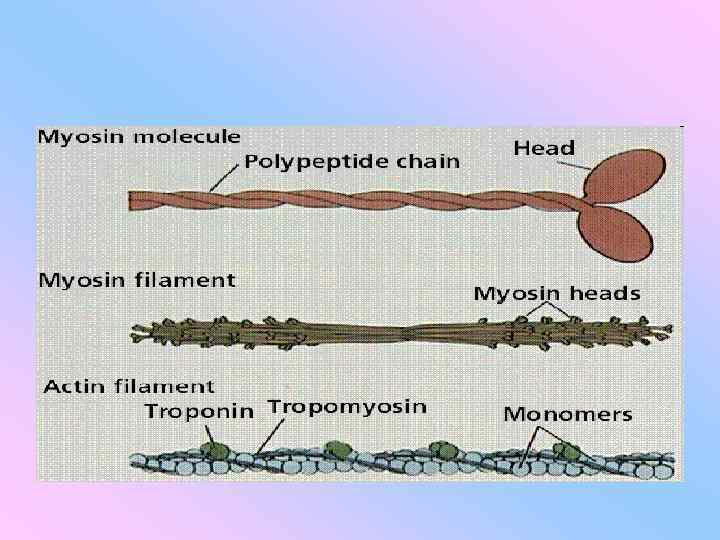
Molecular characteristics of myosin • 2 heavy chain + 4 light chain • Tail & head • Tails bundle together → body • Light chain help to control the function of the head during contraction
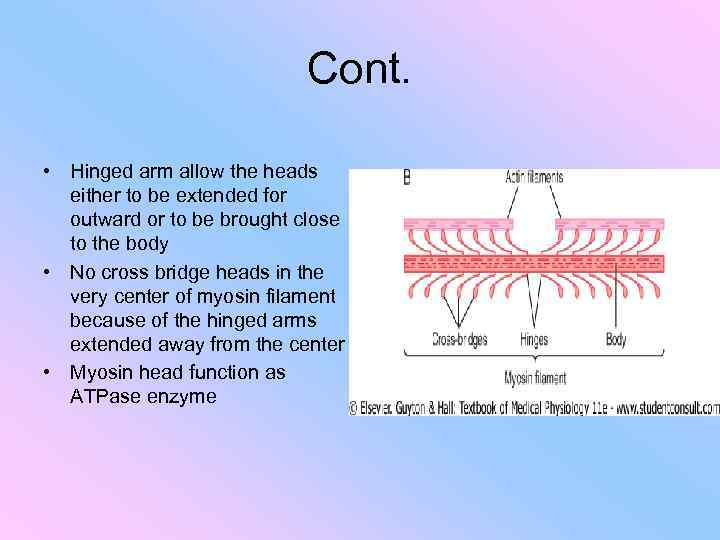
Cont. • Hinged arm allow the heads either to be extended for outward or to be brought close to the body • No cross bridge heads in the very center of myosin filament because of the hinged arms extended away from the center • Myosin head function as ATPase enzyme
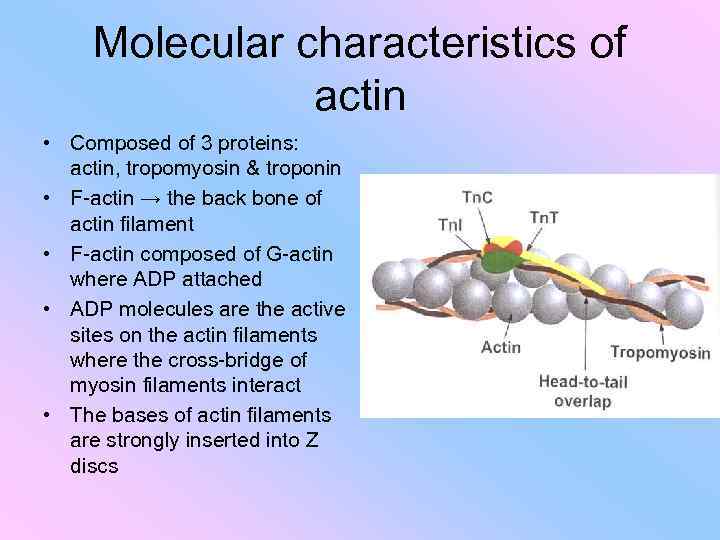
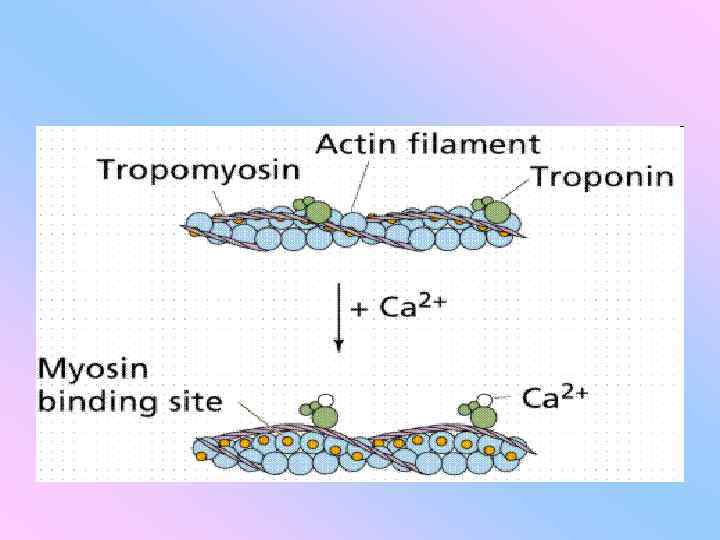
Molecular characteristics of actin • Composed of 3 proteins: actin, tropomyosin & troponin • F-actin → the back bone of actin filament • F-actin composed of G-actin where ADP attached • ADP molecules are the active sites on the actin filaments where the cross-bridge of myosin filaments interact • The bases of actin filaments are strongly inserted into Z discs
Tropomyosin & Troponin • In resting state: tropomyosin lie on top of the active site of actin strands → prevent contraction • Troponin is 3 types : - I → strong affinity to actin - T → strong affinity to tropomyosin - C → strong affinity to Ca • The strong affinity of troponin to Ca ions → initiate contraction process
General mechanism of muscle contraction 1 - action potential travel along nerve to its endings on muscle fibers 2 - at each ending, nerve secrete Ach 3 - Ach-gated channel open 4 - large quantities of Na enter the muscle fiber cell 5 - initiation of action potential & travel along muscle fiber 6 - sarcoplasmic reticulum release large quantities of Ca 7 - sliding of actin on myosin filaments 8 - Ca pumped back into sarcoplasmic reticulum by Ca membrane pump → muscle contraction cease
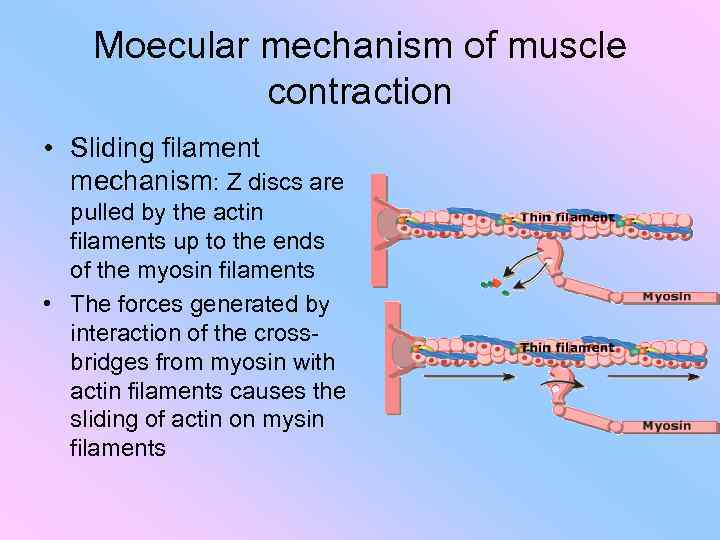
Moecular mechanism of muscle contraction • Sliding filament mechanism: Z discs are pulled by the actin filaments up to the ends of the myosin filaments • The forces generated by interaction of the crossbridges from myosin with actin filaments causes the sliding of actin on mysin filaments
Interaction between actin & myosin filaments • If the troponin-tropomyosin complex is added to actin filament, the binding between myosin & actin doesn’t take place • The active sites on normal actin filaments of relaxed muscle are inhibited or covered by that complex • Role of Ca ions: 1 - Ca combine with troponin C 2 - troponin complex undergoes a conformational changes → tropomyosin molecule deeper into the groove between the 2 actin strands 3 - active sites of actin uncovers → allow them to attract the myosin cross-bridge heads → contraction
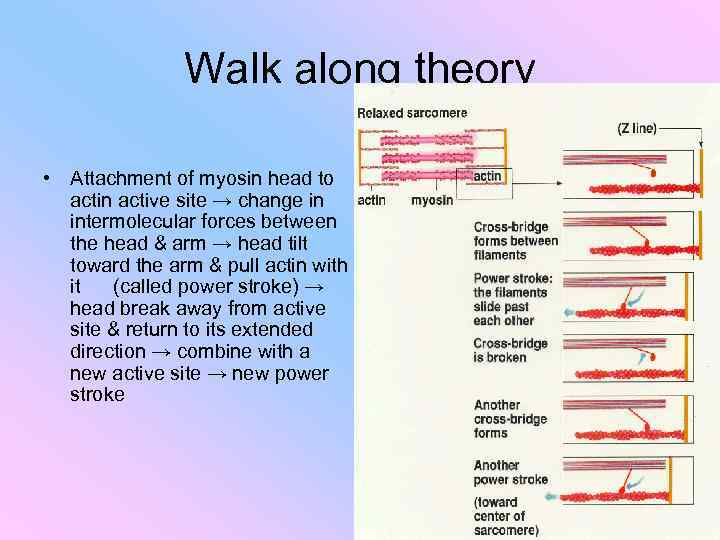
Walk along theory • Attachment of myosin head to actin active site → change in intermolecular forces between the head & arm → head tilt toward the arm & pull actin with it (called power stroke) → head break away from active site & return to its extended direction → combine with a new active site → new power stroke
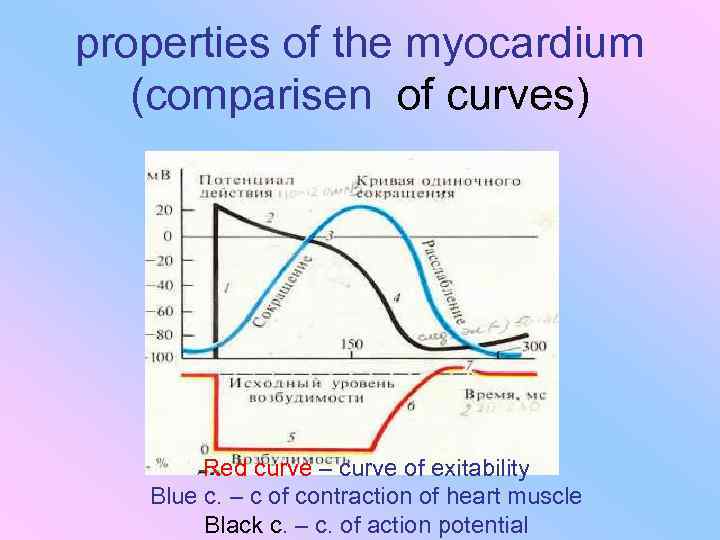
properties of the myocardium (comparisen of curves) Red curve – curve of exitability Blue c. – c of contraction of heart muscle Black c. – c. of action potential
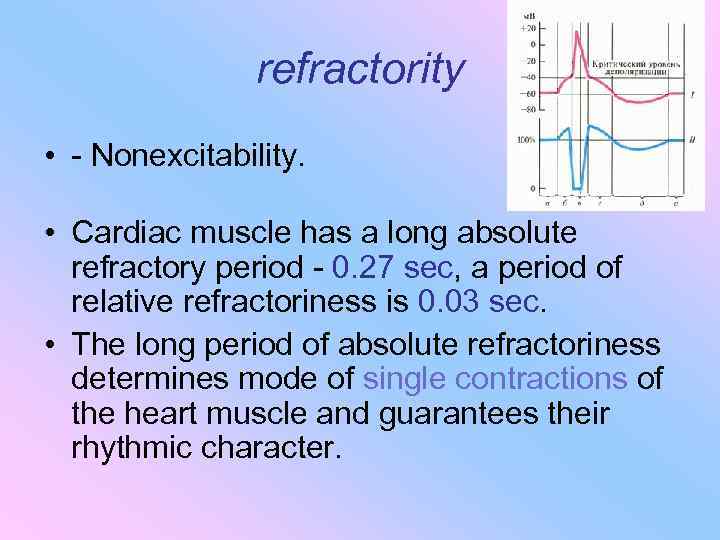
refractority • - Nonexcitability. • Cardiac muscle has a long absolute refractory period - 0. 27 sec, a period of relative refractoriness is 0. 03 sec. • The long period of absolute refractoriness determines mode of single contractions of the heart muscle and guarantees their rhythmic character.
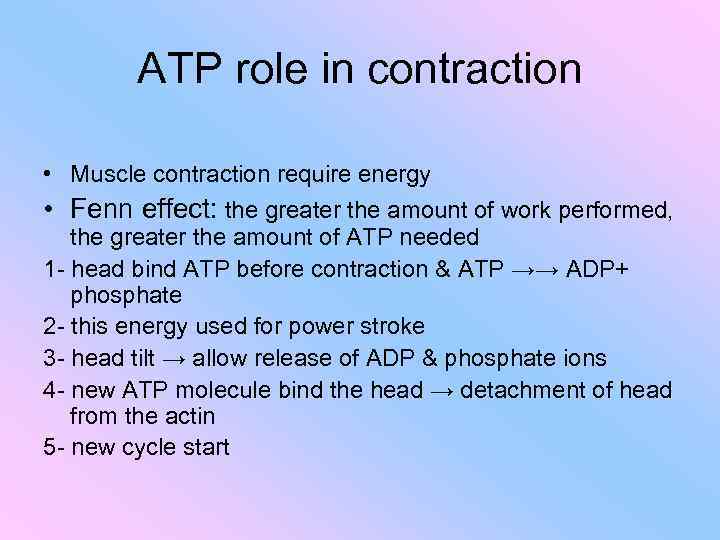
ATP role in contraction • Muscle contraction require energy • Fenn effect: the greater the amount of work performed, the greater the amount of ATP needed 1 - head bind ATP before contraction & ATP →→ ADP+ phosphate 2 - this energy used for power stroke 3 - head tilt → allow release of ADP & phosphate ions 4 - new ATP molecule bind the head → detachment of head from the actin 5 - new cycle start
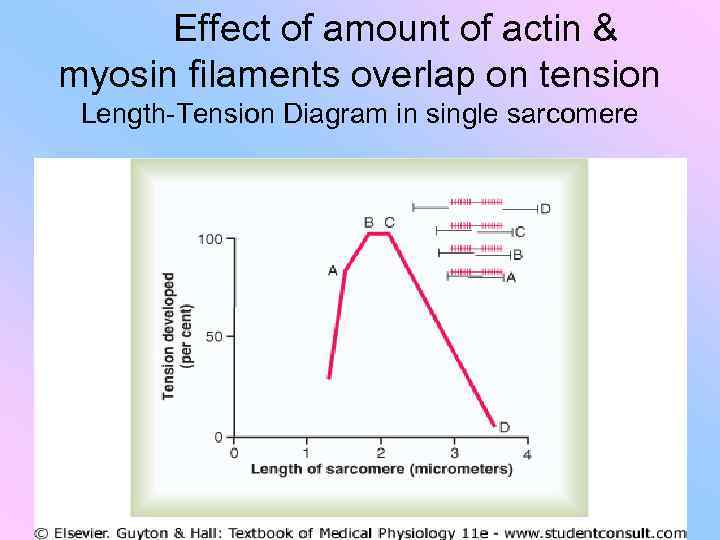
Effect of amount of actin & myosin filaments overlap on tension Length-Tension Diagram in single sarcomere
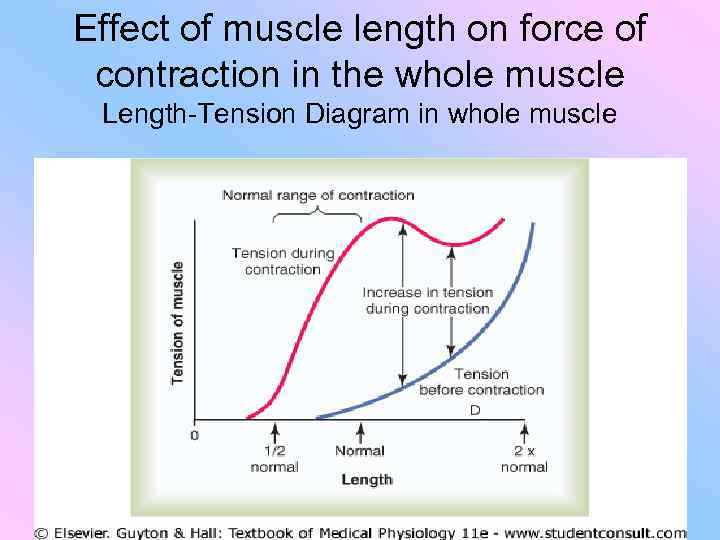
Effect of muscle length on force of contraction in the whole muscle Length-Tension Diagram in whole muscle
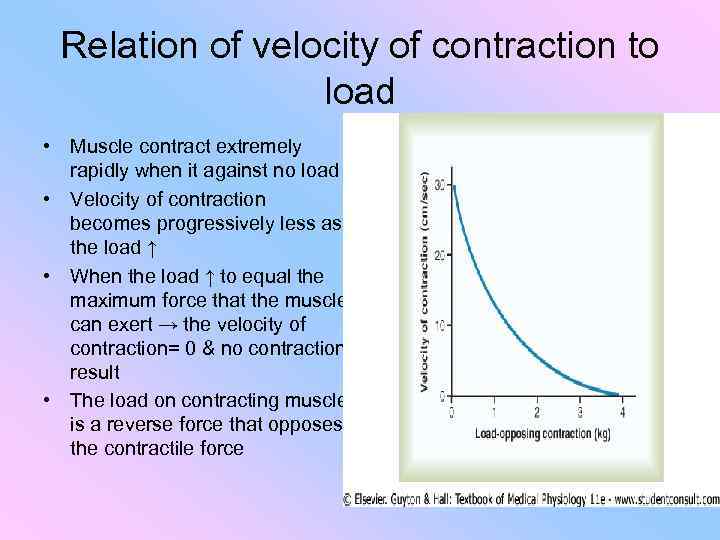
Relation of velocity of contraction to load • Muscle contract extremely rapidly when it against no load • Velocity of contraction becomes progressively less as the load ↑ • When the load ↑ to equal the maximum force that the muscle can exert → the velocity of contraction= 0 & no contraction result • The load on contracting muscle is a reverse force that opposes the contractile force
Work output during contraction • When a muscle contracts against a load, it perform work • W= L* D
Sources of energy for contraction • Most of ATP is used for walk-along mechanism • Small amount required for: 1 - pumping Ca ions into the sarcoplasmic reticulum 2 - pumping Na & K to maintain appropriate ionic environment for propagation of muscle fiber action potential • ATP is sufficient to maintain full contraction for only 1 to 2 sec. • ATP → ADP + phosphate • ADP is rephosphorylated again to form ATP
Cont. • Sources for rephosphorylation to form ATP: 1 - phosphocreatine: - with ATP cause maximal contraction for 5 to 8 sec. 2 - glycolysis of glucogen: - Contraction for 1 min. 3 - oxidative metabolism: - Combining O 2 with the end products of glycolysis & other cellular foodstuffs - 95% of all energy used by muscles - The foodstuffs that are consumed are carbohydrate, fat and protein - For long-term muscle activity → energy come from fat - For short-term activity → energy come from carbohydrate
Efficiency of muscle contraction • The percentage of energy input that is converted into work instead of heat • The efficiency for muscle contraction is 25%
Characteristics of whole muscle contraction • • - Isometric contraction: Muscle contract against a force transducer Muscle doesn’t shorten Static Tension ↑ Work= 0 Eg: muscle of thigh while standing Isotonic contraction: Tension remain constant Muscle is shorten against fixed load Dynamic Eg: lifting weight
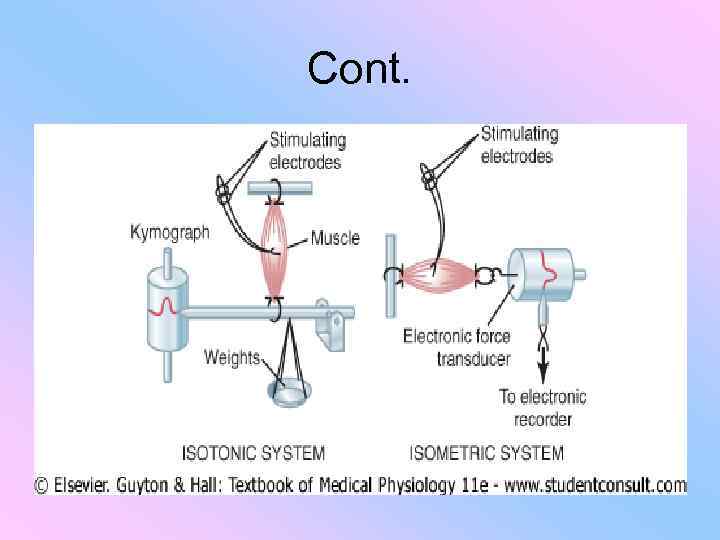
Cont.
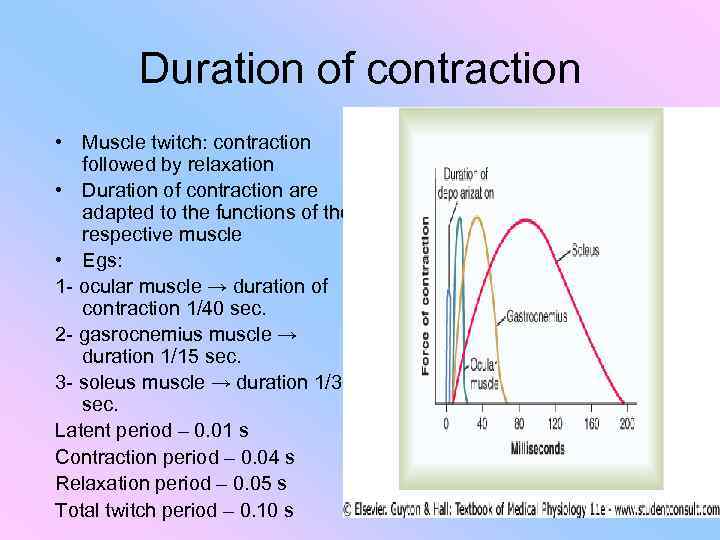
Duration of contraction • Muscle twitch: contraction followed by relaxation • Duration of contraction are adapted to the functions of the respective muscle • Egs: 1 - ocular muscle → duration of contraction 1/40 sec. 2 - gasrocnemius muscle → duration 1/15 sec. 3 - soleus muscle → duration 1/3 sec. Latent period – 0. 01 s Contraction period – 0. 04 s Relaxation period – 0. 05 s Total twitch period – 0. 10 s
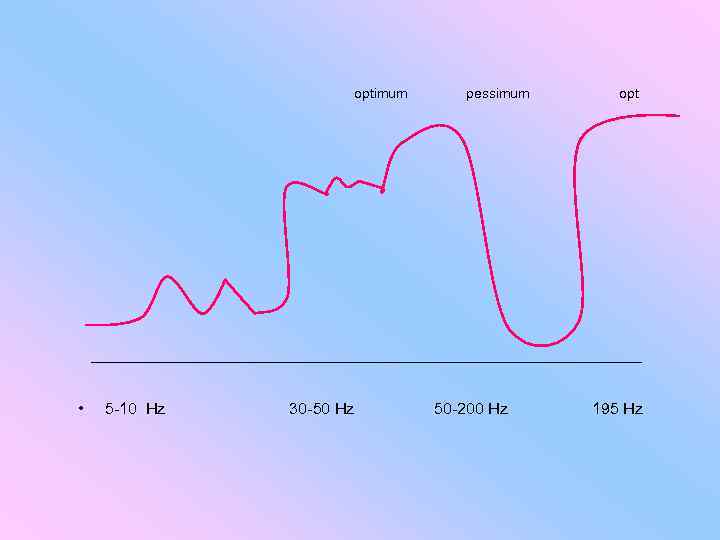
optimum pessimum opt • 5 -10 Hz 30 -50 Hz 50 -200 Hz 195 Hz
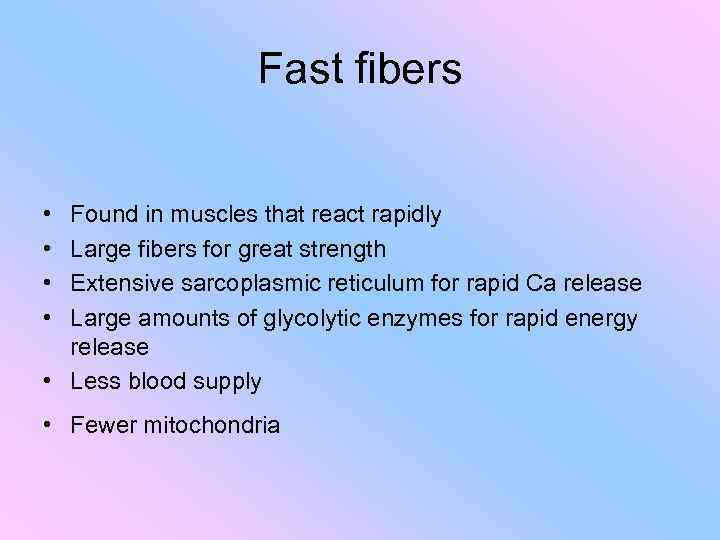
Fast fibers • • Found in muscles that react rapidly Large fibers for great strength Extensive sarcoplasmic reticulum for rapid Ca release Large amounts of glycolytic enzymes for rapid energy release • Less blood supply • Fewer mitochondria
Slow fibers • Found in muscles that react slowly with prolonged contraction • Small fibers • Innervated by smaller nerve fibers • More extensive blood supply to supply O 2 • Great number of mitochondria • Large amounts of myoglobin • Myoglobin combines with O 2 & stores it until needed • Myoglobin give the reddish appearance of those muscle, called red muscle
Mechanics of skeletal muscle contraction Motor unit • Def: all the muscle fibers innervated by a single nerve fiber • In general, small muscles that react rapidly have more nerve fibers for fewer muscle fibers (eg: laryngeal muscles) • Large muscle (eg: soleus muscle) may have several hundred muscle fibers in a motor unit • Muscle fibers in each motor unit overlap other motor units → allow the separate motor units to contract in support of one another
Force summation • Def: adding together of individual twitch to ↑ the intensity of overall contraction • Occur in 2 ways: 1 - multiple fiber summation: - ↑Ing the number of motor units contracting simultaneously - The features of summation: A- size principle: - Weak signals can stimulate smaller motor units - As strength of signals ↑ → large units can be excited - The cause is smaller motor units are driven by small motor nerve fibers which are easier to be excited B- driven asynochronously: - Contraction alternate among motor units one after the other → provide smooth contraction even at low frequencies
2 - frequency summation & tetanization • ↑Ing frequency of contraction which lead to tetanization • As the frequency ↑→ the 2 nd contraction is added partially to the 1 st → the total strength of contraction ↑ progressively with ↑ing frequency • When the frequency reach critical level → the contractions become so rapid → fuse together (tetanization) • At slightly higher frequency, the strength of contraction reach its maximum → any additional ↑ in frequency has no further effect in increasing contractile force
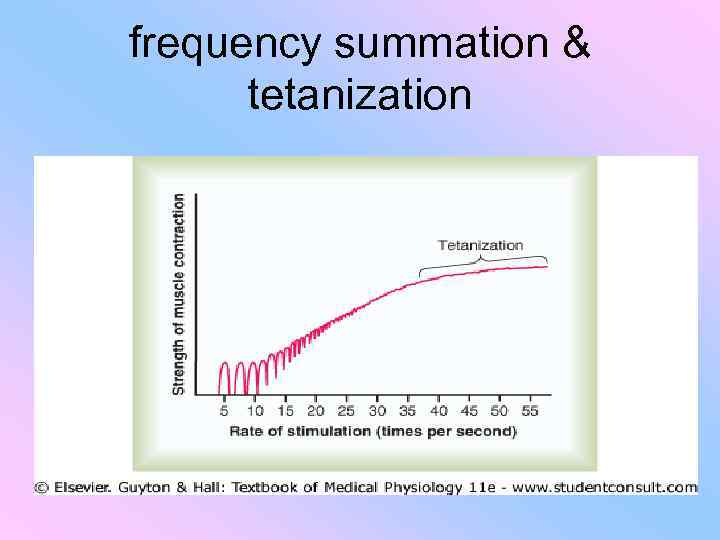
frequency summation & tetanization
Stair case effect (Treppe) • The initial strength of contraction after a long period of rest is less than that after 10 to 50 muscle twitches later • The strength of contraction ↑ to a plateau, called stair effect (Treppe) • Caused by ↑ing Ca ions in cytosol because of the release of more & more ions from the sarcoplasmic reticulum
Skeletal muscle tone • Even when muscle at rest, amount of tautness still remain • Result from low rate nerve impulses coming from spinal cord • Controlled by signals transmitted from the brain & signals that originate in muscle spindles
Muscle fatigue • Caused by prolonged & strong contraction of muscle • ↑ In direct proportion to the rate of depletion of muscle glycogen • Causes: 1 -inability of contractile & metabolic processes to continue supplying the same work output 2 - transmittion of nerve signals ↓ 3 - blood supply ↓
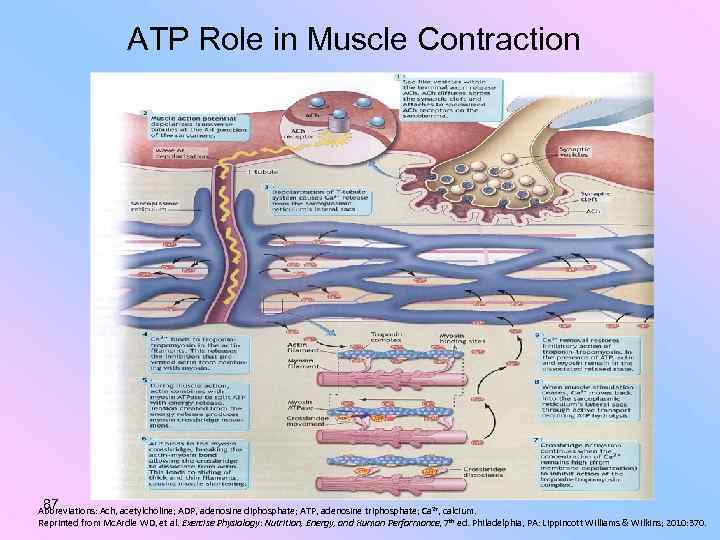
ATP Role in Muscle Contraction 87 Abbreviations: Ach, acetylcholine; ADP, adenosine diphosphate; ATP, adenosine triphosphate; Ca 2+, calcium. Reprinted from Mc. Ardle WD, et al. Exercise Physiology: Nutrition, Energy, and Human Performance, 7 th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010: 370.
Coactivation of agonist & antagonist muscles • All body movements are caused by simultaneous contraction of agonist & antagonist muscle on the opposite sides of joints, called coactivation • Controlled by motor control center in brain & spinal cord • The position of each separate part of the body is determined by the relative degrees of contraction of agonist & antagonist sets of muscles • Eg: place of arm or leg in midrange position • By varying the ratios of the degree of activation of the agonist & antagonist muscles, the nervous system directs the positioning of arm or leg
Remodelling of muscle to match function • Hypertrophy: - ↑ Total body mass - Result from ↑ the number of actin & myosin filaments - Occur when the muscle is loaded during the contractile process - ↑ The enzymes that provide energy (specially for glycolysis) • Atrophy: - ↓ The total body mass - The rate of decay of contractile proteins is more than the rate of replacement
Cont. • Hyperplasia: - ↑ The number of fibers - Rare condition • Adjustment of muscle length: - Hypertrophy →new sarcomeres to be added at the ends of the muscle fibers where they attach to the tendons - The opposite occur in atrophy • Muscle denervation: - Lose of nerve supply →no signals for contraction → atrophy - Muscle fibers destroyed → replaced by fibrous & fatty tissue → shortening of muscles → contracture
Rigor Mortis • All muscles of the body go into contracture after death • This result from loss of ATP, which required to cause separation of cross-bridges to cause relaxation
Situational problem • Muscle of nerve-muscle preparation is subjected to indirect stimulation. • After a while the amplitude of the contractions began to diminish. • Does this mean that the muscle fatigue occurred? How is test this hypothesis? • response • To answer this question, we must go to the direct stimulation of muscles. • If the amplitude of contractions increased, there was no fatigue in the muscle, and was fatigue in the synapse

THANKS
3 мыш сокращение 2014-2015 англ.ppt