94a8be7ea7bdc488b794ea445cff6338.ppt
- Количество слайдов: 77
 MEDICAL GRANDROUNDS SUWENDI, M. D. Medicine Resident January 11, 2007 Ledesma Hall Makati Medical Center
MEDICAL GRANDROUNDS SUWENDI, M. D. Medicine Resident January 11, 2007 Ledesma Hall Makati Medical Center
 OBJECTIVES To present a case of infection in an immunocompromised host To be able to do a thorough evaluation of an immunocompromised patient with persistent cough To discuss the pathogenesis, clinical manifestations, diagnosis and management of an immunocompromised patient with Aspergillosis
OBJECTIVES To present a case of infection in an immunocompromised host To be able to do a thorough evaluation of an immunocompromised patient with persistent cough To discuss the pathogenesis, clinical manifestations, diagnosis and management of an immunocompromised patient with Aspergillosis
 GENERAL DATA Z. C. 47 y/o, female single Filipino business woman
GENERAL DATA Z. C. 47 y/o, female single Filipino business woman
 CHIEF COMPLAINT Pancytopenia
CHIEF COMPLAINT Pancytopenia
 HISTORY OF PRESENT ILLNESS 6 months PTA pallor easy bruisability generalized body weakness
HISTORY OF PRESENT ILLNESS 6 months PTA pallor easy bruisability generalized body weakness
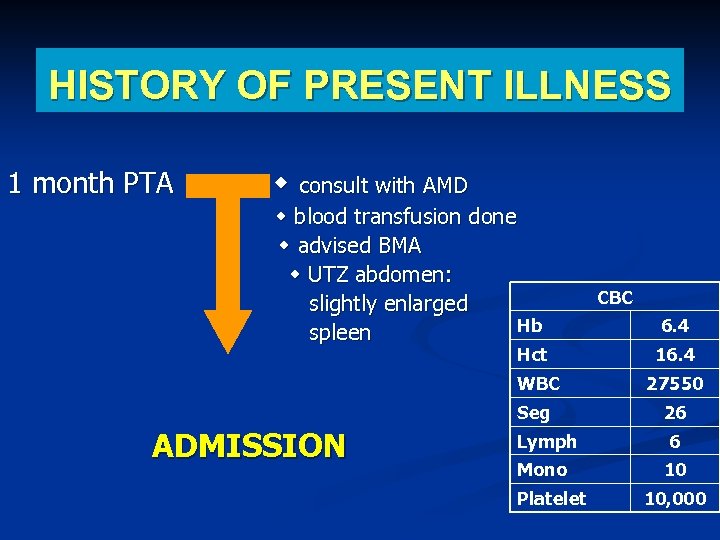 HISTORY OF PRESENT ILLNESS 1 month PTA consult with AMD blood transfusion done advised BMA UTZ abdomen: slightly enlarged Hb spleen Hct CBC 6. 4 16. 4 WBC Seg ADMISSION 27550 26 Lymph Mono Platelet 6 10 10, 000
HISTORY OF PRESENT ILLNESS 1 month PTA consult with AMD blood transfusion done advised BMA UTZ abdomen: slightly enlarged Hb spleen Hct CBC 6. 4 16. 4 WBC Seg ADMISSION 27550 26 Lymph Mono Platelet 6 10 10, 000
 REVIEW OF SYSTEMS (-) fever (-) cough/colds (-) weight loss (-) nausea/vomiting (-) difficulty of breathing (-) chest pain (-) urinary or bowel changes (-) hematochezia / melena
REVIEW OF SYSTEMS (-) fever (-) cough/colds (-) weight loss (-) nausea/vomiting (-) difficulty of breathing (-) chest pain (-) urinary or bowel changes (-) hematochezia / melena
 PAST MEDICAL HISTORY (-) Hypertension (-) Diabetes mellitus (-) Bronchial asthma (+) Hyperthyroidism (2003) -no maintenance medications (-) history of previous operations (-) food / drug allergies
PAST MEDICAL HISTORY (-) Hypertension (-) Diabetes mellitus (-) Bronchial asthma (+) Hyperthyroidism (2003) -no maintenance medications (-) history of previous operations (-) food / drug allergies
 FAMILY MEDICAL HISTORY (-) Hypertension (-) Diabetes mellitus (+) Chronic kidney disease & PTB – father (deceased) (-) Blood dyscrasias
FAMILY MEDICAL HISTORY (-) Hypertension (-) Diabetes mellitus (+) Chronic kidney disease & PTB – father (deceased) (-) Blood dyscrasias
 PERSONAL / SOCIAL HISTORY Non-alcoholic beverage drinker Non-smoker denies illicit drug use nor environmental exposure to chemicals
PERSONAL / SOCIAL HISTORY Non-alcoholic beverage drinker Non-smoker denies illicit drug use nor environmental exposure to chemicals
 PHYSICAL EXAMINATION conscious, coherent, ambulatory BP 110/70, CR 112 bpm, RR 22 cpm, Temp. 37. 2 C Good skin turgor, no jaundice, no petechial rashes Pale palpebral conjunctivae, anicteric sclerae Supple neck, no cervical lymphadenopathies
PHYSICAL EXAMINATION conscious, coherent, ambulatory BP 110/70, CR 112 bpm, RR 22 cpm, Temp. 37. 2 C Good skin turgor, no jaundice, no petechial rashes Pale palpebral conjunctivae, anicteric sclerae Supple neck, no cervical lymphadenopathies
 PHYSICAL EXAMINATION Symmetrical chest expansion, no retractions, clear breath sounds Adynamic precordium, AB 5 th LICS MCL, tachycardic, regular rate and rhythm, no murmurs Soft, flat abdomen, normoactive bowel sounds, non tender, no hepatosplenomegaly Extremities : no edema, no cyanosis, pulses full and equal
PHYSICAL EXAMINATION Symmetrical chest expansion, no retractions, clear breath sounds Adynamic precordium, AB 5 th LICS MCL, tachycardic, regular rate and rhythm, no murmurs Soft, flat abdomen, normoactive bowel sounds, non tender, no hepatosplenomegaly Extremities : no edema, no cyanosis, pulses full and equal
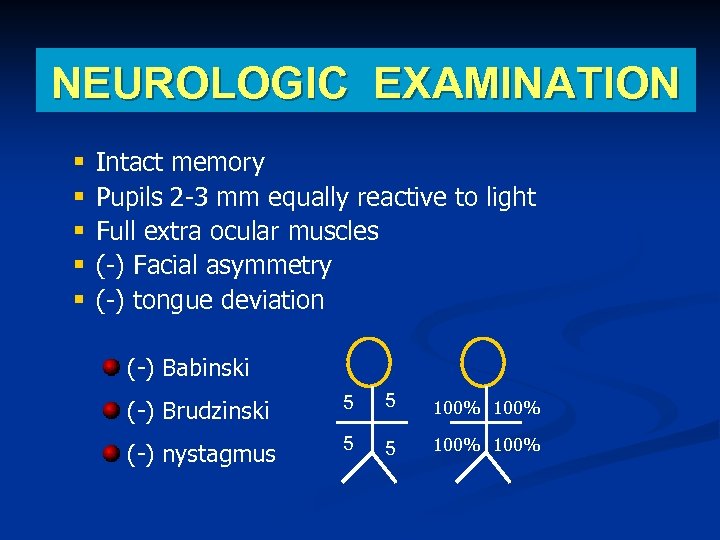 NEUROLOGIC EXAMINATION § § § Intact memory Pupils 2 -3 mm equally reactive to light Full extra ocular muscles (-) Facial asymmetry (-) tongue deviation (-) Babinski (-) Brudzinski 5 5 100% (-) nystagmus 5 5 100%
NEUROLOGIC EXAMINATION § § § Intact memory Pupils 2 -3 mm equally reactive to light Full extra ocular muscles (-) Facial asymmetry (-) tongue deviation (-) Babinski (-) Brudzinski 5 5 100% (-) nystagmus 5 5 100%
 SALIENT FEATURES 47 y. o. , female Pallor, easy bruisability & generalized body weakness Ultrasound finding: slightly enlarged spleen Pancytopenia on CBC
SALIENT FEATURES 47 y. o. , female Pallor, easy bruisability & generalized body weakness Ultrasound finding: slightly enlarged spleen Pancytopenia on CBC
 ADMITTING IMPRESSION Pancytopenia R/o blood dyscrasia
ADMITTING IMPRESSION Pancytopenia R/o blood dyscrasia
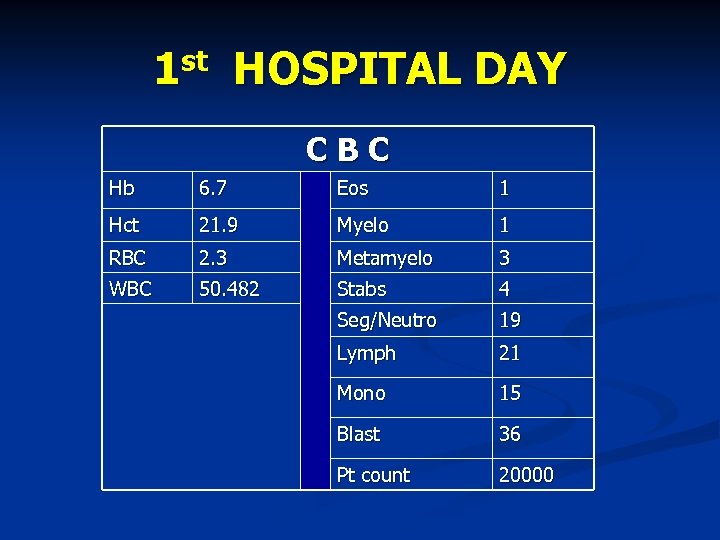 1 st HOSPITAL DAY CBC Hb 6. 7 Eos 1 Hct 21. 9 Myelo 1 RBC 2. 3 Metamyelo 3 WBC 50. 482 Stabs 4 Seg/Neutro 19 Lymph 21 Mono 15 Blast 36 Pt count 20000
1 st HOSPITAL DAY CBC Hb 6. 7 Eos 1 Hct 21. 9 Myelo 1 RBC 2. 3 Metamyelo 3 WBC 50. 482 Stabs 4 Seg/Neutro 19 Lymph 21 Mono 15 Blast 36 Pt count 20000
 1 st HOSPITAL DAY Tranfused 2 unit of PRBC & 4 units of platelet concentrate
1 st HOSPITAL DAY Tranfused 2 unit of PRBC & 4 units of platelet concentrate
 nd 2 HOSPITAL DAY Bone Marrow Aspiration Biopsy : • myeloblastosis with minimal maturation with predominantly dysplastic and megaloblastic erythroid
nd 2 HOSPITAL DAY Bone Marrow Aspiration Biopsy : • myeloblastosis with minimal maturation with predominantly dysplastic and megaloblastic erythroid
 2 nd HOSPITAL DAY Bone Marrow Aspiration Biopsy : • The rest of the hematopoetic cells shows unremarkable morphology: lymp (5, 18%) , mono(0. 52%) , plasma cells (0. 52%), macrophages (1. 55%) and megakaryocytes (0. 0%) • Histopathological Diagnosis : ACUTE MYELOGENOUS LEUKEMIA
2 nd HOSPITAL DAY Bone Marrow Aspiration Biopsy : • The rest of the hematopoetic cells shows unremarkable morphology: lymp (5, 18%) , mono(0. 52%) , plasma cells (0. 52%), macrophages (1. 55%) and megakaryocytes (0. 0%) • Histopathological Diagnosis : ACUTE MYELOGENOUS LEUKEMIA
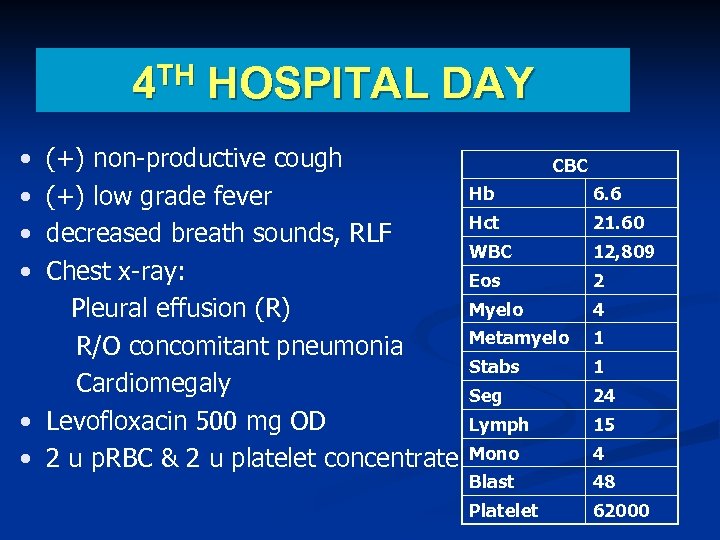 4 TH HOSPITAL DAY • • (+) non-productive cough (+) low grade fever decreased breath sounds, RLF Chest x-ray: Pleural effusion (R) R/O concomitant pneumonia Cardiomegaly • Levofloxacin 500 mg OD • 2 u p. RBC & 2 u platelet concentrate CBC Hb 6. 6 Hct 21. 60 WBC 12, 809 Eos 2 Myelo 4 Metamyelo 1 Stabs 1 Seg 24 Lymph 15 Mono 4 Blast 48 Platelet 62000
4 TH HOSPITAL DAY • • (+) non-productive cough (+) low grade fever decreased breath sounds, RLF Chest x-ray: Pleural effusion (R) R/O concomitant pneumonia Cardiomegaly • Levofloxacin 500 mg OD • 2 u p. RBC & 2 u platelet concentrate CBC Hb 6. 6 Hct 21. 60 WBC 12, 809 Eos 2 Myelo 4 Metamyelo 1 Stabs 1 Seg 24 Lymph 15 Mono 4 Blast 48 Platelet 62000
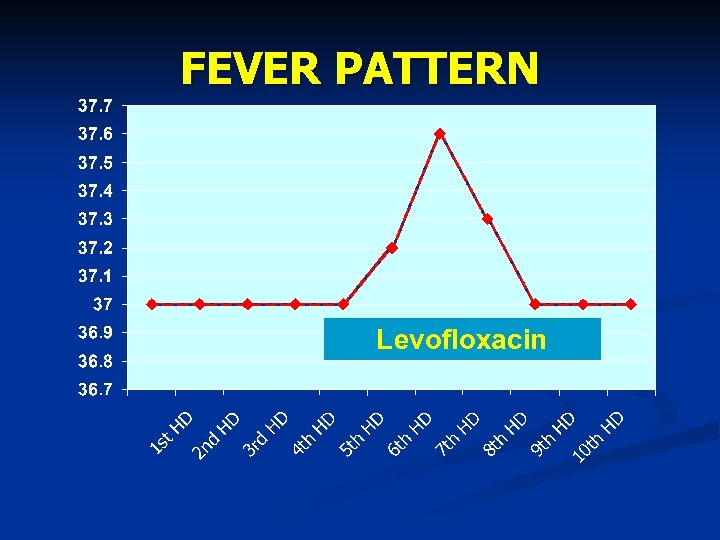 FEVER PATTERN Levofloxacin
FEVER PATTERN Levofloxacin
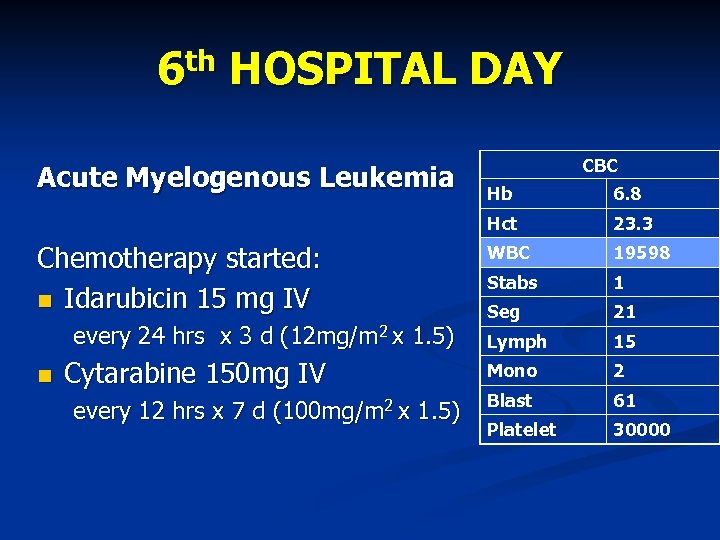 6 th HOSPITAL DAY Acute Myelogenous Leukemia CBC every 24 hrs x 3 d (12 mg/m 2 x 1. 5) Cytarabine 150 mg IV every 12 hrs x 7 d (100 mg/m 2 x 1. 5) 6. 8 Hct Chemotherapy started: Idarubicin 15 mg IV Hb 23. 3 WBC 19598 Stabs 1 Seg 21 Lymph 15 Mono 2 Blast 61 Platelet 30000
6 th HOSPITAL DAY Acute Myelogenous Leukemia CBC every 24 hrs x 3 d (12 mg/m 2 x 1. 5) Cytarabine 150 mg IV every 12 hrs x 7 d (100 mg/m 2 x 1. 5) 6. 8 Hct Chemotherapy started: Idarubicin 15 mg IV Hb 23. 3 WBC 19598 Stabs 1 Seg 21 Lymph 15 Mono 2 Blast 61 Platelet 30000
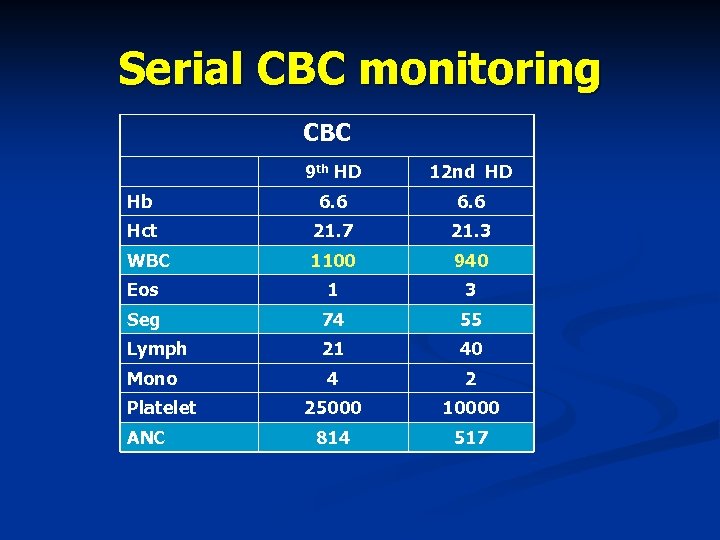 Serial CBC monitoring CBC 9 th HD 12 nd HD Hb 6. 6 Hct 21. 7 21. 3 WBC 1100 940 Eos 1 3 Seg 74 55 Lymph 21 40 4 2 25000 10000 814 517 Mono Platelet ANC
Serial CBC monitoring CBC 9 th HD 12 nd HD Hb 6. 6 Hct 21. 7 21. 3 WBC 1100 940 Eos 1 3 Seg 74 55 Lymph 21 40 4 2 25000 10000 814 517 Mono Platelet ANC
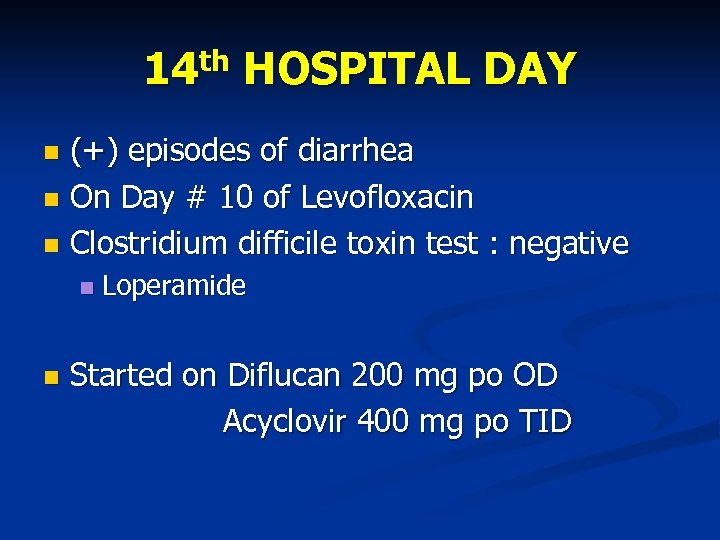 14 th HOSPITAL DAY (+) episodes of diarrhea On Day # 10 of Levofloxacin Clostridium difficile toxin test : negative Loperamide Started on Diflucan 200 mg po OD Acyclovir 400 mg po TID
14 th HOSPITAL DAY (+) episodes of diarrhea On Day # 10 of Levofloxacin Clostridium difficile toxin test : negative Loperamide Started on Diflucan 200 mg po OD Acyclovir 400 mg po TID
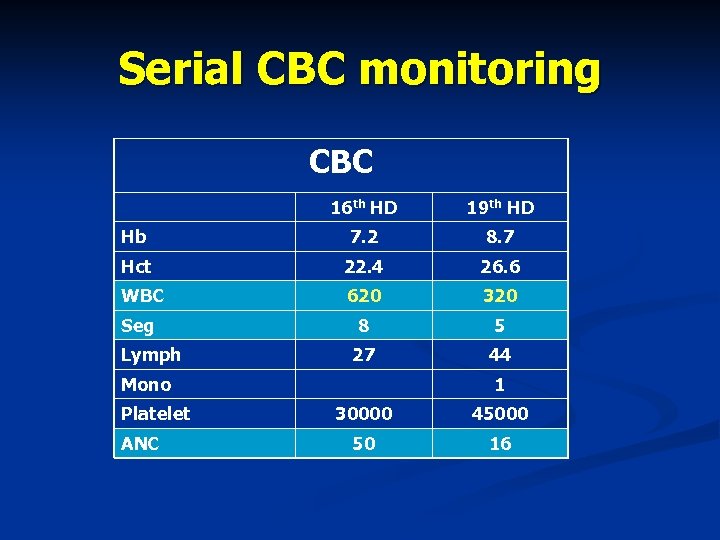 Serial CBC monitoring CBC 16 th HD 19 th HD Hb 7. 2 8. 7 Hct 22. 4 26. 6 WBC 620 320 Seg 8 5 27 44 Lymph Mono Platelet ANC 1 30000 45000 50 16
Serial CBC monitoring CBC 16 th HD 19 th HD Hb 7. 2 8. 7 Hct 22. 4 26. 6 WBC 620 320 Seg 8 5 27 44 Lymph Mono Platelet ANC 1 30000 45000 50 16
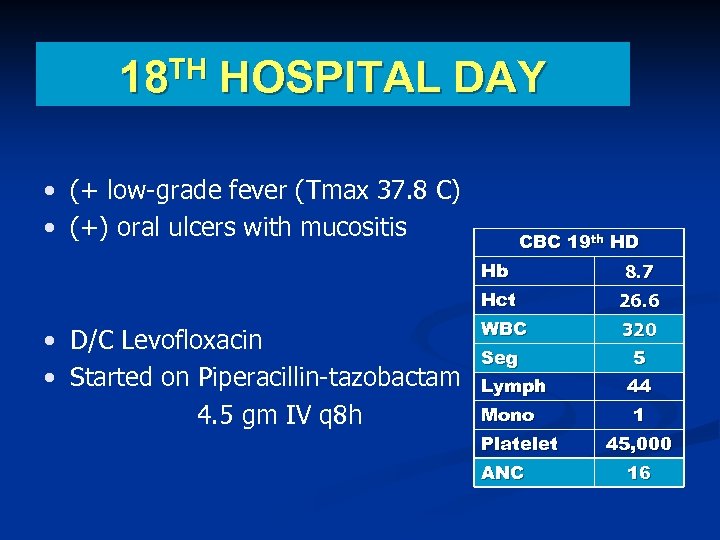 TH 18 HOSPITAL DAY • (+ low-grade fever (Tmax 37. 8 C) • (+) oral ulcers with mucositis CBC 19 th HD Hb Hct • D/C Levofloxacin • Started on Piperacillin-tazobactam 4. 5 gm IV q 8 h 8. 7 26. 6 WBC Seg 320 5 Lymph 44 Mono Platelet ANC 1 45, 000 16
TH 18 HOSPITAL DAY • (+ low-grade fever (Tmax 37. 8 C) • (+) oral ulcers with mucositis CBC 19 th HD Hb Hct • D/C Levofloxacin • Started on Piperacillin-tazobactam 4. 5 gm IV q 8 h 8. 7 26. 6 WBC Seg 320 5 Lymph 44 Mono Platelet ANC 1 45, 000 16
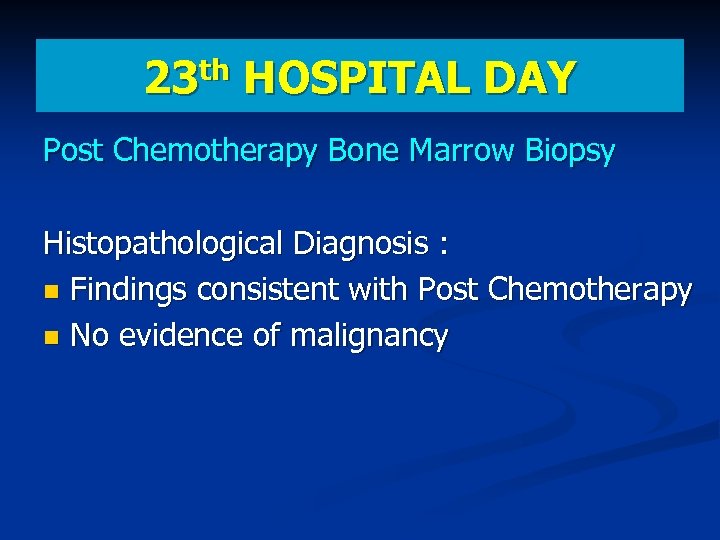 th 23 HOSPITAL DAY Post Chemotherapy Bone Marrow Biopsy Histopathological Diagnosis : Findings consistent with Post Chemotherapy No evidence of malignancy
th 23 HOSPITAL DAY Post Chemotherapy Bone Marrow Biopsy Histopathological Diagnosis : Findings consistent with Post Chemotherapy No evidence of malignancy
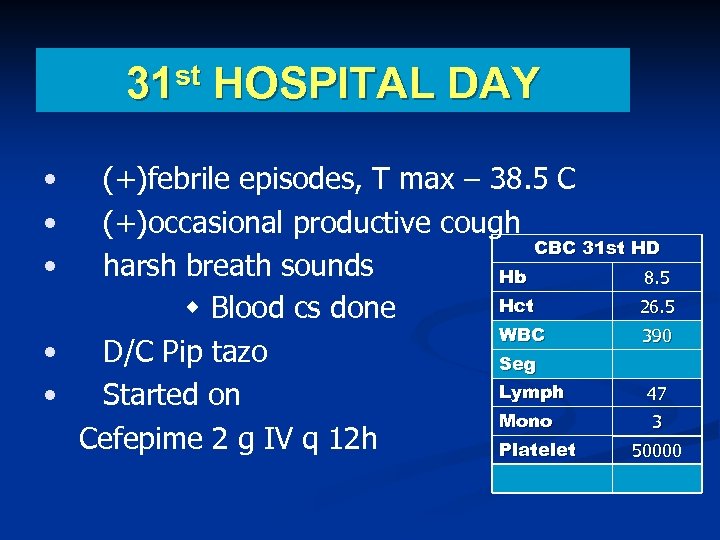 31 st HOSPITAL DAY • • • (+)febrile episodes, T max – 38. 5 C (+)occasional productive cough CBC 31 st HD harsh breath sounds Hb 8. 5 Hct 26. 5 Blood cs done WBC 390 • D/C Pip tazo Seg Lymph 47 • Started on Mono 3 Cefepime 2 g IV q 12 h Platelet 50000
31 st HOSPITAL DAY • • • (+)febrile episodes, T max – 38. 5 C (+)occasional productive cough CBC 31 st HD harsh breath sounds Hb 8. 5 Hct 26. 5 Blood cs done WBC 390 • D/C Pip tazo Seg Lymph 47 • Started on Mono 3 Cefepime 2 g IV q 12 h Platelet 50000
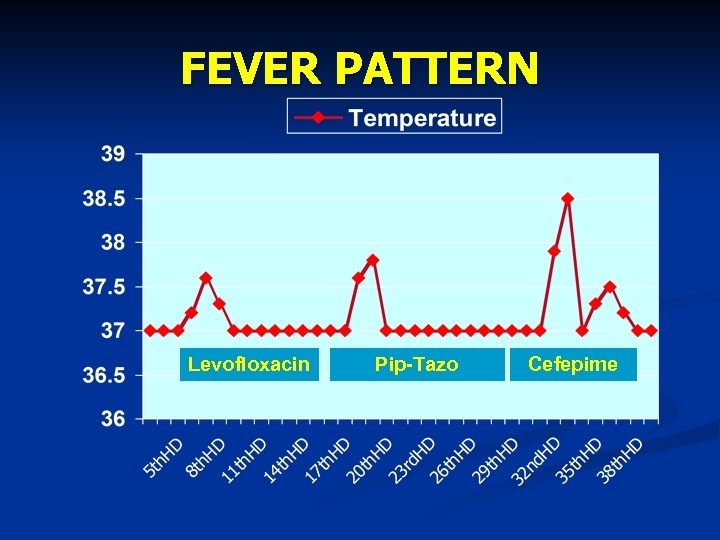 FEVER PATTERN Levofloxacin Pip-Tazo Cefepime
FEVER PATTERN Levofloxacin Pip-Tazo Cefepime
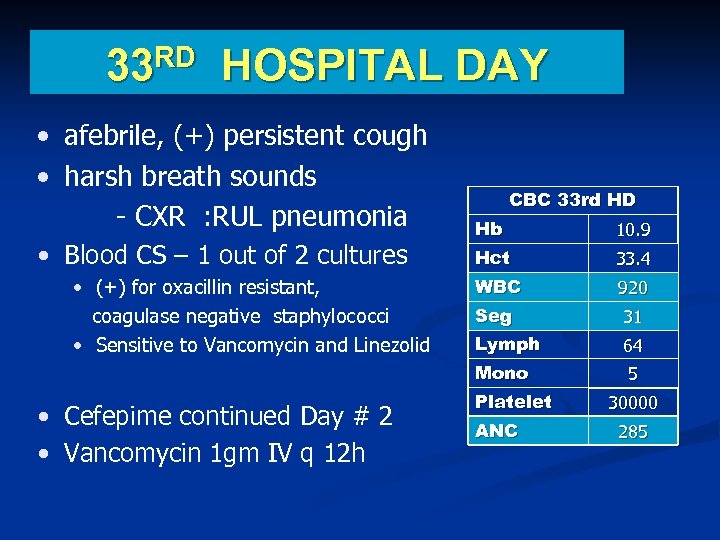 RD 33 HOSPITAL DAY • afebrile, (+) persistent cough • harsh breath sounds - CXR : RUL pneumonia CBC 33 rd HD • (+) for oxacillin resistant, coagulase negative staphylococci • Sensitive to Vancomycin and Linezolid • Cefepime continued Day # 2 • Vancomycin 1 gm IV q 12 h 10. 9 Hct 33. 4 WBC 920 Seg 31 Lymph 64 Mono • Blood CS – 1 out of 2 cultures Hb 5 Platelet ANC 30000 285
RD 33 HOSPITAL DAY • afebrile, (+) persistent cough • harsh breath sounds - CXR : RUL pneumonia CBC 33 rd HD • (+) for oxacillin resistant, coagulase negative staphylococci • Sensitive to Vancomycin and Linezolid • Cefepime continued Day # 2 • Vancomycin 1 gm IV q 12 h 10. 9 Hct 33. 4 WBC 920 Seg 31 Lymph 64 Mono • Blood CS – 1 out of 2 cultures Hb 5 Platelet ANC 30000 285
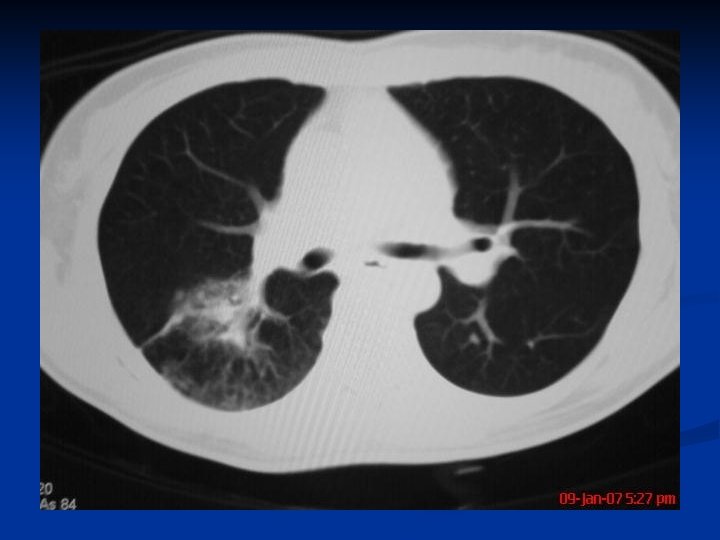
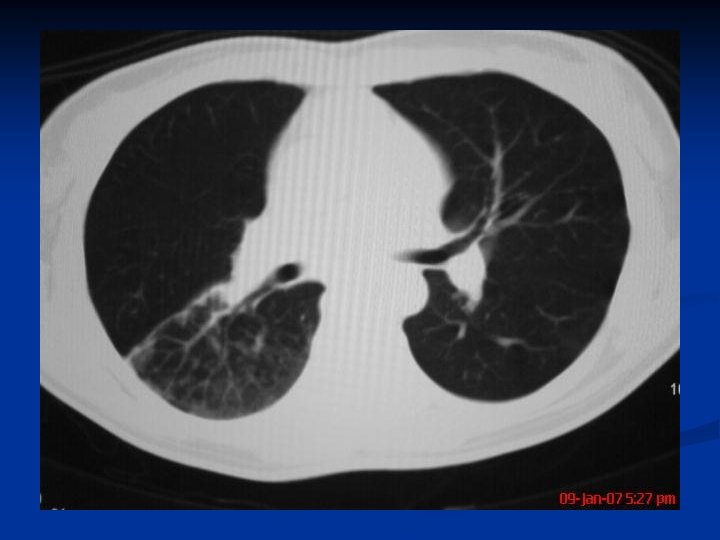
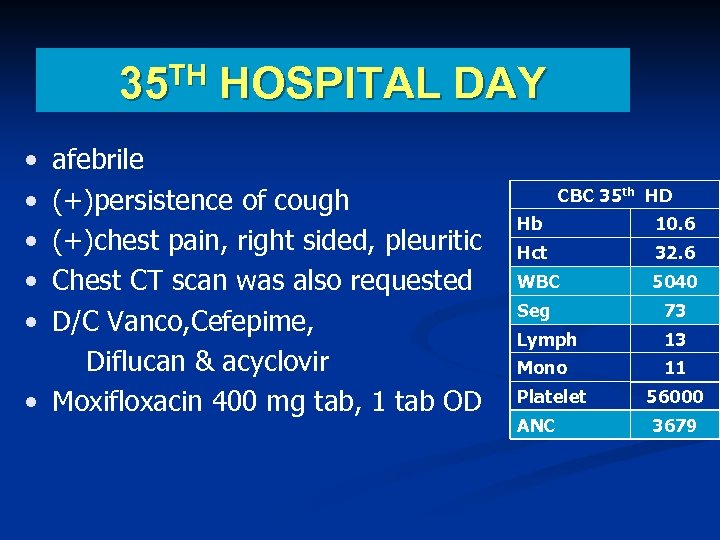 35 TH HOSPITAL DAY • • • afebrile (+)persistence of cough (+)chest pain, right sided, pleuritic Chest CT scan was also requested D/C Vanco, Cefepime, Diflucan & acyclovir • Moxifloxacin 400 mg tab, 1 tab OD CBC 35 th HD Hb 10. 6 Hct 32. 6 WBC 5040 Seg 73 Lymph 13 Mono 11 Platelet ANC 56000 3679
35 TH HOSPITAL DAY • • • afebrile (+)persistence of cough (+)chest pain, right sided, pleuritic Chest CT scan was also requested D/C Vanco, Cefepime, Diflucan & acyclovir • Moxifloxacin 400 mg tab, 1 tab OD CBC 35 th HD Hb 10. 6 Hct 32. 6 WBC 5040 Seg 73 Lymph 13 Mono 11 Platelet ANC 56000 3679
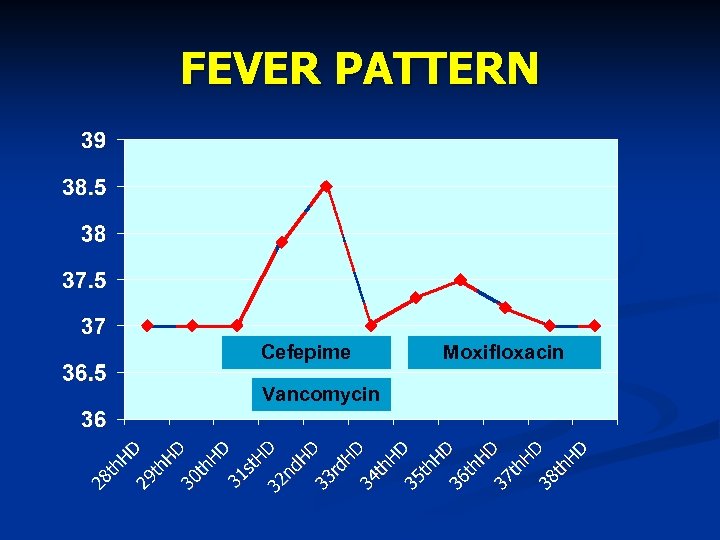 FEVER PATTERN Cefepime Vancomycin Moxifloxacin
FEVER PATTERN Cefepime Vancomycin Moxifloxacin
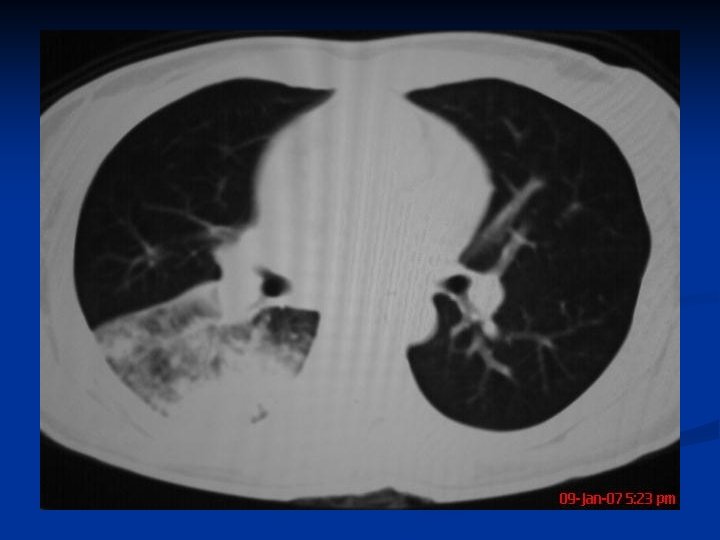
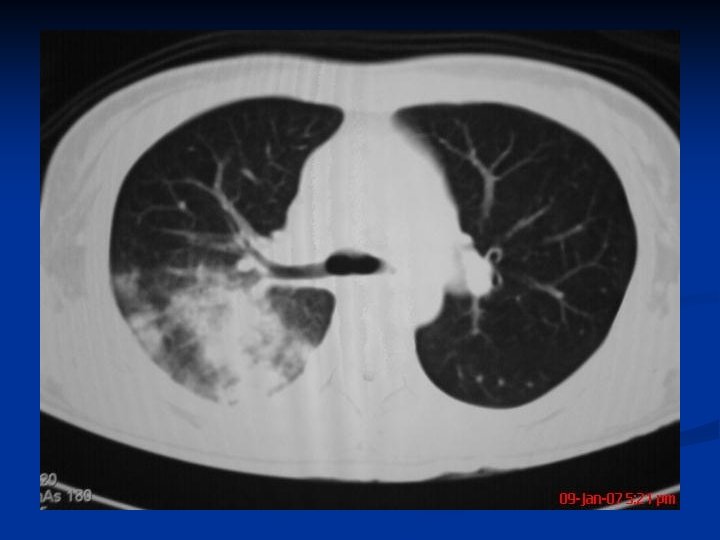
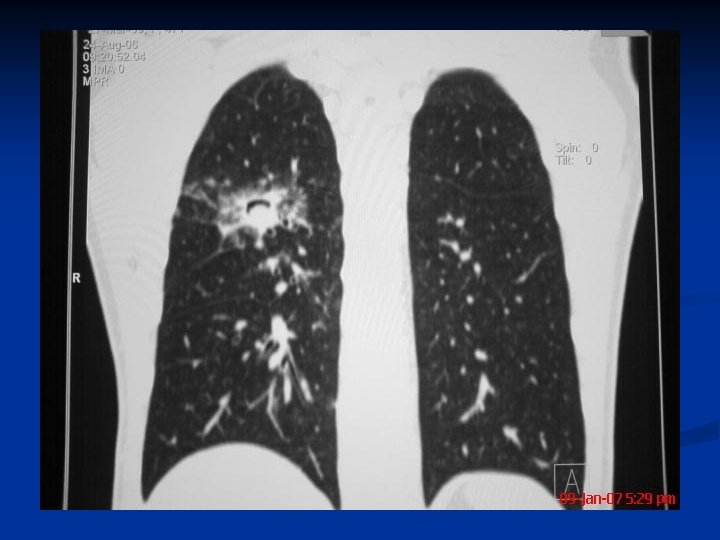
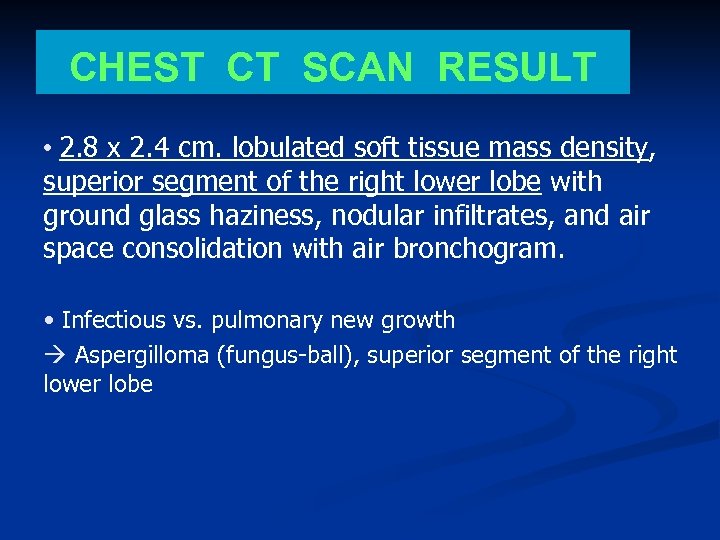 CHEST CT SCAN RESULT • 2. 8 x 2. 4 cm. lobulated soft tissue mass density, superior segment of the right lower lobe with ground glass haziness, nodular infiltrates, and air space consolidation with air bronchogram. • Infectious vs. pulmonary new growth à Aspergilloma (fungus-ball), superior segment of the right lower lobe
CHEST CT SCAN RESULT • 2. 8 x 2. 4 cm. lobulated soft tissue mass density, superior segment of the right lower lobe with ground glass haziness, nodular infiltrates, and air space consolidation with air bronchogram. • Infectious vs. pulmonary new growth à Aspergilloma (fungus-ball), superior segment of the right lower lobe

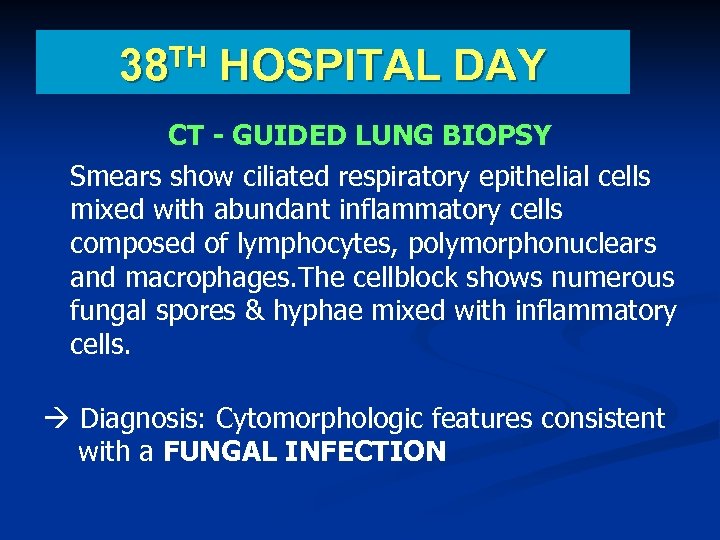 TH 38 HOSPITAL DAY CT - GUIDED LUNG BIOPSY Smears show ciliated respiratory epithelial cells mixed with abundant inflammatory cells composed of lymphocytes, polymorphonuclears and macrophages. The cellblock shows numerous fungal spores & hyphae mixed with inflammatory cells. à Diagnosis: Cytomorphologic features consistent with a FUNGAL INFECTION
TH 38 HOSPITAL DAY CT - GUIDED LUNG BIOPSY Smears show ciliated respiratory epithelial cells mixed with abundant inflammatory cells composed of lymphocytes, polymorphonuclears and macrophages. The cellblock shows numerous fungal spores & hyphae mixed with inflammatory cells. à Diagnosis: Cytomorphologic features consistent with a FUNGAL INFECTION
 th 38 HOSPITAL DAY CHEST X RAY No evidence of pneumothorax Patient was discharged pending CT guided lung aspirate culture results THM: Moxifloxacin 400 mg OD x 3 more days
th 38 HOSPITAL DAY CHEST X RAY No evidence of pneumothorax Patient was discharged pending CT guided lung aspirate culture results THM: Moxifloxacin 400 mg OD x 3 more days
 CT - GUIDED LUNG ASPIRATE : Light growth of Aspergillus spp.
CT - GUIDED LUNG ASPIRATE : Light growth of Aspergillus spp.
 FOLLOW UP TREATMENT Patient was started on Voriconazole 200 mg BID
FOLLOW UP TREATMENT Patient was started on Voriconazole 200 mg BID
 FOLLOW UP CT SCAN
FOLLOW UP CT SCAN
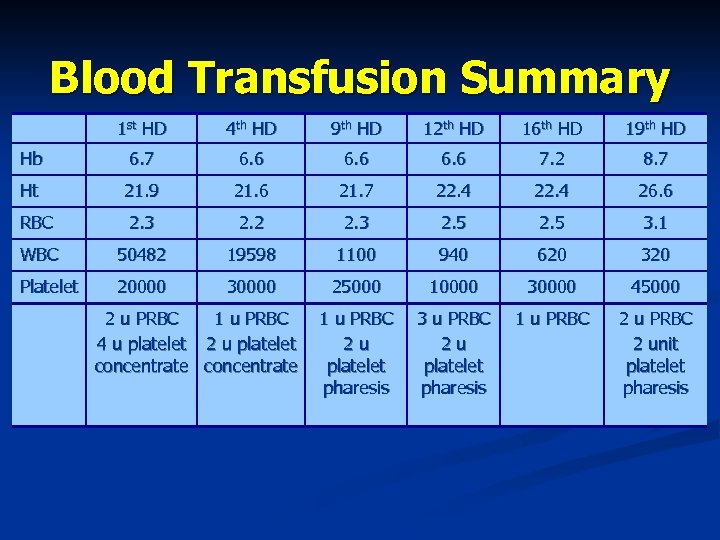 Blood Transfusion Summary 1 st HD 4 th HD 9 th HD 12 th HD 16 th HD 19 th HD Hb 6. 7 6. 6 7. 2 8. 7 Ht 21. 9 21. 6 21. 7 22. 4 26. 6 RBC 2. 3 2. 2 2. 3 2. 5 3. 1 WBC 50482 19598 1100 940 620 320 Platelet 20000 30000 25000 10000 30000 45000 1 u PRBC 2 u platelet pharesis 3 u PRBC 2 u platelet pharesis 1 u PRBC 2 unit platelet pharesis 2 u PRBC 1 u PRBC 4 u platelet 2 u platelet concentrate
Blood Transfusion Summary 1 st HD 4 th HD 9 th HD 12 th HD 16 th HD 19 th HD Hb 6. 7 6. 6 7. 2 8. 7 Ht 21. 9 21. 6 21. 7 22. 4 26. 6 RBC 2. 3 2. 2 2. 3 2. 5 3. 1 WBC 50482 19598 1100 940 620 320 Platelet 20000 30000 25000 10000 30000 45000 1 u PRBC 2 u platelet pharesis 3 u PRBC 2 u platelet pharesis 1 u PRBC 2 unit platelet pharesis 2 u PRBC 1 u PRBC 4 u platelet 2 u platelet concentrate
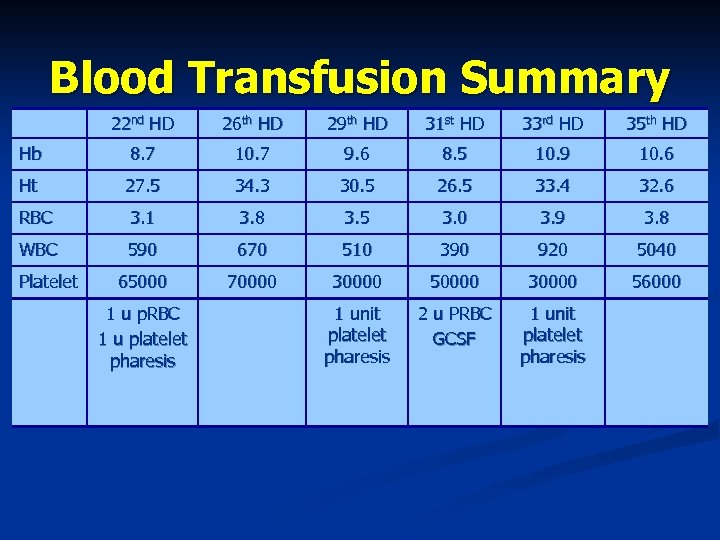 Blood Transfusion Summary 22 nd HD 26 th HD 29 th HD 31 st HD 33 rd HD 35 th HD Hb 8. 7 10. 7 9. 6 8. 5 10. 9 10. 6 Ht 27. 5 34. 3 30. 5 26. 5 33. 4 32. 6 RBC 3. 1 3. 8 3. 5 3. 0 3. 9 3. 8 WBC 590 670 510 390 920 5040 65000 70000 30000 56000 1 unit platelet pharesis 2 u PRBC GCSF 1 unit platelet pharesis Platelet 1 u p. RBC 1 u platelet pharesis
Blood Transfusion Summary 22 nd HD 26 th HD 29 th HD 31 st HD 33 rd HD 35 th HD Hb 8. 7 10. 7 9. 6 8. 5 10. 9 10. 6 Ht 27. 5 34. 3 30. 5 26. 5 33. 4 32. 6 RBC 3. 1 3. 8 3. 5 3. 0 3. 9 3. 8 WBC 590 670 510 390 920 5040 65000 70000 30000 56000 1 unit platelet pharesis 2 u PRBC GCSF 1 unit platelet pharesis Platelet 1 u p. RBC 1 u platelet pharesis
 DISCUSSION
DISCUSSION
 Immunocompromised Host DEFINITION These patients are defined by their susceptibility to infection with organisms of low native virulence for the immunologically normal hosts.
Immunocompromised Host DEFINITION These patients are defined by their susceptibility to infection with organisms of low native virulence for the immunologically normal hosts.
 Immunocompromised Host Spectrum of immunocompromised hosts has expanded with prolonged survival of solid organ and hematopoietic transplant recipients congenital immune deficits and autoimmune disorders epidemic of human immunodeficiency syndrome/acquired immunodeficiency syndrome (HIV/AIDS).
Immunocompromised Host Spectrum of immunocompromised hosts has expanded with prolonged survival of solid organ and hematopoietic transplant recipients congenital immune deficits and autoimmune disorders epidemic of human immunodeficiency syndrome/acquired immunodeficiency syndrome (HIV/AIDS).
 Immunocompromised Host RISK FACTOR: Immunosuppressive therapies create a diverse set of immune deficits that create the substrate for opportunistic infections.
Immunocompromised Host RISK FACTOR: Immunosuppressive therapies create a diverse set of immune deficits that create the substrate for opportunistic infections.
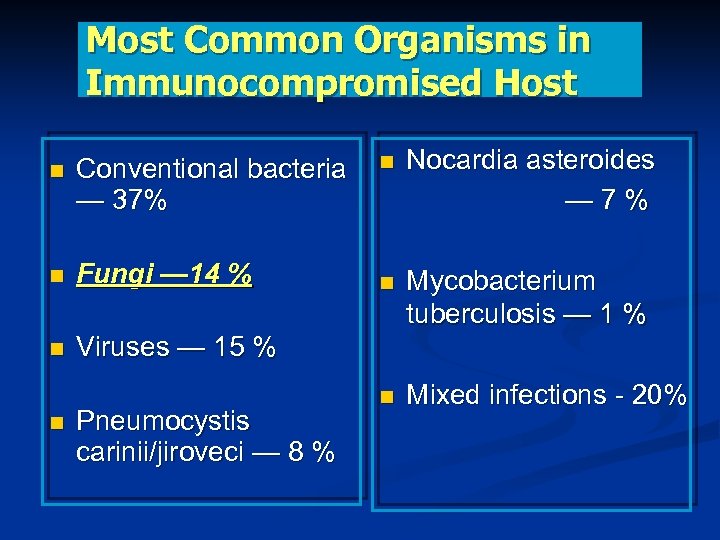 Most Common Organisms in Immunocompromised Host Conventional bacteria Nocardia asteroides — 37% — 7 % Fungi — 14 % Viruses — 15 % Pneumocystis carinii/jiroveci — 8 % Mycobacterium tuberculosis — 1 % Mixed infections - 20%
Most Common Organisms in Immunocompromised Host Conventional bacteria Nocardia asteroides — 37% — 7 % Fungi — 14 % Viruses — 15 % Pneumocystis carinii/jiroveci — 8 % Mycobacterium tuberculosis — 1 % Mixed infections - 20%
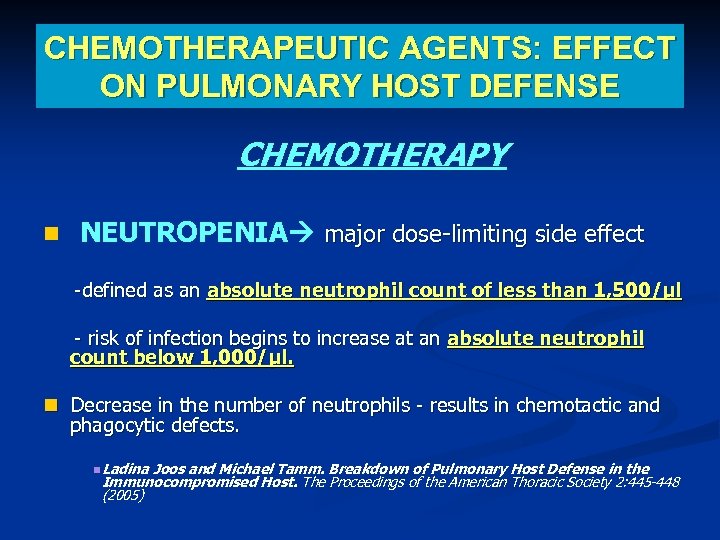 CHEMOTHERAPEUTIC AGENTS: EFFECT ON PULMONARY HOST DEFENSE CHEMOTHERAPY NEUTROPENIA major dose-limiting side effect -defined as an absolute neutrophil count of less than 1, 500/µl - risk of infection begins to increase at an absolute neutrophil count below 1, 000/µl. Decrease in the number of neutrophils - results in chemotactic and phagocytic defects. Ladina Joos and Michael Tamm. Breakdown of Pulmonary Host Defense in the Immunocompromised Host. The Proceedings of the American Thoracic Society 2: 445 -448 (2005)
CHEMOTHERAPEUTIC AGENTS: EFFECT ON PULMONARY HOST DEFENSE CHEMOTHERAPY NEUTROPENIA major dose-limiting side effect -defined as an absolute neutrophil count of less than 1, 500/µl - risk of infection begins to increase at an absolute neutrophil count below 1, 000/µl. Decrease in the number of neutrophils - results in chemotactic and phagocytic defects. Ladina Joos and Michael Tamm. Breakdown of Pulmonary Host Defense in the Immunocompromised Host. The Proceedings of the American Thoracic Society 2: 445 -448 (2005)
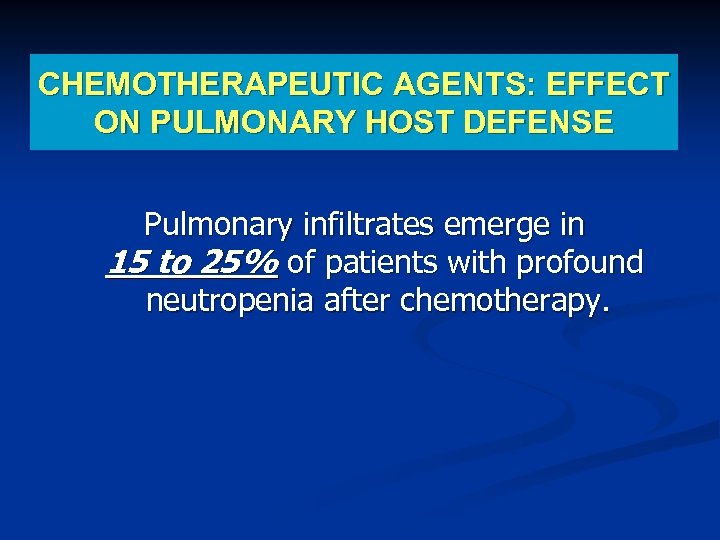 CHEMOTHERAPEUTIC AGENTS: EFFECT ON PULMONARY HOST DEFENSE Pulmonary infiltrates emerge in 15 to 25% of patients with profound neutropenia after chemotherapy.
CHEMOTHERAPEUTIC AGENTS: EFFECT ON PULMONARY HOST DEFENSE Pulmonary infiltrates emerge in 15 to 25% of patients with profound neutropenia after chemotherapy.
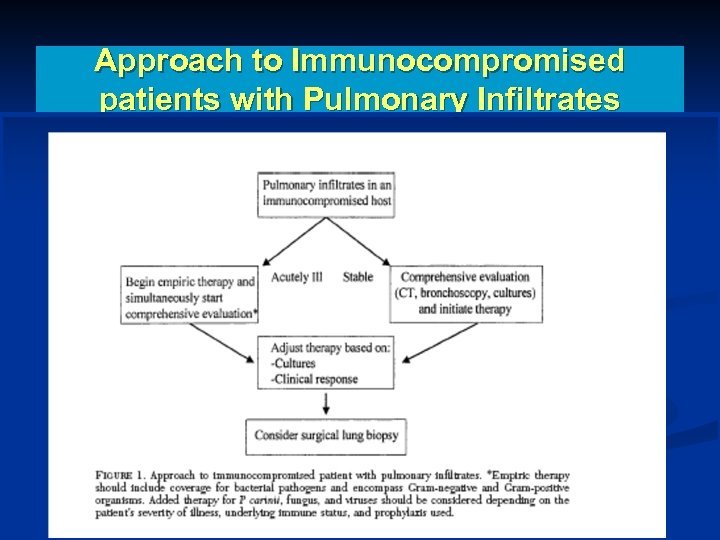 Approach to Immunocompromised patients with Pulmonary Infiltrates
Approach to Immunocompromised patients with Pulmonary Infiltrates
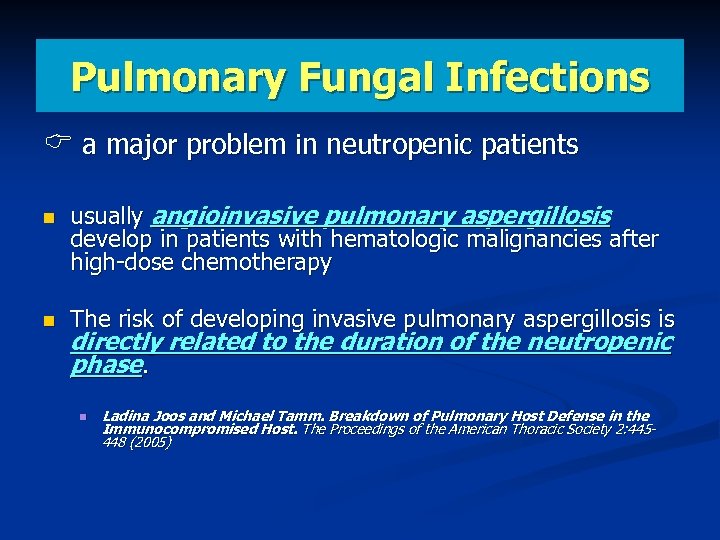 Pulmonary Fungal Infections a major problem in neutropenic patients usually angioinvasive pulmonary aspergillosis develop in patients with hematologic malignancies after high-dose chemotherapy The risk of developing invasive pulmonary aspergillosis is directly related to the duration of the neutropenic phase. Ladina Joos and Michael Tamm. Breakdown of Pulmonary Host Defense in the Immunocompromised Host. The Proceedings of the American Thoracic Society 2: 445448 (2005)
Pulmonary Fungal Infections a major problem in neutropenic patients usually angioinvasive pulmonary aspergillosis develop in patients with hematologic malignancies after high-dose chemotherapy The risk of developing invasive pulmonary aspergillosis is directly related to the duration of the neutropenic phase. Ladina Joos and Michael Tamm. Breakdown of Pulmonary Host Defense in the Immunocompromised Host. The Proceedings of the American Thoracic Society 2: 445448 (2005)
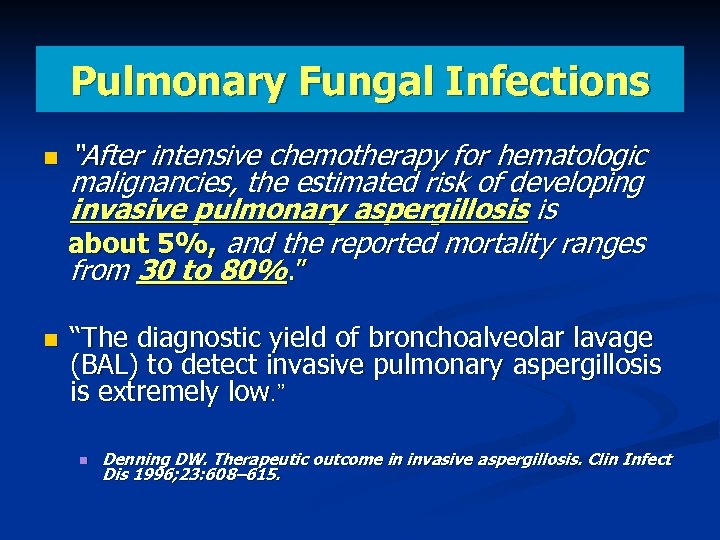 Pulmonary Fungal Infections “After intensive chemotherapy for hematologic malignancies, the estimated risk of developing invasive pulmonary aspergillosis is about 5%, and the reported mortality ranges from 30 to 80%. ” “The diagnostic yield of bronchoalveolar lavage (BAL) to detect invasive pulmonary aspergillosis is extremely low. ” Denning DW. Therapeutic outcome in invasive aspergillosis. Clin Infect Dis 1996; 23: 608– 615.
Pulmonary Fungal Infections “After intensive chemotherapy for hematologic malignancies, the estimated risk of developing invasive pulmonary aspergillosis is about 5%, and the reported mortality ranges from 30 to 80%. ” “The diagnostic yield of bronchoalveolar lavage (BAL) to detect invasive pulmonary aspergillosis is extremely low. ” Denning DW. Therapeutic outcome in invasive aspergillosis. Clin Infect Dis 1996; 23: 608– 615.
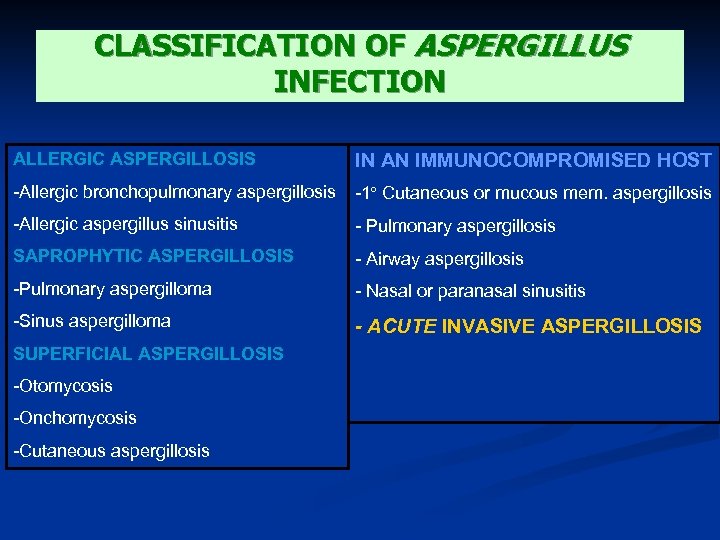 CLASSIFICATION OF ASPERGILLUS INFECTION ALLERGIC ASPERGILLOSIS IN AN IMMUNOCOMPROMISED HOST -Allergic bronchopulmonary aspergillosis -1º Cutaneous or mucous mem. aspergillosis -Allergic aspergillus sinusitis - Pulmonary aspergillosis SAPROPHYTIC ASPERGILLOSIS - Airway aspergillosis -Pulmonary aspergilloma - Nasal or paranasal sinusitis -Sinus aspergilloma - ACUTE INVASIVE ASPERGILLOSIS SUPERFICIAL ASPERGILLOSIS -Otomycosis -Onchomycosis -Cutaneous aspergillosis
CLASSIFICATION OF ASPERGILLUS INFECTION ALLERGIC ASPERGILLOSIS IN AN IMMUNOCOMPROMISED HOST -Allergic bronchopulmonary aspergillosis -1º Cutaneous or mucous mem. aspergillosis -Allergic aspergillus sinusitis - Pulmonary aspergillosis SAPROPHYTIC ASPERGILLOSIS - Airway aspergillosis -Pulmonary aspergilloma - Nasal or paranasal sinusitis -Sinus aspergilloma - ACUTE INVASIVE ASPERGILLOSIS SUPERFICIAL ASPERGILLOSIS -Otomycosis -Onchomycosis -Cutaneous aspergillosis
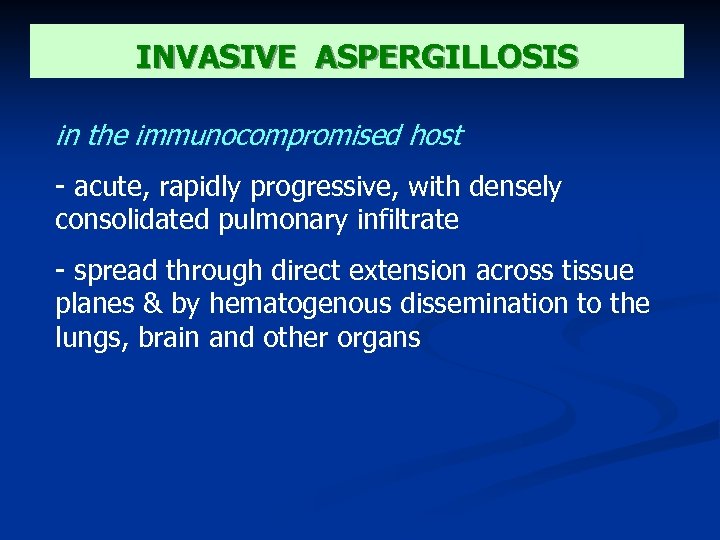 INVASIVE ASPERGILLOSIS in the immunocompromised host - acute, rapidly progressive, with densely consolidated pulmonary infiltrate - spread through direct extension across tissue planes & by hematogenous dissemination to the lungs, brain and other organs
INVASIVE ASPERGILLOSIS in the immunocompromised host - acute, rapidly progressive, with densely consolidated pulmonary infiltrate - spread through direct extension across tissue planes & by hematogenous dissemination to the lungs, brain and other organs
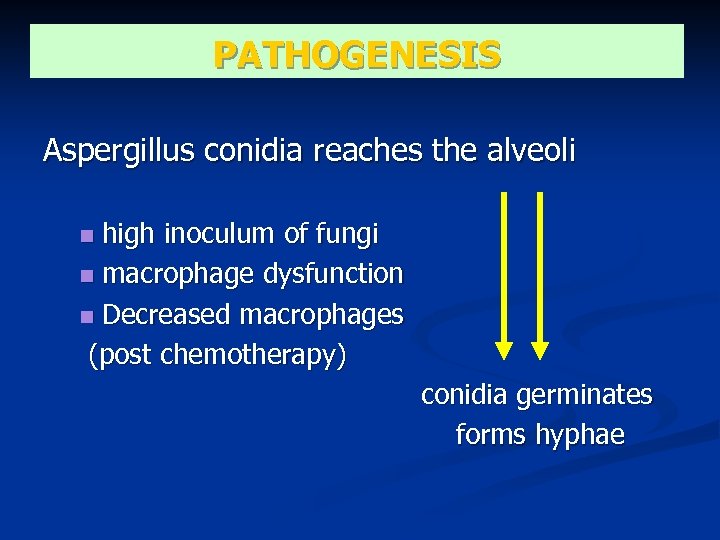 PATHOGENESIS Aspergillus conidia reaches the alveoli high inoculum of fungi macrophage dysfunction Decreased macrophages (post chemotherapy) conidia germinates forms hyphae
PATHOGENESIS Aspergillus conidia reaches the alveoli high inoculum of fungi macrophage dysfunction Decreased macrophages (post chemotherapy) conidia germinates forms hyphae
 PATHOGENESIS With the development of Aspergillus hyphae influx of neutrophils recruited neutrophils attaches & damages the hyphae During hyphal growth, the fungus produces various metabolites that help it evade host defenses. (i. e. complement inhibitors, proteases, and several mycotoxins, including gliotoxin and aflatoxin)
PATHOGENESIS With the development of Aspergillus hyphae influx of neutrophils recruited neutrophils attaches & damages the hyphae During hyphal growth, the fungus produces various metabolites that help it evade host defenses. (i. e. complement inhibitors, proteases, and several mycotoxins, including gliotoxin and aflatoxin)
 PATHOLOGY - progression of the infection across tissue planes vascular invasion subsequent infarction tissue necrosis
PATHOLOGY - progression of the infection across tissue planes vascular invasion subsequent infarction tissue necrosis
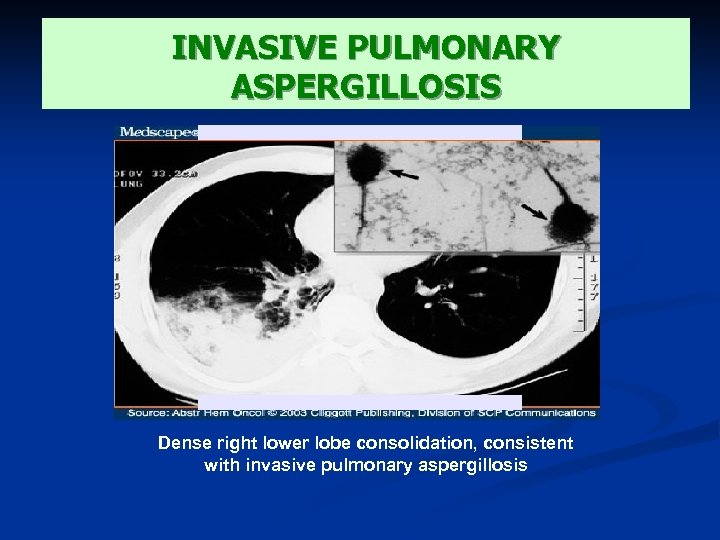 INVASIVE PULMONARY ASPERGILLOSIS Dense right lower lobe consolidation, consistent with invasive pulmonary aspergillosis
INVASIVE PULMONARY ASPERGILLOSIS Dense right lower lobe consolidation, consistent with invasive pulmonary aspergillosis
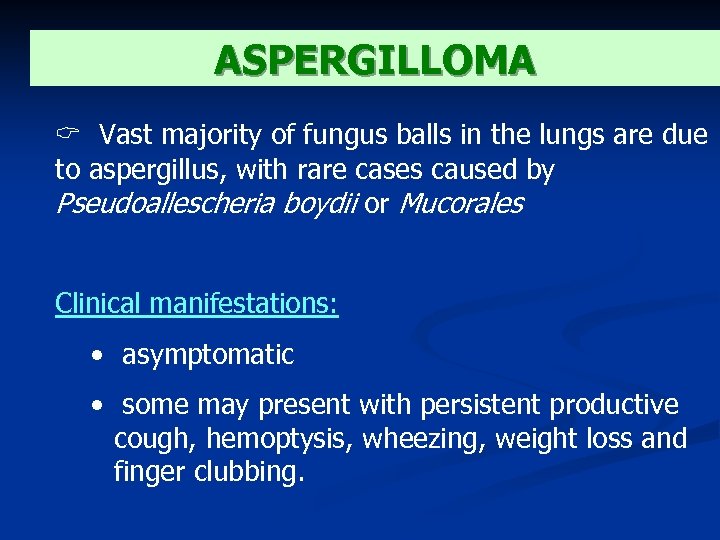 ASPERGILLOMA Vast majority of fungus balls in the lungs are due to aspergillus, with rare cases caused by Pseudoallescheria boydii or Mucorales Clinical manifestations: • asymptomatic • some may present with persistent productive cough, hemoptysis, wheezing, weight loss and finger clubbing.
ASPERGILLOMA Vast majority of fungus balls in the lungs are due to aspergillus, with rare cases caused by Pseudoallescheria boydii or Mucorales Clinical manifestations: • asymptomatic • some may present with persistent productive cough, hemoptysis, wheezing, weight loss and finger clubbing.
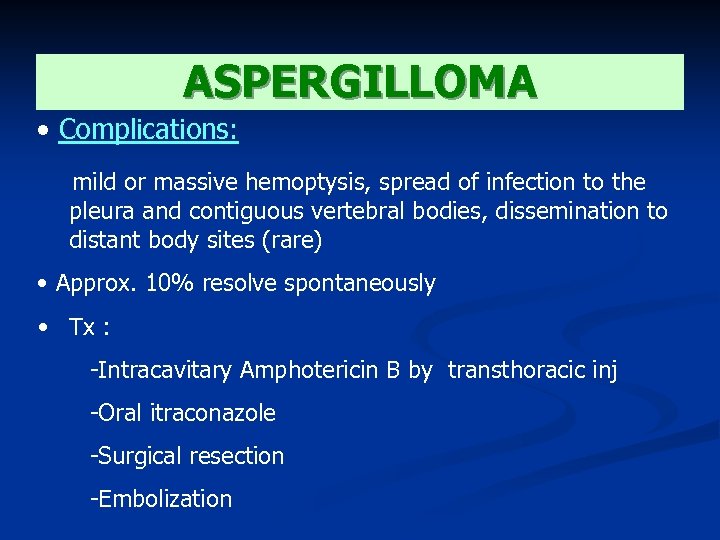 ASPERGILLOMA • Complications: mild or massive hemoptysis, spread of infection to the pleura and contiguous vertebral bodies, dissemination to distant body sites (rare) • Approx. 10% resolve spontaneously • Tx : -Intracavitary Amphotericin B by transthoracic inj -Oral itraconazole -Surgical resection -Embolization
ASPERGILLOMA • Complications: mild or massive hemoptysis, spread of infection to the pleura and contiguous vertebral bodies, dissemination to distant body sites (rare) • Approx. 10% resolve spontaneously • Tx : -Intracavitary Amphotericin B by transthoracic inj -Oral itraconazole -Surgical resection -Embolization
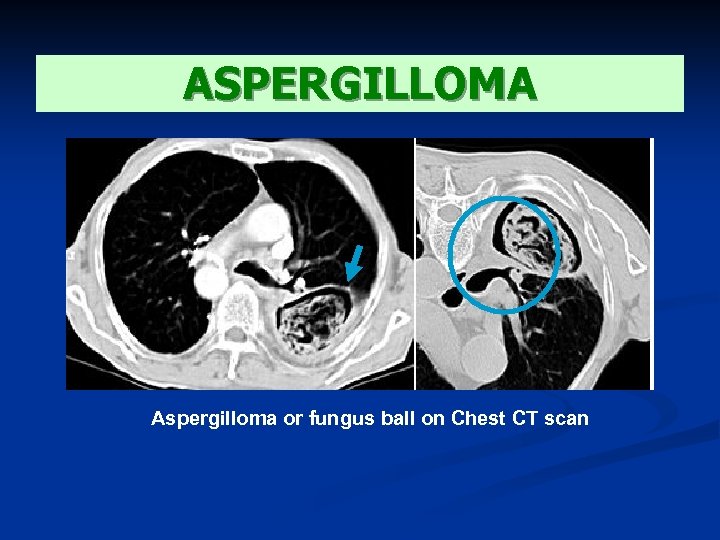 ASPERGILLOMA Aspergilloma or fungus ball on Chest CT scan
ASPERGILLOMA Aspergilloma or fungus ball on Chest CT scan
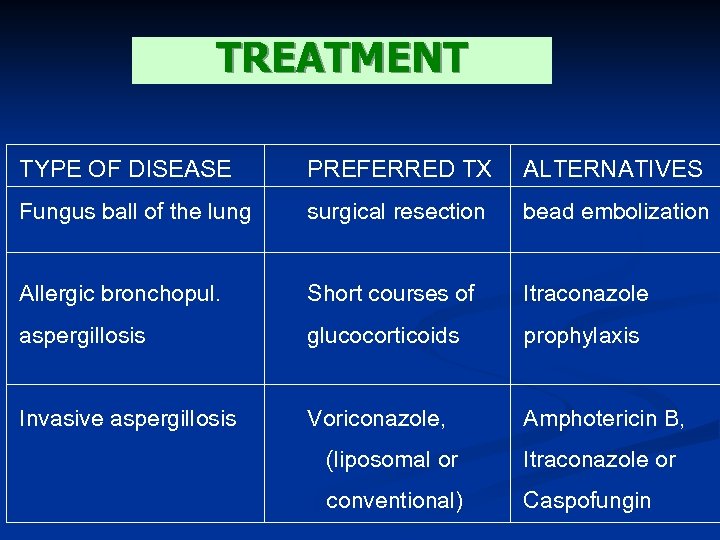 TREATMENT TYPE OF DISEASE PREFERRED TX ALTERNATIVES Fungus ball of the lung surgical resection bead embolization Allergic bronchopul. Short courses of Itraconazole aspergillosis glucocorticoids prophylaxis Invasive aspergillosis Voriconazole, Amphotericin B, (liposomal or Itraconazole or conventional) Caspofungin
TREATMENT TYPE OF DISEASE PREFERRED TX ALTERNATIVES Fungus ball of the lung surgical resection bead embolization Allergic bronchopul. Short courses of Itraconazole aspergillosis glucocorticoids prophylaxis Invasive aspergillosis Voriconazole, Amphotericin B, (liposomal or Itraconazole or conventional) Caspofungin
 TREATMENT 3 classes of antifungal agents are available for the treatment of Aspergillosis : 1. Polyenes (eg : Amphotericin B) 2. Azoles (eg : Itraconazole, Voriconazole) 3. Echinocandins (eg : Caspofungin)
TREATMENT 3 classes of antifungal agents are available for the treatment of Aspergillosis : 1. Polyenes (eg : Amphotericin B) 2. Azoles (eg : Itraconazole, Voriconazole) 3. Echinocandins (eg : Caspofungin)
 TREATMENT AMPHOTERICIN B Treatment is limited by poor toleration & nephrotoxicity Dose : 1 – 1, 5 mg / kg per day Lipid formulation is currently available which can be administered with larger doses but showed fewer toxic effects
TREATMENT AMPHOTERICIN B Treatment is limited by poor toleration & nephrotoxicity Dose : 1 – 1, 5 mg / kg per day Lipid formulation is currently available which can be administered with larger doses but showed fewer toxic effects
 TREATMENT CASPOFUNGIN Is approved for the treatment of invasive aspergillosis in pts who cannot tolerate or who are refractory to standard therapy Dose : IV : loading dose 70 mg/day, followed by 50 mg/day
TREATMENT CASPOFUNGIN Is approved for the treatment of invasive aspergillosis in pts who cannot tolerate or who are refractory to standard therapy Dose : IV : loading dose 70 mg/day, followed by 50 mg/day
 TREATMENT ITRACONAZOLE Is considered a 2 nd line agent for the tx of aspergillosis and is rarely used in immunocompromised pts with invasive disease Dose : 400 mg per day po Require acid environment for absorption, poor bioavailability and important drug interaction
TREATMENT ITRACONAZOLE Is considered a 2 nd line agent for the tx of aspergillosis and is rarely used in immunocompromised pts with invasive disease Dose : 400 mg per day po Require acid environment for absorption, poor bioavailability and important drug interaction
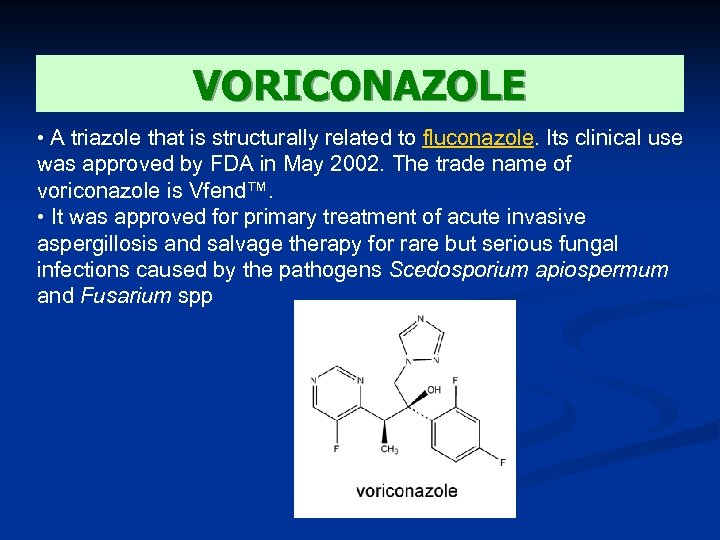 VORICONAZOLE • A triazole that is structurally related to fluconazole. Its clinical use was approved by FDA in May 2002. The trade name of voriconazole is Vfend™. • It was approved for primary treatment of acute invasive aspergillosis and salvage therapy for rare but serious fungal infections caused by the pathogens Scedosporium apiospermum and Fusarium spp
VORICONAZOLE • A triazole that is structurally related to fluconazole. Its clinical use was approved by FDA in May 2002. The trade name of voriconazole is Vfend™. • It was approved for primary treatment of acute invasive aspergillosis and salvage therapy for rare but serious fungal infections caused by the pathogens Scedosporium apiospermum and Fusarium spp
 VORICONAZOLE - works principally by inhibition of cytochrome P 450 14 ademethylase (P 45014 DM). - favorable in vitro activity against a variety of fungi. These include, Candida spp. , Aspergillus spp. , Cryptococcus neoformans, Blastomyces dermatitidis, Coccidioides immitis, Histoplasma capsulatum, Fusarium spp. , and Penicillium marneffei. - a fungistatic agent against Candida spp. and Cryptococcus neoformans. It may be fungicidal against Aspergillus spp.
VORICONAZOLE - works principally by inhibition of cytochrome P 450 14 ademethylase (P 45014 DM). - favorable in vitro activity against a variety of fungi. These include, Candida spp. , Aspergillus spp. , Cryptococcus neoformans, Blastomyces dermatitidis, Coccidioides immitis, Histoplasma capsulatum, Fusarium spp. , and Penicillium marneffei. - a fungistatic agent against Candida spp. and Cryptococcus neoformans. It may be fungicidal against Aspergillus spp.
 VORICONAZOLE - active following both oral and intravenous administrations Doses Oral: 200 mg twice daily IV: 3 to 6 mg/kg every 12 h doses SIDE EFFECTS: transient visual disturbances, skin rash and elevated hepatic enzyme levels
VORICONAZOLE - active following both oral and intravenous administrations Doses Oral: 200 mg twice daily IV: 3 to 6 mg/kg every 12 h doses SIDE EFFECTS: transient visual disturbances, skin rash and elevated hepatic enzyme levels
 TREATMENT POSACONAZOLE is a broad spectrum triazole that is currently in development. Its activity is similar to Voriconazole against Aspergillus sp, but there is little published to date on its efficacy
TREATMENT POSACONAZOLE is a broad spectrum triazole that is currently in development. Its activity is similar to Voriconazole against Aspergillus sp, but there is little published to date on its efficacy
 CLINICAL STUDIES Voriconazole vs. Amphotericin B: Acute invasive aspergillosis National Institute of Allergy and Infectious Diseases Mycoses Study Group June 2001 - 277 patients treated for 12 weeks with Voriconazole and Amphotericin B - majority of study patients had underlying hematologic malignancies, including bone marrow transplantation; patients with solid organ transplantation, solid tumors, and AIDS. CONCLUSION: A satisfactory global response at 12 weeks was seen in 53% of voriconazole treated patients compared to 32% of amphotericin B treated patients. A benefit of voriconazole compared to amphotericin B on patient survival at Day 84 was seen with a 71% survival rate on voriconazole compared to 58% on amphotericin B.
CLINICAL STUDIES Voriconazole vs. Amphotericin B: Acute invasive aspergillosis National Institute of Allergy and Infectious Diseases Mycoses Study Group June 2001 - 277 patients treated for 12 weeks with Voriconazole and Amphotericin B - majority of study patients had underlying hematologic malignancies, including bone marrow transplantation; patients with solid organ transplantation, solid tumors, and AIDS. CONCLUSION: A satisfactory global response at 12 weeks was seen in 53% of voriconazole treated patients compared to 32% of amphotericin B treated patients. A benefit of voriconazole compared to amphotericin B on patient survival at Day 84 was seen with a 71% survival rate on voriconazole compared to 58% on amphotericin B.
 CLINICAL STUDIES Fluconazole and Voriconazole Multidisk Testing of Candida Species for Disk Test Calibration and MIC Estimation Göran Kronvall* and Inga Karlsson Department of Microbiology and Tumor Biology, Sweden January 2001 Fluconazole and voriconazole MICs were determined for 114 clinical Candida isolates, including isolates of Candida albicans, Candida glabrata, Candida krusei, Candida lusitaniae, Candida parapsilosis, and Candida tropicalis. All strains were susceptible to voriconazole, and most strains were also susceptible to fluconazole, with the exception of C. glabrata and C. krusei, the latter being fully fluconazole resistant. Single-strain regression analysis (SRA) was applied to 54 strains. CONCLUSION: Voriconazole might be a first-choice azole in treating Candida infections.
CLINICAL STUDIES Fluconazole and Voriconazole Multidisk Testing of Candida Species for Disk Test Calibration and MIC Estimation Göran Kronvall* and Inga Karlsson Department of Microbiology and Tumor Biology, Sweden January 2001 Fluconazole and voriconazole MICs were determined for 114 clinical Candida isolates, including isolates of Candida albicans, Candida glabrata, Candida krusei, Candida lusitaniae, Candida parapsilosis, and Candida tropicalis. All strains were susceptible to voriconazole, and most strains were also susceptible to fluconazole, with the exception of C. glabrata and C. krusei, the latter being fully fluconazole resistant. Single-strain regression analysis (SRA) was applied to 54 strains. CONCLUSION: Voriconazole might be a first-choice azole in treating Candida infections.
 THANK YOU!
THANK YOU!


