a14d3d2663981fde724c340056a2c13d.ppt
- Количество слайдов: 59

Medical Assistance Program Oversight Council December 13, 2013 Presented by: Value. Options®, Connecticut on Behalf of the Connecticut Behavioral Health Partnership (CT BHP) 1
What is the Connecticut Behavioral Health Partnership (CT BHP)? A partnership among three state agencies: • Department of Children and Families (DCF) • Department of Mental Health & Addiction Services (DMHAS) • Department of Social Services (DSS) 2

Levels of Care Managed • Inpatient Hospital • Inpatient Detox • Observation Beds • Residential Detox • Ambulatory Detox • Methadone Maintenance • Partial Hospitalization Programs (PHP) • Extended Day Treatment • Intensive Outpatient Treatment 3 • Outpatient • Psychological Testing • Adult Mental Health Group Homes • Home Health • Psychiatric Residential Treatment Facilities (PRTF) • Residential and Group Homes for Children • Group Homes for Adults
Program Information Covers approximately 648, 000 individuals Began managing BH services for youth and families in 2006, and for adults in 2011 Manages core Medicaid services and grant-funded interventions including residential care and intensive home-based treatment 4
Value. Options, Connecticut VO CT is part of Value. Options, the nation’s largest independent behavioral health and wellness company. We serve 32 million individuals across the country. VO developed Stamp Out Stigma, an award-winning national initiative to foster a dialogue on mental illness, and to provide resources to those in need of help. As the ASO for the Partnership, Value. Options, Connecticut § supports and improves individual outcomes § effectively manages state resources § promotes federal participation in the funding of behavioral health services 5
Value. Options, Connecticut • Contract Construct – Cost Plus Administrative Contract – Performance Standards (fines for noncompliance with standards) – Performance Targets (administrative fee is withheld pending successful completion) 6

A Regional Approach One of CT BHP’s primary goals is to ensure that people receive the services they need in their local communities. To that end, CT BHP operates in Geographic Teams that focus on each region of the state. 7
Intensive Care Management (ICM) and Peer Services at the CT BHP 8

Why Intensive Care Management? • Persons with SPMI (severe and persistent mental illness) have their lifespans shortened, on average, 15 to 25 years compared to their aged peers • Persons with a chronic medical condition and untreated mental health conditions experience 50% to 100% higher treatment costs • Utilized at both the member and facility level to impact care and quality outcomes 9
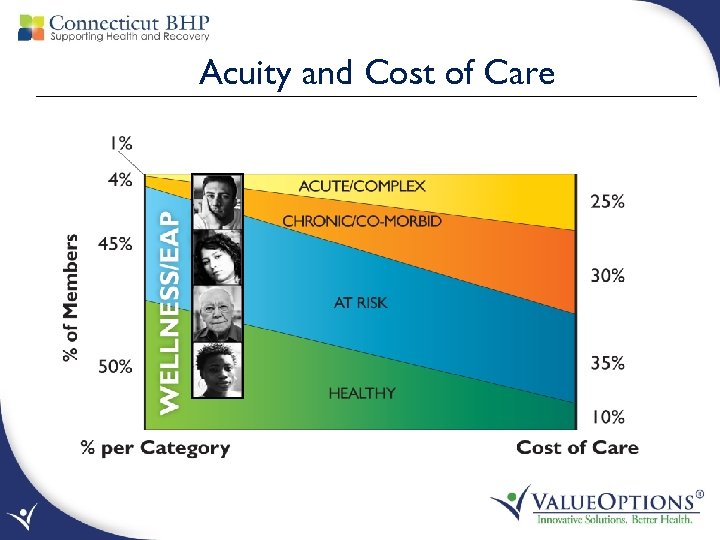
Acuity and Cost of Care
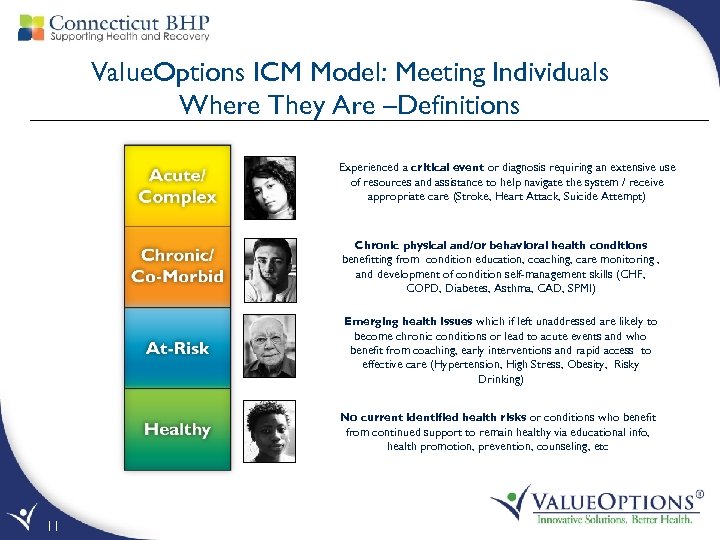
Value. Options ICM Model: Meeting Individuals Where They Are –Definitions Experienced a critical event or diagnosis requiring an extensive use of resources and assistance to help navigate the system / receive appropriate care (Stroke, Heart Attack, Suicide Attempt) Chronic physical and/or behavioral health conditions benefitting from condition education, coaching, care monitoring , and development of condition self-management skills (CHF, COPD, Diabetes, Asthma, CAD, SPMI) Emerging health issues which if left unaddressed are likely to become chronic conditions or lead to acute events and who benefit from coaching, early interventions and rapid access to effective care (Hypertension, High Stress, Obesity, Risky Drinking) No current identified health risks or conditions who benefit from continued support to remain healthy via educational info, health promotion, prevention, counseling, etc 11
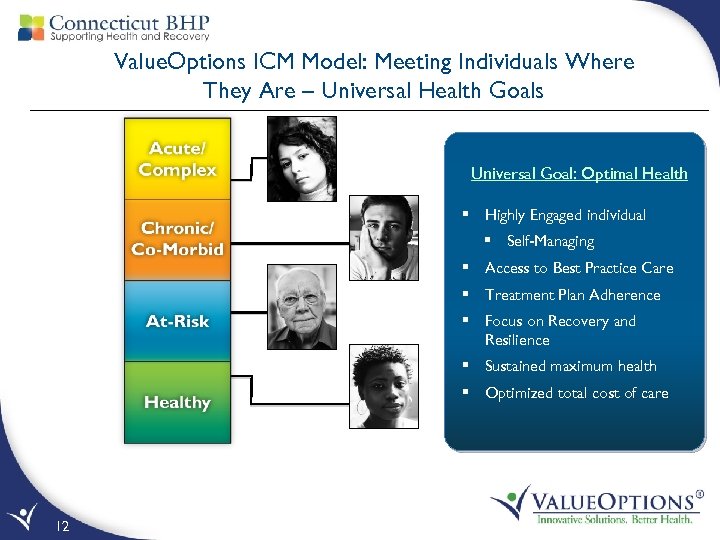
Value. Options ICM Model: Meeting Individuals Where They Are – Universal Health Goals Universal Goal: Optimal Health § Highly Engaged individual § Self-Managing § Access to Best Practice Care § Treatment Plan Adherence § Focus on Recovery and Resilience § Sustained maximum health § Optimized total cost of care 12
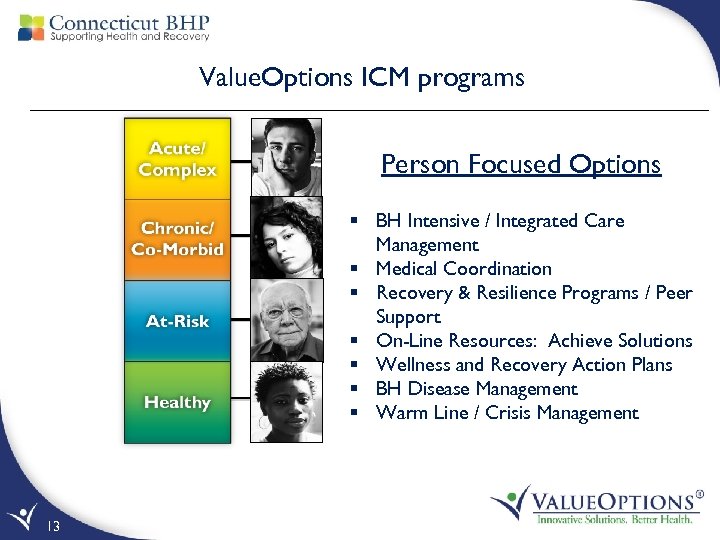
Value. Options ICM programs Person Focused Options § BH Intensive / Integrated Care Management § Medical Coordination § Recovery & Resilience Programs / Peer Support § On-Line Resources: Achieve Solutions § Wellness and Recovery Action Plans § BH Disease Management § Warm Line / Crisis Management 13
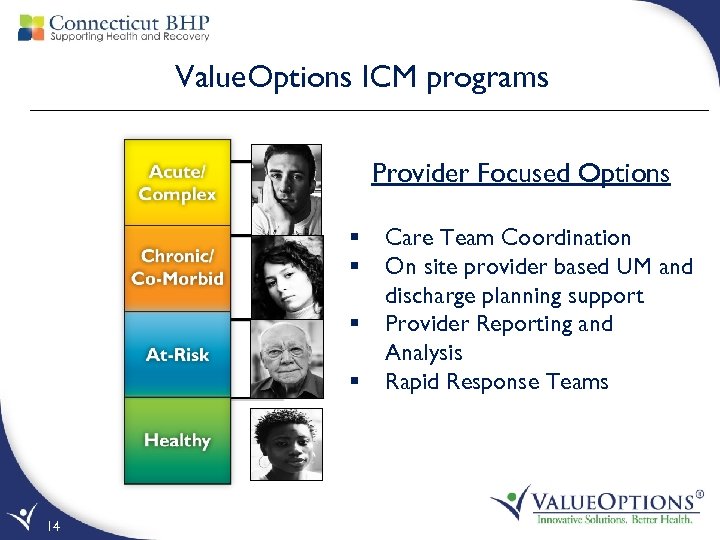
Value. Options ICM programs Provider Focused Options § § 14 Care Team Coordination On site provider based UM and discharge planning support Provider Reporting and Analysis Rapid Response Teams
VO ICM Program Goals • Effectively identify high risk individuals with complex health conditions • Provide comprehensive needs assessment for all identified at risk members • Provide individualized care management via appropriate outreach including assessment, assistance, coordination and consultation related to health care benefits • Develop increased self-care health management skills • Assure efficient benefit utilization via established criteria, guidelines, policies, and benefits 15
VO ICM Program Goals, continued • Orchestrate member centric care plans – input from member, care givers, and treatment providers • Assure effective resource access to help members and families to effectively cope with the stress and life changes resulting from living with behavioral health conditions • Support increased health, wellness, independence and optimal psycho-social functioning with minimal symptom burden, leading to a meaningful life in the community 16
Effective Member Engagement Person-Centered Approach • • Invitation to change rather than coercion Culturally relevant Therapeutic relationship / not therapy Promoting self management versus dependency Recovery principles infused throughout the program/process Motivational enhancement – pacing and matching readiness Balancing agendas – person centered ‘here & now interests’ with ‘potential beyond the present’ • Balancing care/compassion and focused interactions • Building on successes 17
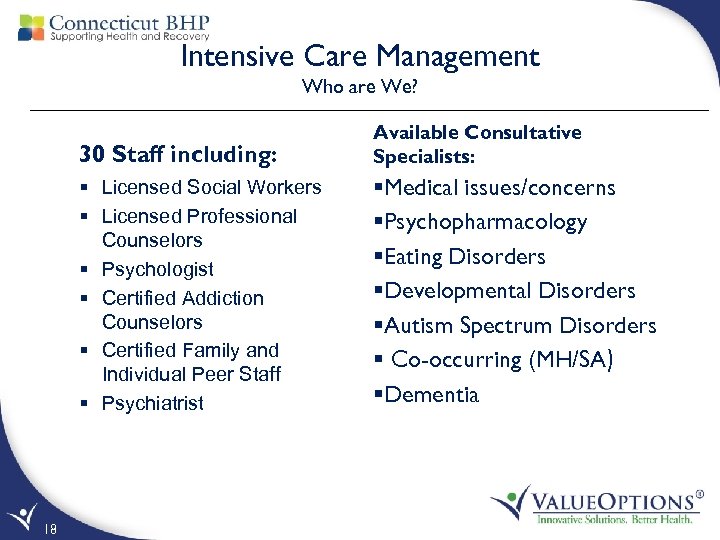
Intensive Care Management Who are We? 30 Staff including: § Licensed Social Workers § Licensed Professional Counselors § Psychologist § Certified Addiction Counselors § Certified Family and Individual Peer Staff § Psychiatrist 18 Available Consultative Specialists: §Medical issues/concerns §Psychopharmacology §Eating Disorders §Developmental Disorders §Autism Spectrum Disorders § Co-occurring (MH/SA) §Dementia
Intensive Care Management How Do We Do it? § Face to face Outreach § Emergency Departments, Inpatient settings, Community Settings, Home, Shelters § § 19 Telephonic Support Assessment of members’ needs Person Centered Care Planning using evidence based approach (WRAP) Cultural competent and sensitive planning via a Recovery oriented framework
Recovery and Resiliency Aspirations • Strengths based focus (beyond deficits) – key to engagement • Hope /restoration of a meaningful life possible, despite serious mental health conditions and within the context of the individuals beliefs/culture • Goal is restoration of self esteem/ identity and attaining a fulfilling life in community • Goal can be but is not simply symptom relief (medical model) • Individual is active participant of process not passive • Individual becomes self-managing 20
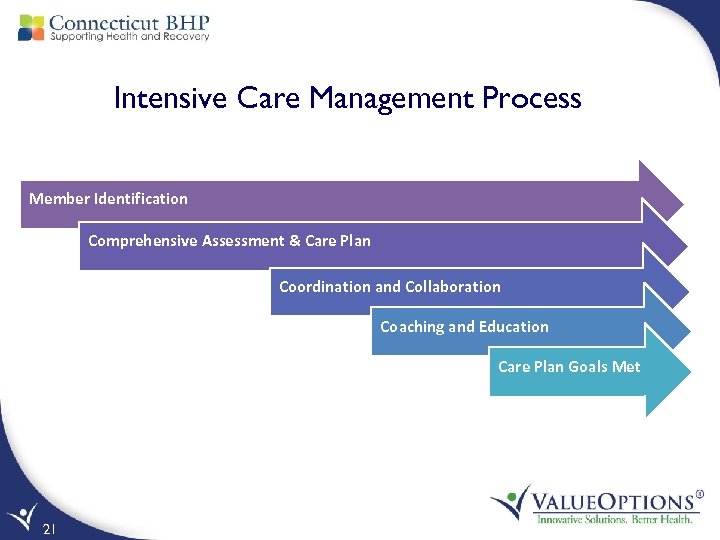
Intensive Care Management Process Member Identification Comprehensive Assessment & Care Plan Coordination and Collaboration Coaching and Education Care Plan Goals Met 21
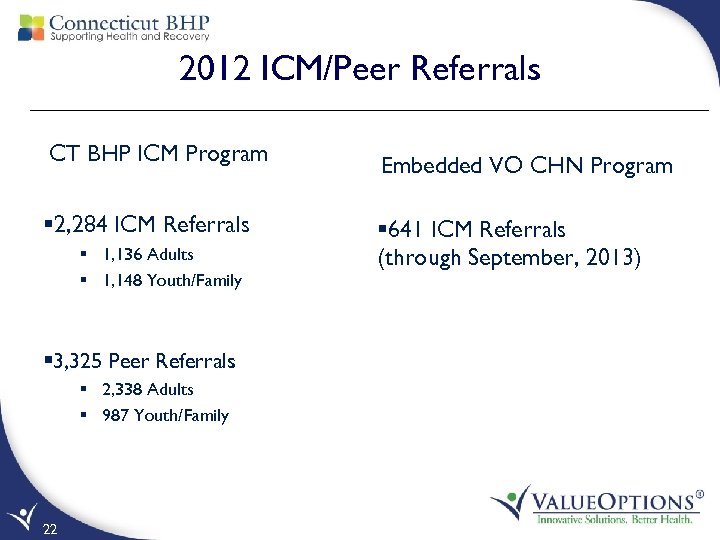
2012 ICM/Peer Referrals CT BHP ICM Program § 2, 284 ICM Referrals § 1, 136 Adults § 1, 148 Youth/Family § 3, 325 Peer Referrals § 2, 338 Adults § 987 Youth/Family 22 Embedded VO CHN Program § 641 ICM Referrals (through September, 2013)
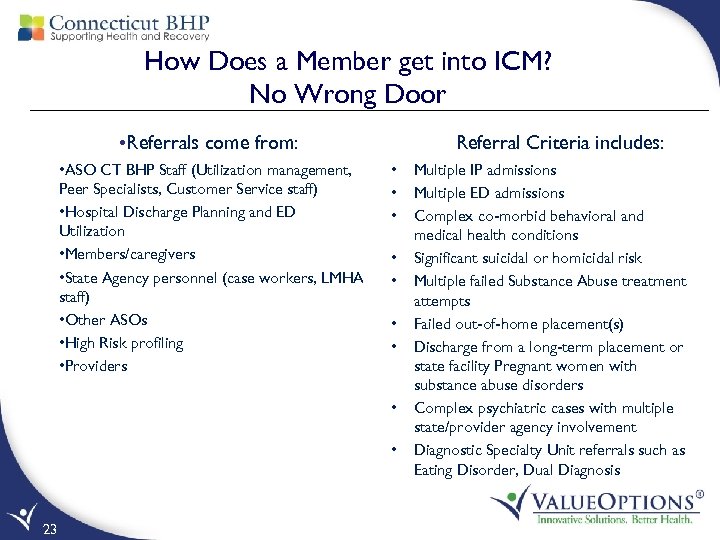
How Does a Member get into ICM? No Wrong Door • Referrals come from: • ASO CT BHP Staff (Utilization management, Peer Specialists, Customer Service staff) • Hospital Discharge Planning and ED Utilization • Members/caregivers • State Agency personnel (case workers, LMHA staff) • Other ASOs • High Risk profiling • Providers Referral Criteria includes: • • • 23 Multiple IP admissions Multiple ED admissions Complex co-morbid behavioral and medical health conditions Significant suicidal or homicidal risk Multiple failed Substance Abuse treatment attempts Failed out-of-home placement(s) Discharge from a long-term placement or state facility Pregnant women with substance abuse disorders Complex psychiatric cases with multiple state/provider agency involvement Diagnostic Specialty Unit referrals such as Eating Disorder, Dual Diagnosis
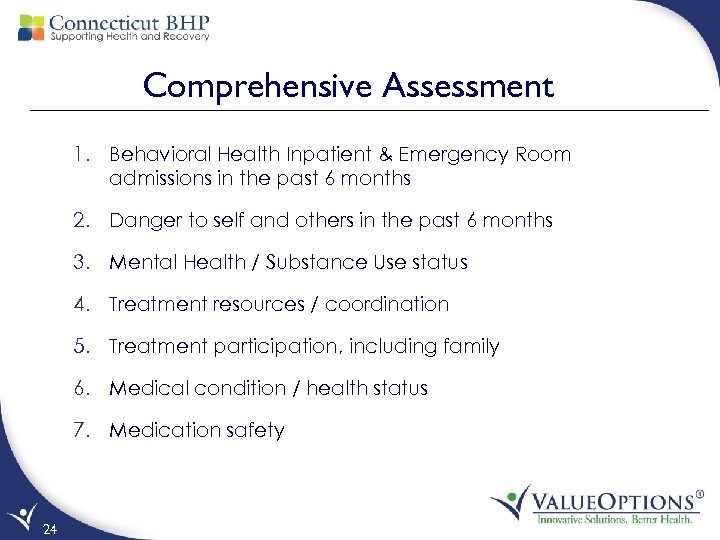
Comprehensive Assessment 1. Behavioral Health Inpatient & Emergency Room admissions in the past 6 months 2. Danger to self and others in the past 6 months 3. Mental Health / Substance Use status 4. Treatment resources / coordination 5. Treatment participation, including family 6. Medical condition / health status 7. Medication safety 24
Comprehensive Assessment (continued) 8. Barriers to care: a) b) Legal Issues – self or family c) Housing – out of home placement d) Transportation e) Cultural / Linguistic Issues f) Social Support / Natural Supports / Faith-Based Supports g) School / Employment h) 25 Finance – self or family Other Disabilities (vision, hearing, mobility)
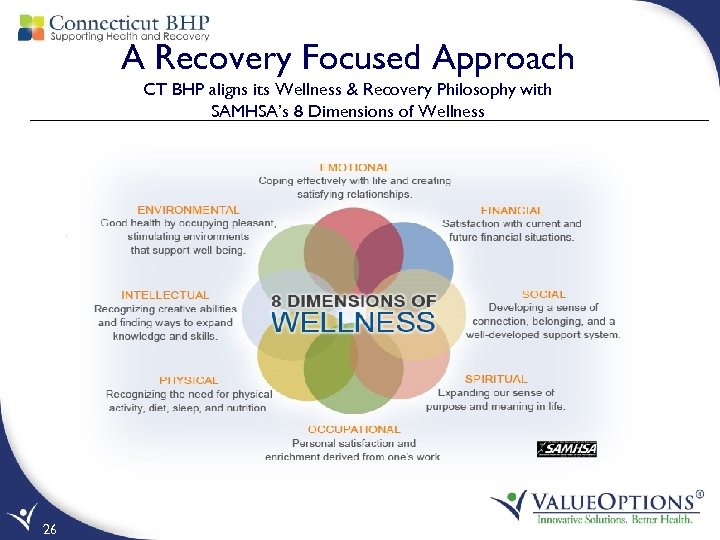
A Recovery Focused Approach CT BHP aligns its Wellness & Recovery Philosophy with SAMHSA’s 8 Dimensions of Wellness 26
A Recovery Focused Approach to Care Planning Wellness and Recovery Action Plans Wellness & Recovery Action Plan Components: Ø Short & Long term goals Ø Interventions Ø Progress toward goals Ø Individual’s involvement with plan Ø Family/Care team involvement with plan Ø Individual receives copy of W&R plan Ø Individual’s hope for recovery/resiliency (their words) Ø Discharge plan 27
Wellness and Recovery Action Planning (cont. ) Identify, Assess and Develop the following: • Current supports – Care team • Living arrangements/housing • Strengths and functioning • Independence level • Safety concerns • Current substance use • Medical/special needs • Triggers/Risk factors • Proactive crisis plan 28
Immediate Needs Addressed CT BHP Peer staff received 12, 355 member calls in 2012 Major Areas included: • Coaching/mentoring supports • Provider Referrals • Community supports Ø Basic Needs Ø 211 Info line Ø DCF Care Coordination Ø Housing assistance Ø Support Groups (NAMI/CCAR) 29
Member Self Direction in Setting Goals Alberto - 68 year old with multiple health issues: Medicaid disabled – Wheelchair bound, hypertension, COPD and on Methadone Maintenance. Being transported >25 miles daily for methadone treatment after moving from one town to another. Assessment: Coordinated with Alberto and community providers to find treatment options closer to home. He expressed his need for continued support and medication assisted therapy to enhance his recovery efforts. Outcome: ICM arranged transfer of care to a methadone clinic within the individual’s home town. Transition was seamless for the individual as all care and records transferred in a timely manner. He had no disruption in treatment. 30
ICM Coordination and Collaboration Supporting the Member and any identified person as part of the care team to work together across all elements of the service delivery system to assure a whole health perspective Coordinate and link individuals with providers to ensure consistent health care management • DMHAS programs/services • ABH Care Coordination • DCF Case Workers • Home Health • Span of BH providers • Primary Care • Transportation • Regional Action Councils, Community Collaboratives 31 Collaborate with members: • Family/caregivers with proper consent when indicated • Health care providers • State agencies and Schools • Waiver programs • Community Supports • Clubhouses, supported housing, Social Clubs, SNAP benefits, food banks, diaper banks, etc
Peer and Family Peer Specialists A Peer is an individual with lived experience, either through a family members encounter with the behavioral health system, or through their own Peers are trained in the following areas: • Certified Recovery Support Specialist (Advocacy Unlimited) • Certified as an Addiction & Recovery Coach (CCAR) • WRAP (Wellness and Recovery Action Planning – an evidenced based model for care planning) • Health Promotion (National VO training which includes chronic illness and motivational interviewing) 32
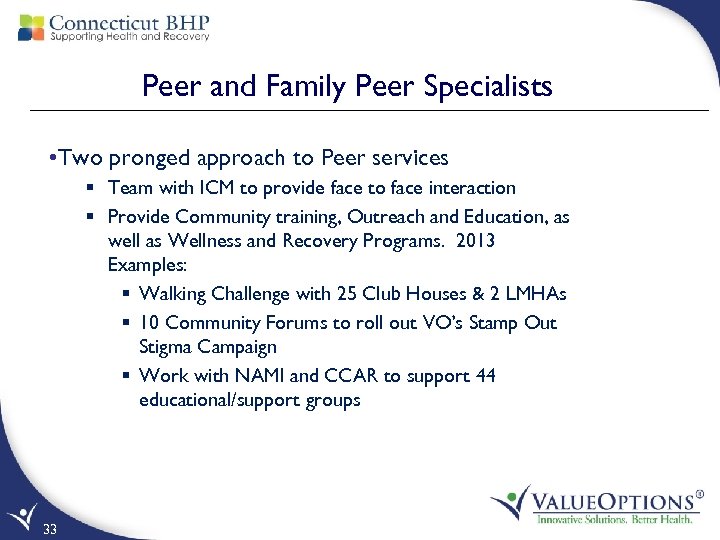
Peer and Family Peer Specialists • Two pronged approach to Peer services § Team with ICM to provide face to face interaction § Provide Community training, Outreach and Education, as well as Wellness and Recovery Programs. 2013 Examples: § Walking Challenge with 25 Club Houses & 2 LMHAs § 10 Community Forums to roll out VO’s Stamp Out Stigma Campaign § Work with NAMI and CCAR to support 44 educational/support groups 33
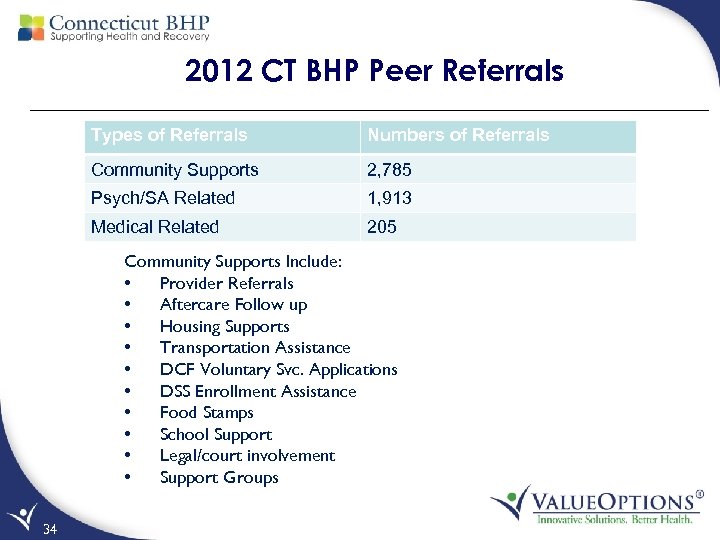
2012 CT BHP Peer Referrals Types of Referrals Numbers of Referrals Community Supports 2, 785 Psych/SA Related 1, 913 Medical Related 205 Community Supports Include: • Provider Referrals • Aftercare Follow up • Housing Supports • Transportation Assistance • DCF Voluntary Svc. Applications • DSS Enrollment Assistance • Food Stamps • School Support • Legal/court involvement • Support Groups 34
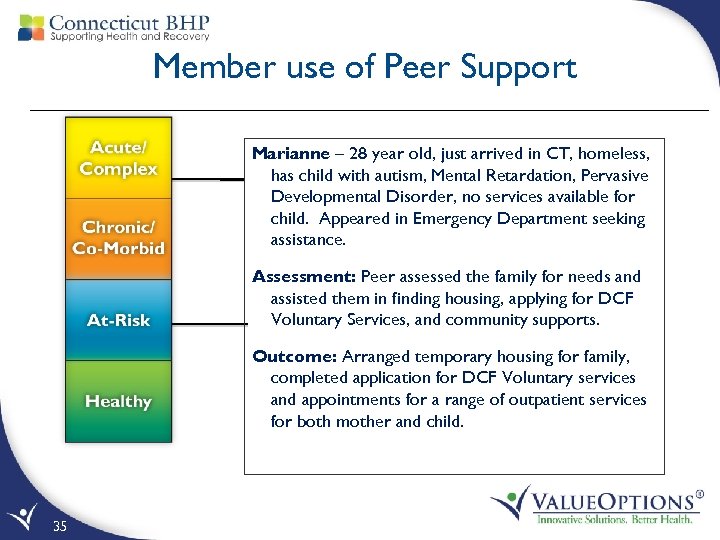
Member use of Peer Support Marianne – 28 year old, just arrived in CT, homeless, has child with autism, Mental Retardation, Pervasive Developmental Disorder, no services available for child. Appeared in Emergency Department seeking assistance. Assessment: Peer assessed the family for needs and assisted them in finding housing, applying for DCF Voluntary Services, and community supports. Outcome: Arranged temporary housing for family, completed application for DCF Voluntary services and appointments for a range of outpatient services for both mother and child. 35
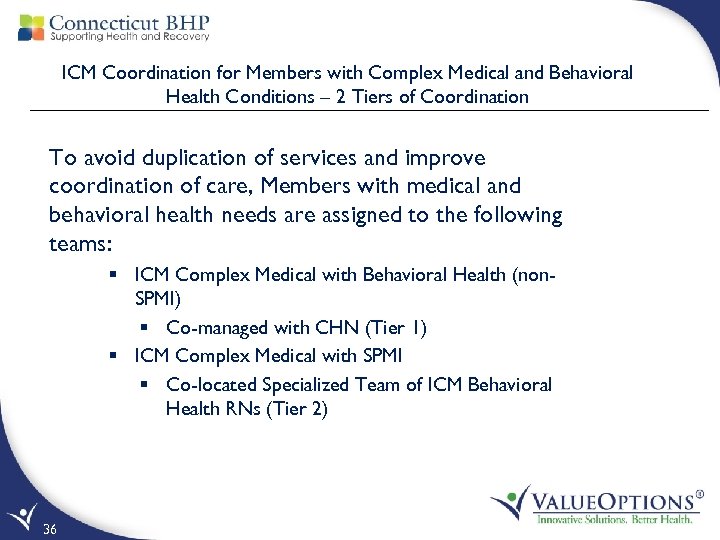
ICM Coordination for Members with Complex Medical and Behavioral Health Conditions – 2 Tiers of Coordination To avoid duplication of services and improve coordination of care, Members with medical and behavioral health needs are assigned to the following teams: § ICM Complex Medical with Behavioral Health (non. SPMI) § Co-managed with CHN (Tier 1) § ICM Complex Medical with SPMI § Co-located Specialized Team of ICM Behavioral Health RNs (Tier 2) 36
Coordination of Medical Needs at Any Level of Member Engagement (Tier 1) • Inpatient Level of Care – Multidisciplinary hospital case rounds including CHN staff twice weekly to: • • 37 Coordinate discharge planning Develop strategies to engage individuals Discuss medication adherence Assign appropriate ICM/Peer contact
Coordination for Behavioral Health Needs at Any Level of Member Engagement (Tier 1) Community Level: • Regional ICM case rounds held month • Focused case rounds of high ED users and members with pain management issues • Monthly meetings with CHN to identify individuals receiving home care who may require ICM services • Monthly ICM case round with CHN • Crisis intervention with CHN for individuals with a BH issue • Coordination among ICM, CT BHP, and DMHAS for individuals in SA treatment 38
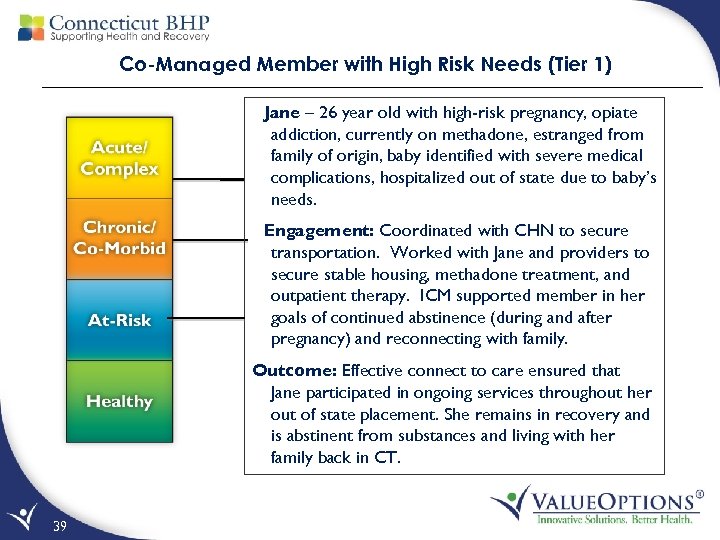
Co-Managed Member with High Risk Needs (Tier 1) Jane – 26 year old with high-risk pregnancy, opiate addiction, currently on methadone, estranged from family of origin, baby identified with severe medical complications, hospitalized out of state due to baby’s needs. Engagement: Coordinated with CHN to secure transportation. Worked with Jane and providers to secure stable housing, methadone treatment, and outpatient therapy. ICM supported member in her goals of continued abstinence (during and after pregnancy) and reconnecting with family. Outcome: Effective connect to care ensured that Jane participated in ongoing services throughout her out of state placement. She remains in recovery and is abstinent from substances and living with her family back in CT. 39
Co-Located VO/CHN ICM Program (Tier 2) • Intensive care management for those individuals with high risk medical needs and also serious and persistent behavioral health needs • Staffed by a team of behavioral health Registered Nurses (co-located with CHN in Wallingford) • Combination of telephonic and face-to-face care management service with the individual 40
Criteria for Tier 2 VO/CHN ICM • Criteria for condition identification: – Primary physical health condition – Severe and Persistent Mental Illness – At least one or more inpatient and/or ED event(s) in the most recent 12 months – Stratified according to intensity of need, informing the frequency and type of services – High Risk, Medium Risk and Low Risk – High Risk individuals receive face-to-face visits 41
Program Activities for Tier 2 VO/CHN ICM • Coordination of physical health an behavioral health care • Addresses gaps in care • System-level interventions • Person and provider specific strategies and care planning • Enhanced access to community resources • Provider member education • Collaboration and communication with applicable external entities 42
Program Activities for Tier 2 VO/CHN ICM • Person Driven Health and Wellness Recovery Plan • Incorporates Physical and Behavioral Health Action Items • Identifies ways to prevent a health crisis and ways to manage a health crisis 43
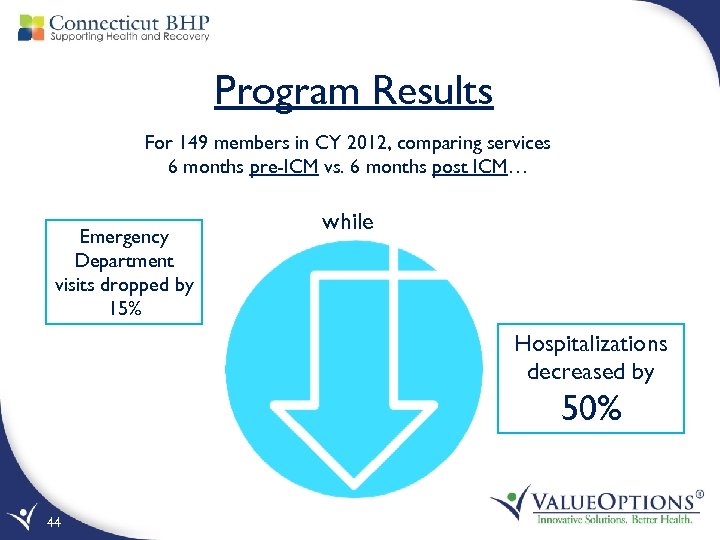
Program Results For 149 members in CY 2012, comparing services 6 months pre-ICM vs. 6 months post ICM… Emergency Department visits dropped by 15% while Hospitalizations decreased by 50% 44
VO/CHN Tier 2 Member Sierra- 57 year old female with medical and behavioral health needs including: Chronic pain, GERD, gastritis, hiatal hernia, PTSD, and Bipolar. Person was referred to ICM services following a medical hospitalization for GI bleed. Engagement- During telephonic assessment, ICM and Sierra identified acute suicidal intent requiring immediate intervention. A referral to the ED was made for additional assessment and disposition. Sierra agreed to an admission to the psychiatric unit. ICM coordinated with behavioral health and medical providers for discharge planning. Outcome- Sierra is responding well to behavioral health treatment and is seeing a PCP and GI specialist regularly. Her recovery from depression is supported in Outpatient therapy and she has not been readmitted for inpatient treatment. 45
EFFECTIVENESS AND OUTCOMES OF THE ICM PROGRAM 46
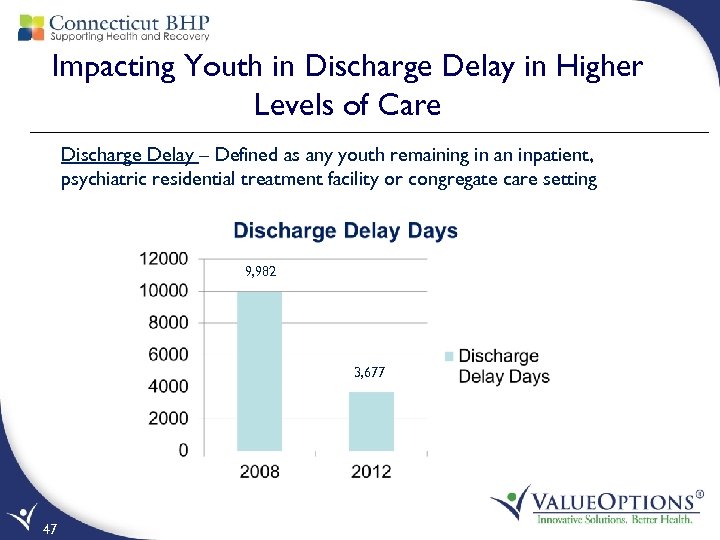
Impacting Youth in Discharge Delay in Higher Levels of Care Discharge Delay – Defined as any youth remaining in an inpatient, psychiatric residential treatment facility or congregate care setting 9, 982 3, 677 47
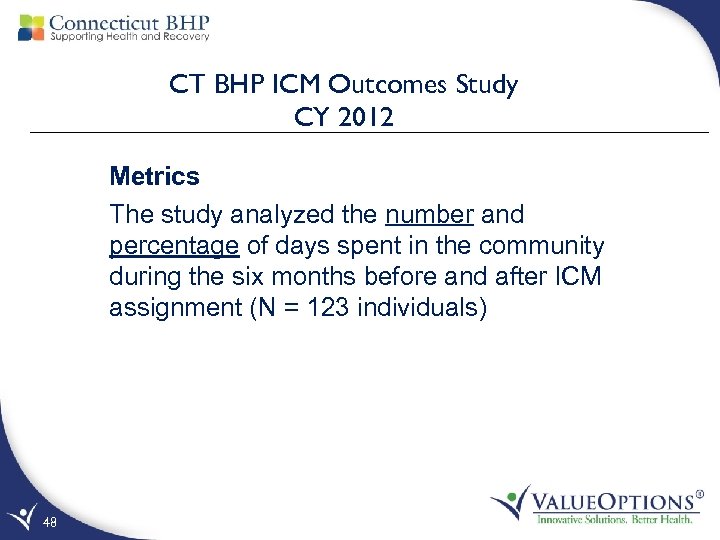
CT BHP ICM Outcomes Study CY 2012 Metrics The study analyzed the number and percentage of days spent in the community during the six months before and after ICM assignment (N = 123 individuals) 48
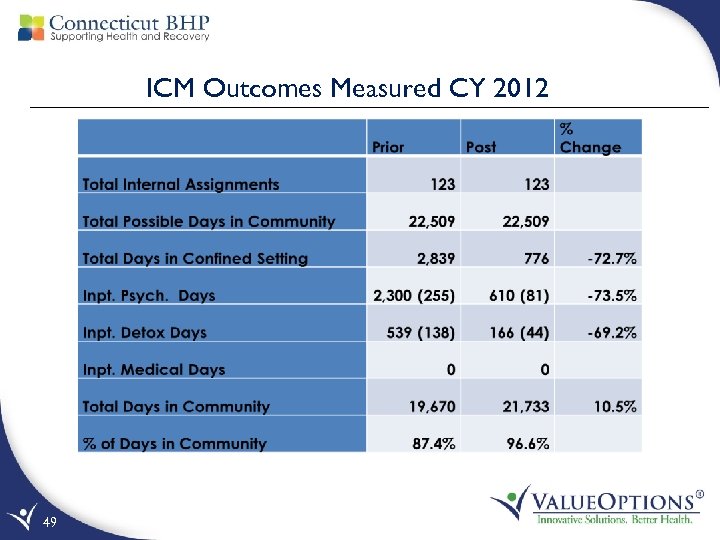
ICM Outcomes Measured CY 2012 49
Other ICM Models being Explored Deploying our staff to System “Hot Spots” to impact Individual Care Experience and Provider Practice 50
St. Francis Pilot- Initiated 1/1/2013 Eligible • Medicaid recipients receiving inpatient care at St. Francis who have BH, SA, and co-morbid medical needs Pilot Goals • To assess the impact of ICM involvement in the care of adults 30 and 60 days prior to, and post, ICM intervention • Increase time in the community • To pilot a face to face vs. brokering ICM model • Decrease re-admission rates for Inpatient level of care • Collect data regarding Peer involvement 51
St. Francis Pilot (Cont. ) • 52 participants as of 5/31/13 • 28 males / 24 females • Average age: 38 y/o • 44 participants – MH diagnosis • 8 participants – SA diagnosis • 88% participants - 3 previous I/P admissions 52
St. Francis Pilot (Cont. ) • The ICM/Peer team spent 20 hours per week on the following activities for each participant • Attending on-site rounds at St. Francis • Facilitating an educational group and/or activities that promote recovery • Providing face-to-face support connecting individuals with community supports to be utilized post discharge • Participating in Connect to Care mtgs. in the Community 53
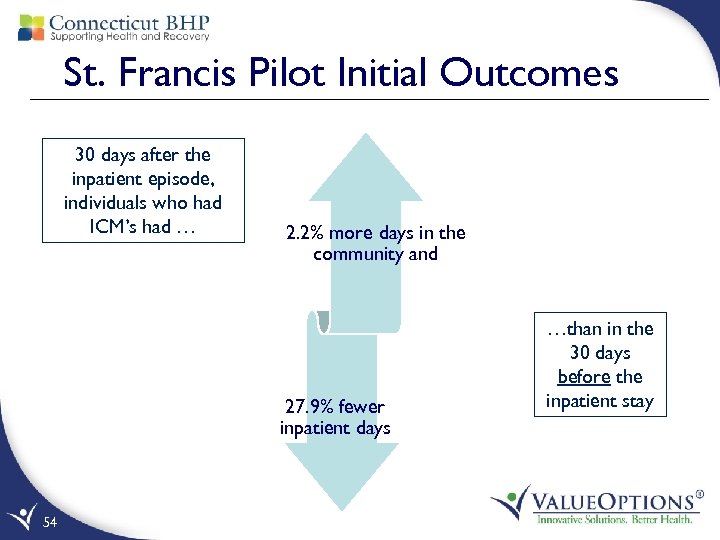
St. Francis Pilot Initial Outcomes 30 days after the inpatient episode, individuals who had ICM’s had … 2. 2% more days in the community and 27. 9% fewer inpatient days 54 …than in the 30 days before the inpatient stay
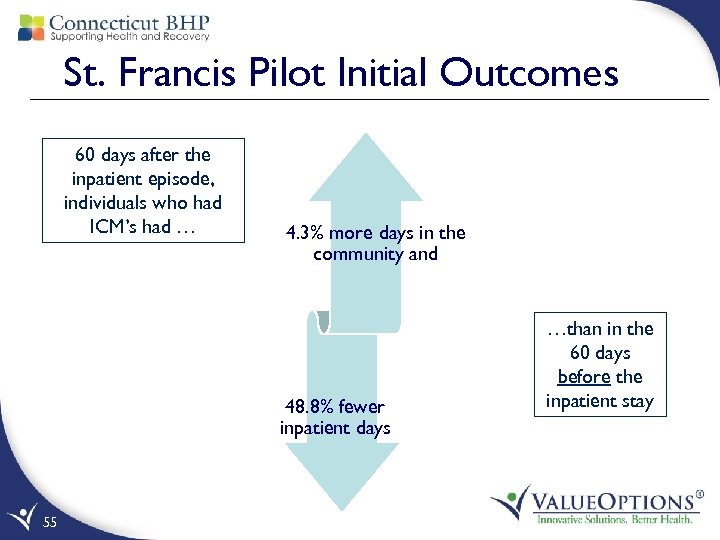
St. Francis Pilot Initial Outcomes 60 days after the inpatient episode, individuals who had ICM’s had … 4. 3% more days in the community and 48. 8% fewer inpatient days 55 …than in the 60 days before the inpatient stay
Home Health Pilot • Collaboration between New England Home Care and the CT BHP • Embedded Peer within a Home Health Team • Works with team to identify opportunities for skill transfer, improved community linkage/support and movement toward recovery • Initial Outcomes: TBD 56

The Future 57

What’s Next? Leveraging Technology • Data integration for non-Value. Options data system • Predictive modeling for high risk case identification • Care gap identification for care management • Care alerts – automated messaging to individuals and providers • Care plan linkage to assessment screens via system based logic • Provider decision support – online practice reports, Evidence Based Practice, registries 58 Exploring Models, assuring impact • Face to Face Models • Embedded ICM clinicians • Expanded role of Peers • Facility vs. Member level intervention • Increased medical integration within CT BHP • New Populations (DOC, CSSD, etc. ) Member centric care record accessible to care management staff (BH and Medical), provider, & individual with integrated care plan • Care utilization dashboard – person specific
Questions 59
a14d3d2663981fde724c340056a2c13d.ppt