9c0618daeecd15fdebf7c1c830eb7b5a.ppt
- Количество слайдов: 57
Medicaid Eligibility Verification Options & CMS-1500 (08 -05) Billing Guidelines October – December 2008 www. dmas. virginia. gov Department of Medical Assistance Services
****** This presentation is to facilitate training of the subject matter in Chapter V of the Virginia Medicaid Psychiatric Services Manual. This training contains only highlights of this manual and is not meant to substitute for or take the place of the Psychiatric Services Manual. 2
Objectives o o o Upon completion of this training you should be able to : Correctly utilize Medicaid options to verify eligibility Understand timely filing guidelines Properly submit Medicaid claims, adjustments and voids 3
As a Participating Provider You Musto o o Determine the patient’s identity. Verify the patient’s age. Verify the patient’s eligibility. Accept, as payment in full, the amount paid by Virginia Medicaid. Bill any and all other third party carriers. 4
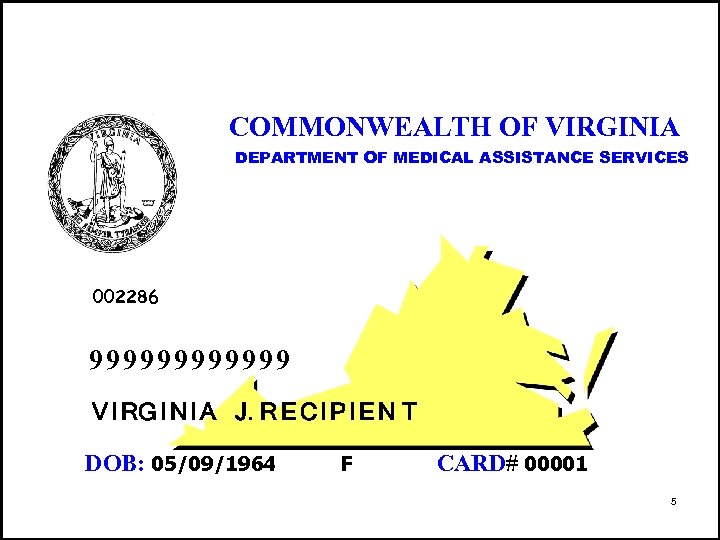
COMMONWEALTH OF VIRGINIA DEPARTMENT OF MEDICAL ASSISTANCE SERVICES 002286 999999 V I RG I N I A J. R E C I P I E N T DOB: 05/09/1964 F CARD# 00001 5
Important Contacts o o Medi. Call ARS- Web-Based Medicaid Eligibility Provider Call Center Provider Enrollment 6

Medi. Call 800 -884 -9730 800 -772 -9996 804 -965 -9732 804 -965 -9733 7
Medi. Call o o o o Available 24 hours a day, 7 days a week Medicaid Eligibility Verification Claims Status Prior Authorization Information Primary Payer Information Medallion Participation Managed Care Organization Assignment 8
Automated Response System ARS o Web-based eligibility verification option n n Free of Charge. Information received in “real time”. Secure Fully HIPAA compliant 9
UAC Registration Process Go to https: //virginia. fhsc. com n n Select the ARS tab on FHSC ARS Home Page Choose “User Administration” Follow the on-screen instructions for help with registration, this is a 3 -step process to request, register and activate a new account Answer the initial ‘Who are you? ’ question by selecting ‘I do not have a User ID and need to be a Delegated Administrator’ 10
ARS –Users o Web Support Helplineo ARS Manual (User Guide) 800 -241 -8726 http: //virginia. fhsc. com 11

Provider Call Center Claims, covered services, billing inquiries: 800 -552 -8627 804 -786 -6273 8: 30 am – 4: 30 pm (Monday-Friday) 11: 00 am – 4: 30 pm (Wednesday) 12
Provider Enrollment New provider numbers or change of address: First Health – PEU P. O. Box 26803 Richmond, VA 23261 888 -829 -5373 804 -270 -5105 804 -270 -7027 - Fax 13
Electronic Billing Electronic Claims Coordinator Mailing Address First Health Services Corporation Virginia Operations Electronic Claims Coordinator 4300 Cox Road Glen Allen, VA 23060 E-mail: edivmap@fhsc. com Phone: (800) 924 -6741 14 Fax: (804) 273 -6797
Billing on the CMS-1500 15
MAIL CMS-1500 FORMS TO: DEPARTMENT OF MEDICAL ASSISTANCE SERVICES PRACTITIONER P. O. Box 27444 Richmond, Virginia 23261 16
TIMELY FILING o o ALL CLAIMS MUST BE SUBMITTED AND PROCESSED WITHIN ONE YEAR FROM THE DATE OF SERVICE EXCEPTIONS n n o Retroactive/Delayed Eligibility Denied Claims NO EXCEPTIONS n Other Primary Insurance 17
TIMELY FILING o Submit claims with documentation attached (to the back of claim) explaining the reason for delayed submission 18
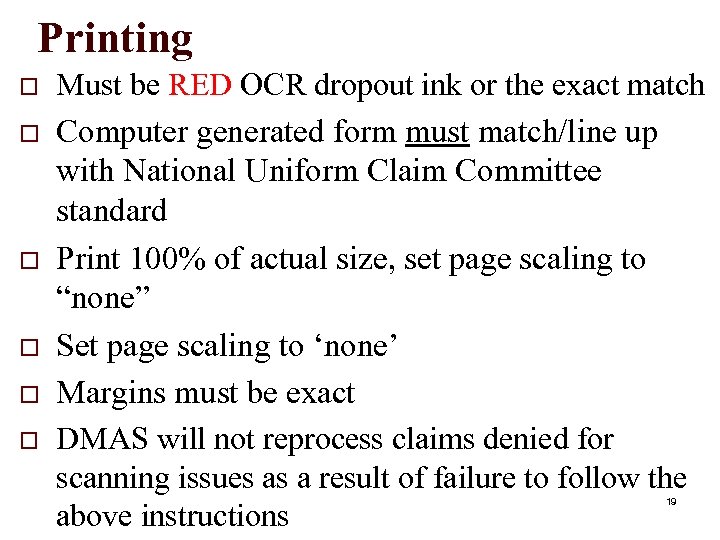
Printing o o o Must be RED OCR dropout ink or the exact match Computer generated form must match/line up with National Uniform Claim Committee standard Print 100% of actual size, set page scaling to “none” Set page scaling to ‘none’ Margins must be exact DMAS will not reprocess claims denied for scanning issues as a result of failure to follow the above instructions 19
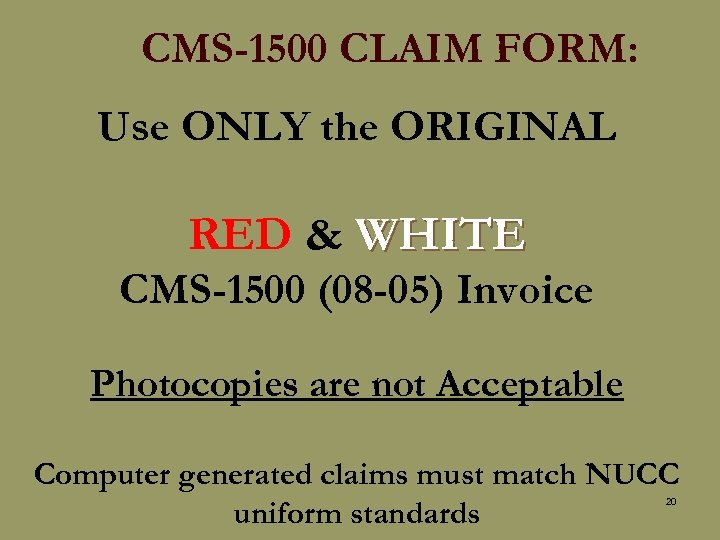
CMS-1500 CLAIM FORM: Use ONLY the ORIGINAL RED & WHITE CMS-1500 (08 -05) Invoice Photocopies are not Acceptable Computer generated claims must match NUCC uniform standards 20
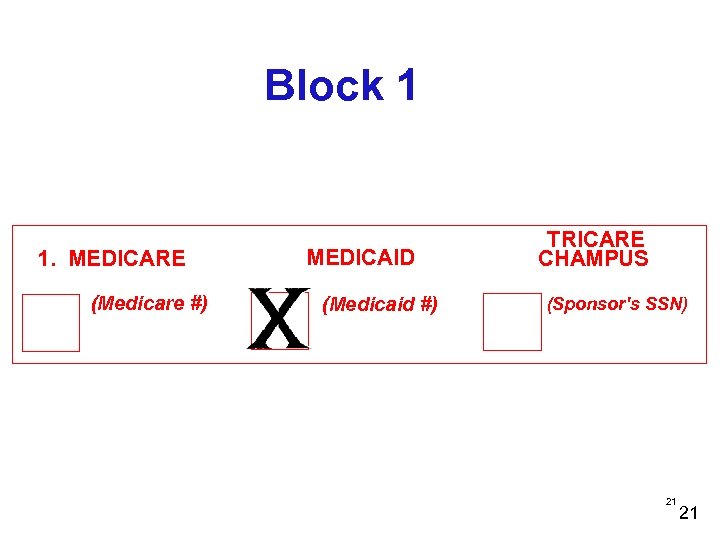
Block 1 1. MEDICARE (Medicare #) MEDICAID (Medicaid #) TRICARE CHAMPUS (Sponsor's SSN) 21 21
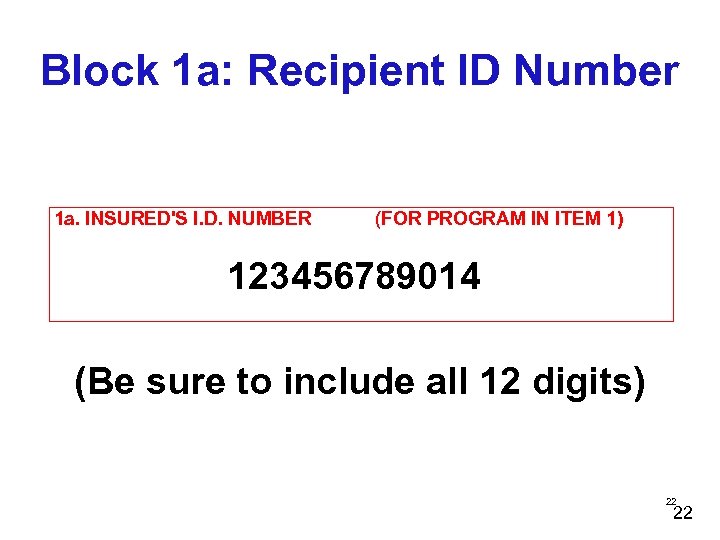
Block 1 a: Recipient ID Number 1 a. INSURED'S I. D. NUMBER (FOR PROGRAM IN ITEM 1) 123456789014 (Be sure to include all 12 digits) 22 22
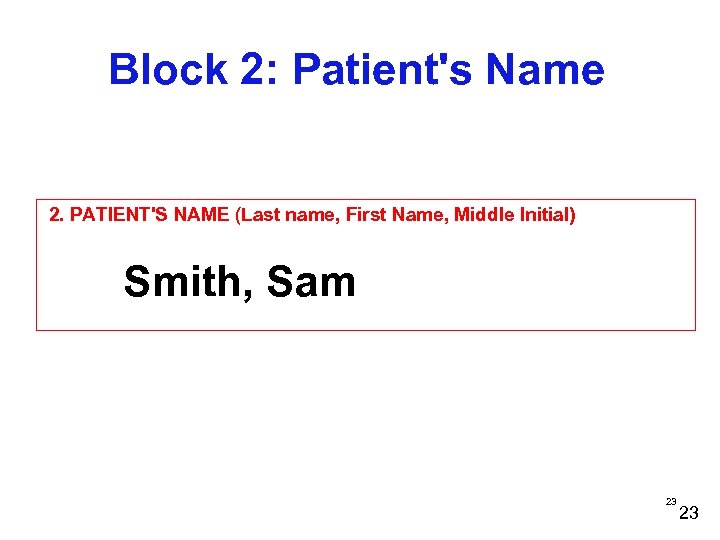
Block 2: Patient's Name 2. PATIENT'S NAME (Last name, First Name, Middle Initial) Smith, Sam 23 23
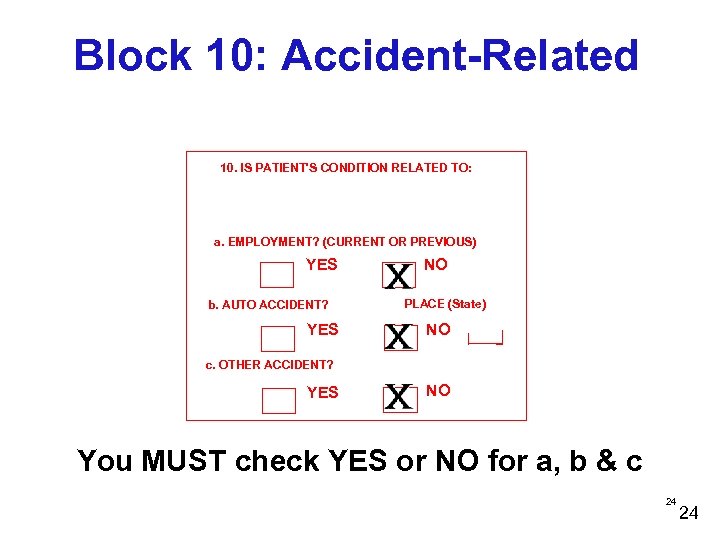
Block 10: Accident-Related 10. IS PATIENT'S CONDITION RELATED TO: a. EMPLOYMENT? (CURRENT OR PREVIOUS) YES b. AUTO ACCIDENT? YES NO PLACE (State) NO c. OTHER ACCIDENT? YES NO You MUST check YES or NO for a, b & c 24 24
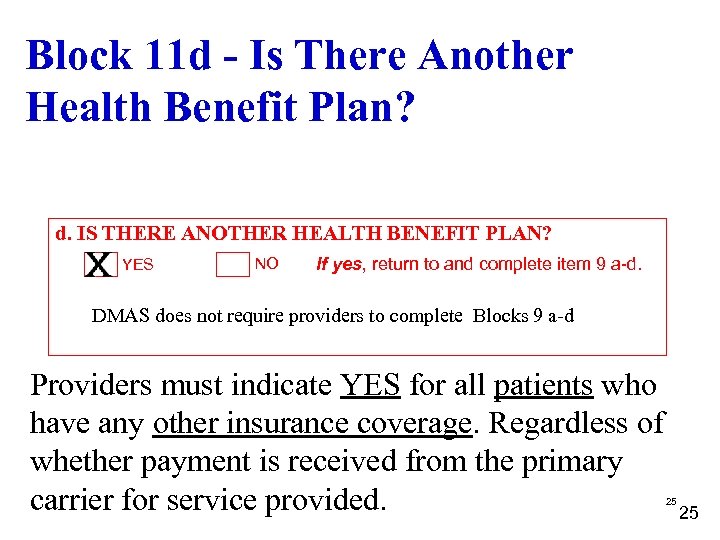
Block 11 d - Is There Another Health Benefit Plan? d. IS THERE ANOTHER HEALTH BENEFIT PLAN? YES NO If yes, return to and complete item 9 a-d. DMAS does not require providers to complete Blocks 9 a-d Providers must indicate YES for all patients who have any other insurance coverage. Regardless of whether payment is received from the primary carrier for service provided. 25 25
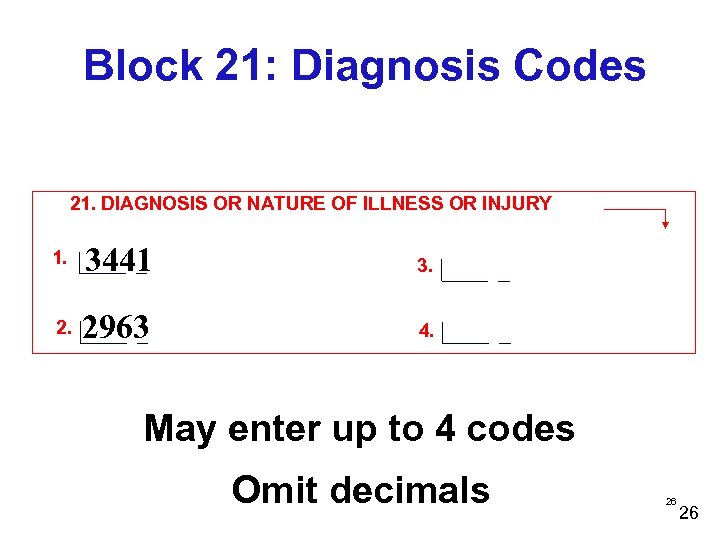
Block 21: Diagnosis Codes 21. DIAGNOSIS OR NATURE OF ILLNESS OR INJURY 1. 3441 3. 2963 4. May enter up to 4 codes Omit decimals 26 26
Block 23: Prior Authorization Number - Conditional 23. PRIOR AUTHORIZATION NUMBER 27 27
Blocks 24 A thru 24 J o o o These blocks have been divided into open areas and a shaded red line area The shaded area is ONLY for supplemental information Instructions will be given on when the use of the shaded area is required for claims processing 28
TPL Information Block 24 A o o Qualifier ‘TPL’ will be used followed by dollars/cents amount whenever an actual payment is made by a third party carrier No spaces between the qualifier and dollars and no $ symbol used Decimal between dollars and cents is required to read paid amount correctly Must be left justified 29
TPL Information Block 24 A o DMAS will set COB code based on the information given in locator 11 d: n n n No, or nothing indicated-no other carrier on file for the recipient, Medicaid will pay primary No, or nothing indicated and system has other insurance coverage on file - claim will deny bill other insurance No, or nothing indicated and ‘TPL’ qualifier with payment listed in 24 a red shaded area – Medicaid will coordinate benefits with other carrier 30
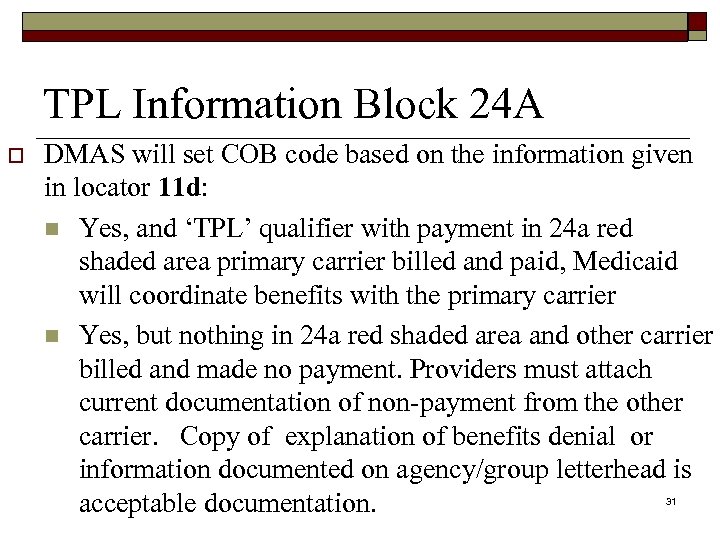
TPL Information Block 24 A o DMAS will set COB code based on the information given in locator 11 d: n Yes, and ‘TPL’ qualifier with payment in 24 a red shaded area primary carrier billed and paid, Medicaid will coordinate benefits with the primary carrier n Yes, but nothing in 24 a red shaded area and other carrier billed and made no payment. Providers must attach current documentation of non-payment from the other carrier. Copy of explanation of benefits denial or information documented on agency/group letterhead is acceptable documentation. 31
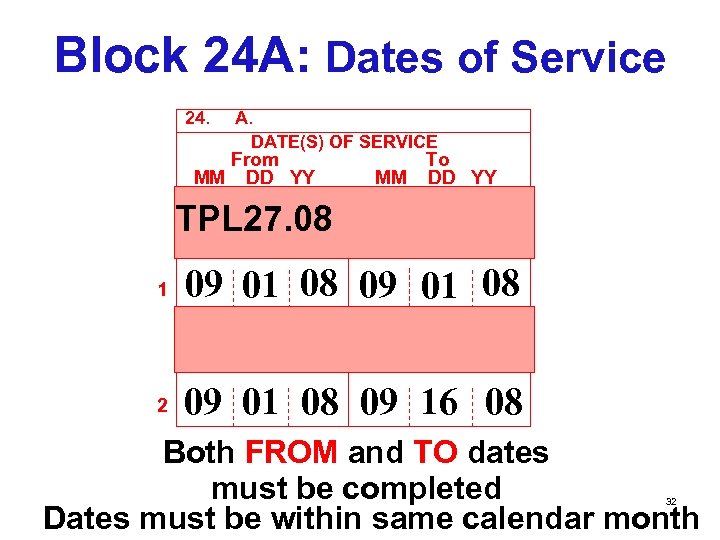
Block 24 A: Dates of Service 24. A. DATE(S) OF SERVICE From MM DD YY To MM DD YY TPL 27. 08 1 09 01 08 2 09 01 08 09 16 08 Both FROM and TO dates must be completed Dates must be within same calendar month 32
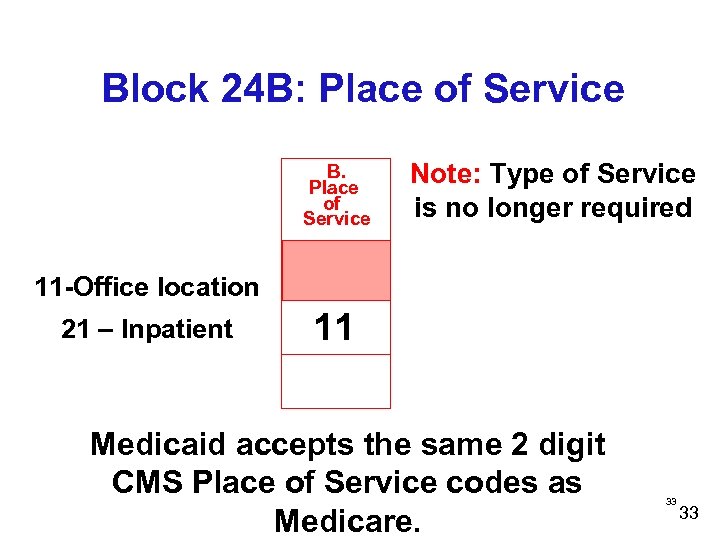
Block 24 B: Place of Service B. Place of Service Note: Type of Service is no longer required 11 -Office location 21 – Inpatient 11 Medicaid accepts the same 2 digit CMS Place of Service codes as Medicare. 33 33
Emergency Indicator-24 C o o o This locator will be used to indicate whether the procedure was an emergency DMAS will only accept a ‘Y’ for yes in this locator If there was no emergency leave blank 34
Block 24 C: EMG C. EMG 35 35
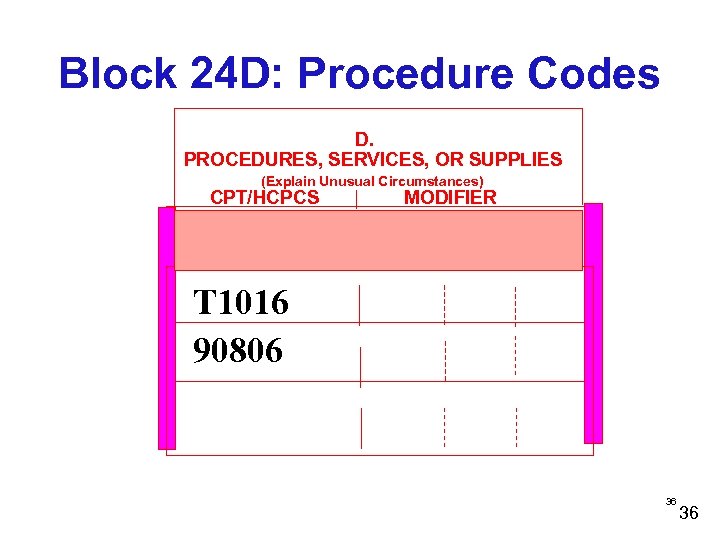
Block 24 D: Procedure Codes D. PROCEDURES, SERVICES, OR SUPPLIES (Explain Unusual Circumstances) CPT/HCPCS MODIFIER T 1016 90806 36 36
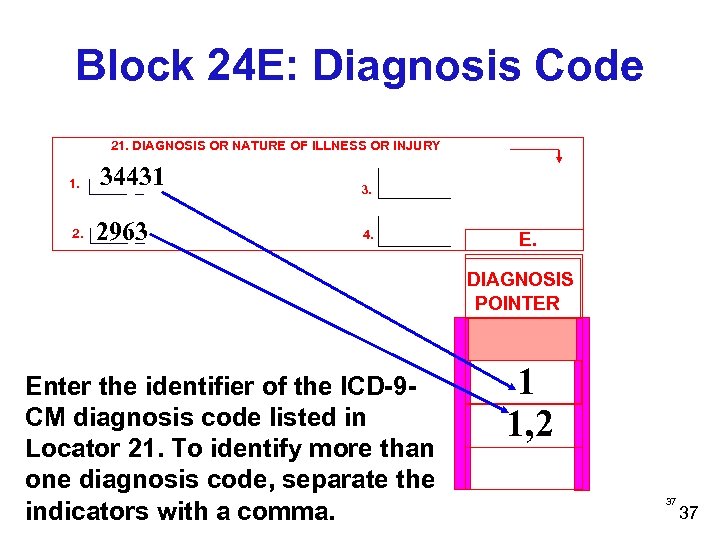
Block 24 E: Diagnosis Code 21. DIAGNOSIS OR NATURE OF ILLNESS OR INJURY 1. 34431 3. 2963 4. E. DIAGNOSIS POINTER Enter the identifier of the ICD-9 CM diagnosis code listed in Locator 21. To identify more than one diagnosis code, separate the indicators with a comma. 1 1, 2 37 37
Block 24 F: Charges F. $ CHARGES Enter the usual and customary charges 38 38
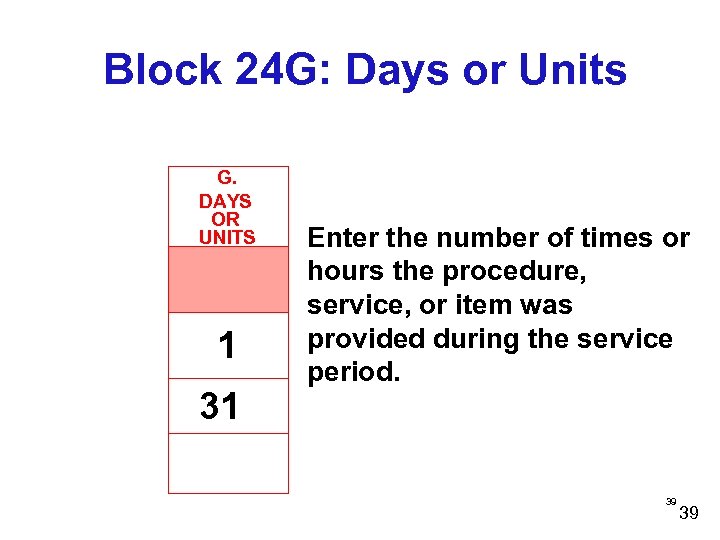
Block 24 G: Days or Units G. DAYS OR UNITS 1 31 Enter the number of times or hours the procedure, service, or item was provided during the service period. 39 39
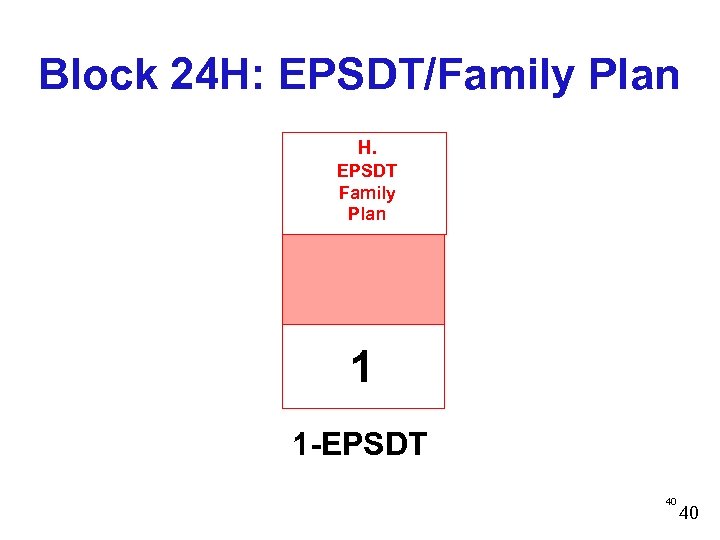
Block 24 H: EPSDT/Family Plan H. EPSDT Family Plan 1 1 -EPSDT 40 40
ID. QUAL o o o Block-24 I Qualifier ‘ 1 D’ is to be used in the red shaded area for claims being submitted using the Atypical Provider Identifier (API). DMAS requires Treatment Foster Care agencies to bill with an API. Qualifier ‘ZZ’ is to be used to indicate the taxonomy code-only when the NPI is used and only if necessary to adjudicate the claim. 41
Rendering Provider ID # Block-24 J o o The shaded red area will contain the API OR The open area will contain the NPI of the provider rendering the service. 42
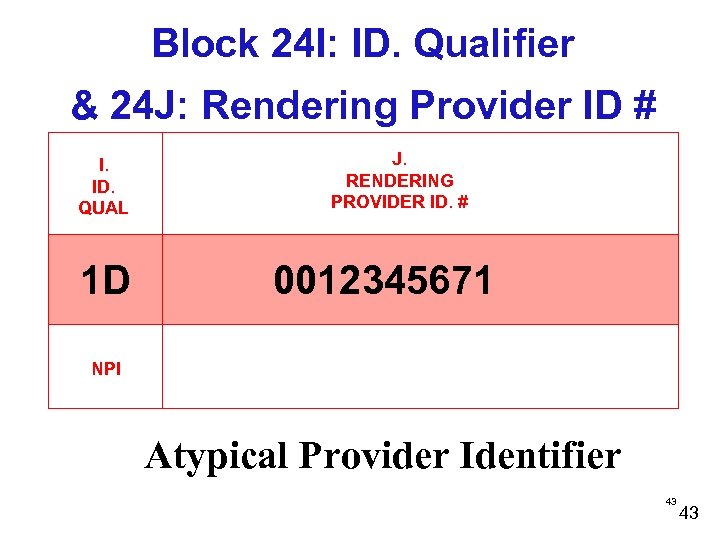
Block 24 I: ID. Qualifier & 24 J: Rendering Provider ID # I. ID. QUAL 1 D J. RENDERING PROVIDER ID. # 0012345671 NPI Atypical Provider Identifier 43 43
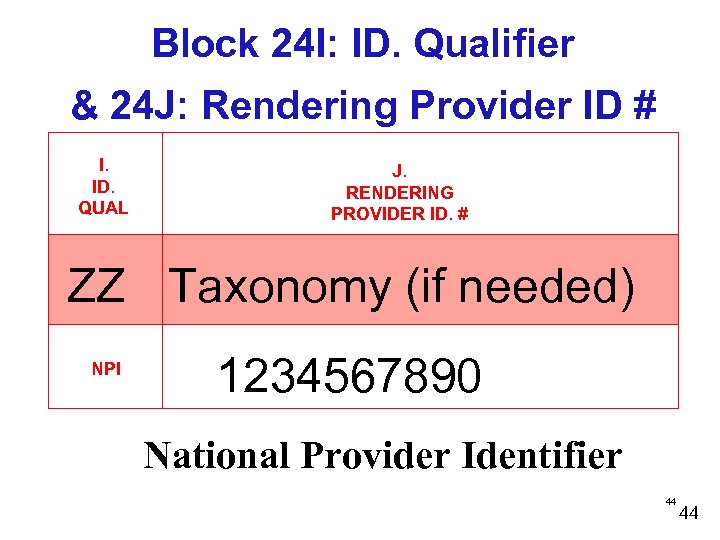
Block 24 I: ID. Qualifier & 24 J: Rendering Provider ID # I. ID. QUAL J. RENDERING PROVIDER ID. # ZZ Taxonomy (if needed) NPI 1234567890 National Provider Identifier 44 44
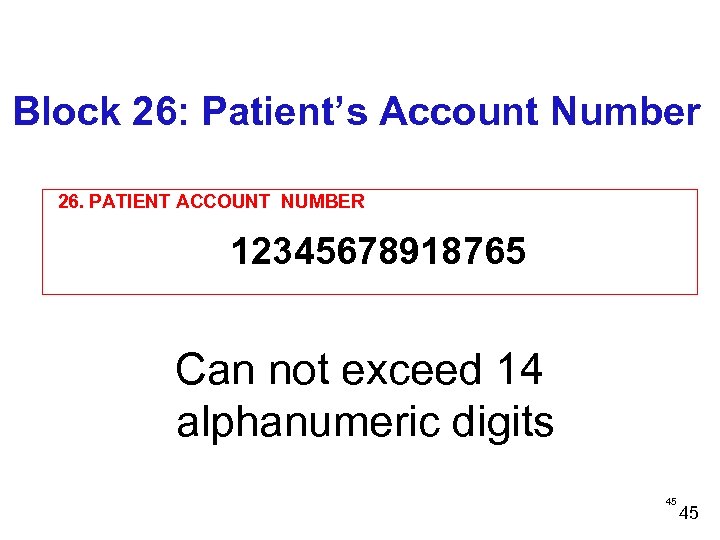
Block 26: Patient’s Account Number 26. PATIENT ACCOUNT NUMBER 12345678918765 Can not exceed 14 alphanumeric digits 45 45
Block 28: Total Charges 28. TOTAL CHARGE $ 46 46
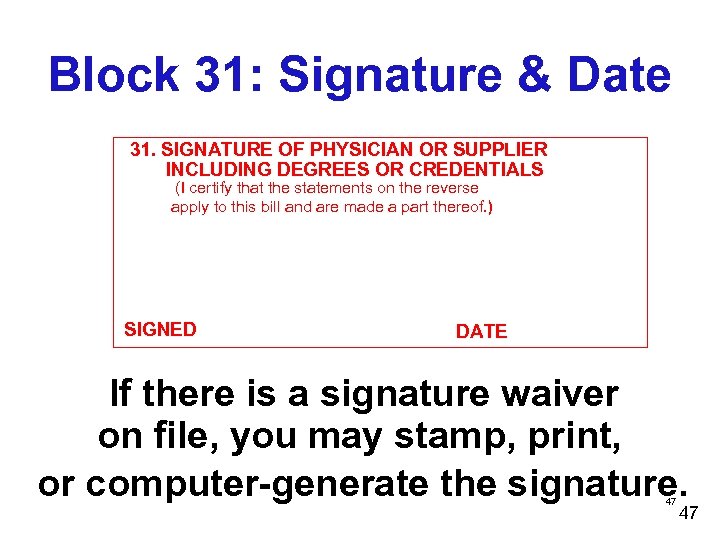
Block 31: Signature & Date 31. SIGNATURE OF PHYSICIAN OR SUPPLIER INCLUDING DEGREES OR CREDENTIALS (I certify that the statements on the reverse apply to this bill and are made a part thereof. ) SIGNED DATE If there is a signature waiver on file, you may stamp, print, or computer-generate the signature. 47 47
Block 32 Service Facility Location Information o Enter information for the location where services were rendered n First line-Name n Second line-Address n Third line-City, State, 9 digit zip code n No punctuation in the address n Space between city and state n Include hyphen for the 9 digit zip code 48
Block 32, cont’d. Service Facility Location Information o Providers with multiple offices/locations the zip code must reflect the office/ location where services were rendered o Enter the 10 digit NPI number of the service location in 32 a. OR Enter ‘ 1 D’ qualifier with the API in 32 b o 49
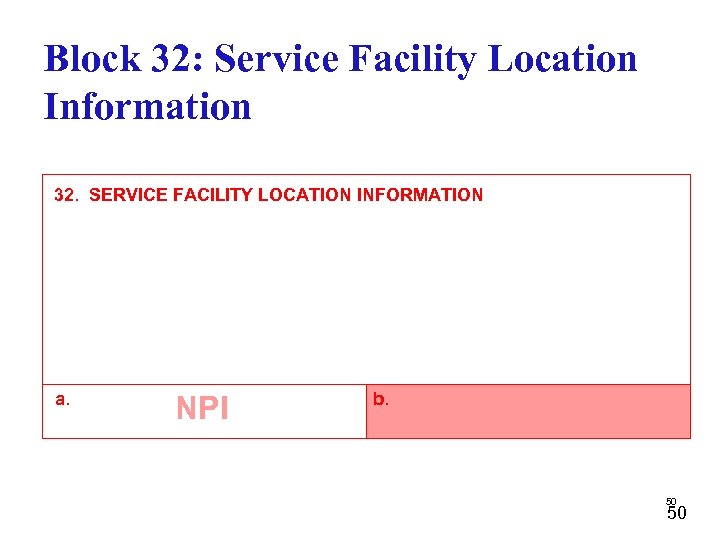
Block 32: Service Facility Location Information 32. SERVICE FACILITY LOCATION INFORMATION a. NPI b. 50 50
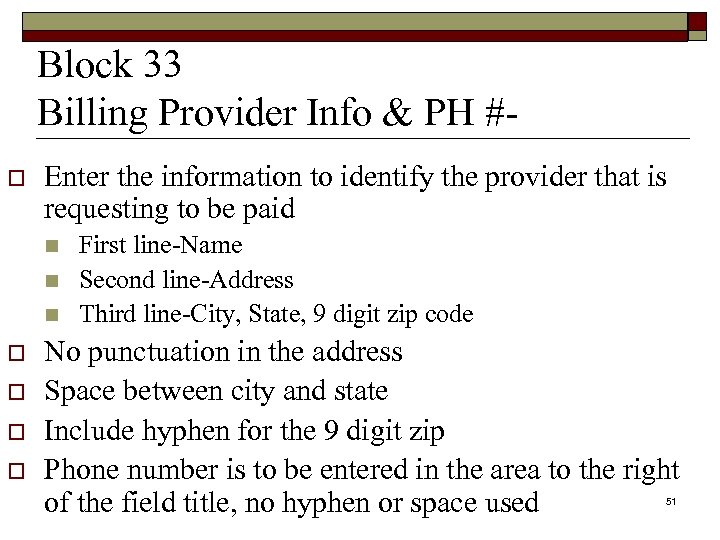
Block 33 Billing Provider Info & PH #o Enter the information to identify the provider that is requesting to be paid n n n o o First line-Name Second line-Address Third line-City, State, 9 digit zip code No punctuation in the address Space between city and state Include hyphen for the 9 digit zip Phone number is to be entered in the area to the right of the field title, no hyphen or space used 51
Billing Provider Info & PH #-Block-33 a-b o o Enter the 10 digit NPI number of the service location in 33 a. OR Enter ‘ 1 D’ qualifier with the API in 33 b. 52
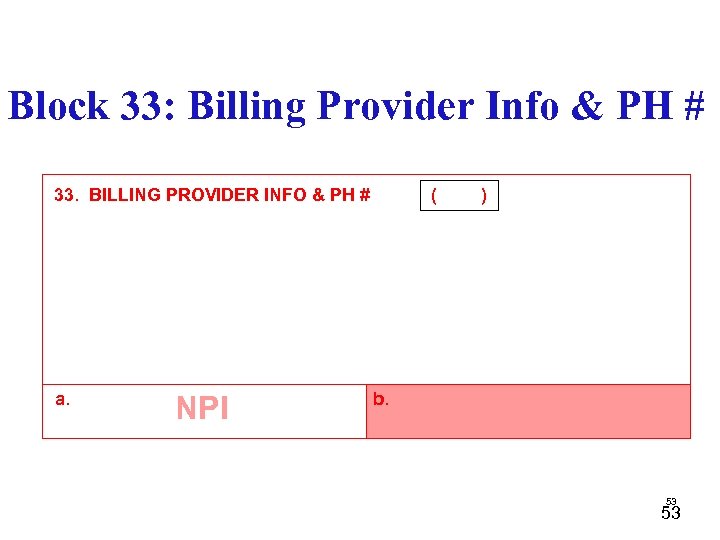
Block 33: Billing Provider Info & PH # 33. BILLING PROVIDER INFO & PH # a. NPI ( ) b. 53 53
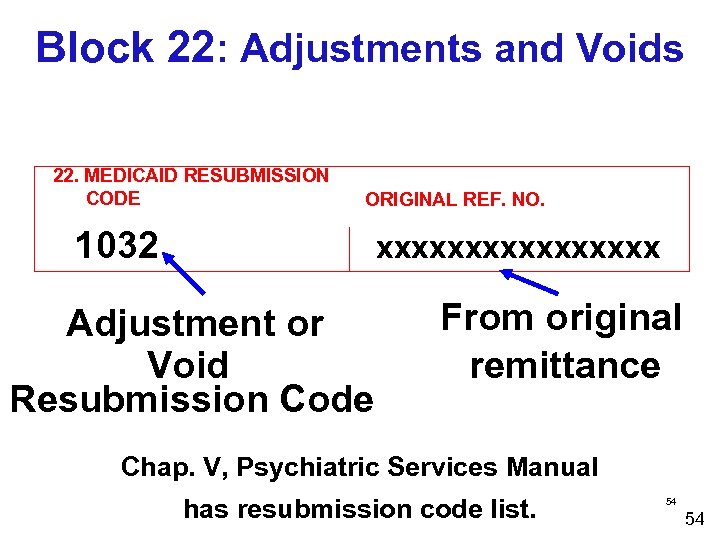
Block 22: Adjustments and Voids 22. MEDICAID RESUBMISSION CODE ORIGINAL REF. NO. 1032 xxxxxxxx Adjustment or Void Resubmission Code From original remittance Chap. V, Psychiatric Services Manual has resubmission code list. 54 54
REMITTANCE VOUCHER Sections of the Voucher 4 APPROVED for payment. 4 PENDING for review of claims. 4 DENIED no payment allowed. 4 DEBIT (+) Adjusted claims creating a positive balance. 4 CREDIT (-) Adjusted/Voided claims creating a negative balance. 55 55
REMITTANCE VOUCHER Sections of the Voucher 4 4 FINANCIAL TRANSACTION EOB DESCRIPTION 4 ADJUSTMENT DESCRIPTION/REMARKS- STATUS DESCRIPTION 4 REMITTANCE SUMMARYPROGRAM TOTALS 56 56
THANK YOU Department of Medical Assistance Services www. dmas. virginia. gov
9c0618daeecd15fdebf7c1c830eb7b5a.ppt