e821ced4158b4be62d0b796f7067beb8.ppt
- Количество слайдов: 17
METABOLIC EMERGENCIES IN THE NEONATE N. Guffon, Edouard Herriot Hospital, Pediatrics, Lyon, France U. Simeoni, Timone University Hospital, Neonatology, Marseille, France J. B. Gouyon, University Hospital, Neonatology, Dijon, France
Index POST EMERGENCY When to « think metabolic » Immediate investigations Which emergency measures need to be undertaken? Diagnostic algorithm Specific investigations Case examples (Saudubray 2002, Saudubray & Ogier de Baulny 1995)
When to « think metabolic » ( 1 ) Initial symptoms: – – – – – lethargy (or “just not well”) refusal to feed, poor sucking, vomiting poor weight gain polypnoea hypothermia axial hypotonia limb hypotonia abnormal movements (boxing, pedalling, tremor, . . . ) hepatomegaly With possible progression to: altered consciousness, seizures, coma, multivisceral failure (Saudubray 2002, Saudubray & Ogier de Baulny 1995)
When to « think metabolic » ( 2 ) Additional factors – – initial symptom free interval consanguinity family history (previous neonatal deaths, possibly unexplained) deterioration despite symptomatic therapy (possibly unexplained) Note: symptoms are usually non specific, metabolic disease may be excluded when obvious cause is known Careful! Metabolic diseases are often associated with infections! (Saudubray 2002, Saudubray & Ogier de Baulny 1995)
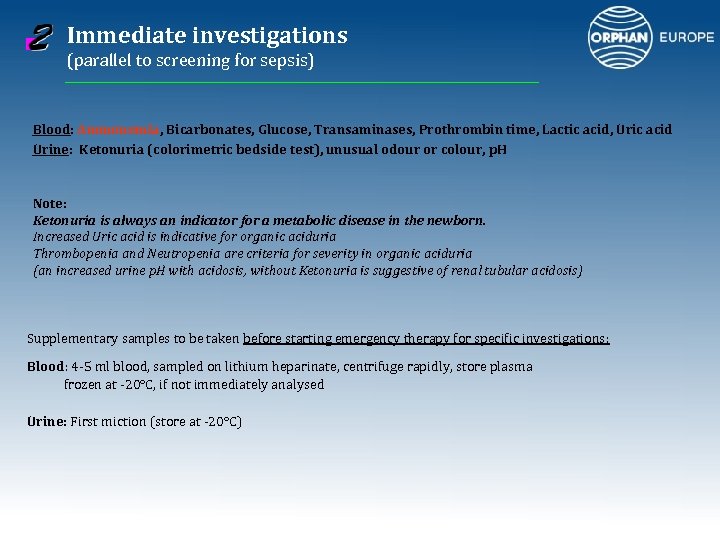
Immediate investigations (parallel to screening for sepsis) Blood: Ammonemia, Bicarbonates, Glucose, Transaminases, Prothrombin time, Lactic acid, Uric acid Urine: Ketonuria (colorimetric bedside test), unusual odour or colour, p. H Note: Ketonuria is always an indicator for a metabolic disease in the newborn. Increased Uric acid is indicative for organic aciduria Thrombopenia and Neutropenia are criteria for severity in organic aciduria (an increased urine p. H with acidosis, without Ketonuria is suggestive of renal tubular acidosis) Supplementary samples to be taken before starting emergency therapy for specific investigations: Blood: 4 -5 ml blood, sampled on lithium heparinate, centrifuge rapidly, store plasma frozen at -20°C, if not immediately analysed Urine: First miction (store at -20°C)
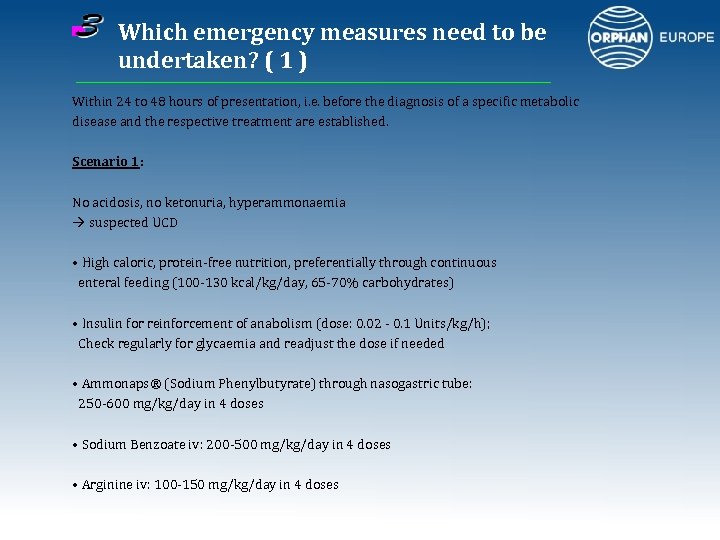
Which emergency measures need to be undertaken? ( 1 ) Within 24 to 48 hours of presentation, i. e. before the diagnosis of a specific metabolic disease and the respective treatment are established. Scenario 1: No acidosis, no ketonuria, hyperammonaemia suspected UCD • High caloric, protein-free nutrition, preferentially through continuous enteral feeding (100 -130 kcal/kg/day, 65 -70% carbohydrates) • Insulin for reinforcement of anabolism (dose: 0. 02 - 0. 1 Units/kg/h); Check regularly for glycaemia and readjust the dose if needed • Ammonaps® (Sodium Phenylbutyrate) through nasogastric tube: 250 -600 mg/kg/day in 4 doses • Sodium Benzoate iv: 200 -500 mg/kg/day in 4 doses • Arginine iv: 100 -150 mg/kg/day in 4 doses
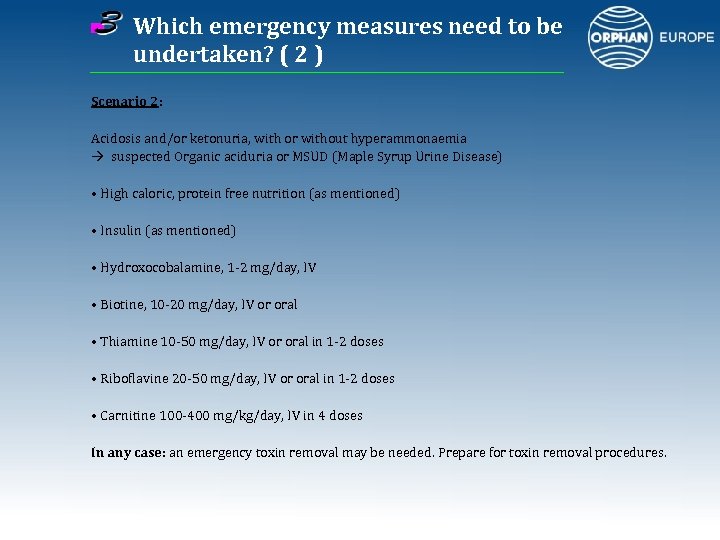
Which emergency measures need to be undertaken? ( 2 ) Scenario 2: Acidosis and/or ketonuria, with or without hyperammonaemia suspected Organic aciduria or MSUD (Maple Syrup Urine Disease) • High caloric, protein free nutrition (as mentioned) • Insulin (as mentioned) • Hydroxocobalamine, 1 -2 mg/day, IV • Biotine, 10 -20 mg/day, IV or oral • Thiamine 10 -50 mg/day, IV or oral in 1 -2 doses • Riboflavine 20 -50 mg/day, IV or oral in 1 -2 doses • Carnitine 100 -400 mg/kg/day, IV in 4 doses In any case: an emergency toxin removal may be needed. Prepare for toxin removal procedures.
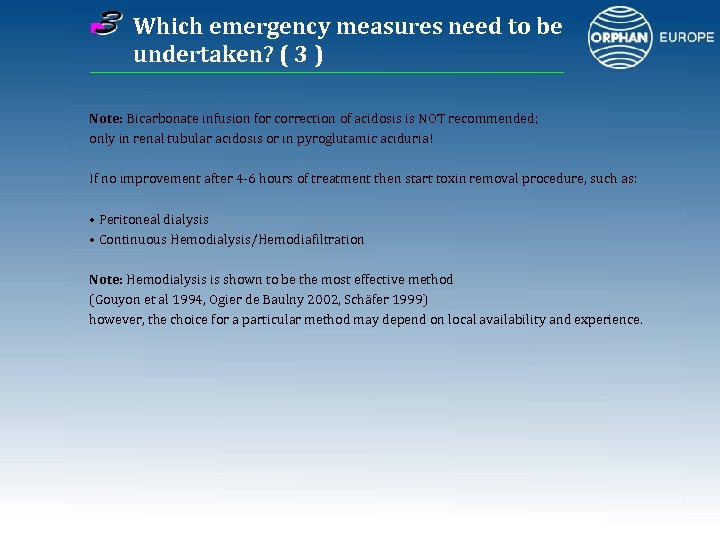
Which emergency measures need to be undertaken? ( 3 ) Note: Bicarbonate infusion for correction of acidosis is NOT recommended; only in renal tubular acidosis or in pyroglutamic aciduria! If no improvement after 4 -6 hours of treatment then start toxin removal procedure, such as: • Peritoneal dialysis • Continuous Hemodialysis/Hemodiafiltration Note: Hemodialysis is shown to be the most effective method (Gouyon et al 1994, Ogier de Baulny 2002, Schäfer 1999) however, the choice for a particular method may depend on local availability and experience.
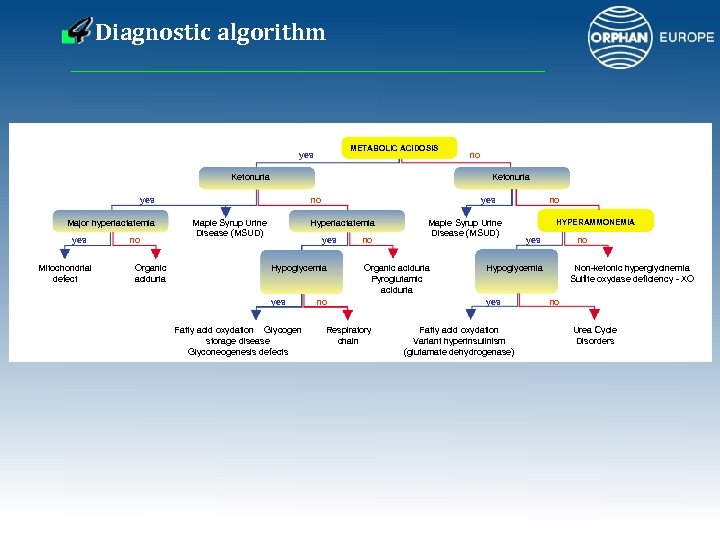
Diagnostic algorithm METABOLIC ACIDOSIS yes Ketonuria yes Major hyperlactatemia yes Mitochondrial defect no Organic aciduria no no Maple Syrup Urine Disease (MSUD) yes Hyperlactatemia yes Hypoglycemia yes Fatty acid oxydation Glycogen storage disease Glyconeogenesis defects no Maple Syrup Urine Disease (MSUD) Organic aciduria Pyroglutamic aciduria no Respiratory chain no HYPERAMMONEMIA yes no Hypoglycemia yes Fatty acid oxydation Variant hyperinsulinism (glutamate dehydrogenase) Non-ketonic hyperglycinemia Sulfite oxydase deficiency - XO no Urea Cycle Disorders
Specific investigations (with the aid of a metabolic specialist) From initial samples: • Blood: Amino acids, Acyl carnitine profile • Urine: Organic acids, Oroticuria Main diagnostic pathways: • Urea Cycle Disorders: Plasma amino acids, oroticuria; then specific enzymatic activity • Organic aciduria: Urinary organic acids; then specific enzymatic activity • Fatty acid oxidation: blood carnitine and acylcarnitine profile, urinary organic acids then specific enzyme activity • Respiratory chain disorders: very high lactatemia then specific enzyme activity, very poor prognosis eventually post mortem samples (see below) Postmortem cases: In the absence of a specific orientation towards a diagnostic pathway the following samples need to be taken (in addition to blood and urine) : • skin biopsy (in saline solution at RT) • muscle and liver biopsy (freeze immediately at – 80°C)
Case examples ( 1 ) Case 1 Child born at 37 weeks of gestation, birthweight 2450 g, consanguineous parents Day 1: episode of cyanosis while breast feeding Day 2: poor feeding Day 3: oliguria, trembling, slight hypotonia Day 4: generalized seizure, progressing lethargy and hypotonia, abnormal movements of the lower limbs Day 5: coma Blood ammonia: 500 µmol/l Emergency measures: peritoneal dialysis, sodium benzoate, arginine hydrochloride, high caloric nasogastric feeding without protein
Case examples ( 2 ) Case 1 (cont. ) Further investigations: low citrulline, ornithine, arginine and isoleucine, normal organic acids Carbamylglutamate given at day 25 because of recurrent ammonaemia (CPS or NAGS deficiency? ) Enzyme test for enzyme activity showed decreased NAGS Function Diagnosis: NAGS deficiency Treatment: Carbaglu® (ongoing) (Guffon et al 1995) Comment: in this case screening for metabolic diseases especially hyperammonemia would have been indicated at day 2, parallel to septic screening.
Case examples ( 3 ) Case 2 Child born at 39 weeks of gestation, birth weight 3250 g, no consanguinity 1 st hospitalisation at day 3: admission with poor feeding, weight loss (16%), intravenous rehydratation then discharged after 24 h At home: poor feeding, no weight gain, attempts of feeding with different milk formulas 2 nd hospitalisation at day 17: poor feeding, no weight gain since birth, diagnosis of low urinary infection (104 E Coli) : Antibiotics, no screening for ketonuria At home: persistent poor feeding and no weight gain, patient sleeps a lot 3 rd hospitalisation at 1. 5 months: poor feeding, weight 3 600 g, vomiting, infectious screening negative, normal abdominal X ray and ultrasound, improvement with glucose infusion. After reintroduction of milk: vomiting, drowsiness, moaning, altered general condition, transfered with the diagnosis of intestinal occlusion.
Case examples ( 4 ) Case 2 (cont. ) At arrival: hypothermia (36°C), bad general condition, drowsiness, a reactivity, no eye contact, huge axial and peripheral hypotonia, polypnea, normal visceral exam Metabolic acidosis (HCO 3 -: 13 mmol/l), ketonuria ++, hyperammonaemia 349 µmol/l, leuconeutropaenia suspicion of organic aciduria emergency care: continuous free protein, high caloric nasogastric feeding IV carnitine 350 mg x 4/day IV vitamine B 12 : 1 mg/day IV biotine 10 mg/day IV insulin Diagnosis: methylmalonic aciduria (mut-) (plasma methyl malonic acid (MMA) 846 µmol/l, urinary MMA 38 245 µmol/l) Good outcome
References and further reading Blau N et al (2003) Simple test in urine and blood. In: Physician’s guide to the laboratory diagnosis of metabolic diseases. Blau N, Duran M, Blaskovics ME, Gibson KM Editors. Springer Verlag, Berlin Heidelberg, 3 -10. Guffon N. et al (1995): A new neonatal case of N-acetylglutamate synthase deficiency treated by carbamylglutamate. J Inherit Metab Dis 18(1): 61 -5. Gouyon JB et al (1994): Removal of branched-chain amino acids by peritoneal dialysis, continuous arterivenous hemofiltration, and continuous arterivenous hemodialysis in rabbits: implications for maple syrup urine disease treatment; Ped Res 35: 357 -61. Leonard JV (1985): The early detection and management of inborn errors presenting acutely in the neonatal period. Eur J Pediatr 143: 253 -7. Ogier de Baulny H (2002): Management and emergency treatments of neonates with a suspicion of inborn errors of metabolism. Semin Neonatol 7: 17 -26. Saudubray JM et al (1995): Clinical approach to inherited metabolic diseases. In: Inborn metabolic diseases. Fernandez J, Saudubray JM, van den Berghe G Editors. Springer Verlag, Berlin Heidelberg, 339. Saudubray JM et al (2002): Clinical approach to inherited metabolic disorders in neonates : an overview. Semin Neonatol 7: 3 -15.

Other documents on this topic are available from Orphan Europe Headquarter at: FRANCE ORPHAN EUROPE SARL Immeuble “Le Wilson” 70, avenue du Général de Gaulle 92058 PARIS LA DEFENSE FRANCE Tel. : +33 (0)1 47 73 64 58 Fax: +33 (0)1 49 06 00 04 e. mail: fra@orphan-europe. com www. orphan-europe. com Or one of its local affiliates: UNITED KINGDOM ORPHAN EUROPE (UK) Ltd. Isis House, 43 Station Road Henley-on-Thames OXFORDSHIRE RG 9 1 AT UNITED KINGDOM Tel. : +44 (0) 1491 414 333 Fax: +44 (0) 1491 414 443 e. mail: info. uk@orphan-europe. com www. orphan-europe. com ITALY ORPHAN EUROPE (Italy) Srl. Via Cellini, 11 20090 SEGRATE (MILANO) ITALY Tel. : + 39 02 26 95 01 39 Fax: + 39 02 26 95 36 74 e. mail: info@orphan-europe. it www. orphan-europe. com
SPAIN – PORTUGAL ORPHAN EUROPE S. L. Gran Via de les Corts Catalanes, 649 Despacho n° 1 08010 BARCELONA SPAIN Tel. : + 34 93 342 51 20 Fax: + 34 93 270 10 50 e. mail: info@orphan-europe. es www. orphan-europe. com GERMANY ORPHAN EUROPE (Germany) Gmbh Max-Planck-Strasse 6 63128 DIETZENBACH GERMANY Tel. : + 49 (0) 60 74 81 21 60 Fax : + 49 (0) 60 74 81 21 66 e. mail: ger@orphan-europe. com www. orphan-europe. com POLAND ORPHAN EUROPE (Germany) Gmbh Przedstawicielstwo w Polsce Ul. Czeresniowa 98 02 – 456 WARZAWA POLAND Tel. : + 48 22 863 86 01 Fax: + 48 22 863 58 96 e. mail: mrogaszewska@orphan-europe. pl www. orphan-europe. com NORDIC COUNTRIES ORPHAN EUROPE AB Banérgatan 37 S 115 22 STOCKHOLM SWEDEN Tel. : + 46 8 545 80 230 Fax: + 46 8 660 5078 e. mail: info@orphan-europe. se www. orphan-europe. com BENELUX ORPHAN EUROPE King Albert I Avenue 48 bus 3 1740 WEMMEL BELGIUM www. orphan-europe. com
e821ced4158b4be62d0b796f7067beb8.ppt