ffcd9653f64c57bdcd25754a0d081966.ppt
- Количество слайдов: 33
 Maximizing Medications for Good Outcomes Lee H. Stringer, Pharm. D. , BCPS, FASCP, CPE Clinical Pharmacist, Certified Pain Educator Montana Pain Initiative May 30, 2014 Health Care, Education and Research www. billingsclinic. com
Maximizing Medications for Good Outcomes Lee H. Stringer, Pharm. D. , BCPS, FASCP, CPE Clinical Pharmacist, Certified Pain Educator Montana Pain Initiative May 30, 2014 Health Care, Education and Research www. billingsclinic. com
 Conflict of Interest Disclosure Lee H. Stringer, Pharm. D. Has no real or apparent conflicts of interest to report.
Conflict of Interest Disclosure Lee H. Stringer, Pharm. D. Has no real or apparent conflicts of interest to report.
 Objectives 1. Explore principles of rational polypharmacy 2. Learn mechanisms of action of non-opioid and adjuvant analgesics 3. Recognize an appropriate analgesic trial including proper titration
Objectives 1. Explore principles of rational polypharmacy 2. Learn mechanisms of action of non-opioid and adjuvant analgesics 3. Recognize an appropriate analgesic trial including proper titration
 Terminology • Narcotic – A substance that causes narcosis – Heroin, cocaine, methamphetamine • Opioid – A substance that binds to the opioid receptor – Morphine, fentanyl, oxycodone
Terminology • Narcotic – A substance that causes narcosis – Heroin, cocaine, methamphetamine • Opioid – A substance that binds to the opioid receptor – Morphine, fentanyl, oxycodone

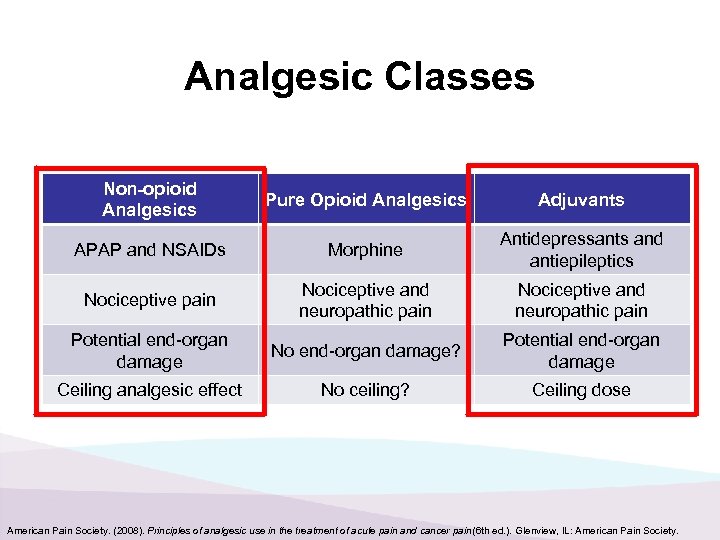 Analgesic Classes Non-opioid Analgesics Pure Opioid Analgesics Adjuvants APAP and NSAIDs Morphine Antidepressants and antiepileptics Nociceptive pain Nociceptive and neuropathic pain Potential end-organ damage No end-organ damage? Potential end-organ damage Ceiling analgesic effect No ceiling? Ceiling dose American Pain Society. (2008). Principles of analgesic use in the treatment of acute pain and cancer pain (6 th ed. ). Glenview, IL: American Pain Society.
Analgesic Classes Non-opioid Analgesics Pure Opioid Analgesics Adjuvants APAP and NSAIDs Morphine Antidepressants and antiepileptics Nociceptive pain Nociceptive and neuropathic pain Potential end-organ damage No end-organ damage? Potential end-organ damage Ceiling analgesic effect No ceiling? Ceiling dose American Pain Society. (2008). Principles of analgesic use in the treatment of acute pain and cancer pain (6 th ed. ). Glenview, IL: American Pain Society.
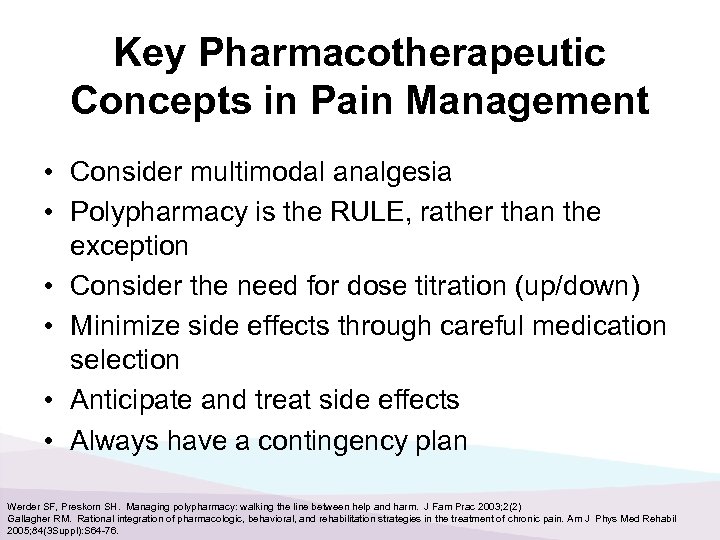 Key Pharmacotherapeutic Concepts in Pain Management • Consider multimodal analgesia • Polypharmacy is the RULE, rather than the exception • Consider the need for dose titration (up/down) • Minimize side effects through careful medication selection • Anticipate and treat side effects • Always have a contingency plan Werder SF, Preskorn SH. Managing polypharmacy: walking the line between help and harm. J Fam Prac 2003; 2(2) Gallagher RM. Rational integration of pharmacologic, behavioral, and rehabilitation strategies in the treatment of chronic pain. Am J Phys Med Rehabil 2005; 84(3 Suppl): S 64 -76.
Key Pharmacotherapeutic Concepts in Pain Management • Consider multimodal analgesia • Polypharmacy is the RULE, rather than the exception • Consider the need for dose titration (up/down) • Minimize side effects through careful medication selection • Anticipate and treat side effects • Always have a contingency plan Werder SF, Preskorn SH. Managing polypharmacy: walking the line between help and harm. J Fam Prac 2003; 2(2) Gallagher RM. Rational integration of pharmacologic, behavioral, and rehabilitation strategies in the treatment of chronic pain. Am J Phys Med Rehabil 2005; 84(3 Suppl): S 64 -76.
 Considerations for Rational Polypharmacy • • • Know drug mechanisms of action Avoid overlapping mechanisms Know drug toxicities Avoid overlapping/additive toxicities Understand drug pharmacokinetics Werder SF, Preskorn SH. Managing polypharmacy: walking the line between help and harm. J Fam Prac 2003; 2(2) Gallagher RM. Rational integration of pharmacologic, behavioral, and rehabilitation strategies in the treatment of chronic pain. Am J Phys Med Rehabil 2005; 84(3 Suppl): S 64 -76.
Considerations for Rational Polypharmacy • • • Know drug mechanisms of action Avoid overlapping mechanisms Know drug toxicities Avoid overlapping/additive toxicities Understand drug pharmacokinetics Werder SF, Preskorn SH. Managing polypharmacy: walking the line between help and harm. J Fam Prac 2003; 2(2) Gallagher RM. Rational integration of pharmacologic, behavioral, and rehabilitation strategies in the treatment of chronic pain. Am J Phys Med Rehabil 2005; 84(3 Suppl): S 64 -76.
 Considerations for Rational Polypharmacy, cont’d • Maximize current regimen • Ensure an appropriate trial is given • Have convincing evidence that combination > monotherapy • Treat “symptom clusters” Werder SF, Preskorn SH. Managing polypharmacy: walking the line between help and harm. J Fam Prac 2003; 2(2) Gallagher RM. Rational integration of pharmacologic, behavioral, and rehabilitation strategies in the treatment of chronic pain. Am J Phys Med Rehabil 2005; 84(3 Suppl): S 64 -76.
Considerations for Rational Polypharmacy, cont’d • Maximize current regimen • Ensure an appropriate trial is given • Have convincing evidence that combination > monotherapy • Treat “symptom clusters” Werder SF, Preskorn SH. Managing polypharmacy: walking the line between help and harm. J Fam Prac 2003; 2(2) Gallagher RM. Rational integration of pharmacologic, behavioral, and rehabilitation strategies in the treatment of chronic pain. Am J Phys Med Rehabil 2005; 84(3 Suppl): S 64 -76.
 Barriers to Rational Polypharmacy • • • Drug-Drug Interactions Drug-Disease Interactions Medication misuse Cost (financial toxicity) Pill burden Werder SF, Preskorn SH. Managing polypharmacy: walking the line between help and harm. J Fam Prac 2003; 2(2) Gallagher RM. Rational integration of pharmacologic, behavioral, and rehabilitation strategies in the treatment of chronic pain. Am J Phys Med Rehabil 2005; 84(3 Suppl): S 64 -76.
Barriers to Rational Polypharmacy • • • Drug-Drug Interactions Drug-Disease Interactions Medication misuse Cost (financial toxicity) Pill burden Werder SF, Preskorn SH. Managing polypharmacy: walking the line between help and harm. J Fam Prac 2003; 2(2) Gallagher RM. Rational integration of pharmacologic, behavioral, and rehabilitation strategies in the treatment of chronic pain. Am J Phys Med Rehabil 2005; 84(3 Suppl): S 64 -76.
 Polypharmacy in Pain Medicine • Goal: achieve optimal pain/function improvement with minimal toxicity – Facilitate use of lower doses of one or more drugs – Maintain efficacy – Synergize effect of two drugs with differing mechanisms of action Fishbain DA. Polypharmacy treatment approaches to the psychiatric and somatic comorbidities found in patients with chronic pain. Am J Phys Med Rehabil. 2005; 84(Suppl 3): S 56 -63.
Polypharmacy in Pain Medicine • Goal: achieve optimal pain/function improvement with minimal toxicity – Facilitate use of lower doses of one or more drugs – Maintain efficacy – Synergize effect of two drugs with differing mechanisms of action Fishbain DA. Polypharmacy treatment approaches to the psychiatric and somatic comorbidities found in patients with chronic pain. Am J Phys Med Rehabil. 2005; 84(Suppl 3): S 56 -63.
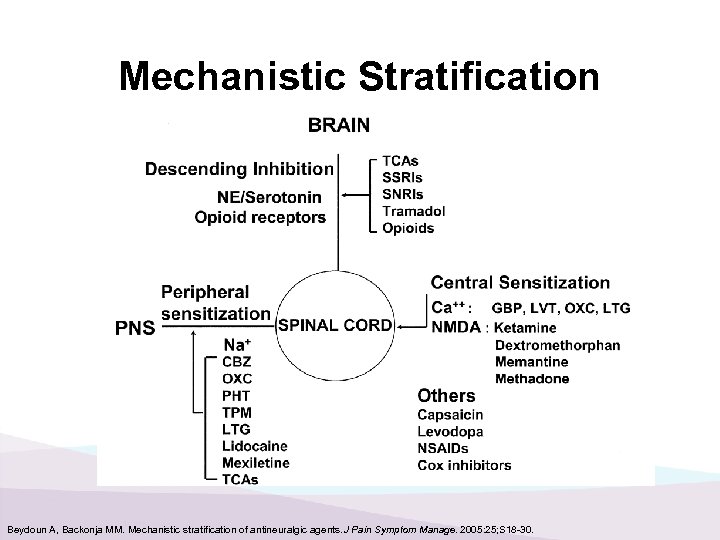 Mechanistic Stratification Beydoun A, Backonja MM. Mechanistic stratification of antineuralgic agents. J Pain Symptom Manage. 2005: 25; S 18 -30.
Mechanistic Stratification Beydoun A, Backonja MM. Mechanistic stratification of antineuralgic agents. J Pain Symptom Manage. 2005: 25; S 18 -30.
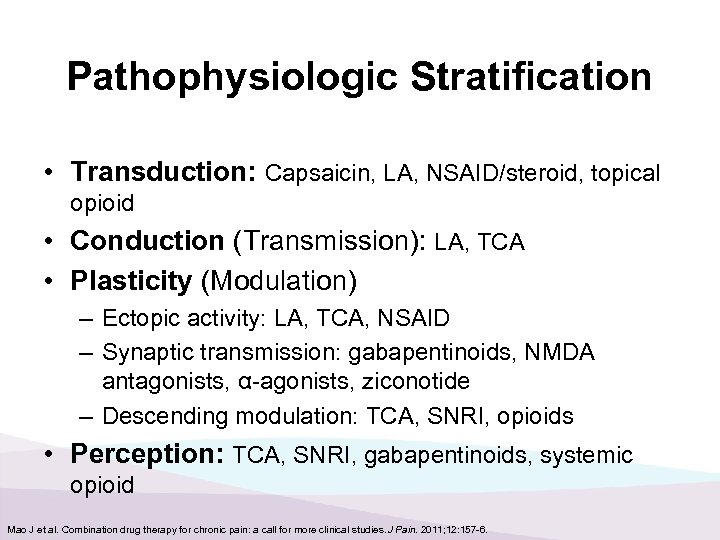 Pathophysiologic Stratification • Transduction: Capsaicin, LA, NSAID/steroid, topical opioid • Conduction (Transmission): LA, TCA • Plasticity (Modulation) – Ectopic activity: LA, TCA, NSAID – Synaptic transmission: gabapentinoids, NMDA antagonists, α-agonists, ziconotide – Descending modulation: TCA, SNRI, opioids • Perception: TCA, SNRI, gabapentinoids, systemic opioid Mao J et al. Combination drug therapy for chronic pain: a call for more clinical studies. J Pain. 2011; 12: 157 -6.
Pathophysiologic Stratification • Transduction: Capsaicin, LA, NSAID/steroid, topical opioid • Conduction (Transmission): LA, TCA • Plasticity (Modulation) – Ectopic activity: LA, TCA, NSAID – Synaptic transmission: gabapentinoids, NMDA antagonists, α-agonists, ziconotide – Descending modulation: TCA, SNRI, opioids • Perception: TCA, SNRI, gabapentinoids, systemic opioid Mao J et al. Combination drug therapy for chronic pain: a call for more clinical studies. J Pain. 2011; 12: 157 -6.
 Non-opioid Analgesics: Acetaminophen
Non-opioid Analgesics: Acetaminophen
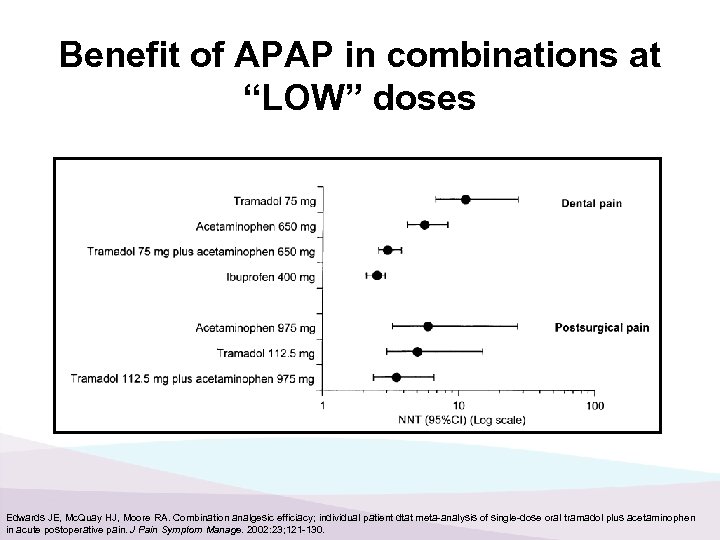 Benefit of APAP in combinations at “LOW” doses Edwards JE, Mc. Quay HJ, Moore RA. Combination analgesic efficiacy; individual patient dtat meta-analysis of single-dose oral tramadol plus acetaminophen in acute postoperative pain. J Pain Symptom Manage. 2002: 23; 121 -130.
Benefit of APAP in combinations at “LOW” doses Edwards JE, Mc. Quay HJ, Moore RA. Combination analgesic efficiacy; individual patient dtat meta-analysis of single-dose oral tramadol plus acetaminophen in acute postoperative pain. J Pain Symptom Manage. 2002: 23; 121 -130.
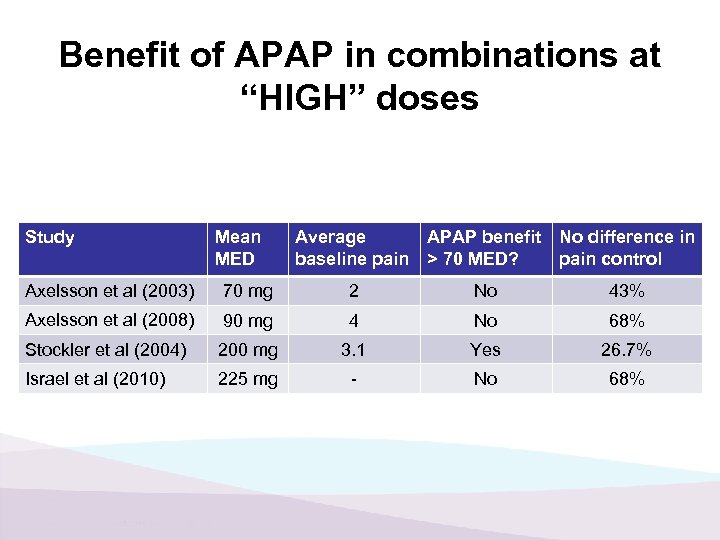 Benefit of APAP in combinations at “HIGH” doses Study Mean MED Average baseline pain APAP benefit > 70 MED? No difference in pain control Axelsson et al (2003) 70 mg 2 No 43% Axelsson et al (2008) 90 mg 4 No 68% Stockler et al (2004) 200 mg 3. 1 Yes 26. 7% Israel et al (2010) 225 mg - No 68%
Benefit of APAP in combinations at “HIGH” doses Study Mean MED Average baseline pain APAP benefit > 70 MED? No difference in pain control Axelsson et al (2003) 70 mg 2 No 43% Axelsson et al (2008) 90 mg 4 No 68% Stockler et al (2004) 200 mg 3. 1 Yes 26. 7% Israel et al (2010) 225 mg - No 68%
 Non-opioid Analgesics: NSAIDs
Non-opioid Analgesics: NSAIDs
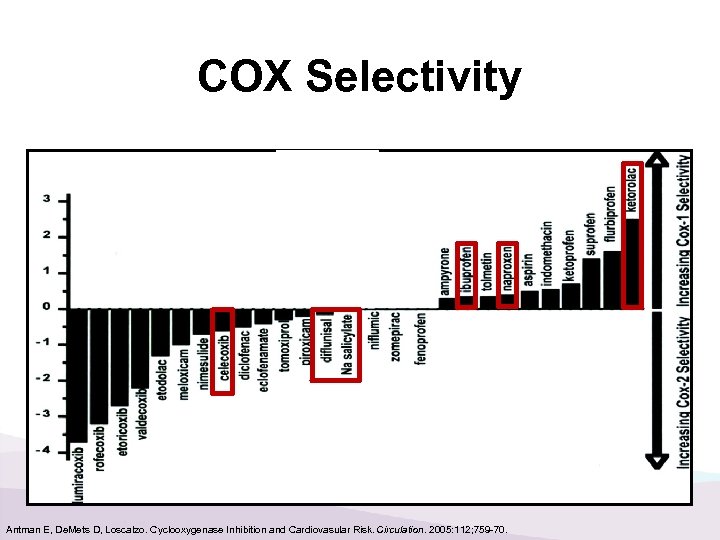 COX Selectivity Antman E, De. Mets D, Loscalzo. Cyclooxygenase Inhibition and Cardiovasular Risk. Circulation. 2005: 112; 759 -70.
COX Selectivity Antman E, De. Mets D, Loscalzo. Cyclooxygenase Inhibition and Cardiovasular Risk. Circulation. 2005: 112; 759 -70.
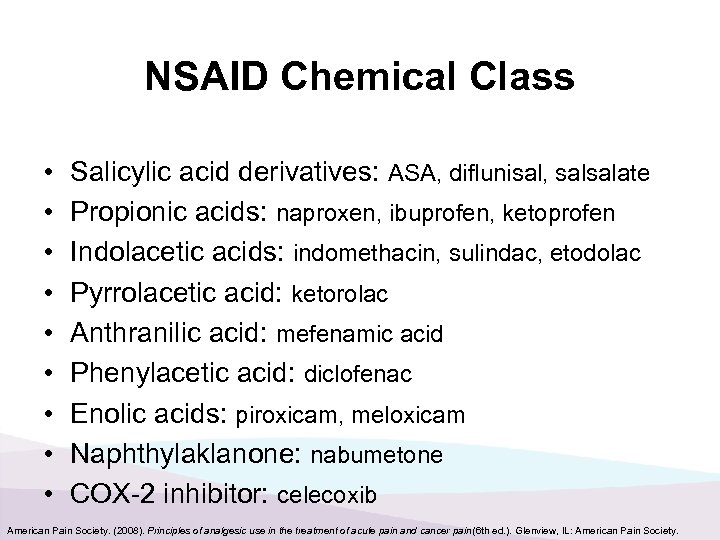 NSAID Chemical Class • • • Salicylic acid derivatives: ASA, diflunisal, salsalate Propionic acids: naproxen, ibuprofen, ketoprofen Indolacetic acids: indomethacin, sulindac, etodolac Pyrrolacetic acid: ketorolac Anthranilic acid: mefenamic acid Phenylacetic acid: diclofenac Enolic acids: piroxicam, meloxicam Naphthylaklanone: nabumetone COX-2 inhibitor: celecoxib American Pain Society. (2008). Principles of analgesic use in the treatment of acute pain and cancer pain (6 th ed. ). Glenview, IL: American Pain Society.
NSAID Chemical Class • • • Salicylic acid derivatives: ASA, diflunisal, salsalate Propionic acids: naproxen, ibuprofen, ketoprofen Indolacetic acids: indomethacin, sulindac, etodolac Pyrrolacetic acid: ketorolac Anthranilic acid: mefenamic acid Phenylacetic acid: diclofenac Enolic acids: piroxicam, meloxicam Naphthylaklanone: nabumetone COX-2 inhibitor: celecoxib American Pain Society. (2008). Principles of analgesic use in the treatment of acute pain and cancer pain (6 th ed. ). Glenview, IL: American Pain Society.
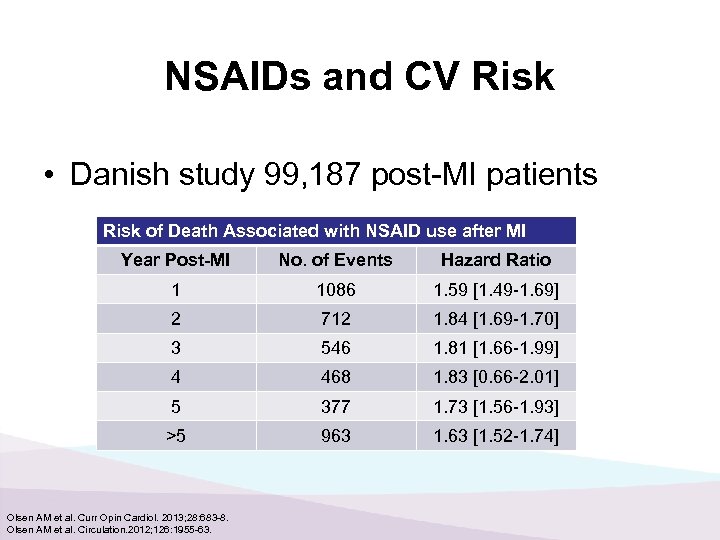 NSAIDs and CV Risk • Danish study 99, 187 post-MI patients Risk of Death Associated with NSAID use after MI Year Post-MI No. of Events Hazard Ratio 1 1086 1. 59 [1. 49 -1. 69] 2 712 1. 84 [1. 69 -1. 70] 3 546 1. 81 [1. 66 -1. 99] 4 468 1. 83 [0. 66 -2. 01] 5 377 1. 73 [1. 56 -1. 93] >5 963 1. 63 [1. 52 -1. 74] Olsen AM et al. Curr Opin Cardiol. 2013; 28: 683 -8. Olsen AM et al. Circulation. 2012; 126: 1955 -63.
NSAIDs and CV Risk • Danish study 99, 187 post-MI patients Risk of Death Associated with NSAID use after MI Year Post-MI No. of Events Hazard Ratio 1 1086 1. 59 [1. 49 -1. 69] 2 712 1. 84 [1. 69 -1. 70] 3 546 1. 81 [1. 66 -1. 99] 4 468 1. 83 [0. 66 -2. 01] 5 377 1. 73 [1. 56 -1. 93] >5 963 1. 63 [1. 52 -1. 74] Olsen AM et al. Curr Opin Cardiol. 2013; 28: 683 -8. Olsen AM et al. Circulation. 2012; 126: 1955 -63.
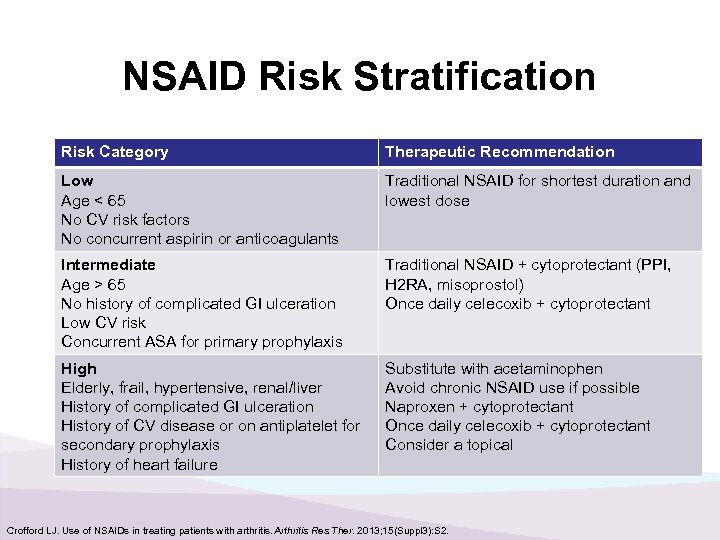 NSAID Risk Stratification Risk Category Therapeutic Recommendation Low Age < 65 No CV risk factors No concurrent aspirin or anticoagulants Traditional NSAID for shortest duration and lowest dose Intermediate Age > 65 No history of complicated GI ulceration Low CV risk Concurrent ASA for primary prophylaxis Traditional NSAID + cytoprotectant (PPI, H 2 RA, misoprostol) Once daily celecoxib + cytoprotectant High Elderly, frail, hypertensive, renal/liver History of complicated GI ulceration History of CV disease or on antiplatelet for secondary prophylaxis History of heart failure Substitute with acetaminophen Avoid chronic NSAID use if possible Naproxen + cytoprotectant Once daily celecoxib + cytoprotectant Consider a topical Crofford LJ. Use of NSAIDs in treating patients with arthritis. Arthritis Res Ther. 2013; 15(Suppl 3): S 2.
NSAID Risk Stratification Risk Category Therapeutic Recommendation Low Age < 65 No CV risk factors No concurrent aspirin or anticoagulants Traditional NSAID for shortest duration and lowest dose Intermediate Age > 65 No history of complicated GI ulceration Low CV risk Concurrent ASA for primary prophylaxis Traditional NSAID + cytoprotectant (PPI, H 2 RA, misoprostol) Once daily celecoxib + cytoprotectant High Elderly, frail, hypertensive, renal/liver History of complicated GI ulceration History of CV disease or on antiplatelet for secondary prophylaxis History of heart failure Substitute with acetaminophen Avoid chronic NSAID use if possible Naproxen + cytoprotectant Once daily celecoxib + cytoprotectant Consider a topical Crofford LJ. Use of NSAIDs in treating patients with arthritis. Arthritis Res Ther. 2013; 15(Suppl 3): S 2.
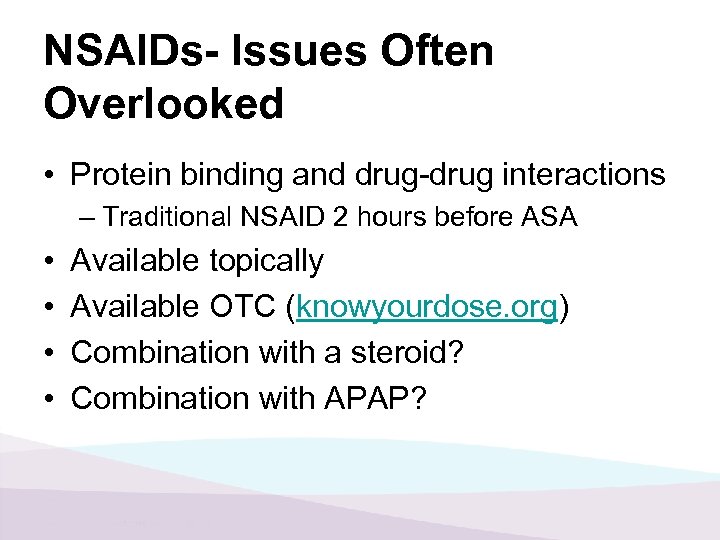 NSAIDs- Issues Often Overlooked • Protein binding and drug-drug interactions – Traditional NSAID 2 hours before ASA • • Available topically Available OTC (knowyourdose. org) Combination with a steroid? Combination with APAP?
NSAIDs- Issues Often Overlooked • Protein binding and drug-drug interactions – Traditional NSAID 2 hours before ASA • • Available topically Available OTC (knowyourdose. org) Combination with a steroid? Combination with APAP?
 Adjuvant Analgesics
Adjuvant Analgesics
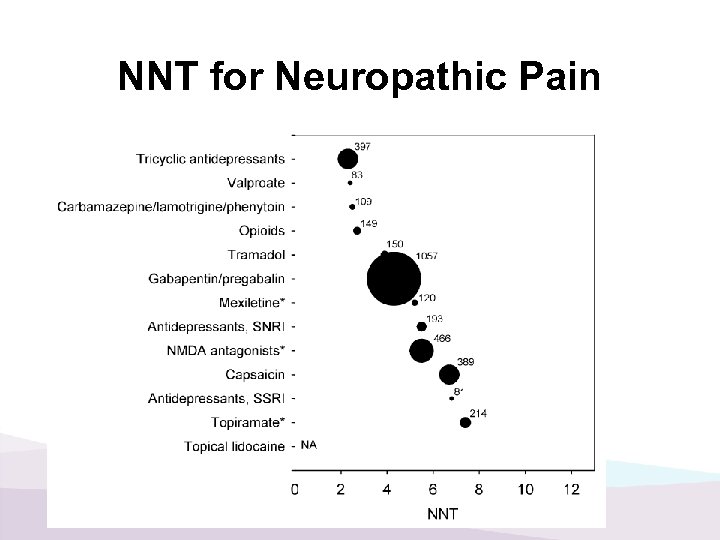 NNT for Neuropathic Pain
NNT for Neuropathic Pain
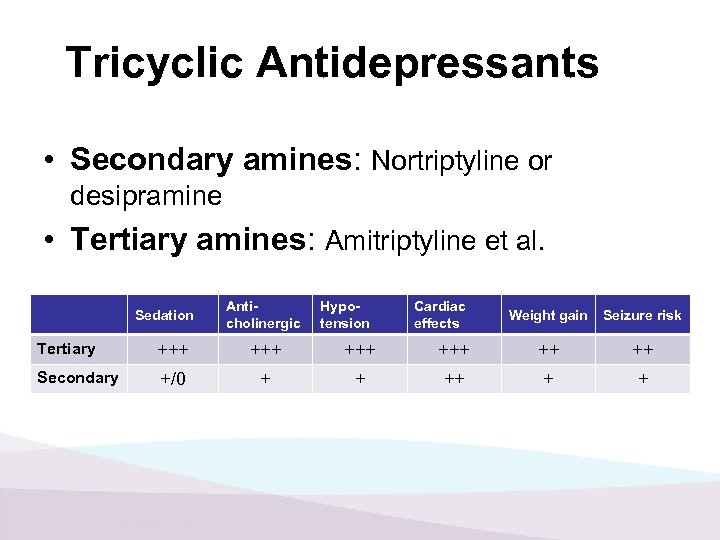 Tricyclic Antidepressants • Secondary amines: Nortriptyline or desipramine • Tertiary amines: Amitriptyline et al. Sedation Anticholinergic Hypotension Cardiac effects Weight gain Seizure risk Tertiary +++ +++ ++ ++ Secondary +/0 + + +
Tricyclic Antidepressants • Secondary amines: Nortriptyline or desipramine • Tertiary amines: Amitriptyline et al. Sedation Anticholinergic Hypotension Cardiac effects Weight gain Seizure risk Tertiary +++ +++ ++ ++ Secondary +/0 + + +
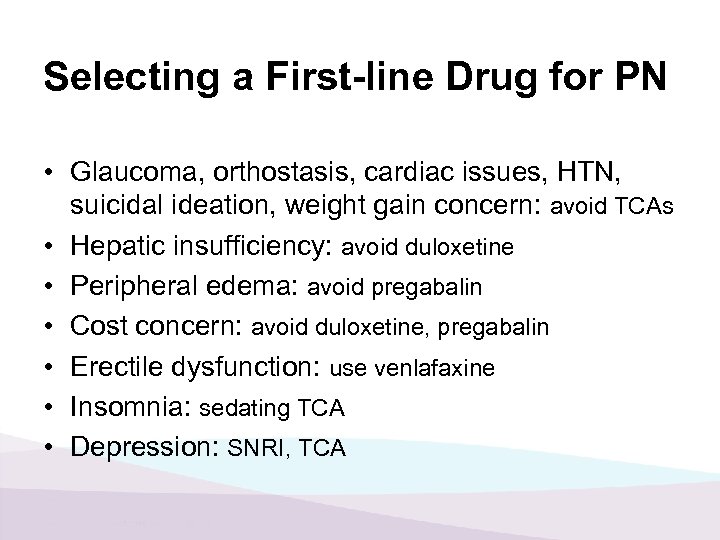 Selecting a First-line Drug for PN • Glaucoma, orthostasis, cardiac issues, HTN, suicidal ideation, weight gain concern: avoid TCAs • Hepatic insufficiency: avoid duloxetine • Peripheral edema: avoid pregabalin • Cost concern: avoid duloxetine, pregabalin • Erectile dysfunction: use venlafaxine • Insomnia: sedating TCA • Depression: SNRI, TCA
Selecting a First-line Drug for PN • Glaucoma, orthostasis, cardiac issues, HTN, suicidal ideation, weight gain concern: avoid TCAs • Hepatic insufficiency: avoid duloxetine • Peripheral edema: avoid pregabalin • Cost concern: avoid duloxetine, pregabalin • Erectile dysfunction: use venlafaxine • Insomnia: sedating TCA • Depression: SNRI, TCA
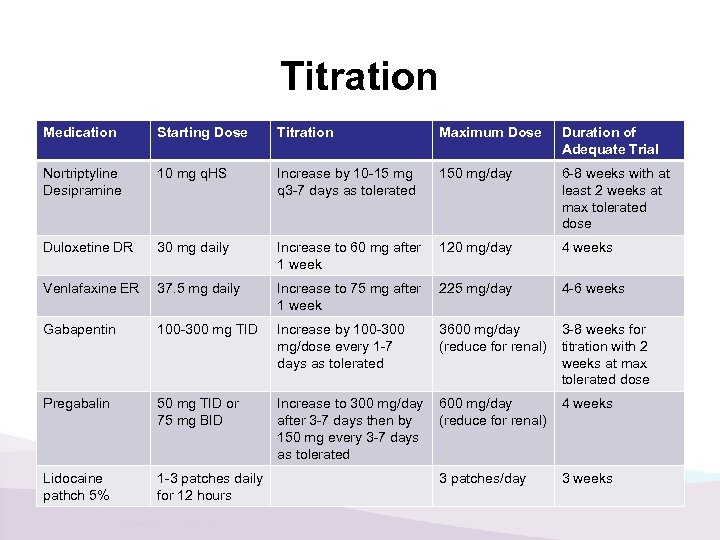 Titration Medication Starting Dose Titration Maximum Dose Duration of Adequate Trial Nortriptyline Desipramine 10 mg q. HS Increase by 10 -15 mg q 3 -7 days as tolerated 150 mg/day 6 -8 weeks with at least 2 weeks at max tolerated dose Duloxetine DR 30 mg daily Increase to 60 mg after 1 week 120 mg/day 4 weeks Venlafaxine ER 37. 5 mg daily Increase to 75 mg after 1 week 225 mg/day 4 -6 weeks Gabapentin 100 -300 mg TID Increase by 100 -300 mg/dose every 1 -7 days as tolerated 3600 mg/day (reduce for renal) 3 -8 weeks for titration with 2 weeks at max tolerated dose Pregabalin 50 mg TID or 75 mg BID Increase to 300 mg/day after 3 -7 days then by 150 mg every 3 -7 days as tolerated 600 mg/day (reduce for renal) 4 weeks Lidocaine pathch 5% 1 -3 patches daily for 12 hours 3 patches/day 3 weeks
Titration Medication Starting Dose Titration Maximum Dose Duration of Adequate Trial Nortriptyline Desipramine 10 mg q. HS Increase by 10 -15 mg q 3 -7 days as tolerated 150 mg/day 6 -8 weeks with at least 2 weeks at max tolerated dose Duloxetine DR 30 mg daily Increase to 60 mg after 1 week 120 mg/day 4 weeks Venlafaxine ER 37. 5 mg daily Increase to 75 mg after 1 week 225 mg/day 4 -6 weeks Gabapentin 100 -300 mg TID Increase by 100 -300 mg/dose every 1 -7 days as tolerated 3600 mg/day (reduce for renal) 3 -8 weeks for titration with 2 weeks at max tolerated dose Pregabalin 50 mg TID or 75 mg BID Increase to 300 mg/day after 3 -7 days then by 150 mg every 3 -7 days as tolerated 600 mg/day (reduce for renal) 4 weeks Lidocaine pathch 5% 1 -3 patches daily for 12 hours 3 patches/day 3 weeks
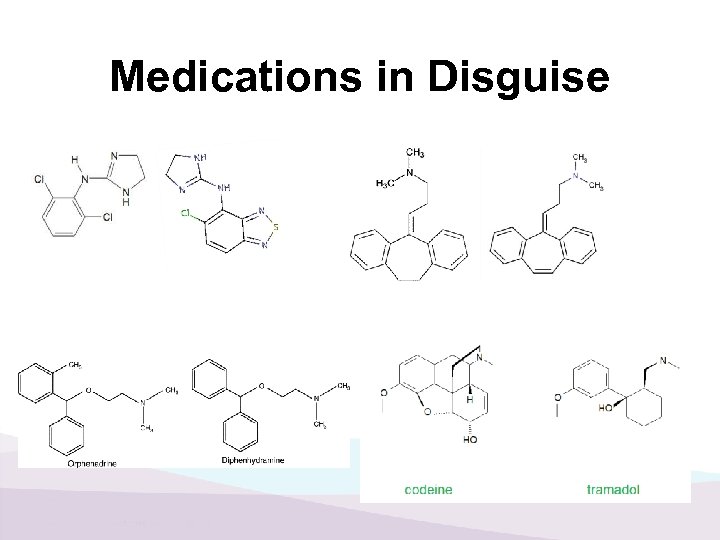 Medications in Disguise
Medications in Disguise
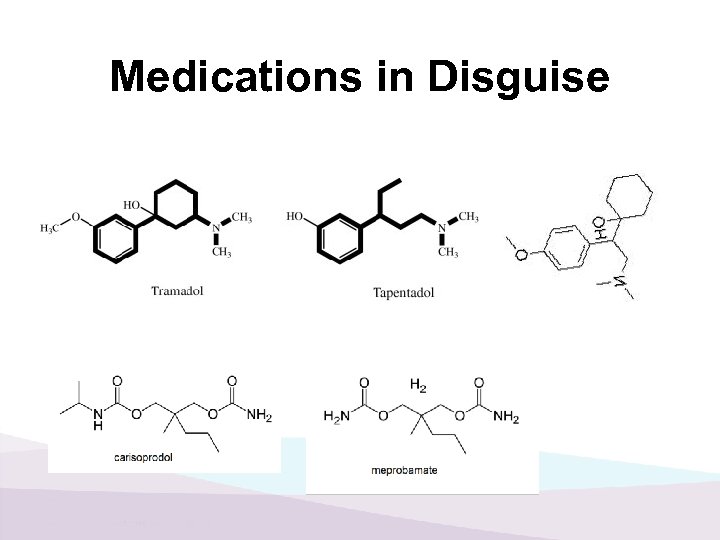 Medications in Disguise
Medications in Disguise
 Conclusions 1. Opioids as the adjuvant 2. Rational polypharmacy is the rule, not the exception 3. Understanding mechanisms of action will facilitate safe and effective polypharmacy 4. Give an appropriate trial and don’t forget to titrate
Conclusions 1. Opioids as the adjuvant 2. Rational polypharmacy is the rule, not the exception 3. Understanding mechanisms of action will facilitate safe and effective polypharmacy 4. Give an appropriate trial and don’t forget to titrate
 QUESTIONS? Lee H. Stringer, Pharm. D. , BCPS, FASCP, CPE 406 -238 -5590 leehallstringer@paineducator. com
QUESTIONS? Lee H. Stringer, Pharm. D. , BCPS, FASCP, CPE 406 -238 -5590 leehallstringer@paineducator. com


