d368cb65d588b6eecc7d9b1a6c8643a4.ppt
- Количество слайдов: 95
Medicaid Substance Use Disorder (SUD) Treatment Service Benefits June 17, 2011 1
Training Objectives Participants will learn: • Overview of Legislative History • Overview of Benefits • Overview of Wrap-Around Coverage for Women and Children Residential Services • Special Considerations Related to Adolescents • Billing Information • Overview: TMHP Web Portal for Claims and Prior Authorization • Eligibility Verification (including new Your Texas Benefits Card) • How a Client Can Access SUD benefits • Resources 2
Legislative History 3
Legislative Direction The 2010 -11 General Appropriations Act (Article IX, Section 17. 15 of S. B. 1) directs HHSC to: • provide Comprehensive Substance Abuse Services in Medicaid to adults with substance abuse disorders; and • analyze and provide data to the Legislative Budget Board (LBB) on the provisions of substance abuse services and discontinue the benefit if services increase overall Medicaid expenditures. 4
Benefits 5
Benefits The benefits include: • Assessment • Ambulatory (outpatient) treatment services • Medication assisted therapy (MAT) • Detoxification (ambulatory and residential) • Residential treatment 6
Phase I Benefits: Outpatient The benefits were implemented in two phases. • Phase I Benefits became effective on September 1, 2010, and include: • • Assessment Ambulatory (outpatient) treatment services Medication assisted therapy (MAT) Ambulatory Detoxification (in STAR and STAR+PLUS managed care only) 7
Assessment: • Reimbursed once per episode of care upon admission to a treatment program. • Conducted on individuals requiring an evaluation to determine if a substance use disorder is present and what level of treatment is needed. • Must be performed by a licensed Qualified Credentialed Counselor and billed by a Licensed Chemical Dependency Treatment Facility. • Must be performed using a comprehensive assessment tool that includes, but is not limited to: an evaluation of substance use and disorder, past history, social history, health and psychological evaluation, readiness assessment etc. (e. g. , CHMBS) • Should not require prior authorization or referral for any client, including STAR and STAR+PLUS. 8
Outpatient Treatment • Outpatient treatment services are a benefit for individuals with a substance use disorder who meet the DSM IV-TR criteria for treatment and can be safely treated in outpatient setting. 9
Outpatient treatment • Limited to combined total of 135 hours of group counseling and 26 hours of individual counseling per client per calendar year. • Limited to certain diagnoses • Additional counseling may be considered with prior authorization for individuals ages 20 and under with physician documentation of medical need for continued treatment. • Must meet DSM IV-TR criteria for substance abuse or dependence. 10
Outpatient Treatment: Exclusions • Client fails to meet eligibility criteria • Diagnostic evaluation shows that the client is experiencing acute withdrawal requiring detoxification services in an inpatient setting. 11
Medication Assisted Therapy • Medication assisted therapy (MAT) is a benefit for clients meeting the DSM IV-TR criteria for substance abuse or dependence for persons addicted to drugs and alcohol. • Effective February 1, 2011, MAT can be billed by both a physician under a physician provider identification number, as well as CDTF, under a CDTF facility provider identification number. Previously, MAT billing was limited to physician provider types. 12
Medication Assisted Therapy MAT includes: • Administration of medication. • Direct observation therapy. • Methadone and non-methadone, for example, buprenorphine. Limitations: • Opioid treatment programs must comply with the requirements in federal regulation 42 CFR part 8. • Services must be provided as a part of a comprehensive treatment program. When needed, maintenance therapy can be provided as a component of relapse prevention 13 for people who have undergone treatment.
Medication Assisted Therapy Exclusions Not a benefit when: • Provided for tobacco, caffeine, hashish, or marijuana addiction. • Client fails to meet treatment criteria. • Therapy is contraindicated. 14
Medication Assisted Therapy: Methadone Take Home Doses in FFS and PCCM After February 1, 2011 • Effective February 1, 2011, providers can bill procedure code H 0020 with modifier U 1 for takehome doses of methadone. • Take home doses must be billed on the same day with the same date of service as a supervised administration claim. • Also effective February 1, 2011, code H 0020 with modifier U 1 is billable one time per day. Previously, providers were allowed to bill H 0020 up to 4 times a day. • The new take home rate for methadone (H 002015 U 1), effective March 1, 2011, is $2/day.
Medication Assisted Therapy: Methadone Treatment in FFS and PCCM starting March 1, 2011 • • For service dates on or after March 1, 2011, use code H 0020 with modifier UA for methadone given in person. Use code H 0020 with modifier U 1 for take home methadone doses. Effective March 1, 2011, providers no longer must bill daily for each take home dose. Rather, the provider can bill for up to a 30 day supply in one billing. Claims for H 0020 with dates of service on or after March 1, 2011 will deny without the appropriate modifiers (UA or U 1). When medically appropriate, methadone providers can also bill separately using their facility TPI number for counseling codes H 0004 and H 0005. These codes apply to individual, group, and family counseling, psychoeducation, and relapse prevention education. Must be provided by a qualified credentialed counselor, graduate or intern. In addition, physicians can bill appropriate Evaluation and Management (E&M) codes under their physician Medicaid provider number. Laboratory services should be billed separately by the lab. 16
Medication Assisted Therapy and Managed Care • HHSC has directed the health plans to: • Allow for both CDTFs and physician provider types to bill for MAT services. • Allow in-person methadone treatment to be billed only once per day (i. e. H 0020 or similar code). • Develop a mechanism to reimburse for take-home doses of methadone, and establish a mechanism to distinguish in their billing the difference between a methadone dose given in person versus a take-home. • Develop a similar mechanism to reimburse for both in-person and take homes of non-methadone treatment doses (e. g. , buprenorphine) • There may be differences in how the services are billed (e. g. , different billing codes); plans may also have differences in prior authorization requirements. • Contact the client’s health plan for more information about billing for medication assisted therapy services, including for clients with takehome privileges. 17
Medication Assisted Therapy in Combination with other services • Prior to June 1, 2011, MAT services (1 -H 0020 and 1 -H 2010) were denied when billed for the same date of service as ambulatory or residential detox, or residential treatment. • Effective June 1, 2011, MAT services can be billed on the same day as residential detoxification, ambulatory detoxification, or residential treatment only when supporting documentation indicates one of the following: – The client is pregnant with an opioid addiction – The client is current in MAT treatment for an opioid addiction and is also receiving residential services for a substance other than opioids. 18
Medication Assisted Therapy: Non-Methadone • Effective June 1, 2011, clarifications have been made related to nonmethadone MAT services. (e. g. , buprenorphine) • When administered in person, providers should use code H 2010, along with HG and UA for an opioid non-methadone treatment administered with supervision in a CDTF. Limit: Once per day, same procedure, any provider. • For non-methadone opioid take home doses, use H 2010, with modifiers HG and U 1. Limit: 30 doses per 30 rolling days. • For non-methadone (non-opioid) in-person administration with supervision, use H 2010, with modifier HF. Limit: Once per day, same procedure, any provider. • Claims for non-methadone administration will deny without all appropriate modifiers. • Take home doses must be billed on the same day with the same date of service as a supervised administration claim. 19
Start Date Phase II Benefits became effective on January 1, 2011, and include: • Residential detoxification • Residential treatment services • Ambulatory detoxification (Fee-for-service Medicaid and Primary Care Case Management) 20
Detoxification • To receive detoxification services, individuals must meet the DSM IV-TR criteria for physiological substance dependence and must meet the admission requirements based on a nationally recognized standard. • Can be provided in a general acute care hospital or residential or ambulatory chemical dependency treatment facility setting. • The CDTF must be licensed by the Department of State Health Services. 21
Detoxification • • Both ambulatory and residential detoxification require prior authorization. Ambulatory detoxification is appropriate for clients who do not require close monitoring. Residential detoxification is appropriate when a client’s medical needs do not warrant inpatient hospital admission, but the client requires close monitoring during withdrawal. May be covered for a medically appropriate duration of care based on treatment need for up to 21 days. Clients ages 20 and under may receive additional days of treatment with prior authorization. Includes: evaluation, monitoring, medication, and daily interaction. Ambulatory detoxification must be provided in coordination with an outpatient treatment program. Exclusions: • Not a benefit for tobacco, caffeine, hashish or marijuana addiction. • Not a benefit when a person does not meet the clinical criteria for coverage. • Crisis stabilization is not a component of detoxification. However, crisis stabilization for a mental health condition can be provided under a client’s 22 mental health benefits if medically necessary and the clinical criteria for psychiatric care met.
Residential Treatment • To receive residential treatment services, individuals must meet the DSM IV-TR criteria for residential treatment and admission standards outlined in the Texas Administrative Code (TAC 28, part 1, Chapter 3, Subchapter HH TAC § 3. 8011. ) • Residential treatment must be rendered by a Medicaid-enrolled CDTF licensed by the Department of State Health Services. 23
Residential Treatment: • Requires prior authorization. • May be covered for a medically appropriate duration of care, with a maximum of 35 days per episode of care. Clients ages 20 and under may receive additional days of treatment with prior authorization. • Limited to 2 episodes of care in 6 month period, with evidence of medical need. • Includes, but is not limited to: physical and clinical evaluation; development of goal-oriented, individualized treatment plan; intensive individual, group, and family counseling; management of medications; and psycho-education. EXCLUSIONS: • Client fails to meet treatment eligibility or criteria. • Services can be effectively managed through an outpatient program. • Diagnostic evaluation shows client has acute withdrawal that requires detoxification services. 24
Wrap-Around Coverage: Women and Children Residential Services Specialized female pregnant women and women with children services may be available as a “wrap-around” service to pregnant women in their third trimester and women who need to bring their children with them to residential treatment. 25
Wrap-Around Coverage: Women and Children Residential Services Wrap-around services: • Must be provided by a DSHS Substance Abuse Treatment and Prevention Block grant provider of women and children residential services; • Are subject to availability; • Include services that are not a benefit of the Medicaid program (e. g. , co-housing of children, parenting and budgeting classes, etc. ) Note: Medicaid will continue to reimburse residential treatment up to the maximum days allowed under the benefit (35 days). 26
Wrap-Around Coverage: Women and Children Residential Services • • • By contract, STAR and STAR+PLUS HMOs must work with DSHS providers to ensure payment for covered services is available to out-of-network providers who also provide related (non-capitated) services (e. g. , wrap around coverage for women and children residential) when the covered services are not available through network providers. Women in a managed care area needing wrap around coverage should contact their health plan first. Providers may also refer clients to an Outreach, Screening, Assessment and Referral (OSAR) organization to locate a provider. http: //www. tcada. state. tx. us/gettinghelp/index. shtml Note that only a limited number of Substance Abuse Treatment and Prevention block grant providers contracted with DSHS currently provide women and children residential services, and each provider has limitations on their capacity. Access is not guaranteed. 27
Non-Covered Services • Aftercare. • Services for which client fails to meet the eligibility or authorization requirements. • Services for tobacco and caffeine addiction. • Services provided by a CDTF that is not licensed by DSHS and enrolled as a Medicaid provider. • Services provided electronically, such as by telemedicine, email, or phone. • Targeted case management. 28
Benefits for Adolescents • Children ages 20 and under continue to have access to substance abuse treatment. • Medicaid requires that children be provided these services as medically necessary. • Benefits mirror new adult benefits, except minors may exceed benefit limitations based on medical necessity. (e. g. , residential treatment limit, outpatient counseling limits, etc. ) • Medicaid considers adolescents as ranging up to age 20. From a regulatory standpoint, adolescent residential treatment is targeted to ages 13 -17. Clients who are ages 18, 19 and 20 receive adult treatment services, but are considered by Medicaid to be adolescents and are 29 paid at the adolescent (children) rate.
Benefits for Adolescents: Special Considerations Residential treatment for adolescents • Adolescents (ages 13 through 17) in traditional Medicaid or PCCM must meet the following additional criteria for treatment in an adolescent CDTF residential treatment program: • Manifesting physical maturation at least in mid-adolescent range (i. e. , post pubescent) • Cognitive development of at least 11 years of age. Regarding developmental status, the client must display: • Documented inability to function in expected age norms, despite normal cognitive and physical maturation; and/or • History of moderate to severe conduct disorder; and/or • Documented difficulty in meeting developmental expectations in a major area of functioning to the extent it interferes with the capacity to remain stable behaviorally. 30
Benefits for Adolescents: Special Considerations Medication Assisted Therapy and Adolescents • No client under 18 can be admitted to narcotic maintenance without written consent from parent, legal guardian, or responsible adult designated by relevant State authority. • To be eligible for narcotic maintenance treatment, clients 18 and under must have had 2 documented attempts at short-term detox or drug-free treatment and must wait at least 7 days between the first and second short-term detox treatment. • Must follow all state and federal regulations, as well as licensure rules. 31
Basic Billing Information: FFS and PCCM 32
Phase I benefits (Assessment, Counseling, Medication Assisted Therapy) 33
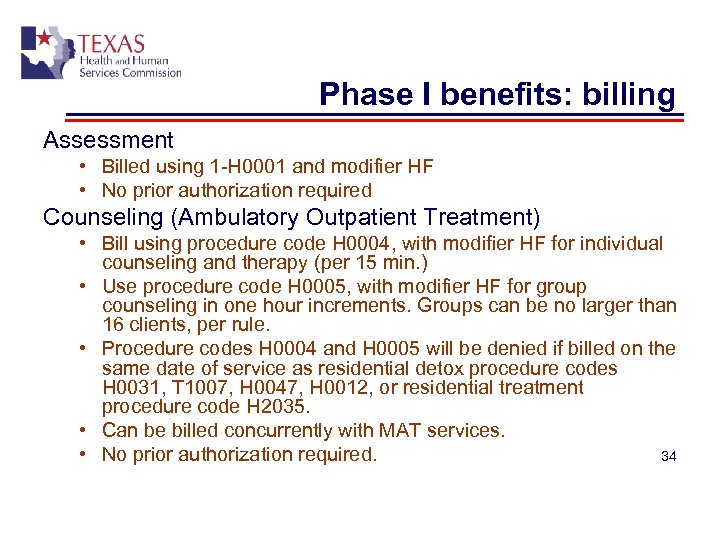
Phase I benefits: billing Assessment • Billed using 1 -H 0001 and modifier HF • No prior authorization required Counseling (Ambulatory Outpatient Treatment) • Bill using procedure code H 0004, with modifier HF for individual counseling and therapy (per 15 min. ) • Use procedure code H 0005, with modifier HF for group counseling in one hour increments. Groups can be no larger than 16 clients, per rule. • Procedure codes H 0004 and H 0005 will be denied if billed on the same date of service as residential detox procedure codes H 0031, T 1007, H 0047, H 0012, or residential treatment procedure code H 2035. • Can be billed concurrently with MAT services. • No prior authorization required. 34
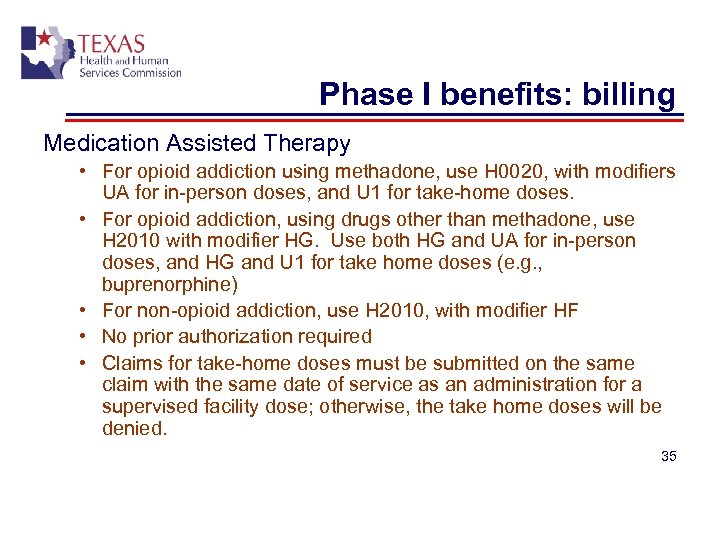
Phase I benefits: billing Medication Assisted Therapy • For opioid addiction using methadone, use H 0020, with modifiers UA for in-person doses, and U 1 for take-home doses. • For opioid addiction, using drugs other than methadone, use H 2010 with modifier HG. Use both HG and UA for in-person doses, and HG and U 1 for take home doses (e. g. , buprenorphine) • For non-opioid addiction, use H 2010, with modifier HF • No prior authorization required • Claims for take-home doses must be submitted on the same claim with the same date of service as an administration for a supervised facility dose; otherwise, the take home doses will be denied. 35
Phase II Benefits Detoxification and Residential Treatment 36
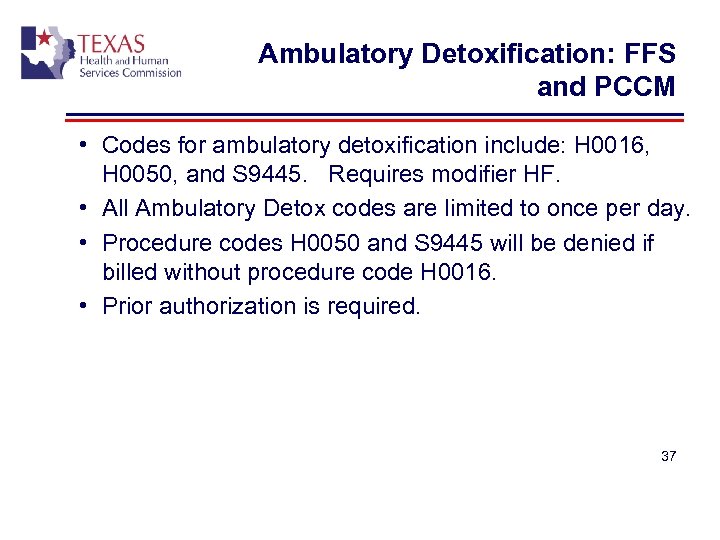
Ambulatory Detoxification: FFS and PCCM • Codes for ambulatory detoxification include: H 0016, H 0050, and S 9445. Requires modifier HF. • All Ambulatory Detox codes are limited to once per day. • Procedure codes H 0050 and S 9445 will be denied if billed without procedure code H 0016. • Prior authorization is required. 37
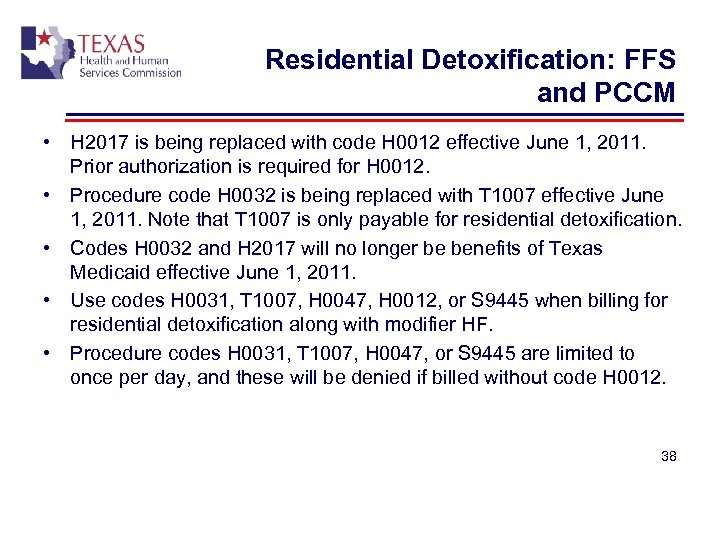
Residential Detoxification: FFS and PCCM • H 2017 is being replaced with code H 0012 effective June 1, 2011. Prior authorization is required for H 0012. • Procedure code H 0032 is being replaced with T 1007 effective June 1, 2011. Note that T 1007 is only payable for residential detoxification. • Codes H 0032 and H 2017 will no longer be benefits of Texas Medicaid effective June 1, 2011. • Use codes H 0031, T 1007, H 0047, H 0012, or S 9445 when billing for residential detoxification along with modifier HF. • Procedure codes H 0031, T 1007, H 0047, or S 9445 are limited to once per day, and these will be denied if billed without code H 0012. 38
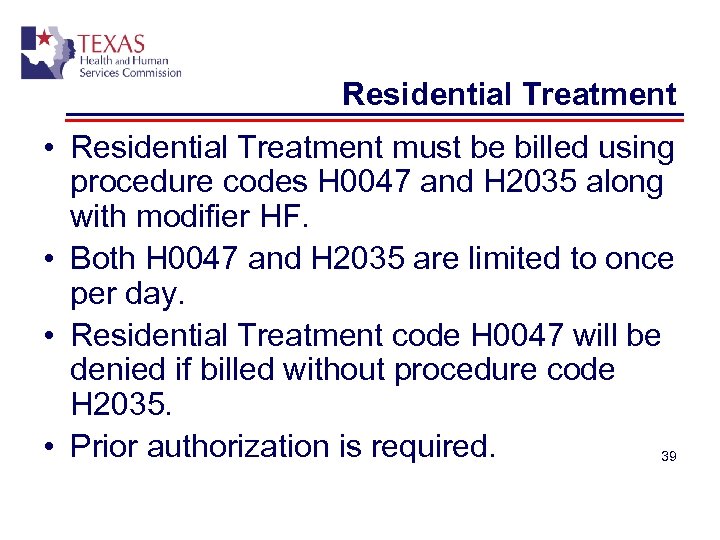
Residential Treatment • Residential Treatment must be billed using procedure codes H 0047 and H 2035 along with modifier HF. • Both H 0047 and H 2035 are limited to once per day. • Residential Treatment code H 0047 will be denied if billed without procedure code H 2035. • Prior authorization is required. 39
Reimbursement 40
Reimbursement Generally, works as follows: • STAR, STAR+PLUS: reimbursement through the Medicaid managed care health plans. Note that the rates paid and billing codes may or may not match FFS or PCCM. • PCCM and FFS: through TMHP. • North. STAR: through the BHO, Value Options. 41
Reimbursement Exceptions: • Aged, blind and disabled STAR clients receiving SSI: claims sent to TMHP. • STAR+PLUS clients who are dually eligible for Medicaid and Medicare, and qualify for “full Medicaid” benefits (also known as MQMBs): paid through TMHP. 42
Fraud and Abuse • • Substance use disorder treatment claims are subject to retrospective review. Federal and state regulations and statutes require Texas Medicaid, through the Office of Inspector General, to have the ability to identify, investigate, sanction and refer cases of suspected fraud and abuse to prosecutors or licensure and certification boards/agencies. HHSC/OIG may impose one or any combination of administration actions or sanctions on providers when fraud, waste or abuse is determined. Administrative actions include but are not limited to: attendance at provider education sessions, prepayment review, post payment review, attendance in a corrective action meeting and more. Administrative sanctions include exclusion from participation in the Medicaid program, withholding of payment, recoupment of overpayments and more. Examples of fraud and abuse include but are not limited to: billing for services that are not medically necessary, submitting false statement or information to meet prior authorization requirements, billing for services not provided to a recipient, and submitting false statements that have the potential of increasing a provider payment rate or fee. Providers can also report suspected fraud and abuse (client and provider) online at: https: //oig. hhsc. state. tx. us/Fraud_Report_Home. aspx 43
Claim Filing to TMHP Fee-for-Service and PCCM 44
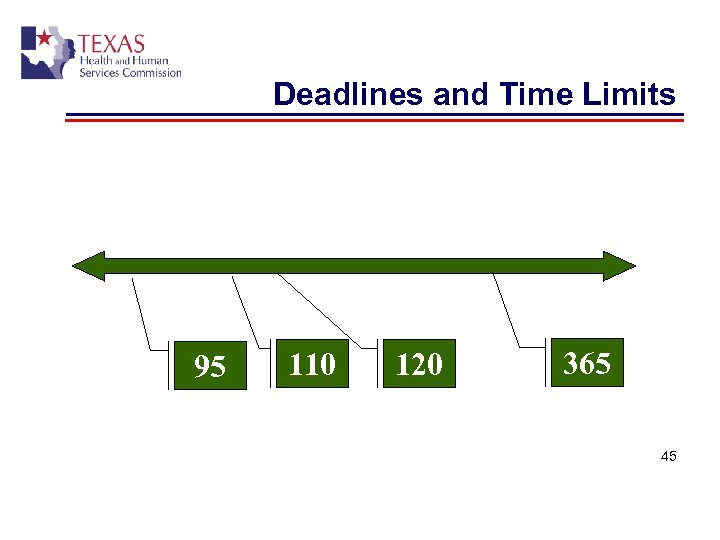
Deadlines and Time Limits 95 110 120 365 45
How to file Paper Claims • Address for paper claims: Texas Medicaid and Healthcare Partnership Claims PO Box 200555 Austin, TX 78720 -0555 • Address for appeals/adjustments of claims: Texas Medicaid and Healthcare Partnership Appeals/Adjustments PO Box 200645 Austin, TX 78720 -0645 Electronic Filing through Tex. Med. Connect: Setting up your Account • Electronic filing is recommended generally because it can be processed more efficiently. • Access at http: //www. tmhp. com • In upper right hand corner, click “Log into my Account” • If you don’t have an account set up, click “cancel” when the system asks you for your user name and Password. The system will redirect you to another page. Then click on “I Want to Activate my Account” and follow the steps. • NOTE: Providers can also file claims through EDI using vendor software and third party billing agents. Claim Forms • Use CMS 1500 for all SUD services, including residential. 46
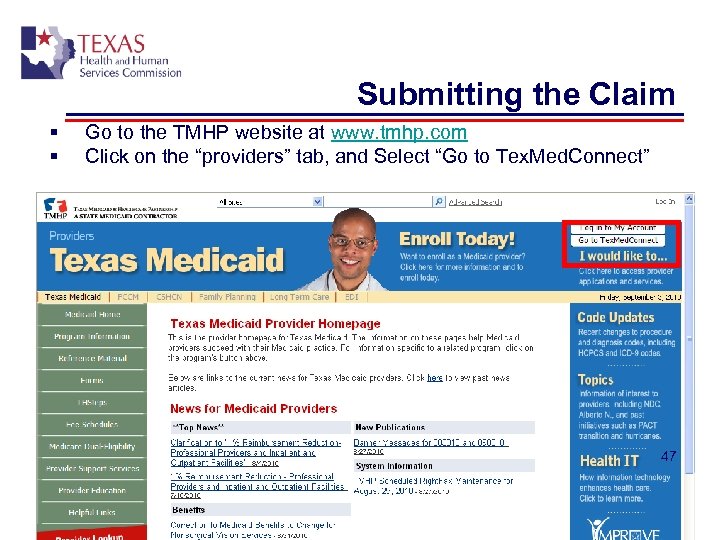
Submitting the Claim § § Go to the TMHP website at www. tmhp. com Click on the “providers” tab, and Select “Go to Tex. Med. Connect” 47
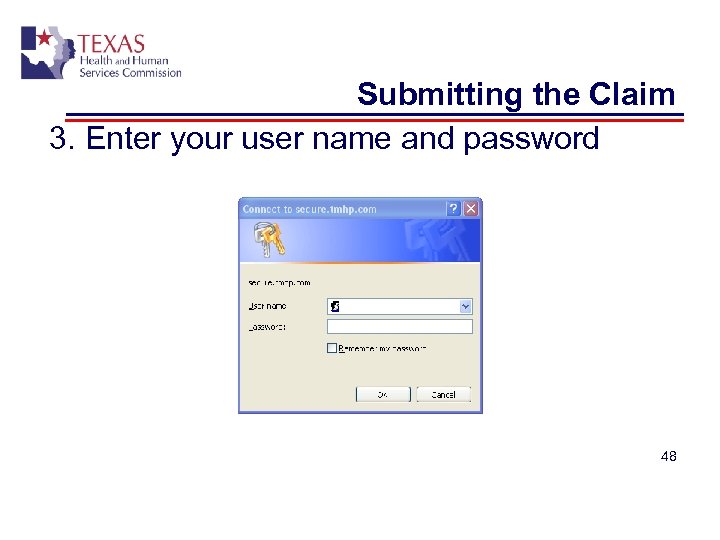
Submitting the Claim 3. Enter your user name and password 48
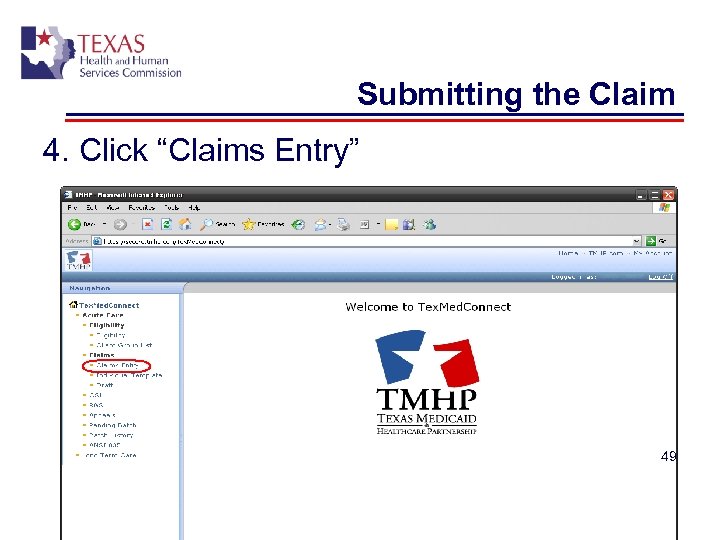
Submitting the Claim 4. Click “Claims Entry” 49
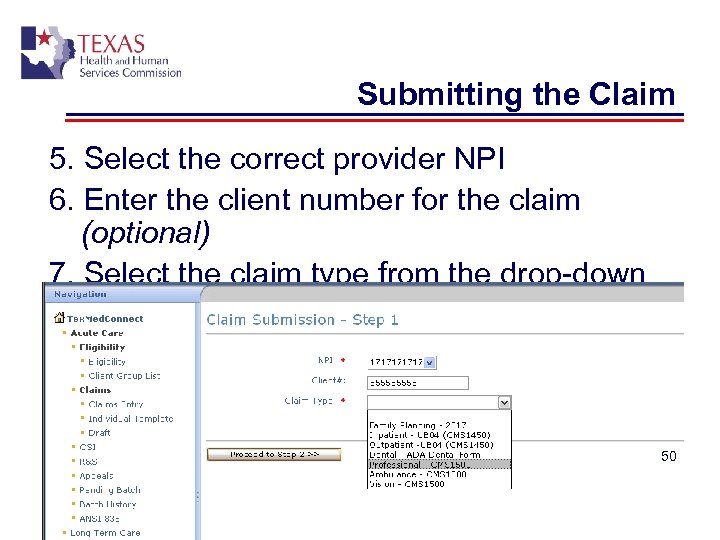
Submitting the Claim 5. Select the correct provider NPI 6. Enter the client number for the claim (optional) 7. Select the claim type from the drop-down menu 8. Click “Proceed to Step 2” 50
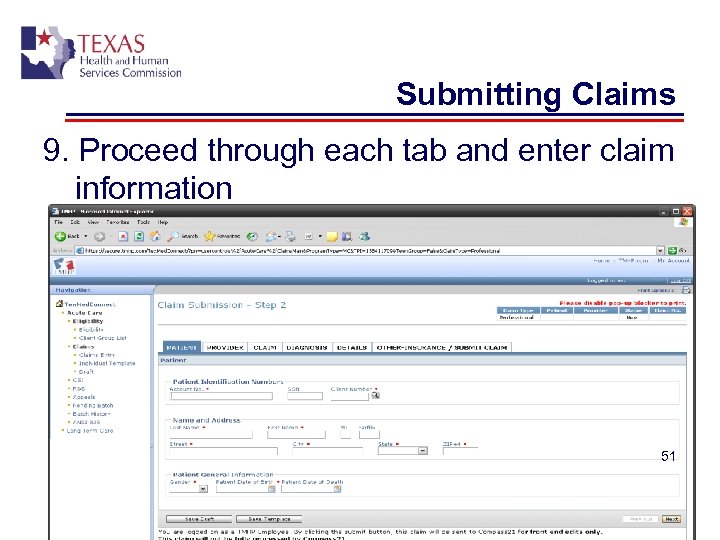
Submitting Claims 9. Proceed through each tab and enter claim information 51
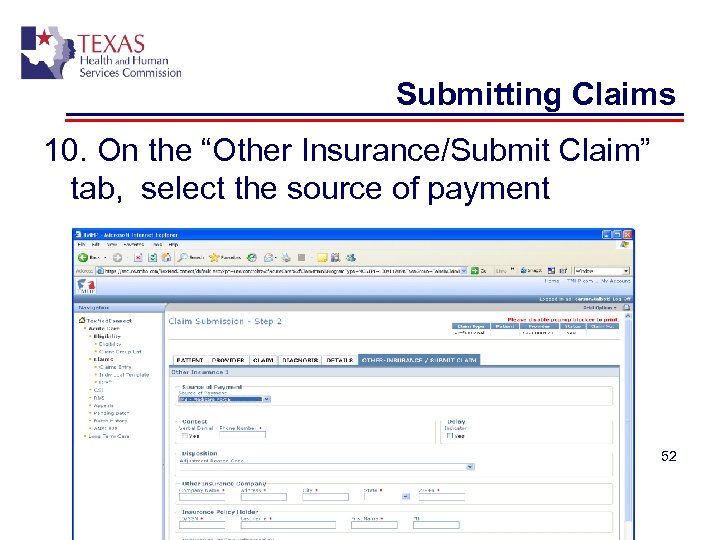
Submitting Claims 10. On the “Other Insurance/Submit Claim” tab, select the source of payment 52
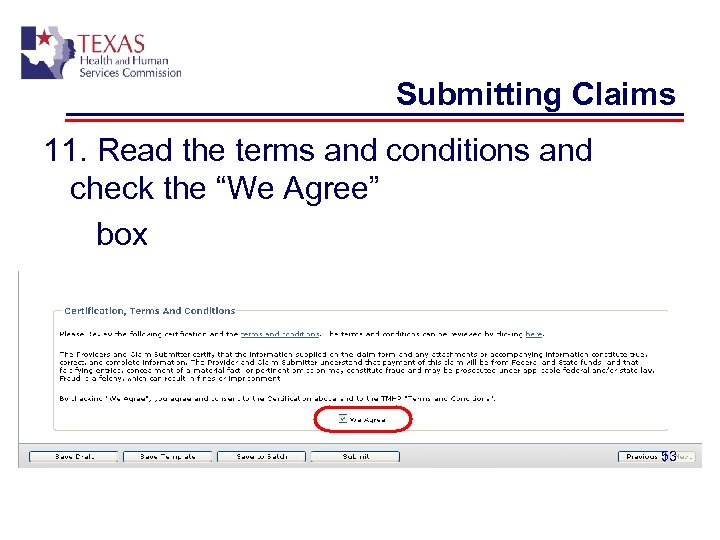
Submitting Claims 11. Read the terms and conditions and check the “We Agree” box 53
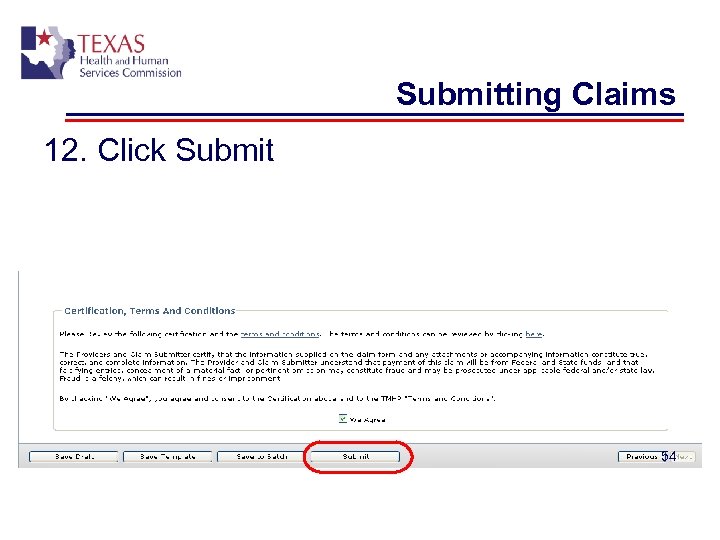
Submitting Claims 12. Click Submit 54
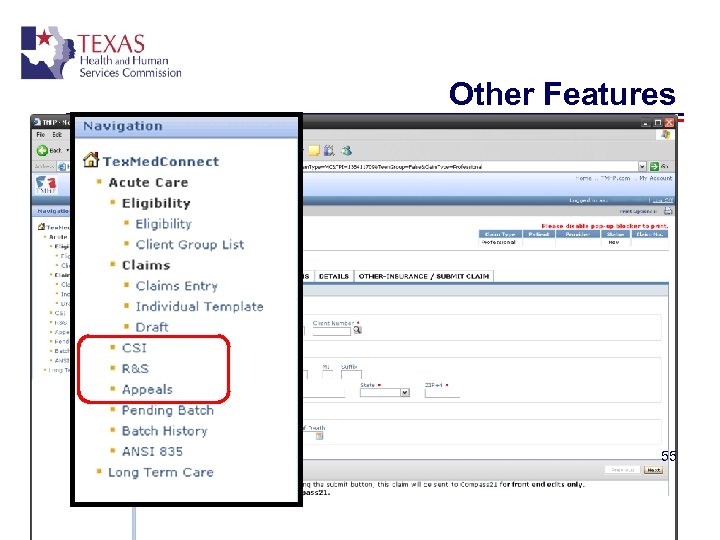
Other Features 55
Claim Status Inquiry (CSI) 56
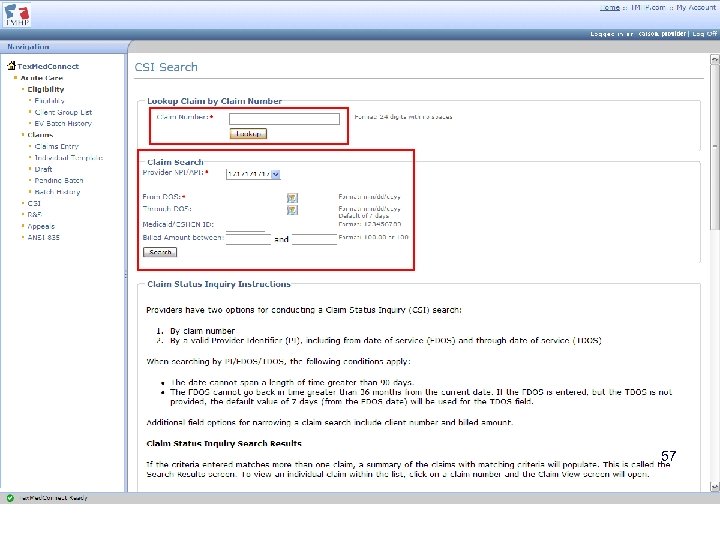
Enter the search information, either the claim number or NPI/FDOS/TDOS and other search criteria at the top of the CSI Search page 57
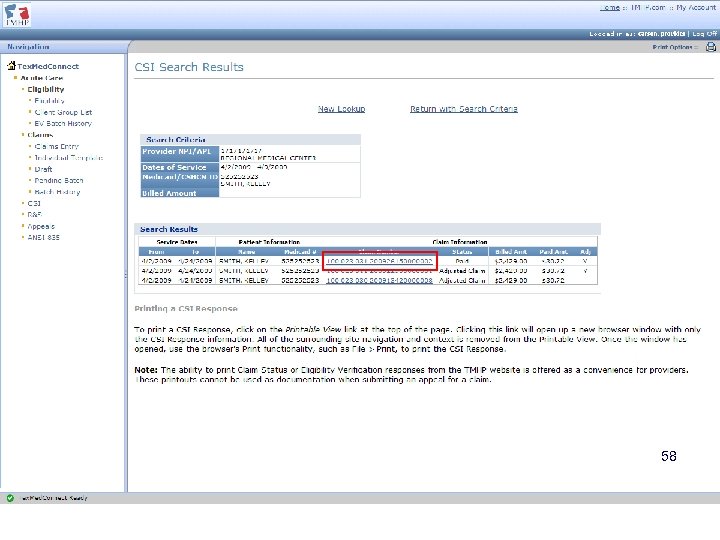
58
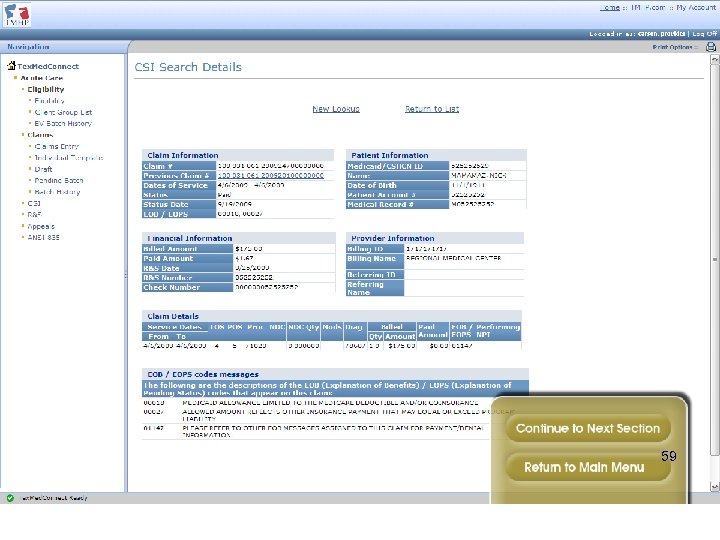
59
TMHP Website • • • Check for HIPAA updates Look up policy and process changes in published articles Download a PDF version of the most current Texas Medicaid Provider Procedures Manual Read the CMS-1500 Online Claims Submission Manual Review all of the fee schedules and reference codes needed for acute and longterm care 60
TMHP Website Computer-Based Training § Tex. Med. Connect - Acute § Provider Enrollment on the Portal (PEP) § Online Fee Lookup § Articles specific to the SUD benefits and rates can be located by accessing the TMHP website at http: //www. tmhp. com, “Providers”. Using the search option at the top of the page, type in “substance use disorder. ” This search will bring up articles including the published rates, required prior authorization forms, as well as detailed articles about the benefits that include treatment or admission criteria. 61
Prior Authorization 62
Prior Authorization for FFS and PCCM These services require prior authorization: • Ambulatory (outpatient) treatment extensions (beyond annual limit of 135 hours of group services, and 26 hours of individual services per calendar year) for clients ages 20 and under • Ambulatory detoxification • Residential treatment Note: Authorization requests must be for the least restrictive environment appropriate to client’s needs 63
Prior Authorization for FFS and PCCM Prior Authorization Request Submission Timelines: • Prior authorization requests for ambulatory detoxification, residential detoxification, or residential treatment services, must be submitted within three business days after the date of admission • Requests for continuation of ambulatory detoxification, residential detoxification, or residential treatment services must be received on or before the last day of the current authorization period. • Prior authorization requests for Ambulatory (outpatient) treatment extensions must be submitted prior to providing the extended services 64
Prior Authorization: Special Considerations for Adolescents Prior authorization for adolescent services (outpatient or residential) • Will not be issued for clients ages 13 or under unless the request includes a waiver from DSHS Regulatory and Licensing Division Residential and ambulatory detoxification: • Prior authorization requests for clients ages 20 and under to exceed 21 days of detoxification require TMHP medical director review with documentation of medical necessity from a physician familiar with client. Ambulatory counseling extensions: • Prior authorization requests for outpatient treatment extensions for clients ages 20 and under exceeding the benefit limits, (135 hours group counseling; 26 hours individual services per calendar year) may be considered with physician documentation of medical need for continued treatment. The physician does not need to be affiliated with a treatment facility. 65
Prior Authorization: Special Considerations for Adolescents Residential treatment: • Prior authorization requests for clients ages 20 and under to exceed the benefit limit of 35 days per episode of residential treatment may be considered only on an individual client basis with documentation from a physician supporting the medical necessity for continuation of the treatment. This documentation must include: – Specific reasons or client conditions that make it medically necessary for this client to receive further care at the residential level. – Specific reasons or client conditions that prevent this client from being treated in less restrictive outpatient services. Note: A residential treatment program’s established length of stay for all clients 20 years of age or younger, which is greater than 35 days is not considered documentation of medical necessity. 66
Prior Authorization for FFS and PCCM The following services do not require prior authorization: • Assessment • Outpatient treatment services, unless calendar year hours are exceeded for clients ages 20 and under • Medication assisted therapy (MAT) 67
Prior Authorization for FFS and PCCM • Providers may submit one of the following forms by fax at 512 -614 -4211 or submit the request online at tmhp. com: • Ambulatory (Outpatient) Substance Abuse Counseling Extension Request Form • Ambulatory (Outpatient) Detoxification Authorization Request Form • Ambulatory (Outpatient) Substance Abuse Counseling Extension Request Form • Residential Substance Abuse Treatment Authorization Request Form • Residential Detoxification Authorization Request Form • These forms can be located at the TMHP website at: http: //www. tmhp. com under Texas Medicaid/Forms 68
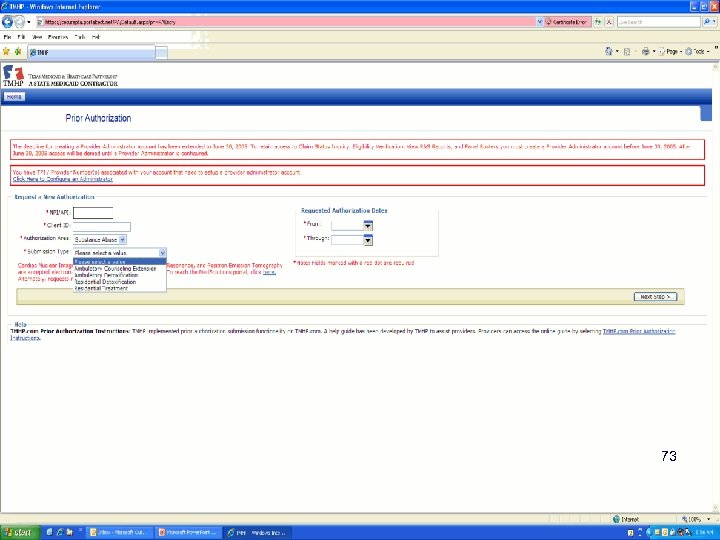
New Online Prior Authorization Request Process: FFS or PCCM • Since March 25, 2011, prior authorization requests for the following SUD services may be submitted online through the secure portion of the TMHP website at http: //www. tmhp. com • Ambulatory (outpatient) detoxification • Ambulatory (outpatient) counseling extensions for clients ages 20 and under • Residential substance abuse treatment • Note: Online prior authorization for residential detoxification will be available beginning June 25, 2011. 69
New Online Prior Authorization Request Process: FFS or PCCM • To get to the online prior authorization for SUD services, follow these steps: 1. Click I would like to in the upper right hand side of any Medicaid providers page. The “I would like to” page appears. 2. Click “Submit a prior authorization request. ” If you haven’t previously logged in to your account, you will be asked to log in. The prior authorization page appears. 3. Select Substance Abuse from the Authorization 70 Area drop-down menu.
New Online Prior Authorization Request Process: FFS or PCCM 4. Select one of the following from the Submission Type drop-down menu: Ambulatory Counseling Extension Ambulatory Detoxification Residential Treatment 5. Complete all remaining fields and questions, and follow the directions to complete the SUD prior authorization request. • Note: Contact TMHP at 1 -800 -925 -9126 or refer to the online Provider Electronic Authorization Submission Guide for more information on submitting online authorization requests The guide may be accessed from the “I would like to” page or the authorization entry pages 71
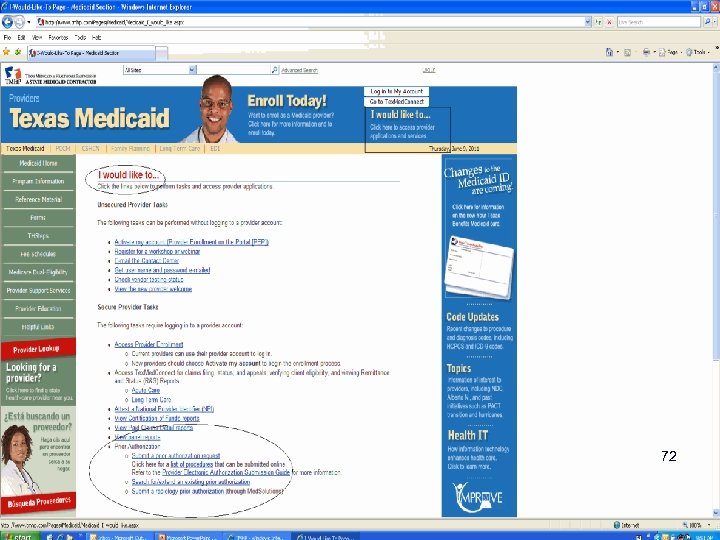
New Online Prior Authorization Request Process: FFS or PCCM 72
73
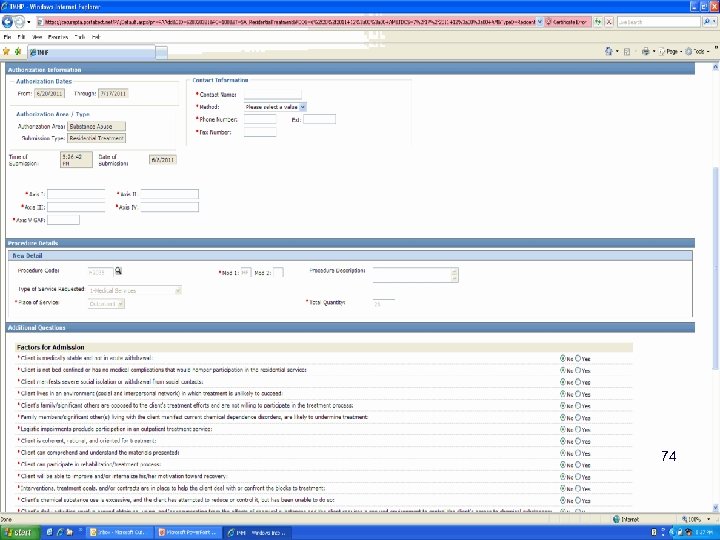
New Online Prior Authorization Request Process: FFS or PCCM 74
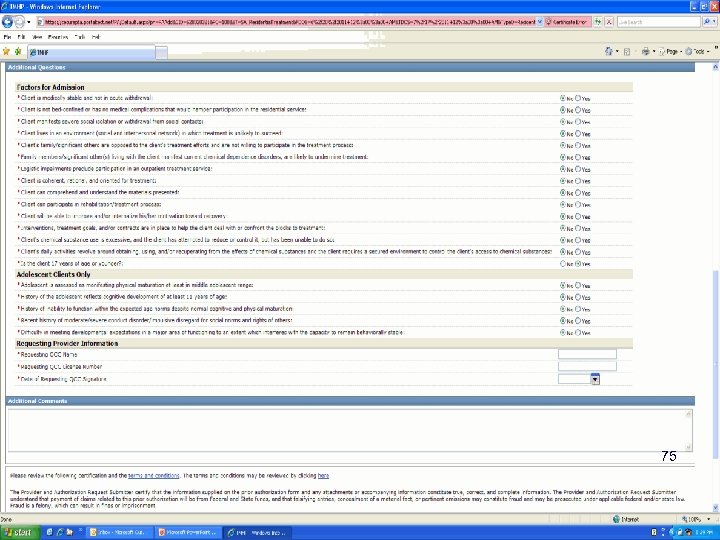
75
New Online Prior Authorization Request Process: FFS or PCCM Additional Prior Authorization Online Functions: • Search for existing authorization requests Providers can search by authorization number, client Medicaid number, or provider number All authorization requests are searchable regardless of submission manner • View an existing authorization Providers can check the authorization status, dates, and other authorization information 76
New Online Prior Authorization Request Process: FFS or PCCM • Request an extension of an existing authorization Basic steps: • • • Open the authorization you want to extend from the search results Click the “Request an Extension” button Enter the dates requested for the extension In the Additional Questions section, select Substance Abuse in the Authorization Area and the Submission Type for the extension request from the drop-down menus Answer all of the associated questions and submit Note: Refer to the online Provider Electronic Authorization Submission Guide for more information on authorization searches and submitting extensions requests The guide may be accessed from the “I would like to” page or the authorization search and extension pages 77
Prior Authorization continued: PCCM and FFS • Authorization requests may also be submitted by mail to: Texas Medicaid and Healthcare Partnership TMHP Prior Authorization Dept. 12357 -B Riata Trace Parkway, Suite 150 Austin, TX 78727 • Call TMHP Prior Authorization Unit at 1 -800 -2138877, Option 2 for more information about the SUD benefits, prior authorization process, or status of a PA request. 78
Prior Authorization: STAR and STAR+PLUS health plans • Prior authorization requirements may vary by health plan. (Note that some health plans may require prior authorization for all services except assessment. ) • Call health plan for specific information. • Exception: Prior Authorization is not required for services for Dual Eligible clients (Medicaid and Medicare) in STAR+PLUS, regardless of the service rendered. • Special situation: STAR SSI recipients should have their SUD services prior-authorized by the health plan, although claim is paid through TMHP. 79
Confirming Eligibility 80
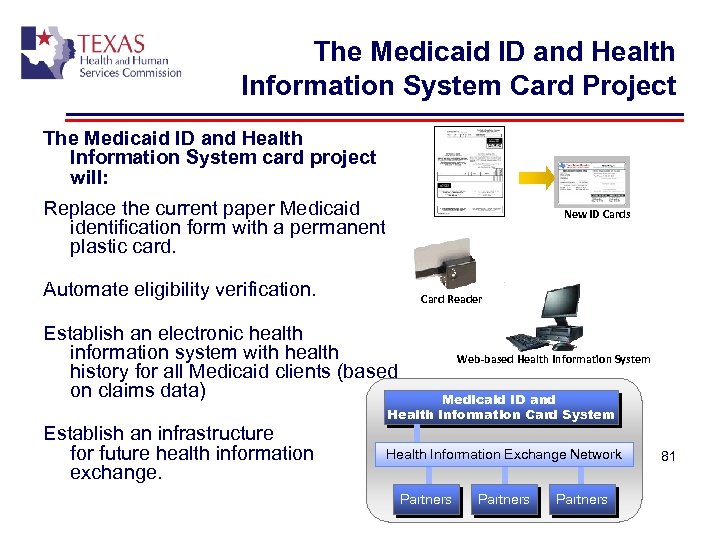
The Medicaid ID and Health Information System Card Project The Medicaid ID and Health Information System card project will: Replace the current paper Medicaid identification form with a permanent plastic card. New ID Cards Automate eligibility verification. Card Reader Establish an electronic health information system with health history for all Medicaid clients (based on claims data) Establish an infrastructure for future health information exchange. Web-based Health Information System Medicaid ID and Health Information Card System Health Information Exchange Network Partners 81
Effective June, 2011: New “Your Texas Benefits Card” • Beginning late June, 2011, clients will begin to receive the “Your Texas Benefits” Medicaid card in the mail. Clients can start using the card in July. • This plastic card with a magnetic stripe uses digital technology to streamline the eligibility verification process. • The card shows the same type of information shown on private health insurance cards. It includes client name, Medicaid program name, Medicaid number, and health plan name and phone number. • The card replaces the Medicaid ID form letter (Form 3087) that clients have been getting in the mail every month. • Certain clients residing in PCCM counties will not get their card until September 2011. These clients will continue receiving the form 3087 until they receive their cards. 82
Effective June, 2011: New “Your Texas Benefits Card” • Use the card to verify eligibility. • No equipment purchase is required to access client information through the Med ID card system. • However, the card’s magnetic stripe has the client’s Med ID number and can be read by most swipe-style card readers. The card is designed to work with standard magnetic card readers available at many electronics retailers or online. 83
Effective June, 2011: New “Your Texas Benefits Card” • At no cost, providers will be able to access the full functionality of the system without any automation by manually entering the Medicaid ID number into the provider website. To verify eligibility, providers can: • Use the secure website – http: //www. Your. Texas. Benefits. Card. com • Call the TMHP Contact Center at 1 -800 -925 -9126. TMHP’s Automated Inquiry System (AIS) can be accessed at this number. • Visit Tex. Med. Connect on the TMHP website. To view client eligibility online, go to http: //www. tmhp. com Click on “Verify Client Eligibility” under the “I would like to” list at the right. • View the client’s Temporary Medicaid Eligibility Verification Form (Form H 1027) or the “old” form H 3087 where applicable. HHSC anticipates that the Form 3087 will be discontinued in August, 2011. 84
Effective June 1, 2011: New Your Texas Benefits Card • Automation devices are optional. If an automation option (i. e. , card reader) is chosen, then providers are responsible for the costs. HHSC will publish specifications for leveraging existing point-of-sale and card readers devices to access the system. • Having a card does not mean the client has Medicaid coverage, because clients will be instructed to keep the card even if their Medicaid coverage expires. It can be reused if the patient regains Medicaid coverage. • If the client fails to bring their card to the office, HHSC eligibility workers can still generate a Temporary Medicaid eligibility verification form (H 1027). It must be requested in person at an HHSC eligibility office. Call 2 -1 -1 for the nearest office. • In August 2011, clients will be able to print the card image from the client portal using a personal computer rather than going to the local office to request the temporary card. 85
Information • FAQs for stakeholders (posted) www. hhsc. state. tx. us/Quick. Answers/Med. Card-FAQs. shtml • Medicaid Call transfer Helpdesk for both clients and providers: 1 -800 -252 -8263. This number is printed on the Your Texas Benefits Card. • Information for Providers (posted) www. tmhp. com (Click on “providers, ” then “Changes to the Med ID are coming” in the blue box to the right) Questions about automation options, provider portal support/issues, THSteps notifications/alerts, and current provider information: 1 -855 -827 -3747 • Information for Clients and Providers(posted) www. Your. Texas. Benefits. com 86
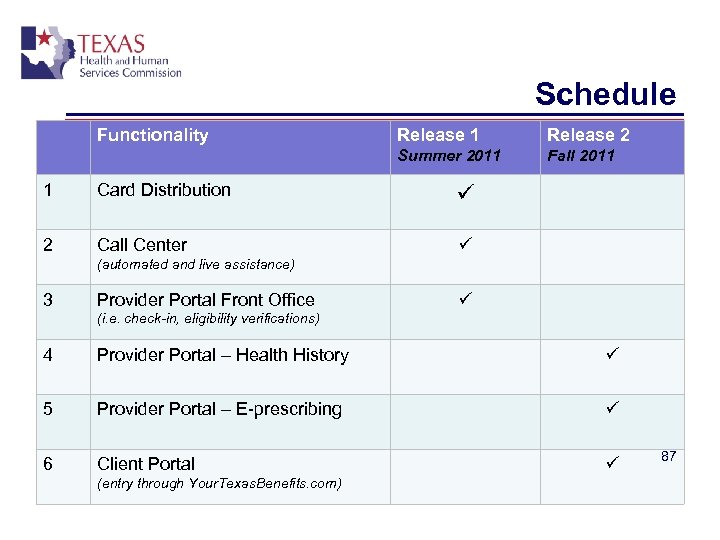
Schedule Functionality Release 1 Release 2 Summer 2011 Fall 2011 1 Card Distribution 2 Call Center (automated and live assistance) 3 Provider Portal Front Office (i. e. check-in, eligibility verifications) 4 Provider Portal – Health History 5 Provider Portal – E-prescribing 6 Client Portal (entry through Your. Texas. Benefits. com) 87
What to do if client does not have Medicaid • Provide the client the resources to access Medicaid application. (e. g. , applications in office, website for application, locations of eligibility offices) • Clients with prior medical bills may be able to have Medicaid established retroactively, but the client must provide this information during the application process. • Block grant providers may bill to the block grant for services rendered prior to Medicaid establishment. • If not a block grant provider, options include accepting client until Medicaid is established, or to refer to a block grant provider. Clients that do not have Medicaid coverage can be billed until Medicaid is established. • Medicaid recipients cannot be billed for Medicaid 88 covered services.
Reminders: How Clients Access Benefits 89
How clients access benefits • Client can self-refer or be referred for an assessment; no referral from a primary care provider (PCP) is required. • Assessment must be made before services can start. No prior authorization needed for assessments, regardless of whether the client is in fee-for-service Medicaid, PCCM, STAR or STAR+PLUS. 90
How clients access benefits STAR and STAR+PLUS • Assessments provided by in-network CDTFs licensed by DSHS. • To find a network provider: – Call health plan (providers can call health plan provider number, clients can call client number on health plan ID) – Contact a provider, ask if they take clients from their health plan – Look in health plan provider directory (provided upon enrollment in Medicaid managed care) – Look up a provider on health plan website (i. e. , online provider directory) 91
How clients access benefits PCCM and FFS • Client assessments by any Medicaid-enrolled DSHSlicensed CDTF. • After assessment, the facility obtains prior authorization from TMHP to begin services, if required. • To locate a Medicaid-enrolled facility, client can: • • Contact a provider, and ask if provider takes Medicaid. PCCM only: Call PCCM client helpline at 1 -888 -302 -6688. FFS only: Call the client helpline at 1 -800 -335 -8957. Providers can assist clients in finding a provider by calling the PCCM provider helpline at 1 -888 -834 -7226 when serving PCCM clients, or the TMHP provider contact center 1 -800 -925 -9126 92 when serving clients that are fee-for-service Medicaid.
Medical Transportation Program • Medicaid recipients qualify for free transportation assistance to their appointments for substance abuse treatment through the Medical Transportation Program if they have no other means to get to their appointments. • MTP phone number for clients is: 1 -877 -6338747 (TTY: 1 -800 -735 -2989), Monday to Friday, 8 a. m. to 5 p. m. • This program can provide help such as local bus fare, gas money, advance travel funds, and bus or plane tickets if the client needs to go out of area for treatment. 93
Resources • Texas Medicaid & Healthcare Partnership (TMHP) Contact Center: 1 -800 -925 -9126 • Questions about benefits – Option #2 for provider inquiries • Provider enrollment—Option #2 for provider inquiries, then option #3 for enrollment • Confirming Medicaid eligibility –Option #1 for automated inquiries • TMHP website: http: //www. tmhp. com (Click “Providers. ” Search for “Substance Use Disorder. ”) • Medicaid bulletin articles for SUD benefits, rates, and prior authorization. • Rates and prior authorization requirements outlined in the Medicaid bulletin articles apply to Primary Care Case Management and fee-for-service Medicaid. There may be differences in rates or prior authorization requirements for Medicaid managed care health plans (STAR and STAR+PLUS). • Call the appropriate health plan, STAR or STAR+PLUS, for: • Managed care-related billing issues • Prior-authorization requirements • Questions, issues or complaints • Health plan provider credentialing 94
Resources • Contact the Health and Human Services Commission for: STAR or STAR+PLUS-related issues or complaints if you feel the health plan has not adequately addressed your issue or concern. • • • HPM_Complaints@hhsc. state. tx. us Dept. of State Health Services Substance Abuse Prevention and Treatment (SAPT) Block Grant Charles Thibodeaux at 1 -512 -206 -4761 or Charles. Thibodeaux@dshs. state. tx. us DSHS Substance Abuse treatment information: http: //www. dshs. state. tx. us/ • Medical Transportation (MTP) phone number for clients is: 1 -877 -633 -8747 (TTY: 1 -800 -7352989), http: //www. hhsc. state. tx. us/Quick. Answers/Get. Ride_FAQs. shtml • More information can be found in the Texas Medicaid Provider Procedures Manual at www. tmhp. com (under “provider manuals and guides” on the lower right side of the home page. ) Includes basic billing information, as well as program-specific information. • Medicaid Managed Care expansion: http: //www. hhsc. state. tx. us/medicaid/MMC-Proposals. shtml 95
d368cb65d588b6eecc7d9b1a6c8643a4.ppt