0895a47a01757598f07f026d2f18f150.ppt
- Количество слайдов: 29
Medicaid Waiver: A Primer Presentation by Randy Laya, M. S. Federal Programs, Manager Regional Center of Orange County (RCOC) and Suzanne Butler RCOC Insurance and Benefits Specialist
What are Home and Community. Based Services (HCBS) Waivers? Medi-Cal waivers are programs under Medi-Cal that: n Provide additional services to specific groups of individuals, n Limit services to specific geographic areas of the state, and n Provide medical coverage to individuals who may not otherwise be eligible under Medicaid rules. n Currently there are ten Waiver programs in California.
A few of the HCBS Medi-Cal Waiver programs currently authorized in CA A. Home and Community Based Services Waiver for Individuals with Developmental Disabilities AKA the Medicaid Waiver or the DDS Waiver B. In-Home Operations: 1. Nursing Facility/Acute Hospital (NF/AH) Waiver 2. In-Home Operations Waiver C. Multipurpose Senior Service Program (MSSP) Waiver D. Acquired Immune Deficiency Syndrome (AIDS) Waiver
Role and Responsibilities of the Regional Centers The 21 regional centers are charged with the responsibility to coordinate, provide, arrange or purchase services and supports for persons with developmental disabilities in California. The regional centers were created under the Lanterman Act and receive their funding through contract with DDS has delegated responsibility to the regional centers for assuring that HCBS Waiver requirements are met.
The Medicaid Waiver (MW) n Allows California to claim Medi-Cal reimbursement for specific Regional Center services n Regional centers must meet consumer’s needs n The major purpose of the Medicaid Waiver program is to bring federal dollars into the state of CA
What are the Medicaid Waiver program requirements?
1. Meet the Lanterman Act definition of developmental disability A “developmental disability” means: q A disability which begins before age 18, q Is expected to continue indefinitely, q Presents a substantial disability for the individual, and q Is due to mental retardation, cerebral palsy, epilepsy, autism or a disabling condition closely related to mental retardation or requiring treatment similar to that required for individuals with mental retardation. The definition expressly excludes other handicapping conditions that are solely learning disabilities, psychiatric disorders or physical in nature.
2. Be an active regional center consumer q. Regional Centers administer three programs: Prevention, Early Intervention, and On-Going (Active) each with their own eligibility criteria q To be active, the individual must have a developmental disability and have an open case with regional center

3. Have full-scope Medi-Cal benefits, q. Be eligible to access all services available through Medi-Cal, or q. Meet the requirements for institutional deeming (we’ll discuss this later)
4. Have substantial limitations in adaptive functioning which qualifies the consumer for the level of care provided in an ICFDD, intermediate care facility for the developmentally disabled. Habilitation (ICF/DD-H), or intermediate care facility for the developmentally disabled-Nursing (ICF/DD-N). q. Evaluation of each consumer’s level of care needs is based on his/her ability to perform activities of daily living and community participation. q. Provides funding for services only to individuals who, but for the provision of these services, would require the level of care provided in an ICF-DD; q. This determination is typically made through two CDER (Client Development and Evaluation Report) deficits or two medical deficits or one of each
5. Not be concurrently enrolled in another HCBS Waiver q Individuals may occasionally qualify for two or more Waiver programs, such as NF/AH Waiver (for medical technology dependency) and the Medicaid Waiver q. Can only be enrolled in one Waiver program at a time
6. Choose to participate and receive services through the HCBS Waiver and to reside in a community setting. q Consumer needs to have a MW qualifying service in place that directly addresses one of the CDER deficits q Must use a MW qualifying service at least once every twelve month q $1000 per month
Services that qualify for the DDS Waiver program: q n n n n Homemaker Home Health Aide Services Respite Care Habilitation: – Residential habilitation for children services – Day habilitation – Prevocational services – Supported employment services Environmental Accessibility Adaptations Skilled Nursing Transportation Specialized Medical Equipment / Supplies Chore Services
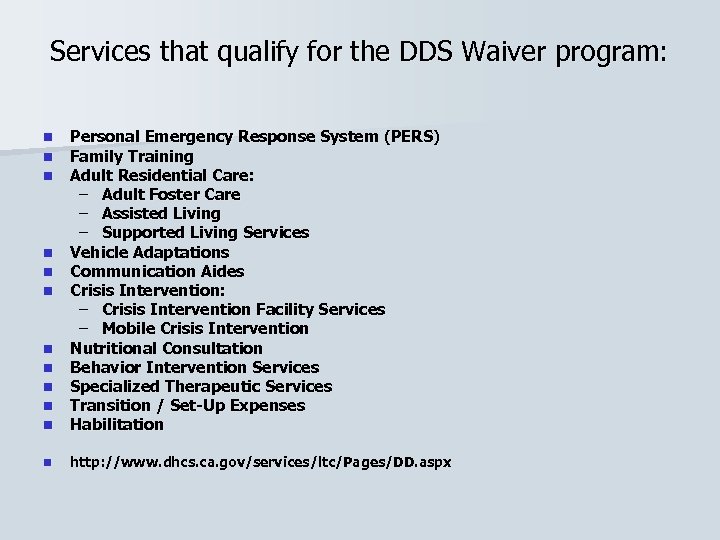
Services that qualify for the DDS Waiver program: n n n Personal Emergency Response System (PERS) Family Training Adult Residential Care: – Adult Foster Care – Assisted Living – Supported Living Services Vehicle Adaptations Communication Aides Crisis Intervention: – Crisis Intervention Facility Services – Mobile Crisis Intervention Nutritional Consultation Behavior Intervention Services Specialized Therapeutic Services Transition / Set-Up Expenses Habilitation n http: //www. dhcs. ca. gov/services/ltc/Pages/DD. aspx n n n
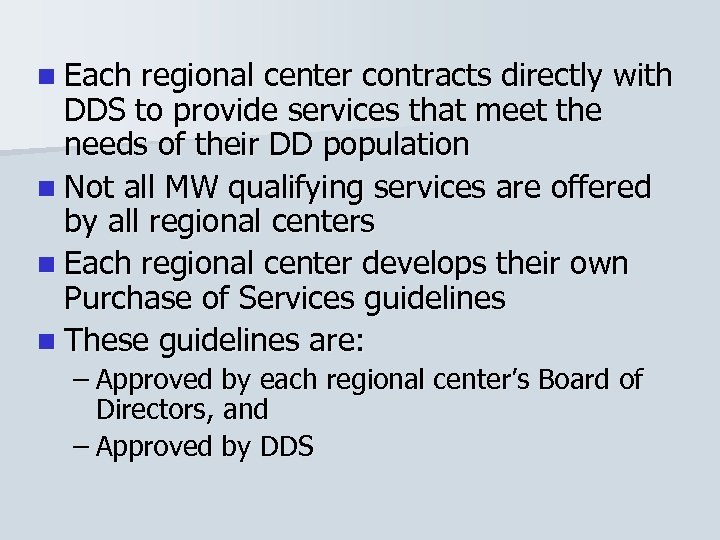
n Each regional center contracts directly with DDS to provide services that meet the needs of their DD population n Not all MW qualifying services are offered by all regional centers n Each regional center develops their own Purchase of Services guidelines n These guidelines are: – Approved by each regional center’s Board of Directors, and – Approved by DDS
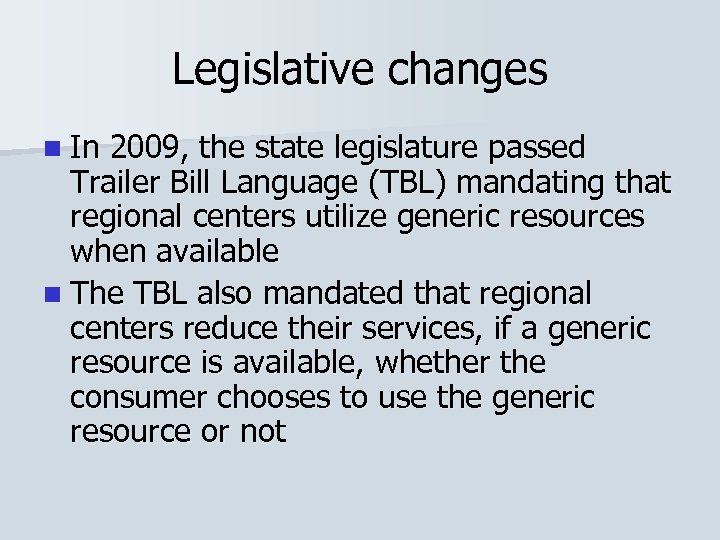
Legislative changes n In 2009, the state legislature passed Trailer Bill Language (TBL) mandating that regional centers utilize generic resources when available n The TBL also mandated that regional centers reduce their services, if a generic resource is available, whether the consumer chooses to use the generic resource or not
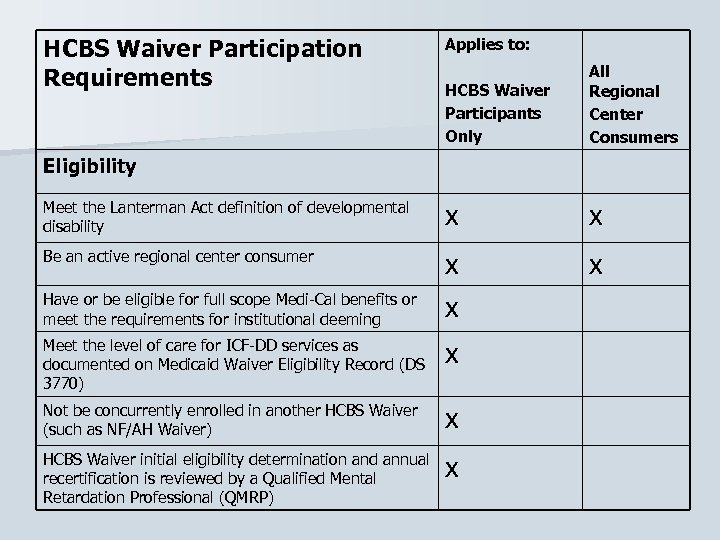
HCBS Waiver Participation Requirements Applies to: HCBS Waiver Participants Only All Regional Center Consumers Meet the Lanterman Act definition of developmental disability x x Be an active regional center consumer x x Have or be eligible for full scope Medi-Cal benefits or meet the requirements for institutional deeming x Meet the level of care for ICF-DD services as documented on Medicaid Waiver Eligibility Record (DS 3770) x Not be concurrently enrolled in another HCBS Waiver (such as NF/AH Waiver) x HCBS Waiver initial eligibility determination and annual recertification is reviewed by a Qualified Mental Retardation Professional (QMRP) x Eligibility
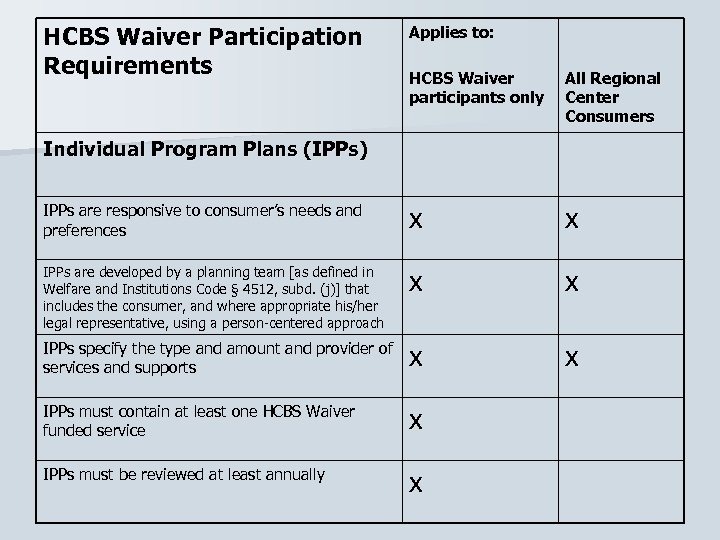
HCBS Waiver Participation Requirements Applies to: HCBS Waiver participants only All Regional Center Consumers IPPs are responsive to consumer’s needs and preferences x x IPPs are developed by a planning team [as defined in Welfare and Institutions Code § 4512, subd. (j)] that includes the consumer, and where appropriate his/her legal representative, using a person-centered approach x x IPPs specify the type and amount and provider of services and supports x x IPPs must contain at least one HCBS Waiver funded service x IPPs must be reviewed at least annually x Individual Program Plans (IPPs)
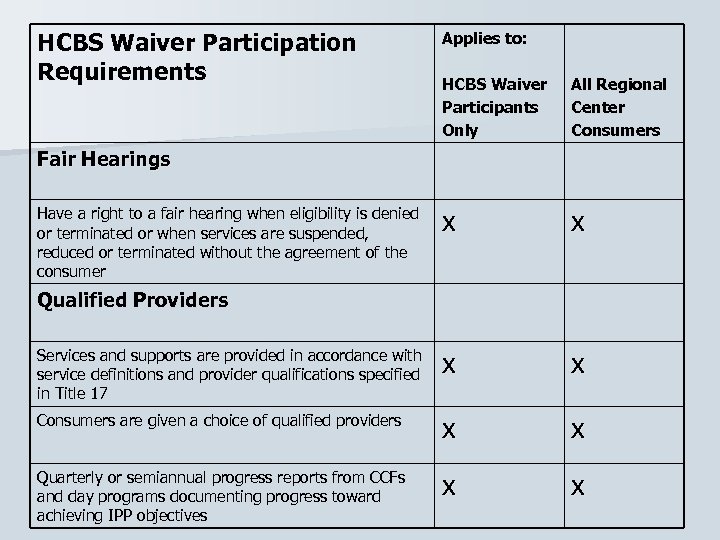
HCBS Waiver Participation Requirements Applies to: HCBS Waiver Participants Only All Regional Center Consumers x x Services and supports are provided in accordance with service definitions and provider qualifications specified in Title 17 x x Consumers are given a choice of qualified providers x x Quarterly or semiannual progress reports from CCFs and day programs documenting progress toward achieving IPP objectives x x Fair Hearings Have a right to a fair hearing when eligibility is denied or terminated or when services are suspended, reduced or terminated without the agreement of the consumer Qualified Providers
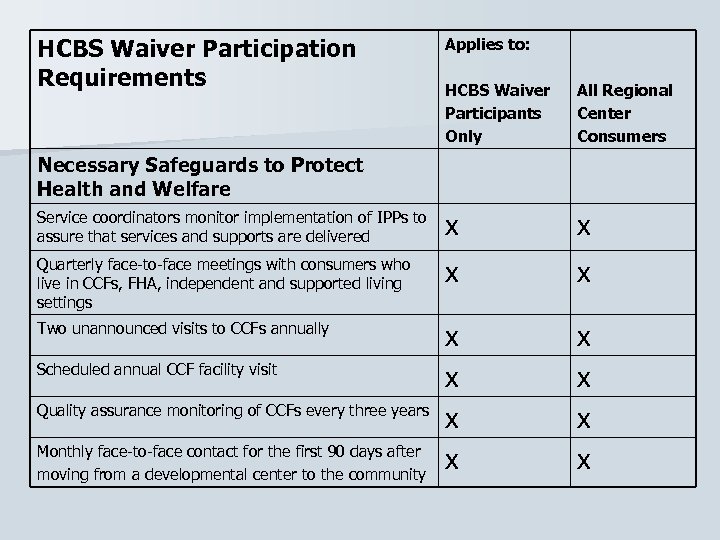
HCBS Waiver Participation Requirements Applies to: HCBS Waiver Participants Only All Regional Center Consumers Service coordinators monitor implementation of IPPs to assure that services and supports are delivered x x Quarterly face-to-face meetings with consumers who live in CCFs, FHA, independent and supported living settings x x Two unannounced visits to CCFs annually x x x x Necessary Safeguards to Protect Health and Welfare Scheduled annual CCF facility visit Quality assurance monitoring of CCFs every three years Monthly face-to-face contact for the first 90 days after moving from a developmental center to the community
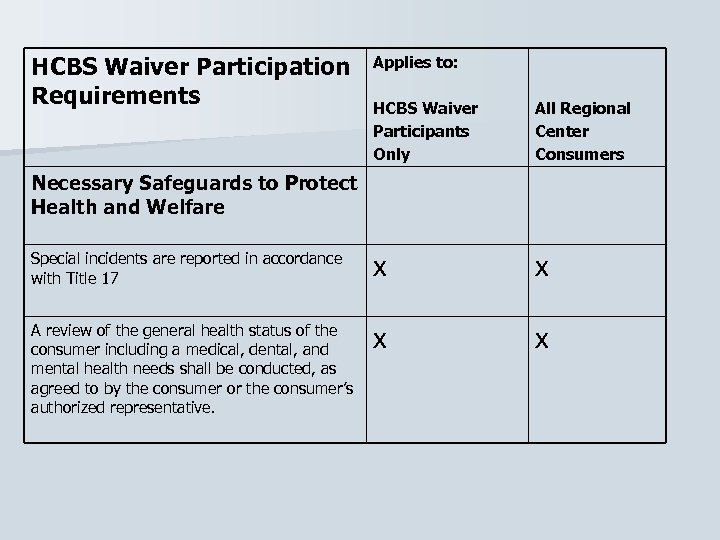
HCBS Waiver Participation Requirements Applies to: HCBS Waiver Participants Only All Regional Center Consumers Special incidents are reported in accordance with Title 17 x x A review of the general health status of the consumer including a medical, dental, and mental health needs shall be conducted, as agreed to by the consumer or the consumer’s authorized representative. x x Necessary Safeguards to Protect Health and Welfare
Any questions about the MW program?
Institutional Deeming Medi-Cal
What is Institutional Deeming? n Institutional deeming means that "the individual is assessed to be Medi-Cal eligible “as if” he/she were in a long-term care facility". n If the family’s income/property/assets exceeds regular Medi-Cal limits, then only the income/property/assets of the child or the disabled adult spouse is considered under institutional deeming.
Who is eligible for ID Medi-Cal? Consumers who meet the criteria of the HCBS Waiver program n Consumers who are citizens or in the US with satisfactory immigration status n Typically a consumer with an income of less than $620/mo and with assets that total less than $2000. n Consumer in the family home up to the age of 21 y. o. who does not otherwise qualify for regular Medi-Cal; child’s income is the only income counted n n However, if the consumer has income and resources of his/her own such as a trust fund or court-appointed child support, the consumer may be assessed with a share of cost or may be denied eligibility
How does a consumer obtain ID Medi-Cal? n. Service Coordinator starts the process by confirming that the consumer meets the eligibility criteria to be added to the MW program. n. The Regional Center sends the DDS Waiver Referral form to the Medi-Cal office. n. The Medi-Cal office assigns a Medi-Cal worker to the child’s case. n. The family is sent a Medi-Cal application to complete. n. The family’s income/assets/property is disregarded in the eligibility determination for the child if it exceeds Medi-Cal’s limits; BUT n. The family must complete the Medi-Cal application and submit their financial, property, and citizenship information or the child’s application will be denied. n. Once the application is completed an eligibility determination is made by the Medi-Cal worker. If the family is eligible for regular Medi-Cal, the child will be added to that program and not the ID Medi-Cal program.
What are the advantages of having ID Medi-Cal? n FCPP (Family Cost Participation Program) assessed for regional center services is waived with Full Scope Medi-Cal n Medi-Cal offers services/supports that may not be covered by private insurance: § Diapers § Dental n Shift nursing through EPSDT Durable Medical Equipment Vision IHSS Mental Health Medi-Cal serves as a secondary insurance for the consumer that has private insurance. – Medi-Cal will cover certain co-pays that are the family’s responsibility once the private insurance has paid their portion § Medications Hospitals DME
What causes the ID Medi-Cal case to be denied or to close? n n n n The Medi-Cal application with the required documentation was not submitted to the Medi-Cal office in a timely manner The consumer has unsatisfactory immigration status Excess income/assets/property The annual redetermination paperwork was not received by the Medi-Cal office – Family moved and didn’t leave forwarding address – Family didn’t realize that paperwork needed to be resubmitted each year The consumer is no longer residing in CA The consumer becomes eligible for regular Medi-Cal The consumer is no longer eligible for the MW program
Questions?
0895a47a01757598f07f026d2f18f150.ppt