462aa24156541ac02902afcfadb2c7d6.ppt
- Количество слайдов: 96
Mild Traumatic Brain Injury (m. TBI) – A Silent Epidemic – Applications for Clinical Practice Patricia S. Benfield, MHDL, CRT, CBIS-CI, CCAA North Carolina Biofeedback Society’s 2012 Conference Greensboro, NC November 2 -4, 2012
Outline Brain development Overview of TBI-definitions & epidemiology Mechanics of brain trauma Review study results Implications for treatment Better assessments & making referrals
Traumatic brain injury is the most misunderstood, misdiagnosed, underfunded public health problem our nation faces. ” Susan Connors, President Brain Injury Association of America
With more than 100 billion neurons and billions of other specialized cells, the human brain is a marvel of nature. It is the organ that makes people unique.
Brain Development
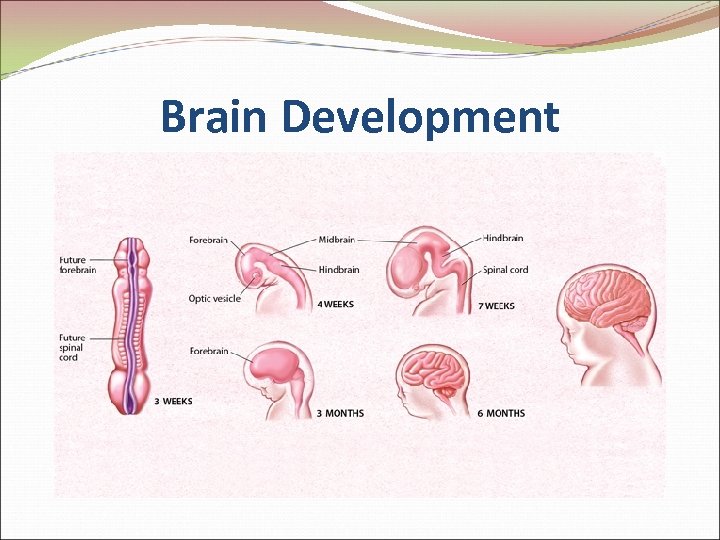
Brain Development
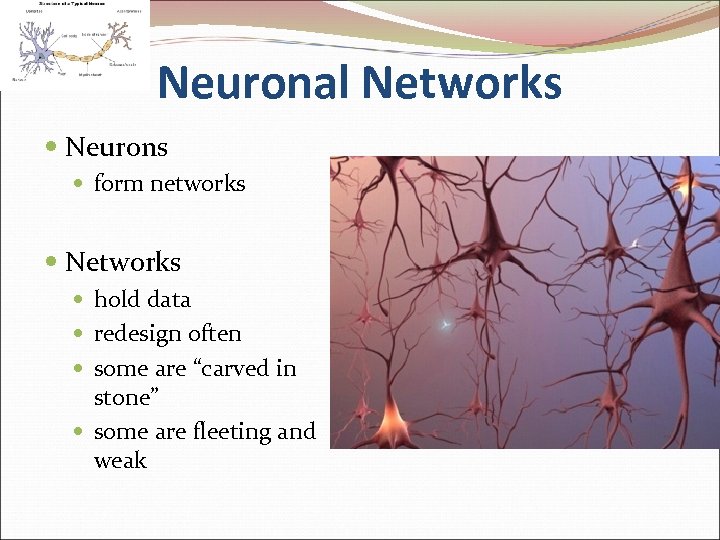
Neuronal Networks Neurons form networks Networks hold data redesign often some are “carved in stone” some are fleeting and weak
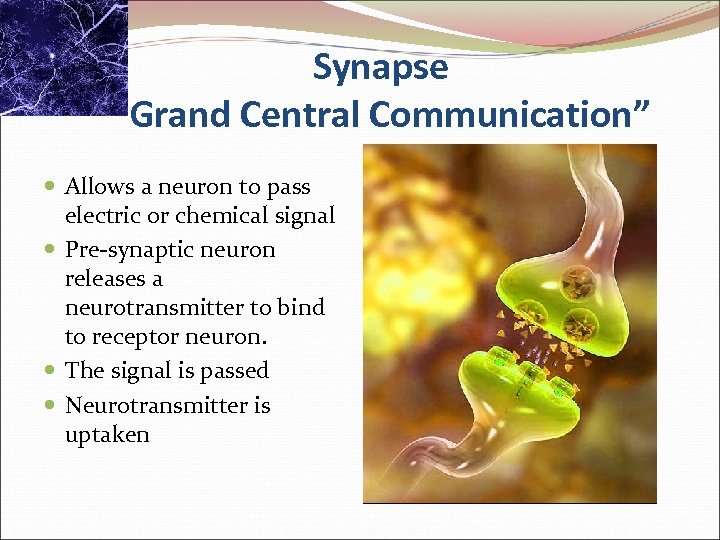
Synapse “Grand Central Communication” Allows a neuron to pass electric or chemical signal Pre-synaptic neuron releases a neurotransmitter to bind to receptor neuron. The signal is passed Neurotransmitter is uptaken
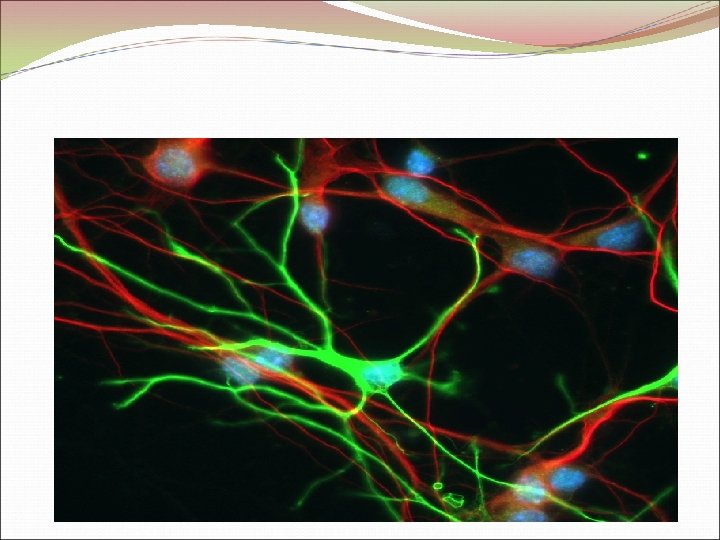
Glial Cells
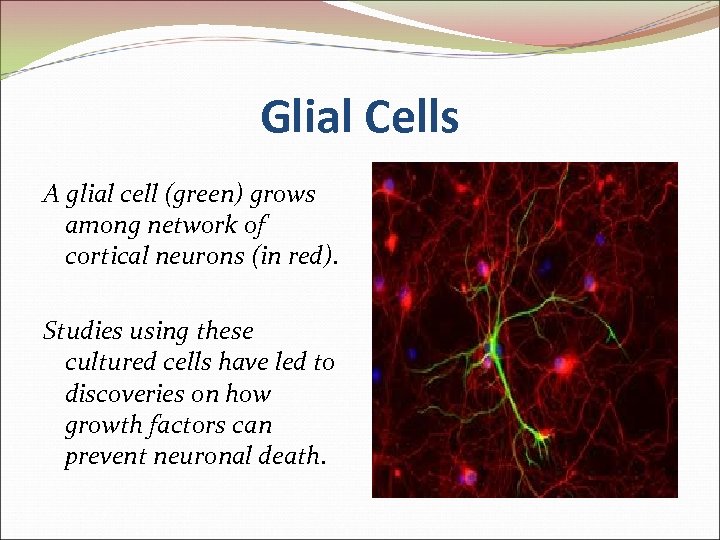
Glial Cells A glial cell (green) grows among network of cortical neurons (in red). Studies using these cultured cells have led to discoveries on how growth factors can prevent neuronal death.
Glial Cells – Structural Support
Glial Cells – Brain’s Supervisors

Pax 6 - Master Regulator of Brain Development
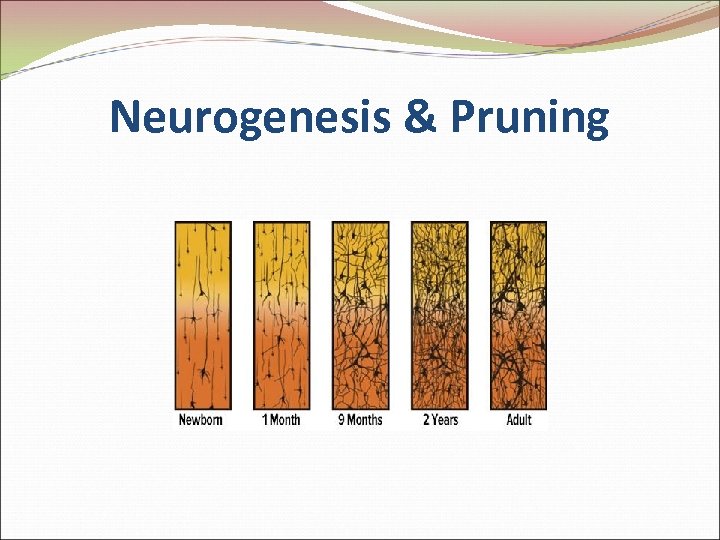
Neurogenesis & Pruning
Making Connections

Making Connections
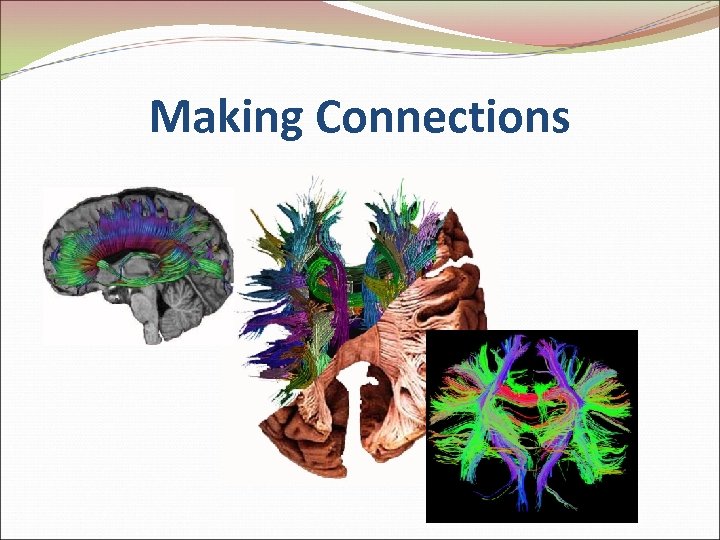
Making Connections
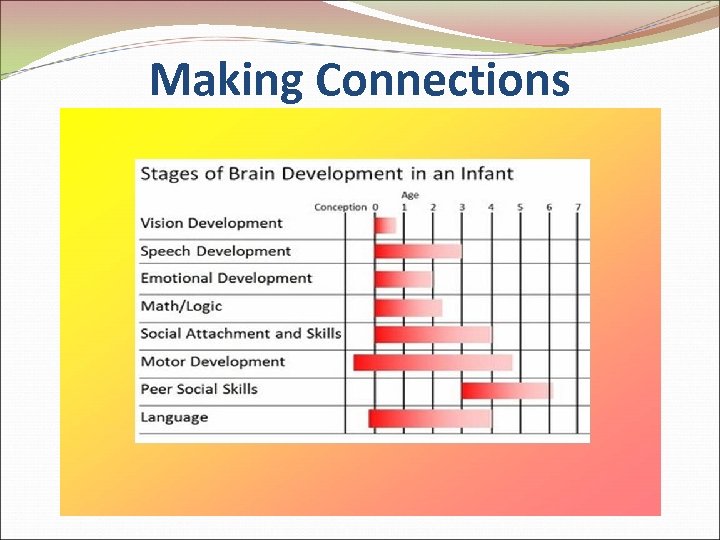
Making Connections
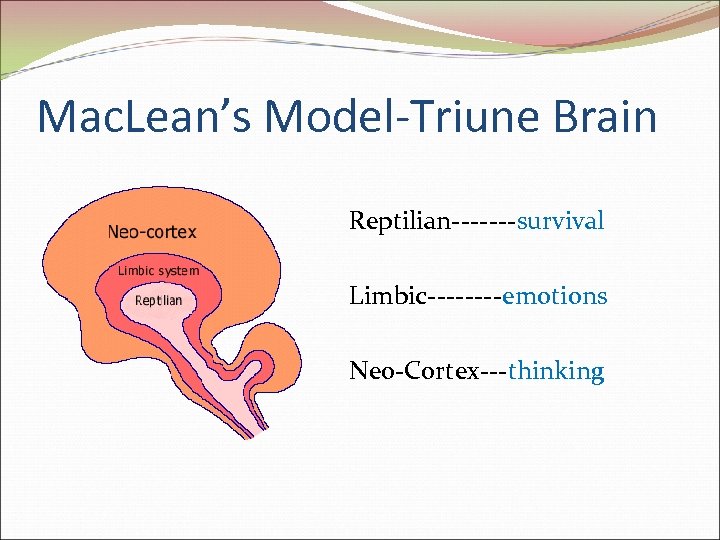
Mac. Lean’s Model-Triune Brain Reptilian-------survival Limbic----emotions Neo-Cortex---thinking
Triune Brain-Reptilian Oldest part Survival or “Fight or Flight” Acts without thinking Threats, real or perceived, causes “downshifting to occur
Triune Brain-Limbic Home of emotions Has visual memory Threat to our well-being will cause “downshifting” Long-term memory
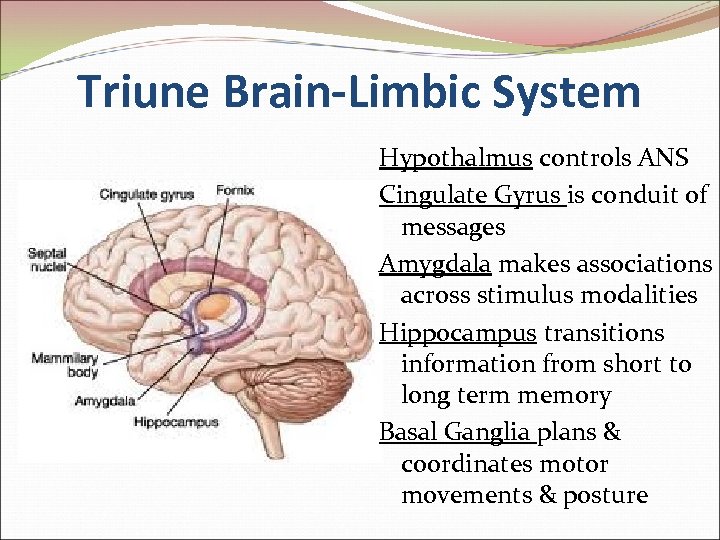
Triune Brain-Limbic System Hypothalmus controls ANS Cingulate Gyrus is conduit of messages Amygdala makes associations across stimulus modalities Hippocampus transitions information from short to long term memory Basal Ganglia plans & coordinates motor movements & posture
Triune Brain-Cortex Thinking & new learning Processes 1, 000 s of bits of information/minute Must be free from threat for new learning or will downshift into its more primitive parts

Maslow’s Needs Basic needs must be met in order to reach the highest order of development
Brain Injury
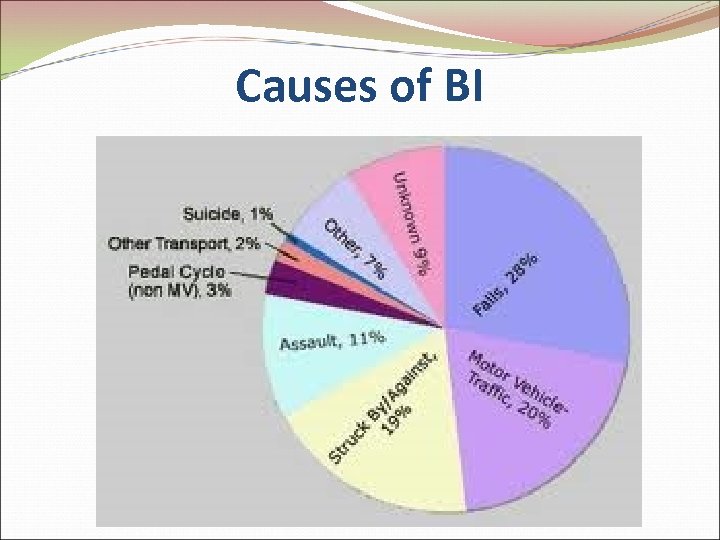
Causes of BI
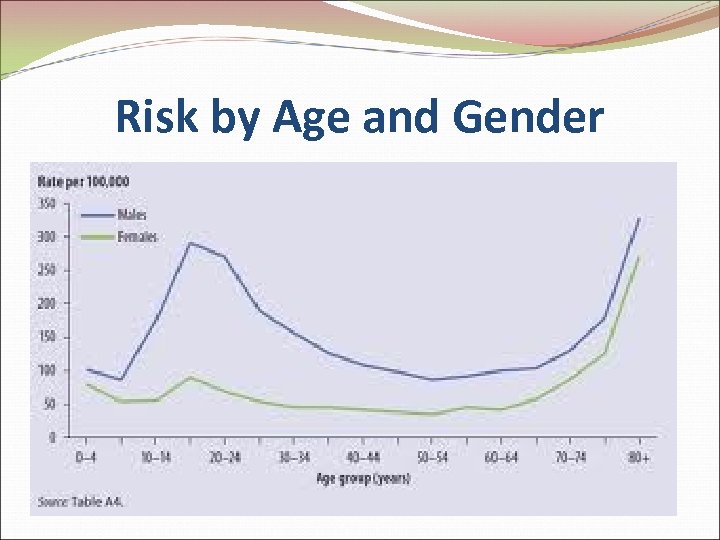
Risk by Age and Gender
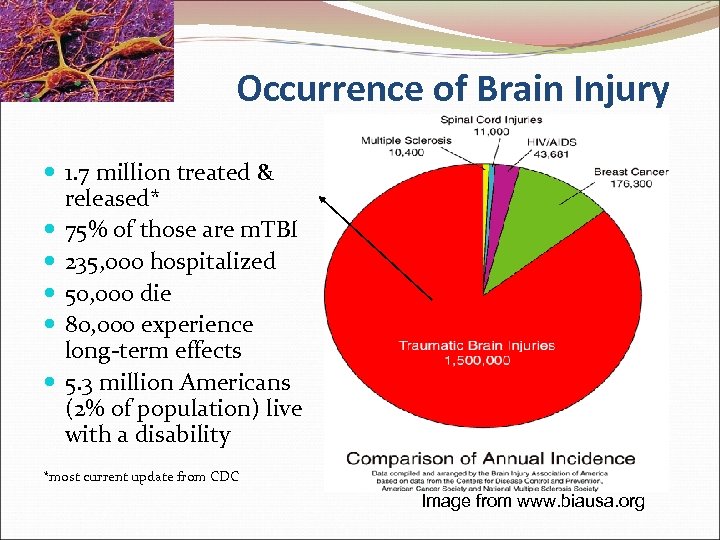
Occurrence of Brain Injury 1. 7 million treated & released* 75% of those are m. TBI 235, 000 hospitalized 50, 000 die 80, 000 experience long-term effects 5. 3 million Americans (2% of population) live with a disability *most current update from CDC Image from www. biausa. org
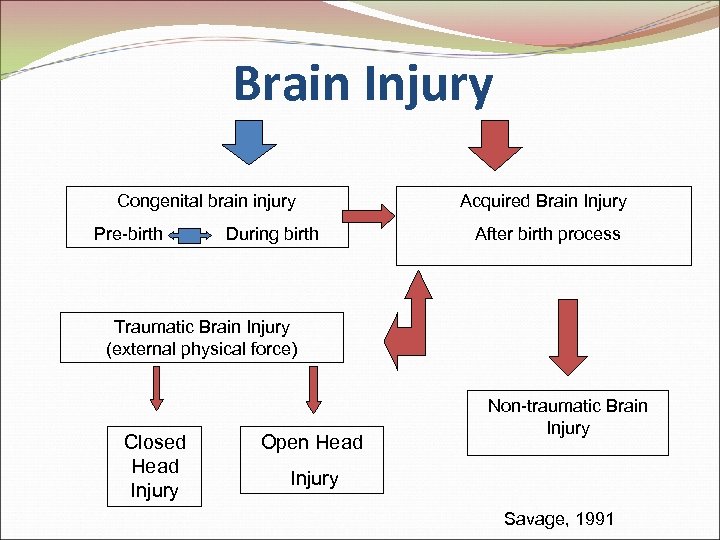
Brain Injury Congenital brain injury Acquired Brain Injury Pre-birth During birth After birth process Traumatic Brain Injury (external physical force) Closed Head Injury Open Head Non-traumatic Brain Injury Savage, 1991
Acquired Brain Injury (ABI) …is an injury to the brain that has occurred after birth and is not related to congenital defect or degenerative disease. Causes of ABI include (but are not limited to) hypoxia, illness, infection, stroke, substance abuse, toxic exposure, trauma, and tumor. …may cause temporary or permanent impairment in such areas as cognitive, emotional, metabolic, motor, perceptual motor and/or sensory brain function. The Brain Injury Network
What is TBI? As of February 6, 2011, BIAA adopts a new definition TBI is defined as an alteration in brain function, or other evidence of brain pathology, caused by an external force.
2 Types of TBI Two major types: Penetrating brain injuries 2. Closed head injuries 1.
Type of TBI-Penetrating Foreign object enters brain (e. g. bullet) Damage occurs along path of injury Symptoms vary according to part of brain that is damaged
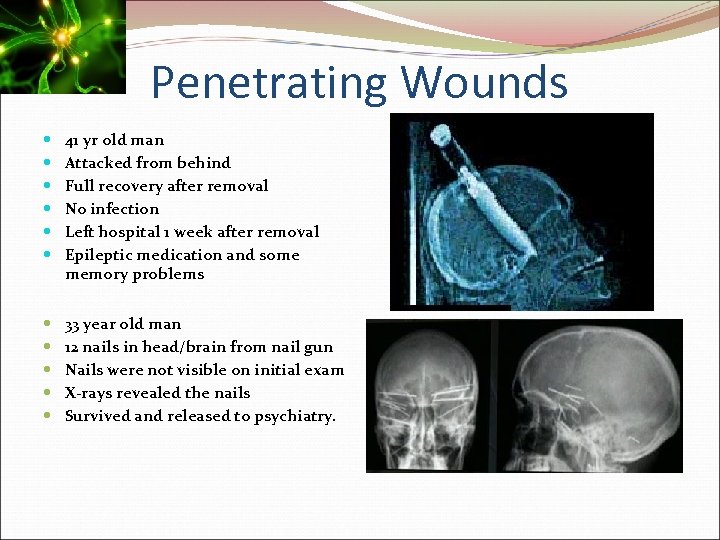
Penetrating Wounds 41 yr old man Attacked from behind Full recovery after removal No infection Left hospital 1 week after removal Epileptic medication and some memory problems 33 year old man 12 nails in head/brain from nail gun Nails were not visible on initial exam X-rays revealed the nails Survived and released to psychiatry.
Type of TBI-Closed Head Injury Results from blow to the head (e. g. car accident or assault) Causes two type of brain injuries: 1. Primary 2. Secondary
2 Types of Closed Head Injury Primary Direct trauma to brain and vascular structures Examples: contusions, hemorrhages, and other direct mechanical injury to brain contents (brain, CSF, blood). Secondary Ongoing pathophysiologic processes continue to injure brain for weeks after TBI Primary focus in TBI management is to identify and limit or stop secondary injury mechanisms
Primary Closed Head Injury Skull fracture: breaking of the bony skull Contusions/bruises: often occur right under the location of impact or at points where the force of the blow has driven the brain against the bony ridges inside the skull Hematomas/blood clots: occur between the skull and the brain or inside the brain itself Lacerations: Tearing of the frontal (front) and temporal (on the side) lobes or blood vessels of the brain ---(the force of the blow causes the brain to rotate across the hard ridges of the skull, causing the tears) Nerve damage (diffuse axonal injury): Arises from a cutting, or shearing, force from the blow that damages nerve cells in the brain's connecting nerve fibers (www. asha. org)
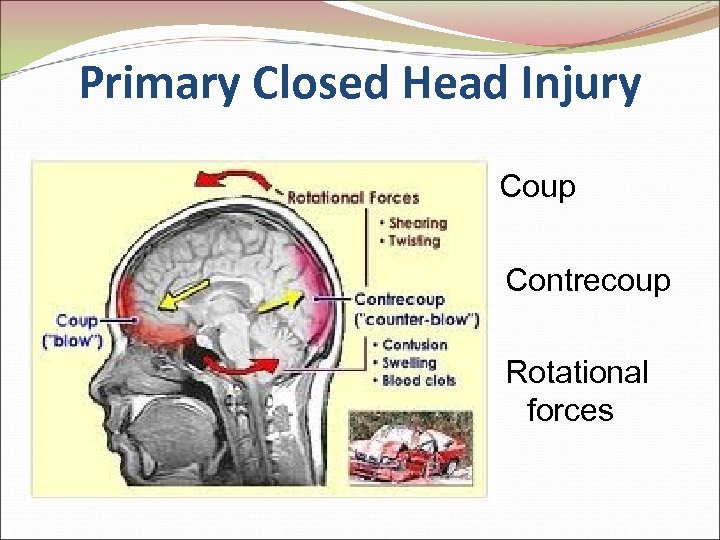
Primary Closed Head Injury Coup Contrecoup Rotational forces
Secondary Closed Head Injury Evolves over time (after trauma has occurred) brain swelling (edema) increased pressure inside of the skull (intracranial pressure) epilepsy intracranial infection fever hematoma (for more info visit: www. asha. org)
TBI – Signature Injury of War Operation Iraqi Freedom (OIF) and Operation Enduring Freedom (OEF) Most service related TBI caused by blast injuries 66% of service personnel in Iraq are exposed to or injured by a blast injury
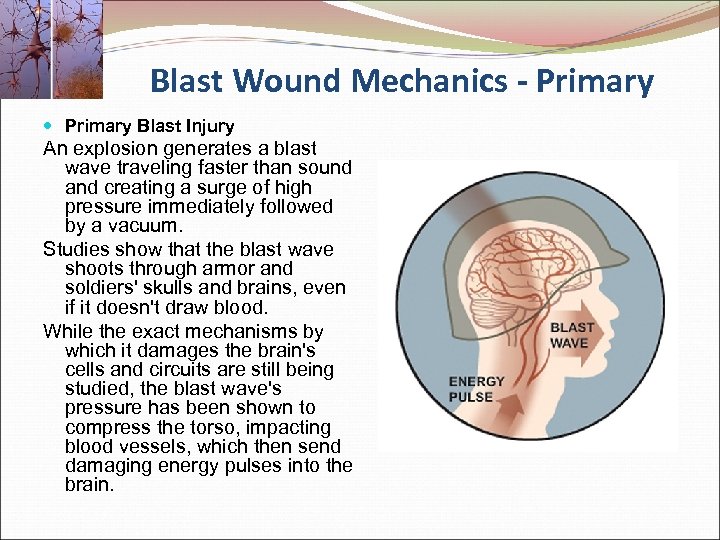
Blast Wound Mechanics - Primary Blast Injury An explosion generates a blast wave traveling faster than sound and creating a surge of high pressure immediately followed by a vacuum. Studies show that the blast wave shoots through armor and soldiers' skulls and brains, even if it doesn't draw blood. While the exact mechanisms by which it damages the brain's cells and circuits are still being studied, the blast wave's pressure has been shown to compress the torso, impacting blood vessels, which then send damaging energy pulses into the brain.
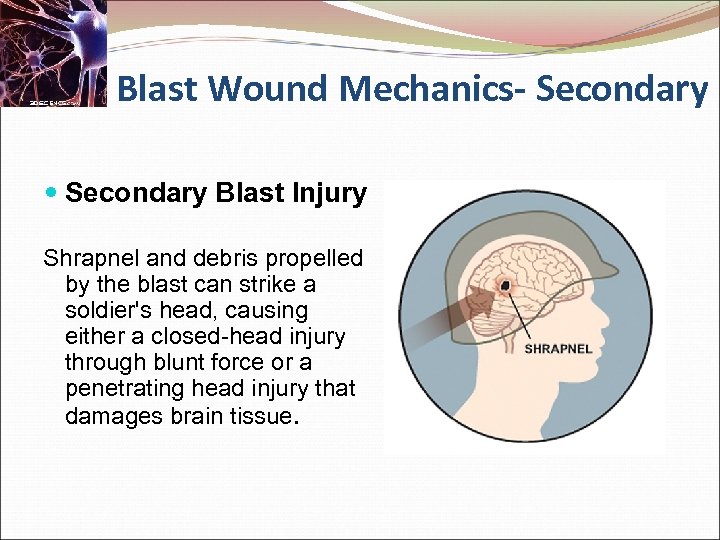
Blast Wound Mechanics- Secondary Blast Injury Shrapnel and debris propelled by the blast can strike a soldier's head, causing either a closed-head injury through blunt force or a penetrating head injury that damages brain tissue.
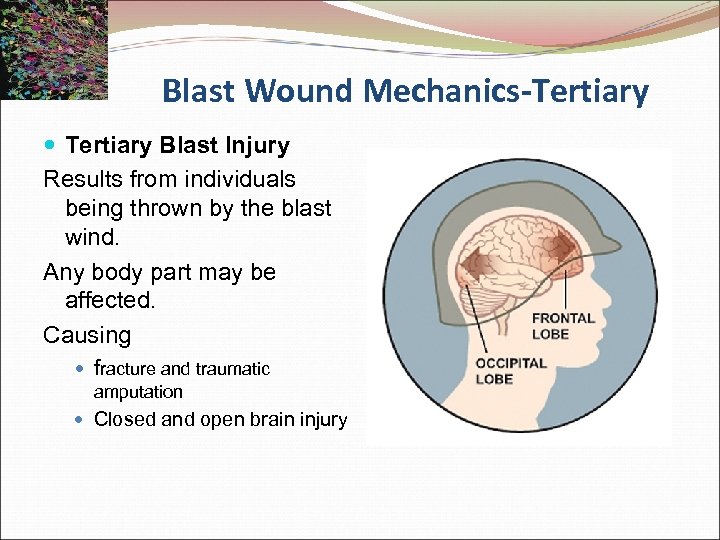
Blast Wound Mechanics-Tertiary Blast Injury Results from individuals being thrown by the blast wind. Any body part may be affected. Causing fracture and traumatic amputation Closed and open brain injury
Blast Wound Mechanics-Quarternary Blast Injury All explosion-related injuries, illnesses, or diseases not due to primary, secondary, or tertiary mechanisms. Includes exacerbation or complications of existing conditions. Any body part may be affected. Includes Burns (flash, partial, and full thickness) Crush injuries Closed and open brain injury Asthma, COPD, or other breathing problems from dust, smoke, or toxic fumes Angina Hyperglycemia, hypertension
Review of Explosive-Related Injuries AUDITORY: TM rupture, ossicular disruption, cochlear damage, foreign body EYE, ORBIT, FACE: Perforated globe, foreign body, air embolism, fractures RESPIRATORY: Blast lung, hemothorax, pneumothorax, pulmonary contusion and hemorrhage, A-V fistulas (source of air embolism), airway epithelial damage, aspiration pneumonitis, sepsis DIGESTIVE: Bowel perforation, hemorrhage, ruptured liver or spleen, sepsis, mesenteric ischemia from air embolism CIRCULATORY: Cardiac contusion, myocardial infarction from air embolism, shock, vasovagal hypotension, peripheral vascular injury, air embolism-induced injury CNS INJURY: Concussion, closed and open brain injury, stroke, spinal cord injury, air embolism-induced injury RENAL INJURY: Renal contusion, laceration, acute renal failure due to rhabdomyolysis, hypotension, and hypovolemia CIRCULATORY: Traumatic amputation, fractures, crush injuries, compartment syndrome, burns, cuts, lacerations, acute arterial occlusion, air embolism-induced injury
Statistics on Service Related Injuries 40% of service personnel returning from OIF & OEF show signs & symptoms of TBI due to a blast injury The large majority (80%) of combat head injuries sustained in Operation Iraqi Freedom and Operation Enduring Freedom are mild concussions as opposed to severe, debilitating TBI. National Institute of Neurological Disorders and Stroke. (http: //www. americasheroesatwork. gov)
More on Occurrences of BI Traumatic brain injuries are among the top injuries of soldiers serving in Iraq and Afghanistan, with military estimates of over 200, 000 affected soldiers. Most of these injuries result in concussions, but repeated injuries can result in permanent neurological problems. While a concussion means that the brain swells and heals, those unseen breaks in the fiber pathways can cause problems later in life. Current diagnostic equipment only permits doctors to see swelling or bleeding.
Mild Traumatic Brain Injury (m. TBI) …defined as a loss or alteration of consciousness <30 minutes, post-traumatic amnesia < 24 hours, focal neurologic deficits that may or may not be transient, and/or Glasgow Coma Score (GCS) of 13 -15. …by definition, typically involves symptoms of brain damage but no sign of damage based on a neurological exam Controversy over whether primary blast injuries damage the brain. Animal models suggest they do.
Mild TBI In most cases of m. TBI, the patient returns to their previous level of function within 3 -6 months. 15% of patients may go on to develop chronic postconcussive symptoms.
Chronic Post Concussive Symptoms These symptoms can be grouped into 3 categories 1. Somatic (headache, tinnitus, vertigo, insomnia, etc. ) 2. Cognitive (memory, attention/concentration difficulties, etc. ) 3. Emotional/behavioral (irritability, depression, anxiety, behavioral dyscontrol)
Chronic Post Traumatic Concussions “Concussions can trigger a chemical chain reaction in brain neurons that leaves an athlete disoriented, unconscious, or dead. They can also impair learning over a period of years. ”
Chronic Post Concussive Symptoms Comorbid Psychiatric Disorders-Patients who have experienced m. TBI are also at risk for psychiatric disorders compared to the general population, including depression and PTSD Video-Mild TBI-Magnetoencephalography http: //www/youtube. com/watch? v=uhl. ANIGAJXA
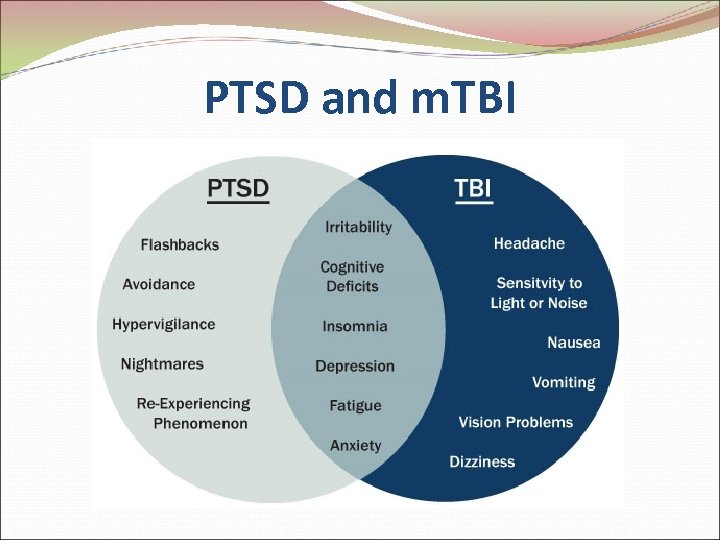
PTSD and m. TBI
Signs of BI Headaches or neck pain that do not go away Difficulty remembering, concentrating, or making decisions Slowness in thinking, speaking, acting, or reading Getting lost or easily confused Increased sensitivity to lights, sounds, or distractions Blurred vision or eyes that tire easily Loss of sense of smell or taste Ringing in the ears (http: //www. cdc. gov/ncipc/factsheets/tbi. htm)
Signs of BI (cont’d) Feeling tired all of the time, having no energy or motivation Mood changes (feeling sad or angry for no reason) Changes in sleep patterns (sleeping a lot more or having a hard time sleeping) Light-headedness, dizziness, or loss of balance Urge to vomit (nausea)
TBI-The Silent Epidemic Results of recent national survey: only 1 in 3 Americans are familiar with term "brain injury. " Rarely associate TBI w/ most common forms of BI-concussions. Brain damage is not visible. No way to assess extent of damage.
Clinical Implications
Studies Provides Evidence for a Need For New Standards in Competent Practice
Mounting Evidence-Studies Links between head injury and mental illness, substance abuse, and criminality (Helgeson, 2010). Approximately 70% w/ co-occurring substance abuse and mental health issues had a history—although not necessarily a diagnosis—of TBI (Corrigan & Deutschle, 2008). 87% of a county jail population reported history of head injury (Slaughter, Fann, & Ehde, 2003).
More Evidence-Comorbidity Symptoms of clinical depression in 15 -40% of survivors (Teasdale & Engberg, 2001). 44% of soldiers returning from Iraq who had clear evidence of m. TBI also experienced PTSD, compared w/ 9% having evidence of PTSD w/ no BI (Hoge et al. , 2008).
More Evidence-Comorbidity Individuals w/ BI were 4 X more likely to attempt suicide than their nonbrain-injured peers (Silver et al. , 2001) Suicide risk is even higher w/ m. TBI group not dx’d or tx’d (Teasdale & Engberg, 2001). These risks are compounded by the co-occurring nature of mental health and substance abuse. 70% of dually-diagnosed reported a hx of TBI—although not necessarily were diagnosed (Corrigan & Deutschle, 2008).
More Evidence-Comorbidity 68% incarcerated for substance-related offenses reported previous head trauma. (Walker, Staton, and Leukefeld, 2001). As high as 87% prevalence of TBI among the populations incarcerated for a range of offenses (Slaughter et al. , 2003). High correlation of TBI to violent criminal behavior, including sexual assault and homicide (Leon-Carrion & Ramos, 2003).
Implications for Clinical Practice Both client/patient and therapist are at risk Ethical responsibility to become better educated about the realities of m. TBI Better and more thorough screening for brain injury Refer clients who report prior head trauma for appropriate evaluation and treatment.
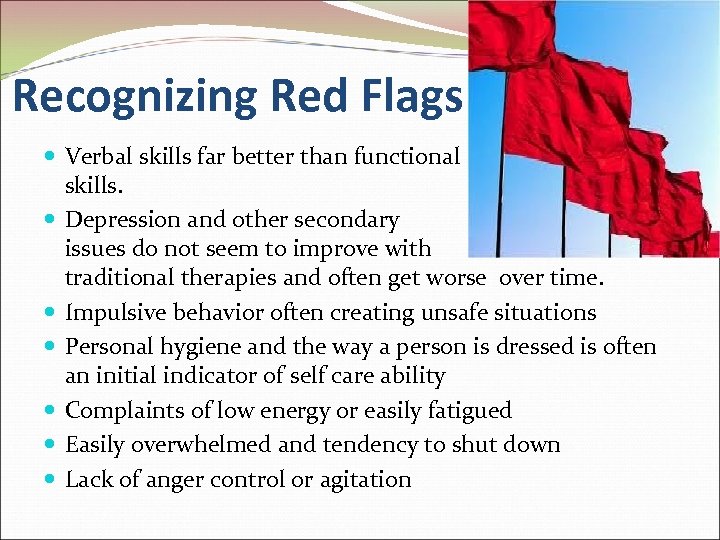
Recognizing Red Flags Verbal skills far better than functional skills. Depression and other secondary issues do not seem to improve with traditional therapies and often get worse over time. Impulsive behavior often creating unsafe situations Personal hygiene and the way a person is dressed is often an initial indicator of self care ability Complaints of low energy or easily fatigued Easily overwhelmed and tendency to shut down Lack of anger control or agitation

More Red Flags Difficult patient Poor memory Poor executive functions Failure to follow through w/o reason although agreeable Failure to progress despite their reasons for attending therapy Getting worse despite treatment especially with prescribed medications Failure to participate in their own treatment Appears to understand but fails to comply Inconsistencies
Some Questions to Ask Have you ever hurt your head or had a head injury that caused you to “see stars” or feel dazed? Have you ever lost consciousness, even momentarily, after hurting your head? After hurting your head, have you ever had headaches, dizziness, or been irritable? Have you ever been diagnosed with a concussion or whiplash, or seen a doctor for a head or neck injury? (Schwab et al. , 2006)
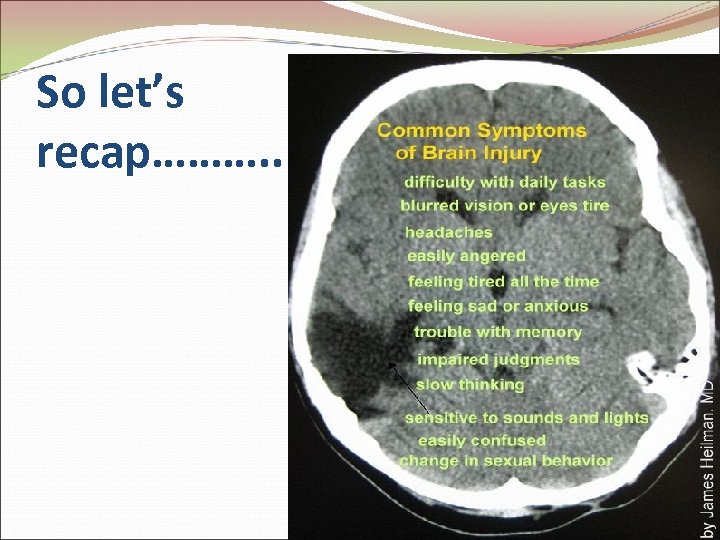
So let’s recap………. .
So Let’s recap…m. TBI… …is a major public health concern, …is difficult to diagnose, …has symptoms that are nearly indistinguishable from other conditions, …has survivors who are often unaware or unwilling to report symptoms, and …is highly correlated with mental health, substance abuse, and criminality.
Rehabilitation Specialists & Counsellors The importance of attending to basic needs, re-training for employment, and social re-involvement must be aligned with the needs of the self, working through the losses, integrating a new sense of purpose and accomplishment.
Possible Barriers to Change Some complexities facing practitioners working with TBI. Lack of awareness Communication Attention/concentration impairment Emotional lability Impulsivity Fatigue Judgement, problem-solving, decision making, & organizational skills Memory Personality disturbance & social isolation Masking
Brain Recovery Brain recovery follows patterns of brain development. Gross or large-scale systems must develop (or be retrained) before fine systems. Attention, focus, and perceptual skills develop (or are retrained) before complex intellectual activity can be successful. Source: NIH Pub. No. 98 -4315
Treating TBI Assessment & diagnosis Address cognitive impairments through retraining & compensatory strategies Biofeedback & neurofeedback Support treatment Education on the nature of their condition Counseling & family support address adjustment issues resolve emotional issues no matter how old the issues are Sleep hygiene for more restorative sleep Brain Perfect Nutrition Daily exercise Medication for symptomatic relief
TBI-The Silent Epidemic “If you cannot see or quantify the damage, it is hard to treat it. ” Dr. Walter Schneider University of Pittsburgh
Treating BI – Diagnosing Extensive case history Screening (BNCE) Formal neuropsychological evaluation by a Neuropsychologist Imaging can be helpful as well as deceptive a normal CT scan mean “no brain bleeding” a normal MRI can mean “no brain parts shifted in skull”
Missed Diagnosis or Misdiagnosis Traditional methods for diagnosing m. HI, i. e. medical history, CAT scan and MRI, often show normal test results even though patients complain of significant neurocognitive dysfunctions. Diagnosis and Treatment of Head Injury by Hoffman DA M. D. , Stockdale S Ph. D. , Hicks LL B. A. , Schwaninger JE B. A.
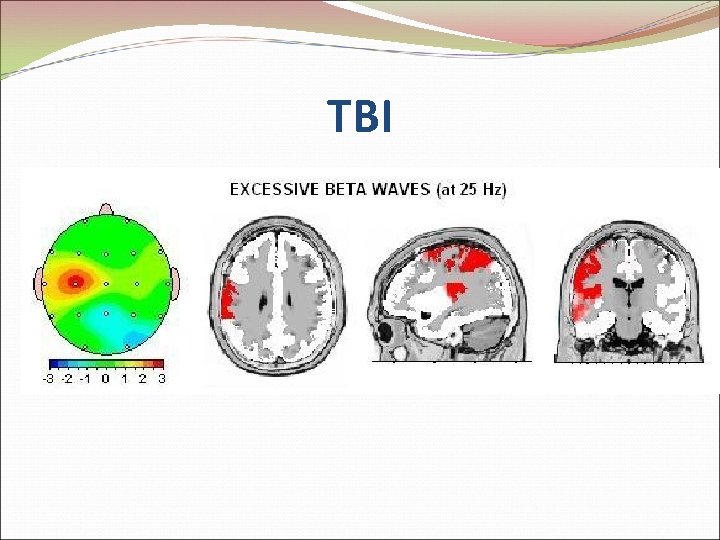
TBI
Using EEG Technology for Treatment National Library of Medicine lists 1, 672 peer reviewed journal articles on the subject of EEG and TBI The vast majority of these studies involved quantitative analyses and, in general, the scientific literature presents a consistent and common quantitative EEG pattern correlated with TBI.
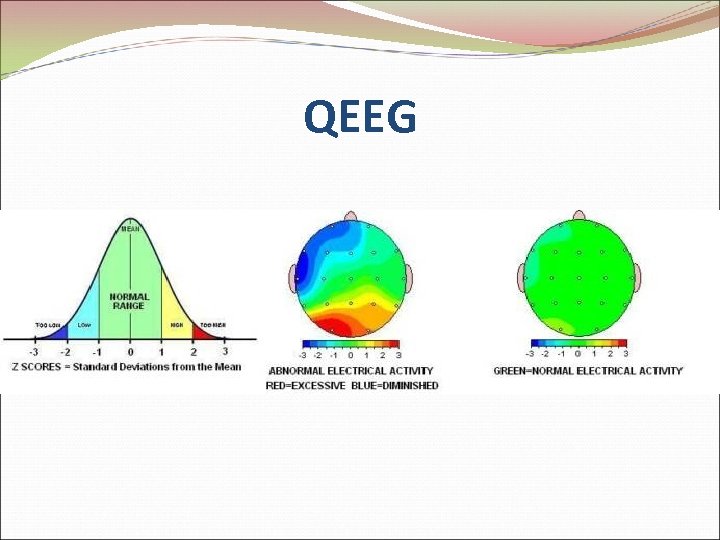
QEEG
q. EEG as a Diagnostic Tool 90 -98% reliability –use of q. EEG for diagnostic purposes (Thatcher et al, 1999; 2003) Strong correlations exist betw/ q. EEG & performance on neuropsychological tests (Thatcher et al, 1998 a; 1998 b; 2001 a; 2001 b)
BI Research - EEG & NF Studies for Treatment Memory, attention and response accuracy during problem solving tasks (Tinius & Tinius, 2000) 88% of m. HI had 50% improvement in EEG coherence scores & all who were employed pre-injury reported RTW following tx (Walker, Norman, & Weber, 2002) Improved cognitive functioning & self-reports of depression & fatigue (Schoenberger, Shif, Esty, Ochs, & Matheis, 2001) Beta feedback improved attention deficits compared to controls (Keller, 2001)
Treating Comorbid and Other Conditions
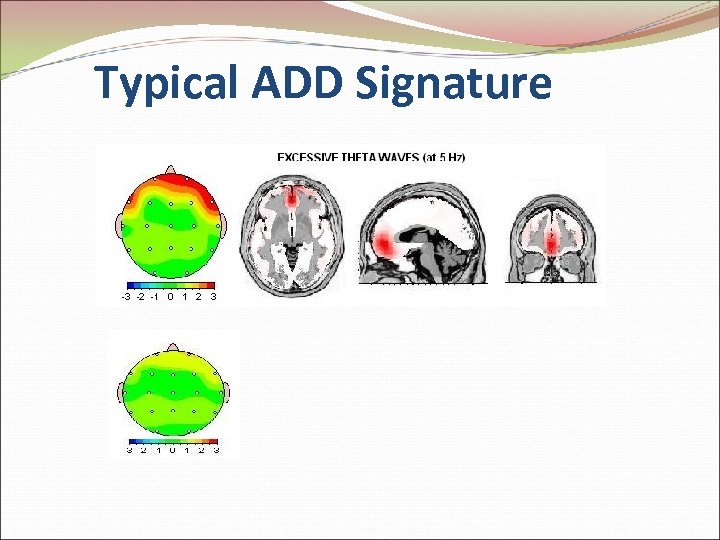
Typical ADD Signature
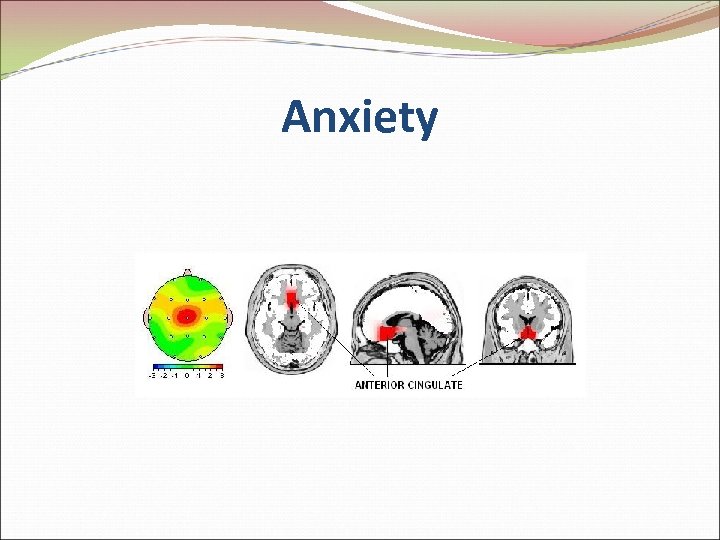
Anxiety
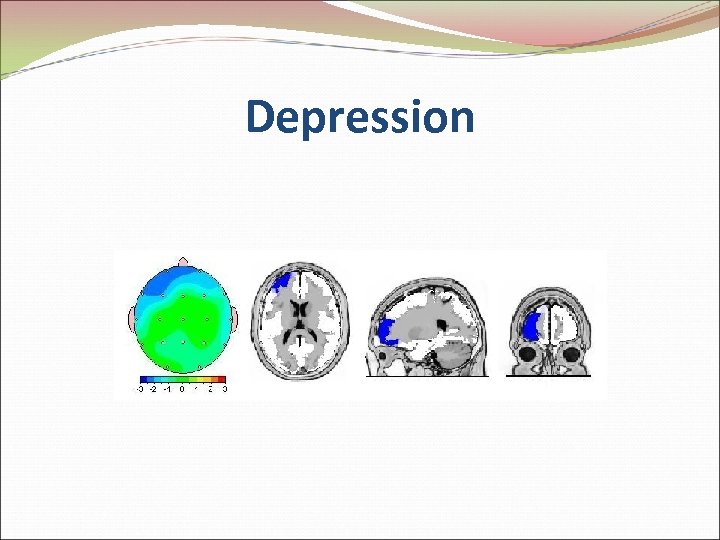
Depression
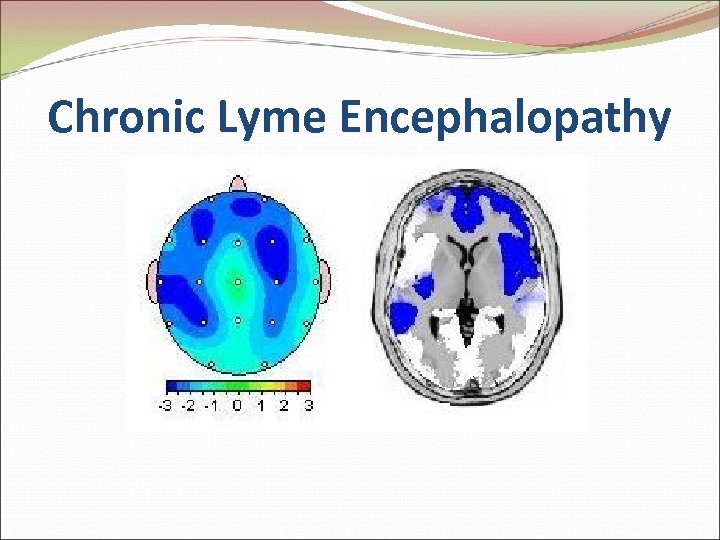
Chronic Lyme Encephalopathy
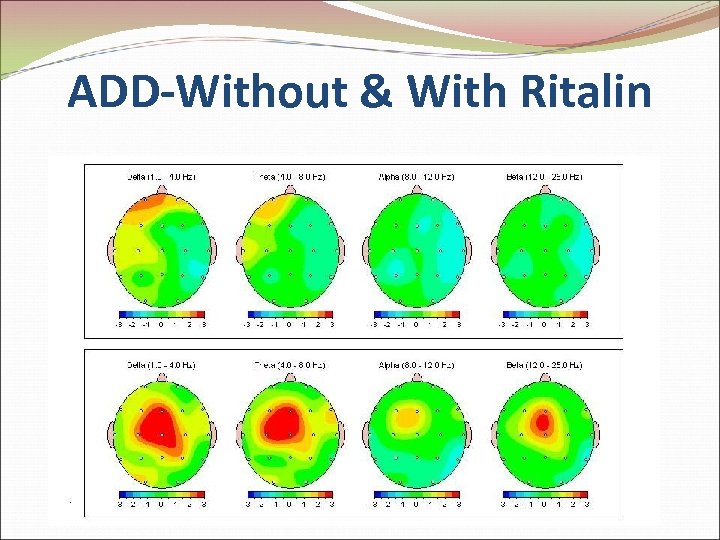
ADD-Without & With Ritalin
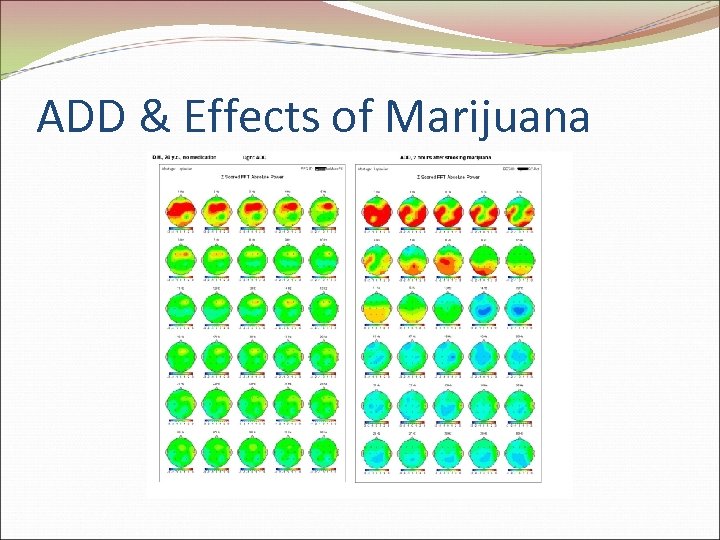
ADD & Effects of Marijuana
Neurofeedback …has been proven so effective in treating TBI that the Texas Legislature recently passed a law preventing insurance companies from denying coverage for it if the patient is being treating for TBI. Another effort is currently under way to lobby the State to mandate the same coverage for those being treated autism spectrum disorders.
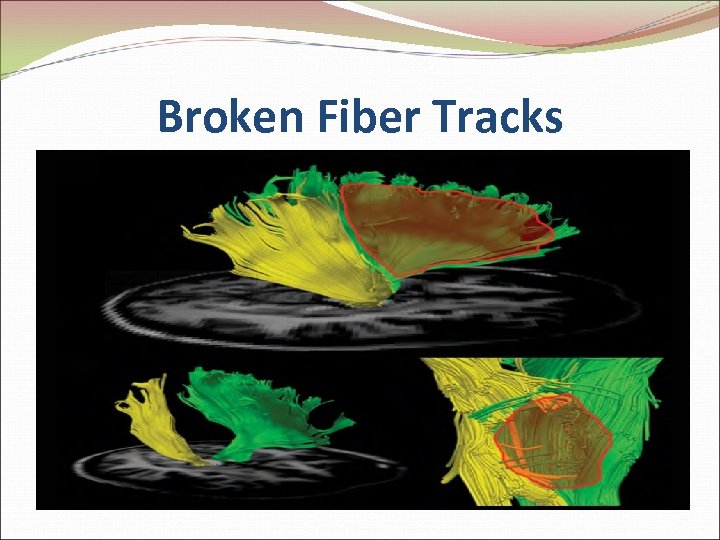
Broken Fiber Tracks
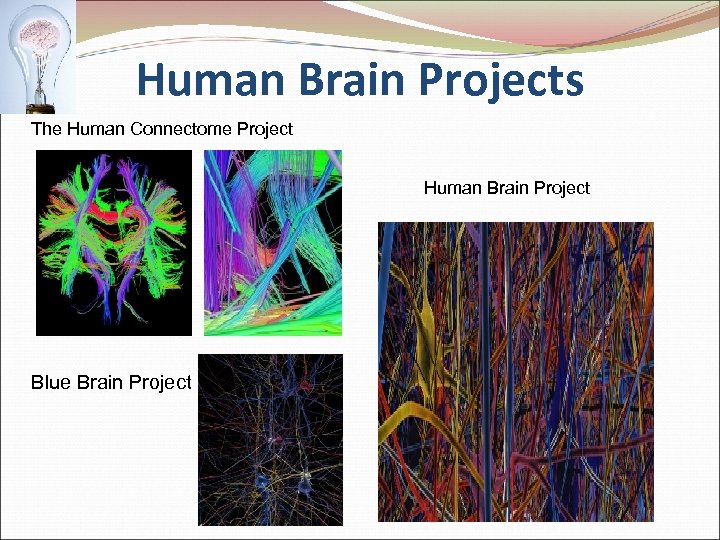
Human Brain Projects The Human Connectome Project Human Brain Project Blue Brain Project
References Buck, P. W. (2011). Mild traumatic brain injury: A silent epidemic in our practices. Health & Social Work, 36(4), 299 -302. Corrigan, J. D. , & Deutschle, J. J. (2008). The presence and impact of traumatic brain injury among clients in treatment for co-occurring mental illness and substance abuse. Brain Injury, 223 -231. Helgeson, S. R. (2010). Identifying brain injury in state juvenile justice, corrections, and homeless populations: Challenges and promising practices. Brain Injury Professional, 7(4), 18 -20.
References (cont’d) Hoge, C. W. , Mc. Gurk, D. , Thomas, J. L. , Cox, A. L. , Engel, C. C. , & Castro, C. A. (2008). Mild traumatic brain injury in US soldiers returning from Iraq. New England Journal of Medicine, 358, 453 -463. Leon-Carrion, J. , & Ramos, F. J. (2003). Blows to the head during development can predispose to violent criminal behaviour: Rehabilitation of consequences of head injury is a measure for crime prevention. Brain Injury, 17, 207 -216.
References (cont’d) Silver, J. M. , Kramer, R. , Greenwald, S. , & Weissman, M. (2001). The association between head injuries and psychiatric disorders: Findings from the new Haven NIMH Epidemiologic Catchment Area Study. Brain Injury, 15, 935 -945. Slaughter, B. , Fann, J. R. , & Ehde, D. (2003). Traumatic brain injury in a county jail population: Prevalence, neuropsychological functioning and psychiatric disorders. Brain Injury, 17, 731 -741. Teasdale, T. W. , & Engberg, A. W. (2001). Suicide after traumatic brain injury: A population study. Journal of Neurology, Neurosurgery & Psychiatry, 71, 436 -440.
References (cont’d) Thatcher, R. , Walker, B. , Biver, C. , North, M. , Curtin, R. (2003). Sensitivity and specificity of an EEG normative data base: Validation and clinical correlation. Journal of Neurotherapy, 7 (3/4): 87121. Walker, R. , Staton, M. , & Leukefeld, C. G. (2001). History of head injury among substance users: Preliminary findings. Substance Use & Misuse, 36, 757 -770.
References (cont’d) Thatcher, R. , Lubar, J. (2009). History of the scientific standards of QEEG normative databases. In Budzynski, T. , Budzynzki, H. , Evans, R. , Abarbanel, A. (Eds). Introduction to Quantitative EEG and Neurofeedback: Advanced Theory and Applications, 2 nd Edition. (pp. 29 -62). New York, NY: Academic Press. Thatcher, R. , Walker, B. , Biver, C. , North, M. , Curtin, R. (2003). Sensitivity and specificity of an EEG normative data base: Validation and clinical correlation. Journal of Neurotherapy, 7 (3/4): 87 -121. Tramontano, G. (2006). QEEG testing can discern reason for cognitive disorder: Digital EEG recordings of brainwaves can determine TBI etiology. Connecticut Lawyer, March 2006, pp. 14 -16.
462aa24156541ac02902afcfadb2c7d6.ppt