e3a277a7f095dff3bd89292cb441da22.ppt
- Количество слайдов: 26
METABOLIC DERANGEMENTS, HEPATIC FAILURE & PCRRT Patrick D. Brophy MD University of Michigan Pediatric Nephrology
Objectives Metabolic Disorders and Amenability to CRRT Hyperammonemia – – – Prescription Fine points of care Combination therapy Considerations of CRRT in Hepatic Failure – – – Hepatic Insufficiency Role of CRRT-bridge to transplant Liver support
Metabolic Disorders Multiple metabolic disorders have been described that are amenable to various forms of RRT. – Maple Syrup Urine Disease (BCAA—Build up lead to cerebral edema) Puliyanda et. al. 2002: 17: 239 -242 Jouvet et. al. 2001: 27: 1798 -1806 – Urea Cycle Defects- hyperammonemia – Organic Acidemias (accumulation of Acyl Co-A esterssecondary inhibition of urea cycle enzymes)
Hyperammonemia- clinical Most Cases develop in neonatal period – Feeding refusal/intolerance – Vomiting – Abnormal muscle tone – Lethargy – Seizures – Coma – Death
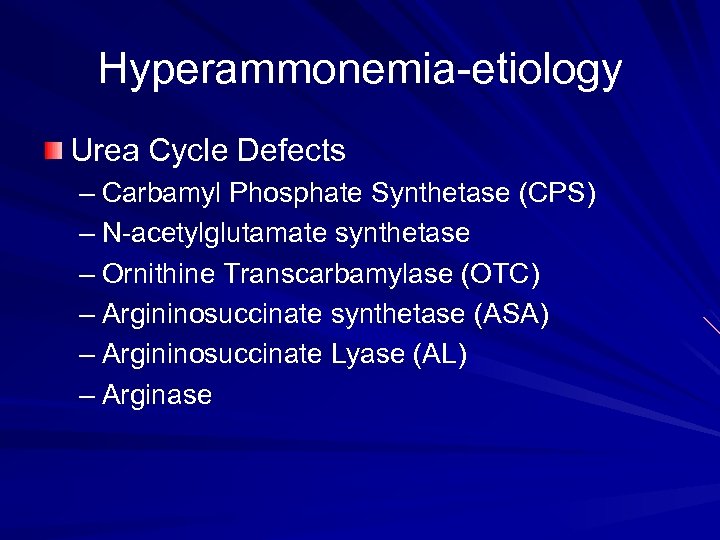
Hyperammonemia-etiology Urea Cycle Defects – Carbamyl Phosphate Synthetase (CPS) – N-acetylglutamate synthetase – Ornithine Transcarbamylase (OTC) – Argininosuccinate synthetase (ASA) – Argininosuccinate Lyase (AL) – Arginase
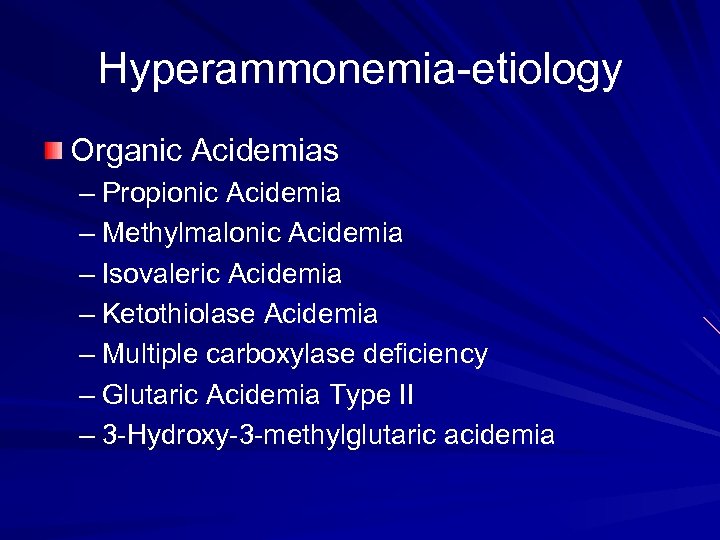
Hyperammonemia-etiology Organic Acidemias – Propionic Acidemia – Methylmalonic Acidemia – Isovaleric Acidemia – Ketothiolase Acidemia – Multiple carboxylase deficiency – Glutaric Acidemia Type II – 3 -Hydroxy-3 -methylglutaric acidemia
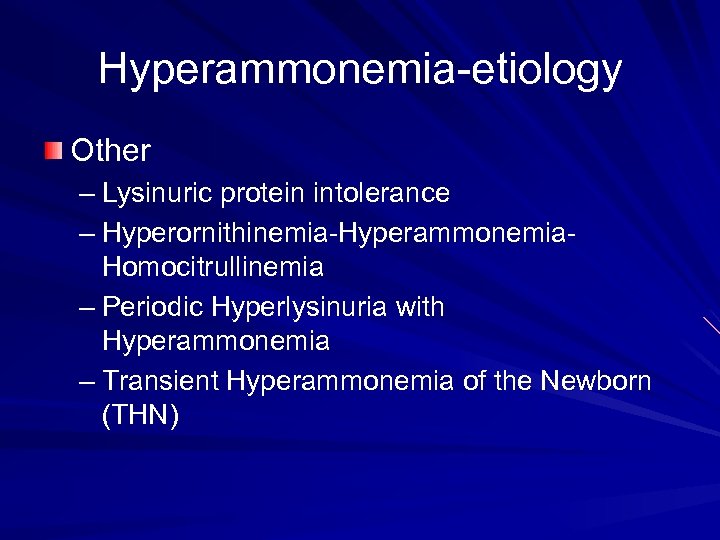
Hyperammonemia-etiology Other – Lysinuric protein intolerance – Hyperornithinemia-Hyperammonemia. Homocitrullinemia – Periodic Hyperlysinuria with Hyperammonemia – Transient Hyperammonemia of the Newborn (THN)
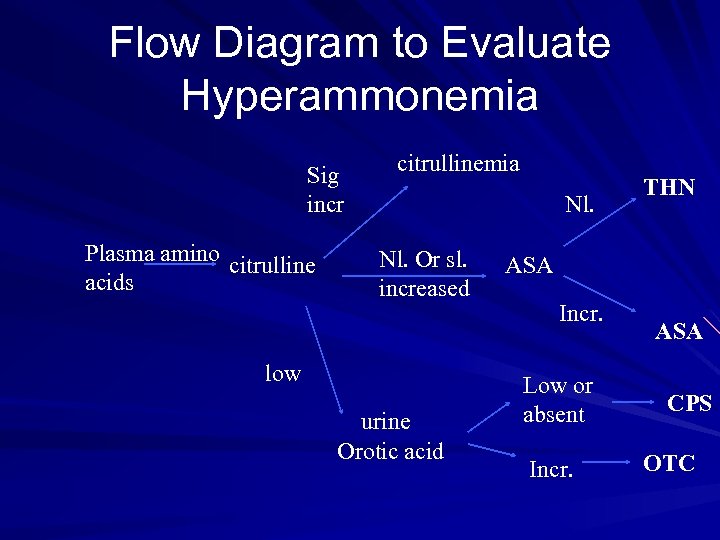
Flow Diagram to Evaluate Hyperammonemia Sig incr Plasma amino citrulline acids citrullinemia Nl. Or sl. increased low urine Orotic acid THN ASA Incr. Low or absent Incr. ASA CPS OTC
Treatment of Hyper. Ammonemia Aim: rapid therapy to prevent permanent brain damage or death Prevent further catabolism by providing adequate calories, fluids and electrolytes Minimize protein intake Provide alternate pathways for ammonia removal – Sodium benzoate – Sodium phenylacetate – Arginine supplementation
Mode of RRT PD – Some clearance-but less than optimal – Too long for optimal removal, may not be able to keep place with NH 4 generation Hemodialysis – looks like a good place to start Hemofiltration – a great way to go home at night
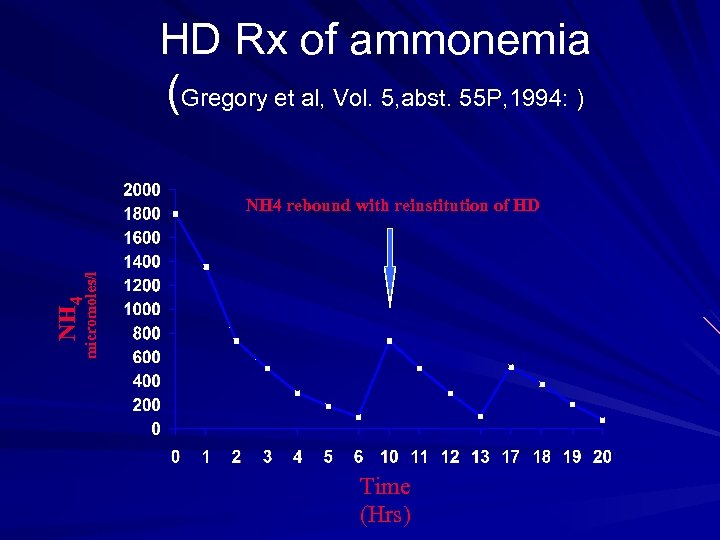
HD Rx of ammonemia (Gregory et al, Vol. 5, abst. 55 P, 1994: ) NH 4 micromoles/l NH 4 rebound with reinstitution of HD Time (Hrs)
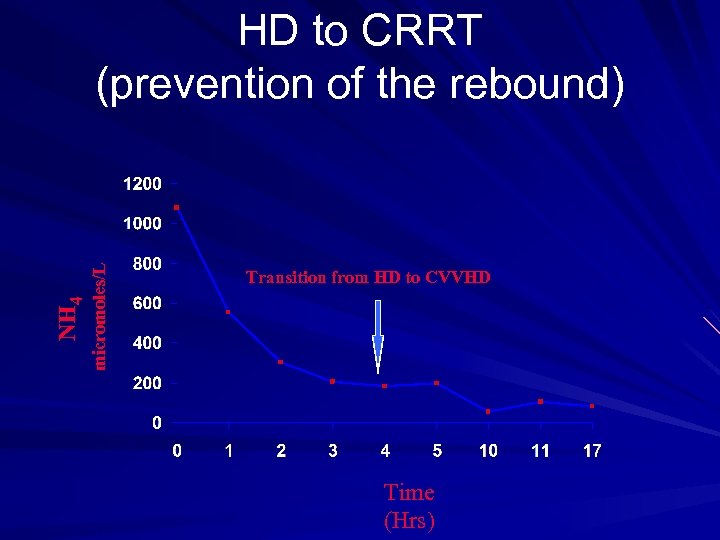
micromoles/L NH 4 HD to CRRT (prevention of the rebound) Transition from HD to CVVHD Time (Hrs)
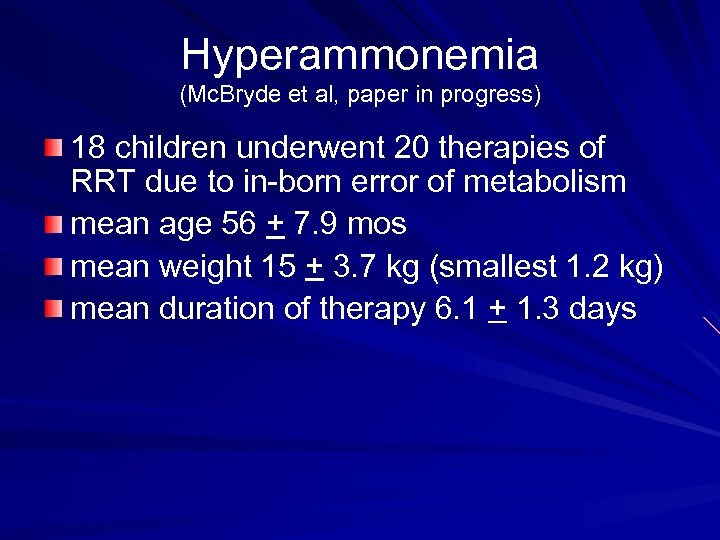
Hyperammonemia (Mc. Bryde et al, paper in progress) 18 children underwent 20 therapies of RRT due to in-born error of metabolism mean age 56 + 7. 9 mos mean weight 15 + 3. 7 kg (smallest 1. 2 kg) mean duration of therapy 6. 1 + 1. 3 days
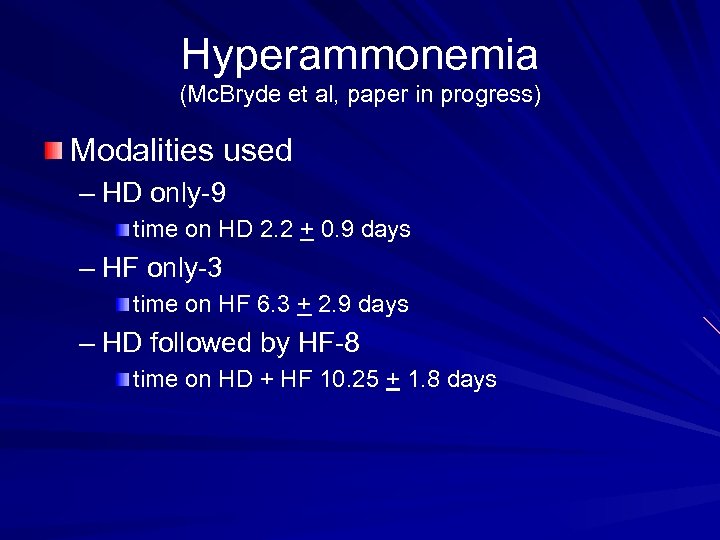
Hyperammonemia (Mc. Bryde et al, paper in progress) Modalities used – HD only-9 time on HD 2. 2 + 0. 9 days – HF only-3 time on HF 6. 3 + 2. 9 days – HD followed by HF-8 time on HD + HF 10. 25 + 1. 8 days
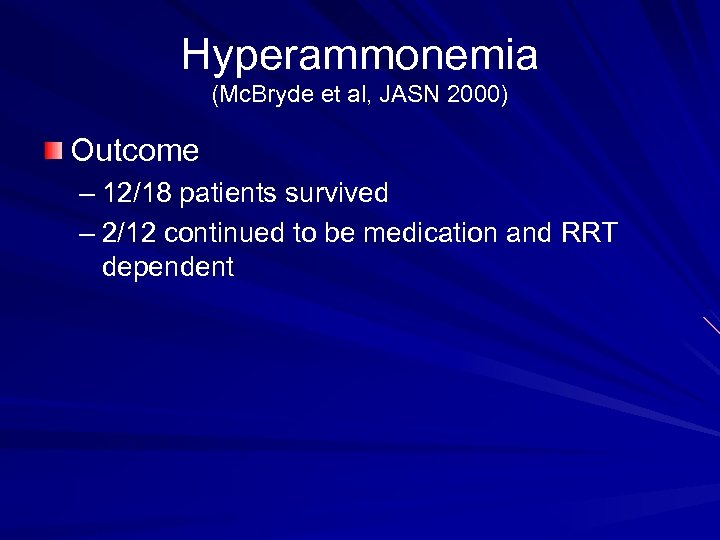
Hyperammonemia (Mc. Bryde et al, JASN 2000) Outcome – 12/18 patients survived – 2/12 continued to be medication and RRT dependent
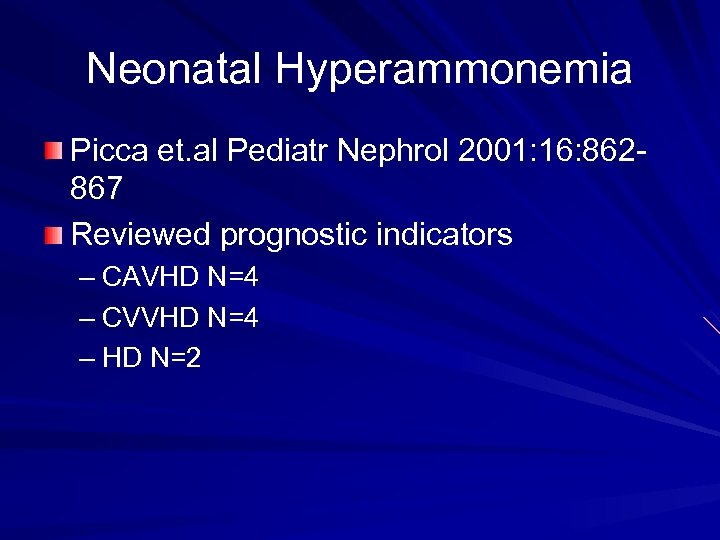
Neonatal Hyperammonemia Picca et. al Pediatr Nephrol 2001: 16: 862867 Reviewed prognostic indicators – CAVHD N=4 – CVVHD N=4 – HD N=2
Neonatal Hyperammonemia Findings: – NH 4 levels decreased with all modalities (1419 to 114 micromoles/L) with CVVHD giving the highest NH 4 clearance & HD giving best NH 4 extraction (hemodynamic instability) – 5 had good outcome/5 had poor (not specific to modality) primarily associated with Coma duration < 33 hrs (CNS delay/Death) – Early intervention is key!
Hepatic Failure Definition: Loss of functional liver cell mass below a critical level results in liver failure (acute or complicating a chronic liver disease) Results in: hepatic encephalopathy & Coma, Jaundice, cholestasis, ascites, bleeding, renal failure, death
Hepatic Failure Production of Endogenous Toxins & Drug metabolic Failure Bile Acids, Bilirubin, Prostacyclins, NO, Toxic fatty acids, Thiols, Indol-phenol metabolites These toxins cause further necrosis/apoptosis and a vicious cycle Detrimental to renal, brain and bone marrow function; results in poor vascular tone
Hepatic Failure- Role of CRRT Objective: – CRRT support can buy time, help prevent further deterioration/complication and allow Potential recovery of functional critical cell mass Management of precipitating events that lead to decompensated disease Bridge to liver transplantation
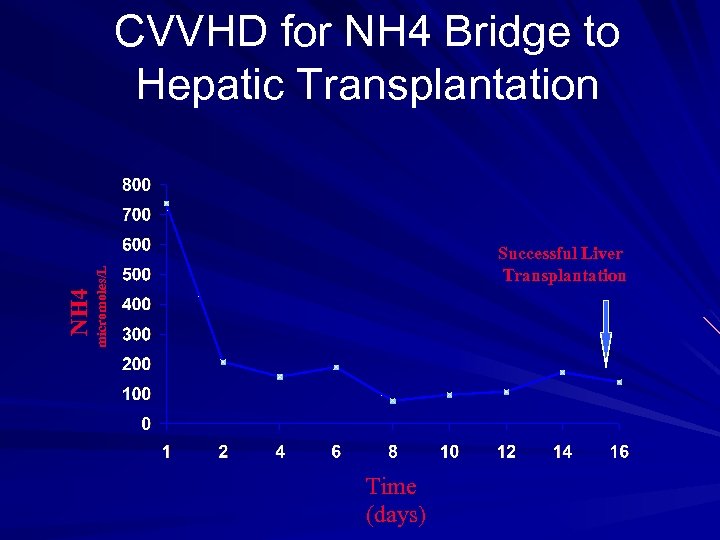
Successful Liver Transplantation micromoles/L NH 4 CVVHD for NH 4 Bridge to Hepatic Transplantation Time (days)
Hepatic Failure-Role of CRRT may not improve overall outcome of liver failure- but does provide stability and prolongs life in the setting of hepatic failure Primary applications include use in control of elevated ICP in fulminant hepatic failure (Davenport Lancet 1991: 2: 1604) Management of Cerebral Edema through middle molecule removal- reversal of Coma (Matsubara et. al. Crit Care Med 1990: 8: 1331)
Hepatic Failure-Role of CRRT Improved Cardiac Stability also noted in patients with Hepatic & Renal Failure – IHD vs CAVHD compared – Noted a decrease in Cardiac Index of ~ 15% in HD treated patients (also increase in ICP ~ 45% in HD) – CAVHD/CVVHD- cardiac index decreased by ~3% and no change noted in ICP – Davenport et. al. Crit Care Med 1993: 21: 328 -338
Hepatic Failure-Role of CRRT Others: – Fluid Balance – Nutritional support – Uremic Clearance
Future Horizons Currently Undergoing Clinical Evaluation – Liver Assist Devices – several companies (ie MARSMolecular Adsorbents Recycling System) – Both Biological and non- biological systems (ie porcine hepatocytes/hemodialysis filters/hemofilters – Engage principles of both convection and diffusion (ie albumin dialysate) and anionic trapping with charcoal regeneration chambers for albumin – Huge potential Impact on critical care & Transplantation!
ACKNOWLEDGEMENTS (p. brophy) – MELISSA GREGORY – ANDREE GARDNER – JOHN GARDNER – THERESA MOTTES – TIM KUDELKA – LAURA DORSEY & BETSY ADAMS
e3a277a7f095dff3bd89292cb441da22.ppt