d64baf1d123f2298b163333eb4c2c32d.ppt
- Количество слайдов: 22
Mental health and Somali Community DR FATUMO ABDI SPECIALITY REGISTRAR IN PUBLIC HEALTH
Somali People
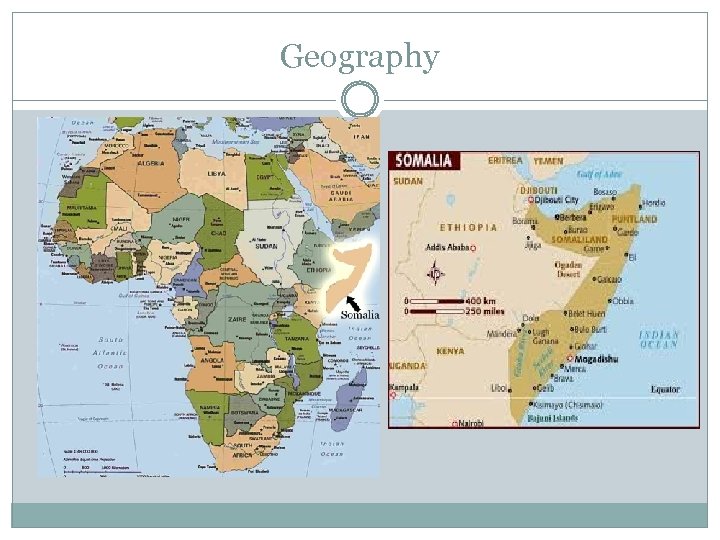
Geography
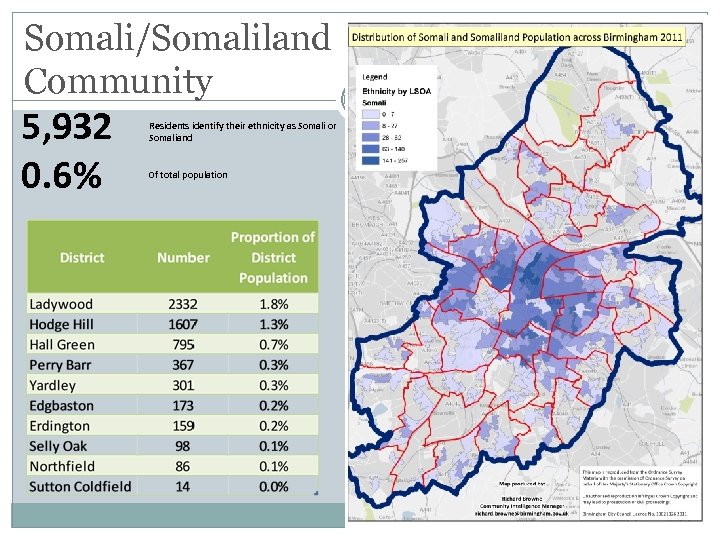
Somali/Somaliland Community 5, 932 0. 6% Residents identify their ethnicity as Somali or Somaliand Of total population
Distribution of ethnic communities across Birmingham
Identity 1 st generation: Economic migrants International students Political refugees Refugees/asylum seekers 2 nd generation 70’s/80’s – economic migrants (UK, middle east, East Africa) Late 80’s – 90’s onwards – fled war or parents settled in one place and re-settled in UK
Identity 3 rd generation - ? ? ? Most similar to indigenous British population Links to land, language and culture weakest More ethnic mixing Not a homogenous community !
Mental health triggers § WAR § Family breakdown § § § family reunion difficulties marital breakdown parenting § Isolation § Unemployment § Money § Acculturation § Identity § Qat, drug/alcohol misuse § PND
Triggers § Expectations not fulfilled § Negative host attitudes § Qualification not recognized
Barriers Stigma Taboo Language/interpreters Self-inflicted (sinful behaviour) Unseen – jinn, black magic, evil eye Concept of time
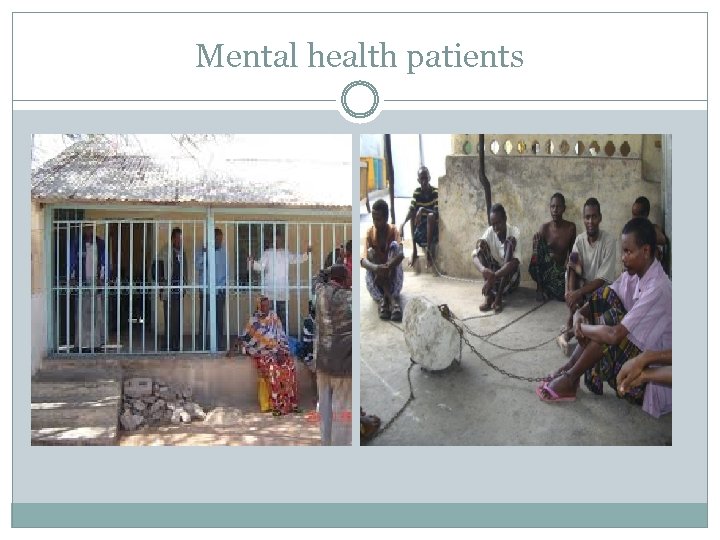
Mental health patients
Common problems Depression Anxiety PTSD Somatic complaints Problems with acculturation Parenting problems Physical disorders associated with chronic stress Hypertension diabetes
Perceptions of mental health “Nin madaxa laga haayo, meeli uma fiyooba” If a person has a sickness or pain in their head, no other parts will work
Language of mental illness ‘Not normal’ Binary view of mental health (ill vs well) Ø Isku buq (Confused) Ø Islahadal (Talking to yourself) Ø Wel wel/ wer (Worried) Ø Buufis (Not normal)
Cultural Barrier to Seeking Services Potential service seekers are afraid of being stigmatized as a crazy, weak or lack faith Not understanding the purpose of mental health and counseling Believing that they can resolve their issues on their own Counseling is perceived as a waste of time
General Barriers to Service Transportation Not being aware or able to identify their problems. Lack more imminent basic needs such as adequate housing, employment and other resources.
Support for Somalis in relation to mental health Religion Family Community
Approaches to Somali-specific mental health initiatives 18 Commissioning Evidence-based interventions targeted at the community range of culturally appropriate early interventions in the community and primary care setting. Data collection identify Somali patients Migration status Primary care

Partnerships 19 Strategic partnerships addressing external factors associated with poor mental health housing, employment and refugee & asylum seekers. Strong links with third sector Somali community organisations: their knowledge Service delivery of BAME-focused initiatives Education/awareness programmes Stigma Building mental health resilience
Prevention 20 Explore targets for primary prevention Risk of psychosis is much higher in populations that experience: family breakdown, urban upbringing, socio-economic disadvantage, bullying, excessive school mobility and cannabis use. Young people and mental health reduce the impact of gang culture and youth crime schools-based initiatives Faith-based organisations community education initiatives which would include improving access to care Building Social capital and Community Health and Well- being initiatives within communities
Clinical Implications Treatment options acceptability chance of success Confidentiality and Empathy Facilitation of Communication

Thank you Fatumo. abdi@birmingham. gov. uk
d64baf1d123f2298b163333eb4c2c32d.ppt