 Medical Education in the UK
Medical Education in the UK
 ME Goal the production of physicians sensitive to the health needs of their country, capable of ministering to those needs, and aware of the necessity of continuing their own education.
ME Goal the production of physicians sensitive to the health needs of their country, capable of ministering to those needs, and aware of the necessity of continuing their own education.
 A Brief History of ME in the UK Early period: Oxford University has been teaching medicine since 13 th century William Harvey – circulation of blood research Thomas Willis - a neuroanatomist Christopher Wren - created a number of detailed anatomical drawings while at Oxford.
A Brief History of ME in the UK Early period: Oxford University has been teaching medicine since 13 th century William Harvey – circulation of blood research Thomas Willis - a neuroanatomist Christopher Wren - created a number of detailed anatomical drawings while at Oxford.
 A Brief History of ME in the UK Royal College of Physicians of London (1518) produced a system that called for examination of medical practitioners
A Brief History of ME in the UK Royal College of Physicians of London (1518) produced a system that called for examination of medical practitioners
 Oxford University In 1749 the Radcliffe Camera was built to house the first library in Oxford dedicated to science. Medical School in Edinburgh Alexander Monro – leading figure in teaching anatomy
Oxford University In 1749 the Radcliffe Camera was built to house the first library in Oxford dedicated to science. Medical School in Edinburgh Alexander Monro – leading figure in teaching anatomy
 A Brief History of ME in the UK 18 th century John Radcliffe founded the Radcliffe Infirmary (1770) one of the first public hospitals outside London;
A Brief History of ME in the UK 18 th century John Radcliffe founded the Radcliffe Infirmary (1770) one of the first public hospitals outside London;
 A Brief History of ME in the UK 19 th century Departments and professorships in anatomy, Comparative Anatomy and Physiology • Sir Charles Sherrington Chair in Physiology won the Nobel Prize for his fundamental studies of the nervous system; • clinical teaching developed with the arrival of Sir William Osler from Johns Hopkins University in 1904. •
A Brief History of ME in the UK 19 th century Departments and professorships in anatomy, Comparative Anatomy and Physiology • Sir Charles Sherrington Chair in Physiology won the Nobel Prize for his fundamental studies of the nervous system; • clinical teaching developed with the arrival of Sir William Osler from Johns Hopkins University in 1904. •
 A Brief History of ME in the UK Medical training in London Infirmaries and hospitals; informal arrangements between the physicians and surgeons of the hospitals and potential students; private anatomy schools which grew up near the hospitals towards the end of the eighteenth century. The London, St Thomas’s, Guy’s, St Bartholomew’s, the Middlesex, the Westminster and St George’s - biggest hospitals in London by the mid 19 th
A Brief History of ME in the UK Medical training in London Infirmaries and hospitals; informal arrangements between the physicians and surgeons of the hospitals and potential students; private anatomy schools which grew up near the hospitals towards the end of the eighteenth century. The London, St Thomas’s, Guy’s, St Bartholomew’s, the Middlesex, the Westminster and St George’s - biggest hospitals in London by the mid 19 th
 St Bartholomew's Hospital, London
St Bartholomew's Hospital, London
 Modern Pattern of ME Premedical Undergraduate Postgraduate Continuing education
Modern Pattern of ME Premedical Undergraduate Postgraduate Continuing education
 Premedical courses in UK Pre-Medical Studies course is designed for students whose A level mix does not allow direct entry to Medicine The course is designed to prepare for a successful entry to medical school and subsequent career. Successful students on the course gain a Certificate in Higher Education. On this one-year course, students take a total of 15 modules covering a range of subjects including: Anatomy and Tissue Structure; Introduction to Biomedical Science; Genetics; Hormones and Development; Infection and Immunity, and Human Physiology. http: //www. lancaster. ac. uk/
Premedical courses in UK Pre-Medical Studies course is designed for students whose A level mix does not allow direct entry to Medicine The course is designed to prepare for a successful entry to medical school and subsequent career. Successful students on the course gain a Certificate in Higher Education. On this one-year course, students take a total of 15 modules covering a range of subjects including: Anatomy and Tissue Structure; Introduction to Biomedical Science; Genetics; Hormones and Development; Infection and Immunity, and Human Physiology. http: //www. lancaster. ac. uk/
 Undergraduate Education The medical curriculum may vary in modules and length; In Britain five years is normal time Medical schools usually begin their work with the study of the structure of the body and its formation: anatomy, histology, and embryology. Then come studies related to function—i. e. , physiology, biochemistry, pharmacology, and, in many schools, biophysics. After the microscopic study of normal tissues (histology) has begun, the student is usually introduced to pathological anatomy, bacteriology, immunology, parasitology—in short, to the agents of disease and the changes that they cause in the structure and function of the tissues
Undergraduate Education The medical curriculum may vary in modules and length; In Britain five years is normal time Medical schools usually begin their work with the study of the structure of the body and its formation: anatomy, histology, and embryology. Then come studies related to function—i. e. , physiology, biochemistry, pharmacology, and, in many schools, biophysics. After the microscopic study of normal tissues (histology) has begun, the student is usually introduced to pathological anatomy, bacteriology, immunology, parasitology—in short, to the agents of disease and the changes that they cause in the structure and function of the tissues
 Undergraduate Education courses in medical psychology, biostatistics, public health, alcoholism, biomedical engineering, emergency medicine, ethical problems are becoming more common in the first years of the medical curriculum. active student participation in small group conferences and discussions; a decrease in the number of formal lectures, an increase in the amount of contact with patients in teaching hospitals and clinics; clinical work begins with general medicine and surgery and goes on to include the major clinical specialties, including obstetrics and gynecology, pediatrics, disorders of the eye, ear, nose, throat, and skin, and psychiatry. students work in the hospital’s outpatient, emergency, and radiology departments, diagnostic laboratories, and surgical theatres.
Undergraduate Education courses in medical psychology, biostatistics, public health, alcoholism, biomedical engineering, emergency medicine, ethical problems are becoming more common in the first years of the medical curriculum. active student participation in small group conferences and discussions; a decrease in the number of formal lectures, an increase in the amount of contact with patients in teaching hospitals and clinics; clinical work begins with general medicine and surgery and goes on to include the major clinical specialties, including obstetrics and gynecology, pediatrics, disorders of the eye, ear, nose, throat, and skin, and psychiatry. students work in the hospital’s outpatient, emergency, and radiology departments, diagnostic laboratories, and surgical theatres.
 Undergraduate degree the academic degree after undergraduate studies is bachelor of medicine (M. B) and of Surgery (B. S. ) Only after further study is the M. D. degree given.
Undergraduate degree the academic degree after undergraduate studies is bachelor of medicine (M. B) and of Surgery (B. S. ) Only after further study is the M. D. degree given.
 Postgraduate education Foundation Programme 2 years graduate training and experience in a hospital under the supervision of competent clinicians and other teachers. Specialty Training advanced training in a hospital specialty 6 years Specialty Registrar (Sp. R) or advanced training in general practice 3 years Specialty Registrar (GPST)
Postgraduate education Foundation Programme 2 years graduate training and experience in a hospital under the supervision of competent clinicians and other teachers. Specialty Training advanced training in a hospital specialty 6 years Specialty Registrar (Sp. R) or advanced training in general practice 3 years Specialty Registrar (GPST)
 The UK Foundation Programme Curriculum The Foundation Programme Curriculum (the Curriculum) sets out the framework for educational progression that will support the first two years of professional development after graduation from medical school. Contains 14 modules structured as syllabus and competences 1. Professionalism 2. Good clinical care 3. Recognition and management of the acutely ill patient 4. Resuscitation 5. Discharge and planning for chronic disease management 6. Relationship with patients and communication skills etc.
The UK Foundation Programme Curriculum The Foundation Programme Curriculum (the Curriculum) sets out the framework for educational progression that will support the first two years of professional development after graduation from medical school. Contains 14 modules structured as syllabus and competences 1. Professionalism 2. Good clinical care 3. Recognition and management of the acutely ill patient 4. Resuscitation 5. Discharge and planning for chronic disease management 6. Relationship with patients and communication skills etc.
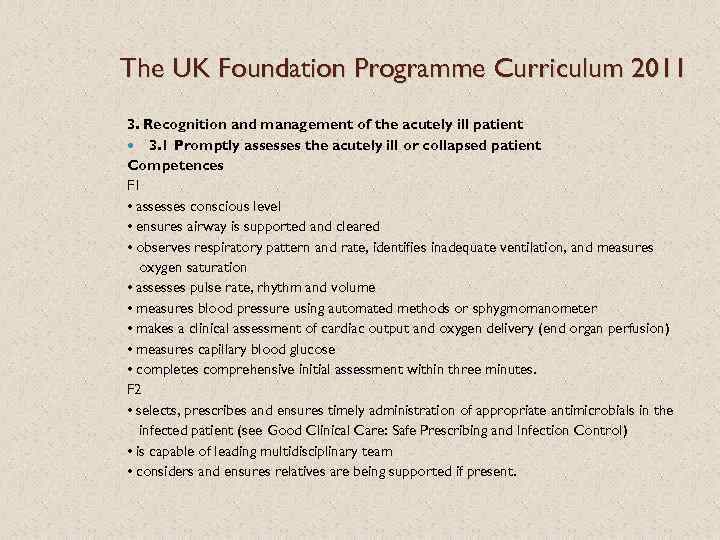 The UK Foundation Programme Curriculum 2011 3. Recognition and management of the acutely ill patient 3. 1 Promptly assesses the acutely ill or collapsed patient Competences F 1 • assesses conscious level • ensures airway is supported and cleared • observes respiratory pattern and rate, identifies inadequate ventilation, and measures oxygen saturation • assesses pulse rate, rhythm and volume • measures blood pressure using automated methods or sphygmomanometer • makes a clinical assessment of cardiac output and oxygen delivery (end organ perfusion) • measures capillary blood glucose • completes comprehensive initial assessment within three minutes. F 2 • selects, prescribes and ensures timely administration of appropriate antimicrobials in the infected patient (see Good Clinical Care: Safe Prescribing and Infection Control) • is capable of leading multidisciplinary team • considers and ensures relatives are being supported if present.
The UK Foundation Programme Curriculum 2011 3. Recognition and management of the acutely ill patient 3. 1 Promptly assesses the acutely ill or collapsed patient Competences F 1 • assesses conscious level • ensures airway is supported and cleared • observes respiratory pattern and rate, identifies inadequate ventilation, and measures oxygen saturation • assesses pulse rate, rhythm and volume • measures blood pressure using automated methods or sphygmomanometer • makes a clinical assessment of cardiac output and oxygen delivery (end organ perfusion) • measures capillary blood glucose • completes comprehensive initial assessment within three minutes. F 2 • selects, prescribes and ensures timely administration of appropriate antimicrobials in the infected patient (see Good Clinical Care: Safe Prescribing and Infection Control) • is capable of leading multidisciplinary team • considers and ensures relatives are being supported if present.
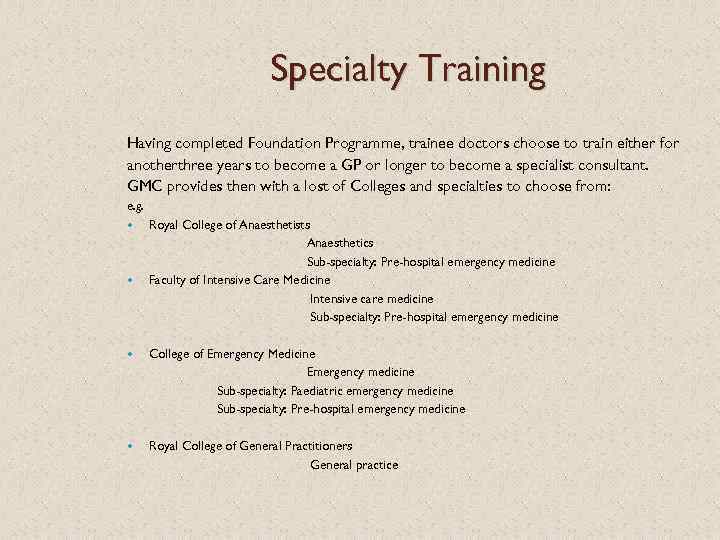 Specialty Training Having completed Foundation Programme, trainee doctors choose to train either for anotherthree years to become a GP or longer to become a specialist consultant. GMC provides then with a lost of Colleges and specialties to choose from: e. g. Royal College of Anaesthetists Anaesthetics Sub-specialty: Pre-hospital emergency medicine Faculty of Intensive Care Medicine Intensive care medicine Sub-specialty: Pre-hospital emergency medicine College of Emergency Medicine Emergency medicine Sub-specialty: Paediatric emergency medicine Sub-specialty: Pre-hospital emergency medicine Royal College of General Practitioners General practice
Specialty Training Having completed Foundation Programme, trainee doctors choose to train either for anotherthree years to become a GP or longer to become a specialist consultant. GMC provides then with a lost of Colleges and specialties to choose from: e. g. Royal College of Anaesthetists Anaesthetics Sub-specialty: Pre-hospital emergency medicine Faculty of Intensive Care Medicine Intensive care medicine Sub-specialty: Pre-hospital emergency medicine College of Emergency Medicine Emergency medicine Sub-specialty: Paediatric emergency medicine Sub-specialty: Pre-hospital emergency medicine Royal College of General Practitioners General practice
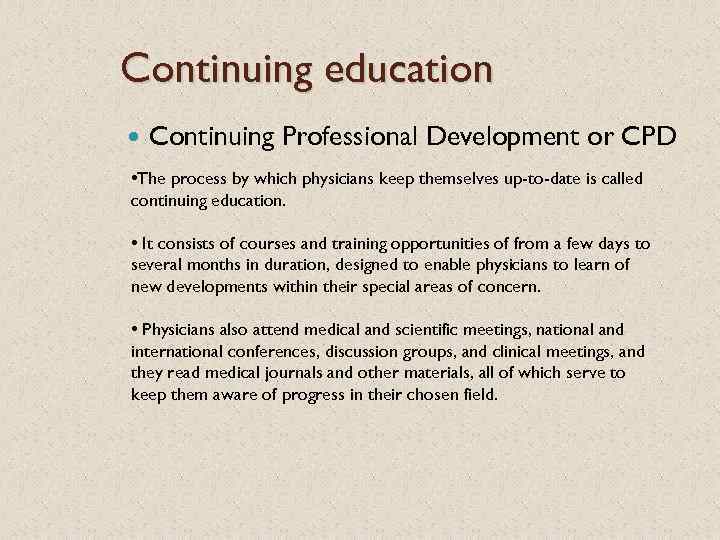 Continuing education Continuing Professional Development or CPD • The process by which physicians keep themselves up-to-date is called continuing education. • It consists of courses and training opportunities of from a few days to several months in duration, designed to enable physicians to learn of new developments within their special areas of concern. • Physicians also attend medical and scientific meetings, national and international conferences, discussion groups, and clinical meetings, and they read medical journals and other materials, all of which serve to keep them aware of progress in their chosen field.
Continuing education Continuing Professional Development or CPD • The process by which physicians keep themselves up-to-date is called continuing education. • It consists of courses and training opportunities of from a few days to several months in duration, designed to enable physicians to learn of new developments within their special areas of concern. • Physicians also attend medical and scientific meetings, national and international conferences, discussion groups, and clinical meetings, and they read medical journals and other materials, all of which serve to keep them aware of progress in their chosen field.
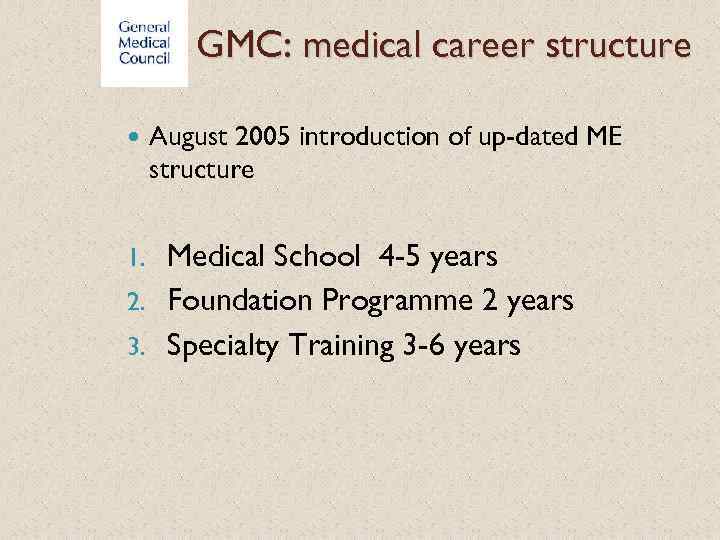 GMC: medical career structure August 2005 introduction of up-dated ME structure Medical School 4 -5 years 2. Foundation Programme 2 years 3. Specialty Training 3 -6 years 1.
GMC: medical career structure August 2005 introduction of up-dated ME structure Medical School 4 -5 years 2. Foundation Programme 2 years 3. Specialty Training 3 -6 years 1.
 GMC Good Medical Practice 2006 Good Medical Practice is a guidance for doctors, which sets out the principles and values on which good practice is founded; these principles together describe medical professionalism in action. The guidance is addressed to doctors, but it is also intended to let the public know what they can expect from doctors.
GMC Good Medical Practice 2006 Good Medical Practice is a guidance for doctors, which sets out the principles and values on which good practice is founded; these principles together describe medical professionalism in action. The guidance is addressed to doctors, but it is also intended to let the public know what they can expect from doctors.
 The state of medical education and practice in the UK report: 2014 Key facts Medical students are concentrated in particular parts of the UK. Some parts of the UK are more reliant on doctors in training than others. The number of doctors not in training under 30 years old is increasing. London, Northern Ireland Scotland have more female doctors. Female doctors form a higher proportion of GPs and a lower proportion of specialists. Two thirds of doctors who are not GPs or specialists and not in training did not graduate in the UK. A higher proportion of specialists than GPs are IMGs. There is a higher proportion of UK graduates in Northern Ireland, Scotland the southwest of England. IMG - international medical graduate
The state of medical education and practice in the UK report: 2014 Key facts Medical students are concentrated in particular parts of the UK. Some parts of the UK are more reliant on doctors in training than others. The number of doctors not in training under 30 years old is increasing. London, Northern Ireland Scotland have more female doctors. Female doctors form a higher proportion of GPs and a lower proportion of specialists. Two thirds of doctors who are not GPs or specialists and not in training did not graduate in the UK. A higher proportion of specialists than GPs are IMGs. There is a higher proportion of UK graduates in Northern Ireland, Scotland the southwest of England. IMG - international medical graduate
 References http: //www. gmc-uk. org/somep 2014/webappendix
References http: //www. gmc-uk. org/somep 2014/webappendix


