6b117dc0184fc7e178ce7b58872afc10.ppt
- Количество слайдов: 64
Medicare and the Affordable Care Act: What you need to know for 2011 and beyond Age & Disability Odyssey June 21, 2011

Stephanie Minor Senior Link. Age Line® Program Consultant, Minnesota Board on Aging Michaela Monoghan Centers for Medicare & Medicaid Services Ashley Setala Centers for Medicare & Medicaid Services Deb Siebenaler Adult Protection, Minnesota Department of Human Services
Overview • In 2011 – Medicare Part A – Medicare Part B – Medicare Part C – Medicare Part D – Affordable Care Act Medicare changes
The Important DISCLAIMER • Information contained within this Power Point about the Affordable Care Act is subject to change at any time – Federal regulations must still be issued and could result in changes to the information contained within this presentation
The Medicare Facts • Medicare covers 47 million Medicare beneficiaries – 39 million seniors; 8 million under-65 disabled – 47 percent live on an income below 200% poverty – 29 percent in fair/poor health • Medicare is a critical part of policy discussions related to the federal budget – 12 percent of federal spending • Medicare is a major player in the US health care system – 23 percent of national personal health care spending
Medicare Part A • Most people receive Part A premium free – Bene and/or spouse paid Federal Insurance Contributions Act (FICA) taxes while working • People with less than 10 years of Medicare- covered employment – Can still get Part A, but will pay a monthly premium • 2011 Part A Premium if worked 30 -39 quarters = $248 • 2011 Part A Premium if worked less than 30 quarters = $450
Medicare Part A Coverage • • • Hospital inpatient care Skilled nursing facility (SNF) care Home health care Hospice care Blood
Medicare Part A Hospital Inpatient Coverage • Up to 90 days of inpatient hospital services in each benefit period – A benefit period begins when bene admitted to hospital and ends when bene has been out of the hospital for 60 days OR – Have not received Medicare-covered care in a SNF or hospital for 60 consecutive days from day of discharge • Lifetime Reserve Days – 60 days of inpatient hospital coverage (not SNF) following a 90 day hospital stay – Can use only once in lifetime • Medicare-certified specialty psychiatric hospital: 190 Lifetime Days

Medicare Part A Hospital Inpatient Coverage • 2011 Part A Deductible – $1, 132 for days 1 -60 • 2011 Copayment – $283 per day for days 61 -90 (same benefit period) – $566 per day for days 91 -150 (60 lifetime reserve days)
• Deductible is a fixed dollar amount paid for benefits before Medicare pays • Copayment is a fixed dollar amount paid when a Medicare covered service is received • Coinsurance is the amount required to be paid after Medicare deductibles; a percentage that can vary
HOT TOPIC: Observation Status • • Days spent in the hospital under Observation Status do not satisfy the 3 day prior hospital stay requirement to qualify for Medicare SNF coverage Hospital services provided under Observation status require the bene to pay a copayment for each individual outpatient hospital service – The copayment for a single outpatient hospital service cannot be more than the Part A Hospital inpatient deductible BUT – The total copayment for all services provided may be more than the Part A Hospital inpatient deductible • New notice for hospitals to provide to beneficiaries alerting them to difference between observation status and inpatient status – Note: Notice is not mandatory at this time. • Please contact the Senior Link. Age Line® about Observation cases where a bene wants to pursue an appeal (1 -800 -333 -2433)

Medicare Part A Skilled Nursing Facility Coverage • Covers up to 100 days of care in a SNF for each benefit period if – Daily skilled nursing and/or rehab services are needed – Prior to SNF admission, the bene must have a 3 day hospital stay • Hospital stays that are Observation Status do not satisfy this requirement – Must be admitted to a SNF within 30 days of the qualifying hospital stay – If Medicare qualified, Medicare pays for day 1 -20 at 100%. Days 21 -100 have a $141. 50 copayment per day (2011 amount)

Medicare Part A Home Health Care Coverage • Care provided must meet Medicare criteria – Plan of care approved by physician requires skilled nursing and skilled home health care services; AND – Bene must be homebound AND – Skilled nursing care is needed on a part-time or intermittent basis AND • Less than 8 hours per day • No more than 28 hours per week – Medicare can cover up to 35 hours in unusual cases – Care is provided by a Medicare-certified home health agency – There is no limit to the number of visits that can be covered

Medicare Part A Home Health Care Coverage • Medicare will not pay for – – 24 hour care Home delivered meals Homemaker or custodial care services Prescription drugs are NOT covered under the Part A Home health care benefit
Medicare Part A Hospice Coverage • For a bene to qualify for Medicare Hospice coverage – Must have Part A – Physician and the hospice medical director certify that bene has a terminal illness and life expectancy is 6 months or less – Bene signs a statement electing to have Medicare pay for palliative care, such as pain management, rather than trying to cure the bene condition. – Bene terminal condition is documented in medical record – Receive care from a Medicare-certified hospice agency – Bene does not need to be homebound to qualify for benefit
Medicare Part A Hospice Coverage • Certification for Hospice Care – At the beginning of each Certification period, the physician must certify that bene is terminally ill • First Certification – 90 days • Second Certification – 90 days • Third Certification and beyond– unlimited number of 60 day periods • Ending Hospice Care – Bene always has the right to stop Medicare hospice care at any time and get Medicare-covered curative care for the terminal illness – Bene can return to hospice again later if qualifies
Medicare Part A Blood Coverage • Covers blood transfusions for hospital or skilled nursing facility bene • There is no limit on the amount of blood or the number of transfusions Medicare will cover • Pay for the first 3 pints of blood unless bene or other donates 3 pints of blood
Medicare Part B • 2011 Monthly Premium for most – $96. 40 -$110. 50 - $115. 40 • 2011 Annual Deductible – $162 • 2011 Coinsurance – 20% of Medicare approved amount for all Part B services except mental health outpatient treatment and home health care – 45% of Medicare approved amount for Part B mental health outpatient treatment
Affordable Care Act and Medicare Part B Premium • Freezes income threshold for Part B premiums paid by higher income beneficiaries from 2011 -2019 – – – $85, 000 individuals $170, 000 couples No longer indexed for inflation More beneficiaries will pay increased Part B premium Begins January 1, 2011
Medicare Part B • • • Physician Services Durable Medical Equipment, Prosthetics, Orthotics, Supplies Ambulance Services Preventive Care Services Outpatient Physical, Speech and Occupational Therapy Blood Chiropractic Care Outpatient Mental Health Services (55%/45%) Home Health Care X-rays and Lab Tests Limited Prescription Drugs

Medicare Part B Outpatient Mental Health Coverage • Medicare covers mental health services on an outpatient basis provided by either a doctor, clinical psychologist, clinical social worker, clinical nurse specialist, or physician assistant in an office setting, clinic, treatment center or hospital outpatient department. • Bene is responsible for 45% of the Medicare-approved amount. – Bene amount will reduce to 40% effective January 1, 2012 – Bene may also have to pay a separate copayment for the facility service
Medicare Part B Prescription Drug Coverage • Part B covers a limited number of outpatient prescription drugs. • Participating pharmacy or doctor must accept assignment on prescription drugs covered under Part B. • Part B covers drugs that aren’t usually self-administered when given in a hospital outpatient department or doctor’s office. – Self-administered drugs provided in an outpatient setting like an emergency room or observation unit may be covered under Medicare Part D, but not Medicare Part B

Medicare Part B Prescription Drug Coverage • Some Antigens: Prepared by doctor and administered by trained person • Osteoporosis Drugs: Injectable drugs for osteoporosis for certain women • Erythropoisis–stimulating Agents (such as Epogen®, Procrit®, Epoetin alfa, or Aranesp®, Darbepoetin alfa): By injection if bene has end -stage renal disease or to treat anemia related to certain conditions • Blood Clotting Factors: Has hemophilia and given to self by injection. • Injectable Drugs: Covers most injectable drugs administered by a licensed medical practitioner, if the drug is considered reasonable and necessary for treatment.
Medicare Part B Prescription Drug Coverage • Immunosuppressive Drugs: For transplant patients if the transplant was paid for by Medicare (or paid by private insurance that paid as a primary payer to bene Medicare Part A coverage) in a Medicare-certified facility. – Note: Medicare Part D plans may cover immunosuppressive drugs, even if Medicare or an employer or union group health plan didn’t pay for the transplant. • • • Oral Cancer Drugs: Some cancer drugs bene takes by mouth if the same drug is available in injectable form. Oral Anti-Nausea Drugs: When used as part of an anti-cancer chemotherapeutic regimen and administered within 48 hours to be used as a full therapeutic replacement for intravenous anti-nausea drugs. Medicare also covers some drugs used in infusion pumps and nebulizers if considered reasonable and necessary. (including insulin)
Medicare Advance Beneficiary Notice • Notice that physician, supplier and provider must give before furnishing an item or service if they believe that Medicare may deny payment. • Providers are not required to give an ABN for services or items explicitly excluded from Medicare coverage – Example: Hearing aids • Advise to always select the option on the ABN that they want a claim submitted to Medicare or the provider is not required to submit the claim • ABNs only apply to bene in Original Medicare, not Medicare Advantage

Minnesota Medicare Supplements • Works with Original Medicare • Basic and Extended Basic benefits are available when a bene enrolls in Medicare, regardless of age or health problems • Effective June 1, 2010, a new hospice benefit was added as a core benefit available with every Medicare supplement purchased – Will cover all cost-sharing for Part B hospice care and respite care expenses • Medicare SELECT
Minnesota Medicare Population • 775, 930 Medicare beneficiaries – 15% of total Minnesota population – 321, 109 enrolled in a Medicare Advantage Plan (Part C) • 2008 -2010 enrollment increased by 27% – 88% of MN Medicare beneficiaries have prescription drug coverage (68% through Part D)
Overall changes with Medicare Advantage (Part C) • Beginning January 2012, payments to the Medicare Advantage plans will be reduced • Effective January 1, 2014, all Medicare Advantage plans will be required to pay at least 85% of the premium dollars toward payment of the beneficiary’s medical claims • 5 Star-rating system: – Beginning January 2012, plans will be able to receive higher payments if they can demonstrate they are providing high-quality care to enrollees (must receive 4 or 5 stars) – Beginning 2012, plans receiving a 5 -star rating may enroll beneficiaries year-round.

New Medicare Advantage Disenrollment Period • January 1, 2011 – February 14, 2011 • During this new Medicare Advantage Disenrollment period, – Beneficiaries can disenroll from a Medicare Advantage plan and switch to Original Medicare – Beneficiaries can enroll in a Stand Alone PDP plan for Part D coverage even if they did not have Medicare Part D coverage with their Medicare Advantage plan – Beneficiaries enrolled in a Medicare Advantage plan cannot switch to another Medicare Advantage plan – Beneficiaries in Original Medicare cannot enroll in a Medicare Advantage plan
Affordable Health Care Act and Medicare Part D: Minnesota Medicare Beneficiaries in 2010 • 775, 930 Medicare beneficiaries in Minnesota – 88% of the Minnesota Medicare population has prescription drug coverage (68% have it through Medicare Part D) – In 2009 • 63, 700 Minnesota Medicare beneficiaries hit the Part D donut hole
Medicare Part D Info • Medicare Part D Benefit for 2011 – Same deductible as 2010 ($310) – Increase in Initial Coverage Limit by $10 • $2840 in 2011 – Out of pocket threshold is same as 2010 ($4, 550) – Donut Hole $2840. 01 -$4, 550 in 2011 • Reduced brand name and generic prices
2011 Part D Plan Changes • 73% of the Stand Alone PDP are not offering any significant gap coverage in 2011 – 67% will have no gap coverage – 6% will cover fewer than 10% of generic drugs on their formulary
Medicare Part D • Higher Part D premium for higher-income beneficiaries – Income related monthly adjustment amount – The additional amount is a percentage based on the national base premium ($32. 34) • The percentage increases as income increases, and ranges from 35% to 80% – The additional amount will be deducted from a beneficiary’s monthly SSA/RRB benefit • Beneficiaries will receive a notice from SSA • It does not go to the Part D plans 8
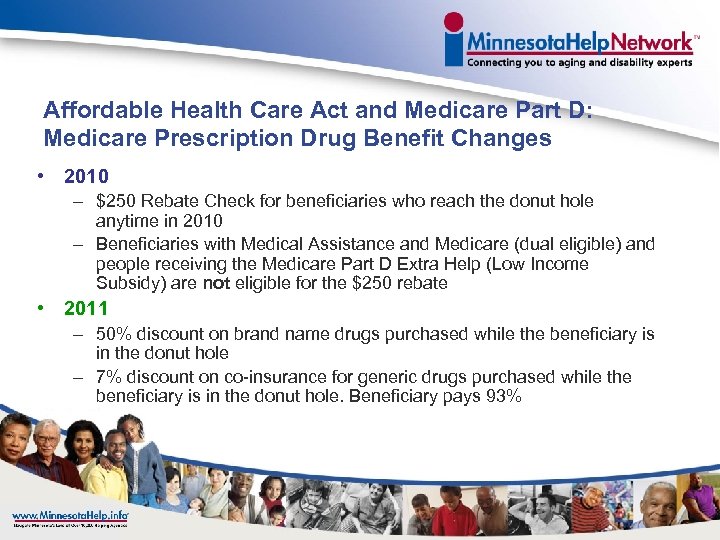
Affordable Health Care Act and Medicare Part D: Medicare Prescription Drug Benefit Changes • 2010 – $250 Rebate Check for beneficiaries who reach the donut hole anytime in 2010 – Beneficiaries with Medical Assistance and Medicare (dual eligible) and people receiving the Medicare Part D Extra Help (Low Income Subsidy) are not eligible for the $250 rebate • 2011 – 50% discount on brand name drugs purchased while the beneficiary is in the donut hole – 7% discount on co-insurance for generic drugs purchased while the beneficiary is in the donut hole. Beneficiary pays 93%
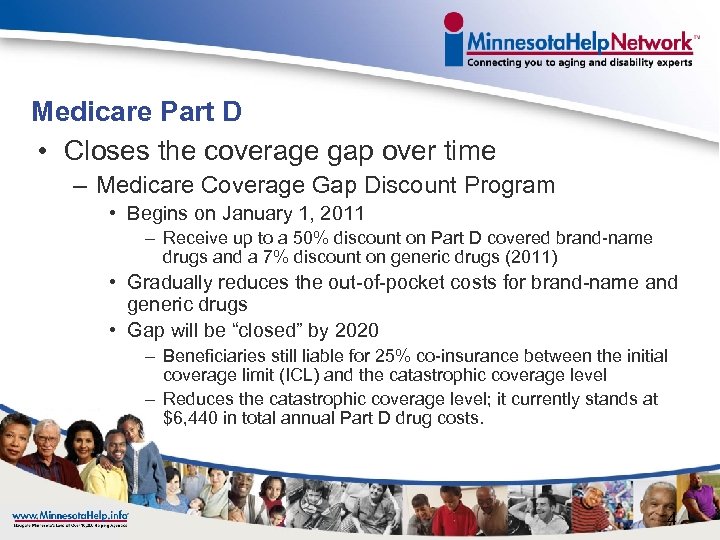
Medicare Part D • Closes the coverage gap over time – Medicare Coverage Gap Discount Program • Begins on January 1, 2011 – Receive up to a 50% discount on Part D covered brand-name drugs and a 7% discount on generic drugs (2011) • Gradually reduces the out-of-pocket costs for brand-name and generic drugs • Gap will be “closed” by 2020 – Beneficiaries still liable for 25% co-insurance between the initial coverage limit (ICL) and the catastrophic coverage level – Reduces the catastrophic coverage level; it currently stands at $6, 440 in total annual Part D drug costs. 4
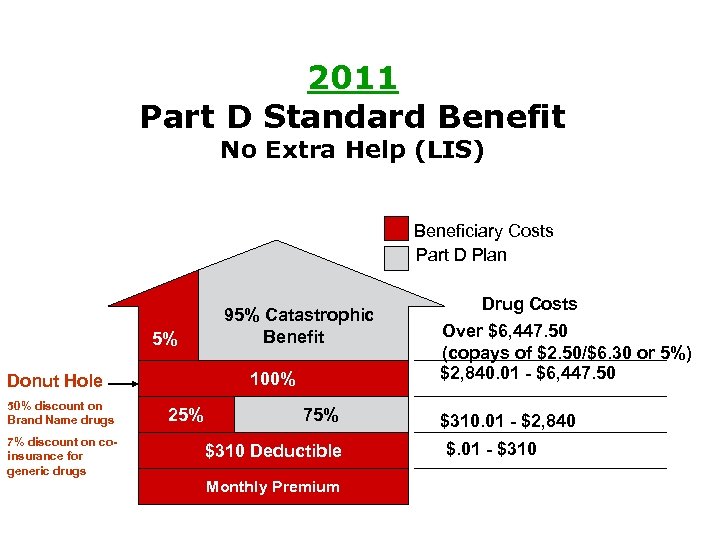
2011 Part D Standard Benefit No Extra Help (LIS) Beneficiary Costs Part D Plan 5% 100% Donut Hole 50% discount on Brand Name drugs 7% discount on coinsurance for generic drugs 95% Catastrophic Benefit 25% 75% $310 Deductible Monthly Premium Drug Costs Over $6, 447. 50 (copays of $2. 50/$6. 30 or 5%) $2, 840. 01 - $6, 447. 50 $310. 01 - $2, 840 $. 01 - $310
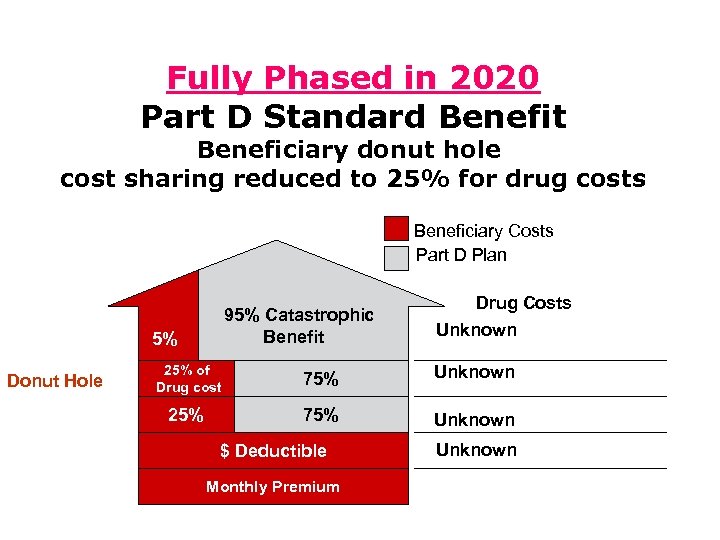
Fully Phased in 2020 Part D Standard Benefit Beneficiary donut hole cost sharing reduced to 25% for drug costs Beneficiary Costs Part D Plan 95% Catastrophic Benefit 5% Donut Hole Drug Costs Unknown 25% of Drug cost 75% Unknown 25% 75% Unknown $ Deductible Monthly Premium Unknown
2011 Benchmark Plans for Minnesota • A prescription drug plan with a monthly premium at or below the low income premium subsidy amount • MN Benchmark Amount in 2011: $37. 47 • 9 Options for 2011 – Ensure plan is still a benchmark in in 2012 • Dual eligible premiums for these plans are completely covered by LIS – Duals can enroll in non-benchmark plans, but will have out of pockets costs for the premium
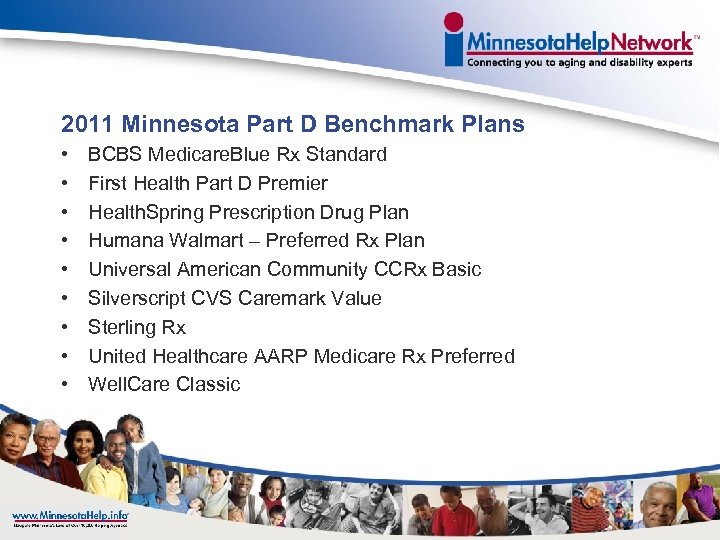
2011 Minnesota Part D Benchmark Plans • • • BCBS Medicare. Blue Rx Standard First Health Part D Premier Health. Spring Prescription Drug Plan Humana Walmart – Preferred Rx Plan Universal American Community CCRx Basic Silverscript CVS Caremark Value Sterling Rx United Healthcare AARP Medicare Rx Preferred Well. Care Classic
Low-Income Subsidy • Redetermination Process – Allows widows and widowers to delay redetermination for the LIS for 1 -year after the death of a spouse (effective January 1, 2011) – Requires CMS to transmit, within 30 days of a beneficiary being automatically reassigned to a new Part D plan, information on the differences between the former plan’s and new plan’s formularies and information on the coverage determination, exception, appeal and grievance processes (begins in 2011) 10
2011 Medicare Part D for Dual Eligibles • All dual eligibles including: – Waivers – MA-EPD • All Medicare Savings Program enrollees – QMB – SLMB – QI • On SSI and no Medicaid
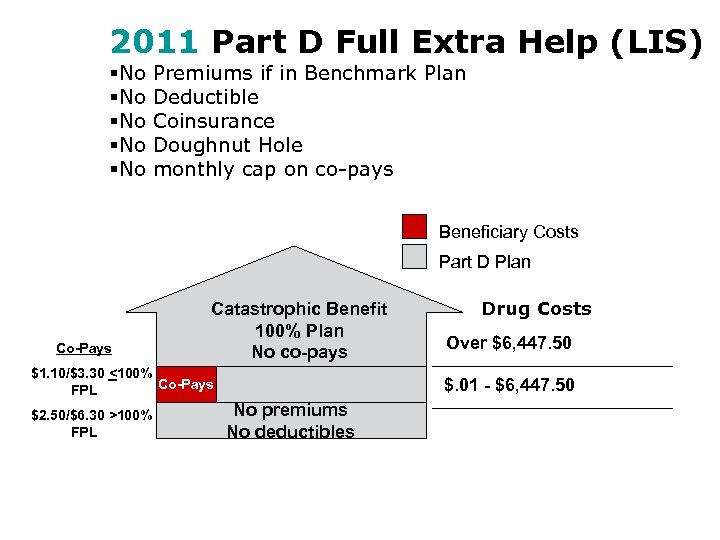
2011 Part D Full Extra Help (LIS) §No §No §No Premiums if in Benchmark Plan Deductible Coinsurance Doughnut Hole monthly cap on co-pays Beneficiary Costs Part D Plan Co-Pays Catastrophic Benefit 100% Plan No co-pays $1. 10/$3. 30 <100% Co-Pays FPL $2. 50/$6. 30 >100% FPL Drug Costs Over $6, 447. 50 $. 01 - $6, 447. 50 No premiums No deductibles
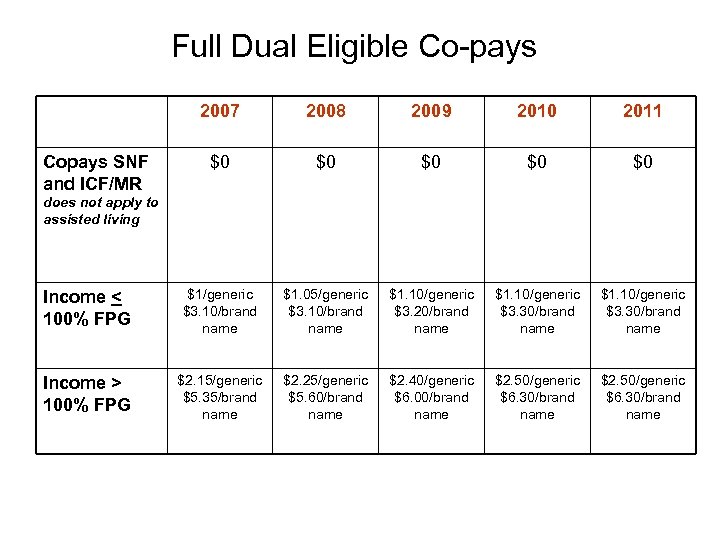
Full Dual Eligible Co-pays 2007 2008 2009 2010 2011 $0 $0 $0 Income < 100% FPG $1/generic $3. 10/brand name $1. 05/generic $3. 10/brand name $1. 10/generic $3. 20/brand name $1. 10/generic $3. 30/brand name Income > 100% FPG $2. 15/generic $5. 35/brand name $2. 25/generic $5. 60/brand name $2. 40/generic $6. 00/brand name $2. 50/generic $6. 30/brand name Copays SNF and ICF/MR does not apply to assisted living
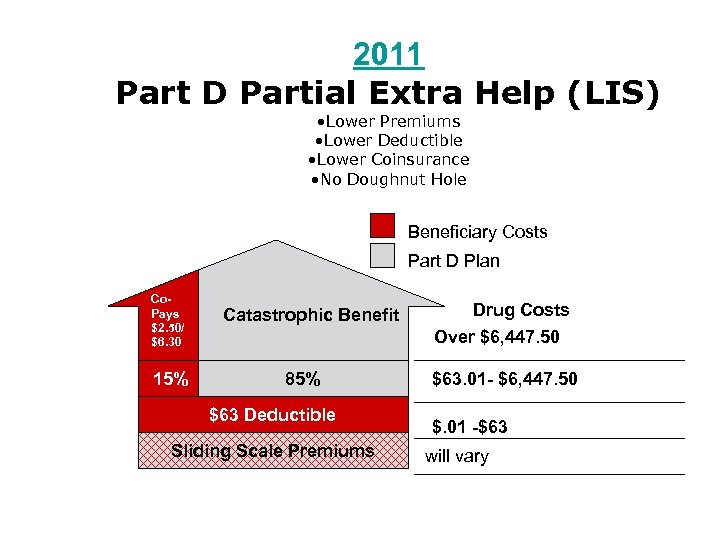
2011 Part D Partial Extra Help (LIS) • Lower Premiums • Lower Deductible • Lower Coinsurance • No Doughnut Hole Beneficiary Costs Part D Plan Co. Pays $2. 50/ $6. 30 15% Catastrophic Benefit 85% $63 Deductible Sliding Scale Premiums Drug Costs Over $6, 447. 50 $63. 01 - $6, 447. 50 $. 01 -$63 will vary
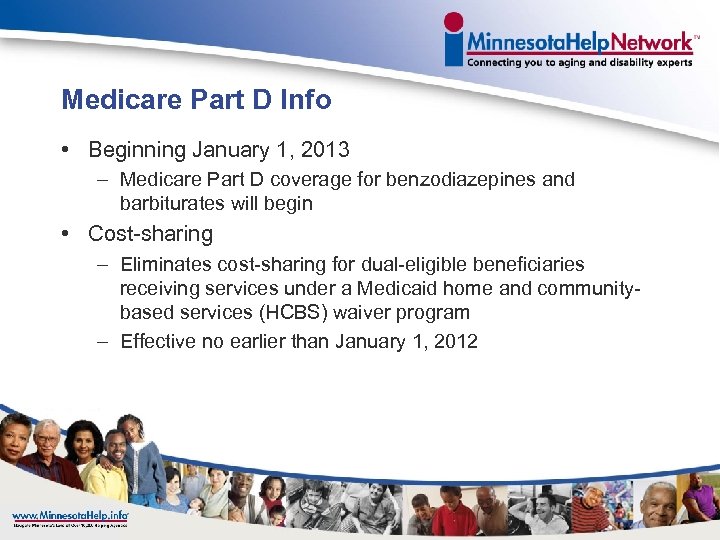
Medicare Part D Info • Beginning January 1, 2013 – Medicare Part D coverage for benzodiazepines and barbiturates will begin • Cost-sharing – Eliminates cost-sharing for dual-eligible beneficiaries receiving services under a Medicaid home and communitybased services (HCBS) waiver program – Effective no earlier than January 1, 2012
Annual Election Period Change • Beginning Fall 2011, the Annual Election Period will change to • October 15, 2011 - December 7, 2011 (54 days) • Will need to make plan changes during this time period – No changes from December 8 – December 31, 2011 • Plan enrollment effective date will be January 1, 2012 • Can change Medicare Advantage Plans or Stand Alone PDP Plans • PLEASE HELP spread the word to your Medicare beneficiaries!
Preventive Services • New Annual Wellness visit – Beneficiaries receive personalized prevention plan services (PPPS) • Establish or update the individual’s medical and family history • List individual’s current medical providers and suppliers and all prescribed medications • Record measurements of height, weight, body mass index, blood pressure and other routine measurements • Detect any cognitive impairment • Establish a screening schedule for the next 5 to 10 years • Provide personal health advice and coordinate appropriate referrals and health education 18
Preventive Services • Eliminates cost-sharing for most Medicare-covered preventive services – Annual Part B deductible and 20% coinsurance – Effective January 1, 2011 • Eliminates the Part B deductible for tests that begin as colorectal cancer screening tests, but based on findings from the test, become diagnostic or therapeutic services 19
Web Tools for Beneficiaries and Caregivers • Nursing Home Compare Website: Requires CMS to add certain information to its Nursing Home Compare Medicare website that includes: • Staffing data • Links to state websites regarding state nursing home survey and certification programs • Model complaint form • Summary of substantiated complaints • Information on criminal violations by a facility or its employees 23
Web Tools for Beneficiaries And Caregivers • Physician Compare Website – Requires the Secretary of HHS to develop by January 1, 2011 a “Physician Compare” website with information on physicians enrolled in the Medicare program and other eligible professionals who participate in the Physician Quality Reporting Initiative – Adding to the new Physician Compare website (available no later than January 1, 2011), requires the Secretary of HHS to implement, by January 1, 2013, a plan for making available comparable information on physician performance including quality and patient experience measures, patient outcomes, coordination of care, safety, effectiveness and timeliness of care, and other information 24
Your Link to An Expert: Senior Link. Age Line® • Senior Link. Age Line® 1 -800 -333 -2433 – – • Statewide Objective Comprehensive Individualized assistance by phone, in your community and in your home – Federally designated State Health Insurance Assistance Program (SHIP) for Minnesota – There is no fee or charge for assistance provided – Does not sell, endorse or promote any insurance, long-term care or health care product Senior Link. Age Line® is your Long-term Care Options and Medicare Expert in Minnesota

Minnesota. Help Network™ is here to help you • • • Senior Link. Age Line® 1 -800 -333 -2433 Disability Linkage Line® 1 -866 -333 -2466 Veterans Linkage Line™ 1 -888 -Link. Vet www. Minnesota. Help. info® (including Live Chat) http: //longtermcarechoices. minnesotahelp. info/ Local community based sites throughout Minnesota

Questions? • Contact Information – Stephanie Minor – 651 -431 -2602 – Stephanie. A. Minor@state. mn. us
Elder Justice Act/ MN Adult Protection overview Age and Disability Odyssey June 21, 2011 Deb Siebenaler 54
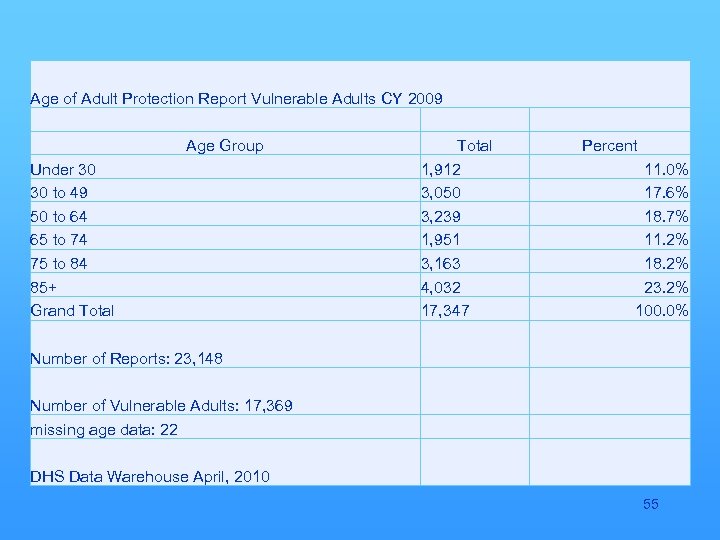
Age of Adult Protection Report Vulnerable Adults CY 2009 Age Group Total Under 30 1, 912 30 to 49 3, 050 50 to 64 3, 239 65 to 74 1, 951 75 to 84 3, 163 85+ 4, 032 Grand Total 17, 347 Percent 11. 0% 17. 6% 18. 7% 11. 2% 18. 2% 23. 2% 100. 0% Number of Reports: 23, 148 Number of Vulnerable Adults: 17, 369 missing age data: 22 DHS Data Warehouse April, 2010 55
Elder Justice Act § Title XX of the Social Security Act is amended to include Elder Justice. § Elder Justice Coordinating Council § Authorization – such sums § Advisory Board on Elder Abuse, Neglect, and Exploitation § Authorization such sums 56
Elder Justice Act § § Forensic Centers § Authorization – 4 M FY 2011 (to 8 M FY 2013, 2014) Enhancement of long-term care -Grants to enhance training and recruitment and retention of staff, coordination with secretary of labor to recruit and train long term care staff § Authorization: 20 M FY 2011, 17 M FY 2012, 15 M FY 2013 and 2014 57
Elder Justice Act § Adult Protective Services Functions and Grants § Grants to States: appropriated by the percentage of total number of elders who reside in the United States who resides in that State - MN 2007 Census 60 and Older Population = 878, 200 (1. 68% of total population) Estimated EJA funds for MN = 1, 566, 435 § continued 58
continued § § § Adult Protective Services (Only for Adult Protective Services – may not be used for any other purpose) Funds provided to unit of government responsible for providing adult protective services within the State. Funds will supplement not supplant current expenditures for Adult Protective services in the State. § Authorization: 100 M FY 2011 -2014 59
Elder Justice Act § Adult Protection - State Demonstration Programs – Grants § Training modules for purpose of detecting or preventing elder abuse § Prevention financial exploitation of elders § Methods to detect elder abuse § Evaluation on forensic training § Other matters relating to elder abuse § Authorization: 25 M each FY 2011 - 2014 60
Elder Justice Act § Long-Term Care Ombudsman Program Grants and Training § Improve capacity for Long-Term Care Ombudsman Program to respond to and resolve complaints about abuse and neglect § Authorization: 5 M 2011 l 7. 5 M 2012; 10 M 2013 and 2014 61
Elder Justice Act § Protecting Residents of Long-Term Care Facilities § National Training Institute for Surveyors § National Back up system (24/7) to State complaint intake systems. § Authorization: 12 M for each FY 2011 – 2014 62
Elder Justice Act § Reporting to law enforcement of crimes occurring in federally funded long-term care facilities. § Individual shall report to the Secretary and 1 or more law enforcement entities any reasonable suspicion of a crime against any individual who is a resident of or is receiving care from the facility. § No authorization 63
Elder Justice Act § National Nurse Aide Registry § Authorization – Such sums 64
6b117dc0184fc7e178ce7b58872afc10.ppt