Water Salt Balance 2008.ppt
- Количество слайдов: 42
Metabolic disorders Part 3 07. 12. 08
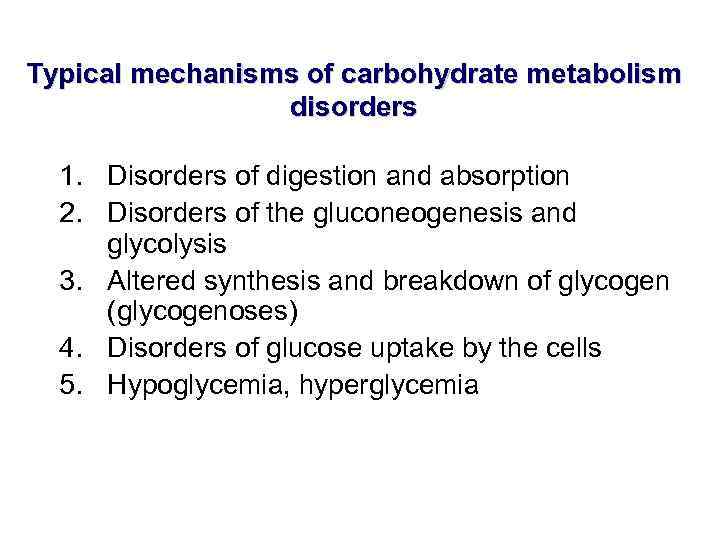
Typical mechanisms of carbohydrate metabolism disorders 1. Disorders of digestion and absorption 2. Disorders of the gluconeogenesis and glycolysis 3. Altered synthesis and breakdown of glycogen (glycogenoses) 4. Disorders of glucose uptake by the cells 5. Hypoglycemia, hyperglycemia
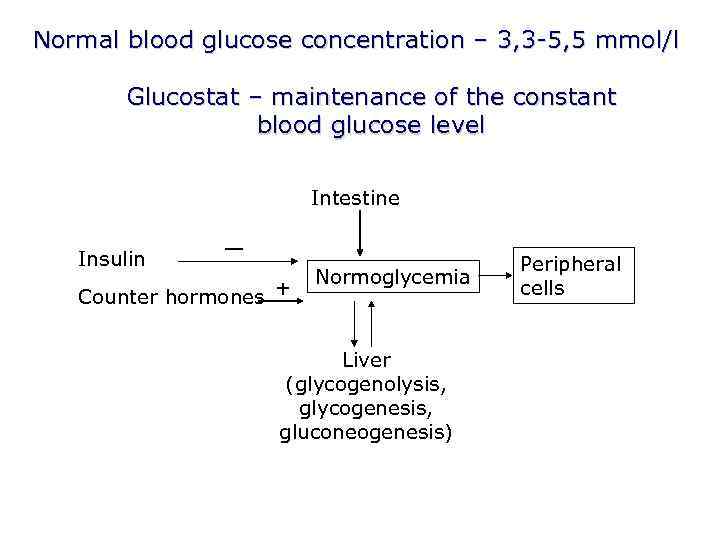
Normal blood glucose concentration – 3, 3 -5, 5 mmol/l Glucostat – maintenance of the constant blood glucose level Intestine Insulin — Counter hormones + Normoglycemia Liver (glycogenolysis, glycogenesis, gluconeogenesis) Peripheral cells
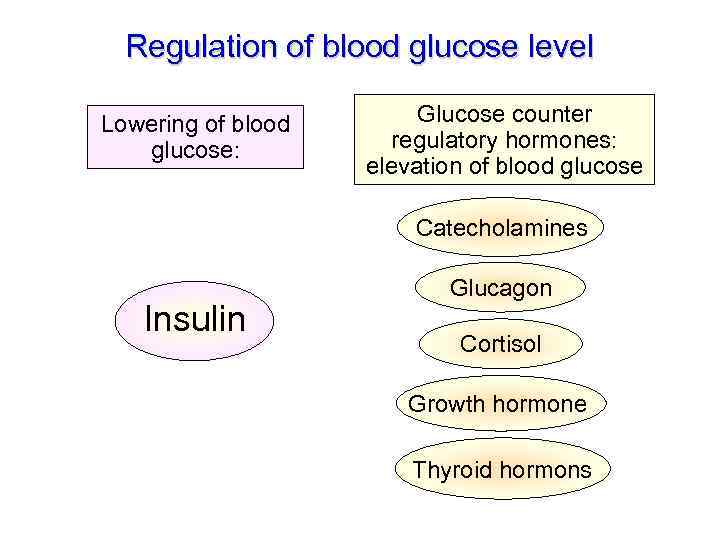
Regulation of blood glucose level Lowering of blood glucose: Glucose counter regulatory hormones: elevation of blood glucose Catecholamines Insulin Glucagon Cortisol Growth hormone Thyroid hormons
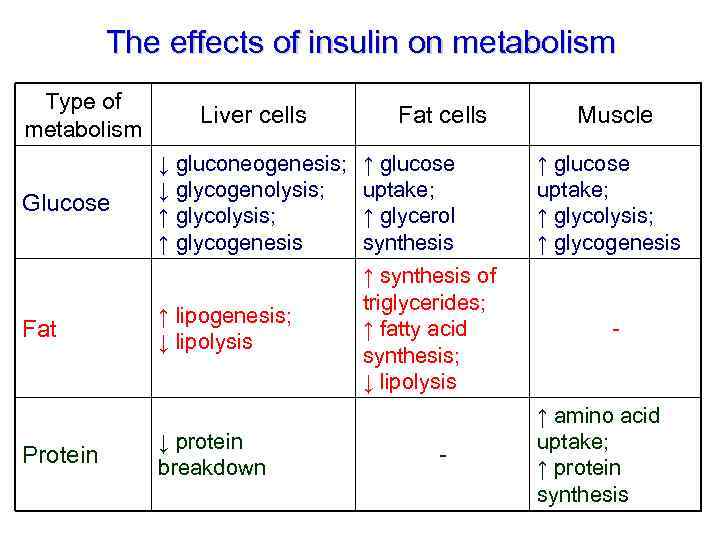
The effects of insulin on metabolism Type of metabolism Glucose Fat Protein Liver cells Fat cells ↓ gluconeogenesis; ↓ glycogenolysis; ↑ glycogenesis ↑ glucose uptake; ↑ glycerol synthesis ↑ lipogenesis; ↓ lipolysis ↑ synthesis of triglycerides; ↑ fatty acid synthesis; ↓ lipolysis ↓ protein breakdown - Muscle ↑ glucose uptake; ↑ glycolysis; ↑ glycogenesis - ↑ amino acid uptake; ↑ protein synthesis
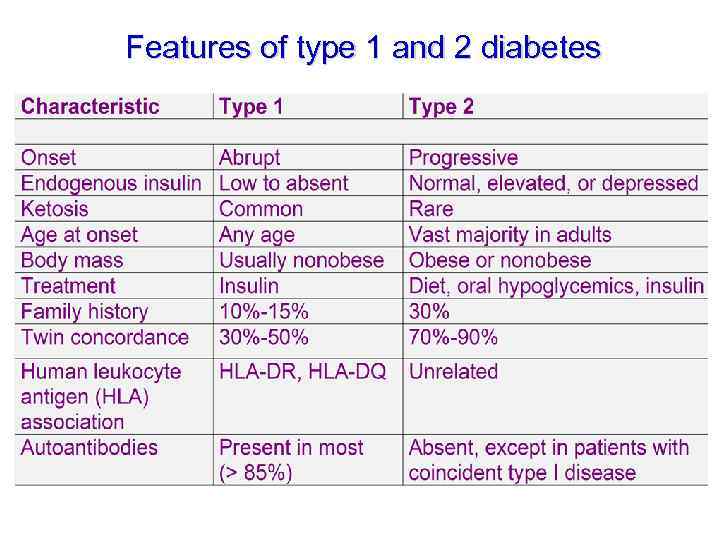
Features of type 1 and 2 diabetes
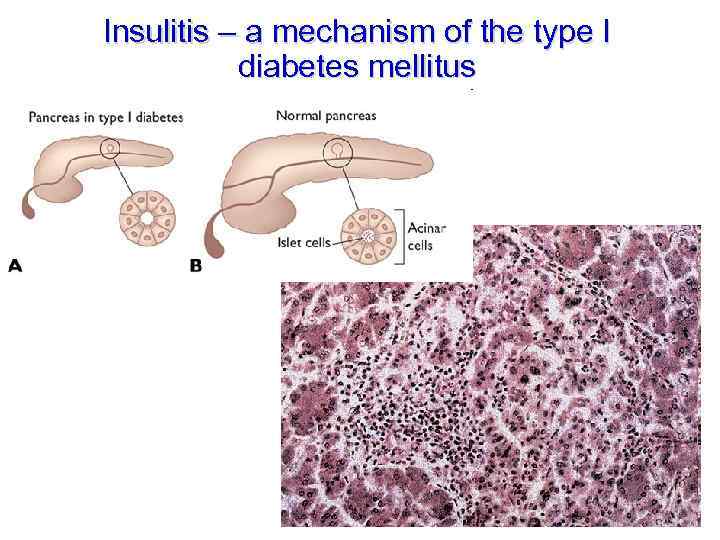
Insulitis – a mechanism of the type I diabetes mellitus
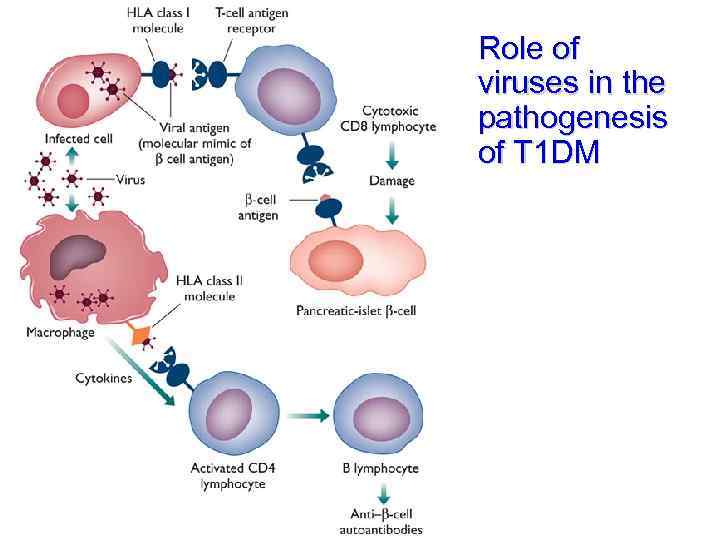
Role of viruses in the pathogenesis of T 1 DM
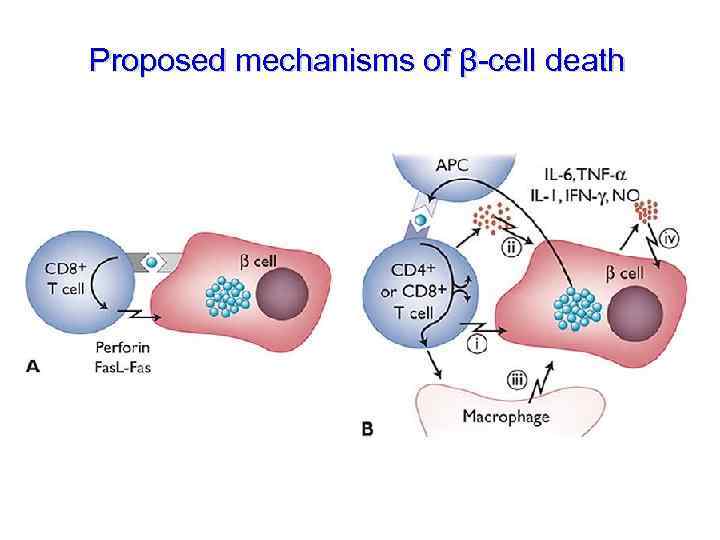
Proposed mechanisms of β-cell death
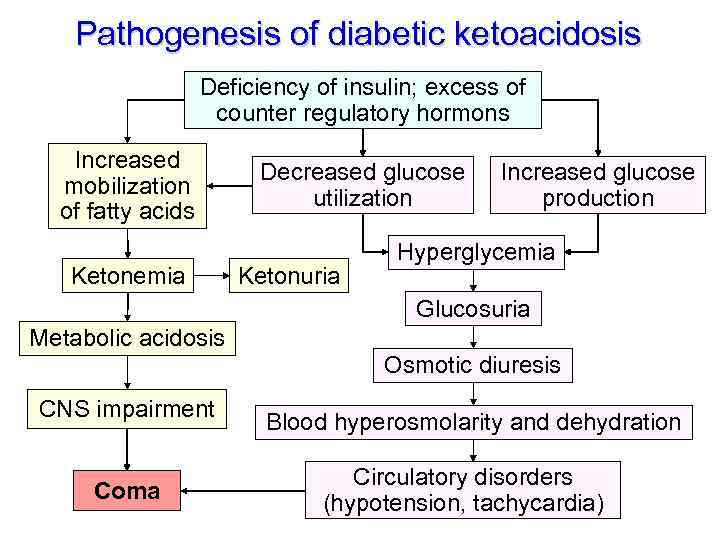
Pathogenesis of diabetic ketoacidosis Deficiency of insulin; excess of counter regulatory hormons Increased mobilization of fatty acids Ketonemia Decreased glucose utilization Ketonuria Increased glucose production Hyperglycemia Glucosuria Metabolic acidosis Osmotic diuresis CNS impairment Coma Blood hyperosmolarity and dehydration Circulatory disorders (hypotension, tachycardia)
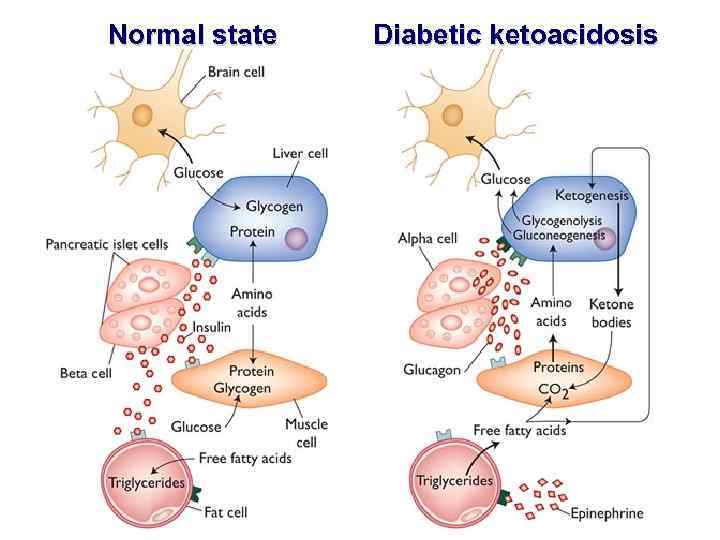
Normal state Diabetic ketoacidosis
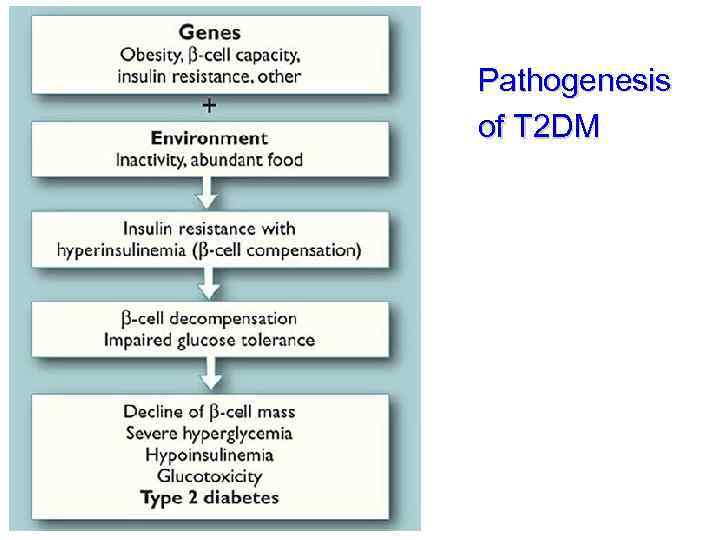
Pathogenesis of T 2 DM
Mechanisms of insulin resistance 1. Prereceptor level (anomalous insulin) 2. Receptor level (decreased number of insulin receptors, decreased affinity of the receptors) 3. At the level of glucose transport (decreased number of GLUT) 4. Postreceptor level (disorders of signal transduction and kinase phosphorylation)
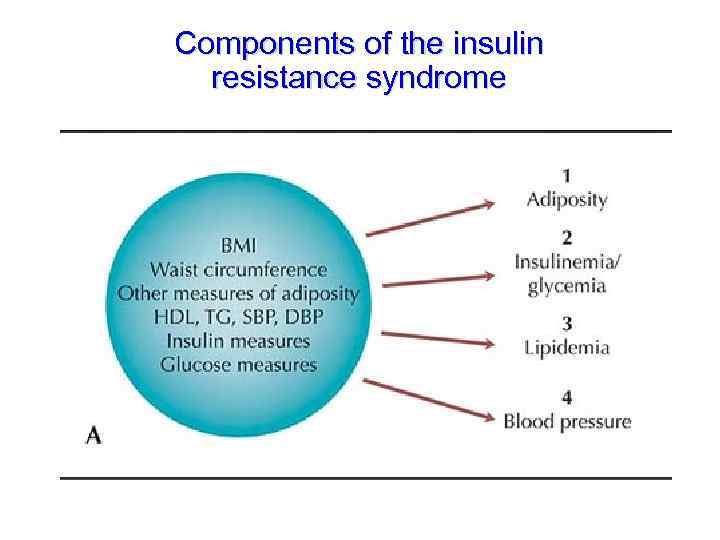
Components of the insulin resistance syndrome
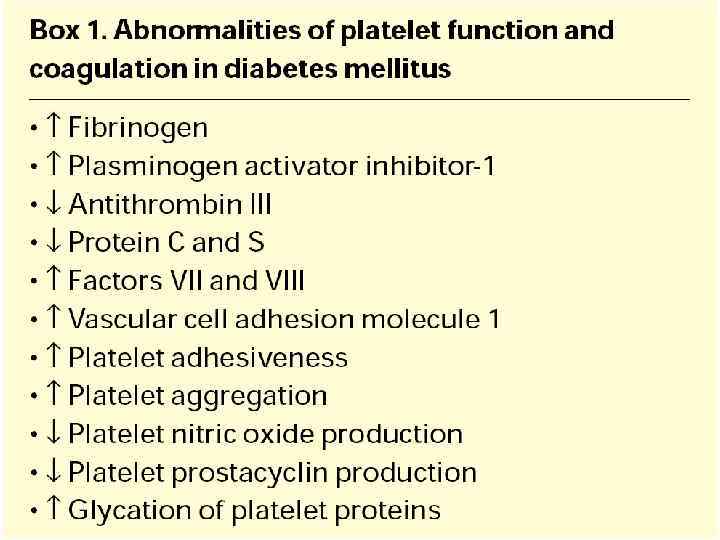
Consequences of hyperglycemia ● Glucosuria, polyuria, secondary polydipsia … ● Blood hyperosmolarity, tissue dehydration, hyperosmolar coma ● Non-enzymatic glycation of proteins (albumins, hemoglobin etc. ) – formation of advanced glycation end-products ● Endothelial dysfunction (micro- and macroangiopathy) ● Formation of autoantigens (autoimmune reactions)
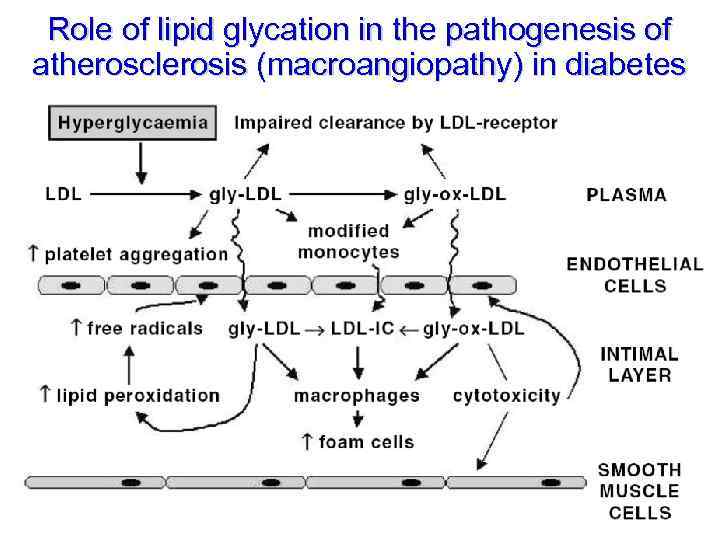
Role of lipid glycation in the pathogenesis of atherosclerosis (macroangiopathy) in diabetes
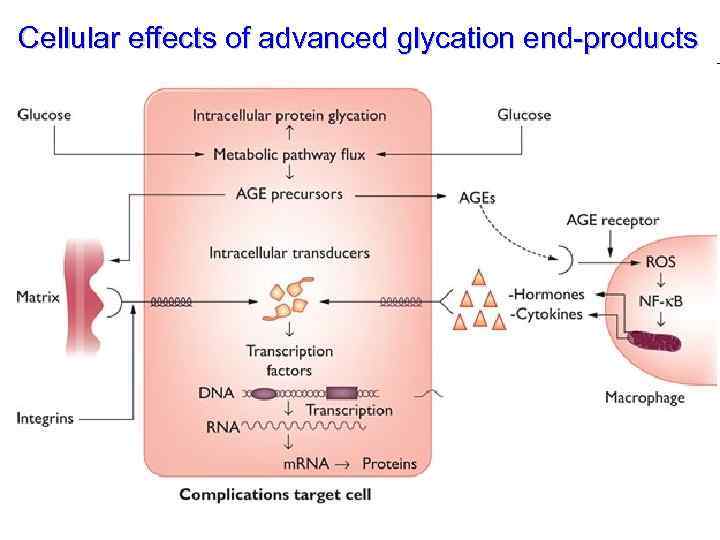
Cellular effects of advanced glycation end-products
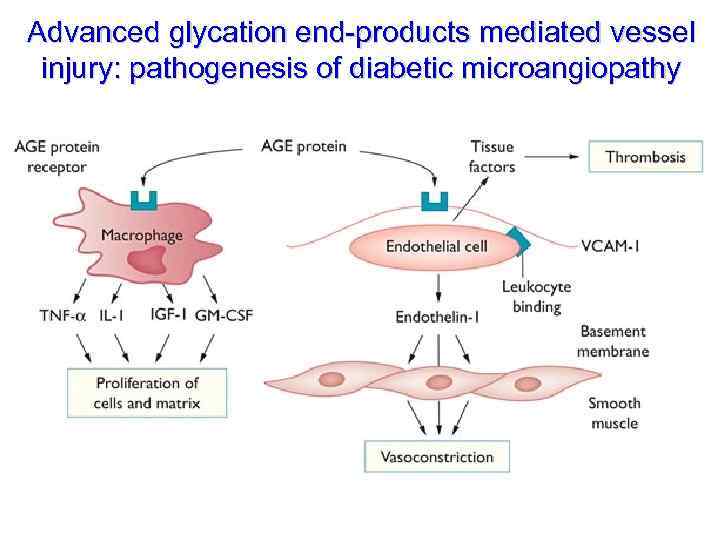
Advanced glycation end-products mediated vessel injury: pathogenesis of diabetic microangiopathy
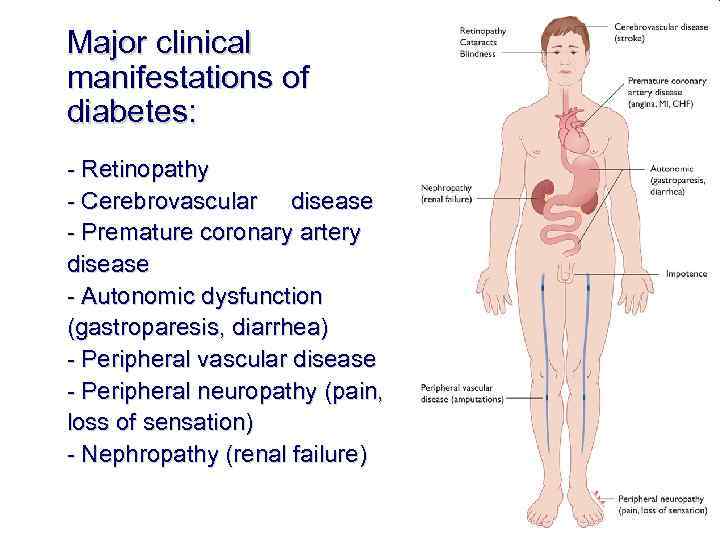
Major clinical manifestations of diabetes: - Retinopathy - Cerebrovascular disease - Premature coronary artery disease - Autonomic dysfunction (gastroparesis, diarrhea) - Peripheral vascular disease - Peripheral neuropathy (pain, loss of sensation) - Nephropathy (renal failure)
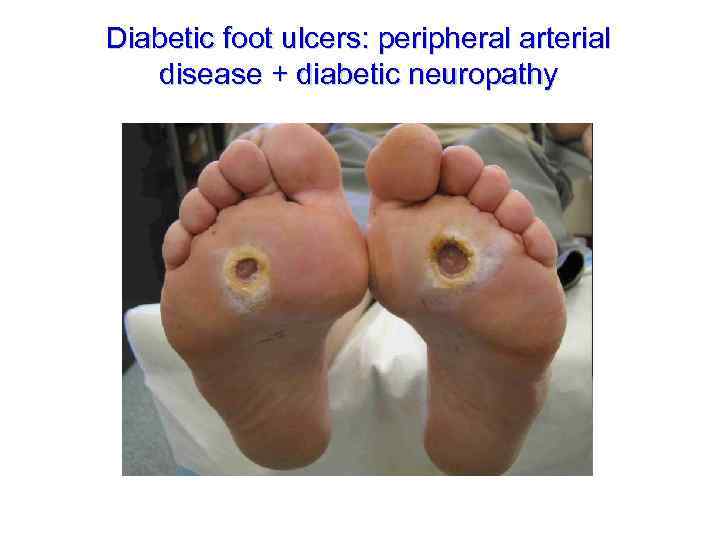
Diabetic foot ulcers: peripheral arterial disease + diabetic neuropathy
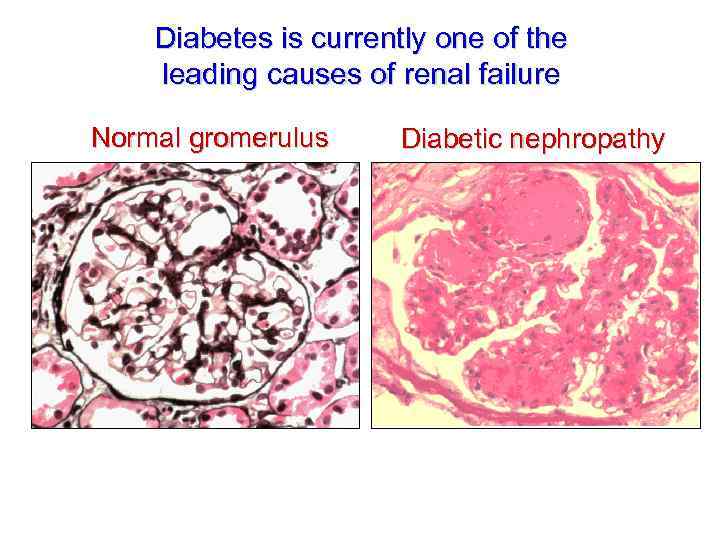
Diabetes is currently one of the leading causes of renal failure Normal gromerulus Diabetic nephropathy
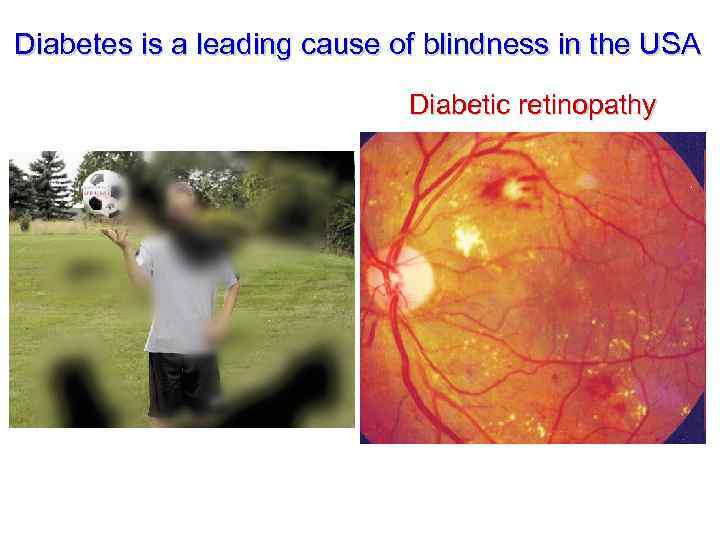
Diabetes is a leading cause of blindness in the USA Diabetic retinopathy
Mechanisms of hypoglycemia • Increased utilization of glucose by the cells – increased insulin production, treatment with insulin – formation of insulin-like growth factors • Disorders of glycogenolysis (glycogenoses, liver cirrhosis) • Disorders of glucose reabsorption (renal diabtes) • Prolonged intensive physical exercise
Mechanisms of compensation in hypoglycemia ● Activation of sympathetic nervous system (glycogenolysis) ● Increased production of glucose counter regulatory hormones, gluconeogenesis, activation of lipolysis and decreased utilization of glucose
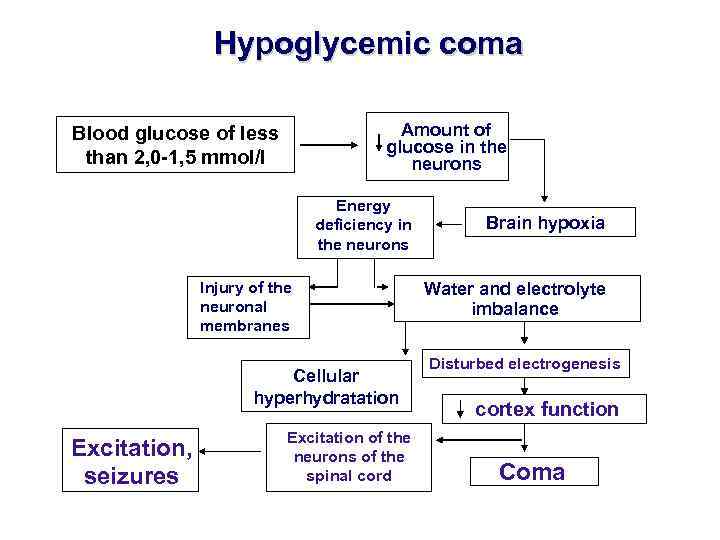
Hypoglycemic coma Amount of glucose in the neurons Blood glucose of less than 2, 0 -1, 5 mmol/l Energy deficiency in the neurons Injury of the neuronal membranes Cellular hyperhydratation Excitation, seizures Excitation of the neurons of the spinal cord Brain hypoxia Water and electrolyte imbalance Disturbed electrogenesis cortex function Coma
Basics of Body Fluids • Water is primary body fluid. 40%-60% of weight in adult. Affected by age, sex, & body fat. • Distribution: 2 major compartments-ICF & ECF. • ICF: in cells. 2/3 of body fluid in adults. • ECF: outside cells. 1/3 of body fluid. 4 compartments-intravascular, interstitial, lymph, & transcellular
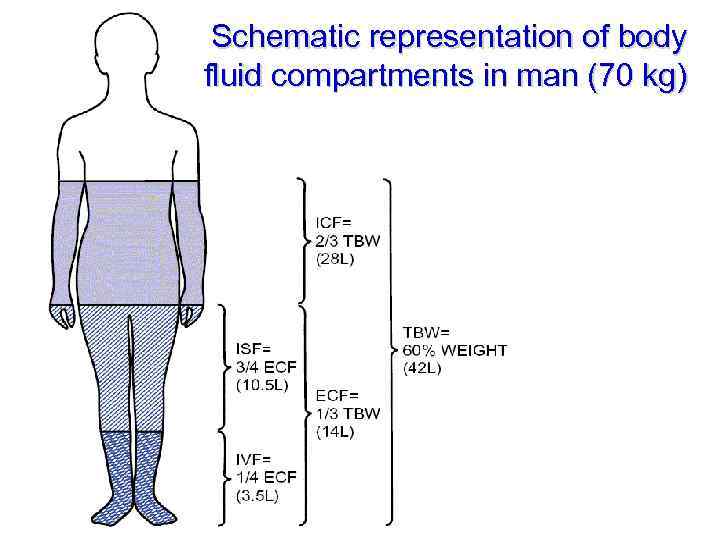
Schematic representation of body fluid compartments in man (70 kg)
Basics of Body Fluids • • Intravascular: plasma Interstitial: surrounds the cells; 3/4 ECF Transcellular: CSF, pericardial, pleural, etc Lymph: lymphatic system
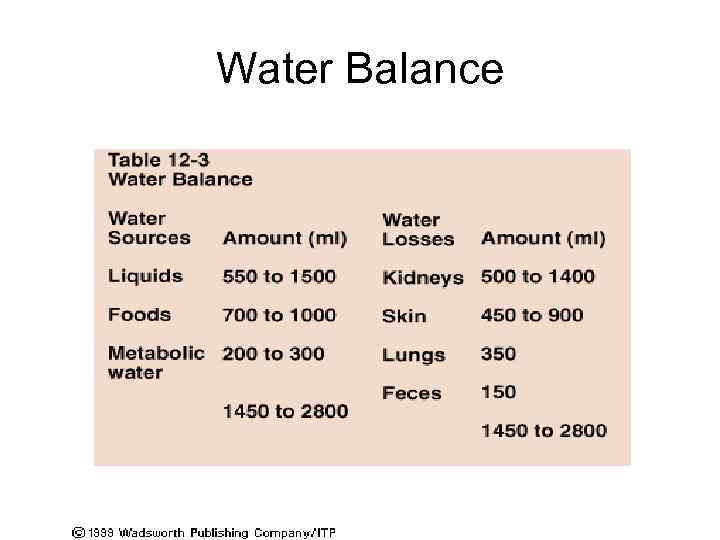
Water Balance
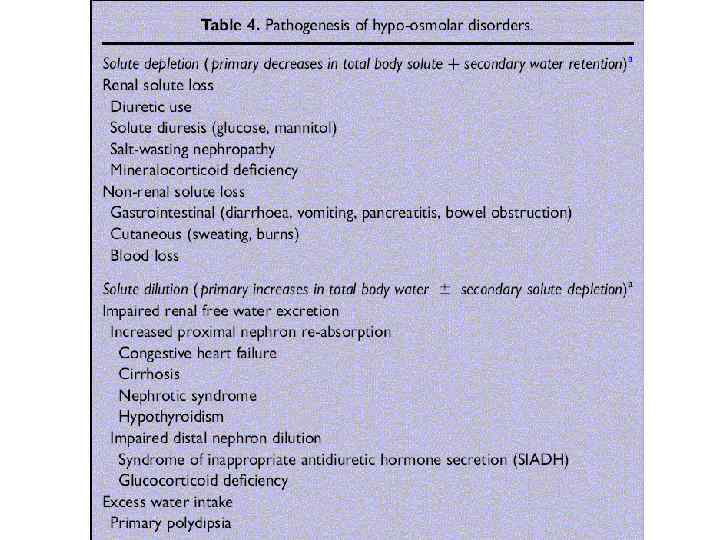
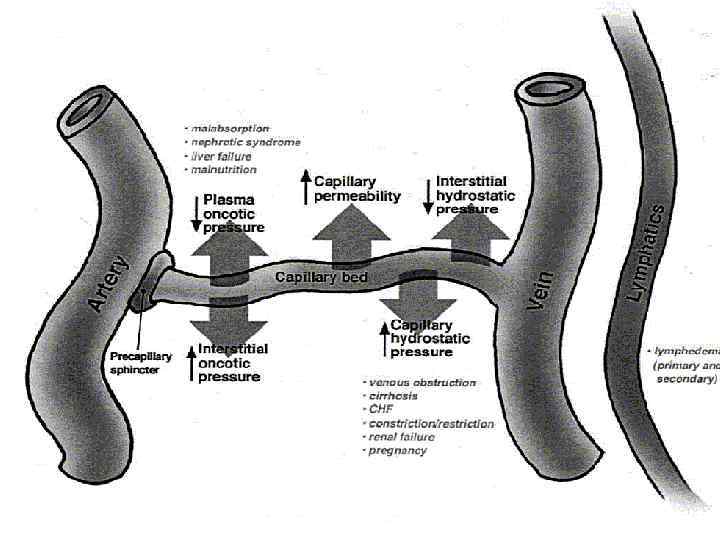
Edema – pathological accumulation of the fluid within the extravascular space, i. e. , interstitium and/or cells Main mechanisms of edema: 1. Increased microvascular permeability (hypersensitivity type I); 2. Decreased lymph drainage (elephant leg); 3. Increased hydrostatic pressure in the capillaries (venous congestion); 4. Decreased oncotic pressure of the blood (hypoproteinemia); 5. Severe retention of water and salts (renal failure)
Water Salt Balance 2008.ppt