3bd51e86821d65304f96b3e2b4510da6.ppt
- Количество слайдов: 90
Metabolic Syndrome, Diabetes and Cardiovascular Disease: Strategies for Management Nathan D. Wong, Ph. D, FACC, FAHA Professor and Director, Heart Disease Prevention Program, Division of Cardiology, University of California, Irvine Past President, American Society of Preventive Cardiology
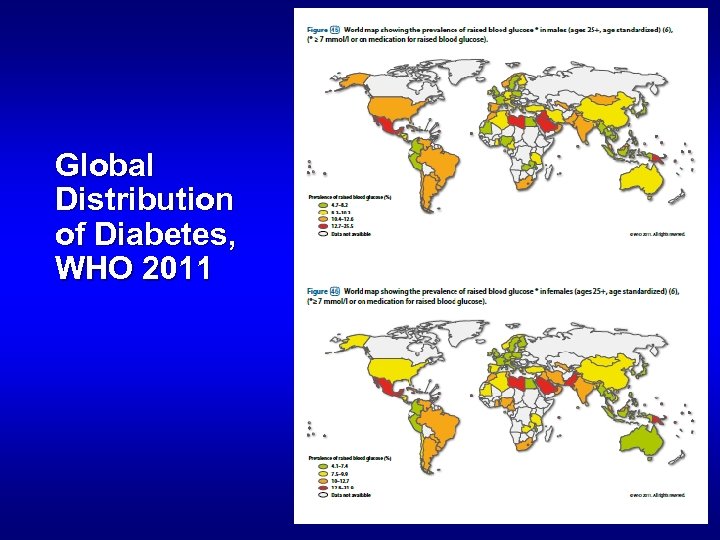
Global Distribution of Diabetes, WHO 2011
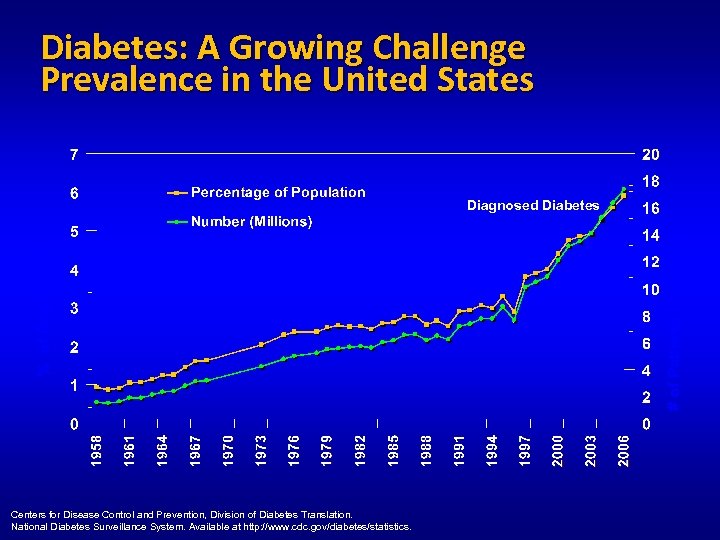
Diabetes: A Growing Challenge Prevalence in the United States Centers for Disease Control and Prevention, Division of Diabetes Translation. National Diabetes Surveillance System. Available at http: //www. cdc. gov/diabetes/statistics. # of Patients in Millions % of Population Diagnosed Diabetes
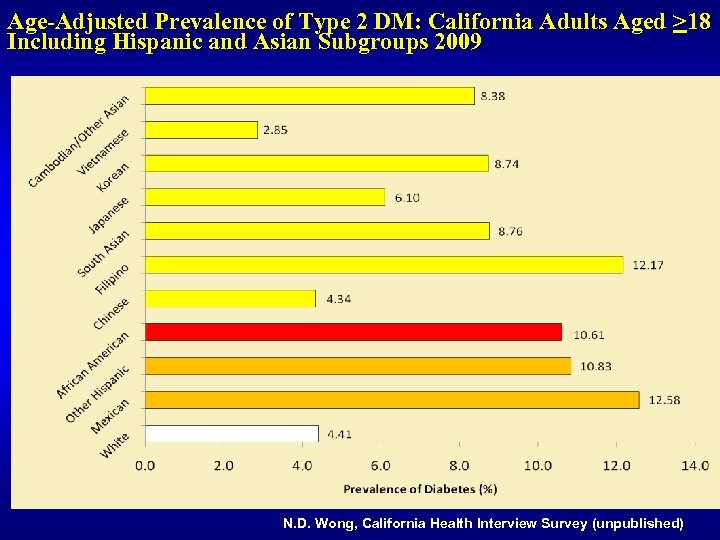
Age-Adjusted Prevalence of Type 2 DM: California Adults Aged >18 Including Hispanic and Asian Subgroups 2009 N. D. Wong, California Health Interview Survey (unpublished)

Diabetes Mellitus: Lifetime Risk Narayan et al. JAMA 2003; 290: 1884 -1890.
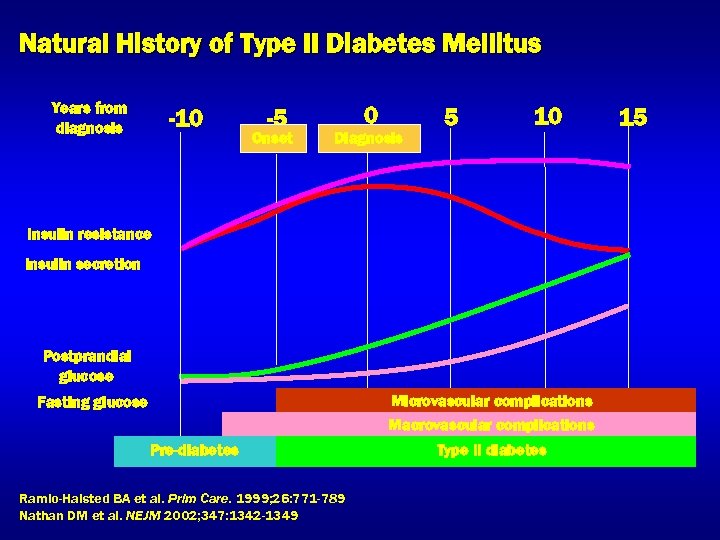
Natural History of Type II Diabetes Mellitus Years from diagnosis -10 -5 Onset 0 Diagnosis 5 10 Insulin resistance Insulin secretion Postprandial glucose Microvascular complications Macrovascular complications Fasting glucose Pre-diabetes Ramlo-Halsted BA et al. Prim Care. 1999; 26: 771 -789 Nathan DM et al. NEJM 2002; 347: 1342 -1349 Type II diabetes 15
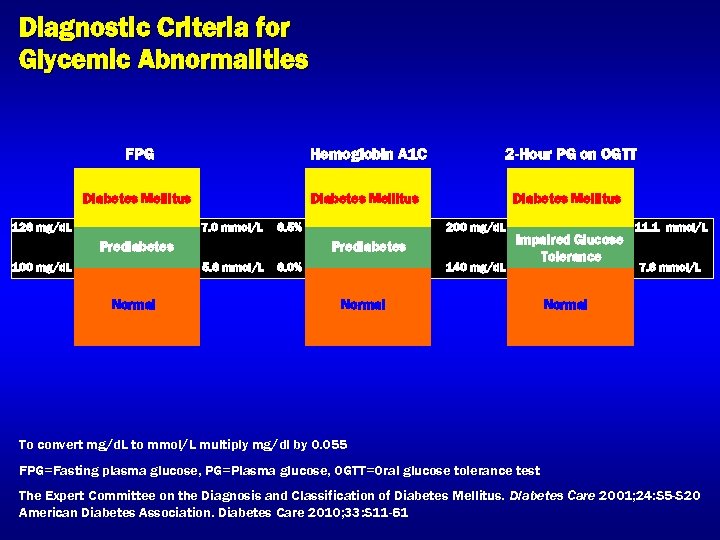
Diagnostic Criteria for Glycemic Abnormalities FPG Hemoglobin A 1 C 2 -Hour PG on OGTT Diabetes Mellitus 126 mg/d. L 7. 0 mmol/L 6. 5% Prediabetes 100 mg/d. L Prediabetes 5. 6 mmol/L Normal 200 mg/d. L 6. 0% 140 mg/d. L Impaired Glucose Tolerance Normal 11. 1 mmol/L 7. 8 mmol/L Normal To convert mg/d. L to mmol/L multiply mg/dl by 0. 055 FPG=Fasting plasma glucose, PG=Plasma glucose, OGTT=Oral glucose tolerance test The Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 2001; 24: S 5 -S 20 American Diabetes Association. Diabetes Care 2010; 33: S 11 -61
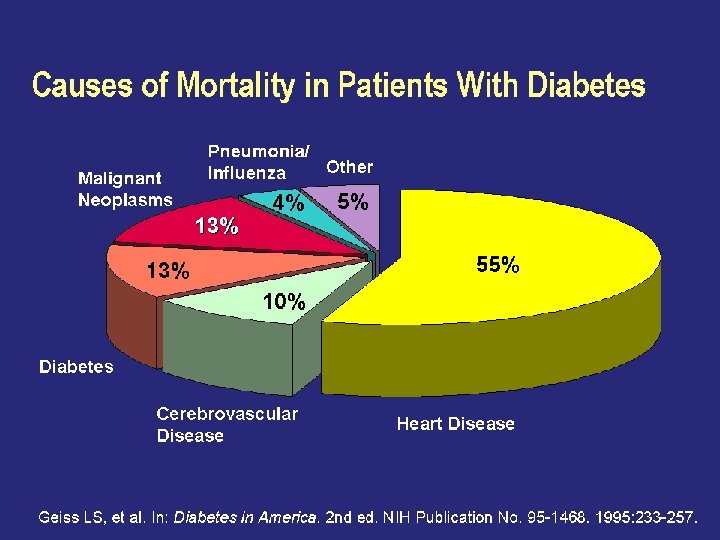
Causes of Mortality in Patients With Diabetes
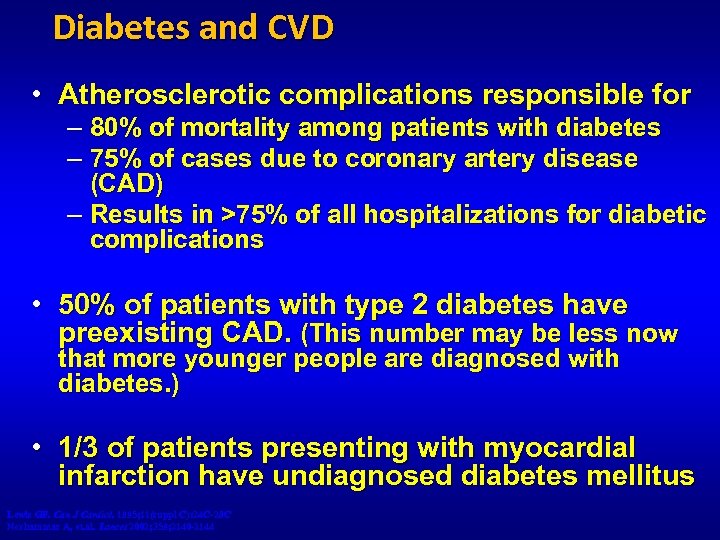
Diabetes and CVD • Atherosclerotic complications responsible for – 80% of mortality among patients with diabetes – 75% of cases due to coronary artery disease (CAD) – Results in >75% of all hospitalizations for diabetic complications • 50% of patients with type 2 diabetes have preexisting CAD. (This number may be less now that more younger people are diagnosed with diabetes. ) • 1/3 of patients presenting with myocardial infarction have undiagnosed diabetes mellitus Lewis GF. Can J Cardiol. 1995; 11(suppl C): 24 C-28 C Norhammar A, et. al. Lancet 2002; 359; 2140 -2144
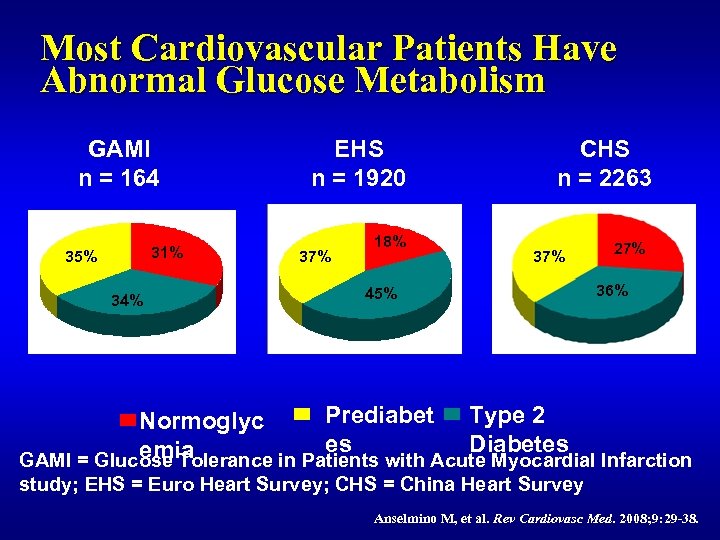
Most Cardiovascular Patients Have Abnormal Glucose Metabolism GAMI n = 164 31% 35% 34% EHS n = 1920 37% 18% CHS n = 2263 37% 45% 27% 36% Prediabet Type 2 Normoglyc es Diabetes emia GAMI = Glucose Tolerance in Patients with Acute Myocardial Infarction study; EHS = Euro Heart Survey; CHS = China Heart Survey Anselmino M, et al. Rev Cardiovasc Med. 2008; 9: 29 -38.

Mechanisms by which Diabetes Mellitus Leads to Coronary Heart Disease Hyperglycemia Insulin Resistance Inflammation Infection IL-6 CRP SAA Defense mechanisms Pathogen burden HTN Endothelial dysfunction AGE Oxidative stress Dyslipidemia LDL TG HDL Subclinical Atherosclerosis Thrombosis PAI-1 TF t. PA Disease Progression Atherosclerotic Clinical Events AGE=Advanced glycation end products, CRP=C-reactive protein, CHD=Coronary heart disease HDL=High-density lipoprotein, HTN=Hypertension, IL-6=Interleukin-6, LDL=Low-density lipoprotein, PAI-1=Plasminogen activator inhibitor-1, SAA=Serum amyloid A protein, TF=Tissue factor, TG=Triglycerides, t. PA=Tissue plasminogen activator Biondi-Zoccai GGL et al. JACC 2003; 41: 10711077.
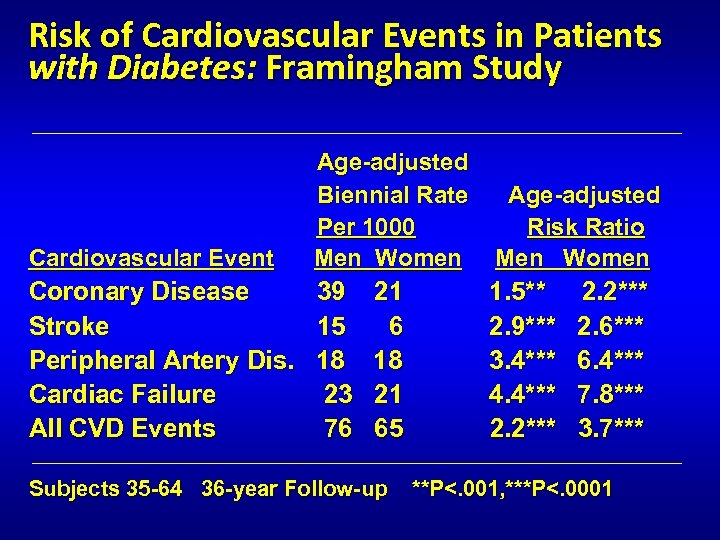
Risk of Cardiovascular Events in Patients with Diabetes: Framingham Study _________________________________ Age-adjusted Biennial Rate Age-adjusted Per 1000 Risk Ratio Cardiovascular Event Men Women Men Women Coronary Disease 39 21 1. 5** 2. 2*** Stroke 15 6 2. 9*** 2. 6*** Peripheral Artery Dis. 18 3. 4*** 6. 4*** Cardiac Failure 23 21 4. 4*** 7. 8*** All CVD Events 76 65 2. 2*** 3. 7*** _________________________________ Subjects 35 -64 36 -year Follow-up **P<. 001, ***P<. 0001
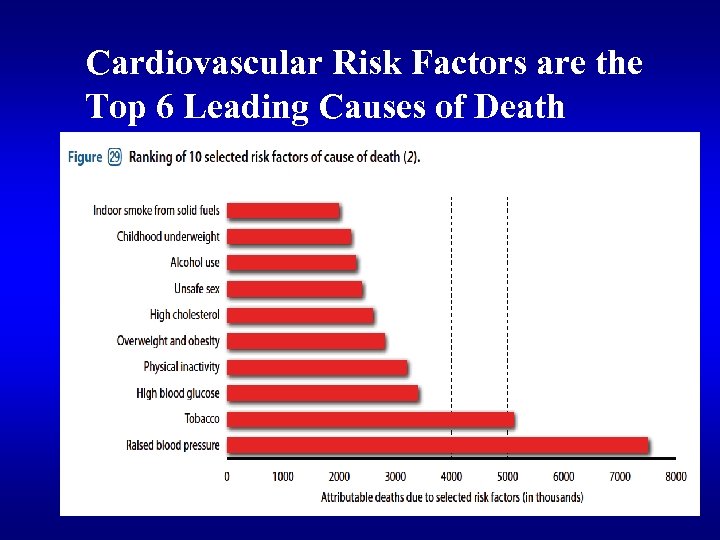
Cardiovascular Risk Factors are the Top 6 Leading Causes of Death
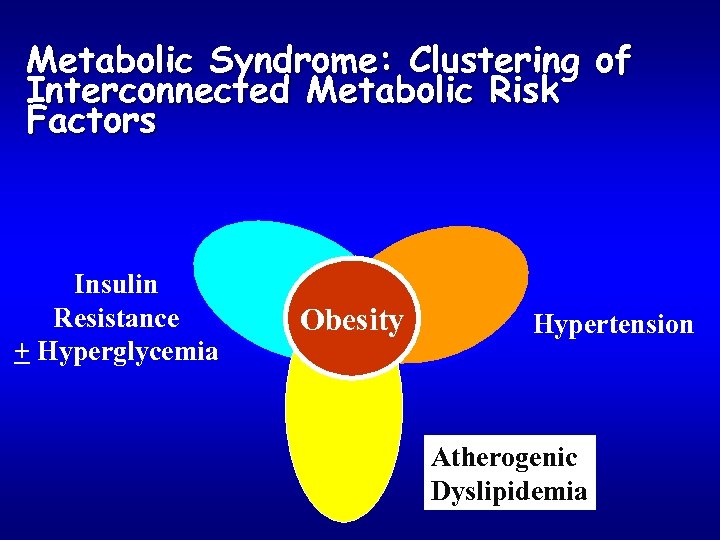
Metabolic Syndrome: Clustering of Interconnected Metabolic Risk Factors Insulin Resistance + Hyperglycemia Obesity Hypertension Atherogenic Dyslipidemia
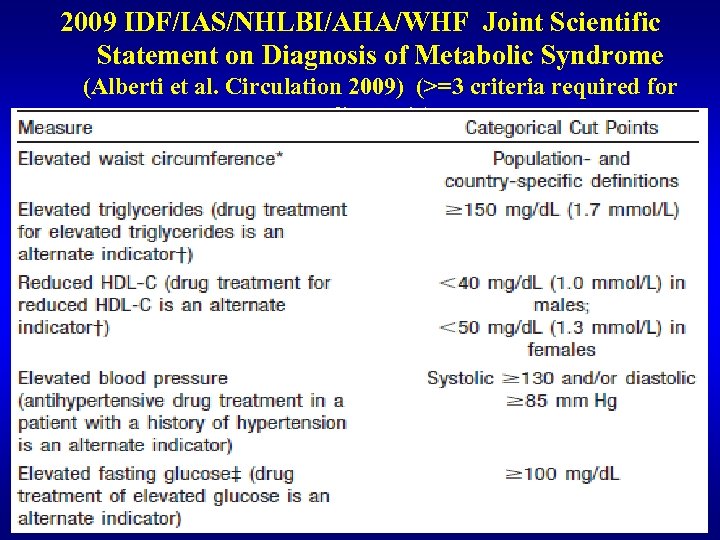
2009 IDF/IAS/NHLBI/AHA/WHF Joint Scientific Statement on Diagnosis of Metabolic Syndrome (Alberti et al. Circulation 2009) (>=3 criteria required for diagnosis)
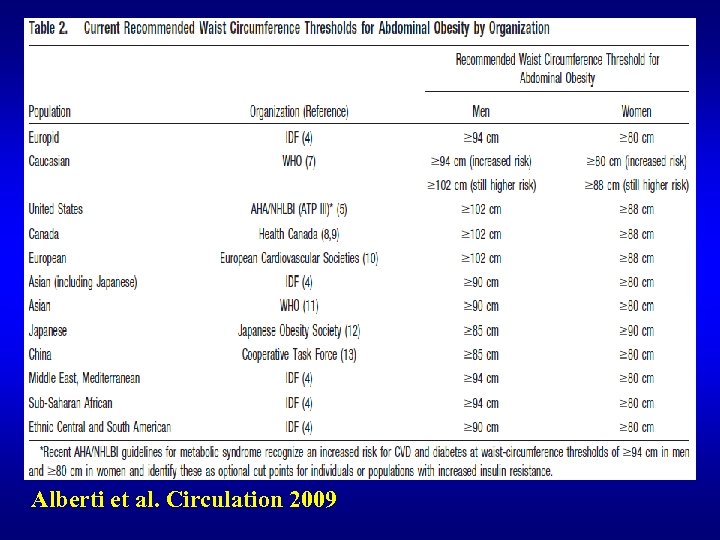
Alberti et al. Circulation 2009
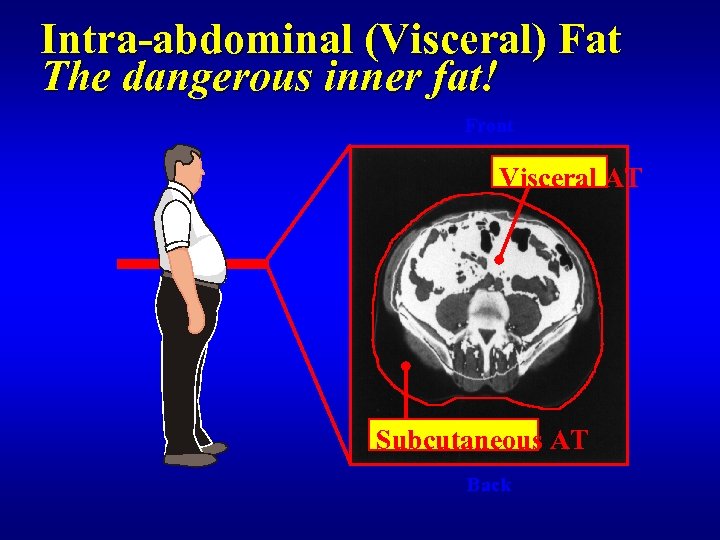
Intra-abdominal (Visceral) Fat The dangerous inner fat! Front Visceral AT Subcutaneous AT Back
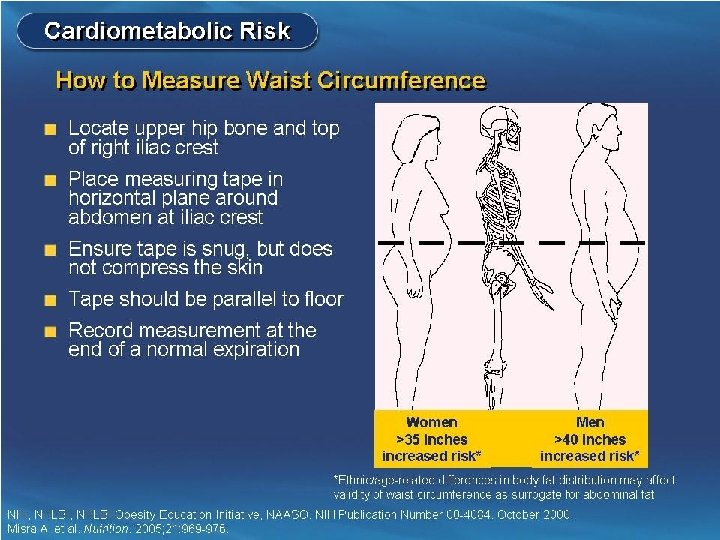
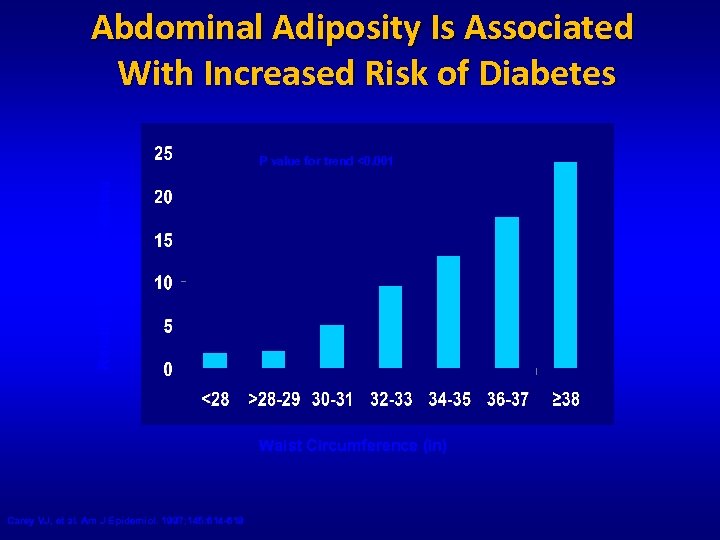
Abdominal Adiposity Is Associated With Increased Risk of Diabetes Relative Risk of Diabetes P value for trend <0. 001 Waist Circumference (in) Carey VJ, et al. Am J Epidemiol. 1997; 145: 614 -619
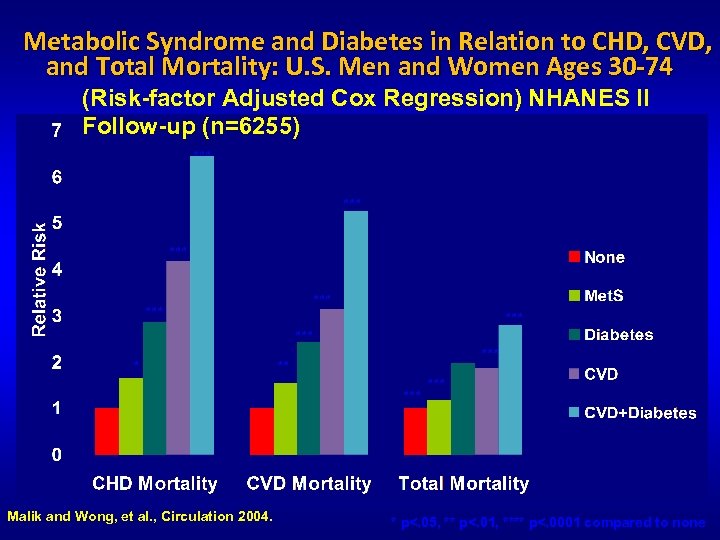
Metabolic Syndrome and Diabetes in Relation to CHD, CVD, and Total Mortality: U. S. Men and Women Ages 30 -74 (Risk-factor Adjusted Cox Regression) NHANES II Follow-up (n=6255) *** *** *** Malik and Wong, et al. , Circulation 2004. *** ** *** * p<. 05, ** p<. 01, **** p<. 0001 compared to none
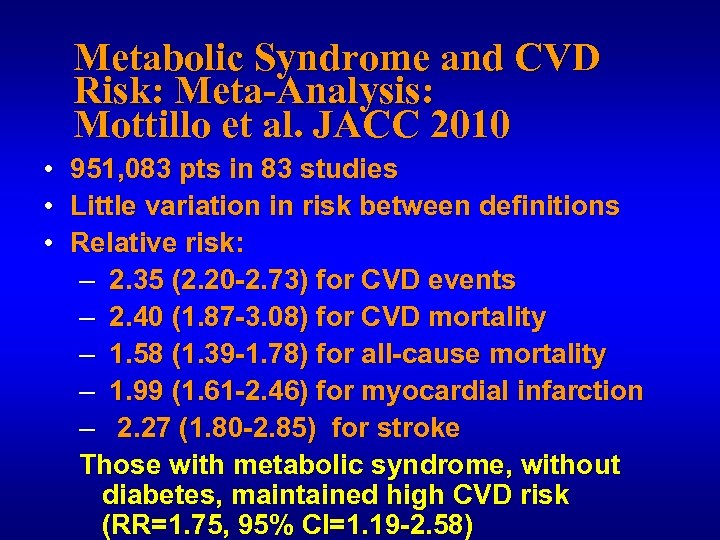
Metabolic Syndrome and CVD Risk: Meta-Analysis: Mottillo et al. JACC 2010 • • • 951, 083 pts in 83 studies Little variation in risk between definitions Relative risk: – 2. 35 (2. 20 -2. 73) for CVD events – 2. 40 (1. 87 -3. 08) for CVD mortality – 1. 58 (1. 39 -1. 78) for all-cause mortality – 1. 99 (1. 61 -2. 46) for myocardial infarction – 2. 27 (1. 80 -2. 85) for stroke Those with metabolic syndrome, without diabetes, maintained high CVD risk (RR=1. 75, 95% CI=1. 19 -2. 58)
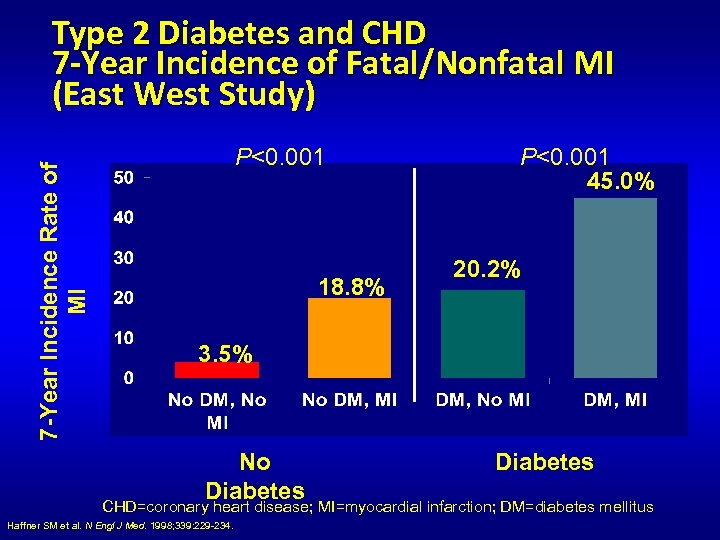
7 -Year Incidence Rate of MI Type 2 Diabetes and CHD 7 -Year Incidence of Fatal/Nonfatal MI (East West Study) P<0. 001 18. 8% P<0. 001 45. 0% 20. 2% 3. 5% No Diabetes CHD=coronary heart disease; MI=myocardial infarction; DM=diabetes mellitus Haffner SM et al. N Engl J Med. 1998; 339: 229 -234.
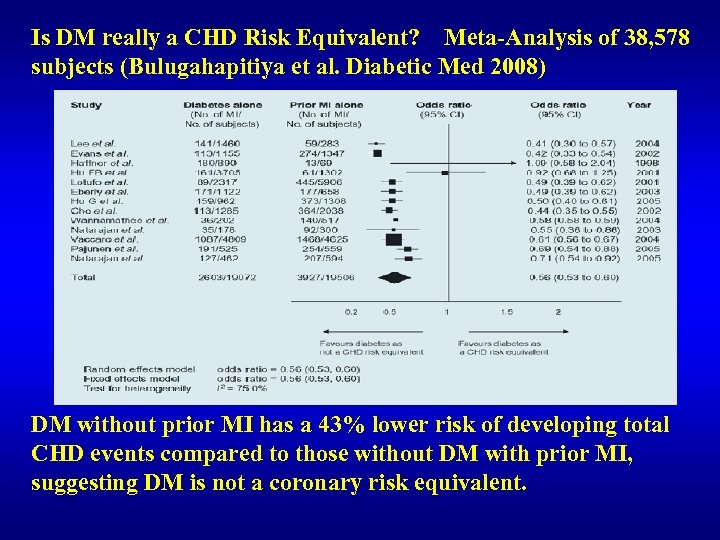
Is DM really a CHD Risk Equivalent? Meta-Analysis of 38, 578 subjects (Bulugahapitiya et al. Diabetic Med 2008) DM without prior MI has a 43% lower risk of developing total CHD events compared to those without DM with prior MI, suggesting DM is not a coronary risk equivalent.
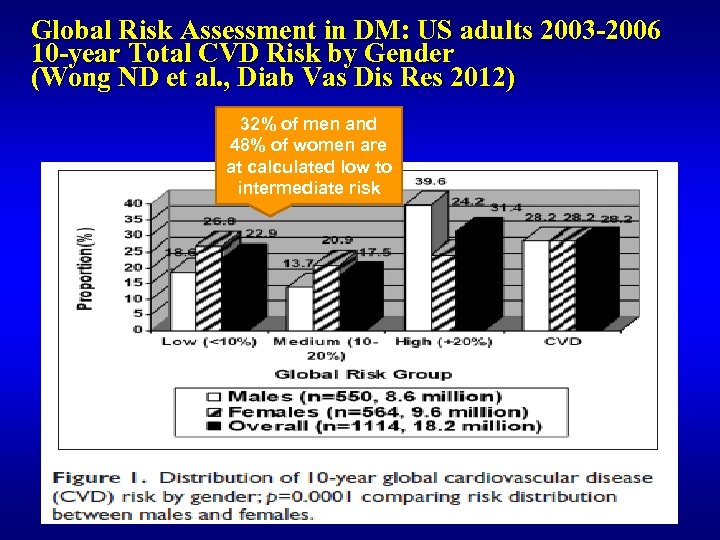
Global Risk Assessment in DM: US adults 2003 -2006 10 -year Total CVD Risk by Gender (Wong ND et al. , Diab Vas Dis Res 2012) 32% of men and 48% of women are at calculated low to intermediate risk
2013 Prevention Guidelines ASCVD Risk Estimator Available at www. cardiosource. com
Screening for Coronary Disease in Diabetes: When and How (Ali and Maron, Clinical Diabetes 2006) “ Screening patients according to traditional risk factors and current guidelines alone will frequently fail to identify CHD, thus losing the opportunity for early diagnosis and intensified management” “A more aggressive approach to identifying asymptomatic coronary disease should therefore be considered in this (diabetic) patient population”
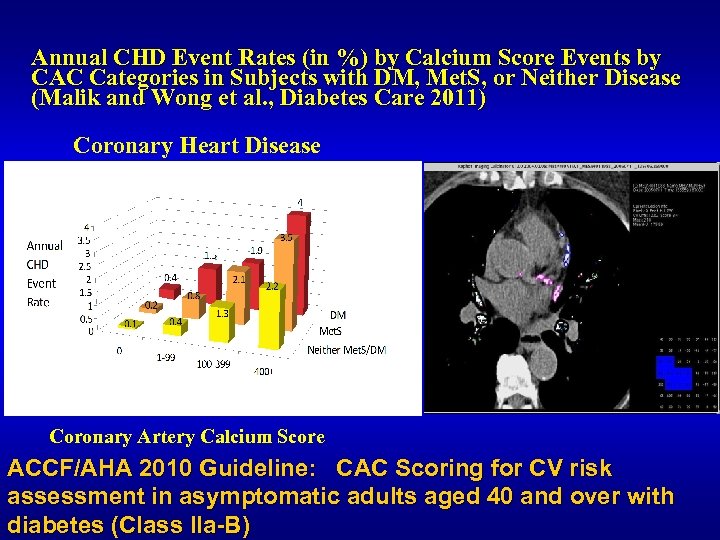
Annual CHD Event Rates (in %) by Calcium Score Events by CAC Categories in Subjects with DM, Met. S, or Neither Disease (Malik and Wong et al. , Diabetes Care 2011) Coronary Heart Disease Coronary Artery Calcium Score ACCF/AHA 2010 Guideline: CAC Scoring for CV risk assessment in asymptomatic adults aged 40 and over with diabetes (Class IIa-B)
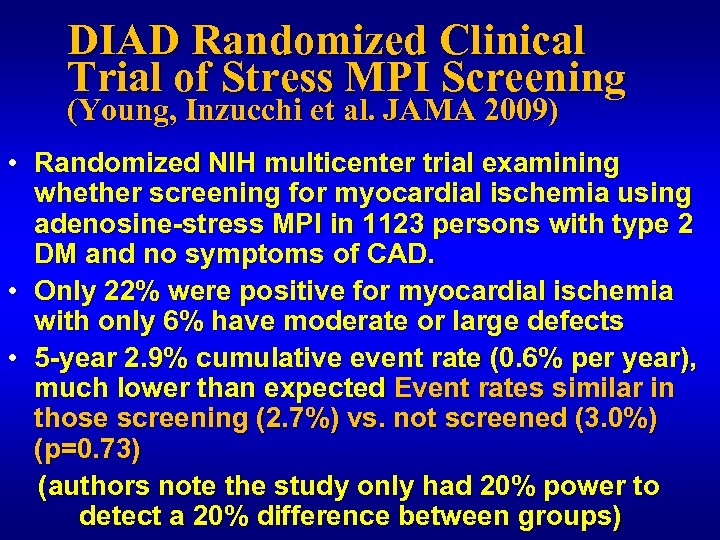
DIAD Randomized Clinical Trial of Stress MPI Screening (Young, Inzucchi et al. JAMA 2009) • Randomized NIH multicenter trial examining whether screening for myocardial ischemia using adenosine-stress MPI in 1123 persons with type 2 DM and no symptoms of CAD. • Only 22% were positive for myocardial ischemia with only 6% have moderate or large defects • 5 -year 2. 9% cumulative event rate (0. 6% per year), much lower than expected Event rates similar in those screening (2. 7%) vs. not screened (3. 0%) (p=0. 73) (authors note the study only had 20% power to detect a 20% difference between groups)
DIAD Study (continued) • The authors conclude that screening for inducible ischemia in asymptomatic patients with T 2 DM cannot be advocated for 4 reasons: • The yield of significant inducible ischemia is very low • Overall cardiac event rates are low • Routine screening does not appear to affect overall outcome • Routine screening would be prohibitively expensive The much lower than expected event rates makes the study inconclusive in demonstrating the lack of efficacy of screening for subclinical CVD
But should we be using stress MPI to screen for CVD in all pts with DM? • Stress MPI is meant to identify short-term risk due to functional deficit, rather than long-term prognosis such as that identified by a test to quantify atherosclerotic burden such as coronary calcium • The radiation and costs are much higher for MPI as compared to coronary calcium, suggesting MPI might be best reserved for those DM at highest risk
ADA 2007 Consensus Statement (Bax et al. Diab Care 2007) “If coronary calcium testing is performed, it appears reasonable to proceed with further testing in diabetic patients with calcium scores >400……. usingle photon emission tomography to assess myocardial perfusion or stress echocardiography to assess ischemic wall motion abnormalities”
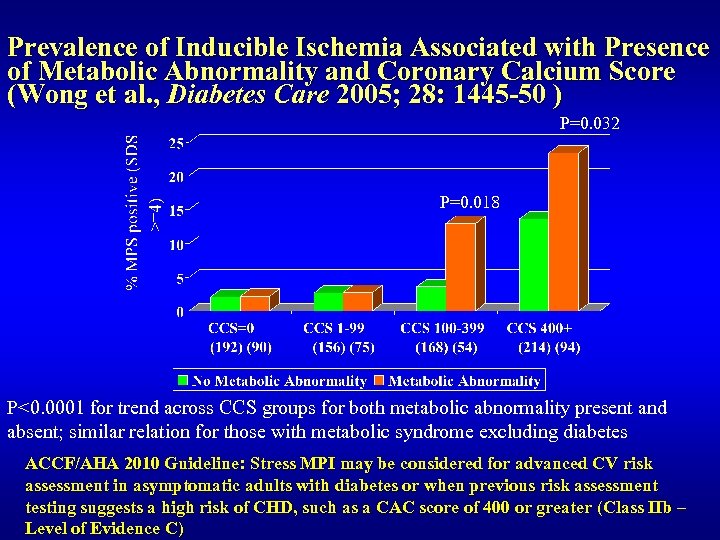
Prevalence of Inducible Ischemia Associated with Presence of Metabolic Abnormality and Coronary Calcium Score (Wong et al. , Diabetes Care 2005; 28: 1445 -50 ) P=0. 032 P=0. 018 P<0. 0001 for trend across CCS groups for both metabolic abnormality present and absent; similar relation for those with metabolic syndrome excluding diabetes ACCF/AHA 2010 Guideline: Stress MPI may be considered for advanced CV risk assessment in asymptomatic adults with diabetes or when previous risk assessment testing suggests a high risk of CHD, such as a CAC score of 400 or greater (Class IIb – Level of Evidence C)
Does Screening for CVD Improve Outcomes? 1) 2) 3) 4) 5) Beneficial Role of Coronary Multidetector CT Screening for 5 -Year All-Cause Mortality among Asymptomatic DM Patients (H Kyung Yang et al. , ADA 2014) Asymptomatic T 2 DM subjects 774 received coronary MDCT and 1548 matched controls did not get screened Groups similar except longer duration DM and higher A 1 c in screened group After 31 month median follow-up, greater lipid decreases and statin prescription in screened group Coronary angiography and revascularization higher in MDCT group
Beneficial Role of Coronary Multidetector CT Screening for 5 -Year All-Cause Mortality among Asymptomatic DM Patients (Yang et al. , ADA 2014) All cause mortality at 5 years lower in the MDCT (4. 5%) vs. non-MDCT (6. 8%) group, p=0. 02 Authors conclude “MDCT may play a beneficial role as a screening test to detect advanced macrovascular complications in asymptomatic T 2 DM patients and to increase survival rate”
Coronary Artery Calcium and Cardiovascular Events in Diabetes: Implications for Primary Prevention Therapies: The Multi-Ethnic Study of Atherosclerosis (MESA) Michael G. Silverman 1, Michael J. Blaha 1, Matthew J. Budoff 2, Ron Blankstein 3, Roger S. Blumenthal 1, Harlan Krumholz 4, Juan J. Rivera 5, Arthur Agatston 6, Nathan D. Wong 7, Steven Shea 8, John Mc. Evoy 1, Khurram Nasir 1, 6 1 Johns Hopkins Ciccarone Center for Prevention of Heart Disease, Baltimore, MD 2 Division of Cardiology, Harbor-UCLA Medical Center, Torrance, CA 3 Brigham and Women's Hospital Non-invasive CV Imaging Program, Boston, MA 4 Yale University School of Medicine, New Haven, CT 5 Division of Cardiology, University of Miami, FL 6 Center for Prevention and Wellness, Baptist Health South Florida, Miami, FL 7 UC Irvine Heart Disease Prevention Program, Irvine, CA 8 College of Physicians and Surgeons, Columbia University, New York, NY Presented at AHA 2012 Presented by: Michael Silverman 15 March 2018 37
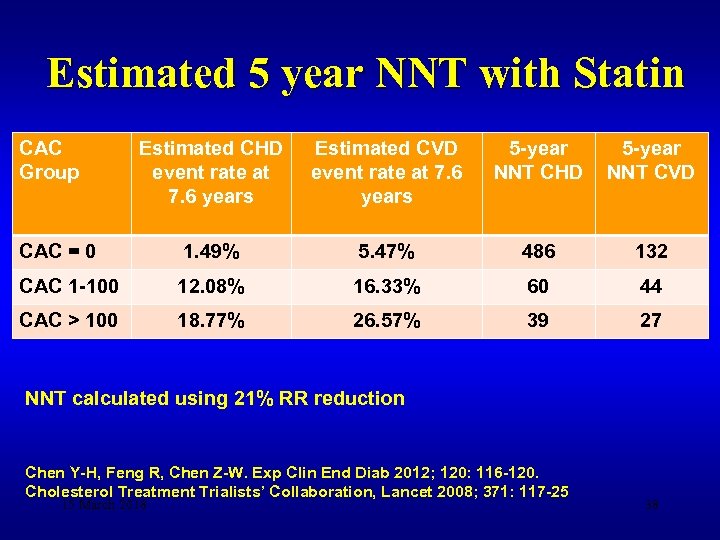
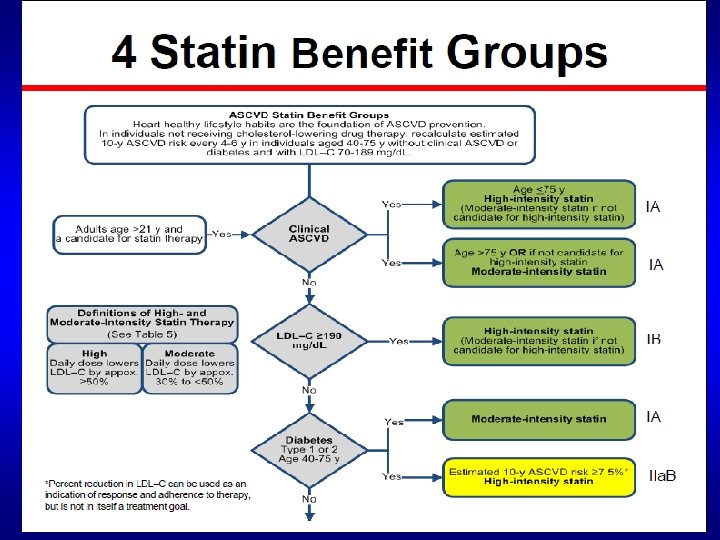
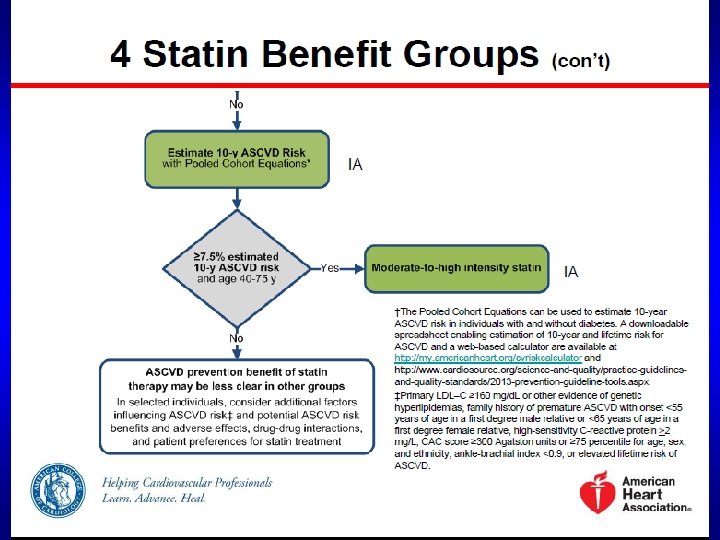
Estimated 5 year NNT with Statin CAC Group Estimated CHD event rate at 7. 6 years Estimated CVD event rate at 7. 6 years 5 -year NNT CHD 5 -year NNT CVD CAC = 0 1. 49% 5. 47% 486 132 CAC 1 -100 12. 08% 16. 33% 60 44 CAC > 100 18. 77% 26. 57% 39 27 NNT calculated using 21% RR reduction Chen Y-H, Feng R, Chen Z-W. Exp Clin End Diab 2012; 120: 116 -120. Cholesterol Treatment Trialists’ Collaboration, Lancet 2008; 371: 117 -25 15 March 2018 38
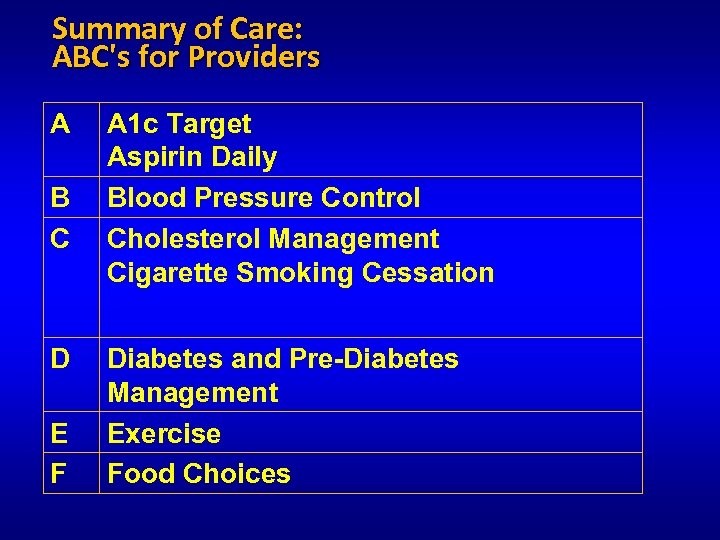
Summary of Care: ABC's for Providers A B C D E F A 1 c Target Aspirin Daily Blood Pressure Control Cholesterol Management Cigarette Smoking Cessation Diabetes and Pre-Diabetes Management Exercise Food Choices
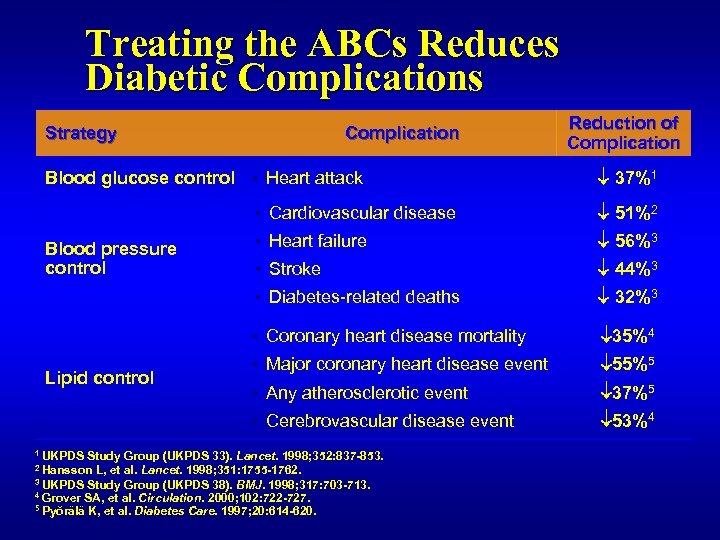
Treating the ABCs Reduces Diabetic Complications Strategy Complication Blood glucose control ▪ Heart attack Reduction of Complication 37%1 ▪ Cardiovascular disease 56%3 ▪ Stroke 44%3 32%3 ▪ Coronary heart disease mortality 35%4 ▪ Major coronary heart disease event 55%5 ▪ Any atherosclerotic event 37%5 ▪ Cerebrovascular disease event Lipid control ▪ Heart failure ▪ Diabetes-related deaths Blood pressure control 51%2 53%4 1 UKPDS Study Group (UKPDS 33). Lancet. 1998; 352: 837 -853. 2 Hansson L, et al. Lancet. 1998; 351: 1755 -1762. 3 UKPDS Study Group (UKPDS 38). BMJ. 1998; 317: 703 -713. 4 Grover SA, et al. Circulation. 2000; 102: 722 -727. 5 Pyŏrälä K, et al. Diabetes Care. 1997; 20: 614 -620.
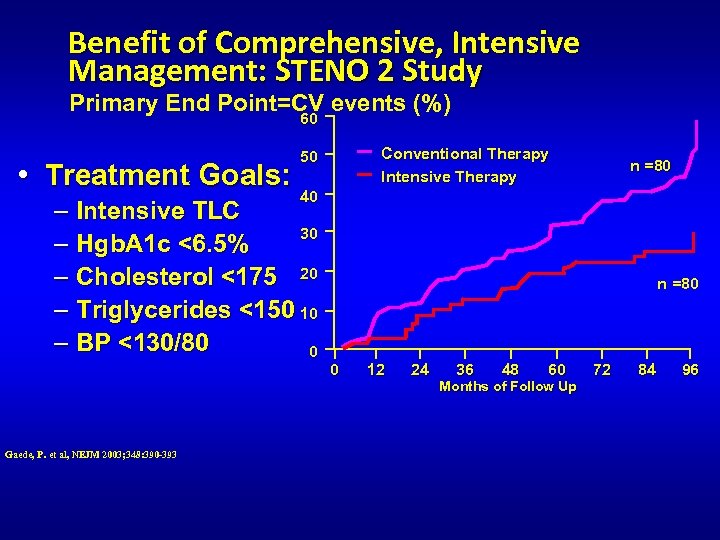
Benefit of Comprehensive, Intensive Management: STENO 2 Study Primary End Point=CV events (%) 60 • Treatment Goals: n =80 40 – Intensive TLC 30 – Hgb. A 1 c <6. 5% – Cholesterol <175 20 – Triglycerides <150 10 – BP <130/80 0 Gaede, P. et al, NEJM 2003; 348: 390 -393 Conventional Therapy Intensive Therapy 50 n =80 0 12 24 36 48 60 Months of Follow Up 72 84 96
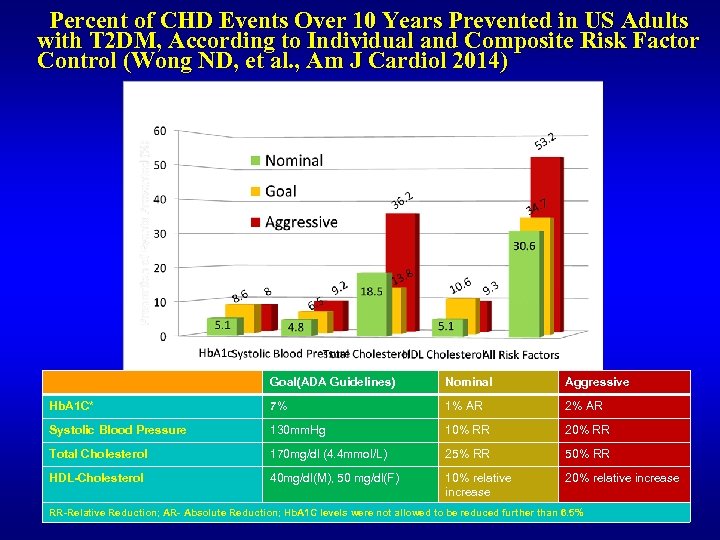
Percent of CHD Events Over 10 Years Prevented in US Adults with T 2 DM, According to Individual and Composite Risk Factor Control (Wong ND, et al. , Am J Cardiol 2014) Goal(ADA Guidelines) Nominal Aggressive Hb. A 1 C* 7% 1% AR 2% AR Systolic Blood Pressure 130 mm. Hg 10% RR 20% RR Total Cholesterol 170 mg/dl (4. 4 mmol/L) 25% RR 50% RR HDL-Cholesterol 40 mg/dl(M), 50 mg/dl(F) 10% relative increase 20% relative increase RR-Relative Reduction; AR- Absolute Reduction; Hb. A 1 C levels were not allowed to be reduced further than 6. 5%
Achieving Risk Factor Targets and CVD Event Risk in Diabetes (Wong et al. ADA 2014) • Potential effects of multifactorial risk factor control are not wellquantitated. • We examined if being at target for LDL-C, Hb. A 1 c, and BP, individually and together, is associated with lower CHD/CVD rates. • 2, 160 multiethnic adults with DM without prior CVD from the ARIC, Jackson, and MESA prospective studies followed for 11 years. • We examined event risk in those at target for LDL-C (<100 mg/dl), Hb. A 1 c (<7%), and blood pressure (BP) (<130/80 mm. Hg) according to American Diabetes Association guidelines. • Overall, 39. 0%, 42. 8%, 30. 5%, and 6. 8% of subjects were at target for LDL-C, Hb. A 1 c, and BP, and all three factors • Being at composite target (vs one or more factors not at target) was associated with a significantly reduced risk of CHD (HR=0. 46, 95% CI = 0. 25 -0. 87) and CVD (HR=0. 66, 95% CI=0. 45 -0. 98) events. • Optimal levels of lipids, blood pressure, and glucose control together are uncommon in persons with DM, but are associated with substantially lower CHD and CVD risks.

Control of DM Risk Factors in a Large Multipayer Outpatient Population in Northern California (n=15, 826) (Holland et al. , J Diab Complic 2013) Individual control of Hb. A 1 c, BP, and LDL ranged from 42 -78% in Asians Composite control of Hb. A 1 c, BP, and LDL ranged from 21 -27% in Asians
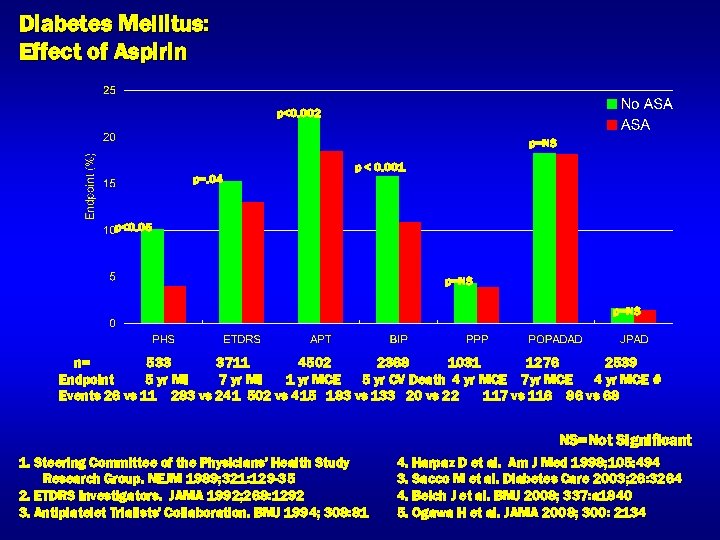
Diabetes Mellitus: Effect of Aspirin p<0. 002 p=NS p=. 04 p < 0. 001 p<0. 05 p=NS n= 533 3711 4502 2368 1031 1276 2539 Endpoint 5 yr MI 7 yr MI 1 yr MCE 5 yr CV Death 4 yr MCE 7 yr MCE 4 yr MCE # Events 26 vs 11 283 vs 241 502 vs 415 183 vs 133 20 vs 22 117 vs 116 86 vs 68 NS=Not Significant 1. Steering Committee of the Physicians' Health Study Research Group. NEJM 1989; 321: 129 -35 2. ETDRS Investigators. JAMA 1992; 268: 1292 3. Antiplatelet Trialists' Collaboration. BMJ 1994; 308: 81 4. Harpaz D et al. Am J Med 1998; 105: 494 3. Sacco M et al. Diabetes Care 2003; 26: 3264 4. Belch J et al. BMJ 2008; 337: a 1840 5. Ogawa H et al. JAMA 2008; 300: 2134
Recommendations: Antiplatelet Agents (1) • Consider aspirin therapy (75– 162 mg/day) (C) – As a primary prevention strategy in those with type 1 or type 2 diabetes at increased cardiovascular risk (10 -year risk >10%) – Includes most men >50 years of age or women >60 years of age who have at least one additional major risk factor u Family history of CVD u Hypertension u Smoking u Dyslipidemia u Albuminuria ADA. VI. Prevention, Management of Complications. Diabetes Care 2013; 36(suppl 1): S 32 -S 33.
Recommendations: Antiplatelet Agents (2) • Aspirin should not be recommended for CVD prevention for adults with diabetes at low CVD risk, since potential adverse effects from bleeding likely offset potential benefits (C) • 10 -year CVD risk <5%: men <50 and women <60 years of age with no major additional CVD risk factors • In patients in these age groups with multiple other risk factors (10 -year risk 5– 10%), clinical judgment is required (E) ADA. VI. Prevention, Management of Complications. Diabetes Care 2013; 36(suppl 1): S 33.

Recommendations: Antiplatelet Agents (3) • Use aspirin therapy (75– 162 mg/day) – Secondary prevention strategy in those with diabetes with a history of CVD (A) • For patients with CVD and documented aspirin allergy – Clopidogrel (75 mg/day) should be used (B) • Combination therapy with aspirin (75– 162 mg/day) and clopidogrel (75 mg/day) – Reasonable for up to a year after an acute coronary syndrome (B) ADA. VI. Prevention, Management of Complications. Diabetes Care 2013; 36(suppl 1): S 33 -S 34.
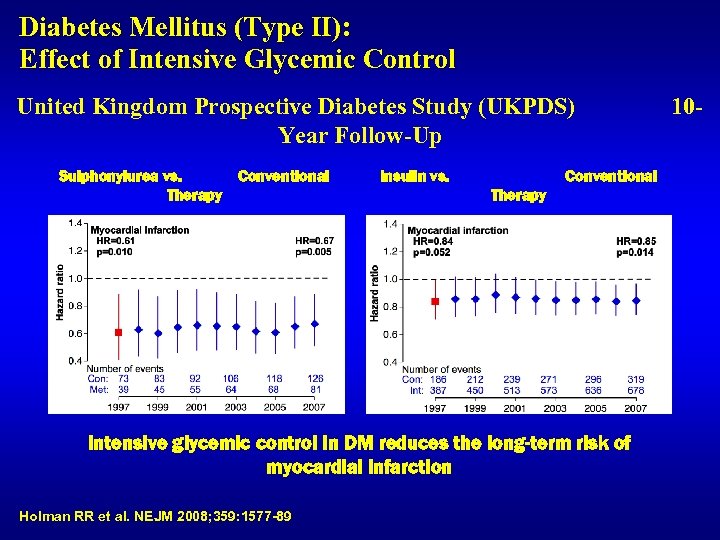
Diabetes Mellitus (Type II): Effect of Intensive Glycemic Control United Kingdom Prospective Diabetes Study (UKPDS) Year Follow-Up Sulphonylurea vs. Conventional Therapy Insulin vs. Conventional Therapy Intensive glycemic control in DM reduces the long-term risk of myocardial infarction Holman RR et al. NEJM 2008; 359: 1577 -89 10 -
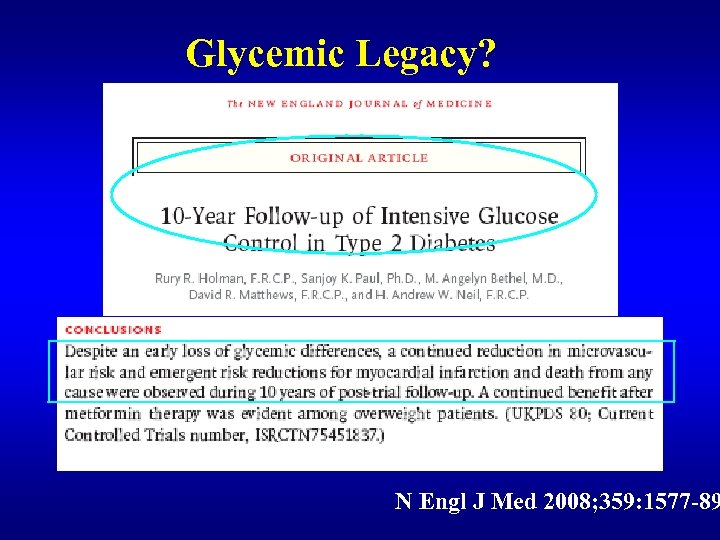
Glycemic Legacy? N Engl J Med 2008; 359: 1577 -89
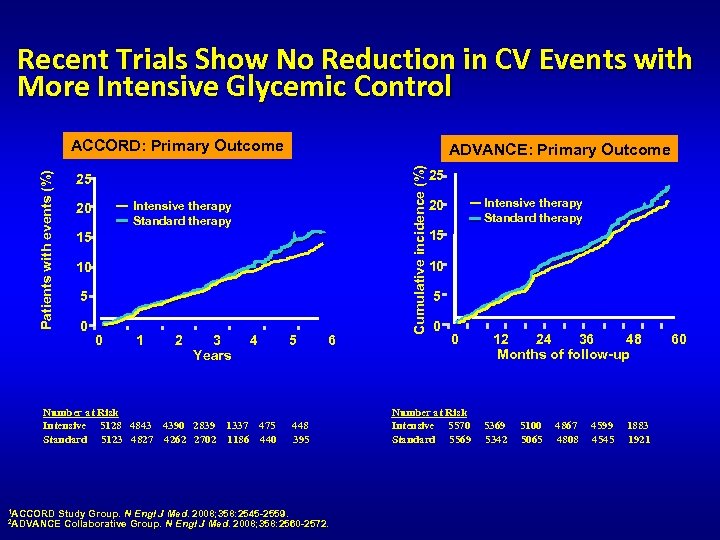
Recent Trials Show No Reduction in CV Events with More Intensive Glycemic Control ADVANCE: Primary Outcome 25 Intensive therapy Standard therapy 20 15 10 5 0 0 1 2 3 4 5 6 Years Number at Risk Intensive 5128 4843 4390 2839 1337 475 Standard 5123 4827 4262 2702 1186 440 1 ACCORD Study Group. N 448 395 Engl J Med. 2008; 358: 2545 -2559. Engl J Med. 2008; 358: 2560 -2572. 2 ADVANCE Collaborative Group. N Cumulative incidence (%) Patients with events (%) ACCORD: Primary Outcome 25 Intensive therapy Standard therapy 20 15 10 5 0 0 12 24 36 48 60 Months of follow-up Number at Risk Intensive 5570 Standard 5569 5342 5100 5065 4867 4808 4599 4545 1883 1921
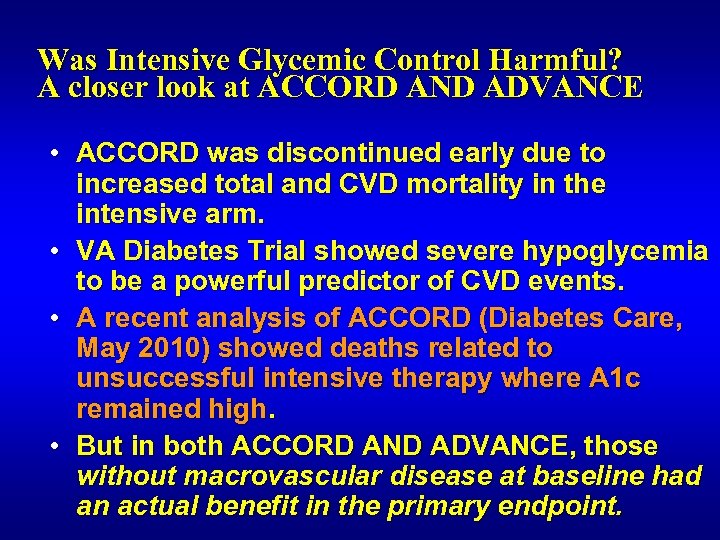
Was Intensive Glycemic Control Harmful? A closer look at ACCORD AND ADVANCE • ACCORD was discontinued early due to increased total and CVD mortality in the intensive arm. • VA Diabetes Trial showed severe hypoglycemia to be a powerful predictor of CVD events. • A recent analysis of ACCORD (Diabetes Care, May 2010) showed deaths related to unsuccessful intensive therapy where A 1 c remained high. • But in both ACCORD AND ADVANCE, those without macrovascular disease at baseline had an actual benefit in the primary endpoint.
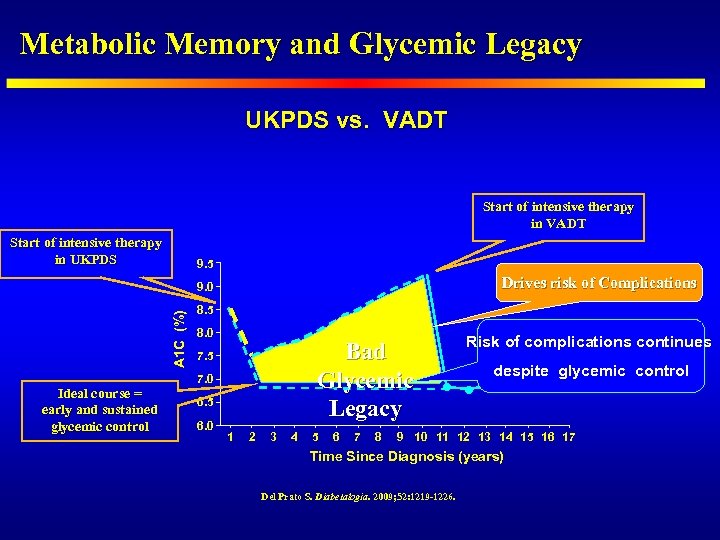
Metabolic Memory and Glycemic Legacy UKPDS vs. VADT Start of intensive therapy in UKPDS 9. 5 Drives risk of Complications A 1 C (%) 9. 0 Ideal course = early and sustained glycemic control 8. 5 8. 0 Bad Glycemic Legacy 7. 5 7. 0 6. 5 6. 0 1 2 3 4 5 6 7 8 Risk of complications continues despite glycemic control 9 10 11 12 13 14 15 16 17 Time Since Diagnosis (years) Del Prato S. Diabetalogia. 2009; 52: 1219 -1226.
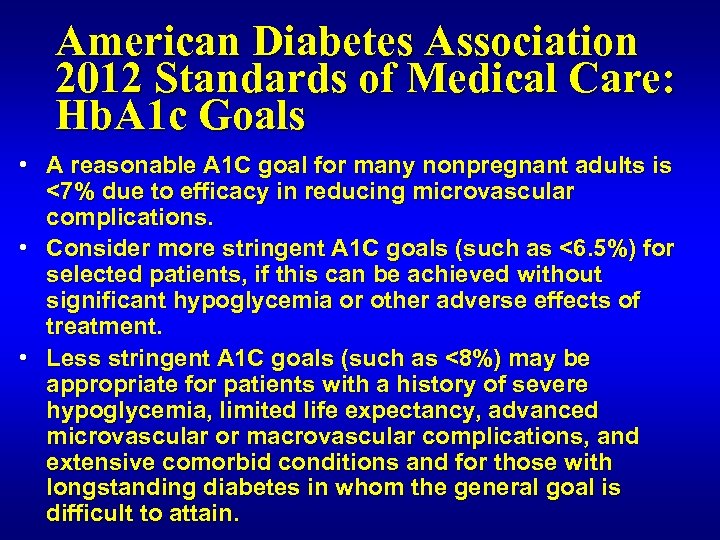
American Diabetes Association 2012 Standards of Medical Care: Hb. A 1 c Goals • A reasonable A 1 C goal for many nonpregnant adults is <7% due to efficacy in reducing microvascular complications. • Consider more stringent A 1 C goals (such as <6. 5%) for selected patients, if this can be achieved without significant hypoglycemia or other adverse effects of treatment. • Less stringent A 1 C goals (such as <8%) may be appropriate for patients with a history of severe hypoglycemia, limited life expectancy, advanced microvascular or macrovascular complications, and extensive comorbid conditions and for those with longstanding diabetes in whom the general goal is difficult to attain.
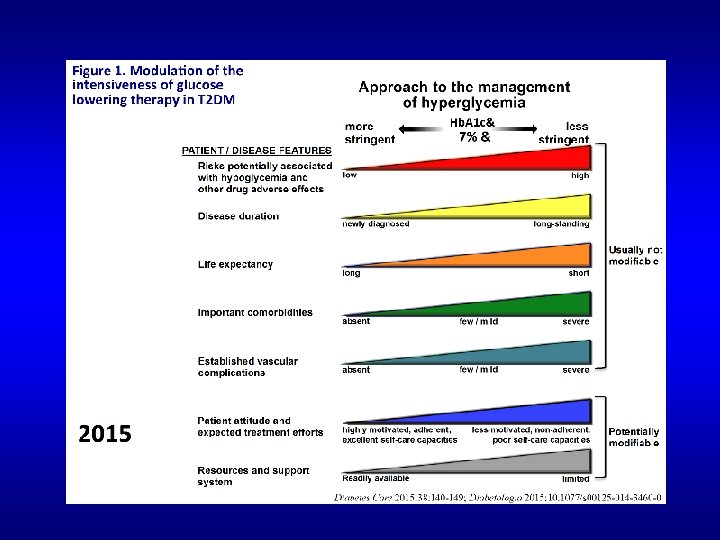
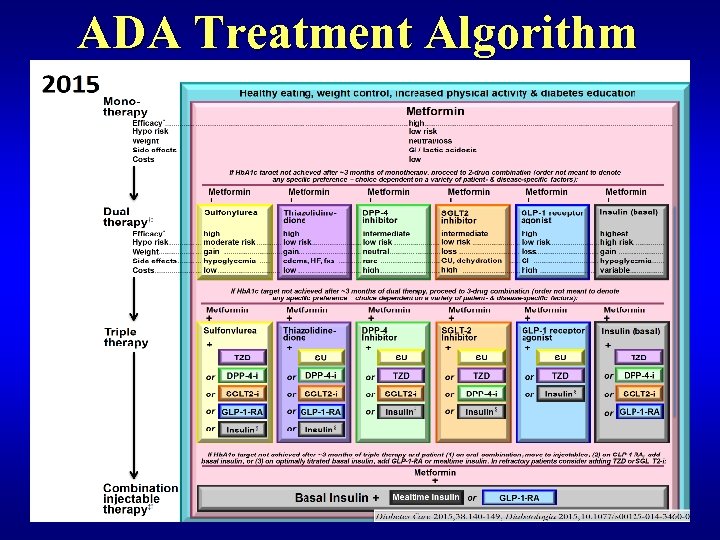
ADA Treatment Algorithm
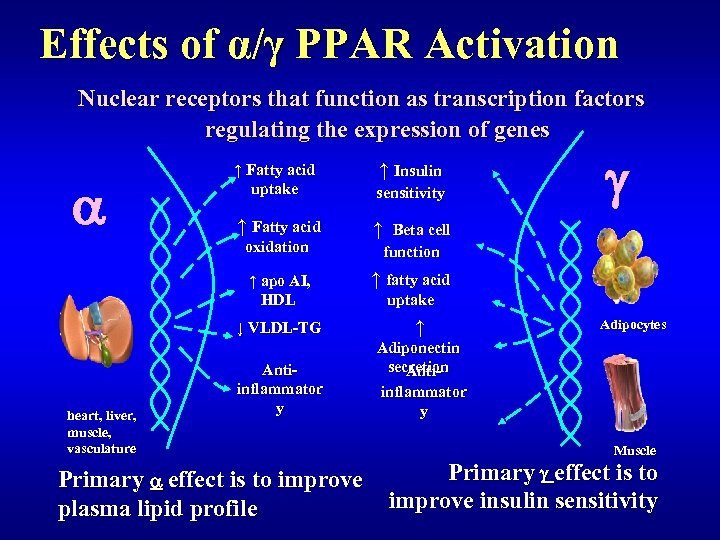
Effects of α/γ PPAR Activation Nuclear receptors that function as transcription factors regulating the expression of genes a ↑ Insulin ↑ Fatty acid uptake sensitivity ↑ Fatty acid ↑ oxidation ↑ apo AI, HDL Beta cell function ↑ fatty acid uptake ↓ VLDL-TG heart, liver, muscle, vasculature g ↑ Antiinflammator y Adiponectin secretion Antiinflammator y Primary a effect is to improve plasma lipid profile Adipocytes Muscle Primary g effect is to improve insulin sensitivity
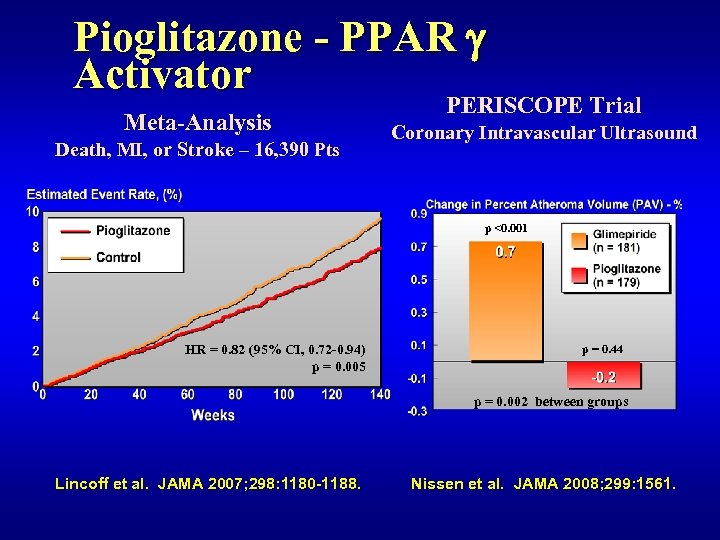
Pioglitazone - PPAR g Activator Meta-Analysis Death, MI, or Stroke – 16, 390 Pts PERISCOPE Trial Coronary Intravascular Ultrasound p <0. 001 HR = 0. 82 (95% CI, 0. 72 -0. 94) p = 0. 005 p = 0. 44 p = 0. 002 between groups Lincoff et al. JAMA 2007; 298: 1180 -1188. Nissen et al. JAMA 2008; 299: 1561.
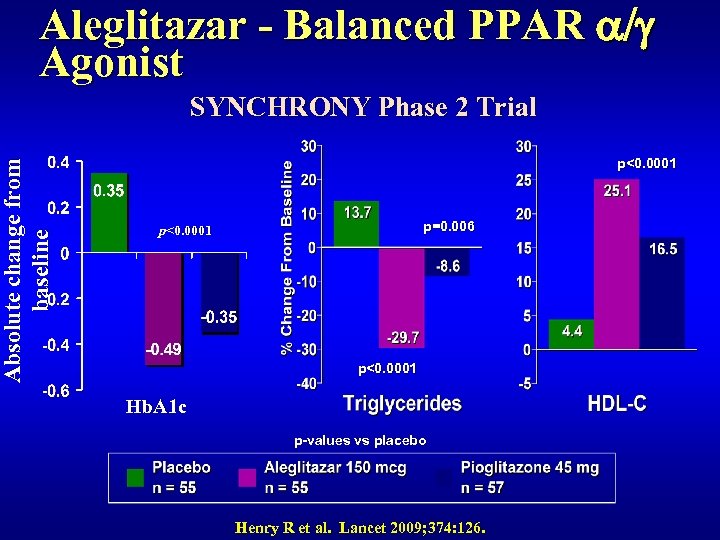
Absolute change from baseline Aleglitazar - Balanced PPAR a/g Agonist SYNCHRONY Phase 2 Trial p<0. 0001 p=0. 006 p<0. 0001 Hb. A 1 c p-values vs placebo Henry R et al. Lancet 2009; 374: 126.
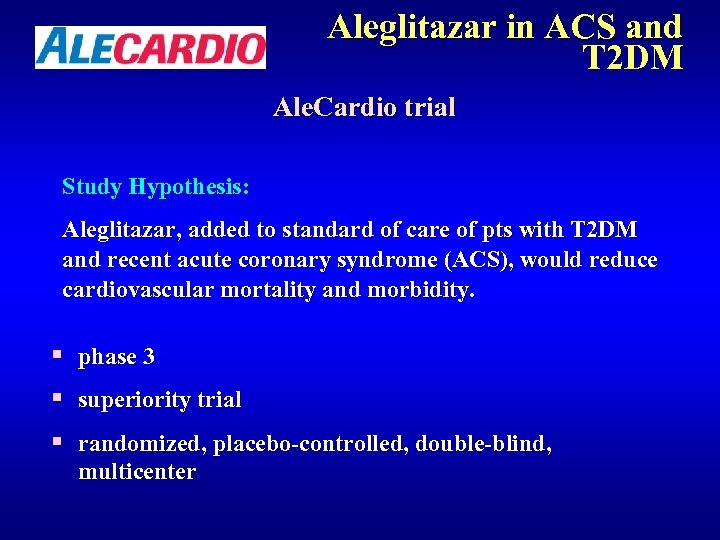
Aleglitazar in ACS and T 2 DM Ale. Cardio trial Study Hypothesis: Aleglitazar, added to standard of care of pts with T 2 DM and recent acute coronary syndrome (ACS), would reduce cardiovascular mortality and morbidity. § phase 3 § superiority trial § randomized, placebo-controlled, double-blind, multicenter
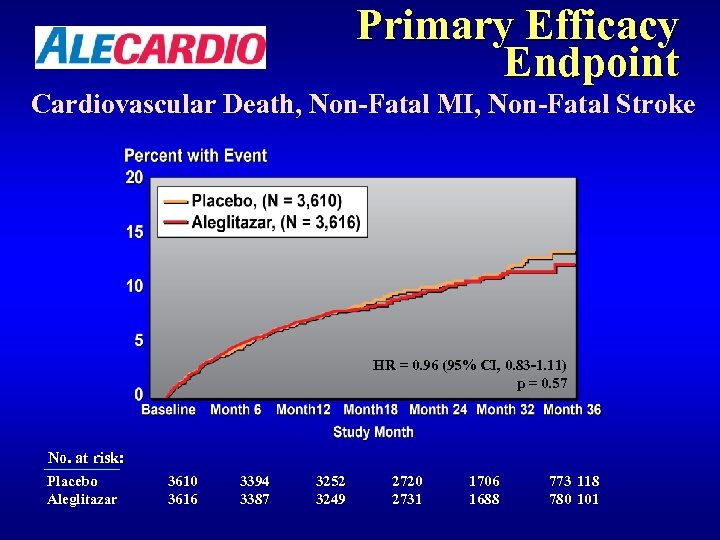
Primary Efficacy Endpoint Cardiovascular Death, Non-Fatal MI, Non-Fatal Stroke HR = 0. 96 (95% CI, 0. 83 -1. 11) p = 0. 57 No. at risk: Placebo Aleglitazar 3610 3616 3394 3387 3252 3249 2720 2731 1706 1688 773 118 780 101
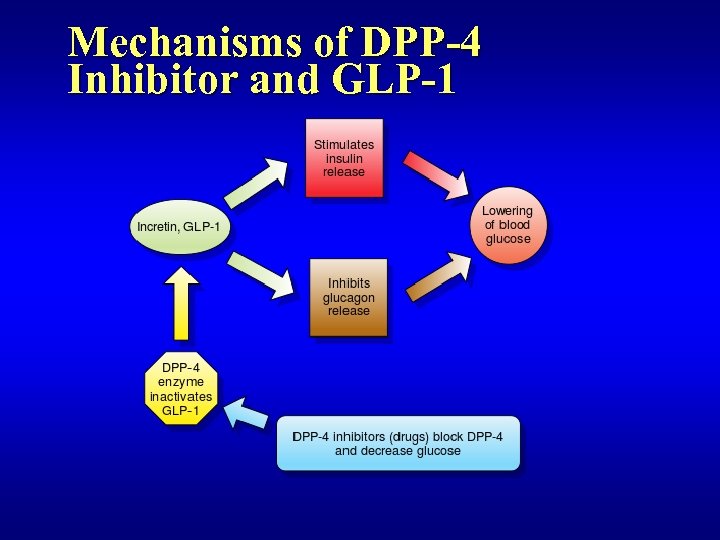
Mechanisms of DPP-4 Inhibitor and GLP-1
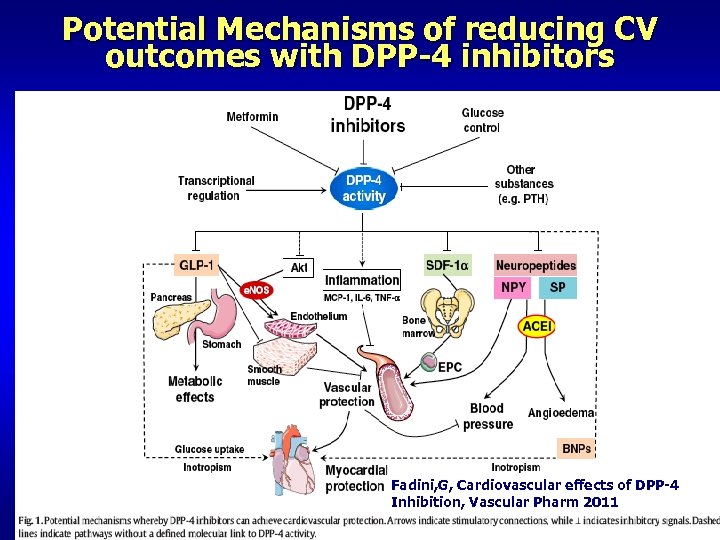
Potential Mechanisms of reducing CV outcomes with DPP-4 inhibitors Fadini, G, Cardiovascular effects of DPP-4 Inhibition, Vascular Pharm 2011
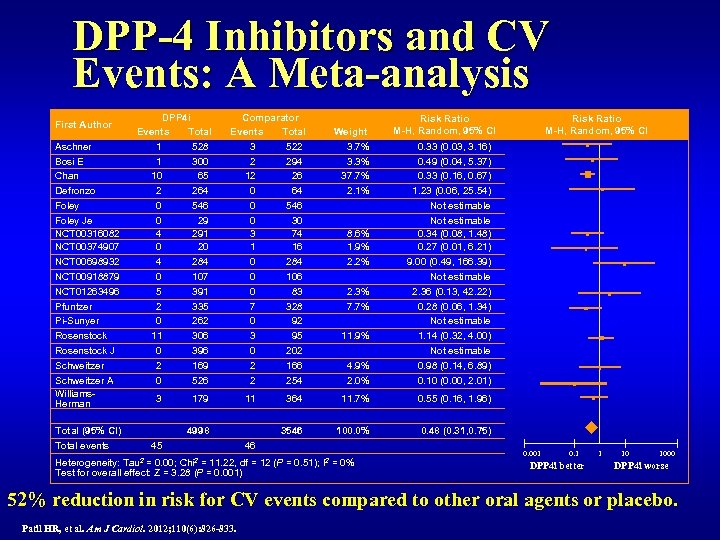
DPP-4 Inhibitors and CV Events: A Meta-analysis First Author Aschner Bosi E Chan Defronzo Foley Je NCT 00316082 NCT 00374907 NCT 00698932 NCT 00918879 NCT 01263496 Pfuntzer Pi-Sunyer Rosenstock J Schweitzer A Williams. Herman DPP 4 i Events Total 1 528 1 300 10 65 2 264 0 546 0 29 4 291 0 20 4 284 0 107 5 391 2 335 0 262 11 306 0 396 2 169 0 526 3 Total (95% CI) Total events Comparator Events Total 3 522 2 294 12 26 0 64 0 546 0 30 3 74 1 16 0 284 0 106 0 83 7 328 0 92 3 95 0 202 2 166 2 254 179 45 4. 9% 2. 0% 364 11. 7% 0. 55 (0. 16, 1. 96) 100. 0% Risk Ratio M-H, Random, 95% CI 0. 33 (0. 03, 3. 16) 0. 49 (0. 04, 5. 37) 0. 33 (0. 16, 0. 67) 1. 23 (0. 06, 25. 54) Not estimable 0. 34 (0. 08, 1. 48) 0. 27 (0. 01, 6. 21) 9. 00 (0. 49, 166. 39) Not estimable 2. 36 (0. 13, 42. 22) 0. 28 (0. 06, 1. 34) Not estimable 1. 14 (0. 32, 4. 00) Not estimable 0. 98 (0. 14, 6. 89) 0. 10 (0. 00, 2. 01) 0. 48 (0. 31, 0. 75) 8. 6% 1. 9% 2. 2% 2. 3% 7. 7% 11. 9% 46 Chi 2 Risk Ratio M-H, Random, 95% CI 3546 11 4998 Tau 2 Weight 3. 7% 3. 3% 37. 7% 2. 1% Heterogeneity: = 0. 00; = 11. 22, df = 12 (P = 0. 51); I 2 = 0% Test for overall effect: Z = 3. 28 (P = 0. 001) 0. 001 0. 1 DPP 4 i better 1 10 1000 DPP 4 i worse 52% reduction in risk for CV events compared to other oral agents or placebo. Patil HR, et al. Am J Cardiol. 2012; 110(6): 826 -833.
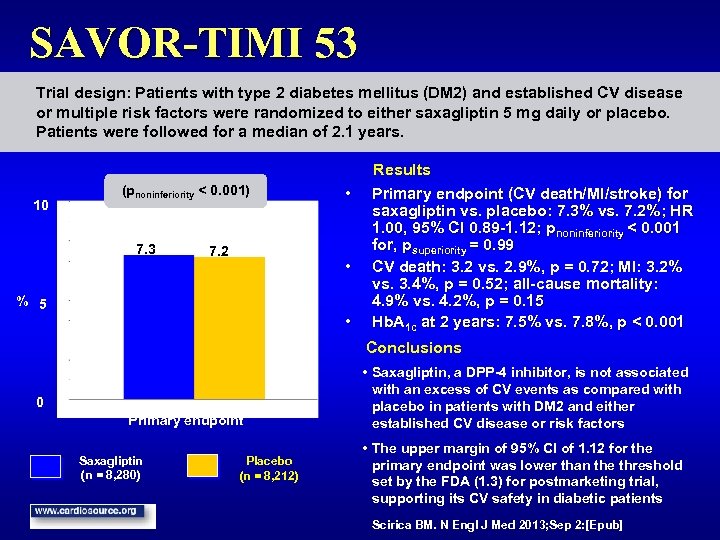
SAVOR-TIMI 53 Trial design: Patients with type 2 diabetes mellitus (DM 2) and established CV disease or multiple risk factors were randomized to either saxagliptin 5 mg daily or placebo. Patients were followed for a median of 2. 1 years. 10 (pnoninferiority < 0. 001) 7. 3 7. 2 • • % 5 • Results Primary endpoint (CV death/MI/stroke) for saxagliptin vs. placebo: 7. 3% vs. 7. 2%; HR 1. 00, 95% CI 0. 89 -1. 12; pnoninferiority < 0. 001 for, psuperiority = 0. 99 CV death: 3. 2 vs. 2. 9%, p = 0. 72; MI: 3. 2% vs. 3. 4%, p = 0. 52; all-cause mortality: 4. 9% vs. 4. 2%, p = 0. 15 Hb. A 1 c at 2 years: 7. 5% vs. 7. 8%, p < 0. 001 Conclusions 0 Primary endpoint Saxagliptin (n = 8, 280) Placebo (n = 8, 212) • Saxagliptin, a DPP-4 inhibitor, is not associated with an excess of CV events as compared with placebo in patients with DM 2 and either established CV disease or risk factors • The upper margin of 95% CI of 1. 12 for the primary endpoint was lower than the threshold set by the FDA (1. 3) for postmarketing trial, supporting its CV safety in diabetic patients Scirica BM. N Engl J Med 2013; Sep 2: [Epub]
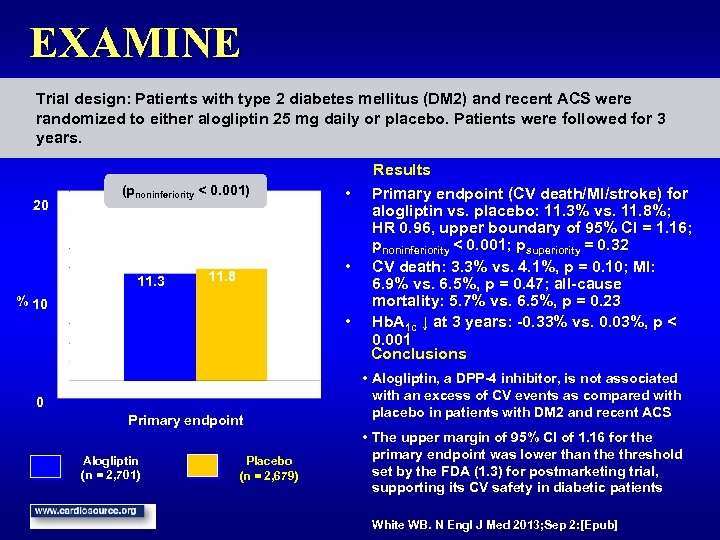
EXAMINE Trial design: Patients with type 2 diabetes mellitus (DM 2) and recent ACS were randomized to either alogliptin 25 mg daily or placebo. Patients were followed for 3 years. 20 (pnoninferiority < 0. 001) 11. 3 • • 11. 8 % 10 • 0 Primary endpoint Alogliptin (n = 2, 701) Placebo (n = 2, 679) Results Primary endpoint (CV death/MI/stroke) for alogliptin vs. placebo: 11. 3% vs. 11. 8%; HR 0. 96, upper boundary of 95% CI = 1. 16; pnoninferiority < 0. 001; psuperiority = 0. 32 CV death: 3. 3% vs. 4. 1%, p = 0. 10; MI: 6. 9% vs. 6. 5%, p = 0. 47; all-cause mortality: 5. 7% vs. 6. 5%, p = 0. 23 Hb. A 1 c ↓ at 3 years: -0. 33% vs. 0. 03%, p < 0. 001 Conclusions • Alogliptin, a DPP-4 inhibitor, is not associated with an excess of CV events as compared with placebo in patients with DM 2 and recent ACS • The upper margin of 95% CI of 1. 16 for the primary endpoint was lower than the threshold set by the FDA (1. 3) for postmarketing trial, supporting its CV safety in diabetic patients White WB. N Engl J Med 2013; Sep 2: [Epub]
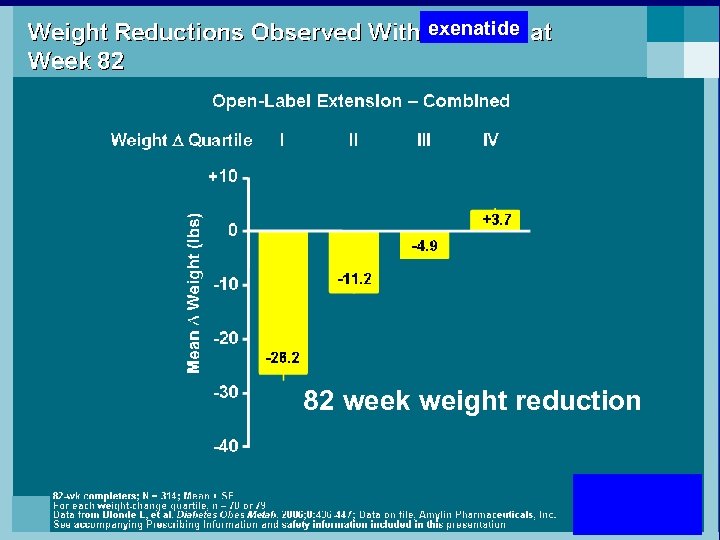
exenatide 82 week weight reduction 67
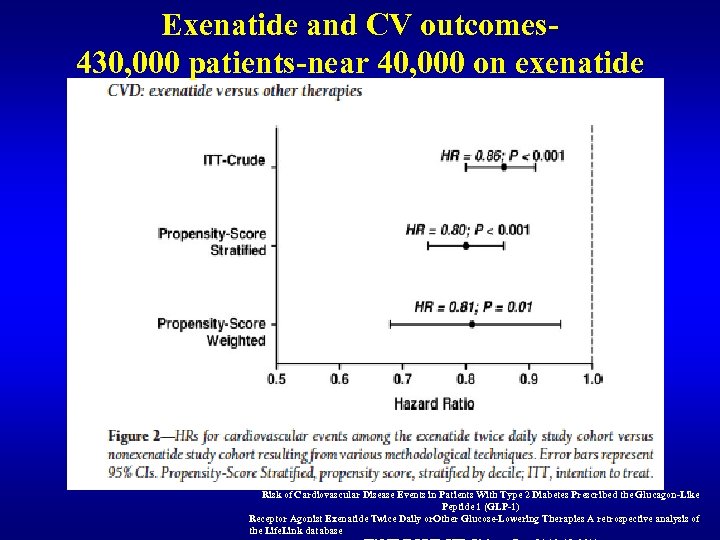
Exenatide and CV outcomes 430, 000 patients-near 40, 000 on exenatide Risk of Cardiovascular Disease Events in Patients With Type 2 Diabetes Prescribed the Glucagon-Like Peptide 1 (GLP-1) Receptor Agonist Exenatide Twice Daily or. Other Glucose-Lowering Therapies A retrospective analysis of the Life. Link database
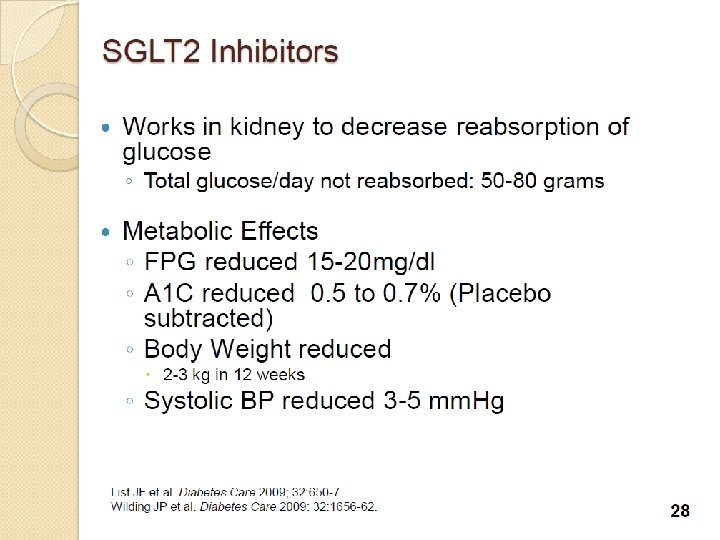
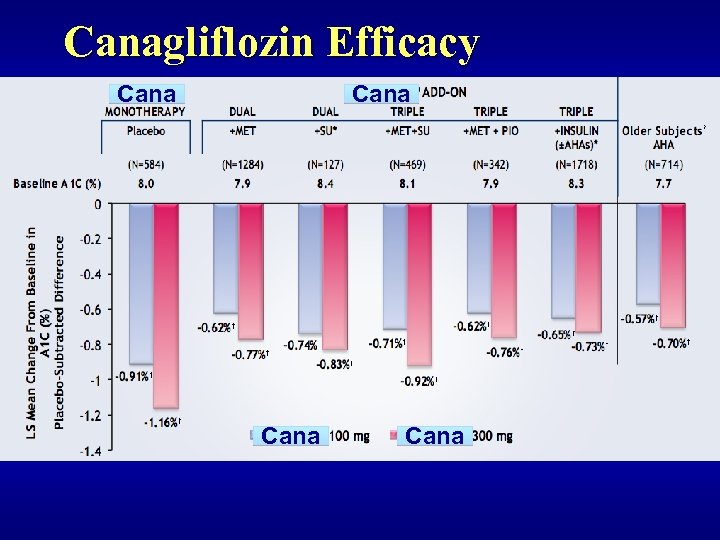
Canagliflozin Efficacy Cana
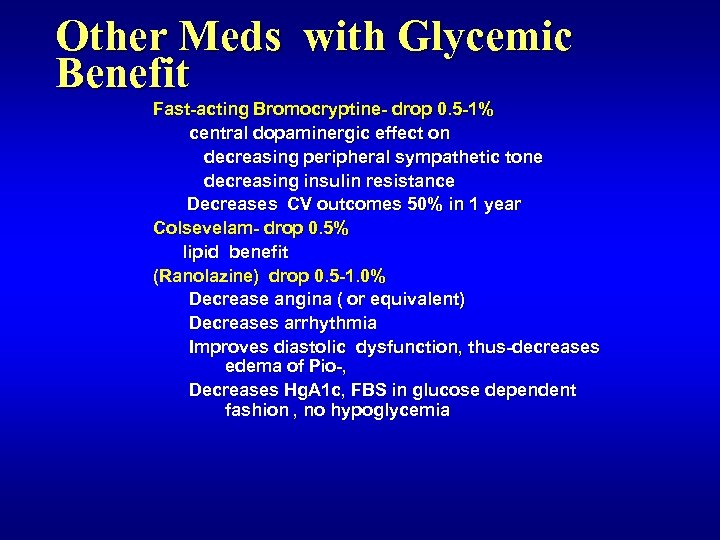
Other Meds with Glycemic Benefit Fast-acting Bromocryptine- drop 0. 5 -1% central dopaminergic effect on decreasing peripheral sympathetic tone decreasing insulin resistance Decreases CV outcomes 50% in 1 year Colsevelam- drop 0. 5% lipid benefit (Ranolazine) drop 0. 5 -1. 0% Decrease angina ( or equivalent) Decreases arrhythmia Improves diastolic dysfunction, thus-decreases edema of Pio-, Decreases Hg. A 1 c, FBS in glucose dependent fashion , no hypoglycemia
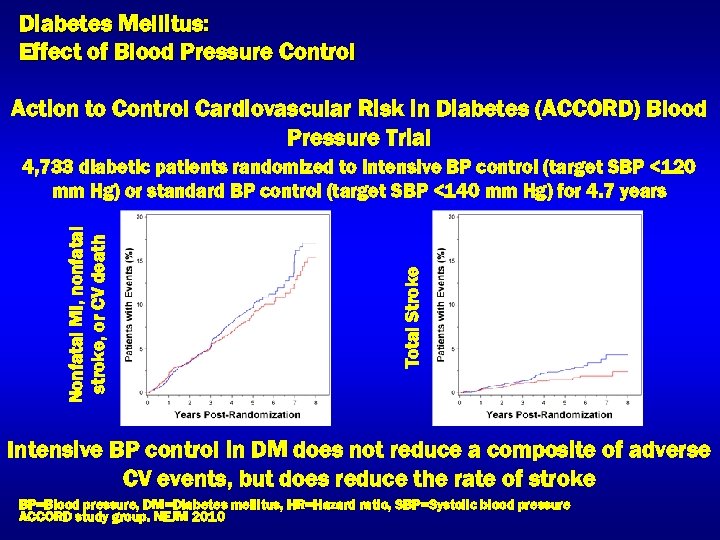
Diabetes Mellitus: Effect of Blood Pressure Control Action to Control Cardiovascular Risk in Diabetes (ACCORD) Blood Pressure Trial HR=0. 88 95% CI (0. 73 -1. 06) HR=0. 59 95% CI (0. 39 -0. 89) Total Stroke Nonfatal MI, nonfatal stroke, or CV death 4, 733 diabetic patients randomized to intensive BP control (target SBP <120 mm Hg) or standard BP control (target SBP <140 mm Hg) for 4. 7 years Intensive BP control in DM does not reduce a composite of adverse CV events, but does reduce the rate of stroke BP=Blood pressure, DM=Diabetes mellitus, HR=Hazard ratio, SBP=Systolic blood pressure ACCORD study group. NEJM 2010
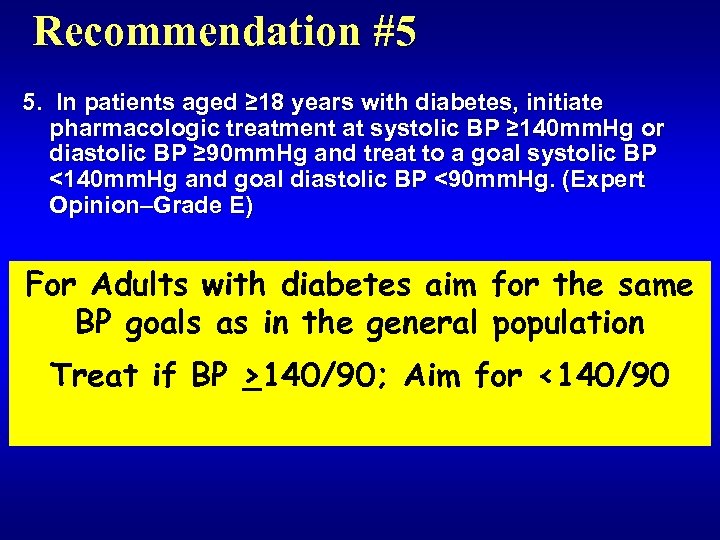
Recommendation #5 5. In patients aged ≥ 18 years with diabetes, initiate pharmacologic treatment at systolic BP ≥ 140 mm. Hg or diastolic BP ≥ 90 mm. Hg and treat to a goal systolic BP <140 mm. Hg and goal diastolic BP <90 mm. Hg. (Expert Opinion–Grade E) For Adults with diabetes aim for the same BP goals as in the general population Treat if BP >140/90; Aim for <140/90
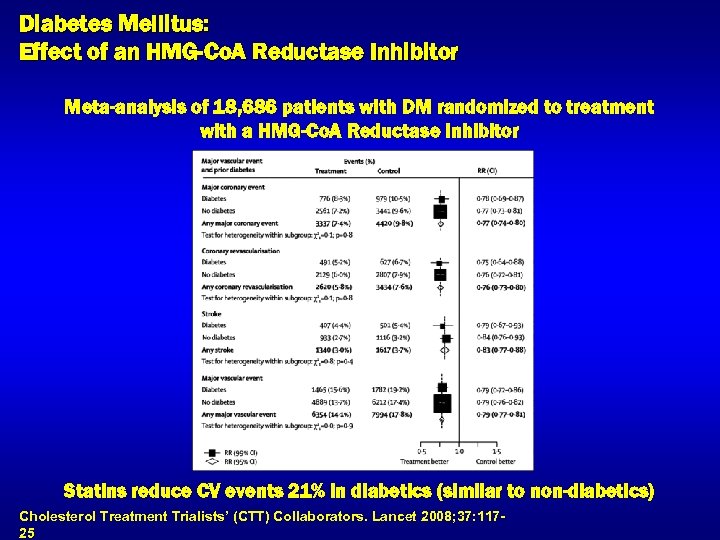
Diabetes Mellitus: Effect of an HMG-Co. A Reductase Inhibitor Meta-analysis of 18, 686 patients with DM randomized to treatment with a HMG-Co. A Reductase Inhibitor Statins reduce CV events 21% in diabetics (similar to non-diabetics) Cholesterol Treatment Trialists’ (CTT) Collaborators. Lancet 2008; 37: 11725
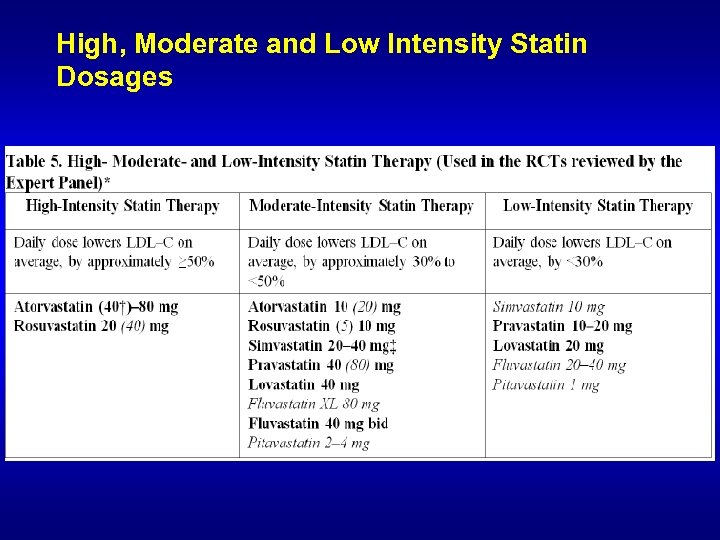
High, Moderate and Low Intensity Statin Dosages
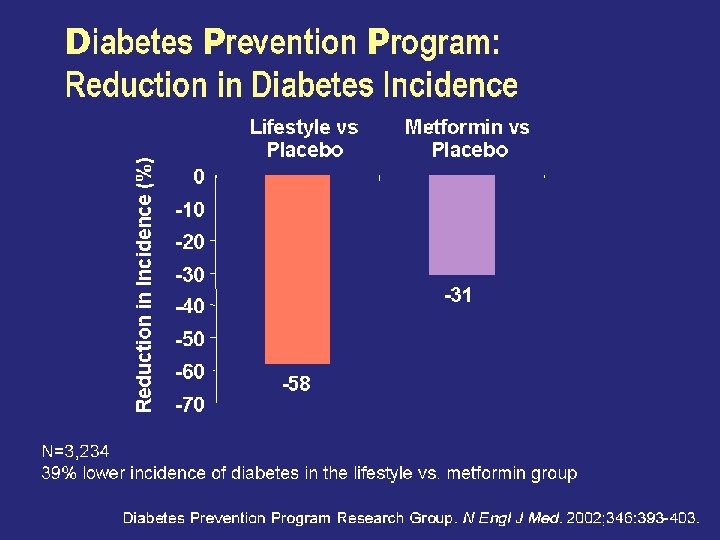
Diabetes Prevention Program: Reduction in Diabetes Incidence
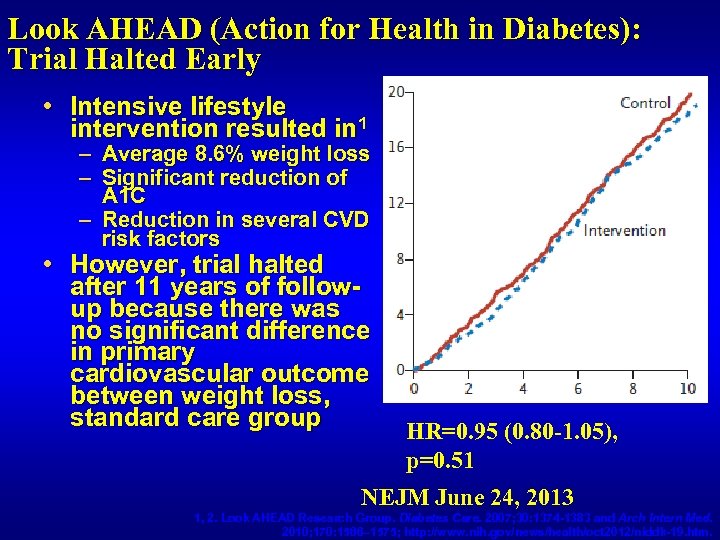
Look AHEAD (Action for Health in Diabetes): Trial Halted Early • Intensive lifestyle intervention resulted in 1 – Average 8. 6% weight loss – Significant reduction of A 1 C – Reduction in several CVD risk factors • However, trial halted after 11 years of followup because there was no significant difference in primary cardiovascular outcome between weight loss, standard care group HR=0. 95 (0. 80 -1. 05), p=0. 51 NEJM June 24, 2013 1, 2. Look AHEAD Research Group. Diabetes Care. 2007; 30: 1374 -1383 and Arch Intern Med. 2010; 170: 1566– 1575; http: //www. nih. gov/news/health/oct 2012/niddk-19. htm.
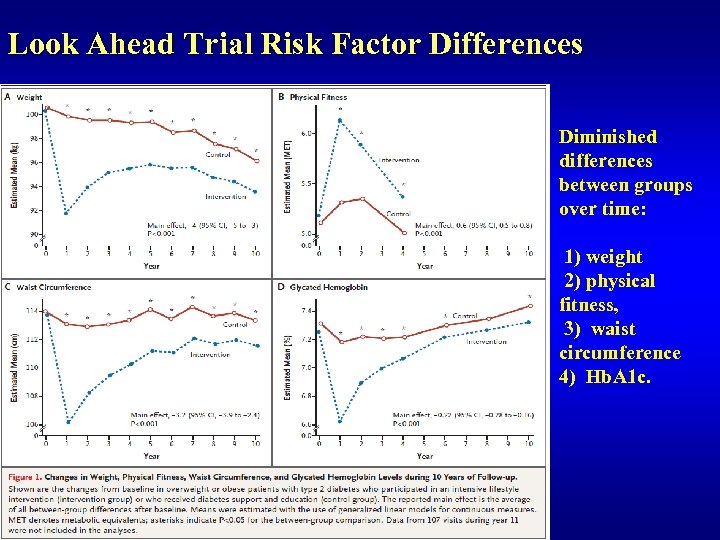
Look Ahead Trial Risk Factor Differences Diminished differences between groups over time: 1) weight 2) physical fitness, 3) waist circumference 4) Hb. A 1 c.
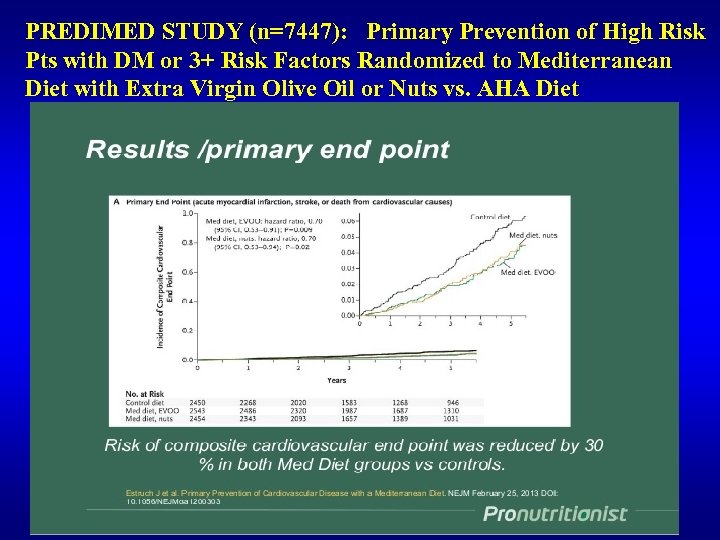
PREDIMED STUDY (n=7447): Primary Prevention of High Risk Pts with DM or 3+ Risk Factors Randomized to Mediterranean Diet with Extra Virgin Olive Oil or Nuts vs. AHA Diet
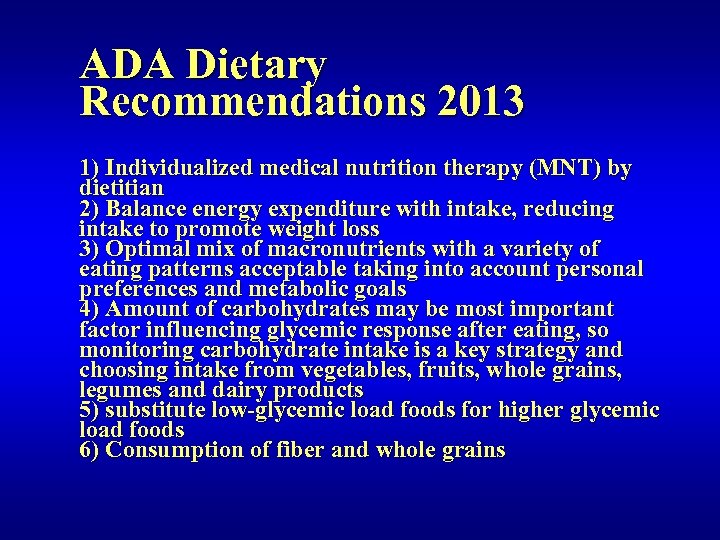
ADA Dietary Recommendations 2013 1) Individualized medical nutrition therapy (MNT) by dietitian 2) Balance energy expenditure with intake, reducing intake to promote weight loss 3) Optimal mix of macronutrients with a variety of eating patterns acceptable taking into account personal preferences and metabolic goals 4) Amount of carbohydrates may be most important factor influencing glycemic response after eating, so monitoring carbohydrate intake is a key strategy and choosing intake from vegetables, fruits, whole grains, legumes and dairy products 5) substitute low-glycemic load foods for higher glycemic load foods 6) Consumption of fiber and whole grains
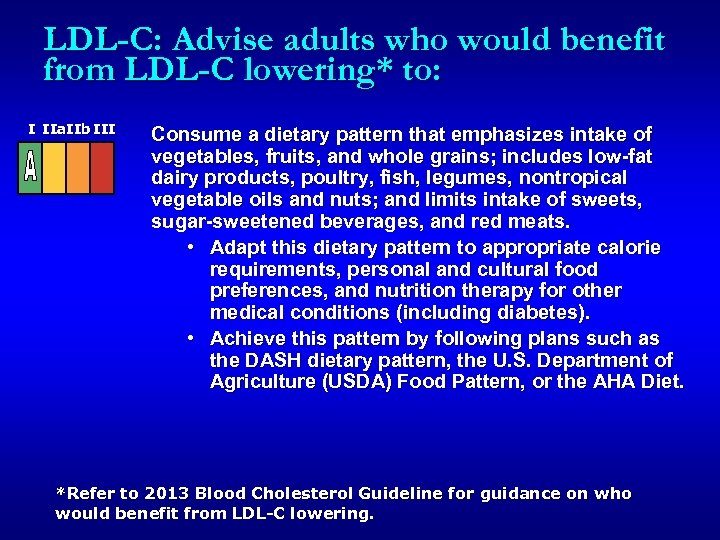
LDL-C: Advise adults who would benefit from LDL-C lowering* to: I IIa. IIb III Consume a dietary pattern that emphasizes intake of vegetables, fruits, and whole grains; includes low-fat dairy products, poultry, fish, legumes, nontropical vegetable oils and nuts; and limits intake of sweets, sugar-sweetened beverages, and red meats. • Adapt this dietary pattern to appropriate calorie requirements, personal and cultural food preferences, and nutrition therapy for other medical conditions (including diabetes). • Achieve this pattern by following plans such as the DASH dietary pattern, the U. S. Department of Agriculture (USDA) Food Pattern, or the AHA Diet. *Refer to 2013 Blood Cholesterol Guideline for guidance on who would benefit from LDL-C lowering.
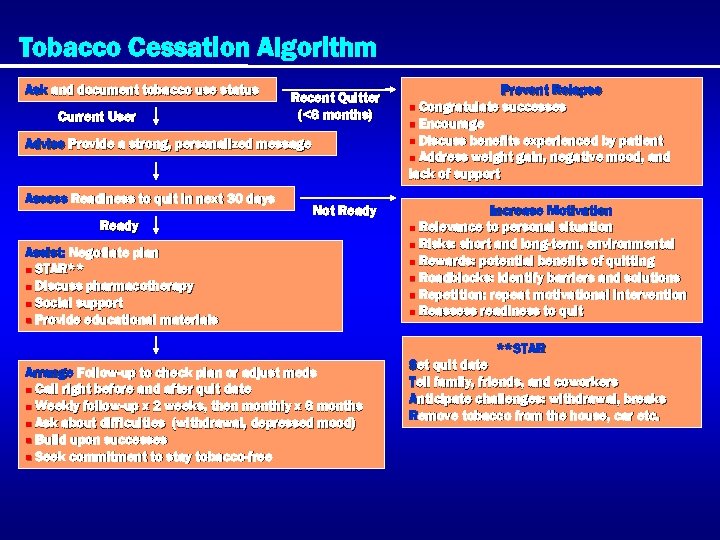
Tobacco Cessation Algorithm Ask and document tobacco use status Current User Recent Quitter (<6 months) Advise Provide a strong, personalized message Assess Readiness to quit in next 30 days Ready Not Ready Assist: Negotiate plan n STAR** n Discuss pharmacotherapy n Social support n Provide educational materials Prevent Relapse n Congratulate successes n Encourage n Discuss benefits experienced by patient n Address weight gain, negative mood, and lack of support Increase Motivation n Relevance to personal situation n Risks: short and long-term, environmental n Rewards: potential benefits of quitting n Roadblocks: identify barriers and solutions n Repetition: repeat motivational intervention n Reassess readiness to quit **STAR Arrange Follow-up to check plan or adjust meds n Call right before and after quit date n Weekly follow-up x 2 weeks, then monthly x 6 months n Ask about difficulties (withdrawal, depressed mood) n Build upon successes n Seek commitment to stay tobacco-free Set quit date Tell family, friends, and coworkers Anticipate challenges: withdrawal, breaks Remove tobacco from the house, car etc.
Recommendations: Physical Activity • Advise people with or without diabetes to perform at least 150 min/week of moderateintensity aerobic physical activity (50– 70% of maximum heart rate), spread over at least 3 days per week with no more than 2 consecutive days without exercise (A) • In absence of contraindications, adults with type 2 diabetes should be encouraged to perform resistance training at least twice per week (A) ADA. V. Diabetes Care 2013; 36(suppl 1): S 24.
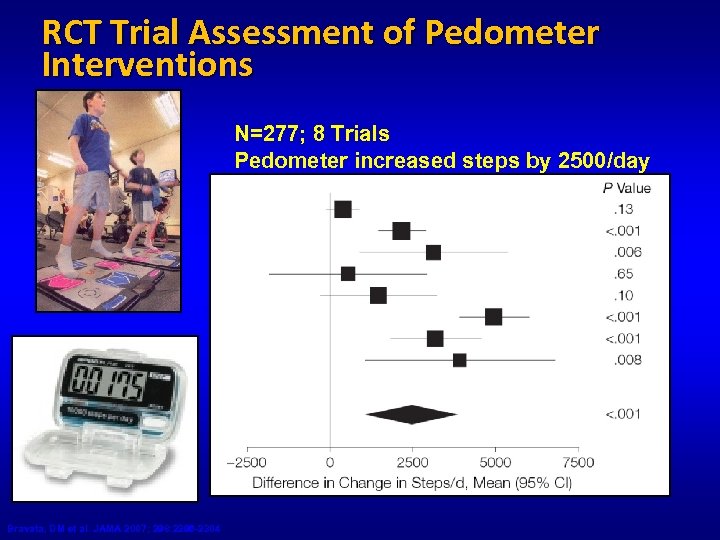
RCT Trial Assessment of Pedometer Interventions N=277; 8 Trials Pedometer increased steps by 2500/day Bravata, DM et al. JAMA 2007; 298: 2296 -2304
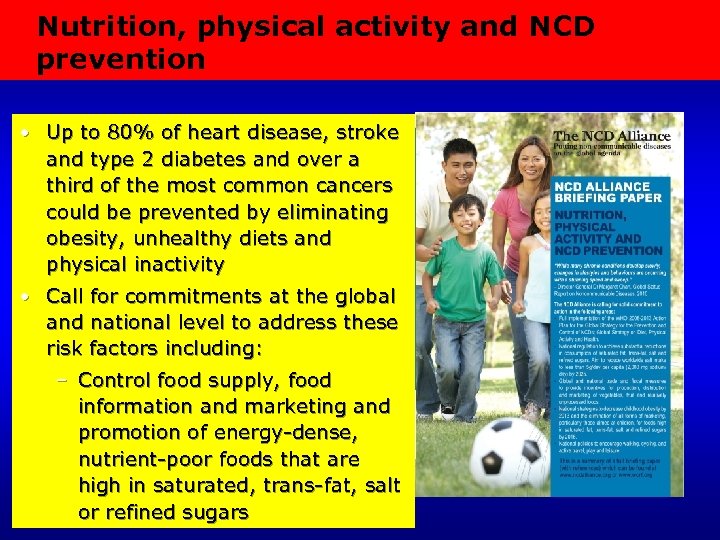
Nutrition, physical activity and NCD prevention • Up to 80% of heart disease, stroke and type 2 diabetes and over a third of the most common cancers could be prevented by eliminating obesity, unhealthy diets and physical inactivity • Call for commitments at the global and national level to address these risk factors including: – Control food supply, food information and marketing and promotion of energy-dense, nutrient-poor foods that are high in saturated, trans-fat, salt or refined sugars
Summary • Most persons with diabetes will suffer and die from cardiovascular consequences • Few persons with diabetes are appropriately controlled for key measures of A 1 c, BP, lipids, and weight. • Combined control of risk factors can result in up to 50% reductions in risk for cardiovascular disease • Greater adherence to lifestyle modifications and use of guidelinebased and newer therapies can help us address remaining residual risks.
THANK YOU! Now Available http: //cardiometabolic. cardiosource. org/ American Society for Preventive Cardiology: www. aspconline. org
3bd51e86821d65304f96b3e2b4510da6.ppt