cee5e5600b24007fb6a4a6e82d186507.ppt
- Количество слайдов: 43
Many Ways to be Safe: Training Providers to Recognize Torture and Aid Survivors Lucia Roncalli, MD, MPH, ABIHM Diversity Rx: Quality Health Care, Cultural Diversity 11 March 2013
Disclosures Nothing to declare
BACKGROUND • Climate change, globalization, and changing patterns of conflict have resulted in violent displacement for millions; ~80, 000/year seek asylum in the U. S. • Asylum seekers have higher probability of having survived torture • One effect: changes in the composition of patient populations presenting for primary care in the U. S. • 6 -12% of foreign-born patients presenting for care in urban outpatient clinics are survivors of torture. – Rates are much higher among some subgroups; up to 89% • Many more have survived political violence and other severe human rights violations • • • Crosby, S. , et al. (2006). Prevalence of torture survivors among foreign-born patients presenting to an urban ambulatory care practice. J Gen Intern Med. 2006 July; 21(7): 764– 768 Eisenman DP, Keller AS, Kim G. Survivors of torture in a general medical setting: how often have patients been tortured, and how often is it missed? West J Med. 2000; 172: 301– 4 Eisenman, D. , et al. (2003). Mental health and health-related quality of life among adult Latino primary care patients living in the United States with previous exposure to political violence. JAMA August 6 2003; 290(5).
CLINICAL NEED • There as many survivors of torture in the U. S. as there are persons with Parkinson’s disease, or with polycystic kidney disease. • There are more survivors of torture in the U. S. than persons with multiple sclerosis. • Doctors receive training in Parkinson’s, PKD and M. S. , but not in human rights law or in health effects of human rights violations. • 67 -78% of survivors haven’t told their doctors what they have been through. • 74% express desire to do so, but fear it may be inappropriate or irrelevant. • Very few physicians ask: 0 -3%. • Care is compromised. • • Miles SH, Garcia-Peltoniemi RE. Torture survivors: what to ask, how to document. J Fam Pract. 2012; 61: E 1– 5. Eisenman (2000). Crosby (2006) Shannon, P. , et al. (undated). Refugees’ perspectives on barriers to communication about trauma histories in primary care. Center for Victims of Torture 4
CLINICAL NEED • In addition to high rates of somatization, survivors have – Significant physical disability (17% in one study; p< 0. 0001 in another) – Many syndromes that are culturally important even if not recognized by western diagnostics and nosology – High rates of somatization: emotional distress expressed as physical symptoms; refractory to usual care Hexom, B. , et al. (2012). Survivors of torture: prevalence in an urban emergency department. ACADEMIC EMERGENCY MEDICINE 2012; 19: 1158– 1165 5
CLINICAL NEED: PSYCHOLOGICAL – Psychological sequelae: • PTSD: 25 -48% point prevalence, up to 60% lifetime – Most studies find significant dose-response relationship – Severity dose-response is also significant • Depression: 31%; co-morbidity with PTSD is common • Anxiety: 31% • Increased rates of familial violence, substance abuse, self-harm • Many complex post-migration stressors • • Fazel, M. , et al. (2007). Prevalence of serious mental disorder in 7000 refugees resettled in western countries: a systematic review. Lancet 2005; 365: 1309– 14 Hollifield, M. (2009). The range of symptoms in refugees of war: New Mexico refugee symptom checklist NMRSCL-121. J Nerv Ment Dis 2009; 197. Tamblyn JM, Calderon AJ, Combs S, O’Brien MM. Patients from abroad becoming patients in everyday practice: torture survivors in primary care. J Immigr Minor Health. 2011; 13: 798– 801 Hooberman, J. , et al. (2007). Classifying the torture experiences of refugees living in the United States. J. Interpersonal Viol 22(1)January 2007 1 -16.
PHYSICIAN IGNORANCE ABOUT HEALTH, HUMAN RIGHTS: CONSEQUENCES • When physicians don’t know to ask about human rights violations, they may waste resources on expensive testing and futile treatment • They may miss important diagnoses • They don’t know to refer appropriately • They may increase their patients’ suffering and isolation – Interpersonally – By insensitivity to routine clinic elements that are triggers for traumatized survivors – By missing opportunities to teach about the relation of extreme stress to physical and psychological illness – By missing opportunities to normalize survivors’ reactions, and reassure them that they are not “broken forever. ” 7
ADDITIONAL CONSEQUENCES OF PHYSICIAN HHR IGNORANCE • Doctors who are not educated in health and human rights are more likely to participate in rights violations • U. S. medical students, including those with military training, are ignorant about human rights law and international humanitarian law – 34%: unable to state when required to disobey orders – 24% disagreed with a blanket prohibition on torture – 22% think it acceptable for physicians to examine people for torture to begin or continue • U. S. physicians and psychologists at Guantanamo: “Without the health professionals, the system would come to a grinding halt. ” • • • Boyd, J. , et al. (2007). U. S. medical students’ knowledge about the military draft, the Geneva Conventions, and military medical ethics. International Journal of Health Services, Volume 37, Number 4, Pages 643– 650, 2007. Bean, J. , et al. (2008). Medical students’ attitudes toward torture. TORTURE vol 18, November 2, 2008. Deborah Popowski, Harvard Center for Law and Human Rights, in DOCTORS OF THE DARK SIDE 8
Med school and residency curricula should include health and human rights training • 1996: educators widely acknowledged the need for such training – yet only 17% of U. S. medical schools included training relevant to immigrant/international issues in their curricula. • 2009: educators still acknowledge the need for such training – 32% of med schools offered HHR education. – Public medical schools less likely to offer than private schools. – – – Sonis, J. , et al. (1996) Teaching of human rights in US medical schools. JAMA. 1996 Nov 27; 276(20): 1676 -8 Cotter, L. E. , et al. (2009, 18 March). Health and Human Rights Education in U. S. Schools of Medicine and Public Health: Current Status and Future Challenges. Iacopino, V. (2002). Teaching Human Rights in Graduate Education. 9
Provider education is “primary prevention” for rights violations – Exposure and documentation lessen violation rates; PCP’s are ideally suited to do this – HHR education makes providers more likely to support and understand fulfillment of human rights as a crucial social determinant of health – HHR education makes providers more likely to initiate and support rights-based programming • HHR: health and human rights
HHR Core competencies • KNOWLEDGE – Of international and national human rights laws – Of common sequelae of rights violations – How to treat, when to refer – How to respond to rights violations – Recognizing dual loyalty situations • SKILLS – Ability to do these things! • ATTITUDE – Willingness to do these things! And to support colleagues who speak out – – London, L. , et al. (2007): Developing health rights competencies for S African health professionals. S. Africa Med J December 2007, Vol. 97, No. 12 Tarantola, D. , Gruskin, S. (2006). Health and human rights education in academic settings. Health and Human Rights 2006, 9: 2 (297 -300). 11
Elements of successful programs • Mixed elective and compulsory elements – Offer certificates for those who electively complete more than the minimum requirements • Inspiring, committed faculty seen as role models • Administrative and collegial support • Adequate protected time for learning • Longitudinal, iterative curriculum • Local application • Culture of wider community 12
Successful pedagogy is varied • Variety of teaching modalities – Lecture, films, journaling, interviews, etc • Opportunities for immersion experiences • Application to local circumstances • Variety in evaluation: – Faculty evaluate students – Students evaluate faculty, courses – “ 360” evaluations from patients and staff – South Africa: need long-range evaluation of graduates’ impact – – – London (2007) Iacopino (2002) Tarantola, D. , Gruskin, S. (2006). Health and human rights education in academic settings. Health and Human Rights 2006, 9: 2 (297 -300). 13
Does this training make a difference? • Ramin Asgarry, Bronx Human Rights Clinic • After training, residents are: – able to identify clinic patients who have high odds of having been tortured, or of suffering torture sequelae – more likely correctly to recognize human rights obligations that inhere in their roles as physicians [p < 0. 01], – more likely to know the most common sequelae of torture [p < 0. 0001], – more likely correctly to apply PTSD criteria during evaluation[p < 0. 0001]. – Changes persist 1 year after graduation – Asgary, R. , et al. (2006). Evaluating asylum seekers/ torture survivors in urban primary care: a collaborative approach at the Bronx Human Rights Clinic. Health and Human Rights 9: 2 (2006). 14
One model: Santa Rosa Family Medicine Residency longitudinal HHR curriculum • First year – 12 dedicated teaching hours. Approaches to human suffering: HHR, liberation medicine/ Paul Farmer, social medicine. • What is health? Is it a right? What is a right? – UN documents, treaty bodies. Geneva Conventions * signatories’ responsibilities to “Respect, Protect, Fulfill” * Progressive realization * Derogable vs non-derogable rights – Case Studies/films: farmworkers in Sonoma County • Labor contractors and human trafficking; response of the local wine industry • Pesticide exposure • Free trade agreements, collapse of subsistence agriculture in rural Mexico. California industrial agriculture. -- Feedback/evaluation 15
SRFMR curriculum years 2 -3: asylum evaluation training • Collaboration with HR organizations, immigration law offices • 3 sessions – 1. didactic desk overview, subsequent evaluation – 2. shadowing experienced evaluator – 3. doing own interview and affidavit, with faculty support • • • Iacopino (2002) Weinstein, H. , et al. (1996). Torture and war trauma survivors in primary care practice. West J Med 1996; 165: 112 -118. Levine, P. (2004). Waking the Tiger: Healing trauma. 16
“Istanbul Protocol” • Aka: Manual on the Effective Investigation and Documentation of Torture and Other Cruel, Inhuman or Degrading Treatment or Punishment. • Collaborative effort of 75 forensic and medical professionals (Turkey, 1996) • Formally accepted by the Office of the UN High Commissioner on Human Rights in 2001, now is the international standard of care for evaluation of survivors • PHR manual expands sections of particular relevance to US physicians and mental health professionals • • PHR: Physicians for Human Rights www. physiciansforhumanrights. org
Significance of obtaining asylum • Secure escape from peril, pain, death – For applicants and also, often, for families • • • Possibility of reunion w/ family members Legal permission to work in US Opportunity to rebuild lives Access to health care for torture sequelae Vindication of moral outrage, and legitimation and documentation of suffering
Odds of obtaining asylum with/without professional testimony • Without medical professional testimony, chances of obtaining asylum in the U. S. are around 23% [or worse] • With health care professional testimony, chances of being granted asylum jump to over 90%
Vicarious trauma, Vicarious Resilience • Providers who work with torture survivors risk symptoms that are worse than garden-variety burn-out, closer to PTSD. • They also report life-enriching awareness catalyzed by the work • Odds of vicarious resilience can be maximized by emotional support of learners, teaching specific skills for uncovering resiliency, and giving a cognitive framework for understanding trauma. • • Hernandez, P. , et al. Vicarious resilience: a new concept in work with those who survive trauma. Family Process 2007 Jun; 46(2): 229 -41. Pross, C. , Burnout, vicarious traumatization, and its prevention. TORTURE (16)1, 2006.
Maximizing Resiliency: Peter A. Levine’s trauma framework • Based on animal behavior and evolutionary neuroscience • Humans possess innate resiliency and ability to overcome trauma • “Trauma is in the nervous system, not in the event. ” • When threat is perceived, humans are biologically programmed to respond defensively • Fight/flight: – Engages the sympathetic nervous system [SNS] – High O 2 consumption – Neurally patterned defensive motor responses to threat vary by species – – Levine, P. (1976). Accumulated stress, reserve capacity, and disease. Levine, P. (2004) 21
Freeze: when fight/flight fails • Under inescapable threat, when fight/flight fails FREEZE – Eg “playing possum” • “Tonic immobility” occurs at maximal SNS activation, is involuntary maximal parasympathetic over-ride – Simultaneous SNS “accelerator” and PNS “brake” • Evolutionary advantages – Predators lose interest [programmed to avoid carrion] – Buys time; prey may have escape opportunity – Endogenous opiate surge, near-death anesthesia • Social shame and guilt – “Why didn’t I fight back? Defend myself/loved ones? ” – “She must have wanted that rape. ” – – – Levine (1976) Bados, A. , et al. (2008). Traumatic events and tonic immobility. The Spanish Journal of Psychology 2008, Vol. 11, No. 2, 516 -521. Schauer, M. , Elbert, T. (2010). Dissociation following traumatic stress: etiology and treatment. Zeitschrift fu¨ r Psychologie / Journal of Psychology 2010; Vol. 218(2): 109– 127. 22
Case in point… The cheetah and the impala
Emergence from freeze • Can be instantaneous, back to SNS defensive responses to predator threat • In safe environment, seemingly disorganized movement, respiration, vocalization, is essential to successful negotiation of stress response – Game wardens: without this, animals die – Seen in slow-motion, are classic fight/flight movements • • Hoagland, H, On the Mechanism of Tonic Immobility in Vertebrates. J. General Physiology, Vol 11, 715 -741, 1928 Cannon, W. B. "Voodoo" death. Psychosom. Med. 19: 182 -190, 1957. Richter, C. P. On the phenomenon of sudden death in animals and man. Psychosom. c Med. 19: 191 -198, 1957. Hofer, M. A. Cardiac respiratory function during sudden prolonged immobility in wild rodents Psychosom. Med. 32: 24 633 -647, 1970
Autonomic re-regulation • Happens spontaneously in the wild – tremor, seemingly disorganized movement, diaphoresis, deep breathing, vocalization
Social Overlay: “Get hold of yourself!” • Social and cultural responses often shortcircuit emergence from freeze, so people are stuck half in, half out – Depression, concentration difficulties, psychomotor retardation • Incomplete SNS responses create panic syndromes and hypervigilant PTSD phenomena • • Levine (2004) Schauer (2010)
Levine’s approach to healing trauma: Somatic Experiencing • “Trauma is incomplete defensive response. ” • Trauma is resolved when defensive response is completed: – slowly, with cortical awareness of physical sensation – in a controlled supportive environment – with trained facilitation • …triggers innate healing responses and sense of exhilaration, mastery, well-being. 27
Levine’s Somatic Experiencing® and derivatives • = Emerging best practice, successfully used in – natural disasters [Katrina, Kobe, Haiti, Indonesian and Japanese tsunamis] – among the chronically vulnerable [India, Israel, S. Africa] – complex humanitarian emergencies [Congo, Rwanda] – U. S. war veterans/ Do. D – – – Leitch, et al. (2009). Somatic experiencing treatment with social service workers following hurricanes Rita and Katrina. Social Work vol. 54(1). Miller-Karas, E. (undated). The Trauma Resiliency Model: Guidelines for Working in Disaster Zones. Selvam, R. (2005). Treating tsunami survivors for trauma: The effectiveness of a short-term psycho-physiological trauma treatment approach among South Asian tsunami survivors. Journal of holistic healthcare. Vol 2: (4) November 2005.
Levine’s approach and asylum evaluations • Applying for asylum: visibility, vulnerability, high-stakes poker without clear rules. Activates PTSD, depression, panic • Evaluation interview is intrinsically antitherapeutic: • Survivors relive worst experiences of their lives, with strangers. • They demonstrate and recount classic threat responses, along with guilt and shame about these • Heightened risk of dissociating in court, and being discredited, deported 29
What Levine’s work contributes to asylum evaluations • Cognitive framework to understand physical reactions is easy to teach; many asylum applicants were rural, lived with animals • Unobtrusive interventions from Levine’s approach ameliorate distress – Survivor symptoms often diminish – Quality of life is enhanced – Survivors are at less risk of dissociating in court
Examples: SE® principles applied to an asylum evaluation • “Orienting is soothing. ” • An animal that has scanned the environment and found it to be safe is in a parasympathetic-dominant state. • Windows! Sky! • We orient applicants – To who we are – To what we do, and who will see the documents – To what the interview will/won’t cover – To their right to refuse ANY request we have for information or physical examination – To our understanding of trauma and memory • Lapses don’t discredit them in our eyes • Lies are unnecessary and useless
SE® and asylum: more examples • “A healthy nervous system can swing between trauma and pleasure. ” • Use the “psychosocial baseline” requirement to uncover sources of pleasure, relationship, competence, spirituality– and draw on these later, when horror must be recounted. • Enact scenarios/draw first on implicit, somatic memory, rather than verbal, declarative memory
Case study • Young African gay man, targeted by family, neighbors, school, police, thugs • Multiple incidents of atrocity necessary to recount for court • “Magnetic pull of the trauma vortex” • Freeze, recovery, initiated connection with female evaluator, enhanced well-being lasting through hearing; no dissociation on stand.
Case study • 23 year old female, outspoken for minority freedoms in former USSR republic • Detained, abused by police • Never told her husband of her experiences • Frequent nightmares. • Per husband, “could have gone psychotic” when recounting events to lawyer • Per husband, nightmares gone after asylum evaluation using SE® principles and skills-- even before asylum granted.
What Levine’s work contributes to student providers • Residents can learn the basics • Having a cognitive framework + practical skills when confronted with massive trauma protects against “secondary traumatization” and burnout. • Skills generalize to general clinic patients. • Uncovering the innate resiliency we all possess is exciting! And intrinsically rewarding. • Skills also generalize to provider self-care
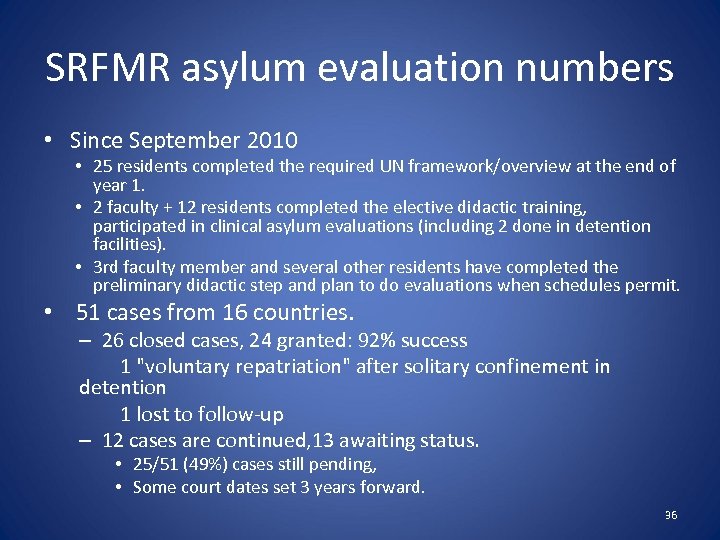
SRFMR asylum evaluation numbers • Since September 2010 • 25 residents completed the required UN framework/overview at the end of year 1. • 2 faculty + 12 residents completed the elective didactic training, participated in clinical asylum evaluations (including 2 done in detention facilities). • 3 rd faculty member and several other residents have completed the preliminary didactic step and plan to do evaluations when schedules permit. • 51 cases from 16 countries. – 26 closed cases, 24 granted: 92% success 1 "voluntary repatriation" after solitary confinement in detention 1 lost to follow-up – 12 cases are continued, 13 awaiting status. • 25/51 (49%) cases still pending, • Some court dates set 3 years forward. 36
Rewards: facilitating the new life that now is possible • Lucia, • • S was granted asylum this afternoon. She was of course overjoyed and immediately started dreaming about this new life which is about to start for her. We are looking forward to celebrating with you soon! •
Rewards: overcoming profiling • Hi Dr. Roncalli, I just wanted to let you know that G's asylum application was approved today. Most Sikh cases get denied by the Asylum Officers and referred to the Immigration Judge, so that is very exciting news. Your report strongly supported his claim so I wanted to thank you again for your great work. • I hope I get to work with you again in the near future. • Happy New Year! • Best wishes,
Rewards: educating the court • • • Hello Lucia, Good news!! D was awarded asylum 11/10, and P also. I couldn't wait to get back to the office to tell you, so I hope that my voice mail message of 10/10 got to you. A million thanks for your help. It was essential in many ways. I will admit that it was not until I read the first draft of your report that I truly understood the extent of D’s sufferings; and this despite the fact that I thought I knew how to detect a “shutdown” victim. But I was somewhat fooled by D’s remarkable composure and self-control. We learn every day, and I won’t forget that particular lesson. . After the interview on 10/27, I feared that the officer would consider all this no more than the actions of a rogue cop, and not rising to the level of “persecution” (or possibly not motivated by anti-Russian or antidemocratic motivations but just by brutish viciousness, and therefore not covered by the statute); so these two weeks were tense, and of course even more so for D and P. You would have been so happy to see the relief and sheer joy on their faces when, after a 3 -hour wait, we got the results on Monday! It is a bright new chapter in their young lives that now opens up. Best regards,
Rewards: intrinsic • • hii dr. Lucia how you doing. . this is g. s just want you to let you know that my case is approved. Thanks for your time and kindneess that you gave to me. beacuse of your help i can move my life forward now . . can fullfill the desire that i had another thanks for your cookies and apple that u gave it to me . i ate'm on my way back they were testy. . . thanks again G. S T
Rounding out the curriculum: survivor care over time • Occasionally, survivors opt to return to clinic for their primary care, with the evaluator as their PMD. • Residents may also participate in an ongoing mental health group for survivors of the Cambodian genocide… • … and in work with their second-generation children • Peter Levine’s approach is carried through these components as well.
HHR curriculum evaluations • Have been piecemeal, collected after post-graduate year 1 overview, and again after didactic asylum training. • In process of adapting Asgarry’s questionnaire to our curriculum. – Standard content – Trauma biology – Personal/attitudinal change • S. Africa: what difference are our graduates making in health and human rights after they graduate? 42
QED • Physician HHR education is urgently needed • Santa Rosa HHR curriculum contains many ingredients found to be associated with success • Adds Peter Levine’s framework re trauma and resolution – Benefits survivors – Offsets provider risk of burnout, secondary traumatization – Generalizes to clinic and hospital encounters with underserved • Used as recruiting “hook, ” some residents come to the program specifically for the HHR curriculum • Needs further work on student, program evaluation • Designed to scale up, be portable to other residencies 43
cee5e5600b24007fb6a4a6e82d186507.ppt