MICROFLORA_AND_SANITARY-INDICATIVE_BACTERIA_OF_SOIL_WATER.pptx
- Количество слайдов: 51
MICROFLORA AND SANITARYINDICATIVE BACTERIA OF THE SOIL, WATER, AIR THE METHODS OF STUDYING
Microorganisms are widespread. Microbes are distributed everywhere in the environment surrounding us. They are found in the Ø Soil Ø Water Ø Air Ø Plants Ø Animals Ø Food products Ø In the human body and on the surface of the human body
The environment is a transmission factor of infectious diseases. Potentially pathogenic and pathogenic microorganisms get to environment mainly, in 2 ways: 1) fecal (with excrement from the intestine) 2) airborne (with droplets of mucus from the respiratory tract) Thus sanitary-microbiological investigations are performed for study and evaluation of different objects for determination of their epidemic potential.
Sanitary microbiology is a science that studies the microflora of the environment and its harmful effect on the human body. Methods for sanitary-microbiological investigation include: 1) determination of a total microbial contamination 2)detection and titration of sanitary-indicative microorganisms 3)detection of pathogenic microorganisms and/or their metabolites
Direct detection of pathogenic microorganisms in the different objects of environment, in general, is complicated because of their small quantity, their temporarily staying in the environment and the duration and laboriousness of methods for their determination. Thus indirect methods of detection of microbial contamination are used: 1) total microbial contamination as indicator of intensity of contamination by organic substances; 2) contamination by sanitary- indicative microorganisms.
Total viable count (TVC) is used for evaluation of total microbial contamination. TVC is the number of microbes in 1 ml of water, 1 g of soil , in 1 m 3 of air.
Sanitary-indicative microorganisms (SIMs) or sanitaryindicative bacteria are used for indirect evaluation of possible presence of pathogens in the environment. SIMs features: Ø are representatives of normal human microflora and homeothermic animals and do not have other habitats Ø get to environment the same ways (fecal and airdrop), as pathogenic m/o Ø the same terms are maintained, as pathogenic m/o Ø its number is constant (they do not multiply in the environment) Ø methods for determining them are easy and affordable Ø have stable and typical properties, so they are easily identified and are quantifiable.
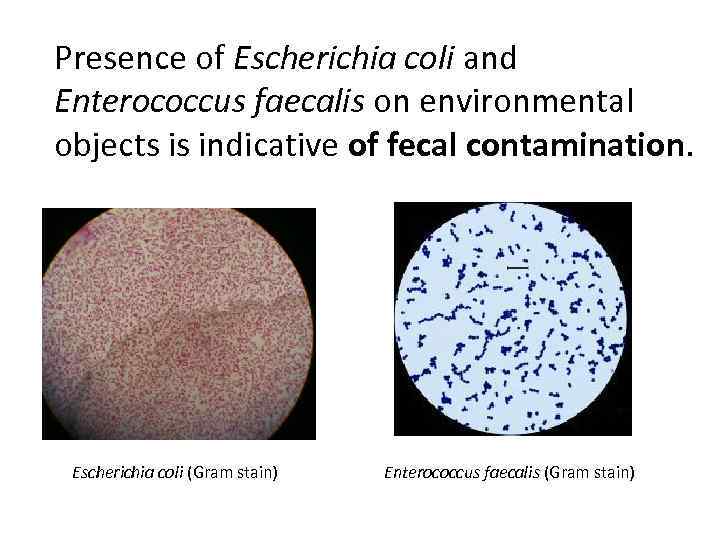
Presence of Escherichia coli and Enterococcus faecalis on environmental objects is indicative of fecal contamination. Escherichia coli (Gram stain) Enterococcus faecalis (Gram stain)
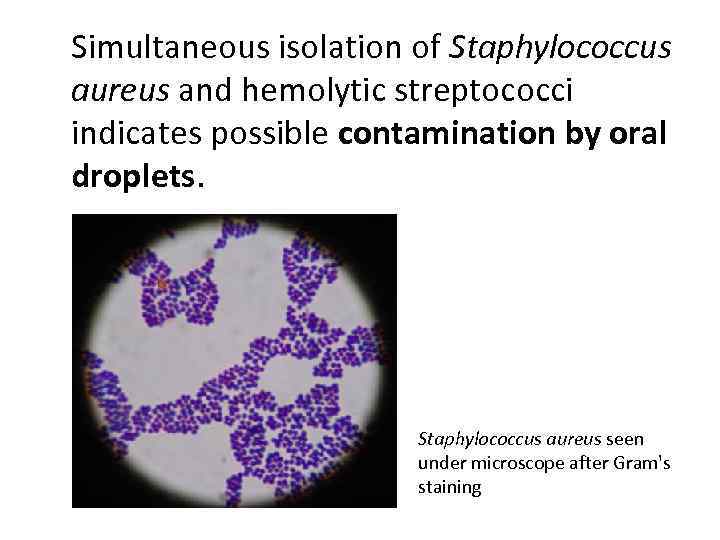
Simultaneous isolation of Staphylococcus aureus and hemolytic streptococci indicates possible contamination by oral droplets. Staphylococcus aureus seen under microscope after Gram's staining
If the amount of SIMs increases in environmental objects, the probability of the presence of pathogenic and opportunistic microbes in them increases. For different objects there are specific SIMs. Presence of sanitary-indicative microorganisms is measured by titer and index. The titer is a minimal mass (in g) or volume (in ml), where else are detected SIMs. The index is the amount of SIMs contained in a 1 l of water, 1 g of soil, 1 m 3 of air.
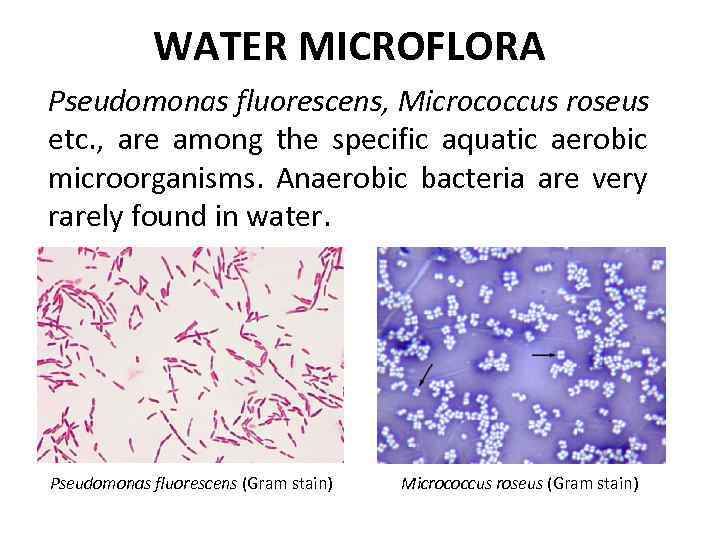
WATER MICROFLORA Pseudomonas fluorescens, Micrococcus roseus etc. , are among the specific aquatic aerobic microorganisms. Anaerobic bacteria are very rarely found in water. Pseudomonas fluorescens (Gram stain) Micrococcus roseus (Gram stain)
The microflora of rivers depends on the degree of pollution and the quality of purification of sewage waters flowing into river beds. Microorganisms are widespread in the waters of the seas and oceans. They have been found at different depths (37009000 m).
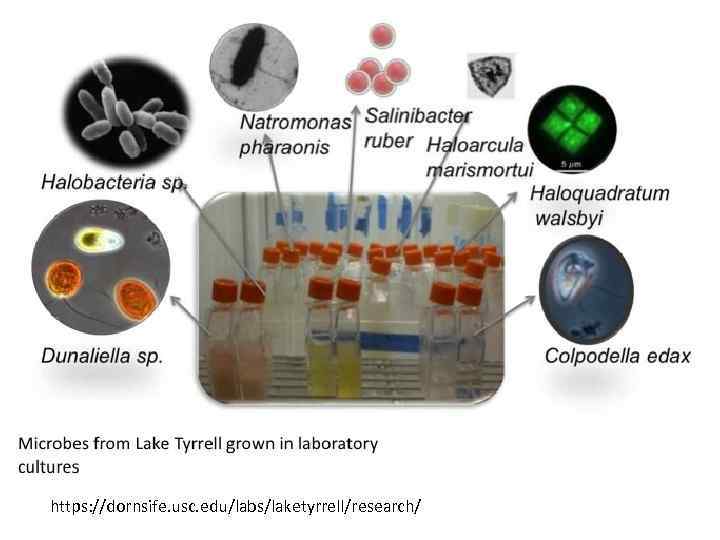
https: //dornsife. usc. edu/labs/laketyrrell/research/
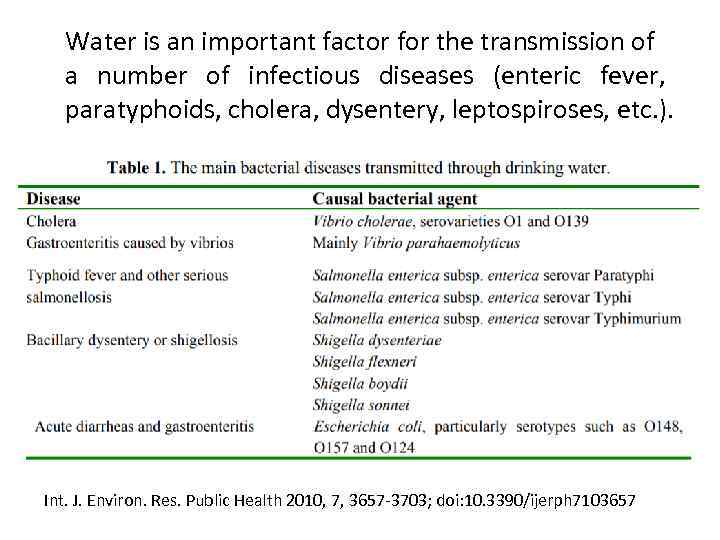
Water is an important factor for the transmission of a number of infectious diseases (enteric fever, paratyphoids, cholera, dysentery, leptospiroses, etc. ). Int. J. Environ. Res. Public Health 2010, 7, 3657 -3703; doi: 10. 3390/ijerph 7103657
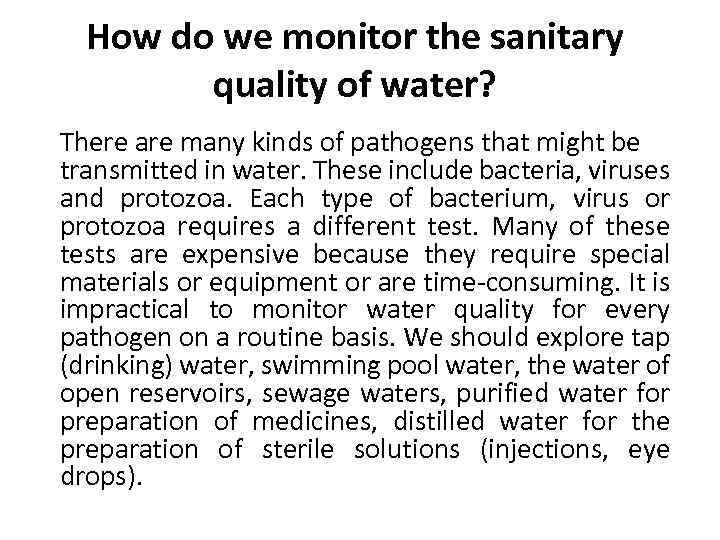
How do we monitor the sanitary quality of water? There are many kinds of pathogens that might be transmitted in water. These include bacteria, viruses and protozoa. Each type of bacterium, virus or protozoa requires a different test. Many of these tests are expensive because they require special materials or equipment or are time-consuming. It is impractical to monitor water quality for every pathogen on a routine basis. We should explore tap (drinking) water, swimming pool water, the water of open reservoirs, sewage waters, purified water for preparation of medicines, distilled water for the preparation of sterile solutions (injections, eye drops).
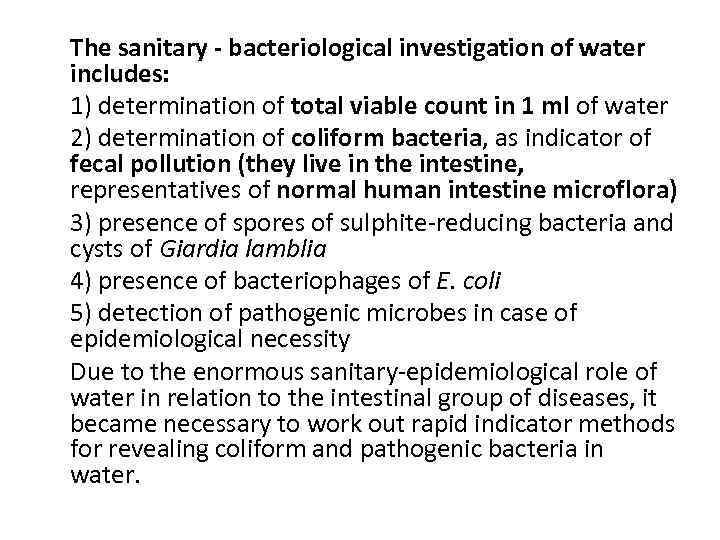
The sanitary - bacteriological investigation of water includes: 1) determination of total viable count in 1 ml of water 2) determination of coliform bacteria, as indicator of fecal pollution (they live in the intestine, representatives of normal human intestine microflora) 3) presence of spores of sulphite-reducing bacteria and cysts of Giardia lamblia 4) presence of bacteriophages of E. coli 5) detection of pathogenic microbes in case of epidemiological necessity Due to the enormous sanitary-epidemiological role of water in relation to the intestinal group of diseases, it became necessary to work out rapid indicator methods for revealing coliform and pathogenic bacteria in water.
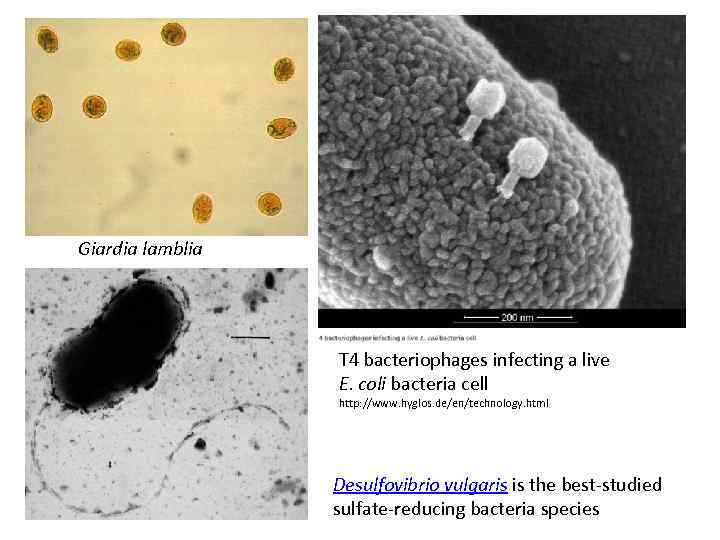
Giardia lamblia T 4 bacteriophages infecting a live E. coli bacteria cell http: //www. hyglos. de/en/technology. html Desulfovibrio vulgaris is the best-studied sulfate-reducing bacteria species
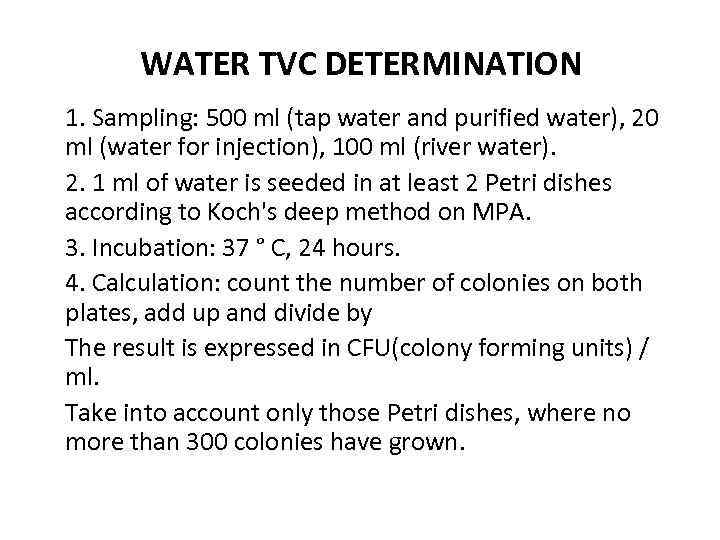
WATER TVC DETERMINATION 1. Sampling: 500 ml (tap water and purified water), 20 ml (water for injection), 100 ml (river water). 2. 1 ml of water is seeded in at least 2 Petri dishes according to Koch's deep method on MPA. 3. Incubation: 37 ° C, 24 hours. 4. Calculation: count the number of colonies on both plates, add up and divide by The result is expressed in CFU(colony forming units) / ml. Take into account only those Petri dishes, where no more than 300 colonies have grown.
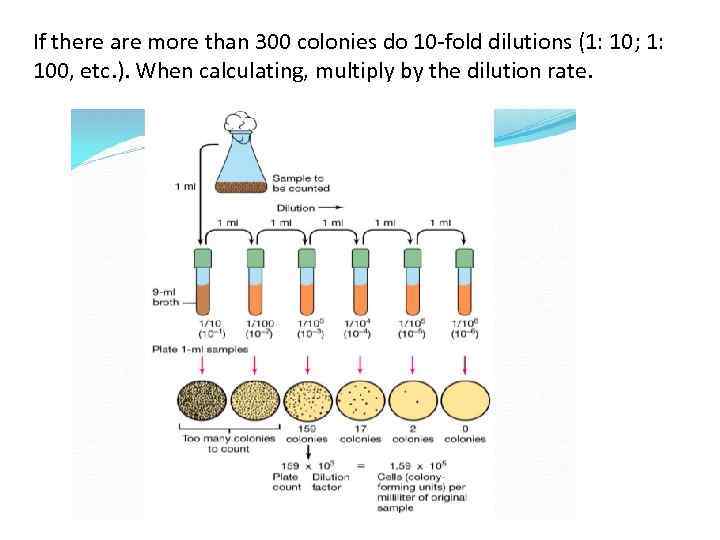
If there are more than 300 colonies do 10 -fold dilutions (1: 10; 1: 100, etc. ). When calculating, multiply by the dilution rate.
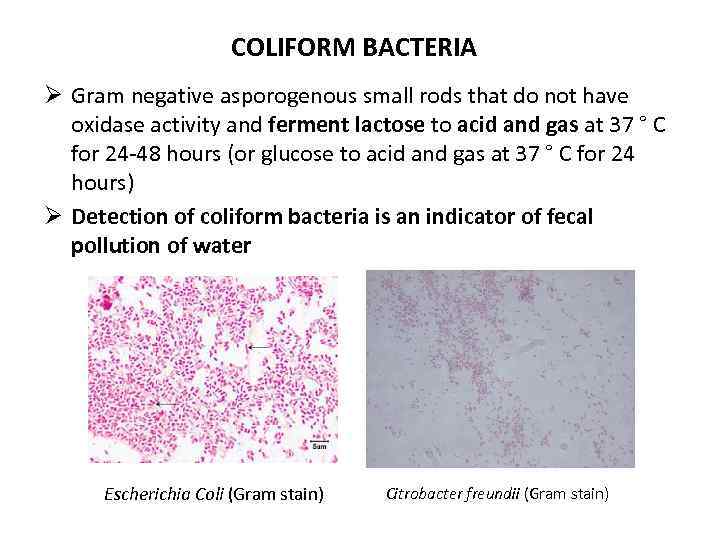
COLIFORM BACTERIA Ø Gram negative asporogenous small rods that do not have oxidase activity and ferment lactose to acid and gas at 37 ° C for 24 -48 hours (or glucose to acid and gas at 37 ° C for 24 hours) Ø Detection of coliform bacteria is an indicator of fecal pollution of water Escherichia Coli (Gram stain) Citrobacter freundii (Gram stain)
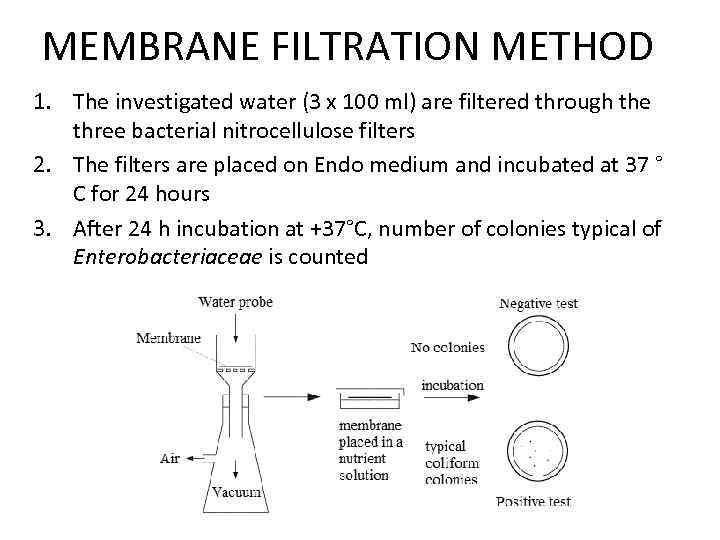
MEMBRANE FILTRATION METHOD 1. The investigated water (3 x 100 ml) are filtered through the three bacterial nitrocellulose filters 2. The filters are placed on Endo medium and incubated at 37 ° C for 24 hours 3. After 24 h incubation at +37°C, number of colonies typical of Enterobacteriaceae is counted
MEMBRANE FILTRATION METHOD 4. From 2 to 3 red-colored colonies are used for preparation of smear and Gram stain, followed by oxidase test allowing to distinguish Escherichia spp. , Citrobacter spp. , Enterobacter spp. and other Enterobacteriaceae from Pseudomonas spp. and other oxidase-positive non-fermenters which might be present in water. 5. For that purpose, filter with grown colonies (do not turn over! ) is transferred with forceps to filter paper disk wetted with dimethyl —n-phenyldiamine. Presence of oxidase will lead to development of blue coloration of colony. 6. After that, 2 or 3 colonies, which did not change color, are inoculated into semi-solid medium with 0. 5% of glucose (lactose), followed by 24 h incubation at +37°C. In case of presence of formation of gas, you make a conclusion about the detection of coliform bacteria. Then number of red colonies is counted and coliform index is determined.
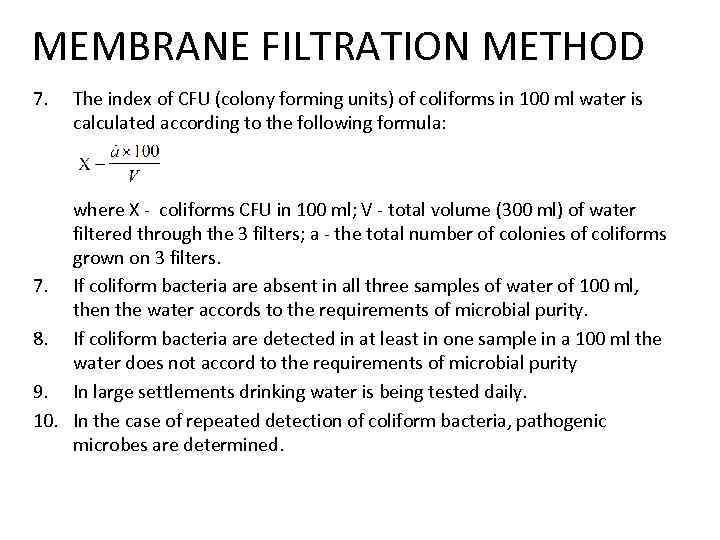
MEMBRANE FILTRATION METHOD 7. The index of CFU (colony forming units) of coliforms in 100 ml water is calculated according to the following formula: where X - coliforms CFU in 100 ml; V - total volume (300 ml) of water filtered through the 3 filters; a - the total number of colonies of coliforms grown on 3 filters. 7. If coliform bacteria are absent in all three samples of water of 100 ml, then the water accords to the requirements of microbial purity. 8. If coliform bacteria are detected in at least in one sample in a 100 ml the water does not accord to the requirements of microbial purity 9. In large settlements drinking water is being tested daily. 10. In the case of repeated detection of coliform bacteria, pathogenic microbes are determined.
What are the standards for drinking water? The USEPA issued revised Primary Drinking Water Standards in mid-1994. These standards address the source of water quality. The Primary Standards. If this test is used, and the sampling agency tests more than 40 samples, no more than 5% of those samples may test positive for total coliforms. If fewer than 40 samples are used, no more than 1 sample may test positive. In addition, the maximum contaminant levels, which vary with treatment technique, are specified for Giardia lamblia, Legionella (the bacterium which causes Legionnaire's disease) and viruses. The USEPA Safe Drinking Water Hotline provides more information. That number is 1 -800 -426 - 4791. The best way to ensure water safety - protection of water sources from microbial contamination!
STANDARDS Ø The drinking water should not have more than 50 microbes in 1 ml. Ø The microbial number in water of open reservoirs can be up 1000.
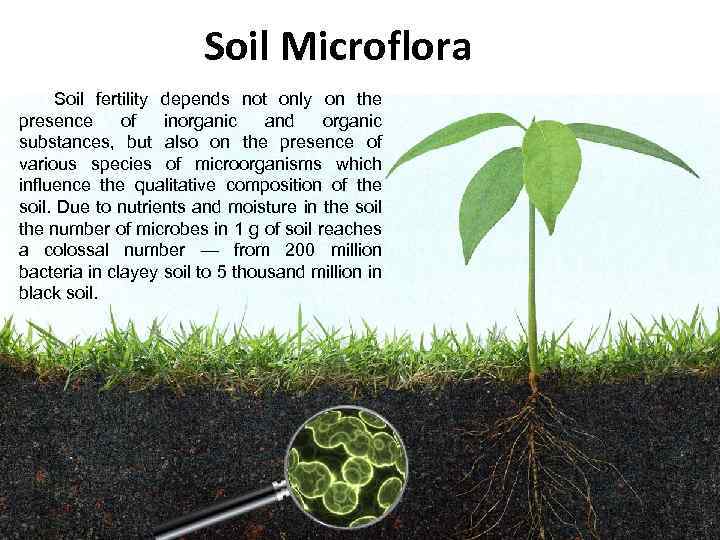
Soil Microflora Soil fertility depends not only on the presence of inorganic and organic substances, but also on the presence of various species of microorganisms which influence the qualitative composition of the soil. Due to nutrients and moisture in the soil the number of microbes in 1 g of soil reaches a colossal number — from 200 million bacteria in clayey soil to 5 thousand million in black soil.
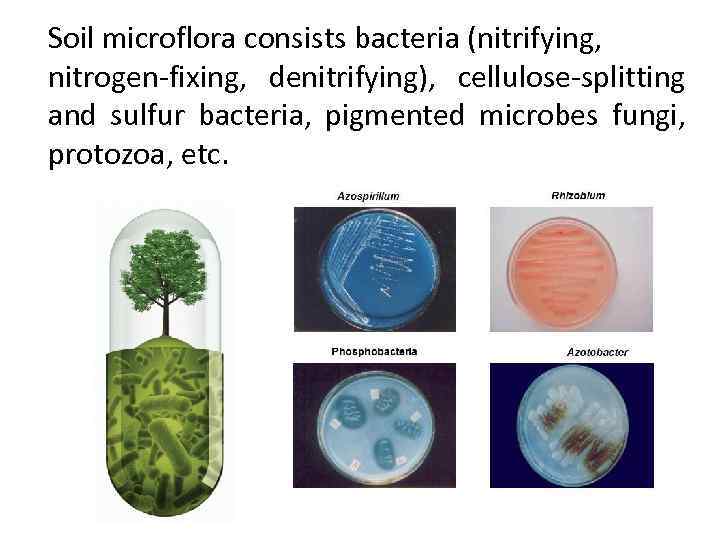
Soil microflora consists bacteria (nitrifying, nitrogen-fixing, denitrifying), cellulose-splitting and sulfur bacteria, pigmented microbes fungi, protozoa, etc.
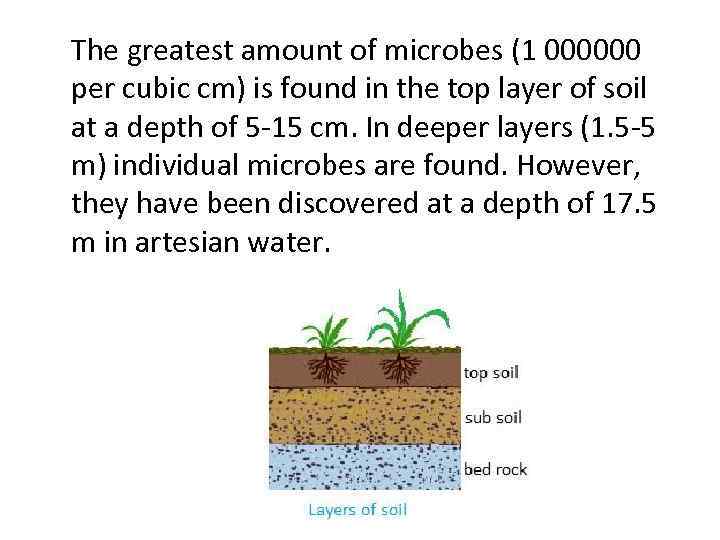
The greatest amount of microbes (1 000000 per cubic cm) is found in the top layer of soil at a depth of 5 -15 cm. In deeper layers (1. 5 -5 m) individual microbes are found. However, they have been discovered at a depth of 17. 5 m in artesian water.
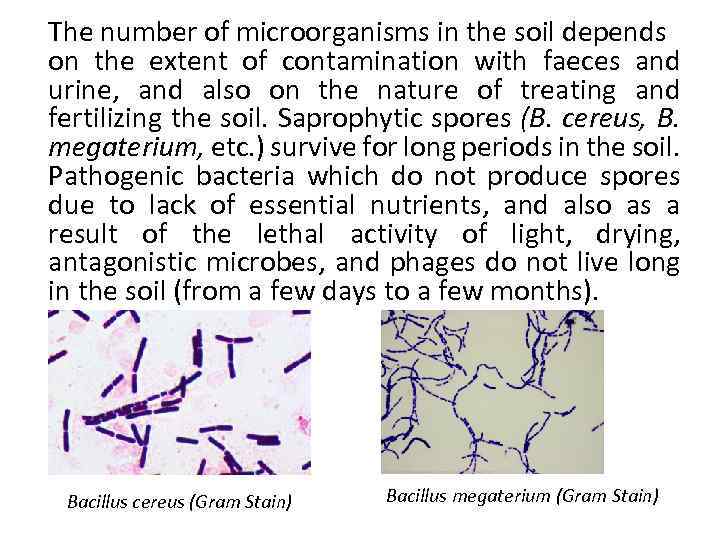
The number of microorganisms in the soil depends on the extent of contamination with faeces and urine, and also on the nature of treating and fertilizing the soil. Saprophytic spores (B. cereus, B. megaterium, etc. ) survive for long periods in the soil. Pathogenic bacteria which do not produce spores due to lack of essential nutrients, and also as a result of the lethal activity of light, drying, antagonistic microbes, and phages do not live long in the soil (from a few days to a few months). Bacillus cereus (Gram Stain) Bacillus megaterium (Gram Stain)
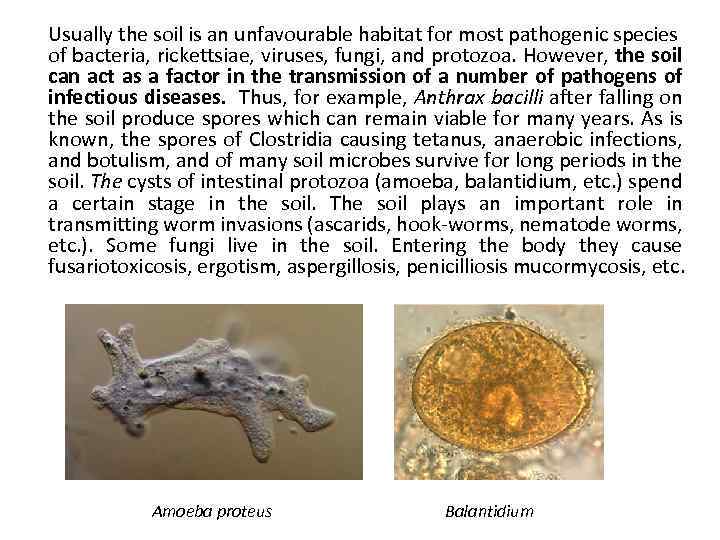
Usually the soil is an unfavourable habitat for most pathogenic species of bacteria, rickettsiae, viruses, fungi, and protozoa. However, the soil can act as a factor in the transmission of a number of pathogens of infectious diseases. Thus, for example, Anthrax bacilli after falling on the soil produce spores which can remain viable for many years. As is known, the spores of Clostridia causing tetanus, anaerobic infections, and botulism, and of many soil microbes survive for long periods in the soil. The cysts of intestinal protozoa (amoeba, balantidium, etc. ) spend a certain stage in the soil. The soil plays an important role in transmitting worm invasions (ascarids, hook-worms, nematode worms, etc. ). Some fungi live in the soil. Entering the body they cause fusariotoxicosis, ergotism, aspergillosis, penicilliosis mucormycosis, etc. Amoeba proteus Balantidium
Microbiological Investigation of Soil Taking into consideration the definite epidemiological role played by the soil in spreading some infectious diseases of animals and man, sanitary-microbiological evaluation of soil is performed. The sanitary - bacteriological investigation of soil includes: 1) a total quantity of saprophytes bacteria in 1 g of soil indicator of fecal contamination
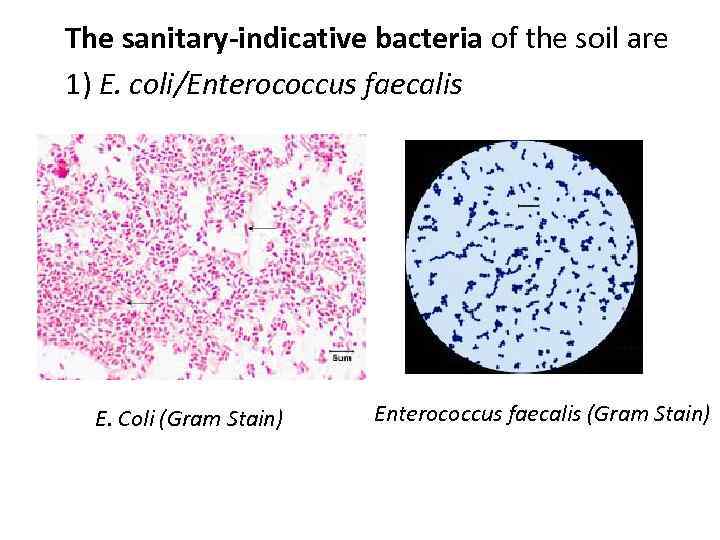
The sanitary-indicative bacteria of the soil are 1) E. coli/Enterococcus faecalis E. Coli (Gram Stain) Enterococcus faecalis (Gram Stain)
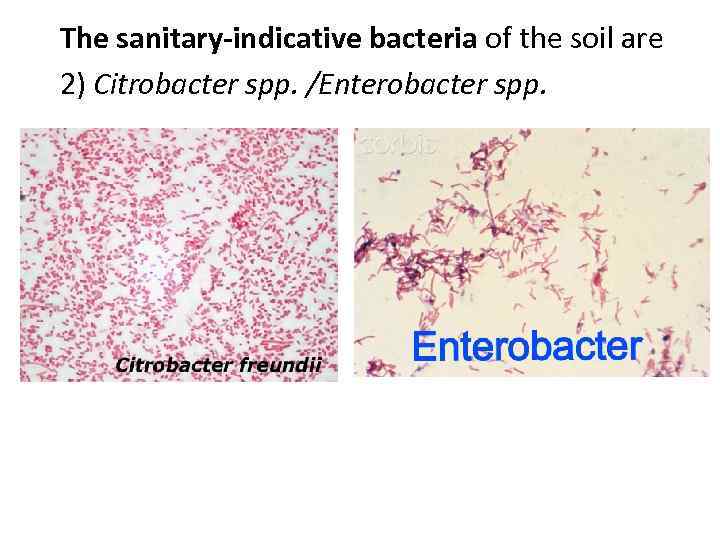
The sanitary-indicative bacteria of the soil are 2) Citrobacter spp. /Enterobacter spp.
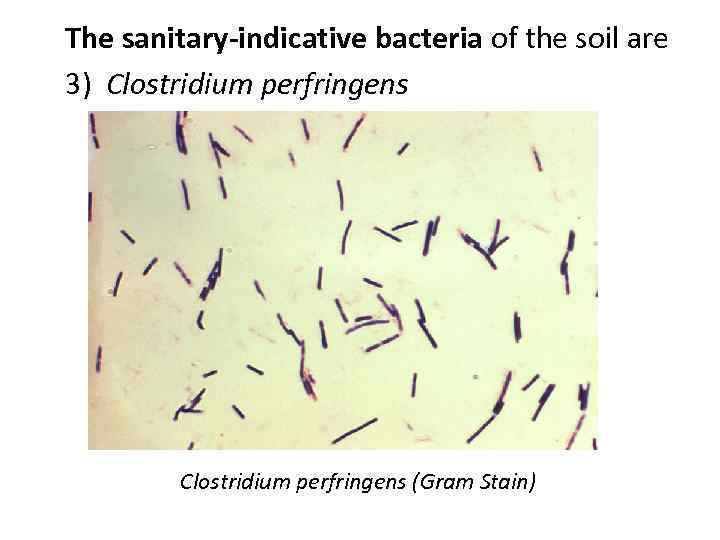
The sanitary-indicative bacteria of the soil are 3) Clostridium perfringens (Gram Stain)
More accurate evaluation is performed using ü coli-index — number of Enterobacteriaceae (so called coliform bacteria) found in 1 g of soil ü perfringens-titer - mass of soil in which 1 cell C. perfringens is found.
Determination of Soil TVC For this purpose it is necessary to select most typical area not more then 25 m 2. The samples are taken from different places of the field along the diagonal, the angles and the center 10 — 20 cm deep. The weight of each sample must be 100 - 200 g. The total weight of the soil 0, 5 - 1 kg. After careful mixing take an average sample of weight 100 - 200 g. Put the samples of soil in the sterile banks, mark and deliver to the laboratory.
Determination of Soil TVC 1. Prepare 10 -fold dilutions (1: 10, 1: 100, etc. ) in an isotonic sterile solution of sodium chloride. 2. Make seeding of the soil dilutions on MPA (for bacteria) and on Saburo medium (for fungi): 1 ml in the depth of agar or 0. 1 ml on the surface of agar. 3. Incubation: at 24 ° C (for fungi) and 37 ° C (for bacteria). After incubation at optimal temperature count the colonies on the plates (1 colony=1 cell). The number of cells in 1 g of soil is calculated, taking into account: - the weight of each sample; - the rate of dilution; - the volume of seeding.
Determination of Perfringens-titer 1. Seeding onto the Wilson-Blair medium: black colonies are formed and the gas breaks up the medium 2. Calculation: maximal dilution, where there are signs of growth of Clostridium perfringens.
AIR MICROFLORA The composition of the microbes of the air is quite variable. Then more dust, smoke, and soot in the air, the greater the number of microbes. Each particle of dust or smoke is able to adsorb on its surface numerous microbes. The number of microbes in the air varies from a few specimens to many tens of thousands per 1 m 3. Depending on the time of the year, the composition and the amount of microflora change. If the total amount of microbes in winter is accepted as 1, then in spring it will be 1. 7, in summer— 2 and in autumn — 1. 2.
The number of microbes in factories and homes is associated closely with the sanitary hygienic conditions of the building. At poor ventilation and natural lighting and if the premises are not properly cleaned, the number of microbes increases. Pathogenic species of microbes (Pyogenic Cocci, Tubercle Bacilli, Anthrax Bacilli, bacteria of tularaemia, rickettsia of Q-fever, etc. ) may be found in the surroundings of sick animals and humans, infected arthropods and insects, and in dust. The causative agents of influenza, measles, scarlet fever, diphtheria, whooping cough, meningococcal infections, tonsillitis, acute catarrhs of the respiratory tract, tuberculosis, smallpox, pneumatic plague, and other diseases can be transmitted through the air together with droplets of mucus and sputum during sneezing, coughing, and talking.
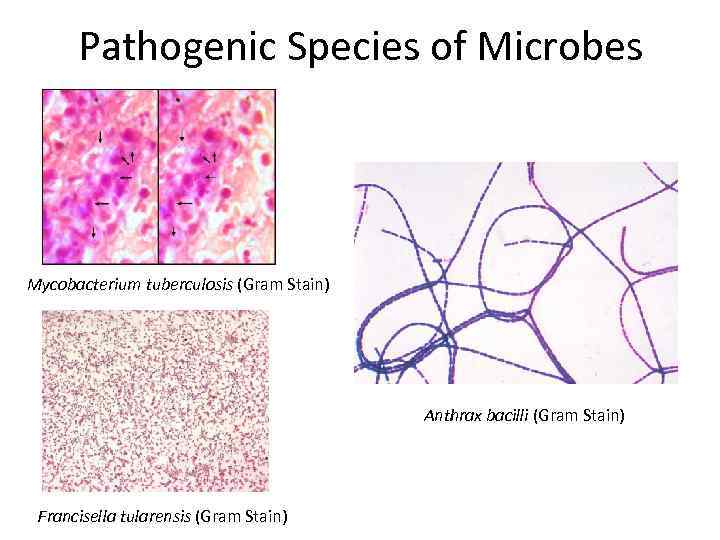
Pathogenic Species of Microbes Mycobacterium tuberculosis (Gram Stain) Anthrax bacilli (Gram Stain) Francisella tularensis (Gram Stain)
The air is an unfavourable medium for microbes. The absence of nutrient substances, the presence of moisture, optimal temperature, the lethal activity of sunlight, and desiccation do not create conditions for keeping microbes viable and most of them perish. However, the relatively short period during which the microbes are in air is quite enough to bring about the transmission of pathogenic bacteria and viruses from sick to healthy persons, and to cause extensive epidemics of diseases such as influenza.
The laboratory investigation of air is carried out to determine the qualitative and quantitative composition of its microflora. This is achieved by using simple and complex methods. For a more accurate investigation of microbial contents of the air special apparatus are used. At present Streptococcus viridans serves as sanitary indices for the air of closed buildings, and haemolytic streptococci and pathogenic staphylococci are a direct epidemiological hazard.
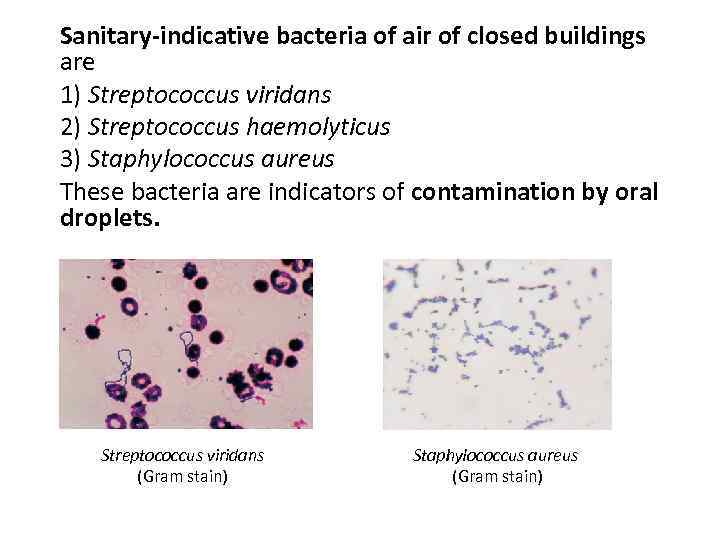
Sanitary-indicative bacteria of air of closed buildings are 1) Streptococcus viridans 2) Streptococcus haemolyticus 3) Staphylococcus aureus These bacteria are indicators of contamination by oral droplets. Streptococcus viridans (Gram stain) Staphylococcus aureus (Gram stain)
Microbiological Investigation of the Air The sanitary - bacteriological investigation of air includes: 1) determination the total viable count (TVC) in 1 m 3 of the air 2) presence of sanitary-indicative bacteria — Str. viridans, Str. haemolyticus , S. aureus. For taking the samples sedimentation and aspiration methods are used.
Plate method (sedimentation method) The Petri’s dishes with meat-peptone agar or another special nutrient media for staphylococci and streptococci, for example blood agar, yolk- salt agar are used. They are opened and are stayed in investigated room. Term of exposition depends on prospective quantity of microbes in the air. With a plenty of microorganisms a plate is opened for 5 -10 minutes to detect a total microbial number, with a little - for 20 — 40 minutes for detection of cocci. Then the dishes put into thermostat at 37 °C for 24 hrs. After incubation all colonies are accounted (for determination of total number of microorganisms). Number of grown colonies indicates degree of air contamination. According to Omeliansky’s data in 5 minutes on a surface of 100 cm 2 so many microbes sedimentate, as they present in 10 L of air. For example, on the dish surface with MPA after 5 minute exposure 32 colonies have grown. It is necessary to calculate amount of microbes which are present in 1 nr 3 of the air, applying the Omeliansky’s formula. The plate has 100 cm 2. 32 colonies of microbes contain in 10 L of the air, and in 1 m 3 (1000 л) there will be (32 • 1000): 10 = 3200.
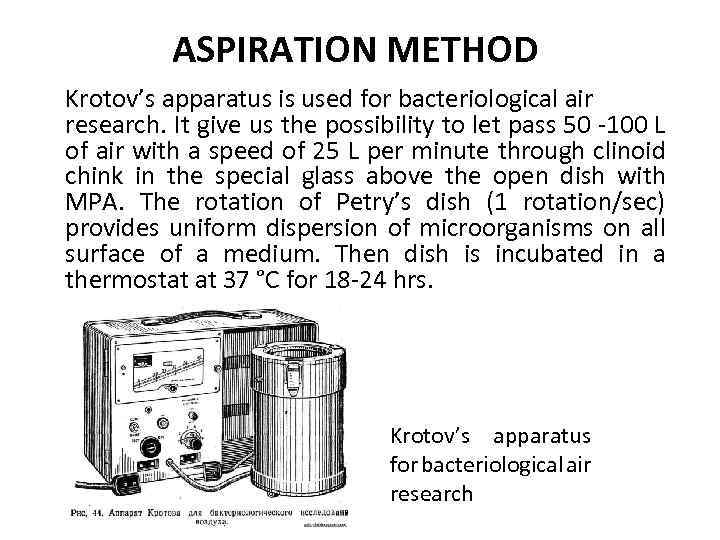
ASPIRATION METHOD Krotov’s apparatus is used for bacteriological air research. It give us the possibility to let pass 50 -100 L of air with a speed of 25 L per minute through clinoid chink in the special glass above the open dish with MPA. The rotation of Petry’s dish (1 rotation/sec) provides uniform dispersion of microorganisms on all surface of a medium. Then dish is incubated in a thermostat at 37 °C for 18 -24 hrs. Krotov’s apparatus for bacteriological air research
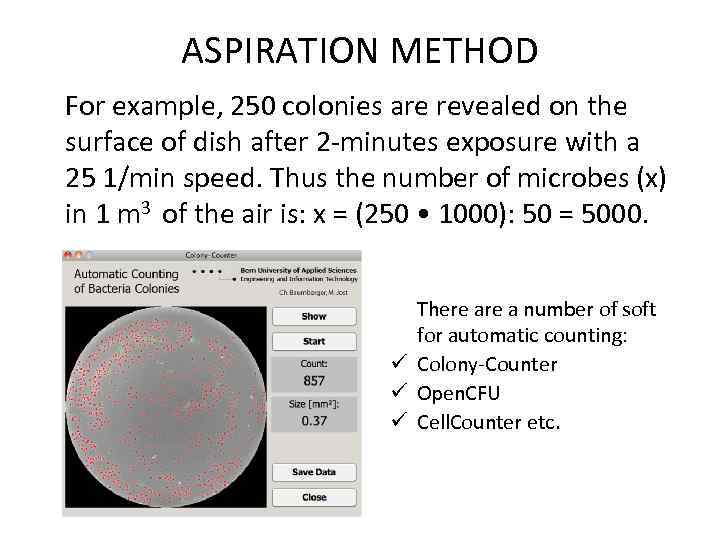
ASPIRATION METHOD For example, 250 colonies are revealed on the surface of dish after 2 -minutes exposure with a 25 1/min speed. Thus the number of microbes (x) in 1 m 3 of the air is: x = (250 • 1000): 50 = 5000. There a number of soft for automatic counting: ü Colony-Counter ü Open. CFU ü Cell. Counter etc.
Determination of Staphylococci and Streptococci Using Krotov’s apparatus 250 L of air are seeded on the surface of open Petri dish with yolk-salt agar for staphylococci and with blood agar for streptococci. Then dishes are incubated in a thermostat at 37 °C for 18 -24 hrs. After incubation growing up colonies are accounted and the number of staphylococci or streptococci in 1 m 3 of the air is calculated.
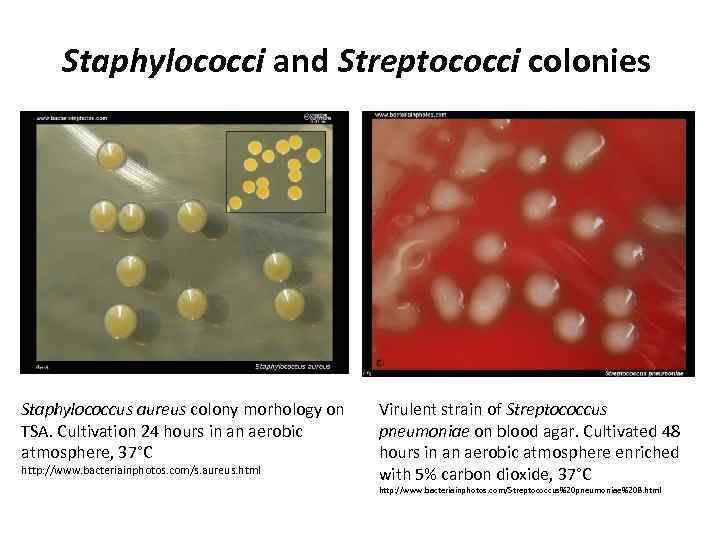
Staphylococci and Streptococci colonies Staphylococcus aureus colony morhology on TSA. Cultivation 24 hours in an aerobic atmosphere, 37°C http: //www. bacteriainphotos. com/s. aureus. html Virulent strain of Streptococcus pneumoniae on blood agar. Cultivated 48 hours in an aerobic atmosphere enriched with 5% carbon dioxide, 37°C http: //www. bacteriainphotos. com/Streptococcus%20 pneumoniae%20 B. html
To the air environment of pharmacies strict hygienic requirements are imposed, which is reflected in normative documents. Sources of air pollution pharmacies: Ø Visitors Ø Employees Ø Infected material (recipes, dishes, packaging material) Ø Poor-quality medicinal plant raw materials. The permissible standards of the microbial number of air in various pharmacy premises have also been developed.
MICROFLORA_AND_SANITARY-INDICATIVE_BACTERIA_OF_SOIL_WATER.pptx