16f4096005ed22df6b41c57857da8175.ppt
- Количество слайдов: 60
Megaloblastic Anemia Teoman SOYSAL Prof. MD
Megaloblastic Anemia n A subclass of macrocytic anemia (under morphologic classification) Or n A subclass of anemias due to defective DNA synthesis (pathogenetic classification)
Megaloblastic Anemia n Main causes of “Megaloblastic Anemia” – Vit. B 12 deficiency – Folic acid deficiency – Others
Megaloblastic Anemia n 30 -50 % of all macrocytic anemias are caused by folic acid and/or Vit. B 12 deficiency.
Vit B 12 n Metabolic active cobalamins in the body are; – Methyl cobalamin and adenosyl cobalamin Hydroxocobalamin can be reversed to the above cobalamins. n Pharmacy: n – Most stable cobalamin: cyanocobalamin
Vit B 12 n Natural forms – Produced by microorganisms (bacteria/fungi) – Plants do not produce or contain Vit B 12 (except contamination) – Colonic bacterial production occurs but their location is distal to the site of absorbtion
Vit. B 12 n Food sources rich in Vit. B 12 – Liver – Kidney – Muscle – Egg – Milk , Cheese and other diary products – Seafood
Plants are not sources of Vit. B 12
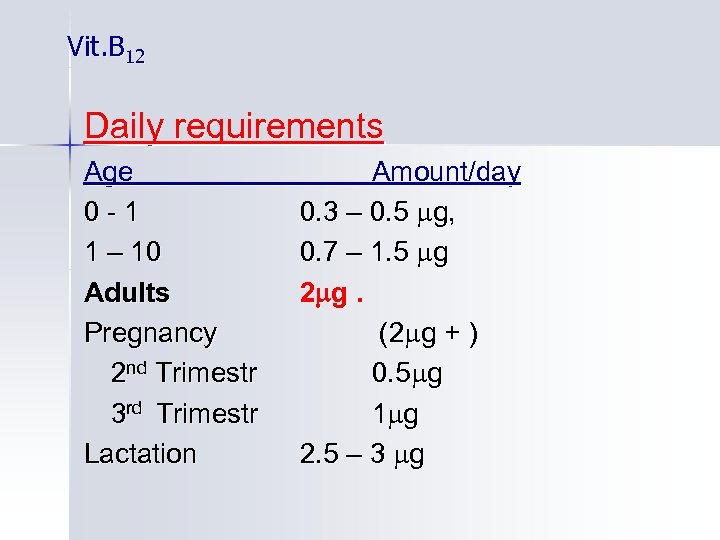
Vit. B 12 Daily requirements Age 0 -1 1 – 10 Adults Pregnancy 2 nd Trimestr 3 rd Trimestr Lactation Amount/day 0. 3 – 0. 5 g, 0. 7 – 1. 5 g 2 g. (2 g + ) 0. 5 g 1 g 2. 5 – 3 g
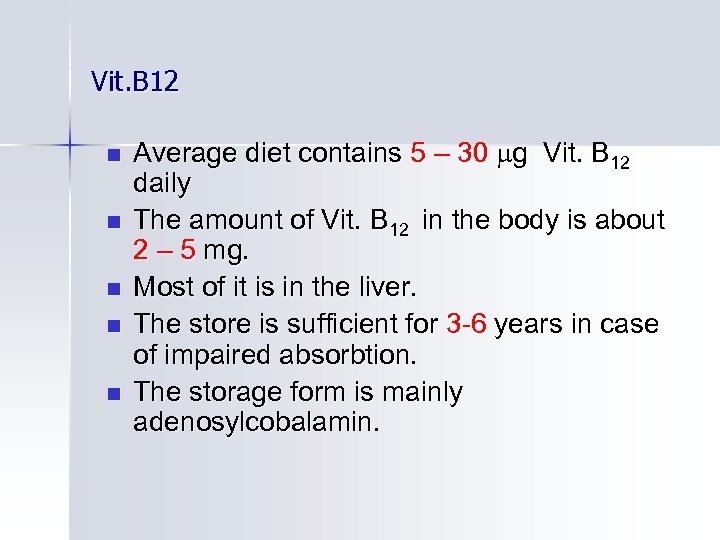
Vit. B 12 n n n Average diet contains 5 – 30 g Vit. B 12 daily The amount of Vit. B 12 in the body is about 2 – 5 mg. Most of it is in the liver. The store is sufficient for 3 -6 years in case of impaired absorbtion. The storage form is mainly adenosylcobalamin.
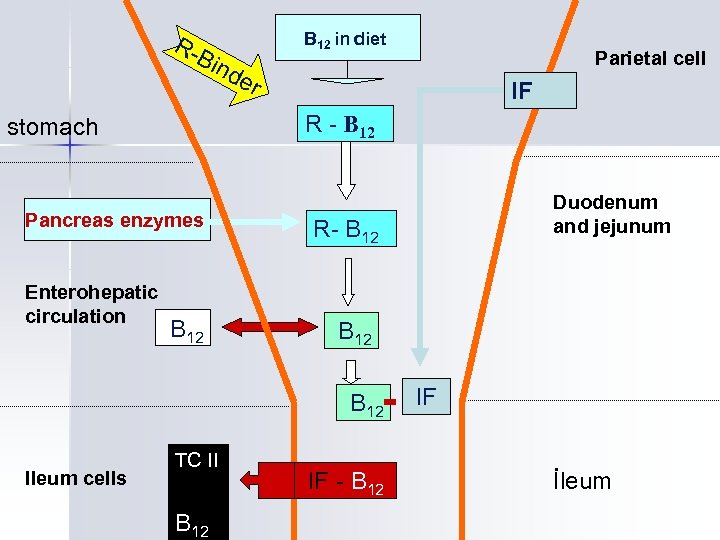
R- Bin B 12 in diet Pancreas enzymes r IF B 12 TC II B 12 Duodenum and jejunum R- B 12 Ileum cells Parietal cell R - B 12 stomach Enterohepatic circulation de IF - B 12 IF İleum
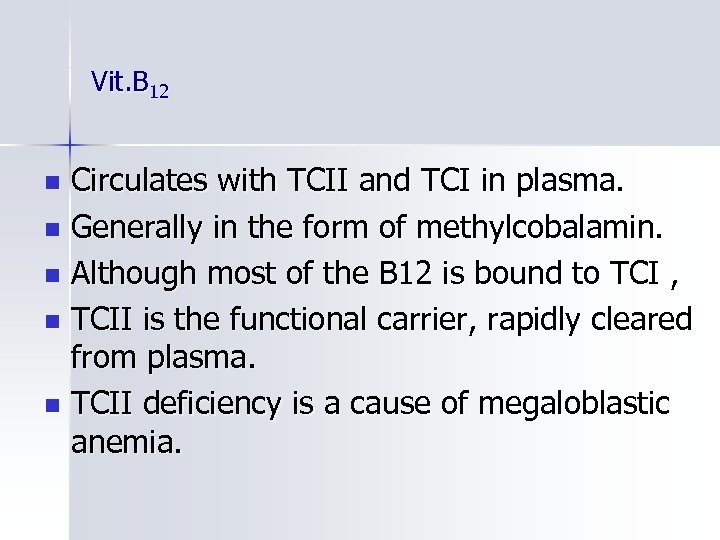
Vit. B 12 Circulates with TCII and TCI in plasma. n Generally in the form of methylcobalamin. n Although most of the B 12 is bound to TCI , n TCII is the functional carrier, rapidly cleared from plasma. n TCII deficiency is a cause of megaloblastic anemia. n
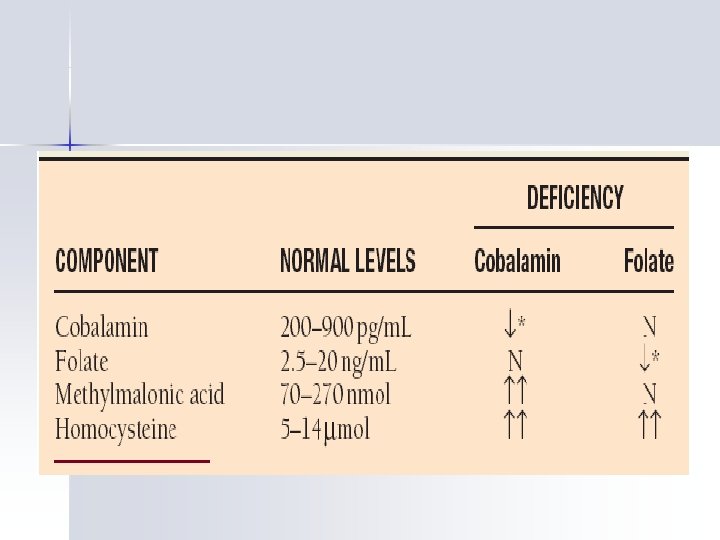
Vit. B 12 Plazma level of Vit. B 12 n 200 - 900 ng/ L
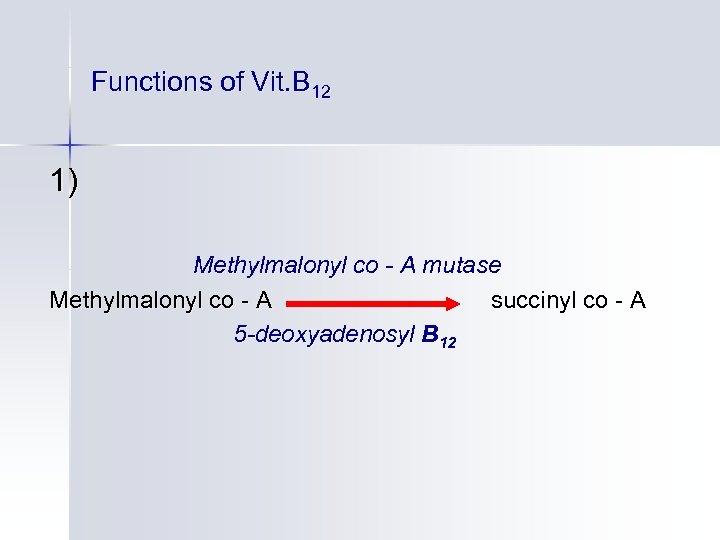
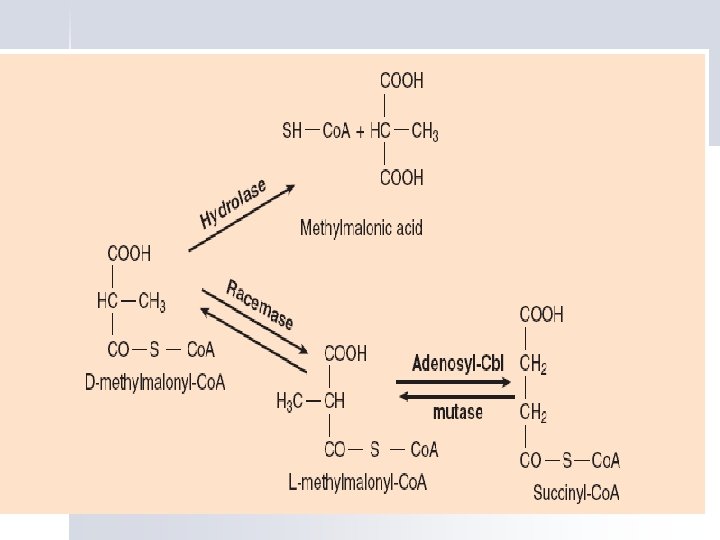
Functions of Vit. B 12 1) Methylmalonyl co - A mutase Methylmalonyl co - A succinyl co - A 5 -deoxyadenosyl B 12
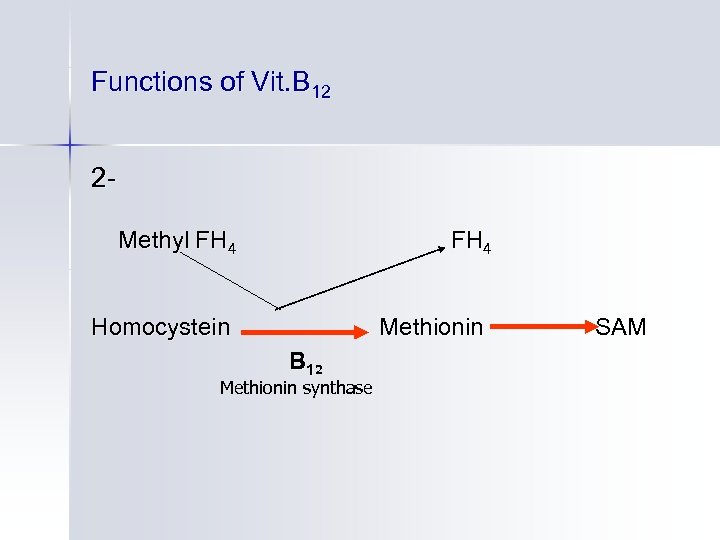
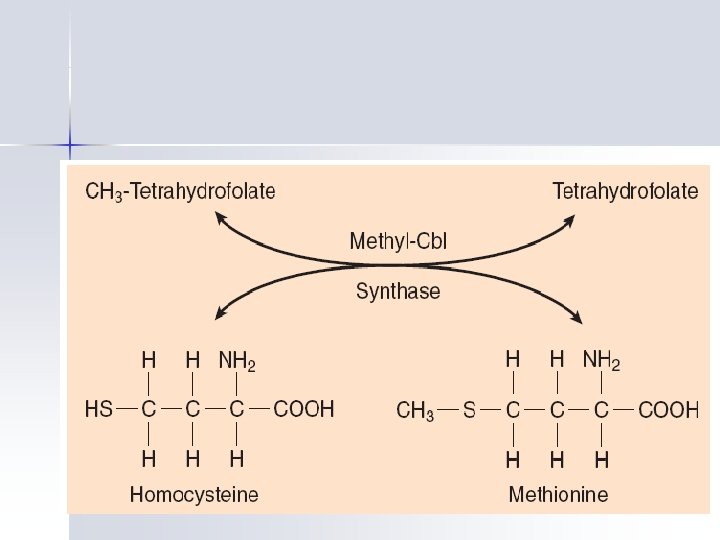
Functions of Vit. B 12 2 Methyl FH 4 Homocystein Methionin B 12 Methionin synthase SAM
Folic Acid Pteroyl glutamic acid and similar compounds are termed as folic acid. Polyglutamate is the natural form. Dihydro or tetrahydro folate are metabolic active forms.
Folic acid Sources : n n Produced by plants and some microorganisms Folate rich foods; – vegetables (Green leaf), – Liver and kidney (parenchymal organs) – Molds.
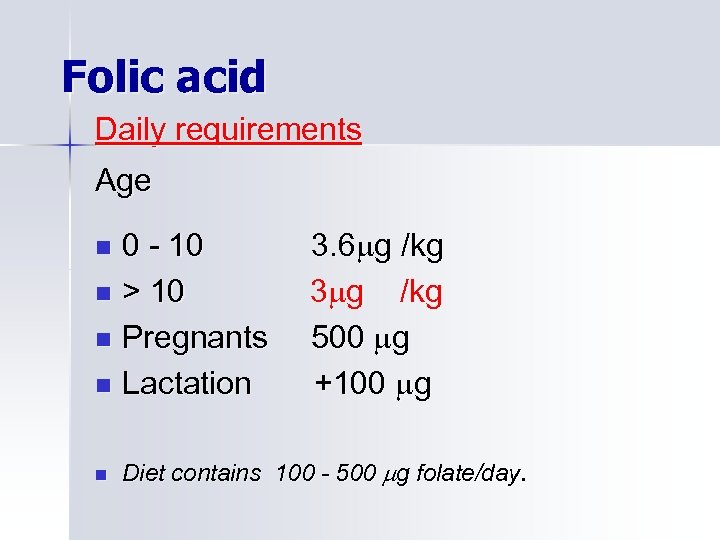
Folic acid Daily requirements Age 0 - 10 n > 10 n Pregnants n Lactation n n 3. 6 g /kg 3 g /kg 500 g +100 g Diet contains 100 - 500 g folate/day.
Folate absorbtion n Mainly jejunum. n In the form of monoglutamate. n Methyltetrahydrofolate monoglutamate is the form it is found in serum.

Folate levels: Normal ranges n n Serum: Red cell: 6 – 21 g/L (RBC volume) 160 – 640 g/L (RBC volume) Folate deficiency n n Serum folate : Red cell folate: <4 g /L <140 g /L
Folate stores n Total body folate: 5 – 20 mg n Storage place : Liver n Storage form: Methyl-FH 4 polyglutamate
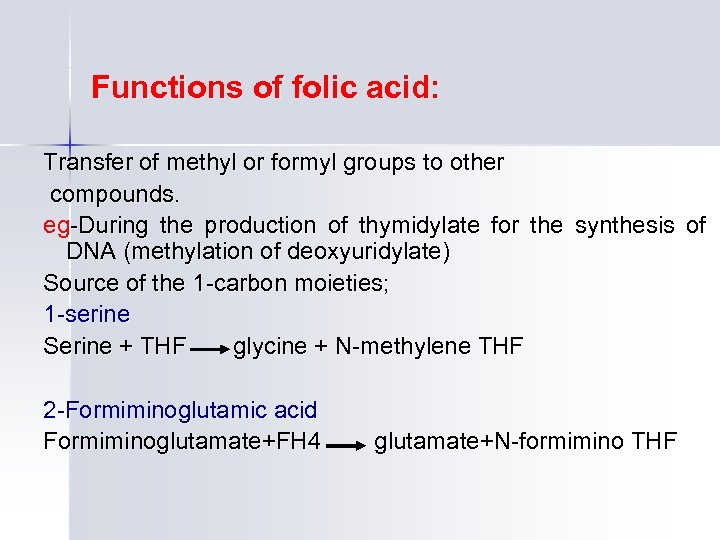
Functions of folic acid: Transfer of methyl or formyl groups to other compounds. eg-During the production of thymidylate for the synthesis of DNA (methylation of deoxyuridylate) Source of the 1 -carbon moieties; 1 -serine Serine + THF glycine + N-methylene THF 2 -Formiminoglutamic acid Formiminoglutamate+FH 4 glutamate+N-formimino THF
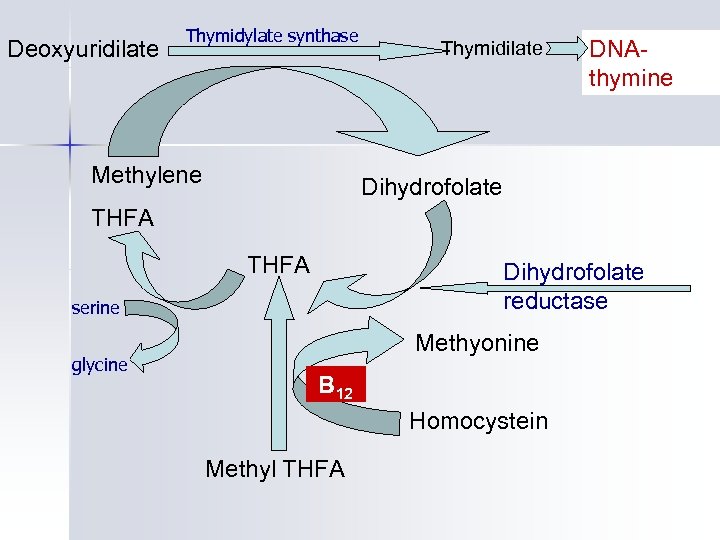
Deoxyuridilate Thymidylate synthase Methylene Thymidilate DNAthymine Dihydrofolate THFA Dihydrofolate reductase serine glycine Methyonine B 12 Homocystein Methyl THFA
Megaloblastic Hematopoiesis Anemia +/- leukopenia +/thrombocytopenia. Causes of cytopenias : 1 -DNA synthesis is deranged 2 -Ineffective hematopoiesis 3 -Shortened RBC survival n
Causes of Megaloblastic Anemia Vit. B 12 deficiency n Folate deficiency n Other causes n
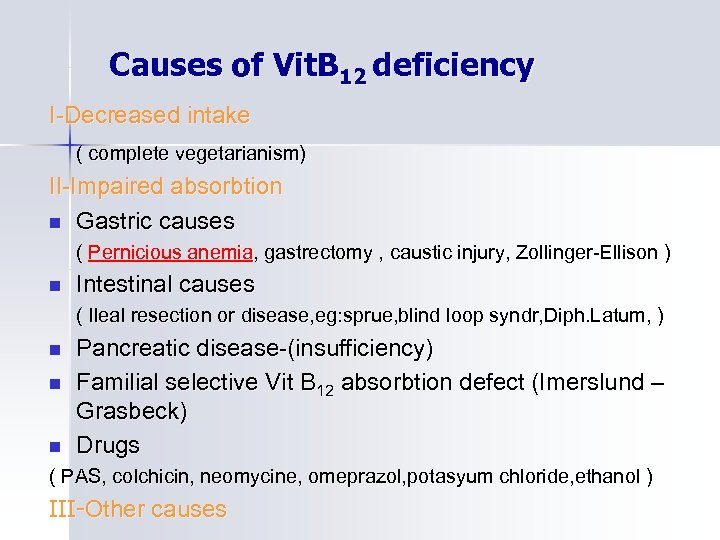
Causes of Vit. B 12 deficiency I-Decreased intake ( complete vegetarianism) II-Impaired absorbtion n Gastric causes ( Pernicious anemia, gastrectomy , caustic injury, Zollinger-Ellison ) n Intestinal causes ( Ileal resection or disease, eg: sprue, blind loop syndr, Diph. Latum, ) n n n Pancreatic disease-(insufficiency) Familial selective Vit B 12 absorbtion defect (Imerslund – Grasbeck) Drugs ( PAS, colchicin, neomycine, omeprazol, potasyum chloride, ethanol ) III-Other causes
Causes of folate deficiency Decreased intake n Increased demands n Drug related folate insufficiency n
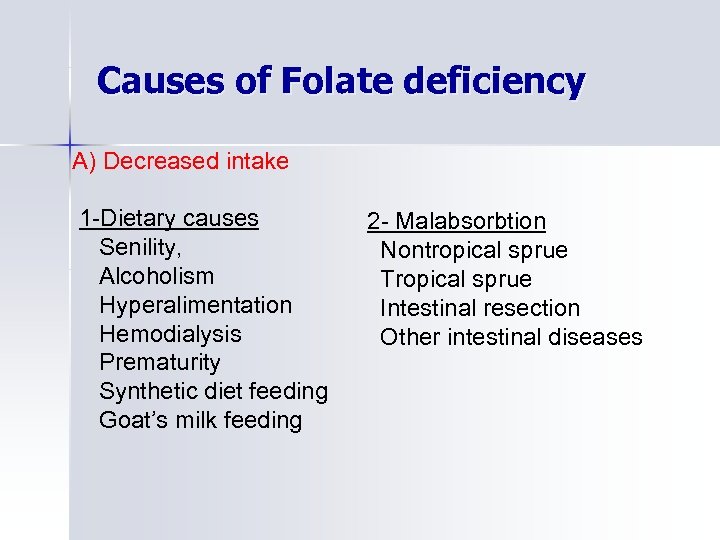
Causes of Folate deficiency A) Decreased intake 1 -Dietary causes Senility, Alcoholism Hyperalimentation Hemodialysis Prematurity Synthetic diet feeding Goat’s milk feeding 2 - Malabsorbtion Nontropical sprue Tropical sprue Intestinal resection Other intestinal diseases
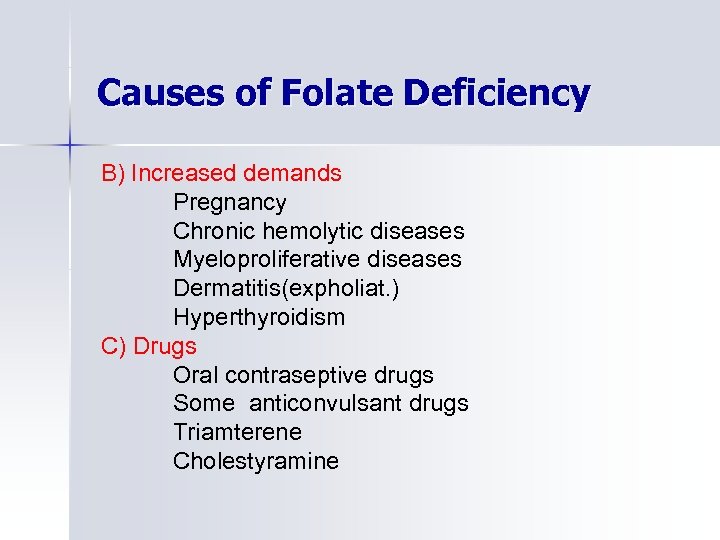
Causes of Folate Deficiency B) Increased demands Pregnancy Chronic hemolytic diseases Myeloproliferative diseases Dermatitis(expholiat. ) Hyperthyroidism C) Drugs Oral contraseptive drugs Some anticonvulsant drugs Triamterene Cholestyramine
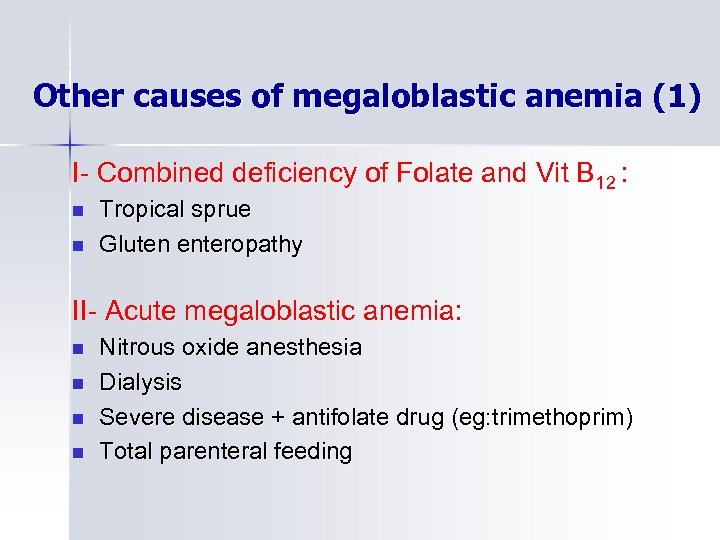
Other causes of megaloblastic anemia (1) I- Combined deficiency of Folate and Vit B 12 : n n Tropical sprue Gluten enteropathy II- Acute megaloblastic anemia: n n Nitrous oxide anesthesia Dialysis Severe disease + antifolate drug (eg: trimethoprim) Total parenteral feeding
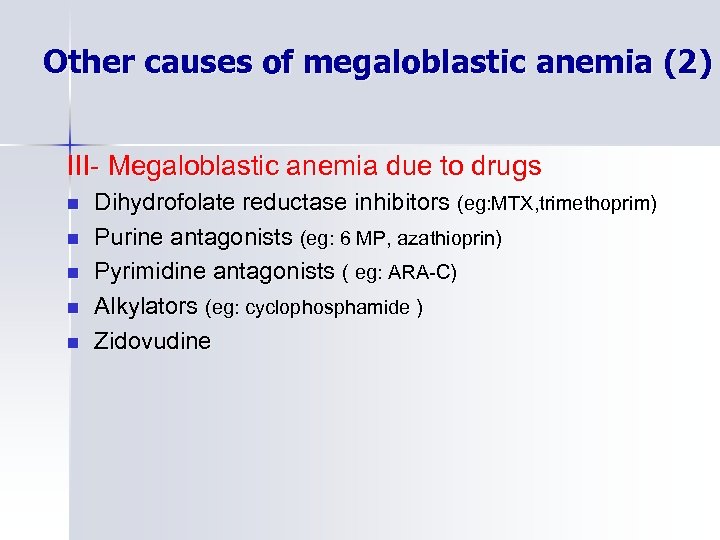
Other causes of megaloblastic anemia (2) III- Megaloblastic anemia due to drugs n n n Dihydrofolate reductase inhibitors (eg: MTX, trimethoprim) Purine antagonists (eg: 6 MP, azathioprin) Pyrimidine antagonists ( eg: ARA-C) Alkylators (eg: cyclophosphamide ) Zidovudine
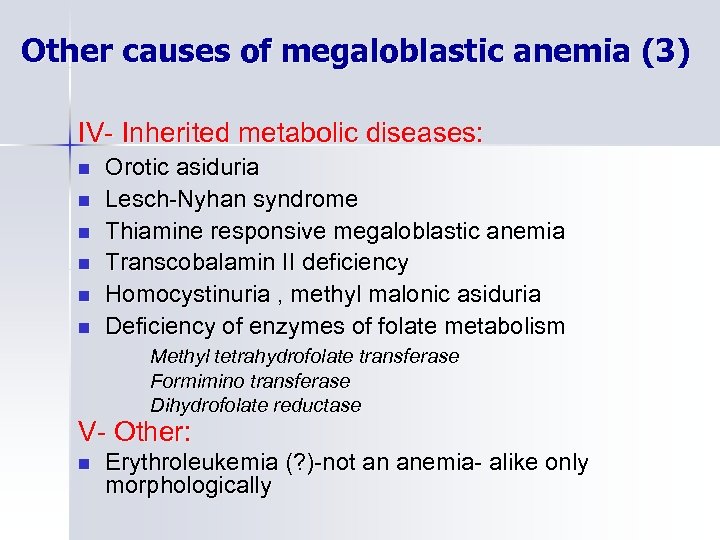
Other causes of megaloblastic anemia (3) IV- Inherited metabolic diseases: n n n Orotic asiduria Lesch-Nyhan syndrome Thiamine responsive megaloblastic anemia Transcobalamin II deficiency Homocystinuria , methyl malonic asiduria Deficiency of enzymes of folate metabolism Methyl tetrahydrofolate transferase Formimino transferase Dihydrofolate reductase V- Other: n Erythroleukemia (? )-not an anemia- alike only morphologically
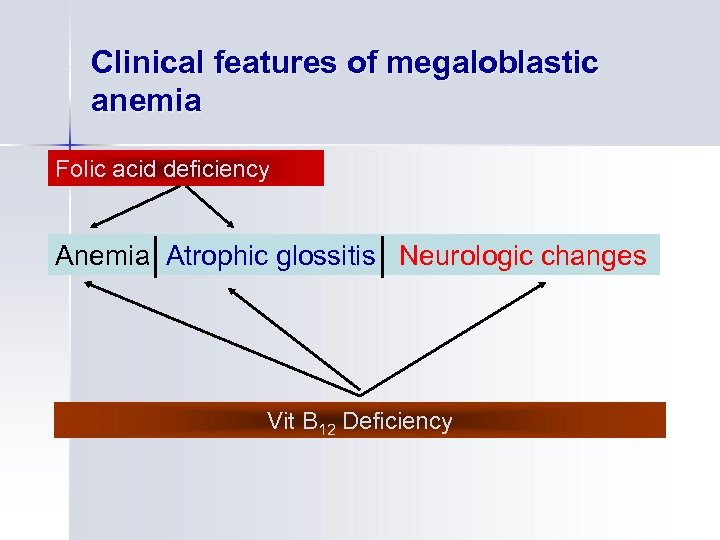
Clinical features of megaloblastic anemia Folic acid deficiency Anemia Atrophic glossitis Neurologic changes Vit B 12 Deficiency
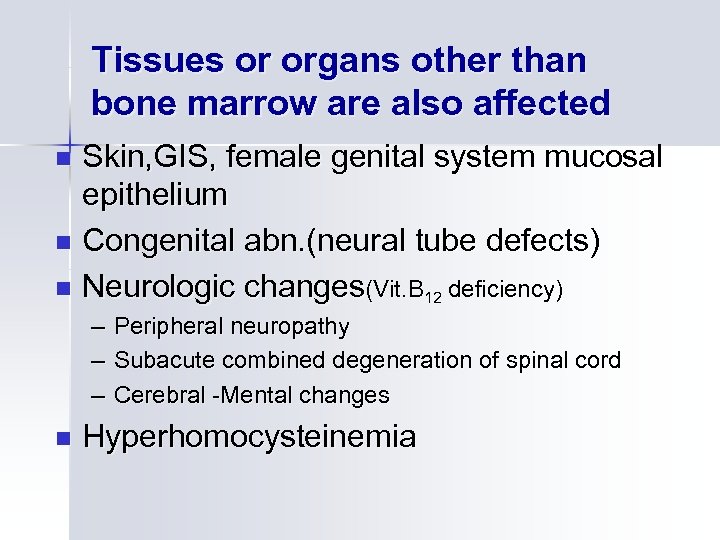
Tissues or organs other than bone marrow are also affected Skin, GIS, female genital system mucosal epithelium n Congenital abn. (neural tube defects) n Neurologic changes(Vit. B 12 deficiency) n – Peripheral neuropathy – Subacute combined degeneration of spinal cord – Cerebral -Mental changes n Hyperhomocysteinemia
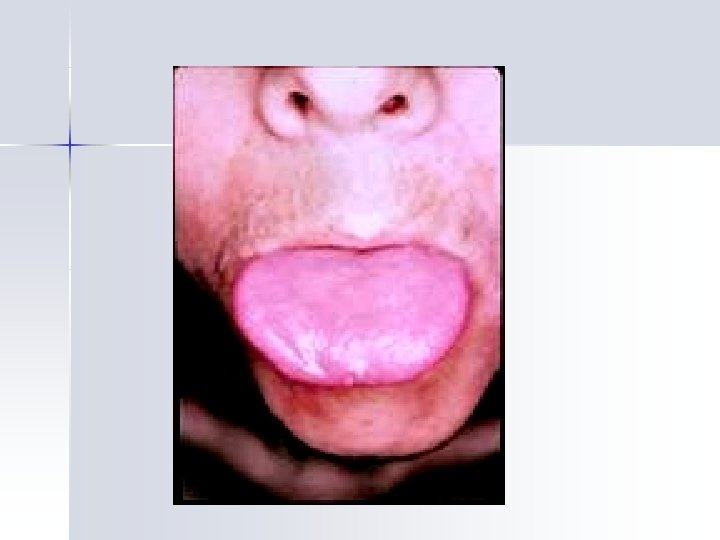
Clinical findings(1) n Anemia: Symptoms of anemia + palor+slight icterus n Glossitis : Sore tongue, poor taste sensation, pain Papill. atrophy-beefy tongue
Clinical findings(2) Neurologic changes-Vit B 12 deficiency (may occur without anemia) Paresthesias Loss of position sense, ataxia Decreased deep tendon reflexes Muscle weakness Loss of vibration sense ( post column ) Spasticity, reflex changes, Babinsky (lateral column ) Romberg Mental changes: Memory loss, confusion, dementia, n hallutination etc
Clinical findings(3) n Other signs: Vitiligo Hyperpigmentation Premature graying of hair Weight loss Fever Diarhea Constipation Meteorismus Splenomegaly
Peripheral blood CBC: Anemia Leukopenia Thrombocytopenia
RBC Indexes: MCV n MCH n RDW n
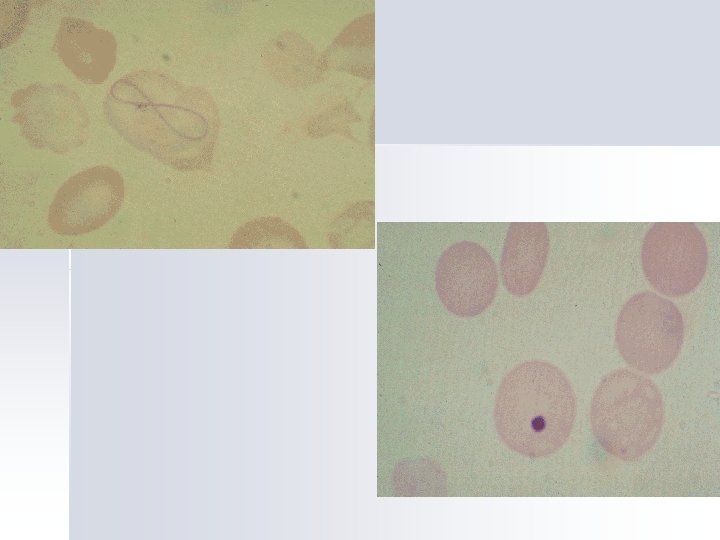
Peripheral smear(1) : RBC’s n n n Macroovalocytosis , Anisocytosis, poikilocytosis , Bazophilic stippling , Howell-Jolly bodies and Cabot ring, Nucleated red cells
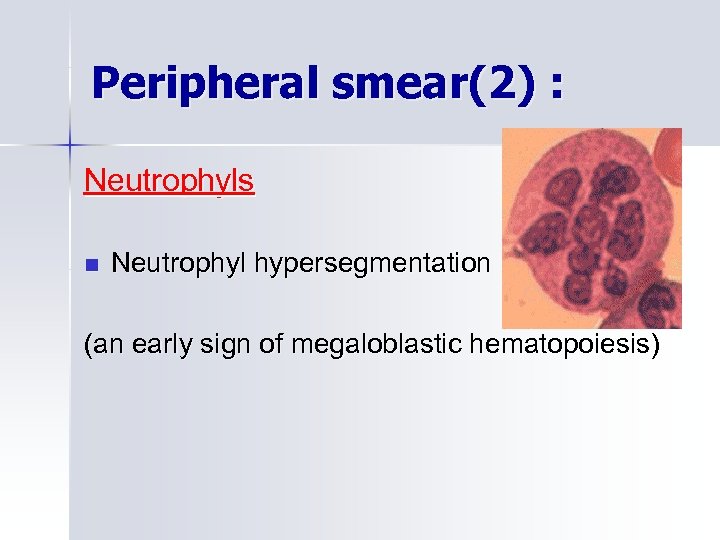
Peripheral smear(2) : Neutrophyls n Neutrophyl hypersegmentation (an early sign of megaloblastic hematopoiesis)
Bone marrow findings in megaloblastic anemia
Bone marrow Hypercellular with erythroid hyperplasia. Erythroid series n n Giant erythroblasts called megaloblasts Increased numbers of early erythroblasts Nuclear cytoplasmic asynchronism Increased mytosis
Bone marrow n Giant metamyelocytes and bands n Giant megakaryocytes n Increased bone marrow iron stores
Biochemical findings n n LDH ( LDH -1> LDH - 2) Bilirubin(indirect) Ferritin and serum iron Haptoglobin
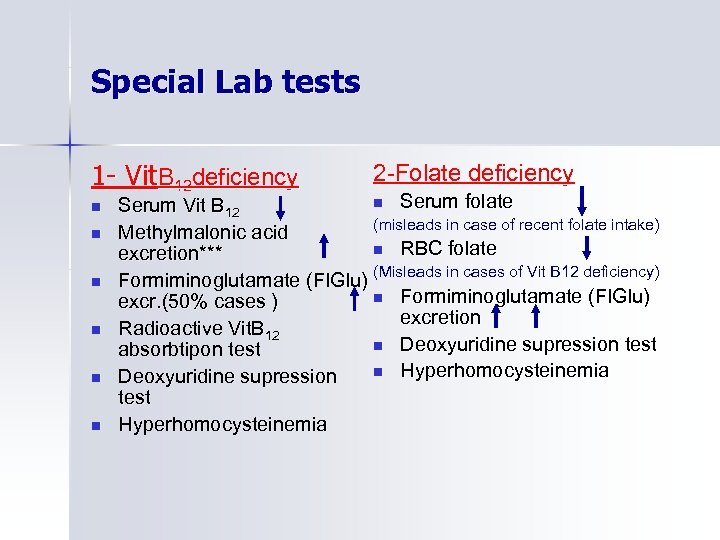
Special Lab tests 1 - Vit. B 12 deficiency n n n 2 -Folate deficiency n Serum folate Serum Vit B 12 (misleads in case of recent folate intake) Methylmalonic acid n RBC folate excretion*** Formiminoglutamate (FIGlu) (Misleads in cases of Vit B 12 deficiency) n Formiminoglutamate (FIGlu) excr. (50% cases ) excretion Radioactive Vit. B 12 n Deoxyuridine supression test absorbtipon test n Hyperhomocysteinemia Deoxyuridine supression test Hyperhomocysteinemia
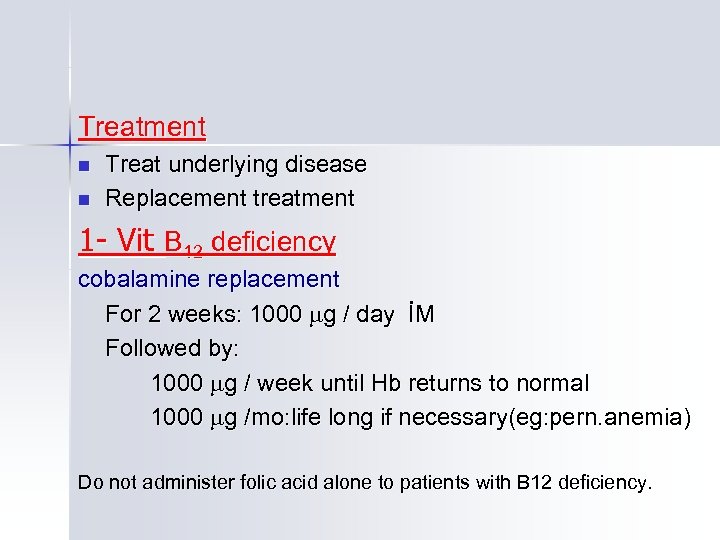
Treatment n n Treat underlying disease Replacement treatment 1 - Vit B 12 deficiency cobalamine replacement For 2 weeks: 1000 g / day İM Followed by: 1000 g / week until Hb returns to normal 1000 g /mo: life long if necessary(eg: pern. anemia) Do not administer folic acid alone to patients with B 12 deficiency.
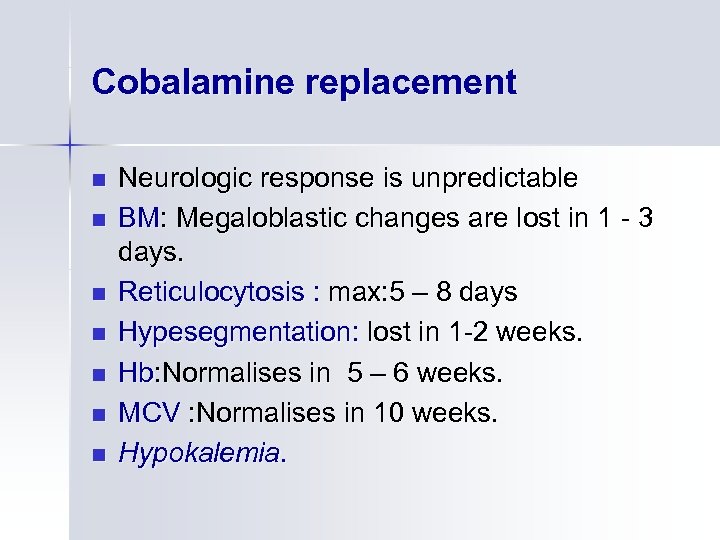
Cobalamine replacement n n n n Neurologic response is unpredictable BM: Megaloblastic changes are lost in 1 - 3 days. Reticulocytosis : max: 5 – 8 days Hypesegmentation: lost in 1 -2 weeks. Hb: Normalises in 5 – 6 weeks. MCV : Normalises in 10 weeks. Hypokalemia.
Treatment 2 - Folate deficiency n Treat underlying condition n Folic acid replacement: Dose : n Start with 1 mg / day ( 2 - 3 weeks ) n Continue with 0. 25 - 0. 50 mg / day n Pregnants: 1 mg / day
Pernicious Anemia ( Addison - Biermer ) Deficiency of intrinsic factor and n Megaloblastic anemia n Athrophic glossitis n Neurologic changes
Types of PA: Adult: Med: 60 years n Juvenile : 10 - 20 years n Congenital : < 2 years n
P. A. Pathogenesis: Adult type Atrophic gastritis: • Gastric (body)Corpus involved • All gastric secretions are decresed • Chief cells and parietal cells are lost and • intestinal metaplasia may occur. Congenital type Selective IF deficiency ( Autosomal res )
Pathogenesis of Gastritis in P. A. Heredity: n n P. A can be found in the relatives of the patients. Related to certain HLA antigens ; HLA-B 7, DW 2, DW 5, DR 2 Autoimmunity: n n Anti –parietal cell antibodies : 85 % Anti-IF antibodies : 55 - 70 % Anti-thyroid antibodies Other autoimmune diseases and cellular immunity
P. A. Lab In addition to typical blood findings of megaloblastic anemia; n Serum anti-IF antbd*** n Serum anti-PC antbd n Achilia , serum gastrin level increase n Gastroscopy and biopsy: atrophic gastitis*** n Schilling’s test
P. A. Treatment n Life long n Cobalamine replacement. Complication n Gastric Ca: 2 times normal population
16f4096005ed22df6b41c57857da8175.ppt