cbc52295b7ae6165f4b538dba51a27f3.ppt
- Количество слайдов: 51
 Medications Chapter 35 60 Minutes- The wrong medicine 1
Medications Chapter 35 60 Minutes- The wrong medicine 1
 How are drugs named and classified • • Prescriptive drugs Nonprescriptive drugs Generic name Trade or Brand name 2
How are drugs named and classified • • Prescriptive drugs Nonprescriptive drugs Generic name Trade or Brand name 2
 Legal Aspects • • Nurse Practice Acts Controlled Substances US legislation State laws 3
Legal Aspects • • Nurse Practice Acts Controlled Substances US legislation State laws 3
 Effects of Drugs • • Side effects Adverse effects Drug toxicity Allergy – Anaphylactic reaction • Drug interaction 4
Effects of Drugs • • Side effects Adverse effects Drug toxicity Allergy – Anaphylactic reaction • Drug interaction 4
 Actions of Drugs on the Body • Half life • Onset • Peak plasma level 5
Actions of Drugs on the Body • Half life • Onset • Peak plasma level 5
 Pharmacokinetics • Absorption • Distribution • Biotransformation • Excretion 6
Pharmacokinetics • Absorption • Distribution • Biotransformation • Excretion 6
 Factors Affecting Medication Action • • Developmental Sex Cultural, ethnic, and genetic Diet Environment Psychological Illness and disease Time of administration
Factors Affecting Medication Action • • Developmental Sex Cultural, ethnic, and genetic Diet Environment Psychological Illness and disease Time of administration
 Oral • • Tablets, capsules, liquids Sublingual Buccal Enteral medications 8
Oral • • Tablets, capsules, liquids Sublingual Buccal Enteral medications 8
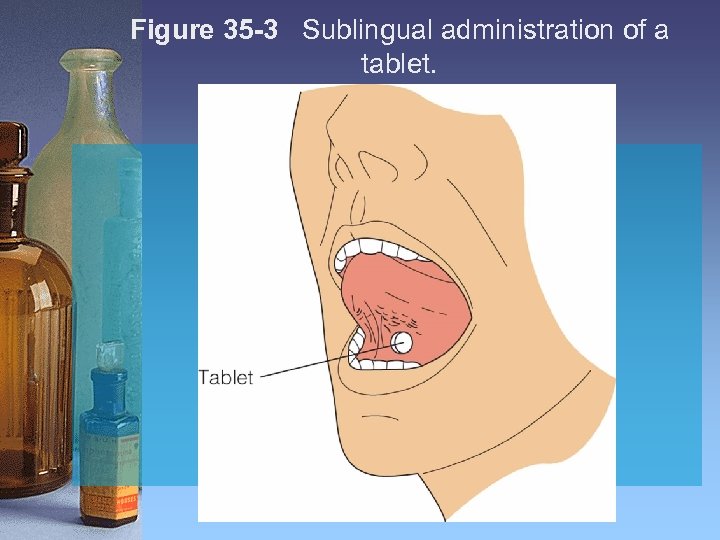 Figure 35 -3 Sublingual administration of a tablet.
Figure 35 -3 Sublingual administration of a tablet.
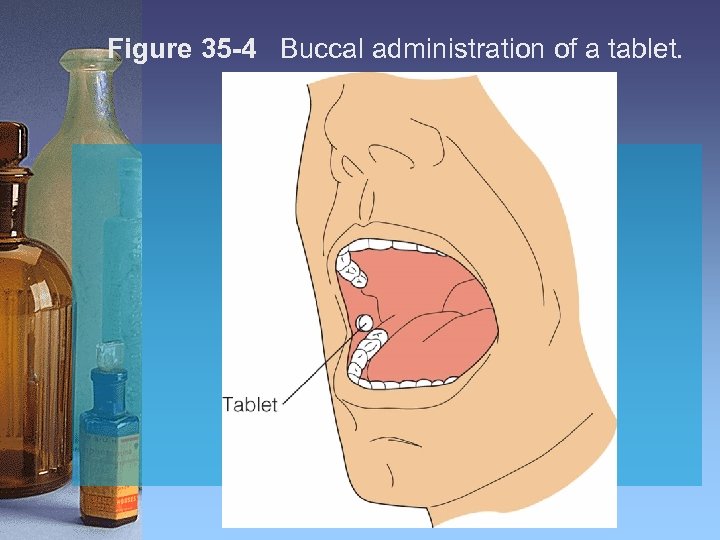 Figure 35 -4 Buccal administration of a tablet.
Figure 35 -4 Buccal administration of a tablet.
 Transdermal • Applied to the skin • Local (and sometimes systemic) effects • Skin lotions, creams, ointments • Transdermal patches 11
Transdermal • Applied to the skin • Local (and sometimes systemic) effects • Skin lotions, creams, ointments • Transdermal patches 11
 Parenteral Medications • Injected via – Intradermal – Subcutaneous – Intramuscular – Intravenous 12
Parenteral Medications • Injected via – Intradermal – Subcutaneous – Intramuscular – Intravenous 12
 Topical • Applied to skin or in a body cavity • Eye, ear, vagina, rectum, nose 13
Topical • Applied to skin or in a body cavity • Eye, ear, vagina, rectum, nose 13
 Types of Medication Orders • • STAT orders Single order Standing orders PRN orders • If written by the nurse (phone or verbal order) must read back to verify accuracy of the order. 14
Types of Medication Orders • • STAT orders Single order Standing orders PRN orders • If written by the nurse (phone or verbal order) must read back to verify accuracy of the order. 14
 Essential Parts of a Drug Order • • Full name of client Date and time the order is written Name of the drug Dosage Frequency of administration Route of administration Signature of the person writing the order
Essential Parts of a Drug Order • • Full name of client Date and time the order is written Name of the drug Dosage Frequency of administration Route of administration Signature of the person writing the order
 Communicating Orders • Telephone/verbal orders • Order placed on Medication Administration Record (MAR) 16
Communicating Orders • Telephone/verbal orders • Order placed on Medication Administration Record (MAR) 16
 • Write the order you receive over the phone from Dr. Jones. 17
• Write the order you receive over the phone from Dr. Jones. 17
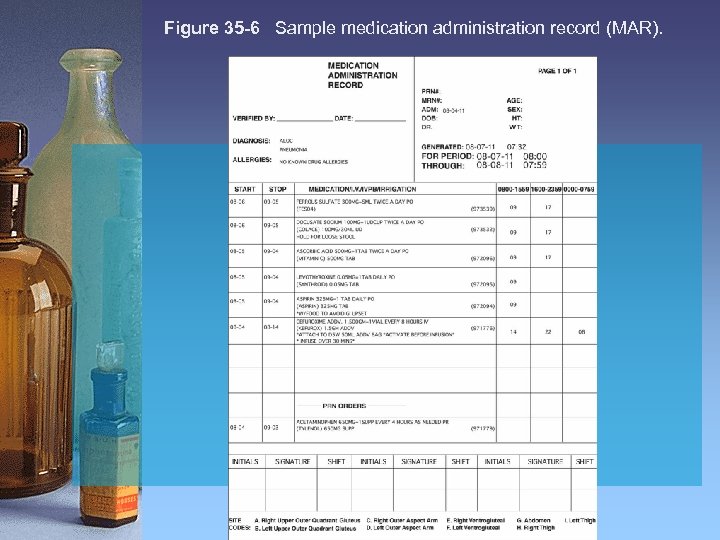 Figure 35 -6 Sample medication administration record (MAR).
Figure 35 -6 Sample medication administration record (MAR).
 Administering Medications Safety • • • Assessment Suitable route Medication history (hx) Drug allergies Specifics to drug Self administration problems 19
Administering Medications Safety • • • Assessment Suitable route Medication history (hx) Drug allergies Specifics to drug Self administration problems 19
 Administering Medications: Practice Guidelines • Pg. 860 20
Administering Medications: Practice Guidelines • Pg. 860 20
 Medication Reconciliation • Ensure clients receive meds as they move or transfer through or out of a facility • Compare complete list of meds to the physician’s orders 21
Medication Reconciliation • Ensure clients receive meds as they move or transfer through or out of a facility • Compare complete list of meds to the physician’s orders 21
 Medication Dispensing Systems • Medication Cart • Automated dispensing system • Unit dosing 22
Medication Dispensing Systems • Medication Cart • Automated dispensing system • Unit dosing 22
 Process of Administering Medications • Identify the client • Inform the client • Administer the drug – After completion of 3 checks
Process of Administering Medications • Identify the client • Inform the client • Administer the drug – After completion of 3 checks
 Process of Administering Medications (cont. ) • Provide adjunctive interventions as indicated • Record the drug administered • Evaluate the client’s response to the drug
Process of Administering Medications (cont. ) • Provide adjunctive interventions as indicated • Record the drug administered • Evaluate the client’s response to the drug
 Three Checks Rule (Box 35 -4 pg. 863) • Check the medication label against MAR • Upon removal • When preparing med • At the bedside 25
Three Checks Rule (Box 35 -4 pg. 863) • Check the medication label against MAR • Upon removal • When preparing med • At the bedside 25
 5 Rights + 5 (p. 864) • Right Patient • Right Drug • Right Route • Right Time • Right Dose • Right Documentation (the 6 th right) • • Client education Right to refuse Right assessment Right evaluation 26
5 Rights + 5 (p. 864) • Right Patient • Right Drug • Right Route • Right Time • Right Dose • Right Documentation (the 6 th right) • • Client education Right to refuse Right assessment Right evaluation 26
 Compare the medication label to the MAR.
Compare the medication label to the MAR.
 Medication Errors • Common errors • How can they be avoided? • Practice safe medication administration !!!! 28
Medication Errors • Common errors • How can they be avoided? • Practice safe medication administration !!!! 28
 What To Do If I Make A Medication Error? • • Assess VS and physical status Notify primary care provider Notify charge nurse Complete incident report 29
What To Do If I Make A Medication Error? • • Assess VS and physical status Notify primary care provider Notify charge nurse Complete incident report 29
 The nurse is taking an oral tablet of Tylenol to a client who is in a private room. He is in the bathroom and says, “just leave it on the table and I will take it when I come out. ” You are very familiar with this client and have cared for him all weekend long. What would you do? Why? 30
The nurse is taking an oral tablet of Tylenol to a client who is in a private room. He is in the bathroom and says, “just leave it on the table and I will take it when I come out. ” You are very familiar with this client and have cared for him all weekend long. What would you do? Why? 30
 Oral Med. Administration • Pg. 865 -871 per Lab discussion 31
Oral Med. Administration • Pg. 865 -871 per Lab discussion 31
 Parental Medications (pg. 872) • • Intradermal Subcutaneous (Sub. Q) Intramuscular Intravenously 32
Parental Medications (pg. 872) • • Intradermal Subcutaneous (Sub. Q) Intramuscular Intravenously 32
 Preparing injectable medications • Ampule • Vial • Reconstituting medications 33
Preparing injectable medications • Ampule • Vial • Reconstituting medications 33
 Intradermal Injections • • Are given in the dermis Use 1 ml. syringe 25 -27 gauge needle, ¼ to 5/8 in. Dose 0. 01 to 0. 1 ml Angle 5 -15 degrees Produces a wheal or bleb See Skill 35 -5 pg. 882 34
Intradermal Injections • • Are given in the dermis Use 1 ml. syringe 25 -27 gauge needle, ¼ to 5/8 in. Dose 0. 01 to 0. 1 ml Angle 5 -15 degrees Produces a wheal or bleb See Skill 35 -5 pg. 882 34
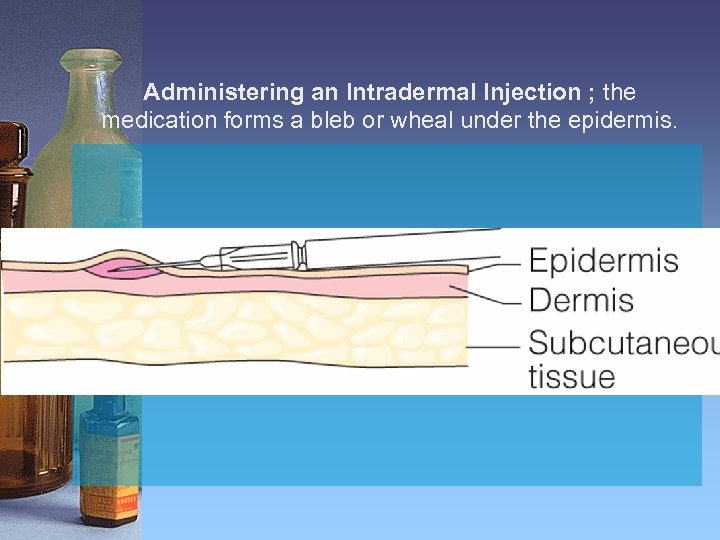 Administering an Intradermal Injection ; the medication forms a bleb or wheal under the epidermis.
Administering an Intradermal Injection ; the medication forms a bleb or wheal under the epidermis.
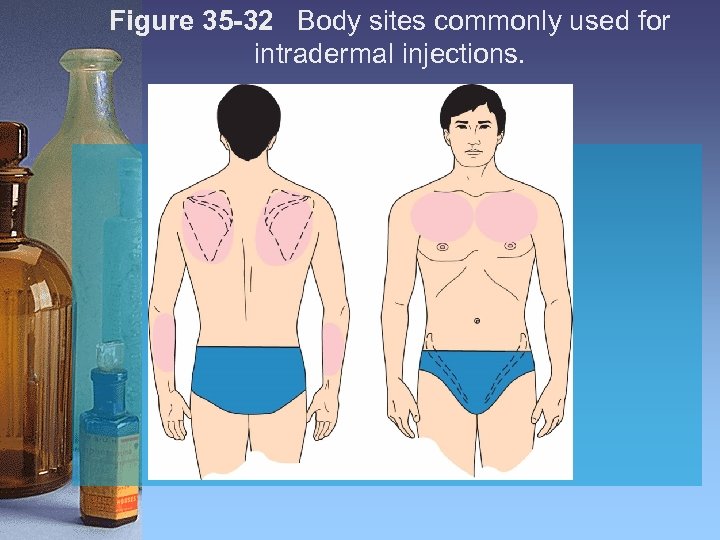 Figure 35 -32 Body sites commonly used for intradermal injections.
Figure 35 -32 Body sites commonly used for intradermal injections.
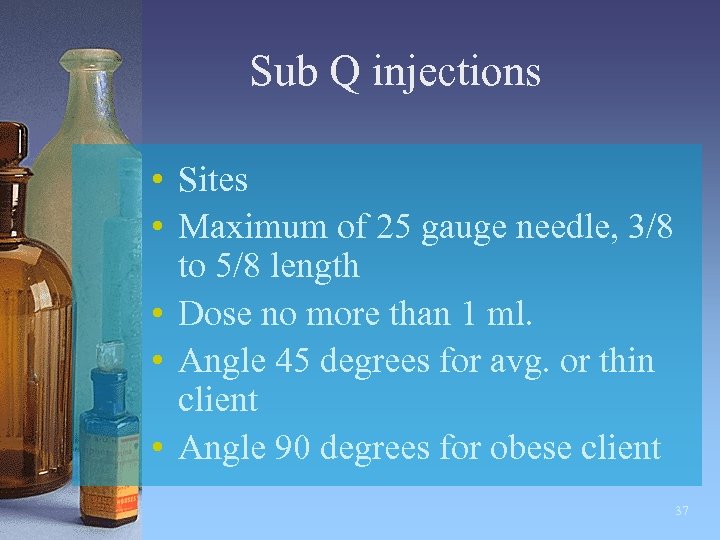 Sub Q injections • Sites • Maximum of 25 gauge needle, 3/8 to 5/8 length • Dose no more than 1 ml. • Angle 45 degrees for avg. or thin client • Angle 90 degrees for obese client 37
Sub Q injections • Sites • Maximum of 25 gauge needle, 3/8 to 5/8 length • Dose no more than 1 ml. • Angle 45 degrees for avg. or thin client • Angle 90 degrees for obese client 37
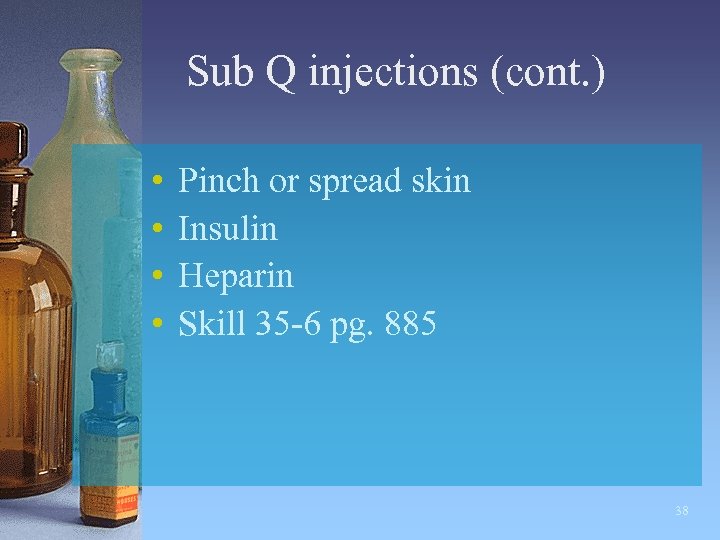 Sub Q injections (cont. ) • • Pinch or spread skin Insulin Heparin Skill 35 -6 pg. 885 38
Sub Q injections (cont. ) • • Pinch or spread skin Insulin Heparin Skill 35 -6 pg. 885 38
 SQ Injection Sites 39
SQ Injection Sites 39
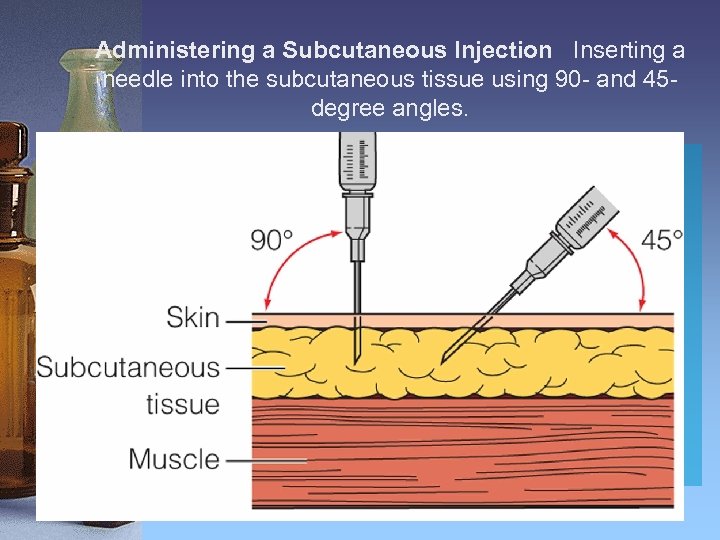 Administering a Subcutaneous Injection Inserting a needle into the subcutaneous tissue using 90 - and 45 degree angles.
Administering a Subcutaneous Injection Inserting a needle into the subcutaneous tissue using 90 - and 45 degree angles.
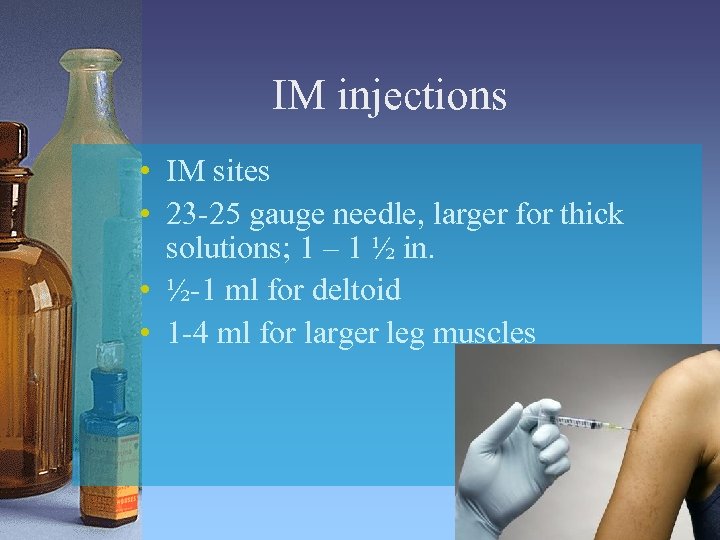 IM injections • IM sites • 23 -25 gauge needle, larger for thick solutions; 1 – 1 ½ in. • ½-1 ml for deltoid • 1 -4 ml for larger leg muscles 41
IM injections • IM sites • 23 -25 gauge needle, larger for thick solutions; 1 – 1 ½ in. • ½-1 ml for deltoid • 1 -4 ml for larger leg muscles 41
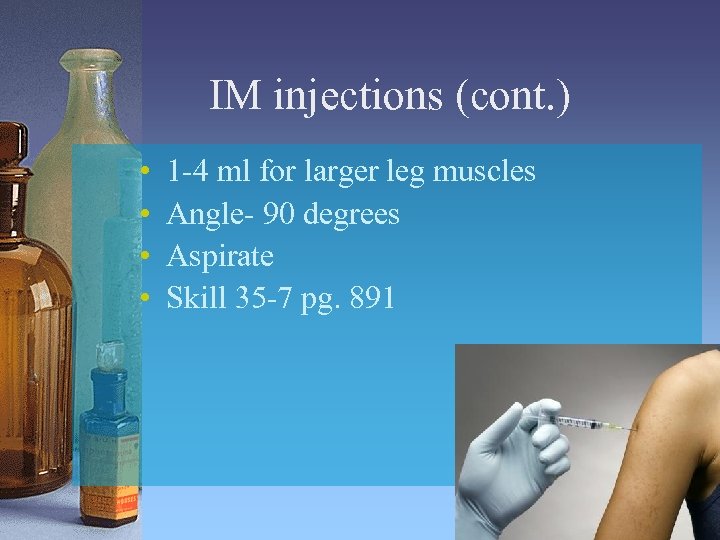 IM injections (cont. ) • • 1 -4 ml for larger leg muscles Angle- 90 degrees Aspirate Skill 35 -7 pg. 891 42
IM injections (cont. ) • • 1 -4 ml for larger leg muscles Angle- 90 degrees Aspirate Skill 35 -7 pg. 891 42
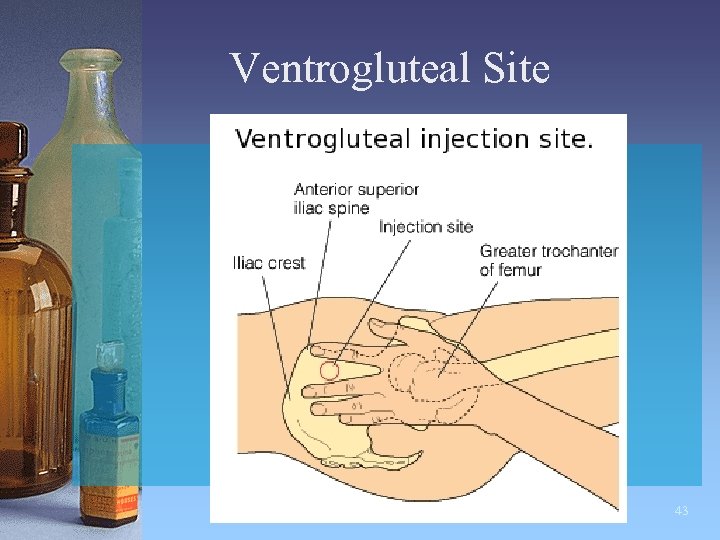 Ventrogluteal Site 43
Ventrogluteal Site 43
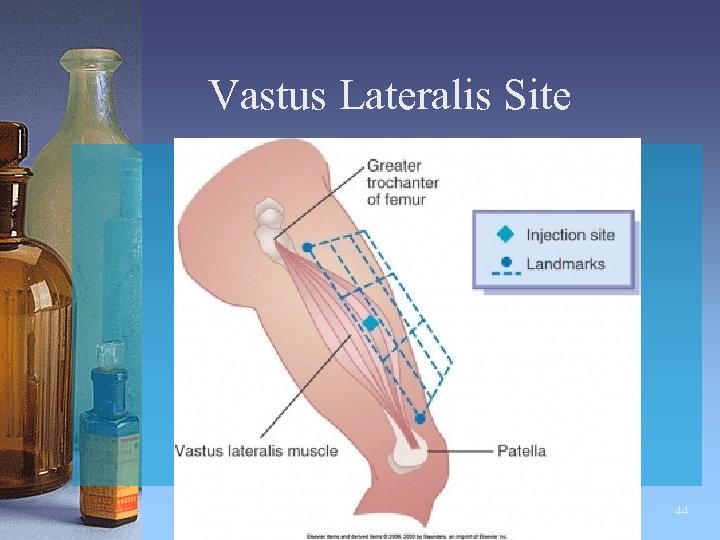 Vastus Lateralis Site 44
Vastus Lateralis Site 44
 Dorsogluteal Site • Not recommended • Injection site close to sciatic nerve 45
Dorsogluteal Site • Not recommended • Injection site close to sciatic nerve 45
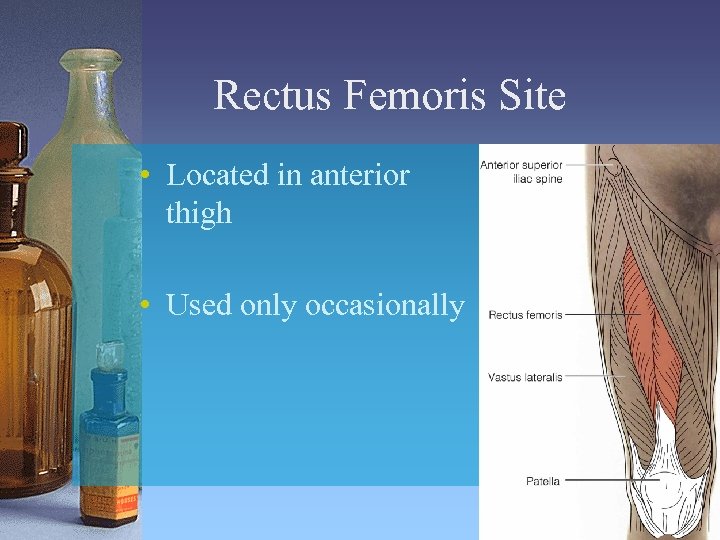 Rectus Femoris Site • Located in anterior thigh • Used only occasionally 46
Rectus Femoris Site • Located in anterior thigh • Used only occasionally 46
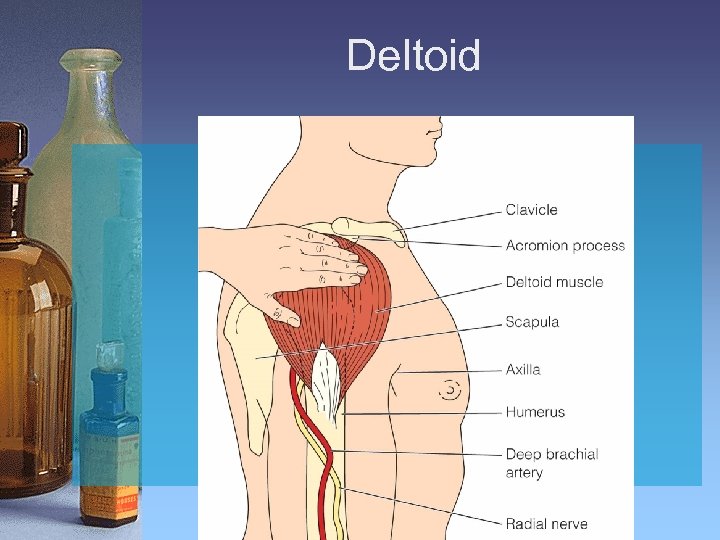 Deltoid
Deltoid
 IM Injection Technique: Z-Track • • Seals needle track Displace or pull skin to the side Insert needle Aspirate Inject (wait 5 -10 sec. ) Withdraw Release skin Skill 35 -7 pg. 892 48
IM Injection Technique: Z-Track • • Seals needle track Displace or pull skin to the side Insert needle Aspirate Inject (wait 5 -10 sec. ) Withdraw Release skin Skill 35 -7 pg. 892 48
 Considerations • A safe distance from nerves, large blood vessels, and bones • Free from injury, abscesses, tenderness, necrosis • Large enough to accommodate the volume of medication to be given 49
Considerations • A safe distance from nerves, large blood vessels, and bones • Free from injury, abscesses, tenderness, necrosis • Large enough to accommodate the volume of medication to be given 49
 Discussed in Lab (pg. 902 -915) • • Skin Ophthalmic (eye) Otic (ear) Nasal Vaginal Rectal Inhaled 50
Discussed in Lab (pg. 902 -915) • • Skin Ophthalmic (eye) Otic (ear) Nasal Vaginal Rectal Inhaled 50
 Let’s put it into practice! 51
Let’s put it into practice! 51


