b3d39d1870e8bc676a7fc9a3196c423a.ppt
- Количество слайдов: 59
 Medical Error Root Cause Analysis and Disclosure Ethan Cumbler MD, FACP Dimitriy Levin MD Hospitalist Section University of Colorado Hospital 2012
Medical Error Root Cause Analysis and Disclosure Ethan Cumbler MD, FACP Dimitriy Levin MD Hospitalist Section University of Colorado Hospital 2012
 How do Physicians Respond to Medical Error?
How do Physicians Respond to Medical Error?
 CASE Transfers Can Be Hazardous To Your Health
CASE Transfers Can Be Hazardous To Your Health
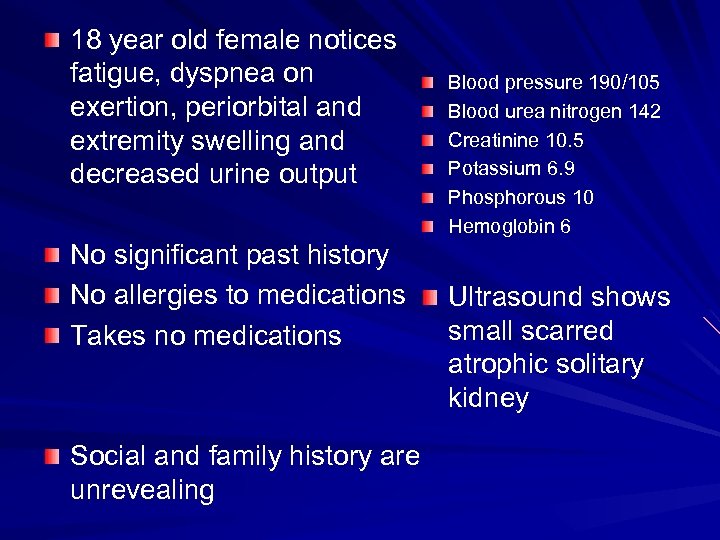 18 year old female notices fatigue, dyspnea on exertion, periorbital and extremity swelling and decreased urine output No significant past history No allergies to medications Takes no medications Social and family history are unrevealing Blood pressure 190/105 Blood urea nitrogen 142 Creatinine 10. 5 Potassium 6. 9 Phosphorous 10 Hemoglobin 6 Ultrasound shows small scarred atrophic solitary kidney
18 year old female notices fatigue, dyspnea on exertion, periorbital and extremity swelling and decreased urine output No significant past history No allergies to medications Takes no medications Social and family history are unrevealing Blood pressure 190/105 Blood urea nitrogen 142 Creatinine 10. 5 Potassium 6. 9 Phosphorous 10 Hemoglobin 6 Ultrasound shows small scarred atrophic solitary kidney
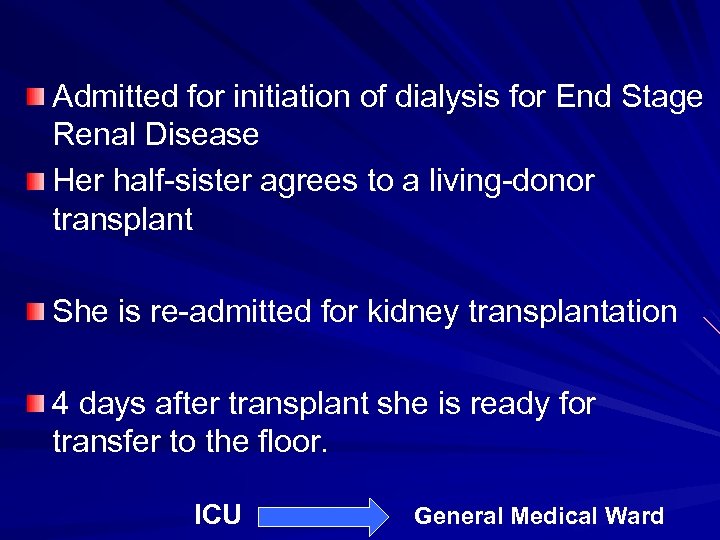 Admitted for initiation of dialysis for End Stage Renal Disease Her half-sister agrees to a living-donor transplant She is re-admitted for kidney transplantation 4 days after transplant she is ready for transfer to the floor. ICU General Medical Ward
Admitted for initiation of dialysis for End Stage Renal Disease Her half-sister agrees to a living-donor transplant She is re-admitted for kidney transplantation 4 days after transplant she is ready for transfer to the floor. ICU General Medical Ward
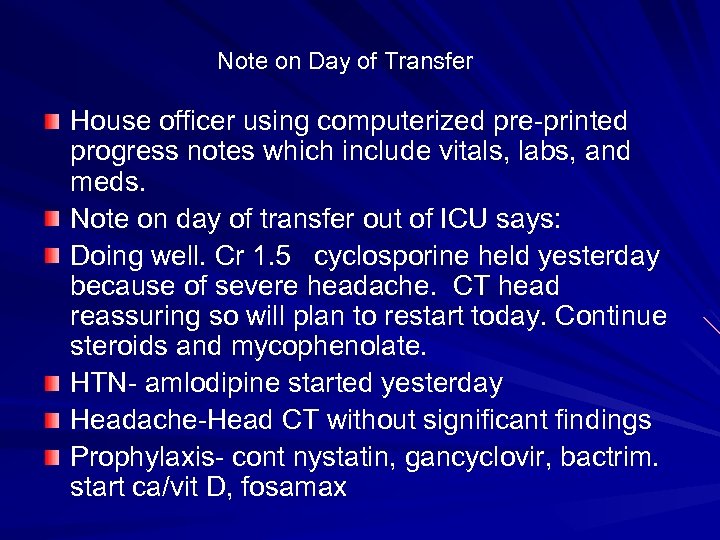 Note on Day of Transfer House officer using computerized pre-printed progress notes which include vitals, labs, and meds. Note on day of transfer out of ICU says: Doing well. Cr 1. 5 cyclosporine held yesterday because of severe headache. CT head reassuring so will plan to restart today. Continue steroids and mycophenolate. HTN- amlodipine started yesterday Headache-Head CT without significant findings Prophylaxis- cont nystatin, gancyclovir, bactrim. start ca/vit D, fosamax
Note on Day of Transfer House officer using computerized pre-printed progress notes which include vitals, labs, and meds. Note on day of transfer out of ICU says: Doing well. Cr 1. 5 cyclosporine held yesterday because of severe headache. CT head reassuring so will plan to restart today. Continue steroids and mycophenolate. HTN- amlodipine started yesterday Headache-Head CT without significant findings Prophylaxis- cont nystatin, gancyclovir, bactrim. start ca/vit D, fosamax
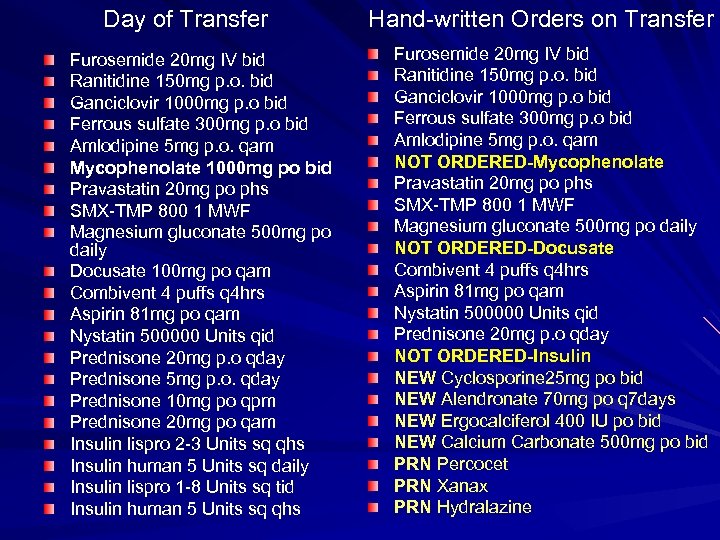 Day of Transfer Furosemide 20 mg IV bid Ranitidine 150 mg p. o. bid Ganciclovir 1000 mg p. o bid Ferrous sulfate 300 mg p. o bid Amlodipine 5 mg p. o. qam Mycophenolate 1000 mg po bid Pravastatin 20 mg po phs SMX-TMP 800 1 MWF Magnesium gluconate 500 mg po daily Docusate 100 mg po qam Combivent 4 puffs q 4 hrs Aspirin 81 mg po qam Nystatin 500000 Units qid Prednisone 20 mg p. o qday Prednisone 5 mg p. o. qday Prednisone 10 mg po qpm Prednisone 20 mg po qam Insulin lispro 2 -3 Units sq qhs Insulin human 5 Units sq daily Insulin lispro 1 -8 Units sq tid Insulin human 5 Units sq qhs Hand-written Orders on Transfer Furosemide 20 mg IV bid Ranitidine 150 mg p. o. bid Ganciclovir 1000 mg p. o bid Ferrous sulfate 300 mg p. o bid Amlodipine 5 mg p. o. qam NOT ORDERED-Mycophenolate Pravastatin 20 mg po phs SMX-TMP 800 1 MWF Magnesium gluconate 500 mg po daily NOT ORDERED-Docusate Combivent 4 puffs q 4 hrs Aspirin 81 mg po qam Nystatin 500000 Units qid Prednisone 20 mg p. o qday NOT ORDERED-Insulin NEW Cyclosporine 25 mg po bid NEW Alendronate 70 mg po q 7 days NEW Ergocalciferol 400 IU po bid NEW Calcium Carbonate 500 mg po bid PRN Percocet PRN Xanax PRN Hydralazine
Day of Transfer Furosemide 20 mg IV bid Ranitidine 150 mg p. o. bid Ganciclovir 1000 mg p. o bid Ferrous sulfate 300 mg p. o bid Amlodipine 5 mg p. o. qam Mycophenolate 1000 mg po bid Pravastatin 20 mg po phs SMX-TMP 800 1 MWF Magnesium gluconate 500 mg po daily Docusate 100 mg po qam Combivent 4 puffs q 4 hrs Aspirin 81 mg po qam Nystatin 500000 Units qid Prednisone 20 mg p. o qday Prednisone 5 mg p. o. qday Prednisone 10 mg po qpm Prednisone 20 mg po qam Insulin lispro 2 -3 Units sq qhs Insulin human 5 Units sq daily Insulin lispro 1 -8 Units sq tid Insulin human 5 Units sq qhs Hand-written Orders on Transfer Furosemide 20 mg IV bid Ranitidine 150 mg p. o. bid Ganciclovir 1000 mg p. o bid Ferrous sulfate 300 mg p. o bid Amlodipine 5 mg p. o. qam NOT ORDERED-Mycophenolate Pravastatin 20 mg po phs SMX-TMP 800 1 MWF Magnesium gluconate 500 mg po daily NOT ORDERED-Docusate Combivent 4 puffs q 4 hrs Aspirin 81 mg po qam Nystatin 500000 Units qid Prednisone 20 mg p. o qday NOT ORDERED-Insulin NEW Cyclosporine 25 mg po bid NEW Alendronate 70 mg po q 7 days NEW Ergocalciferol 400 IU po bid NEW Calcium Carbonate 500 mg po bid PRN Percocet PRN Xanax PRN Hydralazine
 What Set-ups For Error Can You Identify?
What Set-ups For Error Can You Identify?
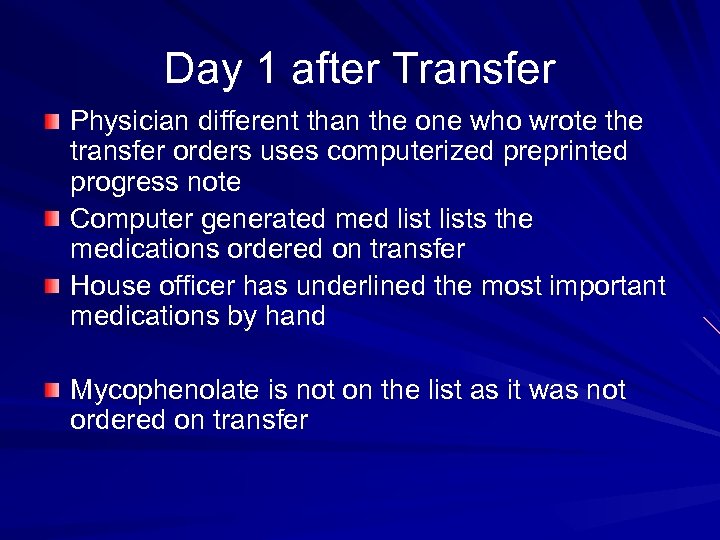 Day 1 after Transfer Physician different than the one who wrote the transfer orders uses computerized preprinted progress note Computer generated med lists the medications ordered on transfer House officer has underlined the most important medications by hand Mycophenolate is not on the list as it was not ordered on transfer
Day 1 after Transfer Physician different than the one who wrote the transfer orders uses computerized preprinted progress note Computer generated med lists the medications ordered on transfer House officer has underlined the most important medications by hand Mycophenolate is not on the list as it was not ordered on transfer
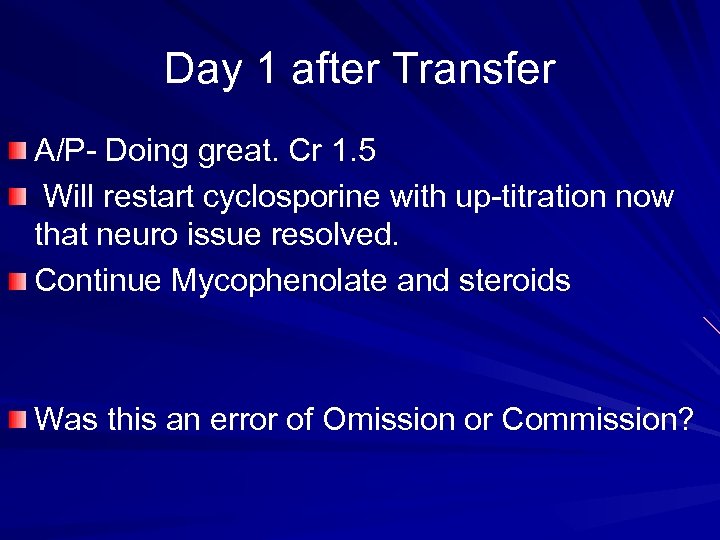 Day 1 after Transfer A/P- Doing great. Cr 1. 5 Will restart cyclosporine with up-titration now that neuro issue resolved. Continue Mycophenolate and steroids Was this an error of Omission or Commission?
Day 1 after Transfer A/P- Doing great. Cr 1. 5 Will restart cyclosporine with up-titration now that neuro issue resolved. Continue Mycophenolate and steroids Was this an error of Omission or Commission?

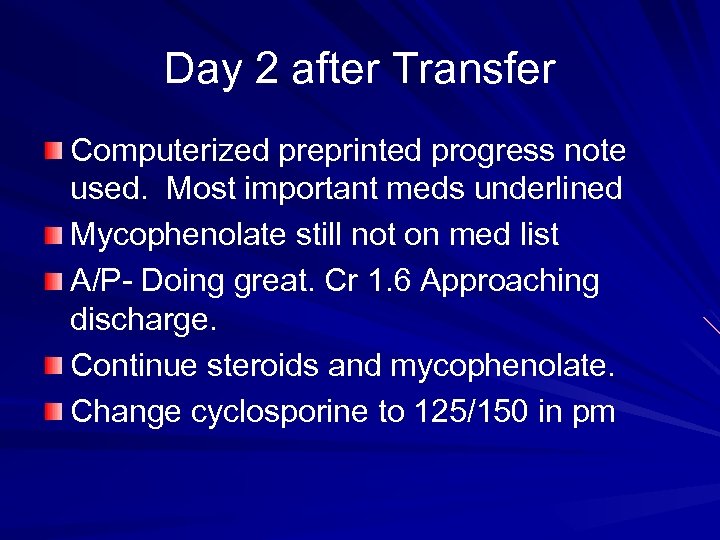 Day 2 after Transfer Computerized preprinted progress note used. Most important meds underlined Mycophenolate still not on med list A/P- Doing great. Cr 1. 6 Approaching discharge. Continue steroids and mycophenolate. Change cyclosporine to 125/150 in pm
Day 2 after Transfer Computerized preprinted progress note used. Most important meds underlined Mycophenolate still not on med list A/P- Doing great. Cr 1. 6 Approaching discharge. Continue steroids and mycophenolate. Change cyclosporine to 125/150 in pm
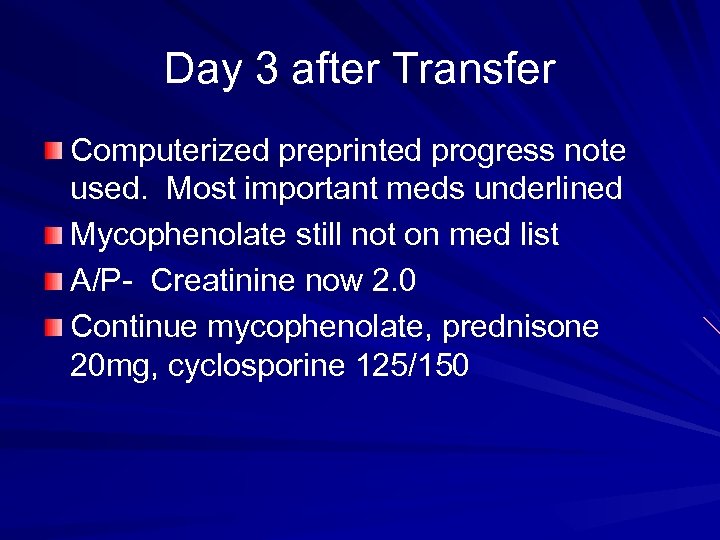 Day 3 after Transfer Computerized preprinted progress note used. Most important meds underlined Mycophenolate still not on med list A/P- Creatinine now 2. 0 Continue mycophenolate, prednisone 20 mg, cyclosporine 125/150
Day 3 after Transfer Computerized preprinted progress note used. Most important meds underlined Mycophenolate still not on med list A/P- Creatinine now 2. 0 Continue mycophenolate, prednisone 20 mg, cyclosporine 125/150
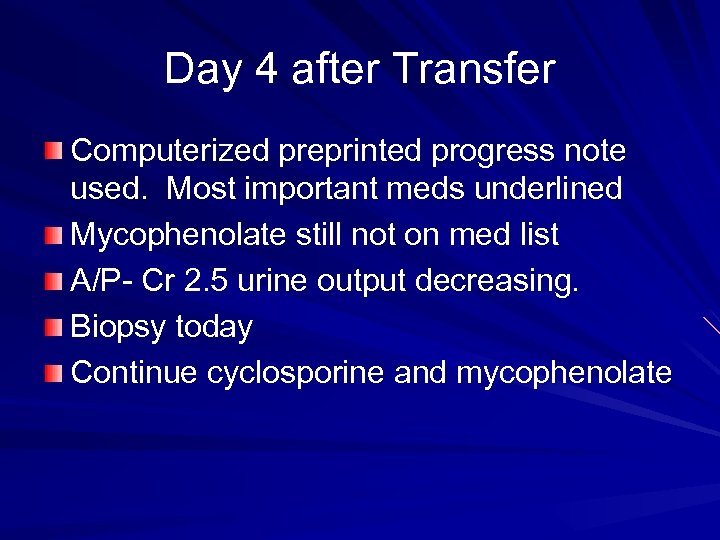 Day 4 after Transfer Computerized preprinted progress note used. Most important meds underlined Mycophenolate still not on med list A/P- Cr 2. 5 urine output decreasing. Biopsy today Continue cyclosporine and mycophenolate
Day 4 after Transfer Computerized preprinted progress note used. Most important meds underlined Mycophenolate still not on med list A/P- Cr 2. 5 urine output decreasing. Biopsy today Continue cyclosporine and mycophenolate
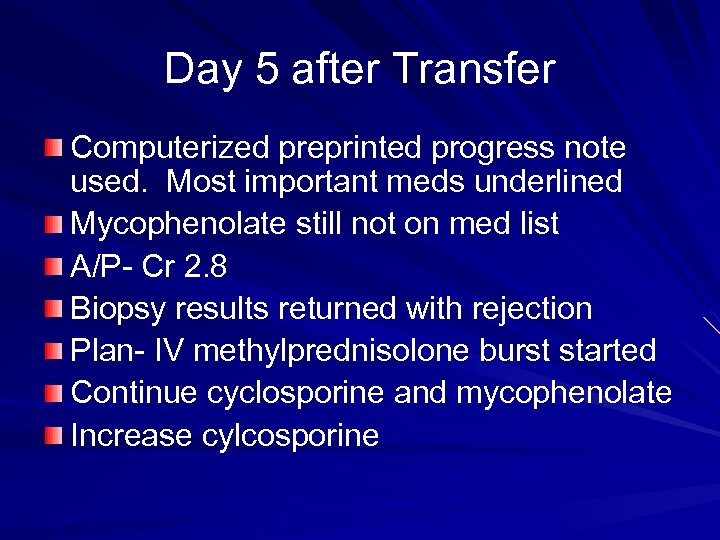 Day 5 after Transfer Computerized preprinted progress note used. Most important meds underlined Mycophenolate still not on med list A/P- Cr 2. 8 Biopsy results returned with rejection Plan- IV methylprednisolone burst started Continue cyclosporine and mycophenolate Increase cylcosporine
Day 5 after Transfer Computerized preprinted progress note used. Most important meds underlined Mycophenolate still not on med list A/P- Cr 2. 8 Biopsy results returned with rejection Plan- IV methylprednisolone burst started Continue cyclosporine and mycophenolate Increase cylcosporine
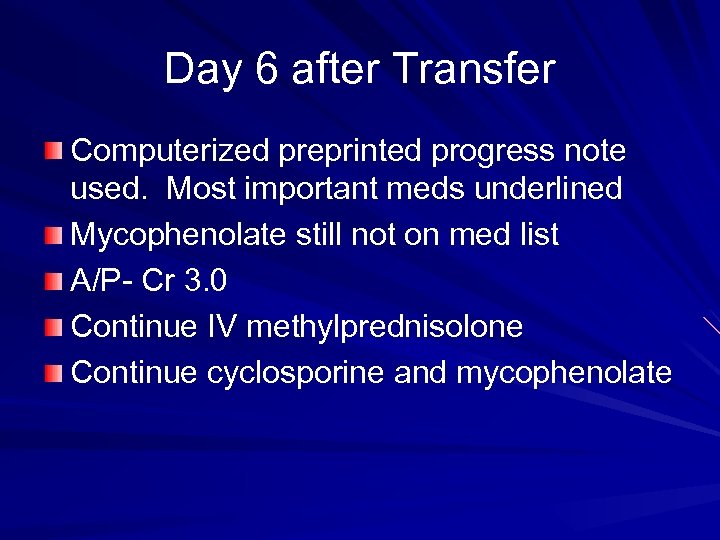 Day 6 after Transfer Computerized preprinted progress note used. Most important meds underlined Mycophenolate still not on med list A/P- Cr 3. 0 Continue IV methylprednisolone Continue cyclosporine and mycophenolate
Day 6 after Transfer Computerized preprinted progress note used. Most important meds underlined Mycophenolate still not on med list A/P- Cr 3. 0 Continue IV methylprednisolone Continue cyclosporine and mycophenolate
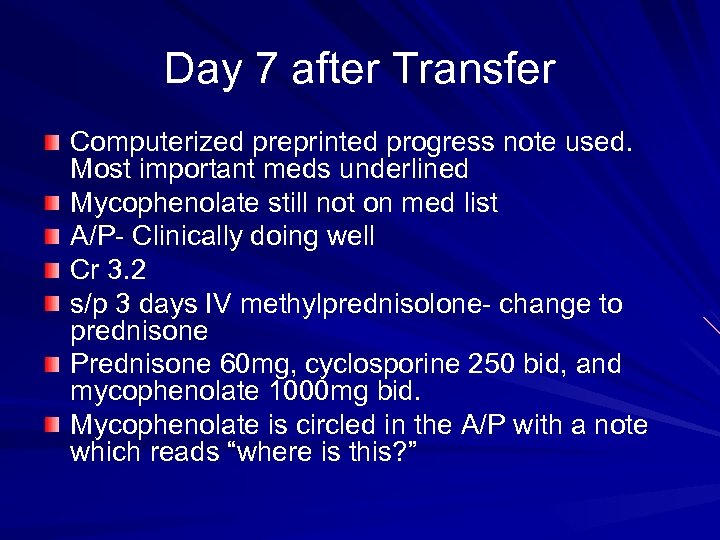 Day 7 after Transfer Computerized preprinted progress note used. Most important meds underlined Mycophenolate still not on med list A/P- Clinically doing well Cr 3. 2 s/p 3 days IV methylprednisolone- change to prednisone Prednisone 60 mg, cyclosporine 250 bid, and mycophenolate 1000 mg bid. Mycophenolate is circled in the A/P with a note which reads “where is this? ”
Day 7 after Transfer Computerized preprinted progress note used. Most important meds underlined Mycophenolate still not on med list A/P- Clinically doing well Cr 3. 2 s/p 3 days IV methylprednisolone- change to prednisone Prednisone 60 mg, cyclosporine 250 bid, and mycophenolate 1000 mg bid. Mycophenolate is circled in the A/P with a note which reads “where is this? ”
 Day 7 after Transfer Patient restarted on IV steroids. Addendum comments on the patient missing 7 days of mycophenolate which “had fallen off the MAR for some reason”
Day 7 after Transfer Patient restarted on IV steroids. Addendum comments on the patient missing 7 days of mycophenolate which “had fallen off the MAR for some reason”
 Selective Perception – Information we receive will be processed in a manner that harmonizes with and supports our current beliefs.
Selective Perception – Information we receive will be processed in a manner that harmonizes with and supports our current beliefs.
 Root Cause Analysis
Root Cause Analysis
 But WHY? ?
But WHY? ?
 What is RCA Systematic investigation to find the root cause(s) of an event » There is always a root cause
What is RCA Systematic investigation to find the root cause(s) of an event » There is always a root cause
 Five Identifiable Steps 1. Define the problem 2. Collect data 3. Identify possible causal factors 4. Identify Root Causes 5. Recommend and implement solutions
Five Identifiable Steps 1. Define the problem 2. Collect data 3. Identify possible causal factors 4. Identify Root Causes 5. Recommend and implement solutions
 Adverse events vs. errors Adverse event is injury from medical care Error is doing the wrong thing (commission) or not doing the right thing (omission) » Not all adverse events are due to errors Adverse events due to error are potentially preventable
Adverse events vs. errors Adverse event is injury from medical care Error is doing the wrong thing (commission) or not doing the right thing (omission) » Not all adverse events are due to errors Adverse events due to error are potentially preventable
 Define the problem
Define the problem
 Collect Data Proof? Expert and front line input Impact of the problem
Collect Data Proof? Expert and front line input Impact of the problem
 Identify Causal Factors As many potential causal or contributing factors Tools – – Appreciation 5 Whys Drill Down Fishbone/Cause and Effect Diagrams
Identify Causal Factors As many potential causal or contributing factors Tools – – Appreciation 5 Whys Drill Down Fishbone/Cause and Effect Diagrams
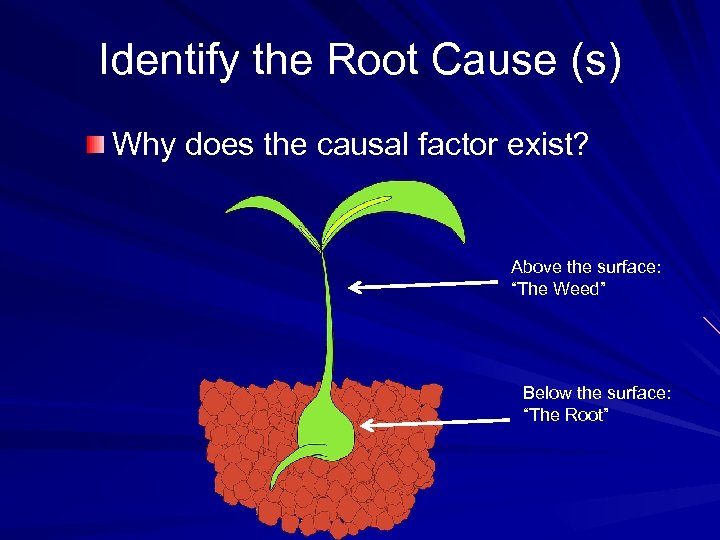 Identify the Root Cause (s) Why does the causal factor exist? Above the surface: “The Weed” Below the surface: “The Root”
Identify the Root Cause (s) Why does the causal factor exist? Above the surface: “The Weed” Below the surface: “The Root”
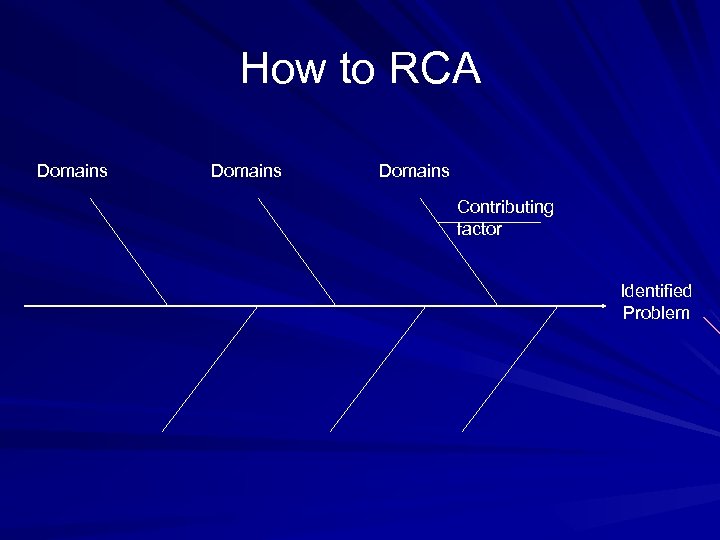 How to RCA Domains Contributing factor Identified Problem
How to RCA Domains Contributing factor Identified Problem
 How to RCA Create a fishbone diagram Select a domain Ask why Repeat until a root cause is identified
How to RCA Create a fishbone diagram Select a domain Ask why Repeat until a root cause is identified
 Process inputs - Domains 1. Materials 2. People 3. Machines 4. Environment 5. Management 6. Methods
Process inputs - Domains 1. Materials 2. People 3. Machines 4. Environment 5. Management 6. Methods
 Process inputs Materials – Defective, shortage, wrong type People – Lack of skills, lack of knowledge, lack of motivation, stress, lack of capability Machines – Wrong tools, improper maintenance, bad design, defective
Process inputs Materials – Defective, shortage, wrong type People – Lack of skills, lack of knowledge, lack of motivation, stress, lack of capability Machines – Wrong tools, improper maintenance, bad design, defective
 Process inputs Environment – Physical layout of the workspace, physical demands of the task, forces of nature Management – Inattention, lack of supervision, lack of communication, lack of proper training Methods – Lack of process/procedure, deviation from written procedures, poor communication
Process inputs Environment – Physical layout of the workspace, physical demands of the task, forces of nature Management – Inattention, lack of supervision, lack of communication, lack of proper training Methods – Lack of process/procedure, deviation from written procedures, poor communication
 Recommend and Implement Solutions “An Ounce of prevention” Implementation logistics Risks
Recommend and Implement Solutions “An Ounce of prevention” Implementation logistics Risks
 Our Case Domains Contributing factor Identified Problem
Our Case Domains Contributing factor Identified Problem

 DISCLOSURE What would you disclose in this case Would you apologize How?
DISCLOSURE What would you disclose in this case Would you apologize How?
 We Don’t Disclose In one study of house staff, 50% did not discuss a serious clinical error with colleagues 1 – only 25% disclosed to the patient or family. X Disclosure rate is 30%-50% across a number of surveys in Europe and America 2 -4.
We Don’t Disclose In one study of house staff, 50% did not discuss a serious clinical error with colleagues 1 – only 25% disclosed to the patient or family. X Disclosure rate is 30%-50% across a number of surveys in Europe and America 2 -4.
 Why Don’t We Disclose? Fear of increasing chance of litigation Desire not to lose the trust of the patient – Particularly if the event did not result in harm Desire to avoid conflict Desire to avoid shame Preservation of our self image We don’t know how to do it well.
Why Don’t We Disclose? Fear of increasing chance of litigation Desire not to lose the trust of the patient – Particularly if the event did not result in harm Desire to avoid conflict Desire to avoid shame Preservation of our self image We don’t know how to do it well.
 What Are the Consequences? Patients who discover error causing an adverse event later are likely to lose trust. 8 – May be more likely to pursue legal action A culture of non-disclosure prevents open discussion of errors, which impairs the ability of the system to improve.
What Are the Consequences? Patients who discover error causing an adverse event later are likely to lose trust. 8 – May be more likely to pursue legal action A culture of non-disclosure prevents open discussion of errors, which impairs the ability of the system to improve.
 What does the evidence show? 98. 8% of patients report desiring disclosure of even minor errors. 8 12% of patients report that they would sue for a moderate severity error if the physician informed the patient about the error. 7 – An even higher 20% of patients report they would sue if they discovered the error by another means. 36% of parents report that they would be less likely to pursue legal action if an error involving their children was disclosed. 15
What does the evidence show? 98. 8% of patients report desiring disclosure of even minor errors. 8 12% of patients report that they would sue for a moderate severity error if the physician informed the patient about the error. 7 – An even higher 20% of patients report they would sue if they discovered the error by another means. 36% of parents report that they would be less likely to pursue legal action if an error involving their children was disclosed. 15
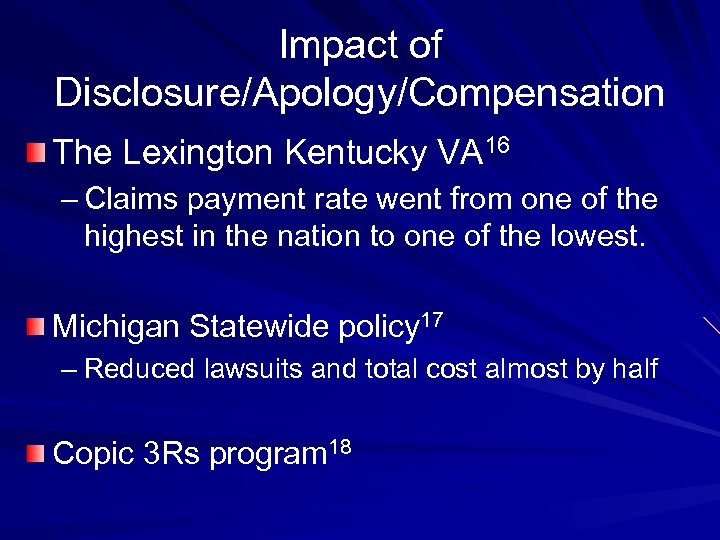 Impact of Disclosure/Apology/Compensation The Lexington Kentucky VA 16 – Claims payment rate went from one of the highest in the nation to one of the lowest. Michigan Statewide policy 17 – Reduced lawsuits and total cost almost by half Copic 3 Rs program 18
Impact of Disclosure/Apology/Compensation The Lexington Kentucky VA 16 – Claims payment rate went from one of the highest in the nation to one of the lowest. Michigan Statewide policy 17 – Reduced lawsuits and total cost almost by half Copic 3 Rs program 18
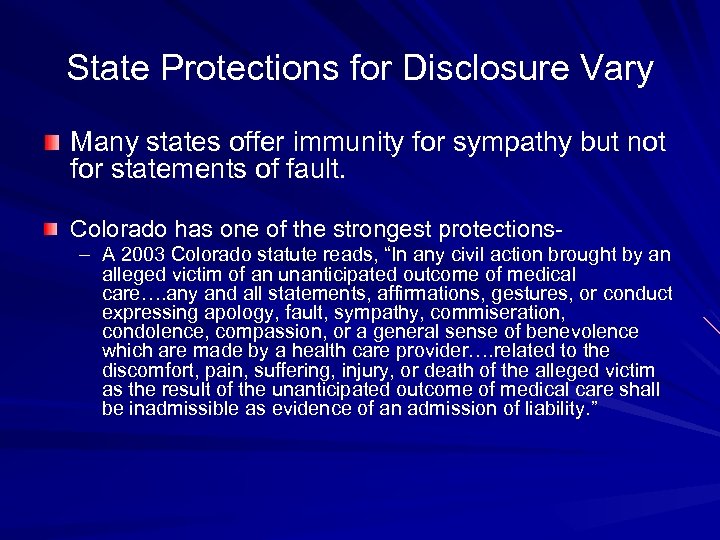 State Protections for Disclosure Vary Many states offer immunity for sympathy but not for statements of fault. Colorado has one of the strongest protections– A 2003 Colorado statute reads, “In any civil action brought by an alleged victim of an unanticipated outcome of medical care…. any and all statements, affirmations, gestures, or conduct expressing apology, fault, sympathy, commiseration, condolence, compassion, or a general sense of benevolence which are made by a health care provider…. related to the discomfort, pain, suffering, injury, or death of the alleged victim as the result of the unanticipated outcome of medical care shall be inadmissible as evidence of an admission of liability. ”
State Protections for Disclosure Vary Many states offer immunity for sympathy but not for statements of fault. Colorado has one of the strongest protections– A 2003 Colorado statute reads, “In any civil action brought by an alleged victim of an unanticipated outcome of medical care…. any and all statements, affirmations, gestures, or conduct expressing apology, fault, sympathy, commiseration, condolence, compassion, or a general sense of benevolence which are made by a health care provider…. related to the discomfort, pain, suffering, injury, or death of the alleged victim as the result of the unanticipated outcome of medical care shall be inadmissible as evidence of an admission of liability. ”
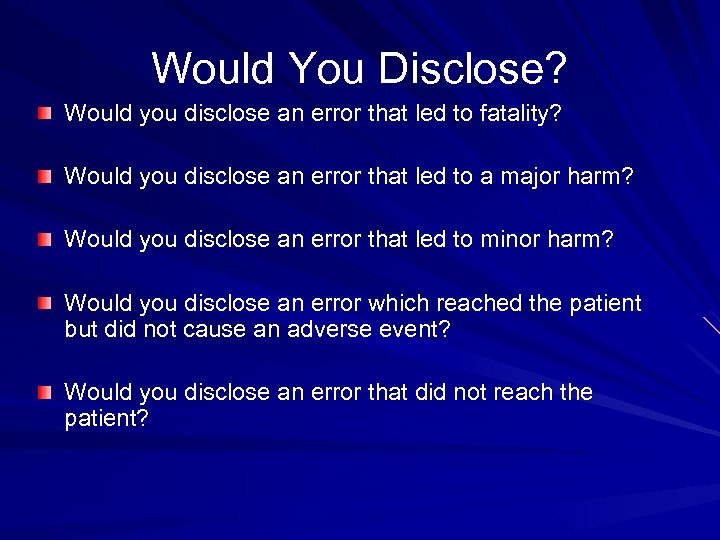 Would You Disclose? Would you disclose an error that led to fatality? Would you disclose an error that led to a major harm? Would you disclose an error that led to minor harm? Would you disclose an error which reached the patient but did not cause an adverse event? Would you disclose an error that did not reach the patient?
Would You Disclose? Would you disclose an error that led to fatality? Would you disclose an error that led to a major harm? Would you disclose an error that led to minor harm? Would you disclose an error which reached the patient but did not cause an adverse event? Would you disclose an error that did not reach the patient?
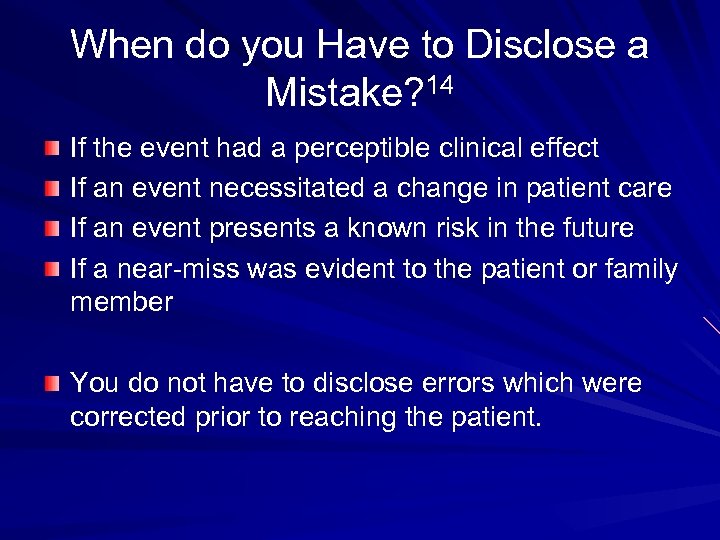 When do you Have to Disclose a Mistake? 14 If the event had a perceptible clinical effect If an event necessitated a change in patient care If an event presents a known risk in the future If a near-miss was evident to the patient or family member You do not have to disclose errors which were corrected prior to reaching the patient.
When do you Have to Disclose a Mistake? 14 If the event had a perceptible clinical effect If an event necessitated a change in patient care If an event presents a known risk in the future If a near-miss was evident to the patient or family member You do not have to disclose errors which were corrected prior to reaching the patient.
 Two Forms of Regret § “I’ m sorry your dog was run over” versus § “I’m sorry I ran over your dog” The first apology is appropriate for a complication that occurs despite standard of care. The second is the more appropriate apology for a medical error.
Two Forms of Regret § “I’ m sorry your dog was run over” versus § “I’m sorry I ran over your dog” The first apology is appropriate for a complication that occurs despite standard of care. The second is the more appropriate apology for a medical error.
 How do you accomplish this? Preparation Setting Participants Body Language Content
How do you accomplish this? Preparation Setting Participants Body Language Content
 Preparation Make sure the facts are known completely before disclosure. It is appropriate to tell a patient or family that an adverse event is being investigated prior to your full discussion with them. – This may require two meetings to do correctly Discuss an medical error leading to major adverse event, especially if it involves other individuals, with risk management prior to talking to family
Preparation Make sure the facts are known completely before disclosure. It is appropriate to tell a patient or family that an adverse event is being investigated prior to your full discussion with them. – This may require two meetings to do correctly Discuss an medical error leading to major adverse event, especially if it involves other individuals, with risk management prior to talking to family
 Setting The setting should be one that conveys calm. Participants should be at the same level, preferably sitting. Avoid interruptions.
Setting The setting should be one that conveys calm. Participants should be at the same level, preferably sitting. Avoid interruptions.
 Participants Avoid having too many people present. Avoid finger pointing between participants. You may want a representative from other disciplines (nursing, pharmacy) if the explanation of the error involves processes with which you are not familiar. You may want the patient care advocate. You may want a representative from risk management.
Participants Avoid having too many people present. Avoid finger pointing between participants. You may want a representative from other disciplines (nursing, pharmacy) if the explanation of the error involves processes with which you are not familiar. You may want the patient care advocate. You may want a representative from risk management.
 Body Language Patient and physician at the same level Open body posture (not crossing arms or legs) Leaning forward Avoiding expressions of psychomotor agitation (tapping feet). Unconscious mimicry of body position Eye contact
Body Language Patient and physician at the same level Open body posture (not crossing arms or legs) Leaning forward Avoiding expressions of psychomotor agitation (tapping feet). Unconscious mimicry of body position Eye contact
 Content Factual Explanation Expression of Regret Recognition of Distress Redress of Harm Keep it simple. Avoid becoming defensive. Take responsibility (if appropriate) Apologize personally (if appropriate )
Content Factual Explanation Expression of Regret Recognition of Distress Redress of Harm Keep it simple. Avoid becoming defensive. Take responsibility (if appropriate) Apologize personally (if appropriate )
 Content Offer concrete actions that will be taken to rectify the situation – You will need risk management to assist with any financial promises. Discuss how this event will create change in your actions or in the system.
Content Offer concrete actions that will be taken to rectify the situation – You will need risk management to assist with any financial promises. Discuss how this event will create change in your actions or in the system.
 Why do Apologies Fail Appearing insincere Overly vague--“I am sorry for any errors that were made. ” Using passive tense--“Mistakes were made. ” Adding conditions--“If any errors occurred, then I am sorry. ” Unacceptable explanations--“I had to leave the surgery to go to the bank. ” Arrogance--“Even the best doctors make mistakes at times. ” A botched apology may be worse than no apology at all.
Why do Apologies Fail Appearing insincere Overly vague--“I am sorry for any errors that were made. ” Using passive tense--“Mistakes were made. ” Adding conditions--“If any errors occurred, then I am sorry. ” Unacceptable explanations--“I had to leave the surgery to go to the bank. ” Arrogance--“Even the best doctors make mistakes at times. ” A botched apology may be worse than no apology at all.
 Case of Difficult Disclosure Two volunteers – Transplant Recipient – Attending Physician post-transfer Not individual who committed the error of omission but was the doctor who cared for the patient for the last 4 days before error identified Pharmacist also did not catch error Lets Role Play!
Case of Difficult Disclosure Two volunteers – Transplant Recipient – Attending Physician post-transfer Not individual who committed the error of omission but was the doctor who cared for the patient for the last 4 days before error identified Pharmacist also did not catch error Lets Role Play!
 References 1. 2. 3. 4. 5. Wu AW, Folkman S, Mc. Phee SJ, Lo B. So House Officers Learn From Their Mistakes? JAMA 1991; 265: 2089 -2094 Gallagher TH, Waterman AD, Garbutt JM, et al. US and Canadian Physicians’ Attitudes and Experiences Regarding Disclosing Errors to Patients. Arch Intern Med 2006; 166: 1605 -1611 Boyle D, O’Connell D, Platt FW, Albert RK. Disclosing Errors and Adverse Events in the Intensive Care Unit. Crit Care Med 2006; 34: 1532 -1537 Gallagher TH, Waterman AD, Ebers AG, Fraser VJ, Levinson W. Patients’ and Physicians’ Attitudes Regarding the Disclosure of Medical Errors. JAMA 2003; 289: 1001 -1007 Gallagher TH, Garbutt JM, Waterman AD et al. Choosing Your Words Carefully: How Physicians Would Disclose Harmful Medical Errors to Patients. Arch Intern Med 2006; 166: 1585 -1593
References 1. 2. 3. 4. 5. Wu AW, Folkman S, Mc. Phee SJ, Lo B. So House Officers Learn From Their Mistakes? JAMA 1991; 265: 2089 -2094 Gallagher TH, Waterman AD, Garbutt JM, et al. US and Canadian Physicians’ Attitudes and Experiences Regarding Disclosing Errors to Patients. Arch Intern Med 2006; 166: 1605 -1611 Boyle D, O’Connell D, Platt FW, Albert RK. Disclosing Errors and Adverse Events in the Intensive Care Unit. Crit Care Med 2006; 34: 1532 -1537 Gallagher TH, Waterman AD, Ebers AG, Fraser VJ, Levinson W. Patients’ and Physicians’ Attitudes Regarding the Disclosure of Medical Errors. JAMA 2003; 289: 1001 -1007 Gallagher TH, Garbutt JM, Waterman AD et al. Choosing Your Words Carefully: How Physicians Would Disclose Harmful Medical Errors to Patients. Arch Intern Med 2006; 166: 1585 -1593
 References 6. 7. 8. 9. 10. Stewart RM, Corneille MG, Johnston J, et al. Transparent and Open Discussion of Errors Does Not Increase Malpractice Risk in Trauma Patients. Ann Surg 2006; 243: 645 -651 Witman AB, Park DM, Hardin SB. How Do Patients Want Physicians to Handle Mistakes? A Survey of Internal Medicine Patients in an Academic Setting. Arch Intern Med 1996; 156: abstract Mazor KM, Simon SR, Yood RA, et al. Health Plan Members’ Views About Disclosure of Medical Errors. Ann Intern Med 2004; 140: 409 -418 Gallagher TH, Studdert D, Levinson W. Disclosing Harmful Medical Errors to Patients. NEJM 2007; 356: 2713 -0 Brazeau C, Disclosing the Truth About a Medical Error. AAFP 1999; 60:
References 6. 7. 8. 9. 10. Stewart RM, Corneille MG, Johnston J, et al. Transparent and Open Discussion of Errors Does Not Increase Malpractice Risk in Trauma Patients. Ann Surg 2006; 243: 645 -651 Witman AB, Park DM, Hardin SB. How Do Patients Want Physicians to Handle Mistakes? A Survey of Internal Medicine Patients in an Academic Setting. Arch Intern Med 1996; 156: abstract Mazor KM, Simon SR, Yood RA, et al. Health Plan Members’ Views About Disclosure of Medical Errors. Ann Intern Med 2004; 140: 409 -418 Gallagher TH, Studdert D, Levinson W. Disclosing Harmful Medical Errors to Patients. NEJM 2007; 356: 2713 -0 Brazeau C, Disclosing the Truth About a Medical Error. AAFP 1999; 60:
 References 11. 12. 13. 14. 15. Lazare A. Apology in Medical Practice. JAMA 2006; 296: 14011404 Malaty W, Crane S. How Might Acknowledging a Medical Error Promote Patient Safety? Journal of Family Practice 55: 775 -780 Berlin L. Will Saying “I’m Sorry” Prevent a Malpractice Lawsuit? ARJ 2006; 187: 10 -15 Butterfield S. Apologize like a Pro. ACP Hospitalist Jan 2008: 14 -16 Hobgood C, et al. Parental Preferences for Error Disclosure, Reporting, and Legal Action After Medical Error in the Care of Their Children Pediatrics 2005; 116: 1276 -1286
References 11. 12. 13. 14. 15. Lazare A. Apology in Medical Practice. JAMA 2006; 296: 14011404 Malaty W, Crane S. How Might Acknowledging a Medical Error Promote Patient Safety? Journal of Family Practice 55: 775 -780 Berlin L. Will Saying “I’m Sorry” Prevent a Malpractice Lawsuit? ARJ 2006; 187: 10 -15 Butterfield S. Apologize like a Pro. ACP Hospitalist Jan 2008: 14 -16 Hobgood C, et al. Parental Preferences for Error Disclosure, Reporting, and Legal Action After Medical Error in the Care of Their Children Pediatrics 2005; 116: 1276 -1286
 References 16. 17. 18. Kraman SS, Hamm G. Risk management: extreme honesty may be the best policy. Ann Intern Med 1999; 131: 963 -967 Clinton HR, Obama B. Making patient safety the centerpiece of medical liability reform. N Engl J Med 2006; 354: 2205 -2208 http: //www. callcopic. com/home/what-weoffer/coverages/medical-professional-liability-insuranceco/physicians-medical-practices/special-programs/3 rs-program/ Last accessed 2/28/2012.
References 16. 17. 18. Kraman SS, Hamm G. Risk management: extreme honesty may be the best policy. Ann Intern Med 1999; 131: 963 -967 Clinton HR, Obama B. Making patient safety the centerpiece of medical liability reform. N Engl J Med 2006; 354: 2205 -2208 http: //www. callcopic. com/home/what-weoffer/coverages/medical-professional-liability-insuranceco/physicians-medical-practices/special-programs/3 rs-program/ Last accessed 2/28/2012.


