Lipid carbohydrate metabolism 2008.ppt
- Количество слайдов: 39
Metabolic disorders Part 2 01. 12. 08
Lecture outline 1. Protein misfolding diseases 2. Dyslipoproteinemias & Atherosclerosis 3. Obesity 4. Diabetes mellitus
The mechanisms of alterations in protein conformation (amyloidogenic transformation) 1. The intrinsic ability of the protein to acquire pathologic conformation under certain circumstances (ageing, increased protein concentration) 2. Mutations leading to replacement of a single amino acid in the protein (hereditary amyloidosis) 3. Proteolytic remodeling of the protein precursor g. , β-amyloid precursor protein in Alzheimer’s disease) (e.
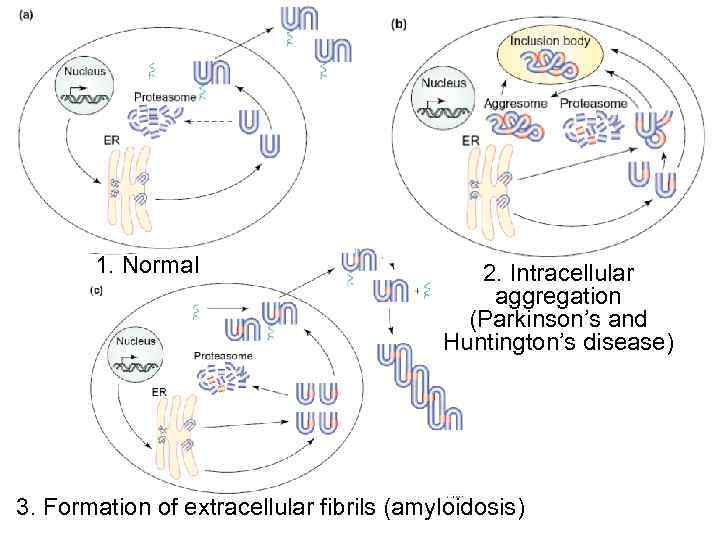
1. Normal 2. Intracellular aggregation (Parkinson’s and Huntington’s disease) 3. Formation of extracellular fibrils (amyloidosis)
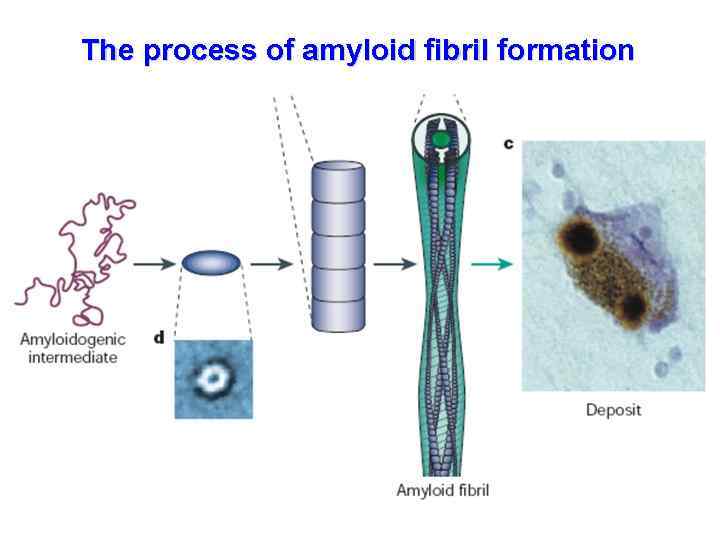
The process of amyloid fibril formation
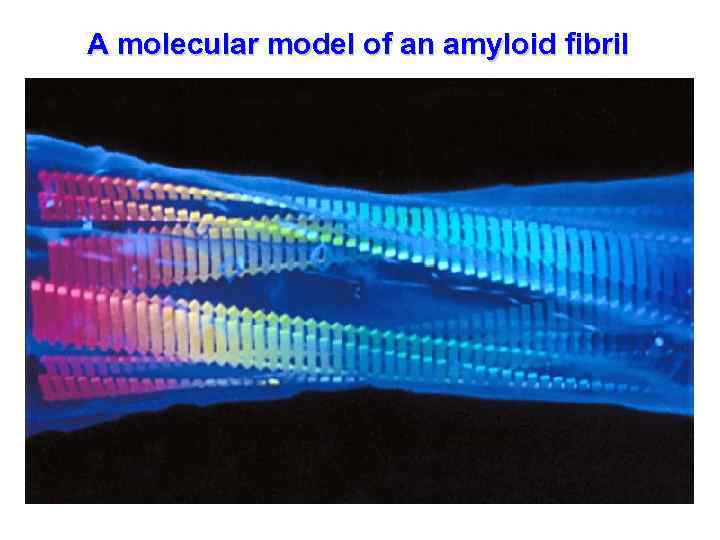
A molecular model of an amyloid fibril

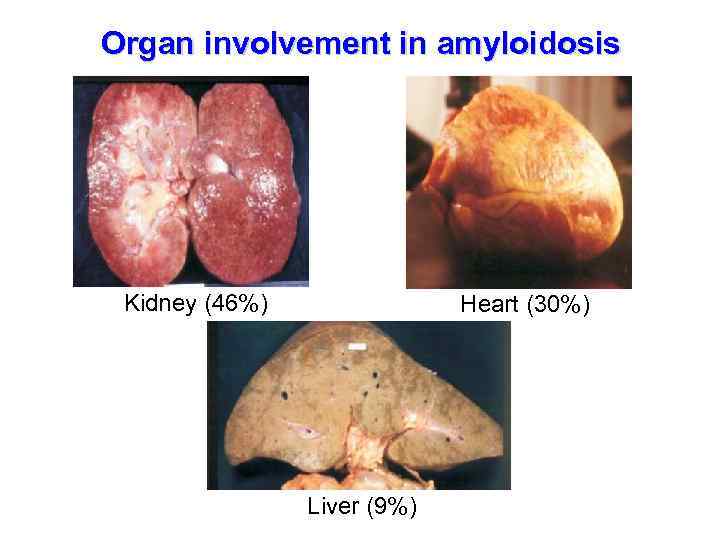
Organ involvement in amyloidosis Kidney (46%) Heart (30%) Liver (9%)
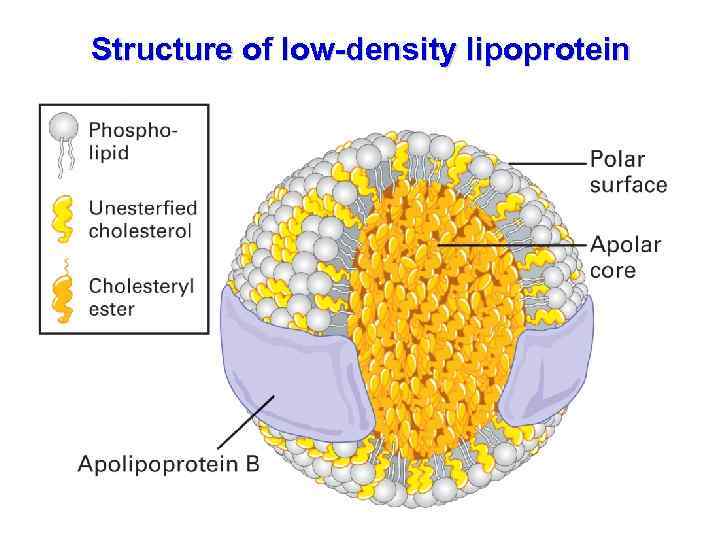
Structure of low-density lipoprotein
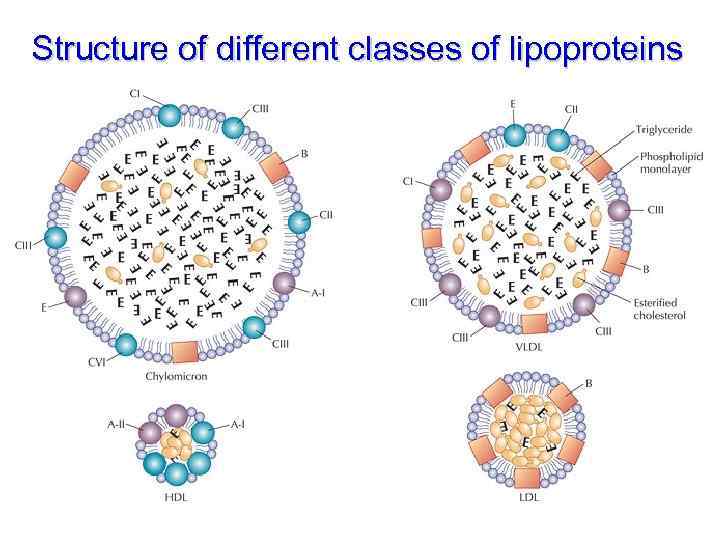
Structure of different classes of lipoproteins
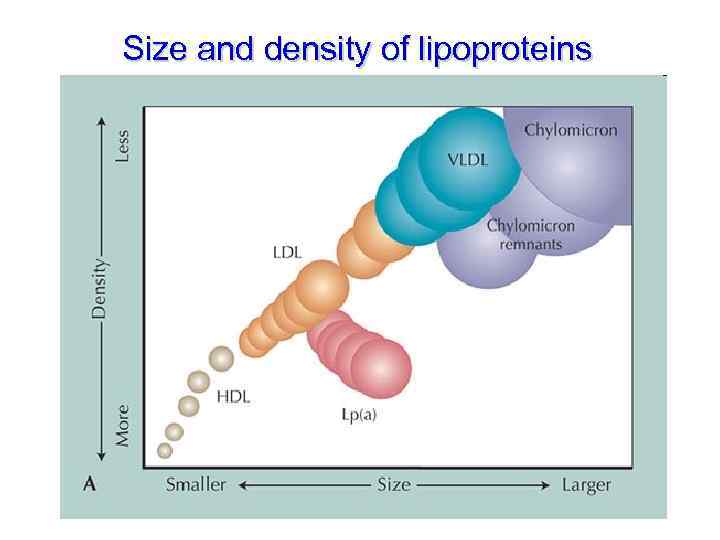
Size and density of lipoproteins
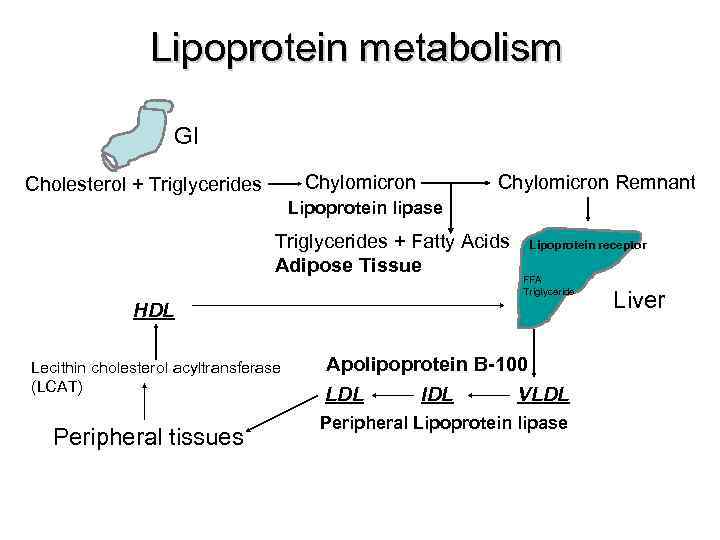
Lipoprotein metabolism GI Chylomicron Cholesterol + Triglycerides Chylomicron Remnant Lipoprotein lipase Triglycerides + Fatty Acids Adipose Tissue Lipoprotein receptor FFA Triglyceride HDL Lecithin cholesterol acyltransferase (LCAT) Peripheral tissues Apolipoprotein B-100 LDL IDL VLDL Peripheral Lipoprotein lipase Liver
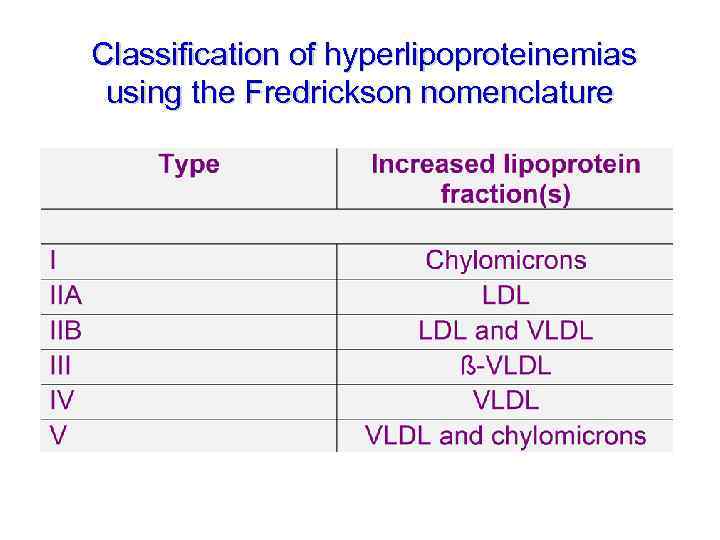
Classification of hyperlipoproteinemias using the Fredrickson nomenclature
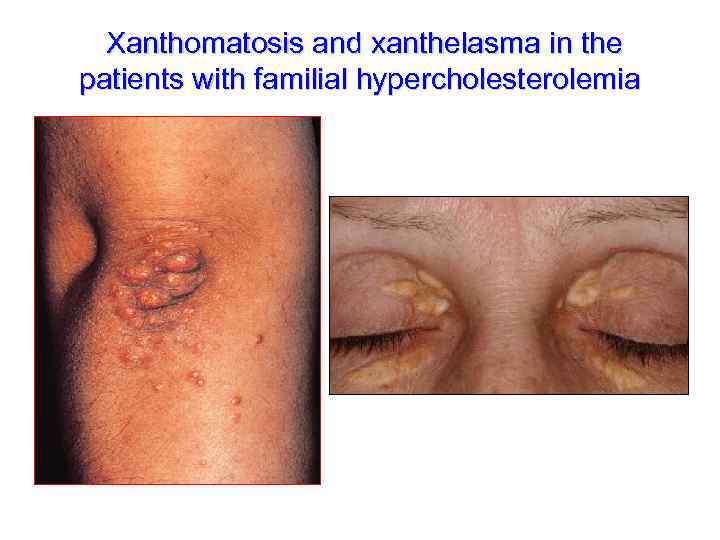
Xanthomatosis and xanthelasma in the patients with familial hypercholesterolemia
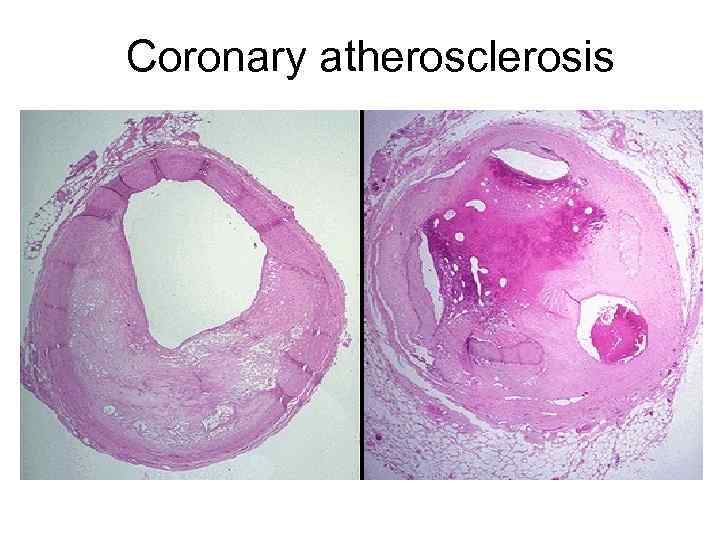
Coronary atherosclerosis
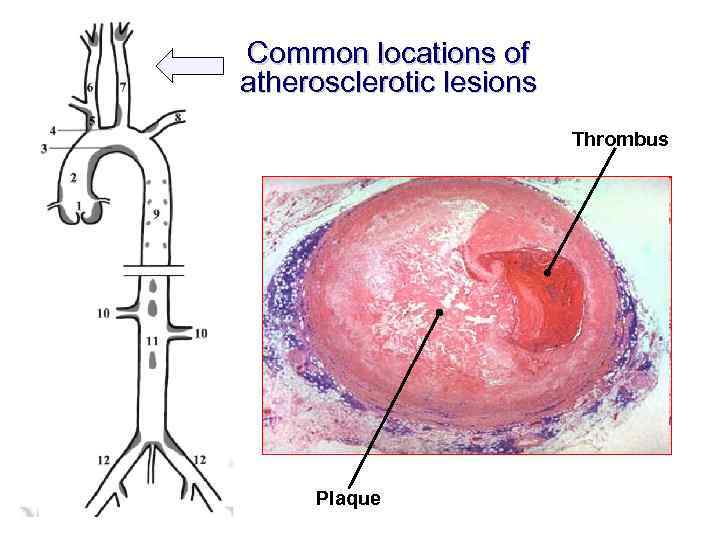
Common locations of atherosclerotic lesions Thrombus Plaque
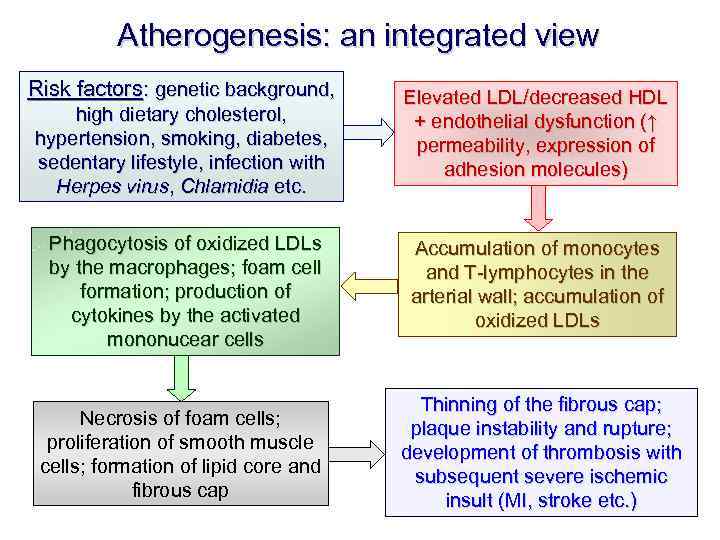
Atherogenesis: an integrated view Risk factors: genetic background, high dietary cholesterol, hypertension, smoking, diabetes, sedentary lifestyle, infection with Herpes virus, Chlamidia etc. Elevated LDL/decreased HDL + endothelial dysfunction (↑ permeability, expression of adhesion molecules) Phagocytosis of oxidized LDLs by the macrophages; foam cell formation; production of cytokines by the activated mononucear cells Accumulation of monocytes and T-lymphocytes in the arterial wall; accumulation of oxidized LDLs Necrosis of foam cells; proliferation of smooth muscle cells; formation of lipid core and fibrous cap Thinning of the fibrous cap; plaque instability and rupture; development of thrombosis with subsequent severe ischemic insult (MI, stroke etc. )
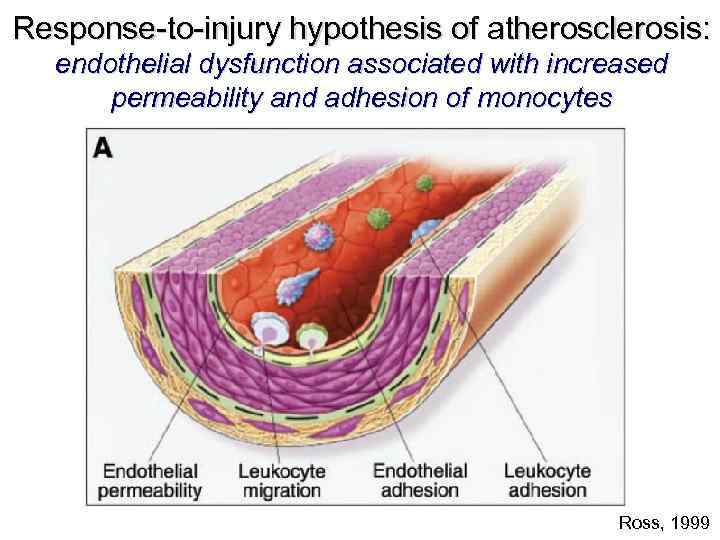
Response-to-injury hypothesis of atherosclerosis: endothelial dysfunction associated with increased permeability and adhesion of monocytes Ross, 1999
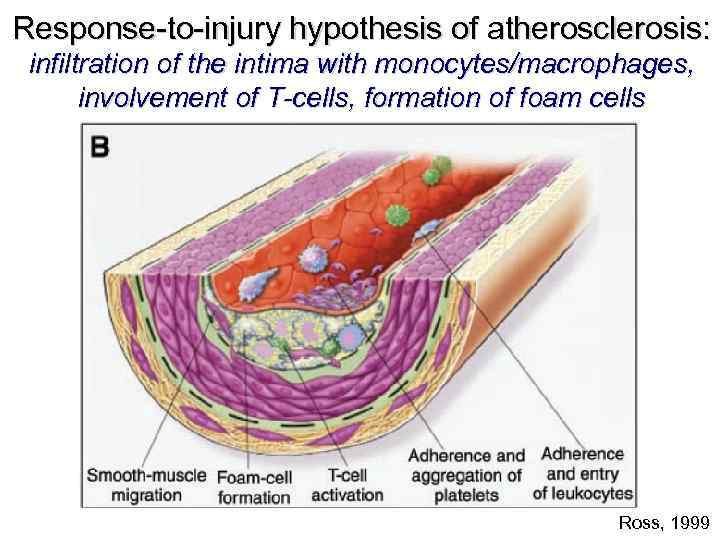
Response-to-injury hypothesis of atherosclerosis: infiltration of the intima with monocytes/macrophages, involvement of T-cells, formation of foam cells Ross, 1999
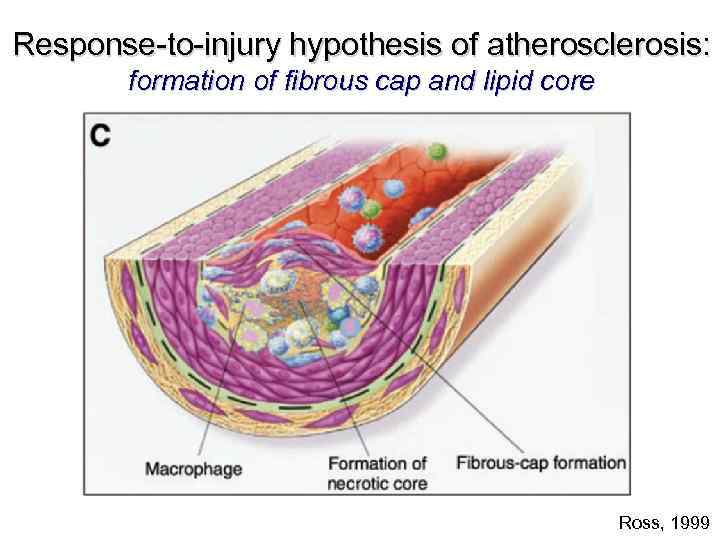
Response-to-injury hypothesis of atherosclerosis: formation of fibrous cap and lipid core Ross, 1999
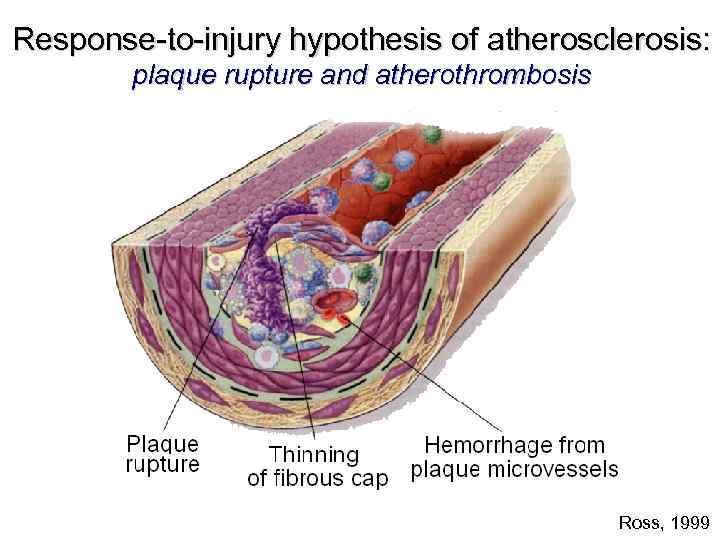
Response-to-injury hypothesis of atherosclerosis: plaque rupture and atherothrombosis Ross, 1999
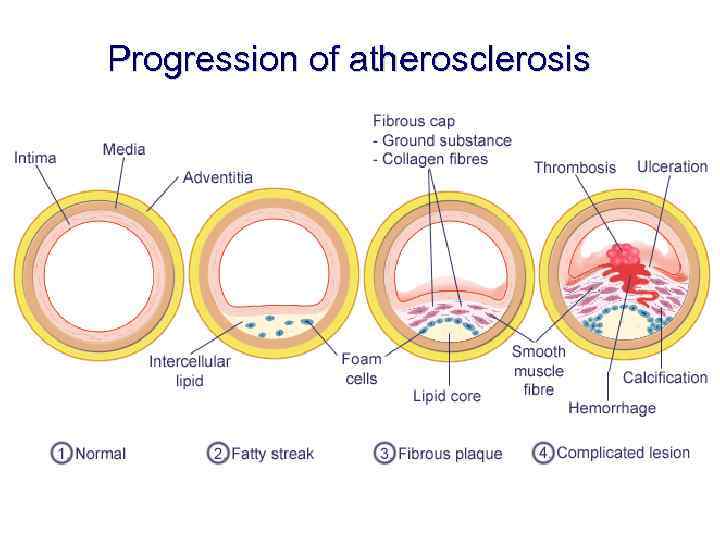
Progression of atherosclerosis
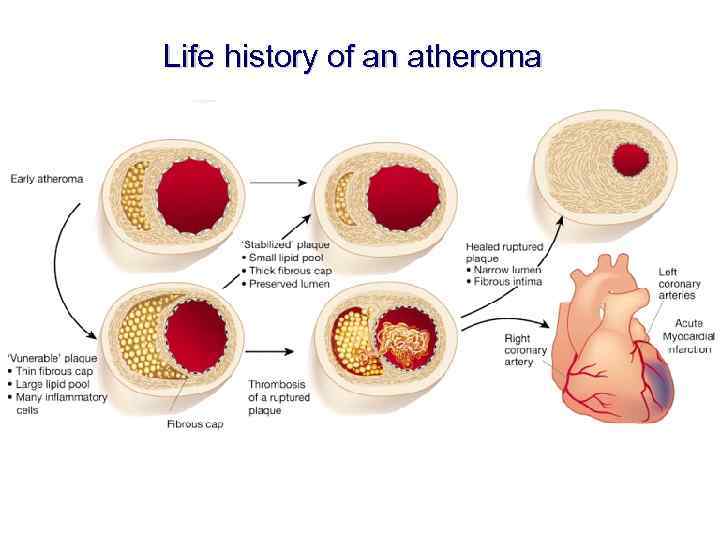
Life history of an atheroma
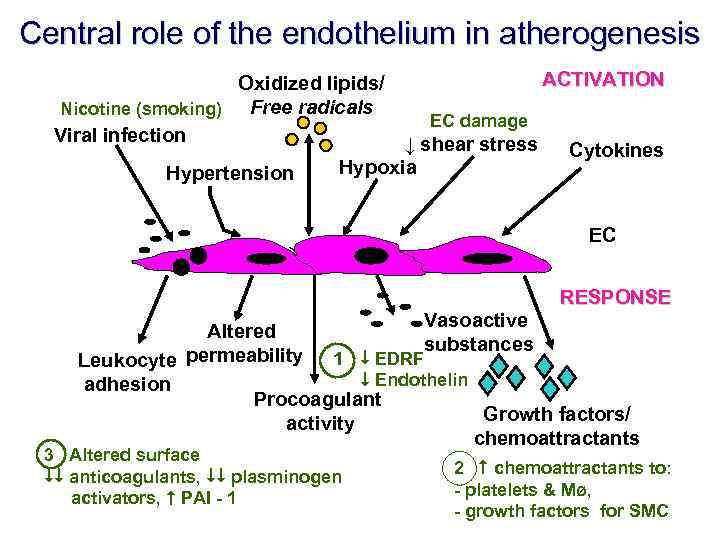
Central role of the endothelium in atherogenesis ACTIVATION Oxidized lipids/ Free radicals Nicotine (smoking) EC damage Viral infection ↓ shear stress Cytokines Hypoxia Hypertension EC RESPONSE Vasoactive Altered substances permeability 1 EDRF Leukocyte Endothelin adhesion Procoagulant Growth factors/ activity chemoattractants 3 Altered surface anticoagulants, plasminogen activators, PAI - 1 2 chemoattractants to: - platelets & Mø, - growth factors for SMC
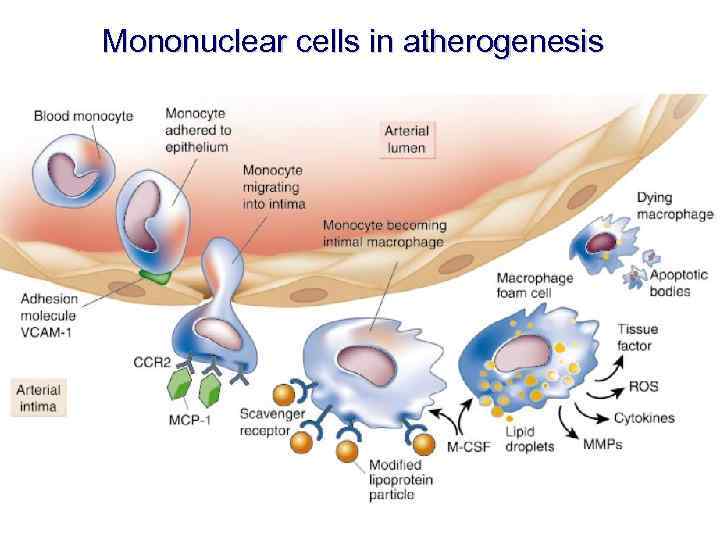
Mononuclear cells in atherogenesis
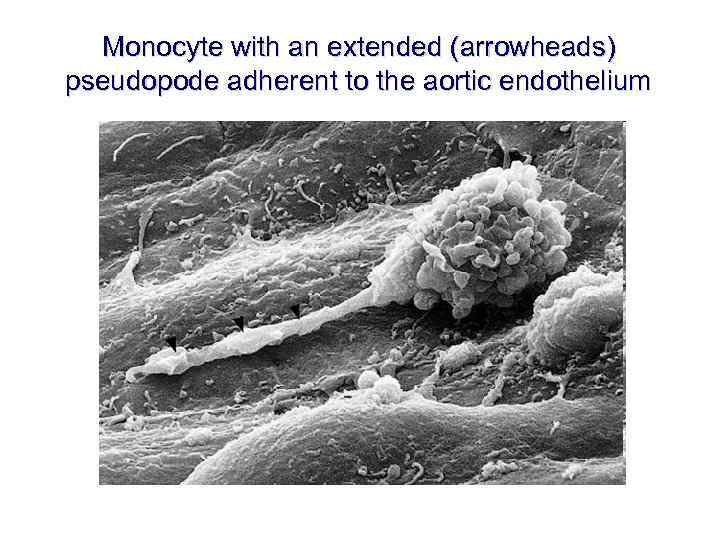
Monocyte with an extended (arrowheads) pseudopode adherent to the aortic endothelium
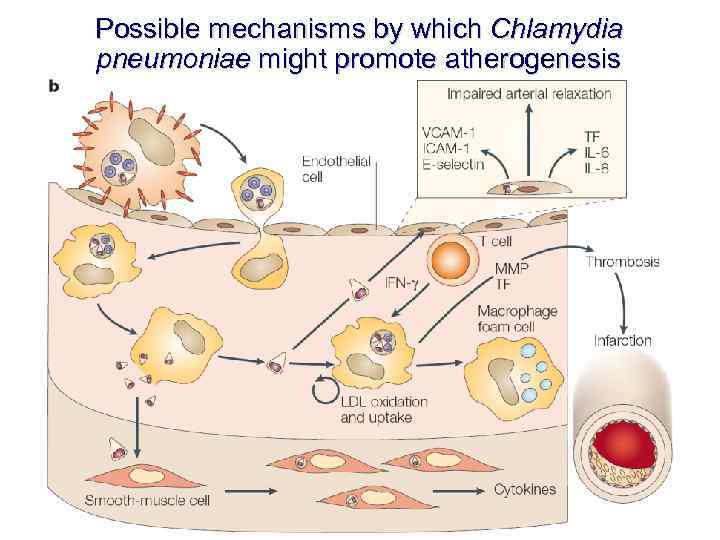
Possible mechanisms by which Chlamydia pneumoniae might promote atherogenesis
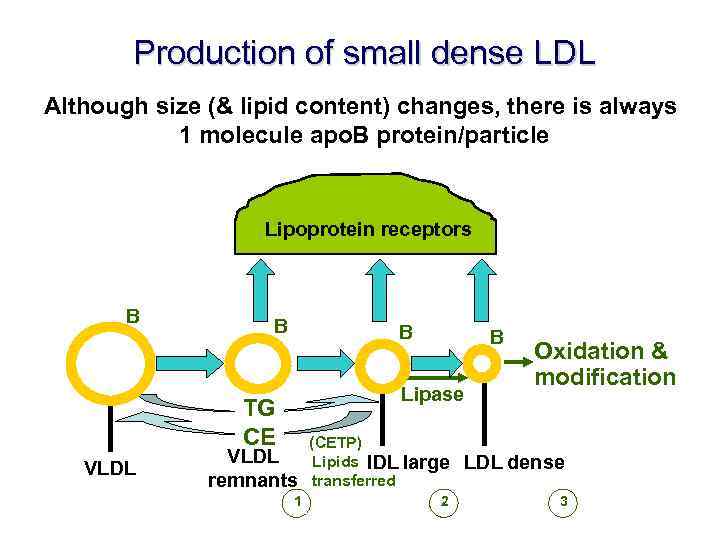
Production of small dense LDL Although size (& lipid content) changes, there is always 1 molecule apo. B protein/particle Lipoprotein receptors B B B Lipase TG CE VLDL B Oxidation & modification VLDL remnants (CETP) Lipids IDL large transferred LDL dense 1 2 3
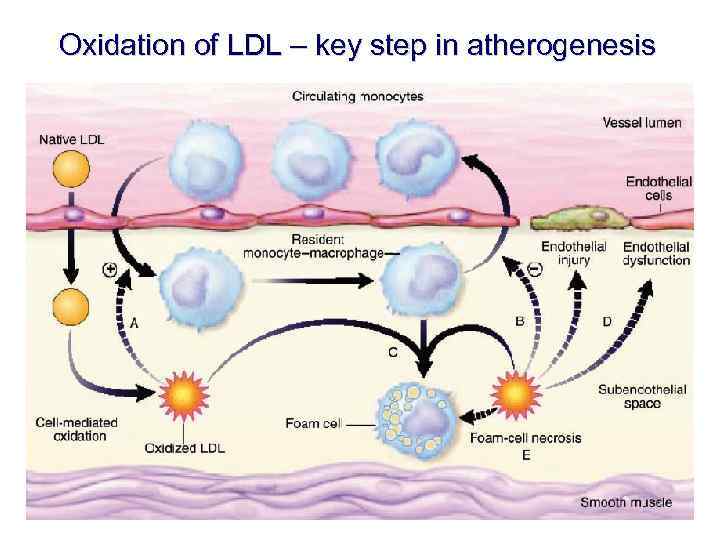
Oxidation of LDL – key step in atherogenesis
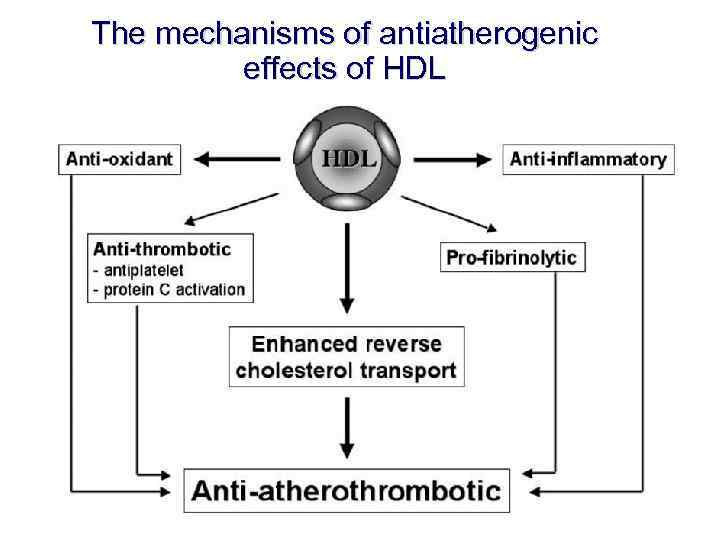
The mechanisms of antiatherogenic effects of HDL
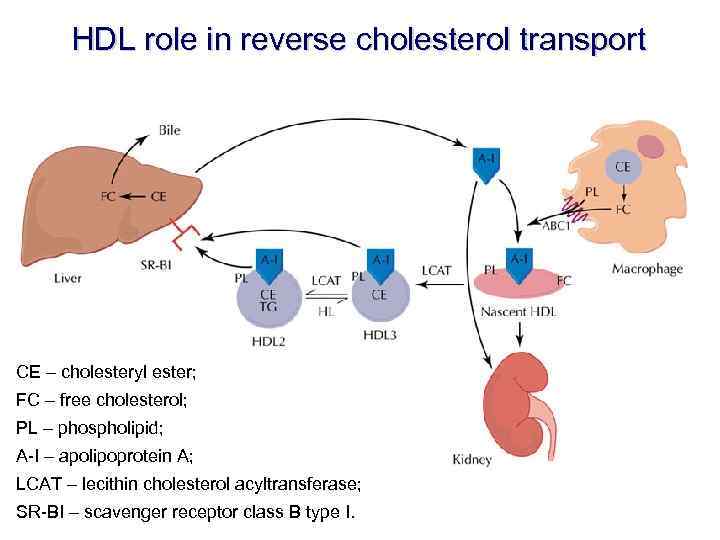
HDL role in reverse cholesterol transport CE – cholesteryl ester; FC – free cholesterol; PL – phospholipid; A-I – apolipoprotein A; LCAT – lecithin cholesterol acyltransferase; SR-BI – scavenger receptor class B type I.
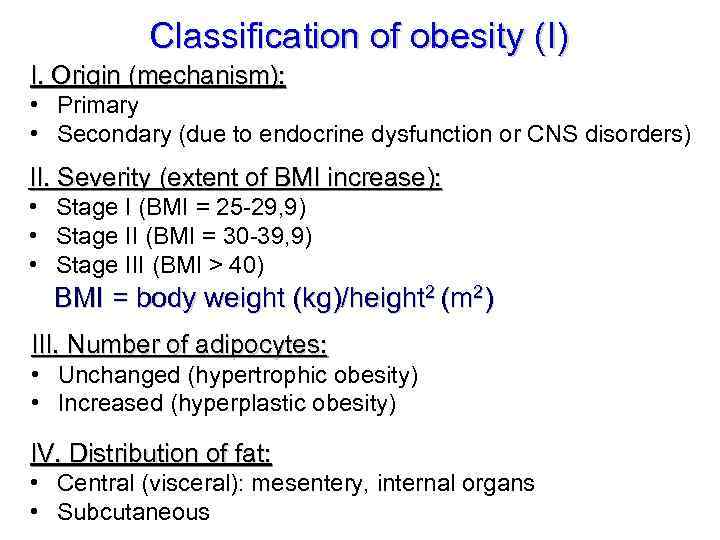
Classification of obesity (I) I. Origin (mechanism): • Primary • Secondary (due to endocrine dysfunction or CNS disorders) II. Severity (extent of BMI increase): • Stage I (BMI = 25 -29, 9) • Stage II (BMI = 30 -39, 9) • Stage III (BMI > 40) BMI = body weight (kg)/height 2 (m 2) III. Number of adipocytes: • Unchanged (hypertrophic obesity) • Increased (hyperplastic obesity) IV. Distribution of fat: • Central (visceral): mesentery, internal organs • Subcutaneous
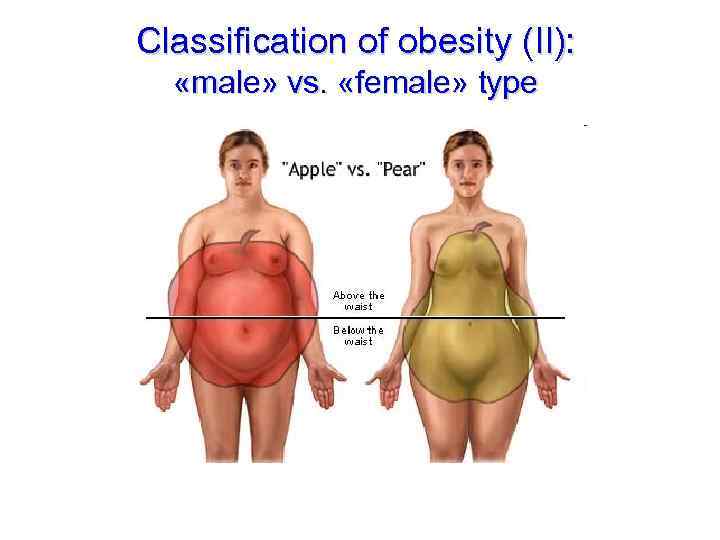
Classification of obesity (II): «male» vs. «female» type
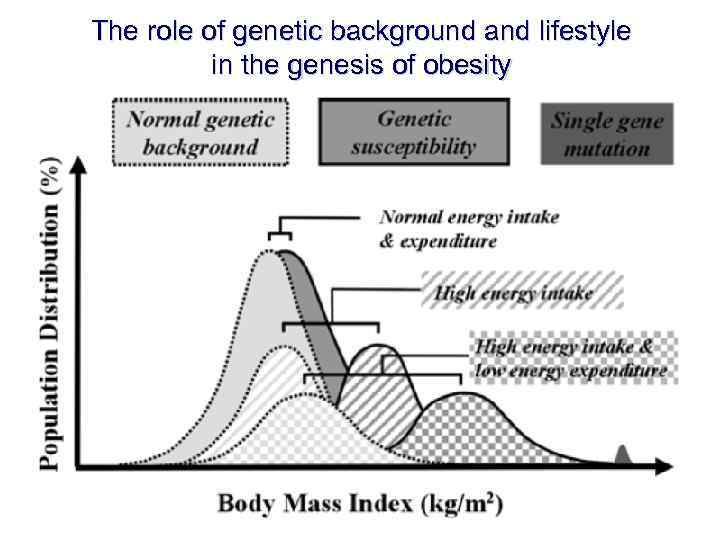
The role of genetic background and lifestyle in the genesis of obesity
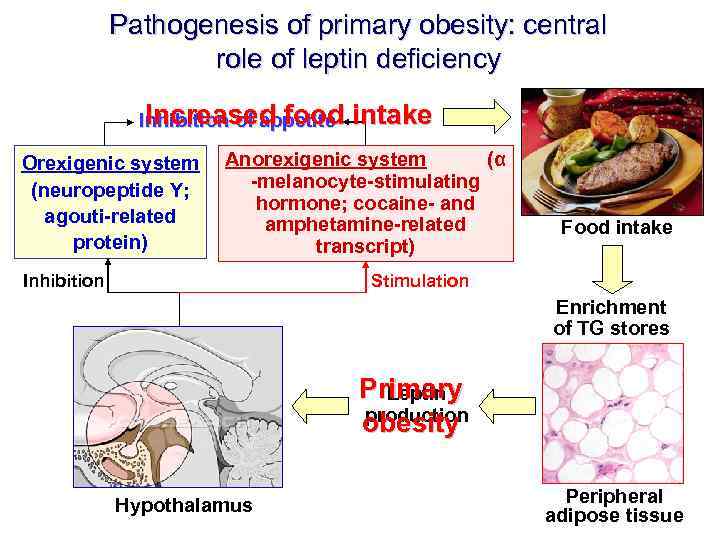
Pathogenesis of primary obesity: central role of leptin deficiency Increased food Inhibition of appetite Orexigenic system (neuropeptide Y; agouti-related protein) intake Anorexigenic system (α -melanocyte-stimulating hormone; cocaine- and amphetamine-related transcript) Inhibition Food intake Stimulation Enrichment of TG stores Primary Leptin production obesity Hypothalamus Peripheral adipose tissue
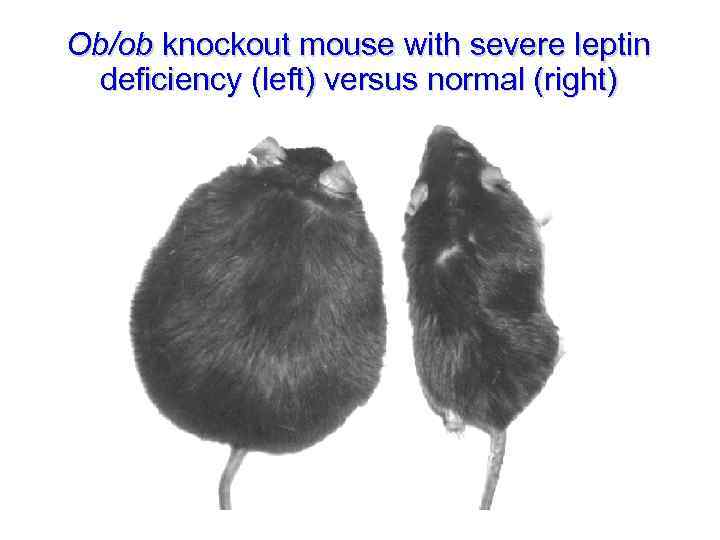
Ob/ob knockout mouse with severe leptin deficiency (left) versus normal (right)
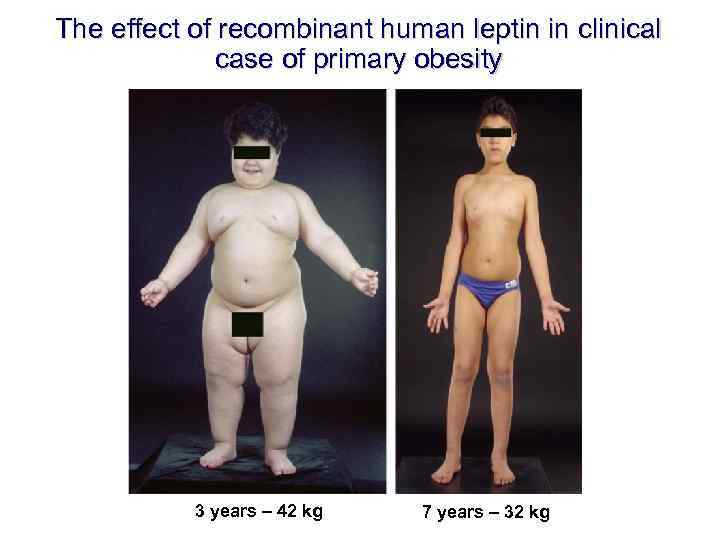
The effect of recombinant human leptin in clinical case of primary obesity 3 years – 42 kg 7 years – 32 kg
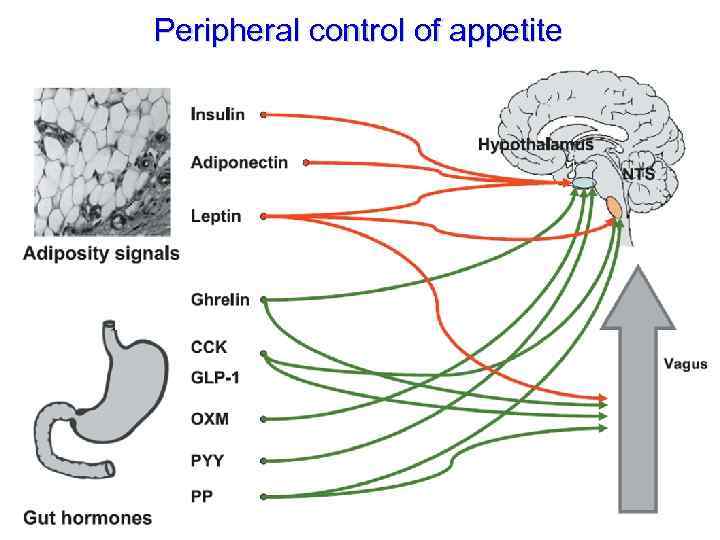
Peripheral control of appetite
Consequences of obesity 1. Increased risk of: 1. 1. Diabetes mellitus type II; 1. 2. Arterial hypertension; 1. 3. Coronary artery disease. 2. Cholelithiasis (gallstones); 3. Hypoventilation syndrome (pickwickian syndrome); 4. Degenerative joint disease (osteoarthritis); 5. Some reports show increased risk of stroke and cancer.
Lipid carbohydrate metabolism 2008.ppt