52942071dfb4c8412868631ae0d53576.ppt
- Количество слайдов: 20
 Maternal Outcomes When a Primary Cesarean is the Only Indication for a Repeat Cesarean Jessica A. Taubner, Eugene Declercq, Ph. D, Mary Barger, CNM, MPH, Howard Cabral, Ph. D, MPH, Stephen R. Evans, MPH, Milton Kotelchuck, Ph. D, MPH, Judith Weiss, Sc. D APHA 134 th Annual Meeting Boston, MA ~ November 6, 2006
Maternal Outcomes When a Primary Cesarean is the Only Indication for a Repeat Cesarean Jessica A. Taubner, Eugene Declercq, Ph. D, Mary Barger, CNM, MPH, Howard Cabral, Ph. D, MPH, Stephen R. Evans, MPH, Milton Kotelchuck, Ph. D, MPH, Judith Weiss, Sc. D APHA 134 th Annual Meeting Boston, MA ~ November 6, 2006
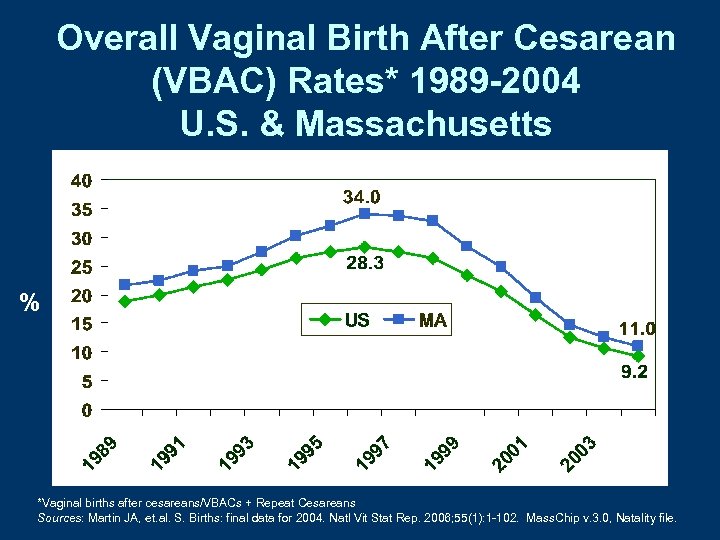 Overall Vaginal Birth After Cesarean (VBAC) Rates* 1989 -2004 U. S. & Massachusetts % *Vaginal births after cesareans/VBACs + Repeat Cesareans Sources: Martin JA, et. al. S. Births: final data for 2004. Natl Vit Stat Rep. 2006; 55(1): 1 -102. Mass. Chip v. 3. 0, Natality file.
Overall Vaginal Birth After Cesarean (VBAC) Rates* 1989 -2004 U. S. & Massachusetts % *Vaginal births after cesareans/VBACs + Repeat Cesareans Sources: Martin JA, et. al. S. Births: final data for 2004. Natl Vit Stat Rep. 2006; 55(1): 1 -102. Mass. Chip v. 3. 0, Natality file.
 Context • Between 1996 -2004, the rate of vaginal birth after cesarean (VBAC) in the U. S. decreased by 67%, while in Massachusetts it decreased by 68%1 • In 1998, 1999, and 2004 ACOG released practice guidelines calling for VBACs to be limited to facilities capable of 24 hour coverage for an emergency cesarean. 2 -4 • As a result, a prior cesarean has become an indication for a repeat cesarean without any other medical indications 1. Martin JA, et. al. S. Births: final data for 2004. Natl Vit Stat Rep. 2006; 55(1): 1 -102. Mass. Chip v. 3. 0, Natality file. 2. ACOG practice bulletin. Vaginal birth after previous cesarean delivery. # 2, 10/98. IJGO. 1999; 64(2): 201 -8 3. ACOG practice bulletin. Vaginal birth after previous cesarean delivery. # 5 7/99 IJGO 1999; 66(2): 197 -204. 4. ACOG Practice Bulletin #54: Vaginal birth after previous cesarean. Obstet Gynecol. 2004 Jul; 104(2): 203 -12.
Context • Between 1996 -2004, the rate of vaginal birth after cesarean (VBAC) in the U. S. decreased by 67%, while in Massachusetts it decreased by 68%1 • In 1998, 1999, and 2004 ACOG released practice guidelines calling for VBACs to be limited to facilities capable of 24 hour coverage for an emergency cesarean. 2 -4 • As a result, a prior cesarean has become an indication for a repeat cesarean without any other medical indications 1. Martin JA, et. al. S. Births: final data for 2004. Natl Vit Stat Rep. 2006; 55(1): 1 -102. Mass. Chip v. 3. 0, Natality file. 2. ACOG practice bulletin. Vaginal birth after previous cesarean delivery. # 2, 10/98. IJGO. 1999; 64(2): 201 -8 3. ACOG practice bulletin. Vaginal birth after previous cesarean delivery. # 5 7/99 IJGO 1999; 66(2): 197 -204. 4. ACOG Practice Bulletin #54: Vaginal birth after previous cesarean. Obstet Gynecol. 2004 Jul; 104(2): 203 -12.
 Objective • No studies to date have examined postpartum or financial outcomes related to repeat cesareans that are not medically indicated • This study analyzes postpartum rehospitalization rates and associated costs for women who had: – A planned repeat cesarean with no other medical indications – A planned VBAC
Objective • No studies to date have examined postpartum or financial outcomes related to repeat cesareans that are not medically indicated • This study analyzes postpartum rehospitalization rates and associated costs for women who had: – A planned repeat cesarean with no other medical indications – A planned VBAC
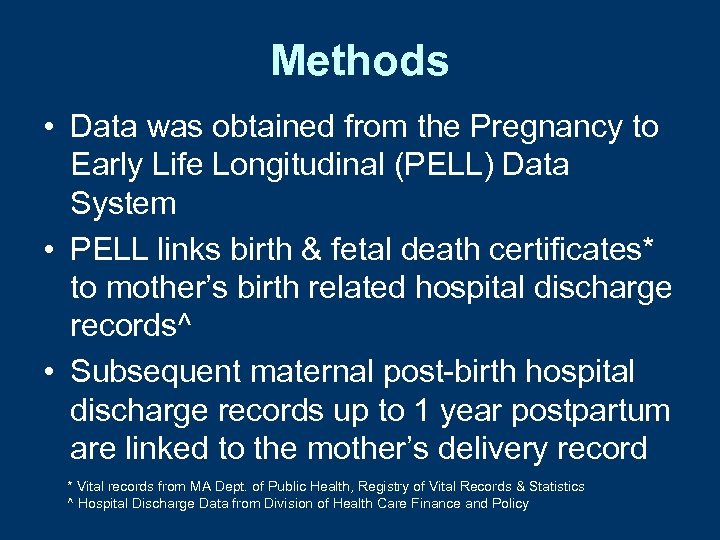 Methods • Data was obtained from the Pregnancy to Early Life Longitudinal (PELL) Data System • PELL links birth & fetal death certificates* to mother’s birth related hospital discharge records^ • Subsequent maternal post-birth hospital discharge records up to 1 year postpartum are linked to the mother’s delivery record * Vital records from MA Dept. of Public Health, Registry of Vital Records & Statistics ^ Hospital Discharge Data from Division of Health Care Finance and Policy
Methods • Data was obtained from the Pregnancy to Early Life Longitudinal (PELL) Data System • PELL links birth & fetal death certificates* to mother’s birth related hospital discharge records^ • Subsequent maternal post-birth hospital discharge records up to 1 year postpartum are linked to the mother’s delivery record * Vital records from MA Dept. of Public Health, Registry of Vital Records & Statistics ^ Hospital Discharge Data from Division of Health Care Finance and Policy
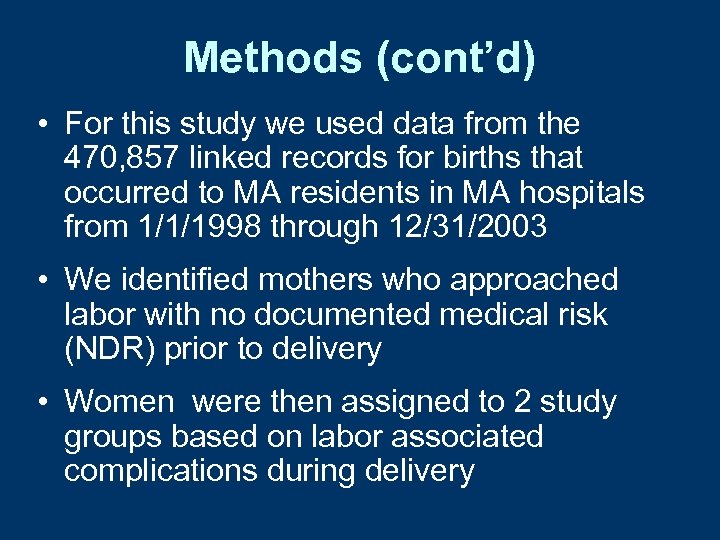 Methods (cont’d) • For this study we used data from the 470, 857 linked records for births that occurred to MA residents in MA hospitals from 1/1/1998 through 12/31/2003 • We identified mothers who approached labor with no documented medical risk (NDR) prior to delivery • Women were then assigned to 2 study groups based on labor associated complications during delivery
Methods (cont’d) • For this study we used data from the 470, 857 linked records for births that occurred to MA residents in MA hospitals from 1/1/1998 through 12/31/2003 • We identified mothers who approached labor with no documented medical risk (NDR) prior to delivery • Women were then assigned to 2 study groups based on labor associated complications during delivery
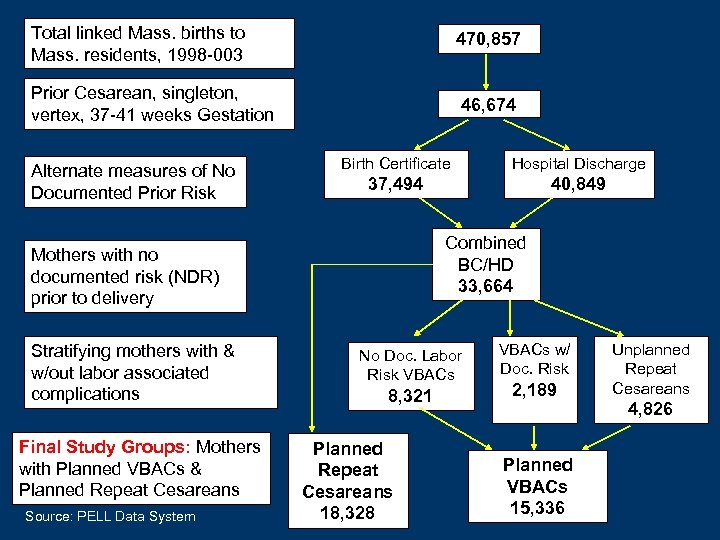 Total linked Mass. births to Mass. residents, 1998 -003 470, 857 Prior Cesarean, singleton, vertex, 37 -41 weeks Gestation 46, 674 Alternate measures of No Documented Prior Risk Birth Certificate Hospital Discharge 37, 494 40, 849 Combined BC/HD 33, 664 Mothers with no documented risk (NDR) prior to delivery Stratifying mothers with & w/out labor associated complications Final Study Groups: Mothers with Planned VBACs & Planned Repeat Cesareans Source: PELL Data System No Doc. Labor Risk VBACs 8, 321 Planned Repeat Cesareans 18, 328 VBACs w/ Doc. Risk 2, 189 Planned VBACs 15, 336 Unplanned Repeat Cesareans 4, 826
Total linked Mass. births to Mass. residents, 1998 -003 470, 857 Prior Cesarean, singleton, vertex, 37 -41 weeks Gestation 46, 674 Alternate measures of No Documented Prior Risk Birth Certificate Hospital Discharge 37, 494 40, 849 Combined BC/HD 33, 664 Mothers with no documented risk (NDR) prior to delivery Stratifying mothers with & w/out labor associated complications Final Study Groups: Mothers with Planned VBACs & Planned Repeat Cesareans Source: PELL Data System No Doc. Labor Risk VBACs 8, 321 Planned Repeat Cesareans 18, 328 VBACs w/ Doc. Risk 2, 189 Planned VBACs 15, 336 Unplanned Repeat Cesareans 4, 826
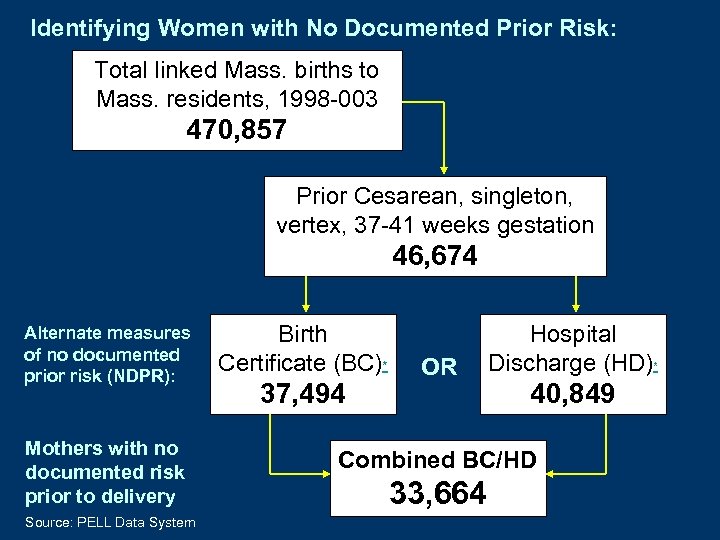 Identifying Women with No Documented Prior Risk: Total linked Mass. births to Mass. residents, 1998 -003 470, 857 Prior Cesarean, singleton, vertex, 37 -41 weeks gestation 46, 674 Alternate measures of no documented prior risk (NDPR): Mothers with no documented risk prior to delivery Source: PELL Data System Birth Certificate (BC)* 37, 494 OR Hospital Discharge (HD)* 40, 849 Combined BC/HD 33, 664
Identifying Women with No Documented Prior Risk: Total linked Mass. births to Mass. residents, 1998 -003 470, 857 Prior Cesarean, singleton, vertex, 37 -41 weeks gestation 46, 674 Alternate measures of no documented prior risk (NDPR): Mothers with no documented risk prior to delivery Source: PELL Data System Birth Certificate (BC)* 37, 494 OR Hospital Discharge (HD)* 40, 849 Combined BC/HD 33, 664
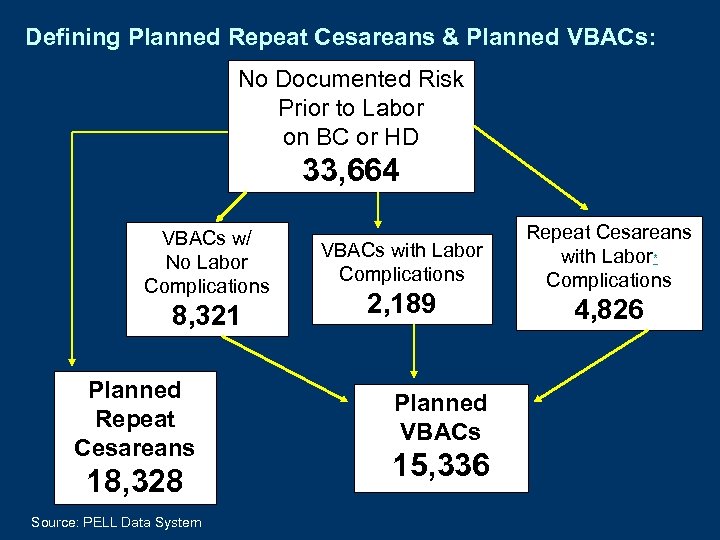 Defining Planned Repeat Cesareans & Planned VBACs: No Documented Risk Prior to Labor on BC or HD 33, 664 VBACs w/ No Labor Complications 8, 321 Planned Repeat Cesareans 18, 328 Source: PELL Data System VBACs with Labor Complications 2, 189 Planned VBACs 15, 336 Repeat Cesareans with Labor* Complications 4, 826
Defining Planned Repeat Cesareans & Planned VBACs: No Documented Risk Prior to Labor on BC or HD 33, 664 VBACs w/ No Labor Complications 8, 321 Planned Repeat Cesareans 18, 328 Source: PELL Data System VBACs with Labor Complications 2, 189 Planned VBACs 15, 336 Repeat Cesareans with Labor* Complications 4, 826
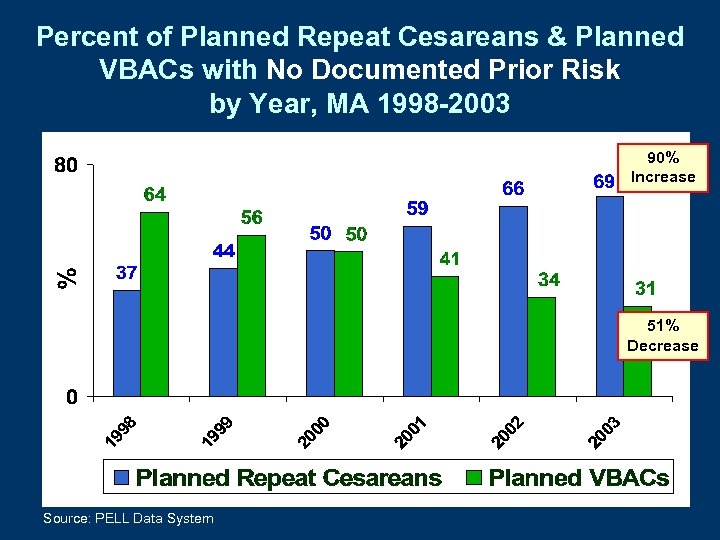 Percent of Planned Repeat Cesareans & Planned VBACs with No Documented Prior Risk by Year, MA 1998 -2003 90% Increase 51% Decrease Source: PELL Data System
Percent of Planned Repeat Cesareans & Planned VBACs with No Documented Prior Risk by Year, MA 1998 -2003 90% Increase 51% Decrease Source: PELL Data System
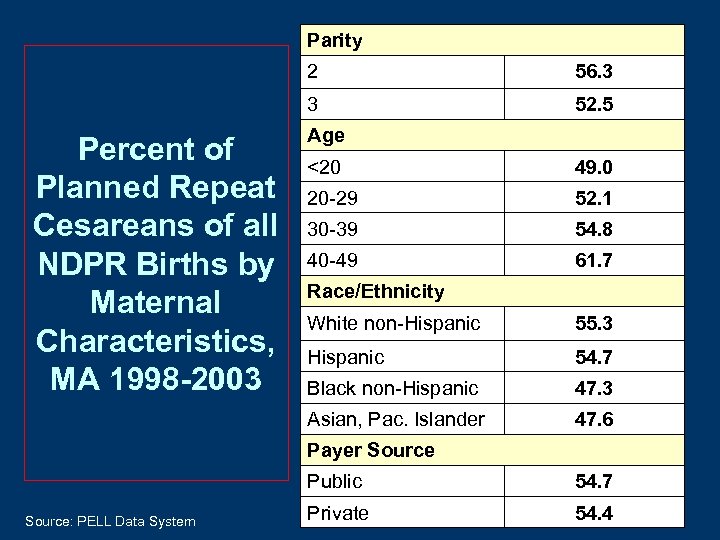 Parity 2 3 Percent of Planned Repeat Cesareans of all NDPR Births by Maternal Characteristics, MA 1998 -2003 56. 3 52. 5 Age <20 49. 0 20 -29 52. 1 30 -39 54. 8 40 -49 61. 7 Race/Ethnicity White non-Hispanic 55. 3 Hispanic 54. 7 Black non-Hispanic 47. 3 Asian, Pac. Islander 47. 6 Payer Source Public Source: PELL Data System 54. 7 Private 54. 4
Parity 2 3 Percent of Planned Repeat Cesareans of all NDPR Births by Maternal Characteristics, MA 1998 -2003 56. 3 52. 5 Age <20 49. 0 20 -29 52. 1 30 -39 54. 8 40 -49 61. 7 Race/Ethnicity White non-Hispanic 55. 3 Hispanic 54. 7 Black non-Hispanic 47. 3 Asian, Pac. Islander 47. 6 Payer Source Public Source: PELL Data System 54. 7 Private 54. 4
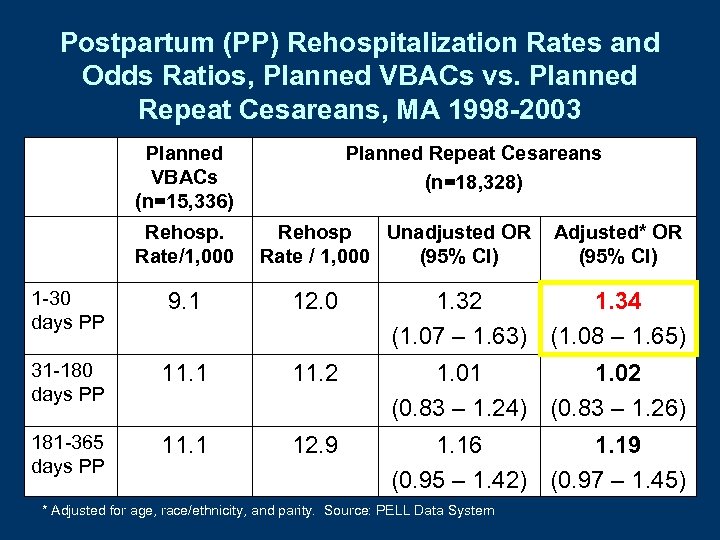 Postpartum (PP) Rehospitalization Rates and Odds Ratios, Planned VBACs vs. Planned Repeat Cesareans, MA 1998 -2003 Planned VBACs (n=15, 336) Rehosp. Rate/1, 000 Planned Repeat Cesareans (n=18, 328) Rehosp Unadjusted OR Rate / 1, 000 (95% CI) Adjusted* OR (95% CI) 1 -30 days PP 9. 1 12. 0 1. 32 1. 34 (1. 07 – 1. 63) (1. 08 – 1. 65) 31 -180 days PP 11. 1 11. 2 1. 01 1. 02 (0. 83 – 1. 24) (0. 83 – 1. 26) 181 -365 days PP 11. 1 12. 9 1. 16 1. 19 (0. 95 – 1. 42) (0. 97 – 1. 45) * Adjusted for age, race/ethnicity, and parity. Source: PELL Data System
Postpartum (PP) Rehospitalization Rates and Odds Ratios, Planned VBACs vs. Planned Repeat Cesareans, MA 1998 -2003 Planned VBACs (n=15, 336) Rehosp. Rate/1, 000 Planned Repeat Cesareans (n=18, 328) Rehosp Unadjusted OR Rate / 1, 000 (95% CI) Adjusted* OR (95% CI) 1 -30 days PP 9. 1 12. 0 1. 32 1. 34 (1. 07 – 1. 63) (1. 08 – 1. 65) 31 -180 days PP 11. 1 11. 2 1. 01 1. 02 (0. 83 – 1. 24) (0. 83 – 1. 26) 181 -365 days PP 11. 1 12. 9 1. 16 1. 19 (0. 95 – 1. 42) (0. 97 – 1. 45) * Adjusted for age, race/ethnicity, and parity. Source: PELL Data System
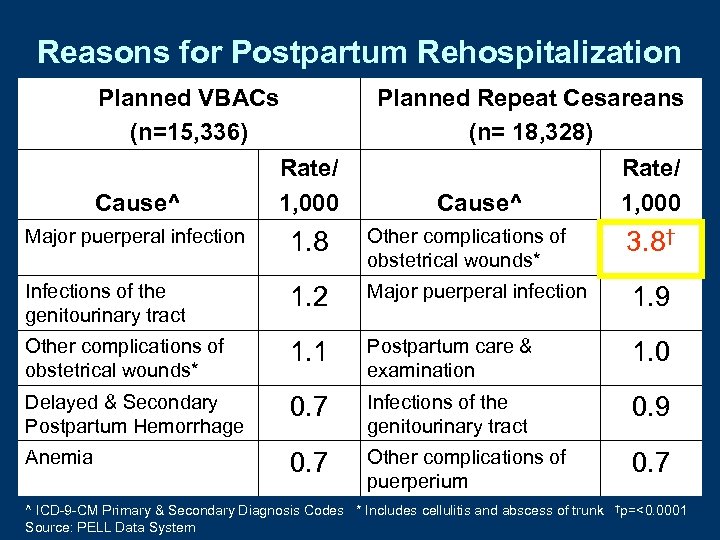 Reasons for Postpartum Rehospitalization Planned VBACs (n=15, 336) Planned Repeat Cesareans (n= 18, 328) Rate/ Cause^ 1, 000 Cause^ Rate/ 1, 000 Major puerperal infection 1. 8 Other complications of obstetrical wounds* 3. 8† Infections of the genitourinary tract 1. 2 Major puerperal infection 1. 9 Other complications of obstetrical wounds* 1. 1 Postpartum care & examination 1. 0 Delayed & Secondary Postpartum Hemorrhage 0. 7 Infections of the genitourinary tract 0. 9 Anemia 0. 7 Other complications of puerperium 0. 7 ^ ICD-9 -CM Primary & Secondary Diagnosis Codes * Includes cellulitis and abscess of trunk Source: PELL Data System †p=<0. 0001
Reasons for Postpartum Rehospitalization Planned VBACs (n=15, 336) Planned Repeat Cesareans (n= 18, 328) Rate/ Cause^ 1, 000 Cause^ Rate/ 1, 000 Major puerperal infection 1. 8 Other complications of obstetrical wounds* 3. 8† Infections of the genitourinary tract 1. 2 Major puerperal infection 1. 9 Other complications of obstetrical wounds* 1. 1 Postpartum care & examination 1. 0 Delayed & Secondary Postpartum Hemorrhage 0. 7 Infections of the genitourinary tract 0. 9 Anemia 0. 7 Other complications of puerperium 0. 7 ^ ICD-9 -CM Primary & Secondary Diagnosis Codes * Includes cellulitis and abscess of trunk Source: PELL Data System †p=<0. 0001
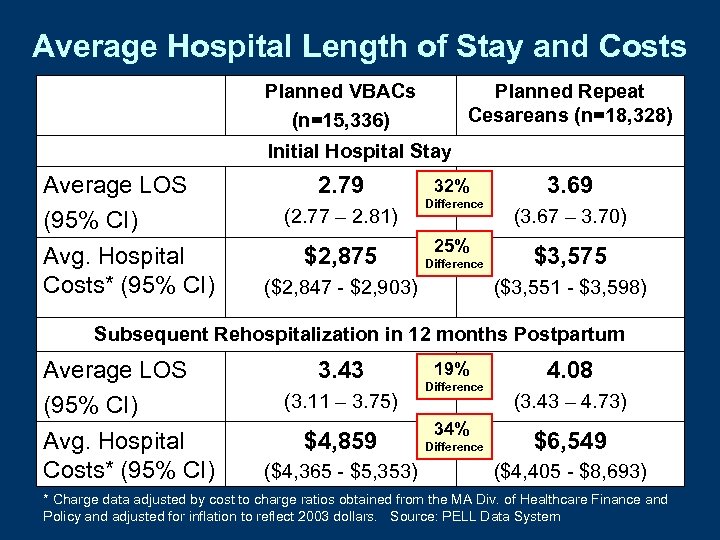 Average Hospital Length of Stay and Costs Planned VBACs (n=15, 336) Planned Repeat Cesareans (n=18, 328) Initial Hospital Stay Average LOS (95% CI) Avg. Hospital Costs* (95% CI) 2. 79 (2. 77 – 2. 81) $2, 875 32% Difference 25% Difference ($2, 847 - $2, 903) 3. 69 (3. 67 – 3. 70) $3, 575 ($3, 551 - $3, 598) Subsequent Rehospitalization in 12 months Postpartum Average LOS (95% CI) Avg. Hospital Costs* (95% CI) 3. 43 (3. 11 – 3. 75) $4, 859 ($4, 365 - $5, 353) 19% Difference 34% Difference 4. 08 (3. 43 – 4. 73) $6, 549 ($4, 405 - $8, 693) * Charge data adjusted by cost to charge ratios obtained from the MA Div. of Healthcare Finance and Policy and adjusted for inflation to reflect 2003 dollars. Source: PELL Data System
Average Hospital Length of Stay and Costs Planned VBACs (n=15, 336) Planned Repeat Cesareans (n=18, 328) Initial Hospital Stay Average LOS (95% CI) Avg. Hospital Costs* (95% CI) 2. 79 (2. 77 – 2. 81) $2, 875 32% Difference 25% Difference ($2, 847 - $2, 903) 3. 69 (3. 67 – 3. 70) $3, 575 ($3, 551 - $3, 598) Subsequent Rehospitalization in 12 months Postpartum Average LOS (95% CI) Avg. Hospital Costs* (95% CI) 3. 43 (3. 11 – 3. 75) $4, 859 ($4, 365 - $5, 353) 19% Difference 34% Difference 4. 08 (3. 43 – 4. 73) $6, 549 ($4, 405 - $8, 693) * Charge data adjusted by cost to charge ratios obtained from the MA Div. of Healthcare Finance and Policy and adjusted for inflation to reflect 2003 dollars. Source: PELL Data System
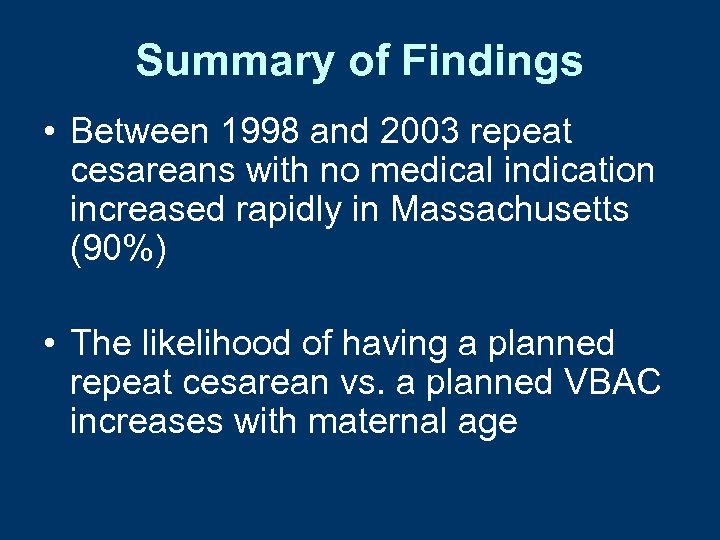 Summary of Findings • Between 1998 and 2003 repeat cesareans with no medical indication increased rapidly in Massachusetts (90%) • The likelihood of having a planned repeat cesarean vs. a planned VBAC increases with maternal age
Summary of Findings • Between 1998 and 2003 repeat cesareans with no medical indication increased rapidly in Massachusetts (90%) • The likelihood of having a planned repeat cesarean vs. a planned VBAC increases with maternal age
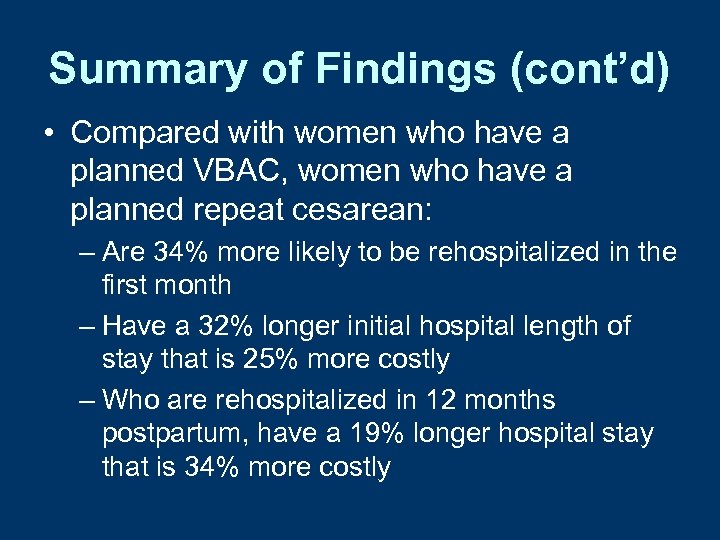 Summary of Findings (cont’d) • Compared with women who have a planned VBAC, women who have a planned repeat cesarean: – Are 34% more likely to be rehospitalized in the first month – Have a 32% longer initial hospital length of stay that is 25% more costly – Who are rehospitalized in 12 months postpartum, have a 19% longer hospital stay that is 34% more costly
Summary of Findings (cont’d) • Compared with women who have a planned VBAC, women who have a planned repeat cesarean: – Are 34% more likely to be rehospitalized in the first month – Have a 32% longer initial hospital length of stay that is 25% more costly – Who are rehospitalized in 12 months postpartum, have a 19% longer hospital stay that is 34% more costly
 Conclusions • Obstetric providers, policy makers, and women should consider the benefits and risks of both repeat cesareans and VBACs
Conclusions • Obstetric providers, policy makers, and women should consider the benefits and risks of both repeat cesareans and VBACs
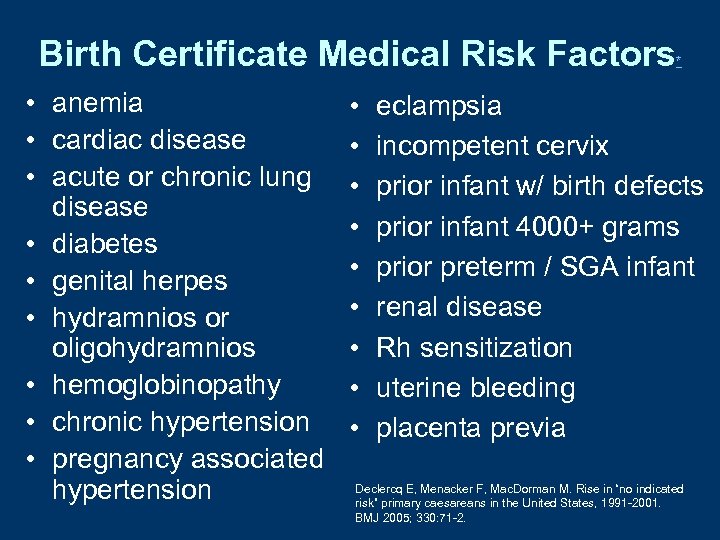 Birth Certificate Medical Risk Factors • anemia • cardiac disease • acute or chronic lung disease • diabetes • genital herpes • hydramnios or oligohydramnios • hemoglobinopathy • chronic hypertension • pregnancy associated hypertension • • • * eclampsia incompetent cervix prior infant w/ birth defects prior infant 4000+ grams prior preterm / SGA infant renal disease Rh sensitization uterine bleeding placenta previa Declercq E, Menacker F, Mac. Dorman M. Rise in “no indicated risk” primary caesareans in the United States, 1991 -2001. BMJ 2005; 330: 71 -2.
Birth Certificate Medical Risk Factors • anemia • cardiac disease • acute or chronic lung disease • diabetes • genital herpes • hydramnios or oligohydramnios • hemoglobinopathy • chronic hypertension • pregnancy associated hypertension • • • * eclampsia incompetent cervix prior infant w/ birth defects prior infant 4000+ grams prior preterm / SGA infant renal disease Rh sensitization uterine bleeding placenta previa Declercq E, Menacker F, Mac. Dorman M. Rise in “no indicated risk” primary caesareans in the United States, 1991 -2001. BMJ 2005; 330: 71 -2.
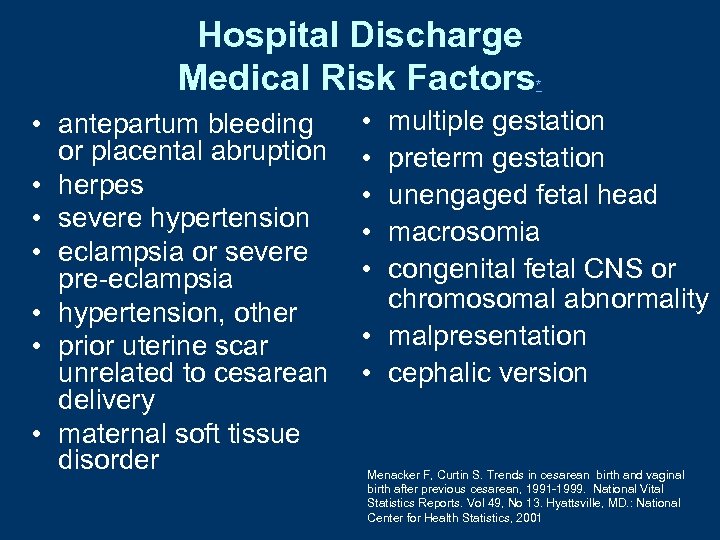 Hospital Discharge Medical Risk Factors • antepartum bleeding or placental abruption • herpes • severe hypertension • eclampsia or severe pre-eclampsia • hypertension, other • prior uterine scar unrelated to cesarean delivery • maternal soft tissue disorder * • • • multiple gestation preterm gestation unengaged fetal head macrosomia congenital fetal CNS or chromosomal abnormality • malpresentation • cephalic version Menacker F, Curtin S. Trends in cesarean birth and vaginal birth after previous cesarean, 1991 -1999. National Vital Statistics Reports. Vol 49, No 13. Hyattsville, MD. : National Center for Health Statistics, 2001
Hospital Discharge Medical Risk Factors • antepartum bleeding or placental abruption • herpes • severe hypertension • eclampsia or severe pre-eclampsia • hypertension, other • prior uterine scar unrelated to cesarean delivery • maternal soft tissue disorder * • • • multiple gestation preterm gestation unengaged fetal head macrosomia congenital fetal CNS or chromosomal abnormality • malpresentation • cephalic version Menacker F, Curtin S. Trends in cesarean birth and vaginal birth after previous cesarean, 1991 -1999. National Vital Statistics Reports. Vol 49, No 13. Hyattsville, MD. : National Center for Health Statistics, 2001
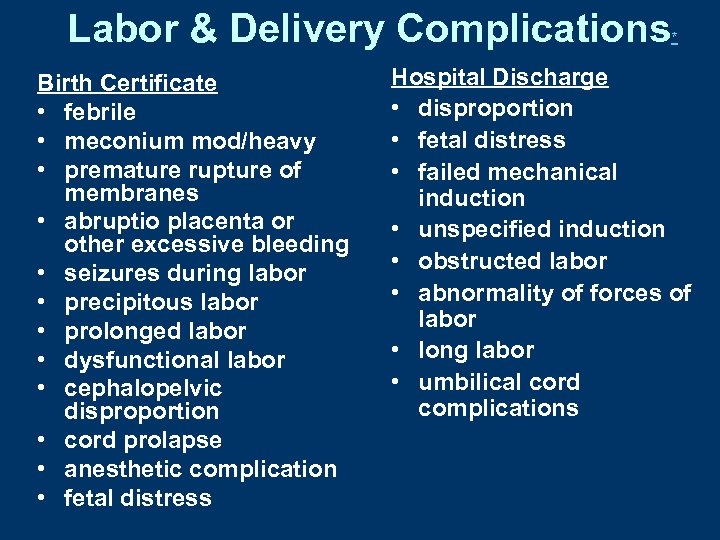 Labor & Delivery Complications Birth Certificate • febrile • meconium mod/heavy • premature rupture of membranes • abruptio placenta or other excessive bleeding • seizures during labor • precipitous labor • prolonged labor • dysfunctional labor • cephalopelvic disproportion • cord prolapse • anesthetic complication • fetal distress * Hospital Discharge • disproportion • fetal distress • failed mechanical induction • unspecified induction • obstructed labor • abnormality of forces of labor • long labor • umbilical cord complications
Labor & Delivery Complications Birth Certificate • febrile • meconium mod/heavy • premature rupture of membranes • abruptio placenta or other excessive bleeding • seizures during labor • precipitous labor • prolonged labor • dysfunctional labor • cephalopelvic disproportion • cord prolapse • anesthetic complication • fetal distress * Hospital Discharge • disproportion • fetal distress • failed mechanical induction • unspecified induction • obstructed labor • abnormality of forces of labor • long labor • umbilical cord complications


