1bc575cc495a70b7818706514f9e6575.ppt
- Количество слайдов: 77
 Medical Surgical Nursing Care The Urinary System Assessment & Disorders Dr Ibrahim Bashayreh, RN, Ph. D 03/05/2011 1
Medical Surgical Nursing Care The Urinary System Assessment & Disorders Dr Ibrahim Bashayreh, RN, Ph. D 03/05/2011 1
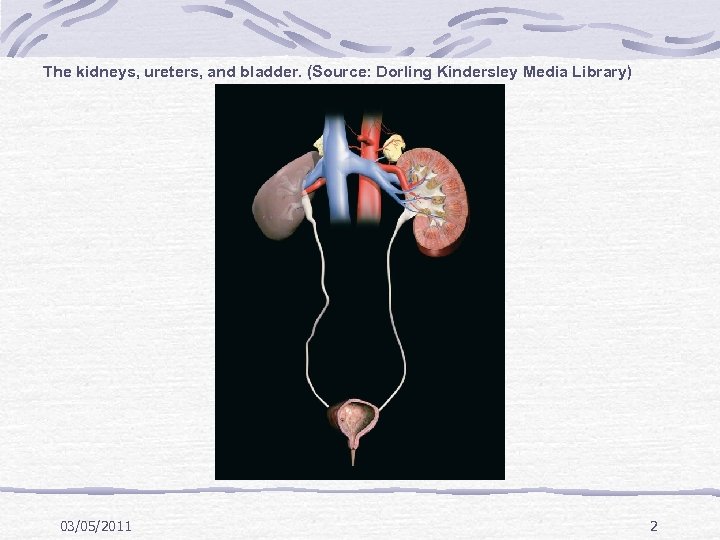 The kidneys, ureters, and bladder. (Source: Dorling Kindersley Media Library) 03/05/2011 2
The kidneys, ureters, and bladder. (Source: Dorling Kindersley Media Library) 03/05/2011 2
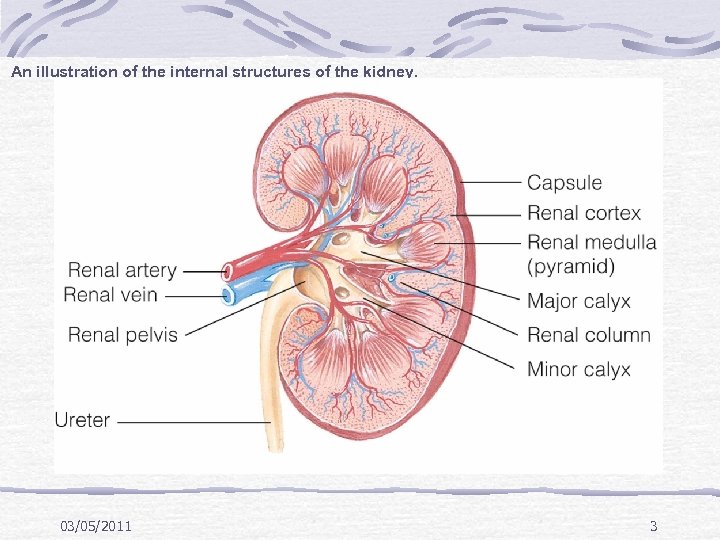 An illustration of the internal structures of the kidney. 03/05/2011 3
An illustration of the internal structures of the kidney. 03/05/2011 3
 The structure of the nephron and the processes of urine formation. (Source: Pearson Education/PH College) 03/05/2011 4
The structure of the nephron and the processes of urine formation. (Source: Pearson Education/PH College) 03/05/2011 4
 Urine Formation Glomerular filtration rate Tubular reabsorption Include water and electrolytes Tubular secretion Urine concentration 03/05/2011 5
Urine Formation Glomerular filtration rate Tubular reabsorption Include water and electrolytes Tubular secretion Urine concentration 03/05/2011 5
 Endocrine Function Renin–angiotensin–aldosterone system Role in blood pressure and sodium reabsorption Erythropoietin Role in RBC production Vitamin D and calcium regulation Acid–base balance 03/05/2011 6
Endocrine Function Renin–angiotensin–aldosterone system Role in blood pressure and sodium reabsorption Erythropoietin Role in RBC production Vitamin D and calcium regulation Acid–base balance 03/05/2011 6
 Age-Related Changes Nephrons lost with aging Reduces kidney mass and GFR Less urine concentration Risk for dehydration 03/05/2011 7
Age-Related Changes Nephrons lost with aging Reduces kidney mass and GFR Less urine concentration Risk for dehydration 03/05/2011 7
 Assessment Color, clarity, amount of urine Difficulty initiating urination or changes in stream Changes in urinary pattern Dysuria, nocturia, hematuria, pyuria 03/05/2011 8
Assessment Color, clarity, amount of urine Difficulty initiating urination or changes in stream Changes in urinary pattern Dysuria, nocturia, hematuria, pyuria 03/05/2011 8
 Assessment History of urinary problems Urinary or abdominal surgeries Smoking, alcohol use, number of sexual partners and type of sexual relationship Chance of pregnancy History of diabetes or other endocrine disorders History of kidney stones 03/05/2011 9
Assessment History of urinary problems Urinary or abdominal surgeries Smoking, alcohol use, number of sexual partners and type of sexual relationship Chance of pregnancy History of diabetes or other endocrine disorders History of kidney stones 03/05/2011 9
 Physical Assessment Obtain clean-catch urine specimen Color, odor, clarity Vital signs and skin assessment 03/05/2011 10
Physical Assessment Obtain clean-catch urine specimen Color, odor, clarity Vital signs and skin assessment 03/05/2011 10
 Diagnostic Tests Clean-catch urine 24 -hour urine Culture and sensitivity BUN, creatinine and creatinine clearance IVP CT scan Renal scan 03/05/2011 11
Diagnostic Tests Clean-catch urine 24 -hour urine Culture and sensitivity BUN, creatinine and creatinine clearance IVP CT scan Renal scan 03/05/2011 11
 Diagnostic Tests Ultrasound Bladder scan Cystoscopy Uroflowmetry 03/05/2011 12
Diagnostic Tests Ultrasound Bladder scan Cystoscopy Uroflowmetry 03/05/2011 12
 Renal Failure Acute and Chronic Renal Obstructive Disorder Medical Surgical Nursing Dr ibraheem Bashayreh, RN, Ph. D 03/05/2011 13
Renal Failure Acute and Chronic Renal Obstructive Disorder Medical Surgical Nursing Dr ibraheem Bashayreh, RN, Ph. D 03/05/2011 13
 Acute Renal Failure Sudden interruption of kidney function resulting from obstruction, reduced circulation, or disease of the renal tissue Results in retention of toxins, fluids, and end products of metabolism Usually reversible with medical treatment May progress to end stage renal disease, uremic syndrome, and death without treatment 03/05/2011 14
Acute Renal Failure Sudden interruption of kidney function resulting from obstruction, reduced circulation, or disease of the renal tissue Results in retention of toxins, fluids, and end products of metabolism Usually reversible with medical treatment May progress to end stage renal disease, uremic syndrome, and death without treatment 03/05/2011 14
 Acute Renal Failure Persons at Risks Major surgery Major trauma Receiving nephrotoxic medications Elderly 03/05/2011 15
Acute Renal Failure Persons at Risks Major surgery Major trauma Receiving nephrotoxic medications Elderly 03/05/2011 15
 03/05/2011 16
03/05/2011 16
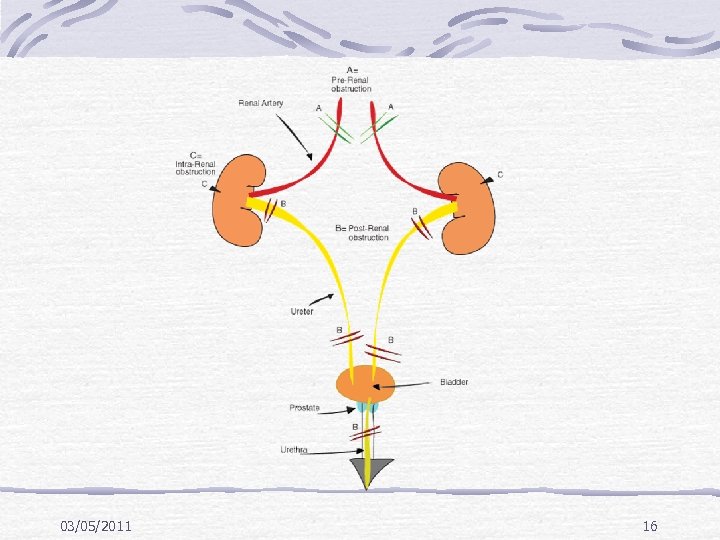
 Acute Renal Failure Causes Prerenal Hypovolemia, shock, blood loss, embolism, pooling of fluid d/t ascites or burns, cardiovascular disorders, sepsis Intrarenal Nephrotoxic agents, infections, ischemia and blockages, polycystic kidney disease Postrenal Stones, blood clots, BPH, urethral edema from invasive procedures 03/05/2011 17
Acute Renal Failure Causes Prerenal Hypovolemia, shock, blood loss, embolism, pooling of fluid d/t ascites or burns, cardiovascular disorders, sepsis Intrarenal Nephrotoxic agents, infections, ischemia and blockages, polycystic kidney disease Postrenal Stones, blood clots, BPH, urethral edema from invasive procedures 03/05/2011 17
 Acute Renal Failure Stages Onset – 1 -3 days with ^ BUN and creatinine and possible decreased UOP Oliguric – UOP < 400/d, ^BUN, Creat, Phos, K, may last up to 14 d Diuretic – UOP ^ to as much as 4000 m. L/d but no waste products, at end of this stage may begin to see improvement Recovery – things go back to normal or may remain insufficient and become chronic 03/05/2011 18
Acute Renal Failure Stages Onset – 1 -3 days with ^ BUN and creatinine and possible decreased UOP Oliguric – UOP < 400/d, ^BUN, Creat, Phos, K, may last up to 14 d Diuretic – UOP ^ to as much as 4000 m. L/d but no waste products, at end of this stage may begin to see improvement Recovery – things go back to normal or may remain insufficient and become chronic 03/05/2011 18
 Acute Renal Failure Subjective symptoms Nausea Loss of appetite Headache Lethargy Tingling in extremities 03/05/2011 19
Acute Renal Failure Subjective symptoms Nausea Loss of appetite Headache Lethargy Tingling in extremities 03/05/2011 19
 Acute Renal Failure Objective symptoms Oliguric phase – vomiting disorientation, edema, ^K+ decrease Na ^ BUN and creatinine Acidosis uremic breath 03/05/2011 CHF and pulmonary edema hypertension caused by hypovolemia, anorexia sudden drop in UOP convulsions, coma changes in bowels 20
Acute Renal Failure Objective symptoms Oliguric phase – vomiting disorientation, edema, ^K+ decrease Na ^ BUN and creatinine Acidosis uremic breath 03/05/2011 CHF and pulmonary edema hypertension caused by hypovolemia, anorexia sudden drop in UOP convulsions, coma changes in bowels 20
 Acute Renal Failure Objective systoms Diuretic phase Increased UOP Gradual decline in BUN and creatinine Hypokalemia Hyponaturmia Tachycardia Improved LOC 03/05/2011 21
Acute Renal Failure Objective systoms Diuretic phase Increased UOP Gradual decline in BUN and creatinine Hypokalemia Hyponaturmia Tachycardia Improved LOC 03/05/2011 21
 Acute Renal Failure Diagnostic tests H&P BUN, creatinine, sodium, potassium. p. H, bicarb. Hgb and Hct Urine studies US of kidneys KUB ABD and renal CT/MRI Retrograde pyloegram: is a urologic procedure where the physician injects contrast into the ureter in order to visualize the ureter and kidney. 03/05/2011 22
Acute Renal Failure Diagnostic tests H&P BUN, creatinine, sodium, potassium. p. H, bicarb. Hgb and Hct Urine studies US of kidneys KUB ABD and renal CT/MRI Retrograde pyloegram: is a urologic procedure where the physician injects contrast into the ureter in order to visualize the ureter and kidney. 03/05/2011 22
 Acute Renal Failure Medical treatment Fluid and dietary restrictions Maintain E-lytes D/C or change cause May need dialysis to jump start renal function May need to stimulate production of urine with IV fluids, Dopomine, diuretics, etc. 03/05/2011 23
Acute Renal Failure Medical treatment Fluid and dietary restrictions Maintain E-lytes D/C or change cause May need dialysis to jump start renal function May need to stimulate production of urine with IV fluids, Dopomine, diuretics, etc. 03/05/2011 23
 Acute Renal Failure Medical treatment Hemodialysis Subclavian approach Femoral approach Peritoneal dialysis Continous renal replacement therapy (CRRT): The concept behind continuous renal replacement techniques is to dialyse patients in a more physiologic way, slowly, over 24 hours, just like the kidney Can be done continuously Does not require dialysate: the fluid and solutes in a dialysis process that flow through the dialyzer, do not pass through the membrane, and are discarded along with removed toxic substances after leaving the dialyzer. 03/05/2011 24
Acute Renal Failure Medical treatment Hemodialysis Subclavian approach Femoral approach Peritoneal dialysis Continous renal replacement therapy (CRRT): The concept behind continuous renal replacement techniques is to dialyse patients in a more physiologic way, slowly, over 24 hours, just like the kidney Can be done continuously Does not require dialysate: the fluid and solutes in a dialysis process that flow through the dialyzer, do not pass through the membrane, and are discarded along with removed toxic substances after leaving the dialyzer. 03/05/2011 24
 Acute Renal Failure Nursing Diagnosisimbalanced fluid volume= excess Altered electrolyte balance Altered cardiac output Impaired tissue perfusion: renal Anxiety Imbalanced nutrition Risk for infection Fatigue Knowledge deficit 03/05/2011 25
Acute Renal Failure Nursing Diagnosisimbalanced fluid volume= excess Altered electrolyte balance Altered cardiac output Impaired tissue perfusion: renal Anxiety Imbalanced nutrition Risk for infection Fatigue Knowledge deficit 03/05/2011 25
 Acute Renal Failure Plan. Promote recovery of optimal kidney function. Maintain normal fluid and electrolyte balance. Decrease anxiety. Increase knowledge. 03/05/2011 26
Acute Renal Failure Plan. Promote recovery of optimal kidney function. Maintain normal fluid and electrolyte balance. Decrease anxiety. Increase knowledge. 03/05/2011 26
 Acute Renal Failure Nursing interventions Monitor I/O, including all body fluids Monitor lab results Watch hyperkalemia symptoms: malaise, anorexia, or muscle weakness, EKG changes watch for hyperglycemia or hypoglycemia if receiving TPN or insulin infusions 03/05/2011 Maintain nutrition Safety measures Mouth care Daily weights Assess for signs of heart failure Skin integrity problems 27
Acute Renal Failure Nursing interventions Monitor I/O, including all body fluids Monitor lab results Watch hyperkalemia symptoms: malaise, anorexia, or muscle weakness, EKG changes watch for hyperglycemia or hypoglycemia if receiving TPN or insulin infusions 03/05/2011 Maintain nutrition Safety measures Mouth care Daily weights Assess for signs of heart failure Skin integrity problems 27
 Kidney failure causes hypoglycemia in three separate ways. The kidneys help to generate new glucose from amino acids (called gluconeogenesis). Gluconeogenesis is impaired in kidney failure. Also, insulin circulates for a longer period of time and is cleared slowly when kidney function is poor. The third important reason is that kidney failure reduces the appetite and consequently, oral intake of food. 03/05/2011 28
Kidney failure causes hypoglycemia in three separate ways. The kidneys help to generate new glucose from amino acids (called gluconeogenesis). Gluconeogenesis is impaired in kidney failure. Also, insulin circulates for a longer period of time and is cleared slowly when kidney function is poor. The third important reason is that kidney failure reduces the appetite and consequently, oral intake of food. 03/05/2011 28
 Chronic Renal Failure Results form gradual, progressive loss of renal function Occasionally results from rapid progression of acute renal failure Symptoms occur when 75% of function is lost but considered cohrnic if 90 -95% loss of function Dialysis is necessary D/T accumulation or uremic toxins, which produce changes in major organs 03/05/2011 29
Chronic Renal Failure Results form gradual, progressive loss of renal function Occasionally results from rapid progression of acute renal failure Symptoms occur when 75% of function is lost but considered cohrnic if 90 -95% loss of function Dialysis is necessary D/T accumulation or uremic toxins, which produce changes in major organs 03/05/2011 29
 Chronic Renal Failure Subjective symptoms are relatively same as acute Objective symptoms Renal Hyponaturmia Dry mouth Poor skin turgor Confusion, salt overload, accumulation of K with muscle weakness Fluid overload and metabolic acidosis Proteinuria, glycosuria Urine = RBC’s, WBC’s, and casts 03/05/2011 30
Chronic Renal Failure Subjective symptoms are relatively same as acute Objective symptoms Renal Hyponaturmia Dry mouth Poor skin turgor Confusion, salt overload, accumulation of K with muscle weakness Fluid overload and metabolic acidosis Proteinuria, glycosuria Urine = RBC’s, WBC’s, and casts 03/05/2011 30
 Chronic Renal Failure Objective symptoms Cardiovascular Hypertension Arrythmias Pericardial effusion CHF Peripheral edema 03/05/2011 Neurological Burning, pain, and itching, paresthesia Motor nerve dysfunction Muscle cramping Shortened memory span Apathy Drowsy, confused, seizures, coma, EEG changes 31
Chronic Renal Failure Objective symptoms Cardiovascular Hypertension Arrythmias Pericardial effusion CHF Peripheral edema 03/05/2011 Neurological Burning, pain, and itching, paresthesia Motor nerve dysfunction Muscle cramping Shortened memory span Apathy Drowsy, confused, seizures, coma, EEG changes 31
 Chronic Renal Failure Objective symptoms GI Stomatitis Ulcers Pancreatitis Uremic fetor (Ammonia breath odour) Vomiting constipation Respiratory ^ chance of infection Pulmonary edema Pleural friction rub and effusion Dyspnea Kussmaul’s respirations is a deep and labored breathing pattern often associated with severe metabolic acidosis, particularly diabetic ketoacidosis (DKA) but also renal failure. 03/05/2011 32
Chronic Renal Failure Objective symptoms GI Stomatitis Ulcers Pancreatitis Uremic fetor (Ammonia breath odour) Vomiting constipation Respiratory ^ chance of infection Pulmonary edema Pleural friction rub and effusion Dyspnea Kussmaul’s respirations is a deep and labored breathing pattern often associated with severe metabolic acidosis, particularly diabetic ketoacidosis (DKA) but also renal failure. 03/05/2011 32
 Chronic Renal Failure Objective symptoms Endocrine Stunted growth in children Amenorrhea Male impotence ^ aldosterone secretion Impaired glucose levels R/T impaired CHO metabolism Thyroid and parathyroid abnormalities 03/05/2011 Hemopoietic Anemia Decrease in RBC survival time Blood loss from dialysis and GI bleed Platelet deficits Bleeding and clotting disorders – purpura and hemorrhage from body orifices , ecchymoses 33
Chronic Renal Failure Objective symptoms Endocrine Stunted growth in children Amenorrhea Male impotence ^ aldosterone secretion Impaired glucose levels R/T impaired CHO metabolism Thyroid and parathyroid abnormalities 03/05/2011 Hemopoietic Anemia Decrease in RBC survival time Blood loss from dialysis and GI bleed Platelet deficits Bleeding and clotting disorders – purpura and hemorrhage from body orifices , ecchymoses 33
 Chronic Renal Failure Objective symptoms Skeletal Skin Yellow-bronze skin with pallor Muscle and bone pain Puritus Bone demineralization Purpura Pathological fractures Blood vessel Uremic frost calcifications in Thin, brittle nails myocardium, joints, Dry, brittle hair, and eyes, and brain may have color changes and alopecia Uremic frost: A clinical finding in severe chronic renal failure, in which the concentration of urea is markedly increased in sweat, causing precipitation of crystallised urea in the skin 03/05/2011 34
Chronic Renal Failure Objective symptoms Skeletal Skin Yellow-bronze skin with pallor Muscle and bone pain Puritus Bone demineralization Purpura Pathological fractures Blood vessel Uremic frost calcifications in Thin, brittle nails myocardium, joints, Dry, brittle hair, and eyes, and brain may have color changes and alopecia Uremic frost: A clinical finding in severe chronic renal failure, in which the concentration of urea is markedly increased in sweat, causing precipitation of crystallised urea in the skin 03/05/2011 34
 Chronic Renal Failure Lab findings BUN – indicator of glomerular filtration rate and is affected by the breakdown of protein. Normal is 10 -20 mg/d. L. When reaches 70 = dialysis Serum creatinine – waste product of skeletal muscle breakdown and is a better indicator of kidney function. Normal is 0. 5 -1. 5 mg/d. L. When reaches 10 x normal, it is time for dialysis Creatinine clearance is best determent of kidney function (GFR). Must be a 12 -24 hour urine collection. Normal is > 100 ml/min 03/05/2011 35
Chronic Renal Failure Lab findings BUN – indicator of glomerular filtration rate and is affected by the breakdown of protein. Normal is 10 -20 mg/d. L. When reaches 70 = dialysis Serum creatinine – waste product of skeletal muscle breakdown and is a better indicator of kidney function. Normal is 0. 5 -1. 5 mg/d. L. When reaches 10 x normal, it is time for dialysis Creatinine clearance is best determent of kidney function (GFR). Must be a 12 -24 hour urine collection. Normal is > 100 ml/min 03/05/2011 35
 Chronic Renal Failure K+ The kidneys are means which K+ is excreted. Normal is 3. 5 -5. 0 , m. Eq/L. maintains muscle contraction and is essential for cardiac function. Both elevated and decreased can cause problems with cardiac rhythm Hyperkalemia is treated with IV glucose and Na Bicarb which pushes K+ back into the cell Kayexalate (Sodium polystyrene sulfonate ) is also used to promote the exchange of sodium and potassium in the body. 03/05/2011 36
Chronic Renal Failure K+ The kidneys are means which K+ is excreted. Normal is 3. 5 -5. 0 , m. Eq/L. maintains muscle contraction and is essential for cardiac function. Both elevated and decreased can cause problems with cardiac rhythm Hyperkalemia is treated with IV glucose and Na Bicarb which pushes K+ back into the cell Kayexalate (Sodium polystyrene sulfonate ) is also used to promote the exchange of sodium and potassium in the body. 03/05/2011 36
 Chronic Renal Failure Ca With disease in the kidney, the enzyme for utilization of Vit D is absent Ca absorption depends upon Vit D Body moves Ca out of the bone to compensate and with that Ca comes phosphate bound to it. Normal Ca level is 4. 5 -5. 5 m. Eq/L Hypocalcemia = tetany Treat with calcium with Vit D and phosphate Avoid antacids with magnesium 03/05/2011 37
Chronic Renal Failure Ca With disease in the kidney, the enzyme for utilization of Vit D is absent Ca absorption depends upon Vit D Body moves Ca out of the bone to compensate and with that Ca comes phosphate bound to it. Normal Ca level is 4. 5 -5. 5 m. Eq/L Hypocalcemia = tetany Treat with calcium with Vit D and phosphate Avoid antacids with magnesium 03/05/2011 37
 Chronic Renal Failure Other abnormal findings Metabolic acidosis Fluid imbalance Insulin resistance Anemia Immunoligical problems 03/05/2011 38
Chronic Renal Failure Other abnormal findings Metabolic acidosis Fluid imbalance Insulin resistance Anemia Immunoligical problems 03/05/2011 38
 Chronic Renal Failure Nursing diagnosis Excess fluid volume Imbalanced nutrition Ineffective coping Risk for infection Risk for injury 03/05/2011 39
Chronic Renal Failure Nursing diagnosis Excess fluid volume Imbalanced nutrition Ineffective coping Risk for infection Risk for injury 03/05/2011 39
 Chronic Renal Failure Nursing care Frequent monitoring Hydration and output Cardiovascular function Respiratory status E-lytes Nutrition Mental status Emotional well being 03/05/2011 Ensure proper medication regimen Skin care Bleeding problems Care of the shunt Education to client and family 40
Chronic Renal Failure Nursing care Frequent monitoring Hydration and output Cardiovascular function Respiratory status E-lytes Nutrition Mental status Emotional well being 03/05/2011 Ensure proper medication regimen Skin care Bleeding problems Care of the shunt Education to client and family 40
 Chronic Renal Failure Treatment 03/05/2011 41
Chronic Renal Failure Treatment 03/05/2011 41
 Chronic Renal Failure Medical treatment IV glucose and insulin Na bicarb, Ca, Vit D, phosphate binders Fluid restriction, diuretics Iron supplements, blood, erythropoietin High carbs, low protein Dialysis - After all other methods have failed 03/05/2011 42
Chronic Renal Failure Medical treatment IV glucose and insulin Na bicarb, Ca, Vit D, phosphate binders Fluid restriction, diuretics Iron supplements, blood, erythropoietin High carbs, low protein Dialysis - After all other methods have failed 03/05/2011 42
 Dialysis ½ of patients with CRF eventually require dialysis Diffuse harmful waste out of body Control BP Keep safe level of chemicals in body 2 types Hemodialysis Peritoneal dialysis 03/05/2011 43
Dialysis ½ of patients with CRF eventually require dialysis Diffuse harmful waste out of body Control BP Keep safe level of chemicals in body 2 types Hemodialysis Peritoneal dialysis 03/05/2011 43
 Dialysis Peritoneal dialysis Semipermeable membrane Catheter inserted through abdominal wall into peritoneal cavity Cost less Fewer restrictions Can be done at home Risk of peritonitis 3 phases – inflow, dwell and outflow 03/05/2011 Automated peritoneal dialysis Done at home at night Maybe 6 -7 times /week CAPD Continous ambulatory peritoneal dialysis Done as outpatient Usually 4 X/d 44
Dialysis Peritoneal dialysis Semipermeable membrane Catheter inserted through abdominal wall into peritoneal cavity Cost less Fewer restrictions Can be done at home Risk of peritonitis 3 phases – inflow, dwell and outflow 03/05/2011 Automated peritoneal dialysis Done at home at night Maybe 6 -7 times /week CAPD Continous ambulatory peritoneal dialysis Done as outpatient Usually 4 X/d 44
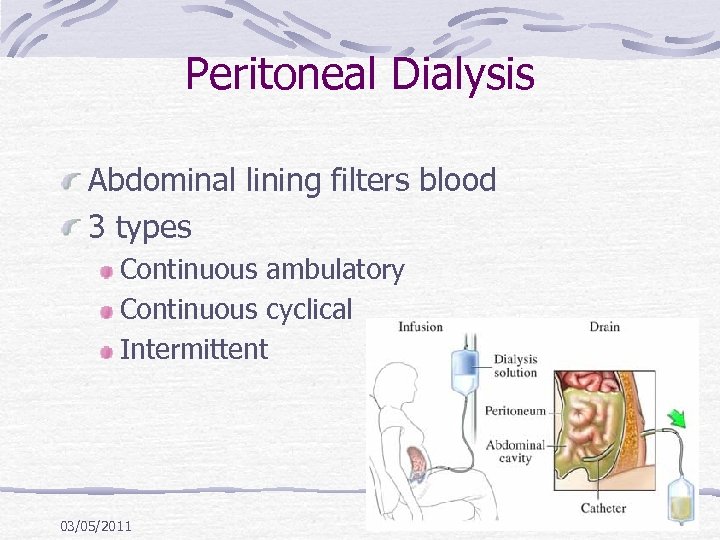 Peritoneal Dialysis Abdominal lining filters blood 3 types Continuous ambulatory Continuous cyclical Intermittent 03/05/2011 45
Peritoneal Dialysis Abdominal lining filters blood 3 types Continuous ambulatory Continuous cyclical Intermittent 03/05/2011 45
 Hemodialysis 3 -4 times a week Takes 2 -4 hours Machine filters blood and returns it to body 03/05/2011 46
Hemodialysis 3 -4 times a week Takes 2 -4 hours Machine filters blood and returns it to body 03/05/2011 46
 Chronic Renal Failure Hemodialysis Vascular access Temporary – subclavian or femoral Permanent – shunt, in arm Care post insertion Can be done rapidly Takes about 4 hours Done 3 x a week 03/05/2011 47
Chronic Renal Failure Hemodialysis Vascular access Temporary – subclavian or femoral Permanent – shunt, in arm Care post insertion Can be done rapidly Takes about 4 hours Done 3 x a week 03/05/2011 47
 Types of Access Temporary site: subclavian or femoral Permanent: shunt, in arm AV fistula Surgeon constructs by combining an artery and a vein 3 to 6 months to mature AV graft Man-made tube inserted by a surgeon to connect artery and vein 2 to 6 weeks to mature 03/05/2011 48
Types of Access Temporary site: subclavian or femoral Permanent: shunt, in arm AV fistula Surgeon constructs by combining an artery and a vein 3 to 6 months to mature AV graft Man-made tube inserted by a surgeon to connect artery and vein 2 to 6 weeks to mature 03/05/2011 48
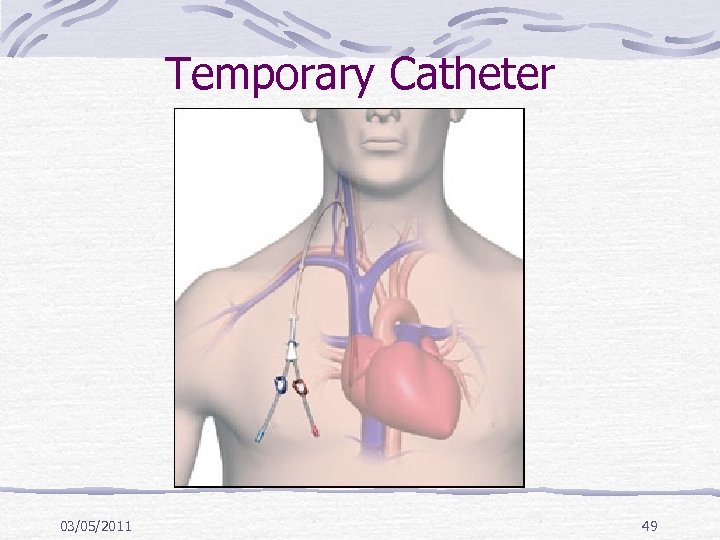 Temporary Catheter 03/05/2011 49
Temporary Catheter 03/05/2011 49
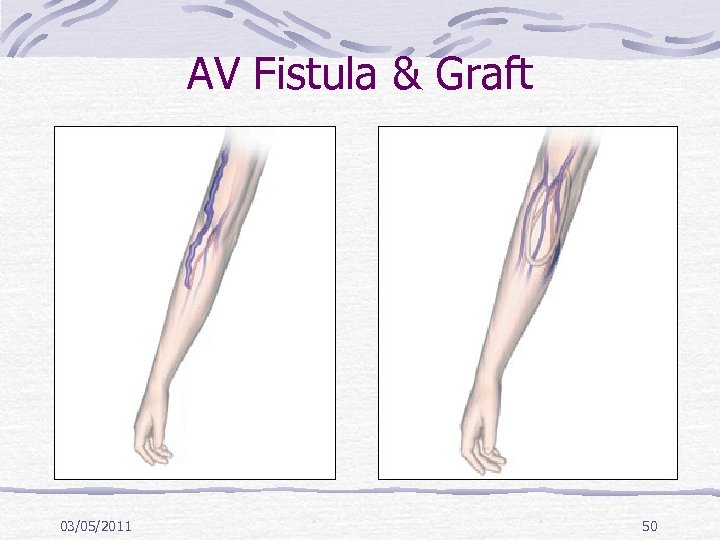 AV Fistula & Graft 03/05/2011 50
AV Fistula & Graft 03/05/2011 50
 What This Means For You No BP on same arm as fistula Protect arm from injury Control obvious hemorrhage Bleeding will be arterial Maintain direct pressure No IV on same arm as fistula A thrill will be felt – this is normal 03/05/2011 51
What This Means For You No BP on same arm as fistula Protect arm from injury Control obvious hemorrhage Bleeding will be arterial Maintain direct pressure No IV on same arm as fistula A thrill will be felt – this is normal 03/05/2011 51
 Access Problems AV graft thrombosis AV fistula or graft bleeding AV graft infection Steal Phenomenon: also called subclavian steal syndrome (SSS), or subclavian steal steno-occlusive disease, is a constellation of signs and symptoms that arise from retrograde (reversed) flow of blood in the vertebral artery or the internal thoracic artery, due to a proximal stenosis (narrowing) and/or occlusion of the subclavian artery. Early post-op Ischemic distally Apply small amount of pressure to reverse symptoms 03/05/2011 52
Access Problems AV graft thrombosis AV fistula or graft bleeding AV graft infection Steal Phenomenon: also called subclavian steal syndrome (SSS), or subclavian steal steno-occlusive disease, is a constellation of signs and symptoms that arise from retrograde (reversed) flow of blood in the vertebral artery or the internal thoracic artery, due to a proximal stenosis (narrowing) and/or occlusion of the subclavian artery. Early post-op Ischemic distally Apply small amount of pressure to reverse symptoms 03/05/2011 52
 Nursing Considerations Make sure the dressing remains intact Do not push or pull on the catheter Do not disconnect any of the catheters Always transport the patient and bags/catheters as one piece Never inject anything into catheter 03/05/2011 53
Nursing Considerations Make sure the dressing remains intact Do not push or pull on the catheter Do not disconnect any of the catheters Always transport the patient and bags/catheters as one piece Never inject anything into catheter 03/05/2011 53
 Dialysis Related Problems Lightheaded –give fluids Hypotension Dysrhythmias Disequilibration Syndrome At end of early sessions Confusion, tremor, seizure Due to decrease concentration of blood versus brain leading to cerebral edema 03/05/2011 54
Dialysis Related Problems Lightheaded –give fluids Hypotension Dysrhythmias Disequilibration Syndrome At end of early sessions Confusion, tremor, seizure Due to decrease concentration of blood versus brain leading to cerebral edema 03/05/2011 54
 Chronic Renal Failure Transplant Must find donor Waiting period long Good survival rate – 1 year 95 -97% Must take immunosuppressant’s for life Rejection Watch for fever, elevated B/P, and pain over site of new kidney 03/05/2011 55
Chronic Renal Failure Transplant Must find donor Waiting period long Good survival rate – 1 year 95 -97% Must take immunosuppressant’s for life Rejection Watch for fever, elevated B/P, and pain over site of new kidney 03/05/2011 55
 End-Stage Renal Disease Slow, insidious process Final stage is end-stage renal disease Increasing in incidence Diabetic nephropathy and hypertension are leading causes in U. S. 03/05/2011 56
End-Stage Renal Disease Slow, insidious process Final stage is end-stage renal disease Increasing in incidence Diabetic nephropathy and hypertension are leading causes in U. S. 03/05/2011 56
 End-Stage Renal Disease Nephrons destroyed by disease process Remaining nephrons hypertrophy and have increased workload Can compensate for a while Renal insufficiency develops Further insult leads to ESRD Uremia develops 03/05/2011 57
End-Stage Renal Disease Nephrons destroyed by disease process Remaining nephrons hypertrophy and have increased workload Can compensate for a while Renal insufficiency develops Further insult leads to ESRD Uremia develops 03/05/2011 57
 End-Stage Renal Disease Manifestations Often not identified until uremia develops Nausea Apathy Weakness Fatigue Confusion 03/05/2011 58
End-Stage Renal Disease Manifestations Often not identified until uremia develops Nausea Apathy Weakness Fatigue Confusion 03/05/2011 58
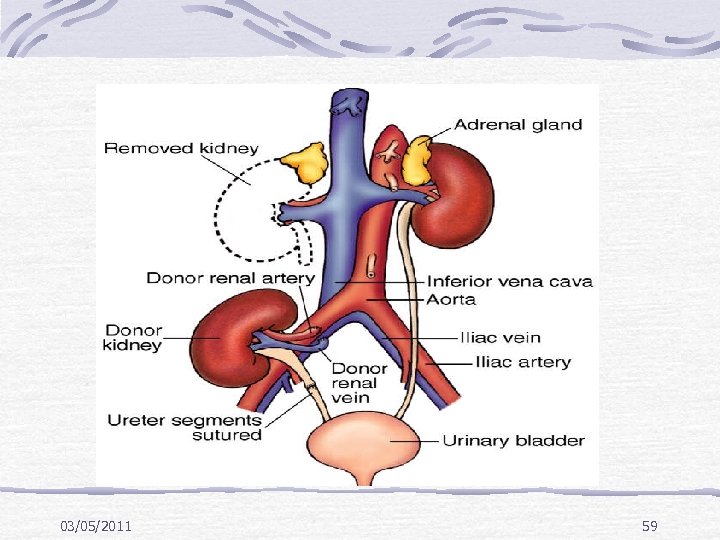 03/05/2011 59
03/05/2011 59
 Chronic Renal Failure Post op care ICU I/O B/P Weight changes Electrolytes May have fluid volume deficit High risk for infection 03/05/2011 60
Chronic Renal Failure Post op care ICU I/O B/P Weight changes Electrolytes May have fluid volume deficit High risk for infection 03/05/2011 60
 Transplant Meds Patients have decreased resistance to infection Corticosteroids – anti-inflammarory Deltosone Medrol Solu-Medrol Cytotoxic – inhibit T and B lymphocytes Imuran Cytoxan Cellcept T-cell depressors - Cyclosporin 03/05/2011 61
Transplant Meds Patients have decreased resistance to infection Corticosteroids – anti-inflammarory Deltosone Medrol Solu-Medrol Cytotoxic – inhibit T and B lymphocytes Imuran Cytoxan Cellcept T-cell depressors - Cyclosporin 03/05/2011 61
 Obstructive Renal Disorders 03/05/2011 62
Obstructive Renal Disorders 03/05/2011 62
 Hydronephrosis, Hydroureter, and Urethral Stricture Outflow obstruction Urethral stricture Causes bladder distention and progresses to the ureters and the kidneys Hydronephrosis – Kidney enlarges as urine collects in the pelvis and kidney tissue due to obstruction in the outflow tract Over a few hours this enlargement can damage the blood vessels and the tubules Hydroureter Effects are similar, but occurs lower in the ureter 03/05/2011 63
Hydronephrosis, Hydroureter, and Urethral Stricture Outflow obstruction Urethral stricture Causes bladder distention and progresses to the ureters and the kidneys Hydronephrosis – Kidney enlarges as urine collects in the pelvis and kidney tissue due to obstruction in the outflow tract Over a few hours this enlargement can damage the blood vessels and the tubules Hydroureter Effects are similar, but occurs lower in the ureter 03/05/2011 63
 Causes of Obstruction Tumor Stones Congenital structural defects Fibrosis Treatment with radiation in pelvis 03/05/2011 64
Causes of Obstruction Tumor Stones Congenital structural defects Fibrosis Treatment with radiation in pelvis 03/05/2011 64
 Complication of Obstruction If untreated, permanent damage can occur within 48 hours Renal failure Retention of Nitrogenous wastes (urea, creatinine, uric acid) Electrolytes (K, Na, Cl, and Phosphorus) Acid base balance impaired 03/05/2011 65
Complication of Obstruction If untreated, permanent damage can occur within 48 hours Renal failure Retention of Nitrogenous wastes (urea, creatinine, uric acid) Electrolytes (K, Na, Cl, and Phosphorus) Acid base balance impaired 03/05/2011 65
 Renal Calculi Called nephrolithiasis or urolithiasis Most commonly develop in the renal pelvis but can be anywhere in the urinary tract Vary in size –from very large to tiny Can be 1 stone or many stones May stay in kidney or travel into the ureter Can damage the urinary tract May cause hydronephrosis More common in white males 30 -50 years of age 03/05/2011 66
Renal Calculi Called nephrolithiasis or urolithiasis Most commonly develop in the renal pelvis but can be anywhere in the urinary tract Vary in size –from very large to tiny Can be 1 stone or many stones May stay in kidney or travel into the ureter Can damage the urinary tract May cause hydronephrosis More common in white males 30 -50 years of age 03/05/2011 66
 Renal Calculi Predisposing factors Dehydration Prolonged immobilization Infection Obstruction Anything which causes the urine to be alkaline Metabolic factors Excessive intake of calcium, calcium based antacids or Vit D Hyperthyroidism Elevated uric acid 03/05/2011 67
Renal Calculi Predisposing factors Dehydration Prolonged immobilization Infection Obstruction Anything which causes the urine to be alkaline Metabolic factors Excessive intake of calcium, calcium based antacids or Vit D Hyperthyroidism Elevated uric acid 03/05/2011 67
 Renal Calculi Subjective symptoms Sever pain in the flank area, suprapubic area, pelvis or external genitalia If in ureter, may have spasms called “renal colic” Urgency, frequency of urination N/V Chills 03/05/2011 68
Renal Calculi Subjective symptoms Sever pain in the flank area, suprapubic area, pelvis or external genitalia If in ureter, may have spasms called “renal colic” Urgency, frequency of urination N/V Chills 03/05/2011 68
 Renal Calculi Objective symptoms Increased temperature Pallor Hematuria Abdominal distention Pyuria Anuria May have UTI on urinalysis 03/05/2011 69
Renal Calculi Objective symptoms Increased temperature Pallor Hematuria Abdominal distention Pyuria Anuria May have UTI on urinalysis 03/05/2011 69
 Renal Calculi- Manifestations Kidney/Pelvis May be asymptomatic Dull, aching flank pain Ureter Acute severe flank pain, may radiate Nausea/vomiting Pallor Hematuria 03/05/2011 70
Renal Calculi- Manifestations Kidney/Pelvis May be asymptomatic Dull, aching flank pain Ureter Acute severe flank pain, may radiate Nausea/vomiting Pallor Hematuria 03/05/2011 70
 Renal Calculi- Manifestations Bladder May be asymptomatic Dull suprapubic pain Hematuria 03/05/2011 71
Renal Calculi- Manifestations Bladder May be asymptomatic Dull suprapubic pain Hematuria 03/05/2011 71
 Renal Calculi Diagnostic procedures Urinalysis with C and S 24 hour urine KUB IVP Renal CT Kidney ultrasound Cystoscopy with retrograde pyleogram 03/05/2011 72
Renal Calculi Diagnostic procedures Urinalysis with C and S 24 hour urine KUB IVP Renal CT Kidney ultrasound Cystoscopy with retrograde pyleogram 03/05/2011 72
 Renal Calculi Treatment Most are passed without intervention May need cysto with basket retrieval Lithotripsy : Extracorporeal shock wave lithotripsy (ESWL) is the non-invasive treatment of kidney stones (urinary calculosis) and biliary calculi (stones in the gallbladder or in the liver) using an acoustic pulse. Lasertripsy : Lithotomy: is a surgical method for removal of calculi, stones formed inside certain hollow organs, such as the bladder and kidneys (urinary calculus) and gallbladder (gallstones), that cannot exit naturally through the urethra, ureter or biliary duct 03/05/2011 73
Renal Calculi Treatment Most are passed without intervention May need cysto with basket retrieval Lithotripsy : Extracorporeal shock wave lithotripsy (ESWL) is the non-invasive treatment of kidney stones (urinary calculosis) and biliary calculi (stones in the gallbladder or in the liver) using an acoustic pulse. Lasertripsy : Lithotomy: is a surgical method for removal of calculi, stones formed inside certain hollow organs, such as the bladder and kidneys (urinary calculus) and gallbladder (gallstones), that cannot exit naturally through the urethra, ureter or biliary duct 03/05/2011 73
 Renal Calculi Assessment History and physical exam Location, severity, and nature of pain I/O Vital signs, looking for fever Palpation of flank area, and abdomen ? N/V 03/05/2011 74
Renal Calculi Assessment History and physical exam Location, severity, and nature of pain I/O Vital signs, looking for fever Palpation of flank area, and abdomen ? N/V 03/05/2011 74
 Renal Calculi Nursing interventions Primary is to treat pain – usually with opioids Ambulate Force fluids, may have IV Watch for fluid overload Strain urine – send stone to lab if passed Accurate I/O Medicate N/V 03/05/2011 75
Renal Calculi Nursing interventions Primary is to treat pain – usually with opioids Ambulate Force fluids, may have IV Watch for fluid overload Strain urine – send stone to lab if passed Accurate I/O Medicate N/V 03/05/2011 75
 Renal Calculi Surgical removal Routine pre and post op care May return with catheter, drains, nephrostomy tube and ureteral stent – must maintain patency and may need to irrigate as ordered Measure drainage from all tubes – need at least 30 cc/hr Watch site for bleeding May need frequent dressing changes due to fluid leakage, or may have collection bag 03/05/2011 76
Renal Calculi Surgical removal Routine pre and post op care May return with catheter, drains, nephrostomy tube and ureteral stent – must maintain patency and may need to irrigate as ordered Measure drainage from all tubes – need at least 30 cc/hr Watch site for bleeding May need frequent dressing changes due to fluid leakage, or may have collection bag 03/05/2011 76
 Renal Calculi Discharge and prevention Continue to force fluids post discharge May need special diet Stones are analyzed for calcium or other minerals May need to watch products with calcium 03/05/2011 77
Renal Calculi Discharge and prevention Continue to force fluids post discharge May need special diet Stones are analyzed for calcium or other minerals May need to watch products with calcium 03/05/2011 77


