a1755ad80e281181570a9f15e9ae4ca7.ppt
- Количество слайдов: 77
 Medicines Adherence Support Service Pilot Project Community Pharmacist Training
Medicines Adherence Support Service Pilot Project Community Pharmacist Training
 Dr Susan Patterson, Pharmacy & Medicines Management Adviser, HSCB Jo Gribben, Pilot Lead, SE Trust Caroline Johnston, Pilot Lead, Northern Trust
Dr Susan Patterson, Pharmacy & Medicines Management Adviser, HSCB Jo Gribben, Pilot Lead, SE Trust Caroline Johnston, Pilot Lead, Northern Trust
 What problems do older people have with medicines? “Transforming Your Care”: more older people will be managed at home 36% of over-65 s take 4 or more medicines for prevention of chronic disease 10% (approx) hospital admissions are due to medication-related problems 50% of people do not adhere to prescribed medication The only medicine that works is the one that the person takes
What problems do older people have with medicines? “Transforming Your Care”: more older people will be managed at home 36% of over-65 s take 4 or more medicines for prevention of chronic disease 10% (approx) hospital admissions are due to medication-related problems 50% of people do not adhere to prescribed medication The only medicine that works is the one that the person takes
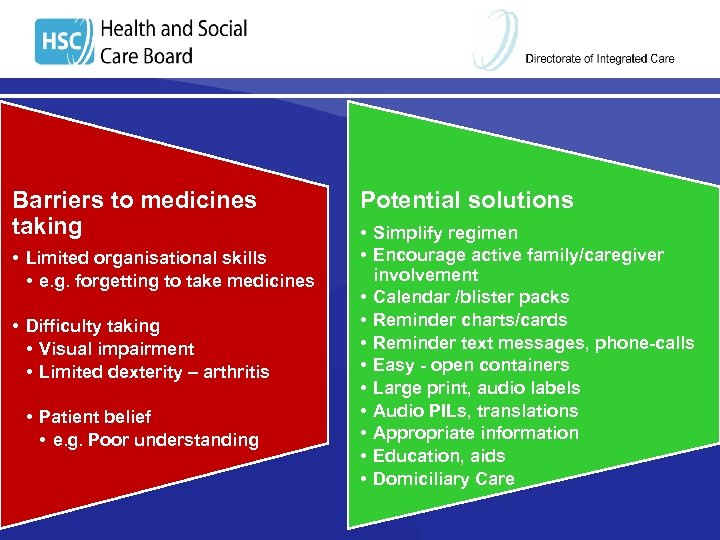 Barriers to medicines taking • Limited organisational skills • e. g. forgetting to take medicines • Difficulty taking • Visual impairment • Limited dexterity – arthritis • Patient belief • e. g. Poor understanding Potential solutions • Simplify regimen • Encourage active family/caregiver involvement • Calendar /blister packs • Reminder charts/cards • Reminder text messages, phone-calls • Easy - open containers • Large print, audio labels • Audio PILs, translations • Appropriate information • Education, aids • Domiciliary Care
Barriers to medicines taking • Limited organisational skills • e. g. forgetting to take medicines • Difficulty taking • Visual impairment • Limited dexterity – arthritis • Patient belief • e. g. Poor understanding Potential solutions • Simplify regimen • Encourage active family/caregiver involvement • Calendar /blister packs • Reminder charts/cards • Reminder text messages, phone-calls • Easy - open containers • Large print, audio labels • Audio PILs, translations • Appropriate information • Education, aids • Domiciliary Care
 SOUTH EASTERN TRUST VERONICA CLELAND RESIDENTIAL, DAY CARE AND DOMICILIARY CARE MANAGER
SOUTH EASTERN TRUST VERONICA CLELAND RESIDENTIAL, DAY CARE AND DOMICILIARY CARE MANAGER
 The Challenges • Increasing older population • By 2019 the population of older people between 65 and 84 is projected to grow by 32% • The population of 85 and over is projected by 2019 to rise by 45%
The Challenges • Increasing older population • By 2019 the population of older people between 65 and 84 is projected to grow by 32% • The population of 85 and over is projected by 2019 to rise by 45%
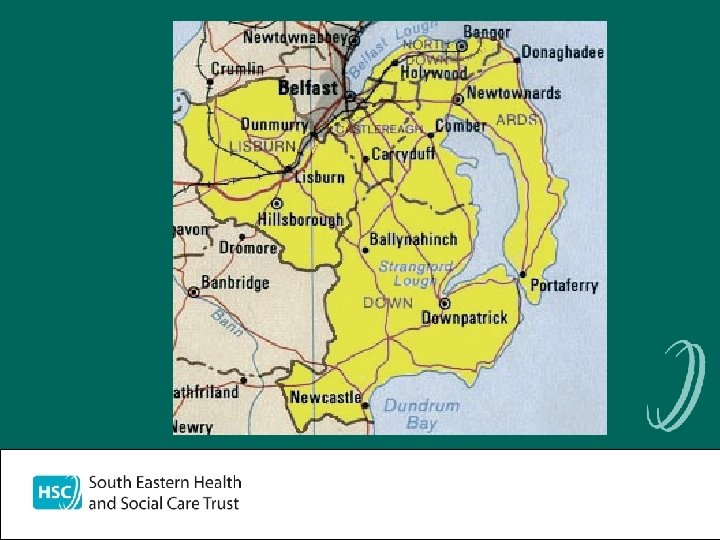
 • Four Localities within South Eastern Health & Social Care Trust: – North Down – Ards – Down – Lisburn • Localities are divided into geographical patches and staff work in GP aligned Integrated Primary Care Teams.
• Four Localities within South Eastern Health & Social Care Trust: – North Down – Ards – Down – Lisburn • Localities are divided into geographical patches and staff work in GP aligned Integrated Primary Care Teams.
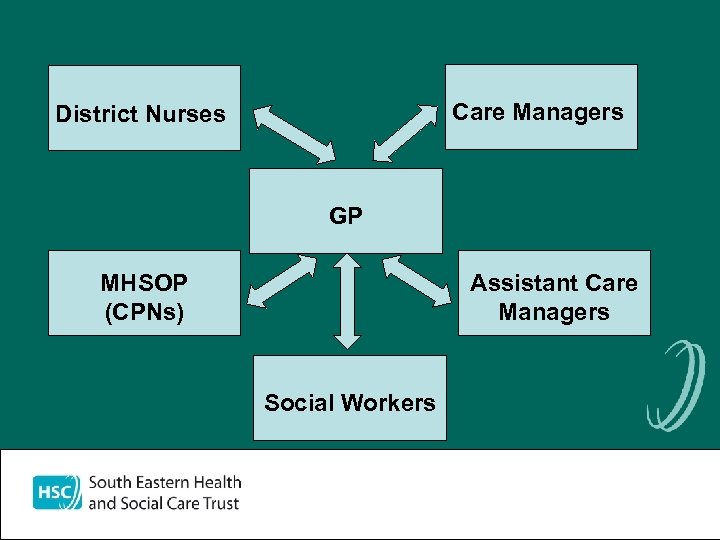 Care Managers District Nurses GP MHSOP (CPNs) Assistant Care Managers Social Workers
Care Managers District Nurses GP MHSOP (CPNs) Assistant Care Managers Social Workers
 Open Referral System into Local Office • Referrals allocated to appropriate Service – Signposted out to Community / Voluntary sector – Reablement – Care Manager / Assistant Care Manager Integrated teams • The majority of Service users should be referred to Reablement unless they have no Reablement potential
Open Referral System into Local Office • Referrals allocated to appropriate Service – Signposted out to Community / Voluntary sector – Reablement – Care Manager / Assistant Care Manager Integrated teams • The majority of Service users should be referred to Reablement unless they have no Reablement potential
 Reablement • Reablement – focuses on the client’s strengths and abilities to help them regain their independence, re-learning daily living skills or gaining new ones. Packages of care focused on the short term with the client moving to other forms of Care Providers if further support is still required.
Reablement • Reablement – focuses on the client’s strengths and abilities to help them regain their independence, re-learning daily living skills or gaining new ones. Packages of care focused on the short term with the client moving to other forms of Care Providers if further support is still required.
 Care Management • Care Management Is a concept which embraces the key functions of: case finding, care screening, undertaking proportionate, person-centred assessment of an individual’s needs, determining eligibility for service(s); developing a care plan and implementing a care package; monitoring and reassessing need and adjusting the care package as required. Source: DHSS&PS Circular HSC (ECCU) 1/2010 March 2010
Care Management • Care Management Is a concept which embraces the key functions of: case finding, care screening, undertaking proportionate, person-centred assessment of an individual’s needs, determining eligibility for service(s); developing a care plan and implementing a care package; monitoring and reassessing need and adjusting the care package as required. Source: DHSS&PS Circular HSC (ECCU) 1/2010 March 2010
 Assessment • A person-centred process whereby the needs of an individual are identified and their impact on daily living and quality of life is evaluated, undertaken with the individual, his/her carers with the individual, his/her carer and relevant professionals. Source: DHSS&PS Circular HSC (ECCU) 1/2010 March 2010 • Service users assessed Using - NISAT – (Northern Ireland Single Assessment Tool)
Assessment • A person-centred process whereby the needs of an individual are identified and their impact on daily living and quality of life is evaluated, undertaken with the individual, his/her carers with the individual, his/her carer and relevant professionals. Source: DHSS&PS Circular HSC (ECCU) 1/2010 March 2010 • Service users assessed Using - NISAT – (Northern Ireland Single Assessment Tool)
 Care Plan • A description of what an individual needs will be met. Source: DHSS&PS Circular HSC (ECCU)1/2010 March 2010
Care Plan • A description of what an individual needs will be met. Source: DHSS&PS Circular HSC (ECCU)1/2010 March 2010
 Care Package • A combination of services designed to meet a person’s assessed needs Source: DHSS&PS Circular HSC (ECCU)1/2010 March 2010
Care Package • A combination of services designed to meet a person’s assessed needs Source: DHSS&PS Circular HSC (ECCU)1/2010 March 2010
 Domiciliary Care • The mechanism for the delivery of domiciliary care is outlined by DHSSPS (2003) and states that people should be helped to live independent lives with safety and dignity in their own homes.
Domiciliary Care • The mechanism for the delivery of domiciliary care is outlined by DHSSPS (2003) and states that people should be helped to live independent lives with safety and dignity in their own homes.
 • All agencies providing Domiciliary Care must be registered with RQIA and operate in accordance with regulation. The Health and Personal Social Services (Quality, Improvement and Regulation) (Northern Ireland) Order 2003 (the Order). • Article 38 of the Order confers powers on DHSSPS to prepare, publish and review statements of minimum standards applicable to all services including regulated services. • Domiciliary Care Agencies Minimum Standards updated August 2011 http: //www. rqia. org. uk/cms_resources/domiciliary_care_standards-%20 Aug%2011. pdf
• All agencies providing Domiciliary Care must be registered with RQIA and operate in accordance with regulation. The Health and Personal Social Services (Quality, Improvement and Regulation) (Northern Ireland) Order 2003 (the Order). • Article 38 of the Order confers powers on DHSSPS to prepare, publish and review statements of minimum standards applicable to all services including regulated services. • Domiciliary Care Agencies Minimum Standards updated August 2011 http: //www. rqia. org. uk/cms_resources/domiciliary_care_standards-%20 Aug%2011. pdf
 Care Providers • NISRA figures survey week in Sept 2013 • 4715 service users received domiciliary care services in the SETIn SET • 15 / 85% split in care provision • http: //www. dhsspsni. gov. uk/domiciliary_care_services_for_adults_in_northern_ireland_20132. pdf
Care Providers • NISRA figures survey week in Sept 2013 • 4715 service users received domiciliary care services in the SETIn SET • 15 / 85% split in care provision • http: //www. dhsspsni. gov. uk/domiciliary_care_services_for_adults_in_northern_ireland_20132. pdf
 Management of Medicines • Standard 7: • The agency has arrangements in place to ensure that care workers manage medicines safely and securely. • http: //www. rqia. org. uk/cms_resources/domiciliary_care_standards%20 Aug%2011. pdf • Requires that staff are both trained and competent to administer medications.
Management of Medicines • Standard 7: • The agency has arrangements in place to ensure that care workers manage medicines safely and securely. • http: //www. rqia. org. uk/cms_resources/domiciliary_care_standards%20 Aug%2011. pdf • Requires that staff are both trained and competent to administer medications.
 Issues • Receiving current up to date lists of medication at referral • Updating medication lists/ new prescriptions / transcribing whose responsibility? ? • Multiple forms of medication administration and competency of staff. • Withdrawal of MDS • Environmental issues • Relatives and informal carer’s giving medication along with formal carer’s • Dual medications in homes (Husband & Wife) • 2 or more providers
Issues • Receiving current up to date lists of medication at referral • Updating medication lists/ new prescriptions / transcribing whose responsibility? ? • Multiple forms of medication administration and competency of staff. • Withdrawal of MDS • Environmental issues • Relatives and informal carer’s giving medication along with formal carer’s • Dual medications in homes (Husband & Wife) • 2 or more providers
 Currently in SEHSCT • Domiciliary care workers in the statutory sector are not trained to administer medications, can prompt / remind / assist under direction of the service users • Need to address issues of transcribing / updating MAR • Safety of service users and protection of staff is paramount.
Currently in SEHSCT • Domiciliary care workers in the statutory sector are not trained to administer medications, can prompt / remind / assist under direction of the service users • Need to address issues of transcribing / updating MAR • Safety of service users and protection of staff is paramount.
 At present we are rolling out a programme of training for the topical administration of medications Approx 526 domiciliary care staff require training Training and on-going competency of staff RQIA mandatory standard – 3 yearly On- going work from Regional perspective,
At present we are rolling out a programme of training for the topical administration of medications Approx 526 domiciliary care staff require training Training and on-going competency of staff RQIA mandatory standard – 3 yearly On- going work from Regional perspective,
 Any Questions?
Any Questions?
 Medicines Adherence Support Service Aim: To improve outcomes from prescribed medicines by ensuring safety and quality in provision of adherence support for older people who are living in their own homes
Medicines Adherence Support Service Aim: To improve outcomes from prescribed medicines by ensuring safety and quality in provision of adherence support for older people who are living in their own homes
 NICE CG 76 (2009): Supporting Adherence Assess adherence • • provide further information on medicines discuss with patient • • Intentional? Discuss beliefs / concerns Non-intentional? Address practical problems if there is a specific need consider case by case address concerns and needs of the individual
NICE CG 76 (2009): Supporting Adherence Assess adherence • • provide further information on medicines discuss with patient • • Intentional? Discuss beliefs / concerns Non-intentional? Address practical problems if there is a specific need consider case by case address concerns and needs of the individual
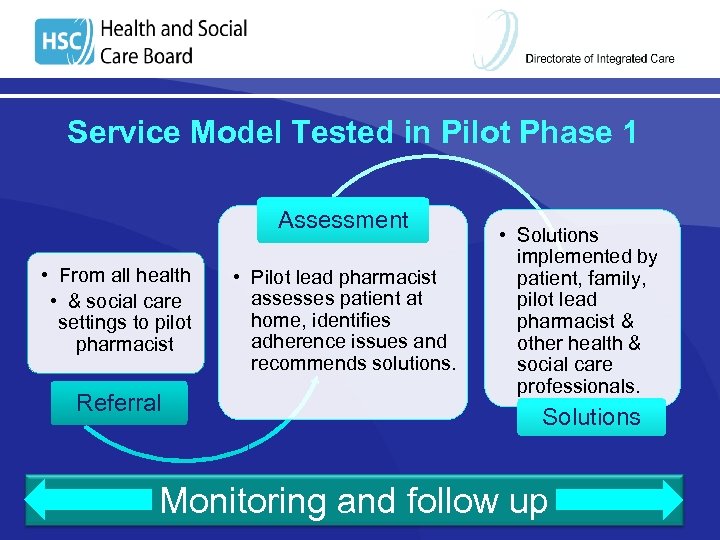 Service Model Tested in Pilot Phase 1 Assessment • From all health • & social care settings to pilot pharmacist Referral • Pilot lead pharmacist assesses patient at home, identifies adherence issues and recommends solutions. • Solutions implemented by patient, family, pilot lead pharmacist & other health & social care professionals. Solutions Monitoring and follow up
Service Model Tested in Pilot Phase 1 Assessment • From all health • & social care settings to pilot pharmacist Referral • Pilot lead pharmacist assesses patient at home, identifies adherence issues and recommends solutions. • Solutions implemented by patient, family, pilot lead pharmacist & other health & social care professionals. Solutions Monitoring and follow up
 Referral Criteria q q q Aged ≥ 65 years old On four or more regular medications Living at home Attending pilot GP + community pharmacist Suspected/actual adherence issue
Referral Criteria q q q Aged ≥ 65 years old On four or more regular medications Living at home Attending pilot GP + community pharmacist Suspected/actual adherence issue
 Phase 1 Locations Northern Trust: • Ballyclare & Ballymoney South Eastern Trust: • Hillsborough & Lisburn Total – 8 GP Practices, 22 Pharmacies
Phase 1 Locations Northern Trust: • Ballyclare & Ballymoney South Eastern Trust: • Hillsborough & Lisburn Total – 8 GP Practices, 22 Pharmacies
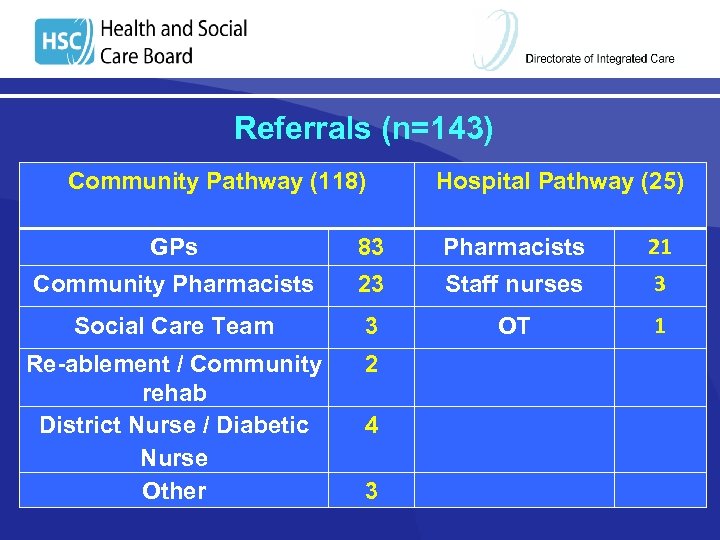 Referrals (n=143) Community Pathway (118) Hospital Pathway (25) GPs 83 Pharmacists 21 Community Pharmacists 23 Staff nurses 3 Social Care Team 3 OT 1 Re-ablement / Community rehab District Nurse / Diabetic Nurse Other 2 4 3
Referrals (n=143) Community Pathway (118) Hospital Pathway (25) GPs 83 Pharmacists 21 Community Pharmacists 23 Staff nurses 3 Social Care Team 3 OT 1 Re-ablement / Community rehab District Nurse / Diabetic Nurse Other 2 4 3
 Reasons for Referral Ø Ø Ø Problems removing tablets from packaging Confusion / confused about medications Problems with ordering/collecting medications Recent hospital discharge Not taking medication as prescribed Requesting Monitored Dosage System (MDS)
Reasons for Referral Ø Ø Ø Problems removing tablets from packaging Confusion / confused about medications Problems with ordering/collecting medications Recent hospital discharge Not taking medication as prescribed Requesting Monitored Dosage System (MDS)
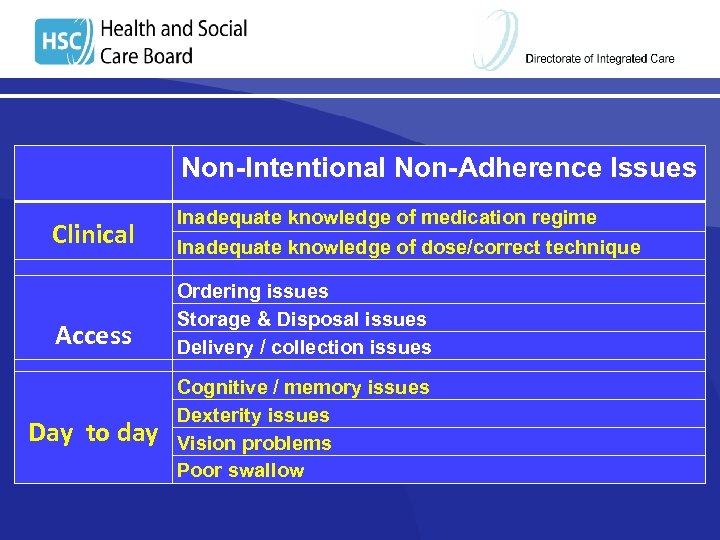 Non-Intentional Non-Adherence Issues Clinical Inadequate knowledge of medication regime Inadequate knowledge of dose/correct technique Access Ordering issues Storage & Disposal issues Delivery / collection issues Day to day Cognitive / memory issues Dexterity issues Vision problems Poor swallow
Non-Intentional Non-Adherence Issues Clinical Inadequate knowledge of medication regime Inadequate knowledge of dose/correct technique Access Ordering issues Storage & Disposal issues Delivery / collection issues Day to day Cognitive / memory issues Dexterity issues Vision problems Poor swallow
 Solutions Implemented Resolution of clinical query Medication List Education (specific) Disposal of medication Sign post /referral to other teams Synchronisation of prescriptions Ordering solutions Altering medication timings Provision of a device New / altered care package
Solutions Implemented Resolution of clinical query Medication List Education (specific) Disposal of medication Sign post /referral to other teams Synchronisation of prescriptions Ordering solutions Altering medication timings Provision of a device New / altered care package
 Phase 2
Phase 2
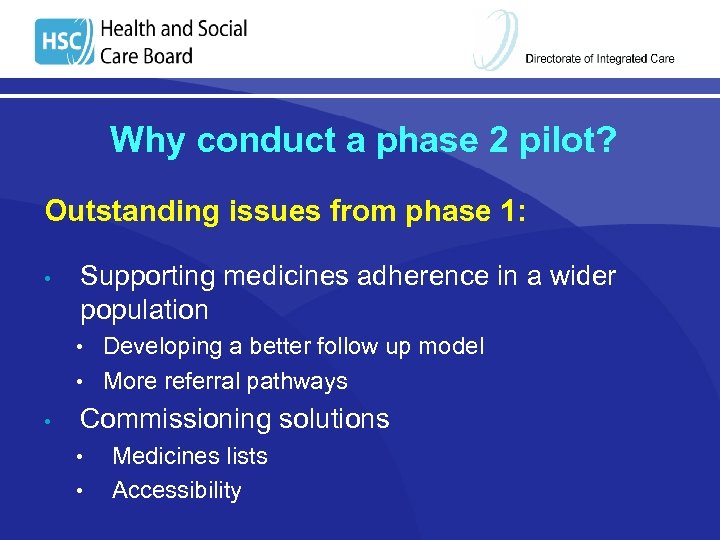 Why conduct a phase 2 pilot? Outstanding issues from phase 1: • Supporting medicines adherence in a wider population • Developing a better follow up model • More referral pathways • Commissioning solutions • • Medicines lists Accessibility
Why conduct a phase 2 pilot? Outstanding issues from phase 1: • Supporting medicines adherence in a wider population • Developing a better follow up model • More referral pathways • Commissioning solutions • • Medicines lists Accessibility
 “Making it Better through Pharmacy in the Community” DHSSPS 2014 Ø Ø Helping people gain better outcomes from medicines Helping people live longer, healthier lives Helping people safely avail of care closer to home Helping people to benefit from advances in treatment and technology
“Making it Better through Pharmacy in the Community” DHSSPS 2014 Ø Ø Helping people gain better outcomes from medicines Helping people live longer, healthier lives Helping people safely avail of care closer to home Helping people to benefit from advances in treatment and technology
 Phase 2 - Locations Integrated Care Partnership Areas South Eastern Trust - Lisburn Northern Trust – East Antrim
Phase 2 - Locations Integrated Care Partnership Areas South Eastern Trust - Lisburn Northern Trust – East Antrim
 Community Pharmacy Pathway § Attend training! § Service Specification & Guidance § Sign contract (HSCB) § Obtain items on stock list § Complete & submit stock claim form (+ receipts) § Organise pharmacy – staff / premises
Community Pharmacy Pathway § Attend training! § Service Specification & Guidance § Sign contract (HSCB) § Obtain items on stock list § Complete & submit stock claim form (+ receipts) § Organise pharmacy – staff / premises
 Stock List
Stock List
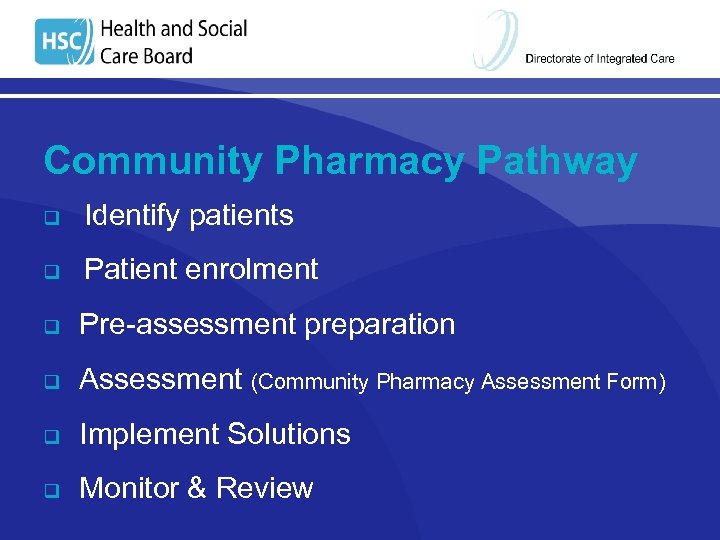 Community Pharmacy Pathway q Identify patients q Patient enrolment q Pre-assessment preparation q Assessment (Community Pharmacy Assessment Form) q Implement Solutions q Monitor & Review
Community Pharmacy Pathway q Identify patients q Patient enrolment q Pre-assessment preparation q Assessment (Community Pharmacy Assessment Form) q Implement Solutions q Monitor & Review
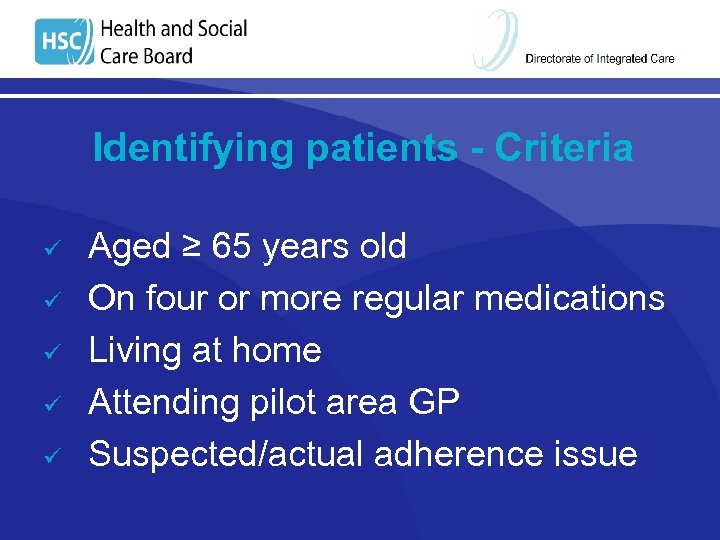 Identifying patients - Criteria ü ü ü Aged ≥ 65 years old On four or more regular medications Living at home Attending pilot area GP Suspected/actual adherence issue
Identifying patients - Criteria ü ü ü Aged ≥ 65 years old On four or more regular medications Living at home Attending pilot area GP Suspected/actual adherence issue
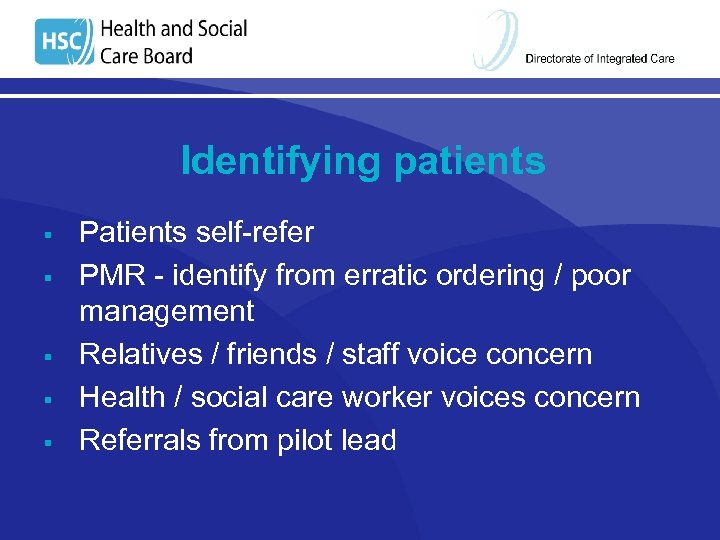 Identifying patients Patients self-refer PMR - identify from erratic ordering / poor management Relatives / friends / staff voice concern Health / social care worker voices concern Referrals from pilot lead § § §
Identifying patients Patients self-refer PMR - identify from erratic ordering / poor management Relatives / friends / staff voice concern Health / social care worker voices concern Referrals from pilot lead § § §
 Patient Enrolment § Information leaflet § Consent form § Arrange appointment Ø In pharmacy or domiciliary visit Ø Family / carer present if appropriate Ø Patient to bring all medicines & compliance aids
Patient Enrolment § Information leaflet § Consent form § Arrange appointment Ø In pharmacy or domiciliary visit Ø Family / carer present if appropriate Ø Patient to bring all medicines & compliance aids
 Patient Information Leaflet
Patient Information Leaflet
 Consent Form
Consent Form
 Community Pharmacy Assessment Form § § § Pre-assessment information (medication) Confirm medicines Assessment of adherence Current support arrangements Issues identified solutions Monitoring & follow-up
Community Pharmacy Assessment Form § § § Pre-assessment information (medication) Confirm medicines Assessment of adherence Current support arrangements Issues identified solutions Monitoring & follow-up
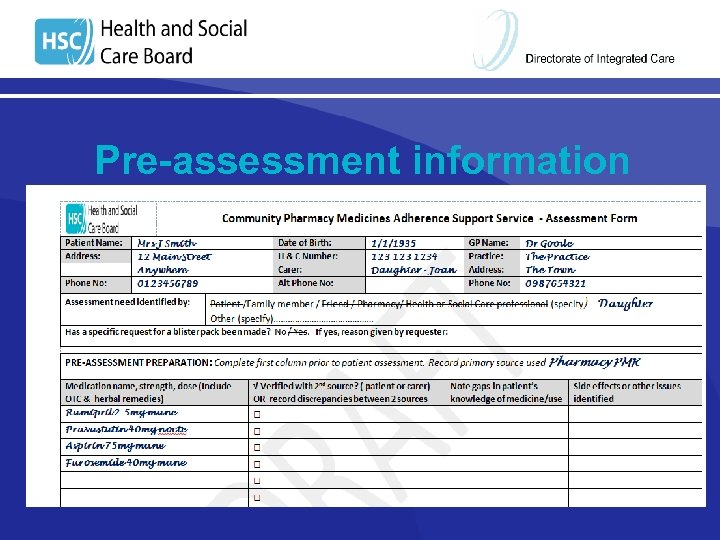
 Pre-assessment information Obtain an accurate list of patient’s medication • GP record • Pharmacy PMR • Recent hospital discharge letter Complete demographic information
Pre-assessment information Obtain an accurate list of patient’s medication • GP record • Pharmacy PMR • Recent hospital discharge letter Complete demographic information
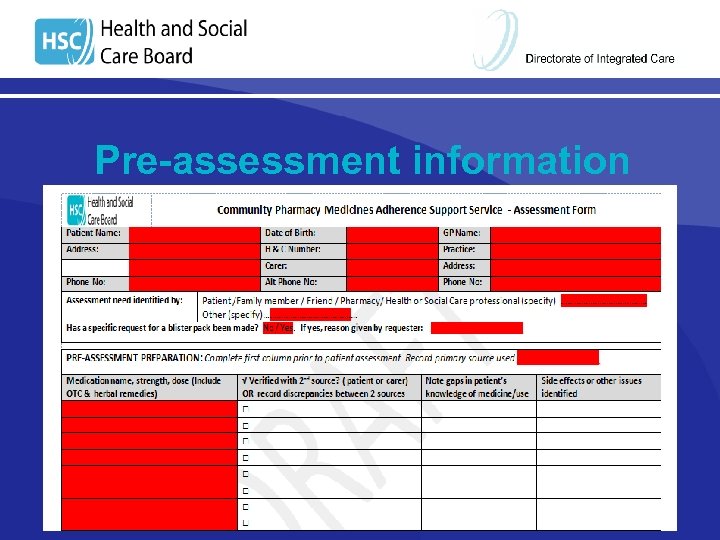 Pre-assessment information
Pre-assessment information
 Assessment (1) § Verify medication list with patient/carer § Reasons for discrepancies (intentional ? ) § Assess patient’s knowledge § Identify side effects / other issues
Assessment (1) § Verify medication list with patient/carer § Reasons for discrepancies (intentional ? ) § Assess patient’s knowledge § Identify side effects / other issues
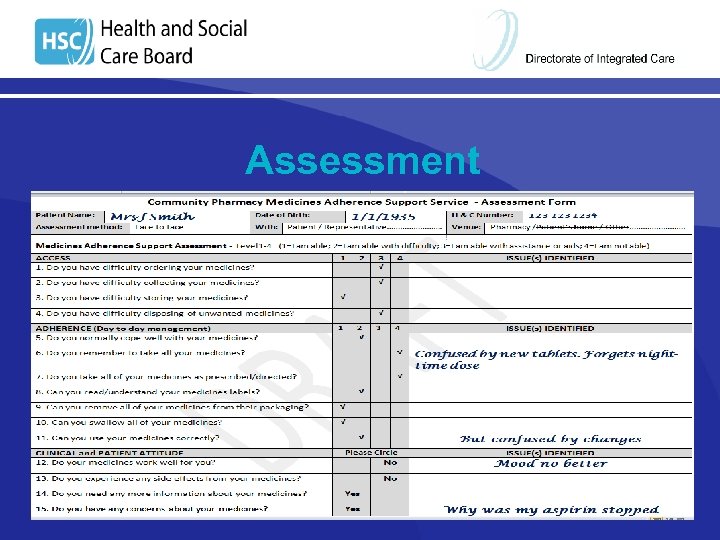
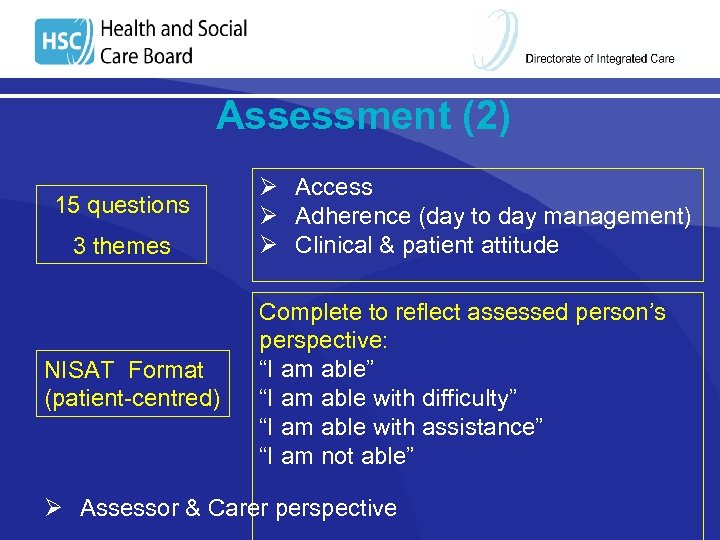 Assessment (2) 15 questions 3 themes NISAT Format (patient-centred) Ø Access Ø Adherence (day to day management) Ø Clinical & patient attitude Complete to reflect assessed person’s perspective: “I am able” “I am able with difficulty” “I am able with assistance” “I am not able” Ø Assessor & Carer perspective
Assessment (2) 15 questions 3 themes NISAT Format (patient-centred) Ø Access Ø Adherence (day to day management) Ø Clinical & patient attitude Complete to reflect assessed person’s perspective: “I am able” “I am able with difficulty” “I am able with assistance” “I am not able” Ø Assessor & Carer perspective
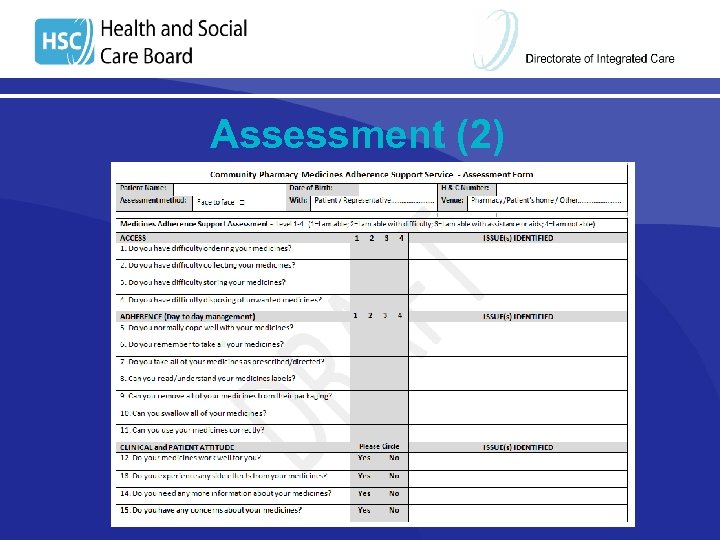 Assessment (2)
Assessment (2)
 Assessment (3) • • • Current arrangements Summary of Issues identified Possible solutions, consider with patient Solution Grid
Assessment (3) • • • Current arrangements Summary of Issues identified Possible solutions, consider with patient Solution Grid
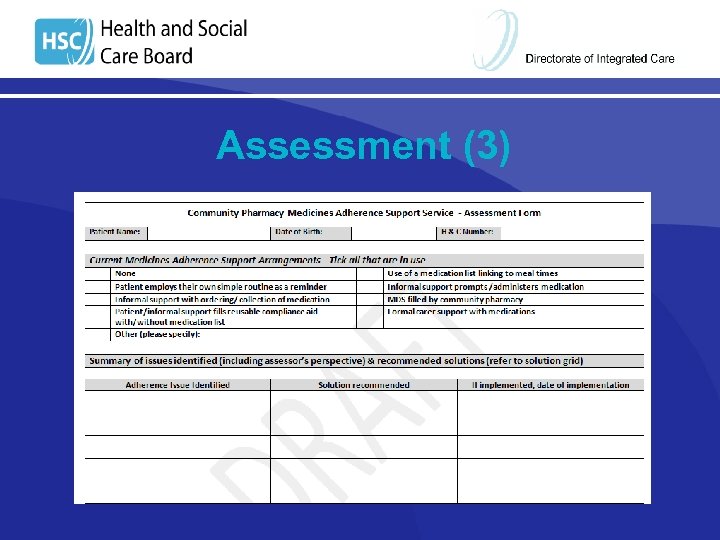 Assessment (3)
Assessment (3)
 Implement Solutions § Education § Advice on storage § Disposal of medications § Synchronisation § Family involvement
Implement Solutions § Education § Advice on storage § Disposal of medications § Synchronisation § Family involvement
 Stock Solutions - Complete stock solution claim form Pill popper Pill splitter Haleraid® / Turbogrip® Eye drop applicator Re-usable compliance aids (range of sizes)
Stock Solutions - Complete stock solution claim form Pill popper Pill splitter Haleraid® / Turbogrip® Eye drop applicator Re-usable compliance aids (range of sizes)
 Personalised (List-based solutions) • • Monthly Claim Form Medicines Reminder Card/list Medicine Administration Record (MAR Chart) * NB for patient/family/informal carer use only • § Monitored Dosage System MUST confirm accuracy of list
Personalised (List-based solutions) • • Monthly Claim Form Medicines Reminder Card/list Medicine Administration Record (MAR Chart) * NB for patient/family/informal carer use only • § Monitored Dosage System MUST confirm accuracy of list
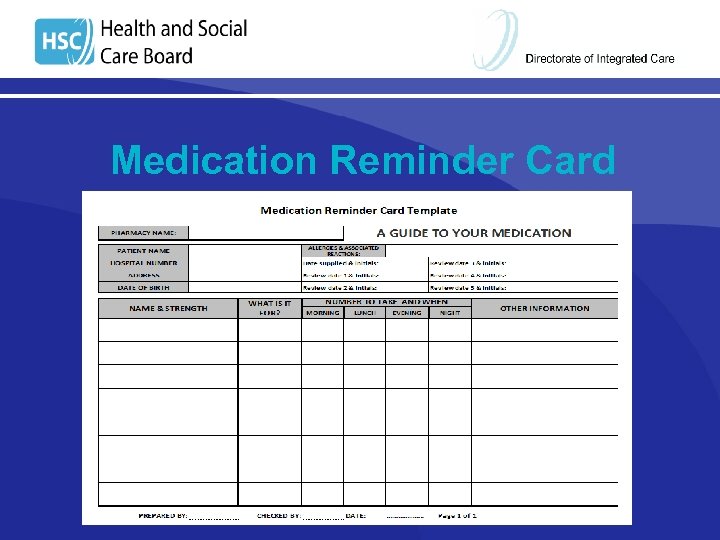 Medication Reminder Card
Medication Reminder Card
 Medication Reminder Card/List Ø Ensure patient / informal carer can use Ø Check monthly, against prescriptions Ø Manage changes Monthly Interim
Medication Reminder Card/List Ø Ensure patient / informal carer can use Ø Check monthly, against prescriptions Ø Manage changes Monthly Interim
 Medicine Administration Record Ø Ø Ø For patient / informal carer use only Assess if suitable for patient Record of medications taken / given Issued monthly against prescriptions Manage changes - New chart Supplementary Chart
Medicine Administration Record Ø Ø Ø For patient / informal carer use only Assess if suitable for patient Record of medications taken / given Issued monthly against prescriptions Manage changes - New chart Supplementary Chart
 Monitored Dosage System Ø Ø Ø Ø Ensure patient can use Check stability of medications (Guidance) Issue weekly against monthly scripts Inform GP - record can be annotated Arrangements for medications not in MDS Procedure for changes Remove old medications from house PSNI standards - Consultation
Monitored Dosage System Ø Ø Ø Ø Ensure patient can use Check stability of medications (Guidance) Issue weekly against monthly scripts Inform GP - record can be annotated Arrangements for medications not in MDS Procedure for changes Remove old medications from house PSNI standards - Consultation
 Information/referral to other HCPs GP- send summary if relevant • Clinical teams (if known) • Social Care • Pilot lead Telephone / written information • Must make it clear if action needed, and by whom
Information/referral to other HCPs GP- send summary if relevant • Clinical teams (if known) • Social Care • Pilot lead Telephone / written information • Must make it clear if action needed, and by whom
 Referral to other HCPs
Referral to other HCPs
 Monitor and Review § Follow-up - Approximately 1 month & 3 months post –assessment (page 4) § Changes to circumstances § Solutions still working / appropriate? § Document actions / referrals / changes § Forward completed form to pilot lead
Monitor and Review § Follow-up - Approximately 1 month & 3 months post –assessment (page 4) § Changes to circumstances § Solutions still working / appropriate? § Document actions / referrals / changes § Forward completed form to pilot lead
 Monitor and Review
Monitor and Review
 Payment model
Payment model
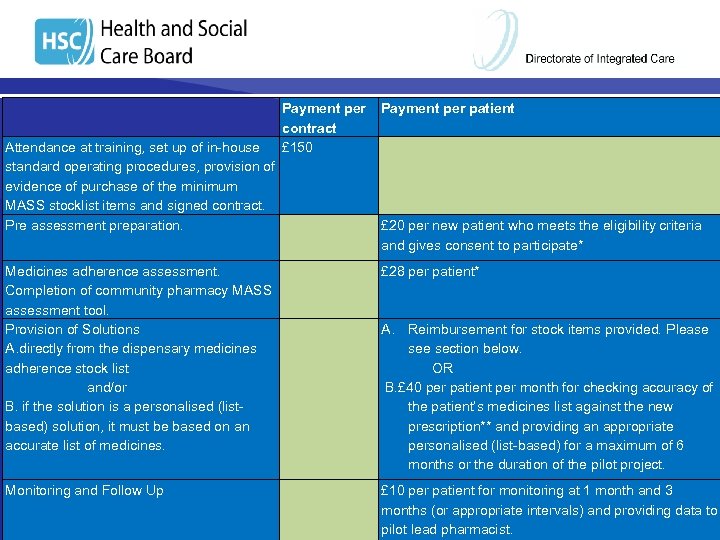 Payment per patient contract £ 150 Attendance at training, set up of in-house standard operating procedures, provision of evidence of purchase of the minimum MASS stocklist items and signed contract. Pre assessment preparation. £ 20 per new patient who meets the eligibility criteria and gives consent to participate* Medicines adherence assessment. Completion of community pharmacy MASS assessment tool. Provision of Solutions A. directly from the dispensary medicines adherence stock list and/or B. if the solution is a personalised (listbased) solution, it must be based on an accurate list of medicines. £ 28 per patient* Monitoring and Follow Up £ 10 per patient for monitoring at 1 month and 3 months (or appropriate intervals) and providing data to pilot lead pharmacist. Payment model A. Reimbursement for stock items provided. Please section below. OR B. £ 40 per patient per month for checking accuracy of the patient’s medicines list against the new prescription** and providing an appropriate personalised (list-based) for a maximum of 6 months or the duration of the pilot project.
Payment per patient contract £ 150 Attendance at training, set up of in-house standard operating procedures, provision of evidence of purchase of the minimum MASS stocklist items and signed contract. Pre assessment preparation. £ 20 per new patient who meets the eligibility criteria and gives consent to participate* Medicines adherence assessment. Completion of community pharmacy MASS assessment tool. Provision of Solutions A. directly from the dispensary medicines adherence stock list and/or B. if the solution is a personalised (listbased) solution, it must be based on an accurate list of medicines. £ 28 per patient* Monitoring and Follow Up £ 10 per patient for monitoring at 1 month and 3 months (or appropriate intervals) and providing data to pilot lead pharmacist. Payment model A. Reimbursement for stock items provided. Please section below. OR B. £ 40 per patient per month for checking accuracy of the patient’s medicines list against the new prescription** and providing an appropriate personalised (list-based) for a maximum of 6 months or the duration of the pilot project.
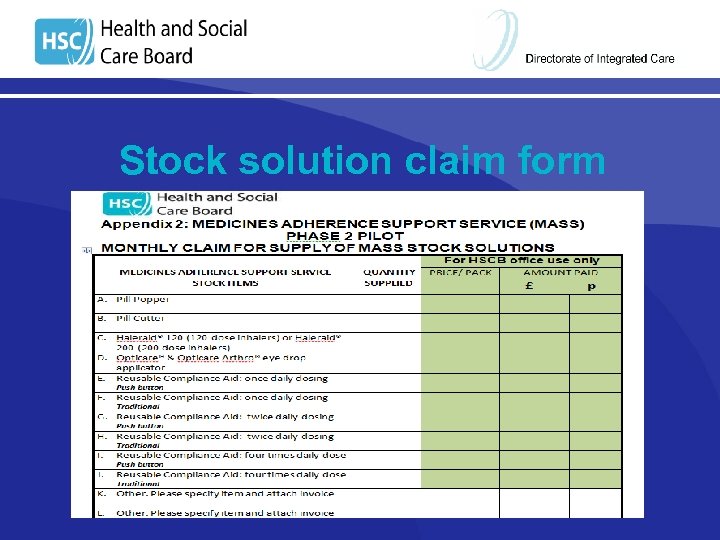 Stock solution claim form
Stock solution claim form
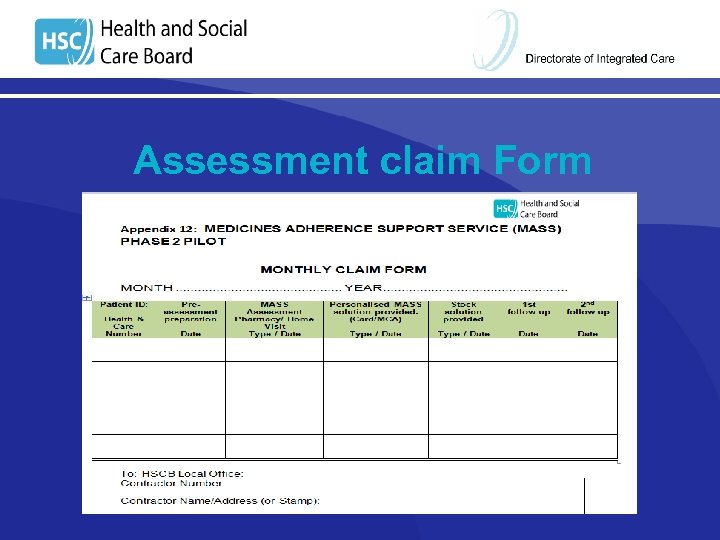 Assessment claim Form
Assessment claim Form
 Example Promote service in pharmacy - Poster - Leaflet in medication bag Patient identified (daughter concerned) - recently discharged from hospital - a lot of medication in the house
Example Promote service in pharmacy - Poster - Leaflet in medication bag Patient identified (daughter concerned) - recently discharged from hospital - a lot of medication in the house
 Recruitment § Patient information leaflet supplied § Patient agrees § Appointment arranged § Patient and daughter to attend pharmacy
Recruitment § Patient information leaflet supplied § Patient agrees § Appointment arranged § Patient and daughter to attend pharmacy
 Pre-assessment information
Pre-assessment information
 Assessment § Consent form signed Medications – including those started in hospital § Assessment completed § Changes to medication noted §
Assessment § Consent form signed Medications – including those started in hospital § Assessment completed § Changes to medication noted §
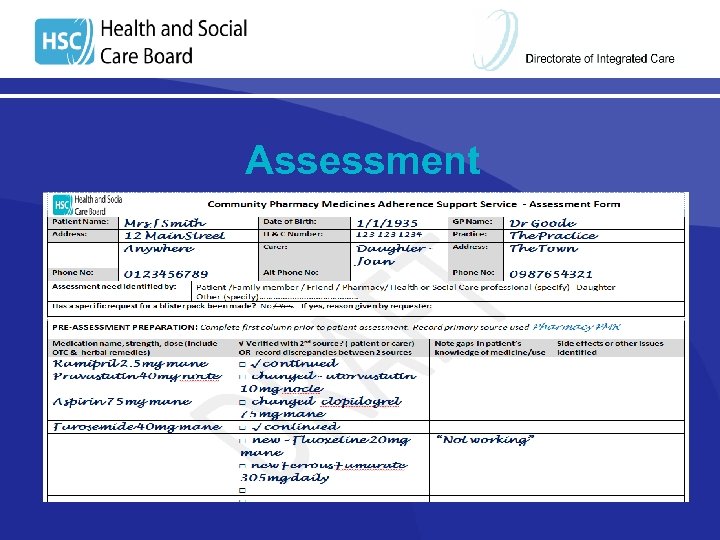 Assessment
Assessment
 Assessment
Assessment
 Solutions § § § Education on new medications Removal of discontinued medications (form) GP – change Atorvastatin to morning Written list of medicines? Synchronise script quantities and dates – daughter to order meds monthly Re-usable compliance aid – daughter will fill
Solutions § § § Education on new medications Removal of discontinued medications (form) GP – change Atorvastatin to morning Written list of medicines? Synchronise script quantities and dates – daughter to order meds monthly Re-usable compliance aid – daughter will fill
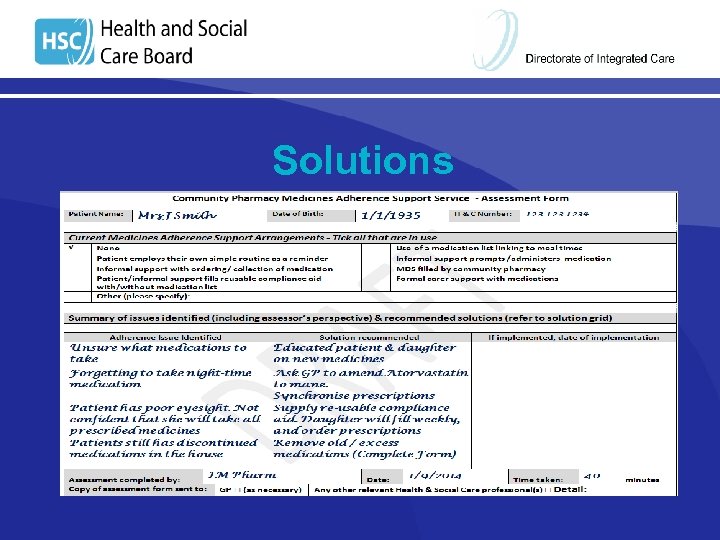 Solutions
Solutions
 Actions § § GP – synchronise scripts, amend Atorvastatin Claim forms § § § Pre-assessment preparation Assessment Stock solution (compliance aid) ? Personalised MASS solution 1 st and 2 nd Follow up
Actions § § GP – synchronise scripts, amend Atorvastatin Claim forms § § § Pre-assessment preparation Assessment Stock solution (compliance aid) ? Personalised MASS solution 1 st and 2 nd Follow up
 Thank you for listening ? ANY QUESTIONS Caroline Johnston, Caroline. Johnston@northerntrust. hscni. net JO Jo Gribben, Josephine. Gribben@setrust. hscni. net Susan Patterson, susan. patterson@hscni. net
Thank you for listening ? ANY QUESTIONS Caroline Johnston, Caroline. Johnston@northerntrust. hscni. net JO Jo Gribben, Josephine. Gribben@setrust. hscni. net Susan Patterson, susan. patterson@hscni. net


