da10fd521fc80bb71fb1e12f238de452.ppt
- Количество слайдов: 17
 Medicaid Coverage Expansion for SUD Services The San Mateo County Experience April 2013
Medicaid Coverage Expansion for SUD Services The San Mateo County Experience April 2013
 Overview n n n Design of LIHP/MCE in SMC Progress in core implementation areas Successes, challenges, lessons Provider Readiness Next Steps
Overview n n n Design of LIHP/MCE in SMC Progress in core implementation areas Successes, challenges, lessons Provider Readiness Next Steps
 What is “MCE” n n n MCE = Medicaid Coverage Expansion Low income health program for adults who have incomes from 0 -133% of the Federal Poverty Level. MCE is a "bridge" program created by the State of California and the federal government for individuals who are expected to qualify for expanded Medicaid benefits in 2014, under the new federal health care reform law.
What is “MCE” n n n MCE = Medicaid Coverage Expansion Low income health program for adults who have incomes from 0 -133% of the Federal Poverty Level. MCE is a "bridge" program created by the State of California and the federal government for individuals who are expected to qualify for expanded Medicaid benefits in 2014, under the new federal health care reform law.
 Covered Substance Use Services* (San Mateo County’s LIHP/MCE Program) n n n n Assessment Behavioral Health Integration Case Management Collateral Services Day Care Rehabilitation Detoxification Group Counseling Individual Counseling Medication Assisted Treatment Narcotic Replacement Therapy (Methadone) Outpatient Treatment Residential Acute Stabilization Residential Perinatal Treatment Residential Treatment Including Detoxification Screening and Intervention *CA Dept of Health Care Services, San Mateo County LIHP Contract, Exhibit A, Attachment 15, 8/18/11
Covered Substance Use Services* (San Mateo County’s LIHP/MCE Program) n n n n Assessment Behavioral Health Integration Case Management Collateral Services Day Care Rehabilitation Detoxification Group Counseling Individual Counseling Medication Assisted Treatment Narcotic Replacement Therapy (Methadone) Outpatient Treatment Residential Acute Stabilization Residential Perinatal Treatment Residential Treatment Including Detoxification Screening and Intervention *CA Dept of Health Care Services, San Mateo County LIHP Contract, Exhibit A, Attachment 15, 8/18/11
 MCE: Year in Review Core Implementation Areas n n n n n Eligibility and Enrollment Medical Necessity Treatment Authorization Treatment Services Service Billing Documentation Managing the Budget Reporting Electronic Health Records Transition
MCE: Year in Review Core Implementation Areas n n n n n Eligibility and Enrollment Medical Necessity Treatment Authorization Treatment Services Service Billing Documentation Managing the Budget Reporting Electronic Health Records Transition
 Eligibility & Enrollment n n n Streamlined health coverage application process for homeless and AOD providers Successful interagency partnership among HPSM, CHA, HCU, BHRS, and AOD Providers FY 11/12 • 385 Clients enrolled via AOD provider sites n n 70% via AOD Provider-HCU Partnership 30% via Palm Detox - BHRS Health Insurance Outreach Program Partnership • Unknown # enrolled by CHAs at county clinics
Eligibility & Enrollment n n n Streamlined health coverage application process for homeless and AOD providers Successful interagency partnership among HPSM, CHA, HCU, BHRS, and AOD Providers FY 11/12 • 385 Clients enrolled via AOD provider sites n n 70% via AOD Provider-HCU Partnership 30% via Palm Detox - BHRS Health Insurance Outreach Program Partnership • Unknown # enrolled by CHAs at county clinics
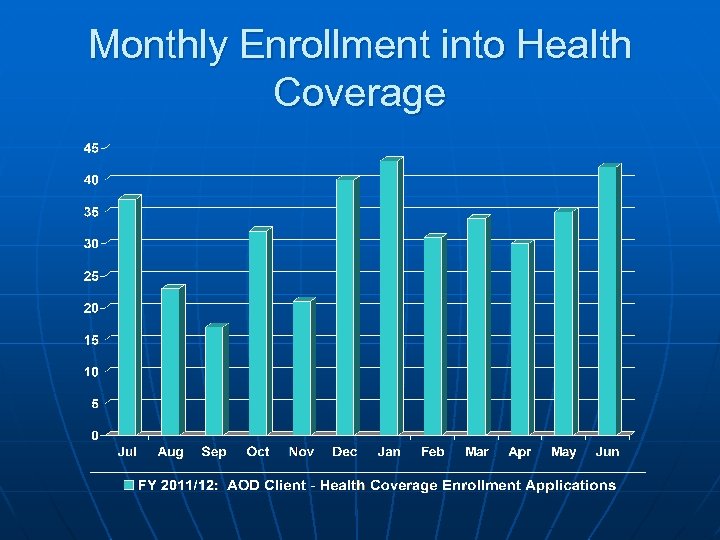 Monthly Enrollment into Health Coverage
Monthly Enrollment into Health Coverage
 Enrollment & Eligibility Challenges and Lessons n n n Transitory nature of population Picture Identification requirements Failure to disclose all income (ie: unemployment) Individuals with benefits in neighboring counties Delayed notification of coverage to providers No automated “back-end” eligibility verification once billing is submitted
Enrollment & Eligibility Challenges and Lessons n n n Transitory nature of population Picture Identification requirements Failure to disclose all income (ie: unemployment) Individuals with benefits in neighboring counties Delayed notification of coverage to providers No automated “back-end” eligibility verification once billing is submitted
 Medical Necessity n n n Developed by team of BHRS, Providers, and clinical experts Informed by ASAM, medical necessity requirements of other health insurers. Provider capacity expansion Diagnosis - staffing implications and recommend language change to diagnostic impression Staff Credentialing Requirements (AOD certified vs licensed)
Medical Necessity n n n Developed by team of BHRS, Providers, and clinical experts Informed by ASAM, medical necessity requirements of other health insurers. Provider capacity expansion Diagnosis - staffing implications and recommend language change to diagnostic impression Staff Credentialing Requirements (AOD certified vs licensed)
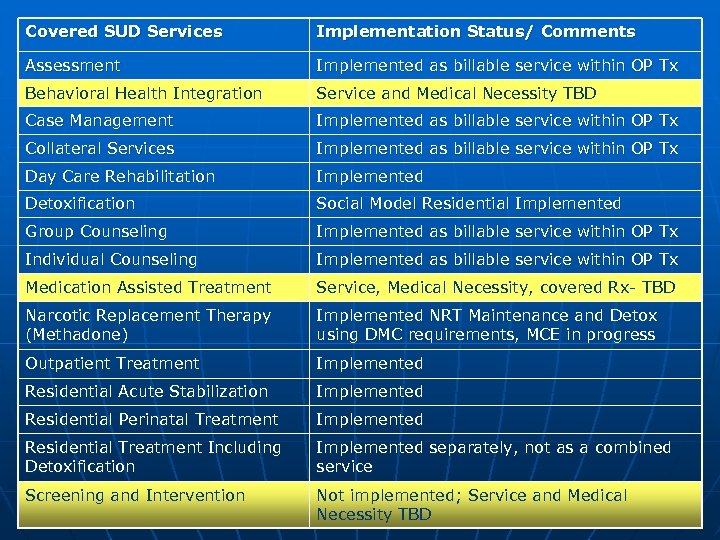 Covered SUD Services Implementation Status/ Comments Assessment Implemented as billable service within OP Tx Behavioral Health Integration Service and Medical Necessity TBD Case Management Implemented as billable service within OP Tx Collateral Services Implemented as billable service within OP Tx Day Care Rehabilitation Implemented Detoxification Social Model Residential Implemented Group Counseling Implemented as billable service within OP Tx Individual Counseling Implemented as billable service within OP Tx Medication Assisted Treatment Service, Medical Necessity, covered Rx- TBD Narcotic Replacement Therapy (Methadone) Implemented NRT Maintenance and Detox using DMC requirements, MCE in progress Outpatient Treatment Implemented Residential Acute Stabilization Implemented Residential Perinatal Treatment Implemented Residential Treatment Including Detoxification Implemented separately, not as a combined service Screening and Intervention Not implemented; Service and Medical Necessity TBD
Covered SUD Services Implementation Status/ Comments Assessment Implemented as billable service within OP Tx Behavioral Health Integration Service and Medical Necessity TBD Case Management Implemented as billable service within OP Tx Collateral Services Implemented as billable service within OP Tx Day Care Rehabilitation Implemented Detoxification Social Model Residential Implemented Group Counseling Implemented as billable service within OP Tx Individual Counseling Implemented as billable service within OP Tx Medication Assisted Treatment Service, Medical Necessity, covered Rx- TBD Narcotic Replacement Therapy (Methadone) Implemented NRT Maintenance and Detox using DMC requirements, MCE in progress Outpatient Treatment Implemented Residential Acute Stabilization Implemented Residential Perinatal Treatment Implemented Residential Treatment Including Detoxification Implemented separately, not as a combined service Screening and Intervention Not implemented; Service and Medical Necessity TBD
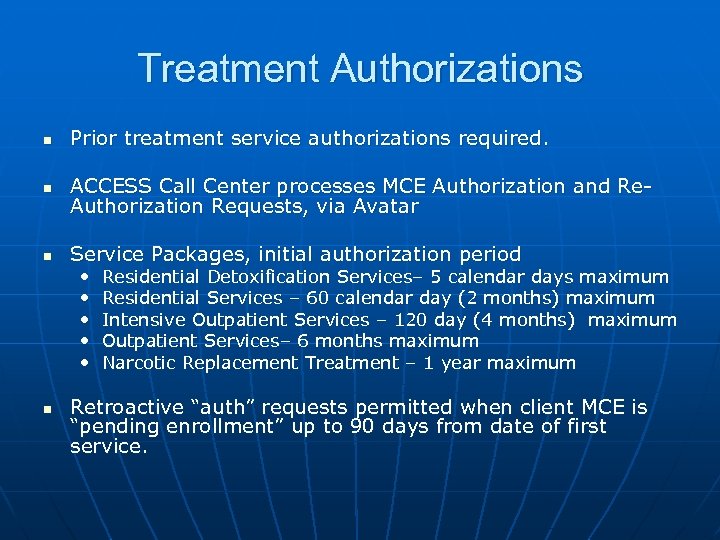 Treatment Authorizations n Prior treatment service authorizations required. n ACCESS Call Center processes MCE Authorization and Re. Authorization Requests, via Avatar n Service Packages, initial authorization period • • • n Residential Detoxification Services– 5 calendar days maximum Residential Services – 60 calendar day (2 months) maximum Intensive Outpatient Services – 120 day (4 months) maximum Outpatient Services– 6 months maximum Narcotic Replacement Treatment – 1 year maximum Retroactive “auth” requests permitted when client MCE is “pending enrollment” up to 90 days from date of first service.
Treatment Authorizations n Prior treatment service authorizations required. n ACCESS Call Center processes MCE Authorization and Re. Authorization Requests, via Avatar n Service Packages, initial authorization period • • • n Residential Detoxification Services– 5 calendar days maximum Residential Services – 60 calendar day (2 months) maximum Intensive Outpatient Services – 120 day (4 months) maximum Outpatient Services– 6 months maximum Narcotic Replacement Treatment – 1 year maximum Retroactive “auth” requests permitted when client MCE is “pending enrollment” up to 90 days from date of first service.
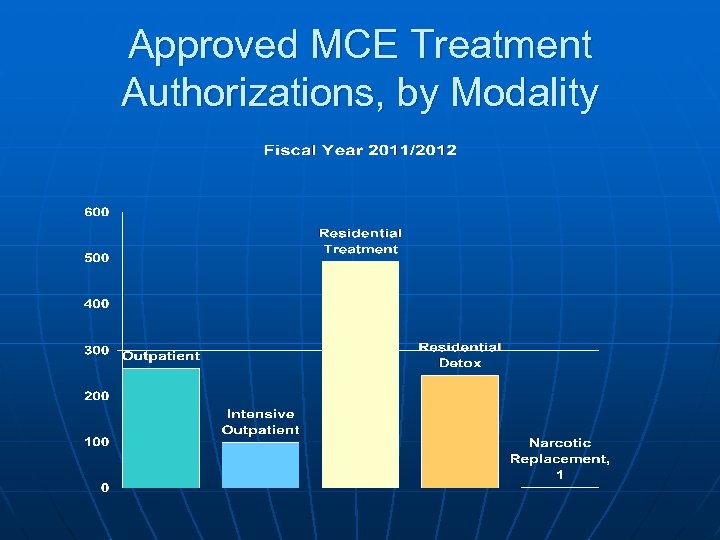 Approved MCE Treatment Authorizations, by Modality
Approved MCE Treatment Authorizations, by Modality
 MCE Service Billing n $2, 894, 627 – FY 11/12 billing total • Represents $1, 447, 313 in new federal funds for SUD treatment in San Mateo County n n Limited provider experience tracking and billing for services by the minute (OP only) Temporary “scantron” was up for billing, until transition to Avatar was completed
MCE Service Billing n $2, 894, 627 – FY 11/12 billing total • Represents $1, 447, 313 in new federal funds for SUD treatment in San Mateo County n n Limited provider experience tracking and billing for services by the minute (OP only) Temporary “scantron” was up for billing, until transition to Avatar was completed
 Medicaid Expansion in 2014 n n The good news…the Supreme Court upheld the Affordable Care Act. In 2014, the estimated 20% of uninsured Californians will be able to obtain health coverage via the Exchange or Medicaid expansion. MCE SUD benefit and provider requirements –still pending State determination CA considering “State” verses “County” option
Medicaid Expansion in 2014 n n The good news…the Supreme Court upheld the Affordable Care Act. In 2014, the estimated 20% of uninsured Californians will be able to obtain health coverage via the Exchange or Medicaid expansion. MCE SUD benefit and provider requirements –still pending State determination CA considering “State” verses “County” option
 SUD Provider Readiness n n n Changing face of partners and referrals sources, from criminal justice to primary care Credentialing of staff – State ADP requirements vs. health insurance requirements (licensing); ability to diagnose. Treatment Program design – care based on individual needs, not on “program design” (ie: 90 day program) Documentation of medical necessity and services Knowledge of billing codes Lack relationships with private insurers, primary care providers.
SUD Provider Readiness n n n Changing face of partners and referrals sources, from criminal justice to primary care Credentialing of staff – State ADP requirements vs. health insurance requirements (licensing); ability to diagnose. Treatment Program design – care based on individual needs, not on “program design” (ie: 90 day program) Documentation of medical necessity and services Knowledge of billing codes Lack relationships with private insurers, primary care providers.
 Next Steps: Primary Care • Navigate the primary care system • Develop relationships • Establish referral & communications protocols (bi-directional) • Provide outreach materials to PCP • Expanding medication assisted treatment • Improve physical and mental health of SUD clients through greater coordination
Next Steps: Primary Care • Navigate the primary care system • Develop relationships • Establish referral & communications protocols (bi-directional) • Provide outreach materials to PCP • Expanding medication assisted treatment • Improve physical and mental health of SUD clients through greater coordination
 Thank you! Clara Boyden SMC Behavioral Health & Recovery Services cboyden@smcgov. org 65 -802 -5101
Thank you! Clara Boyden SMC Behavioral Health & Recovery Services cboyden@smcgov. org 65 -802 -5101


