150bd6bbabe4775ee43aacf974db4c8d.ppt
- Количество слайдов: 44
 Managing the “Other” Patient in Long-Term Care: Skills for Working with Families Daniel Bluestein, MD, Certificate Added Qualifications-Geriatrics Professor & Director, Geriatrics Division Department of Family & Community Medicine Eastern Virginia Medical School Norfolk, Virginia Patricia Latham Bach, Psy. D, RN, MS Post-Doctoral Fellow Center for Neuropsychological Services Kaiser-Permanente Sacramento, California
Managing the “Other” Patient in Long-Term Care: Skills for Working with Families Daniel Bluestein, MD, Certificate Added Qualifications-Geriatrics Professor & Director, Geriatrics Division Department of Family & Community Medicine Eastern Virginia Medical School Norfolk, Virginia Patricia Latham Bach, Psy. D, RN, MS Post-Doctoral Fellow Center for Neuropsychological Services Kaiser-Permanente Sacramento, California
 Need for Geriatrics Education • A demographic imperative • Need knowledge, skills & attitude: • Part of job as Family Physician • Self-efficacy for same
Need for Geriatrics Education • A demographic imperative • Need knowledge, skills & attitude: • Part of job as Family Physician • Self-efficacy for same
 Not always the easiest “sell” • Especially in longterm care. • Solutions • Experiences with mentors • Build on core Family Medicine Precepts (transferable). • Active role
Not always the easiest “sell” • Especially in longterm care. • Solutions • Experiences with mentors • Build on core Family Medicine Precepts (transferable). • Active role
 Families, LTC, & Education • Opportunity to apply Family Systems Concepts • Family Medicine learner in leadership role • Transferable to other settings, types of pts • Rewarding • Responding to need • Families often appreciate
Families, LTC, & Education • Opportunity to apply Family Systems Concepts • Family Medicine learner in leadership role • Transferable to other settings, types of pts • Rewarding • Responding to need • Families often appreciate
 OBJECTIVES 1. Discuss the Pearlin Stress Process Model as a conceptual framework. 2. Review Family Systems concepts that can impact communication with families. 3. Summarize principles for conduct of family meetings. 4. Questions and discussion
OBJECTIVES 1. Discuss the Pearlin Stress Process Model as a conceptual framework. 2. Review Family Systems concepts that can impact communication with families. 3. Summarize principles for conduct of family meetings. 4. Questions and discussion
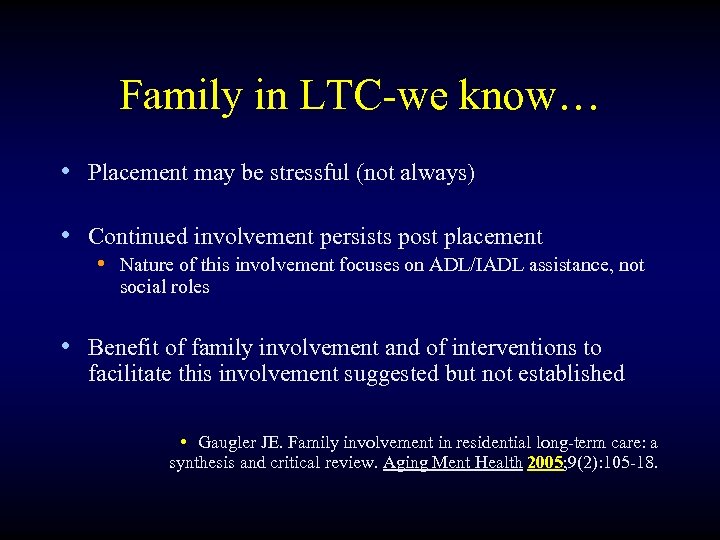 Family in LTC-we know… • Placement may be stressful (not always) • Continued involvement persists post placement • Nature of this involvement focuses on ADL/IADL assistance, not social roles • Benefit of family involvement and of interventions to facilitate this involvement suggested but not established • Gaugler JE. Family involvement in residential long-term care: a synthesis and critical review. Aging Ment Health 2005; 9(2): 105 -18.
Family in LTC-we know… • Placement may be stressful (not always) • Continued involvement persists post placement • Nature of this involvement focuses on ADL/IADL assistance, not social roles • Benefit of family involvement and of interventions to facilitate this involvement suggested but not established • Gaugler JE. Family involvement in residential long-term care: a synthesis and critical review. Aging Ment Health 2005; 9(2): 105 -18.
 Family in LTC research-limits • • • Cross-sectional designs Small samples Use range of LTC settings, not just NHs Quantitative rather than qualitative approach Need for ethnic diversity in study populations
Family in LTC research-limits • • • Cross-sectional designs Small samples Use range of LTC settings, not just NHs Quantitative rather than qualitative approach Need for ethnic diversity in study populations
 Caveats • Our empirical database is limited • Lots of ways to do this (what we describe worked for us). • It’s not just a meeting but a process of continuing communication
Caveats • Our empirical database is limited • Lots of ways to do this (what we describe worked for us). • It’s not just a meeting but a process of continuing communication
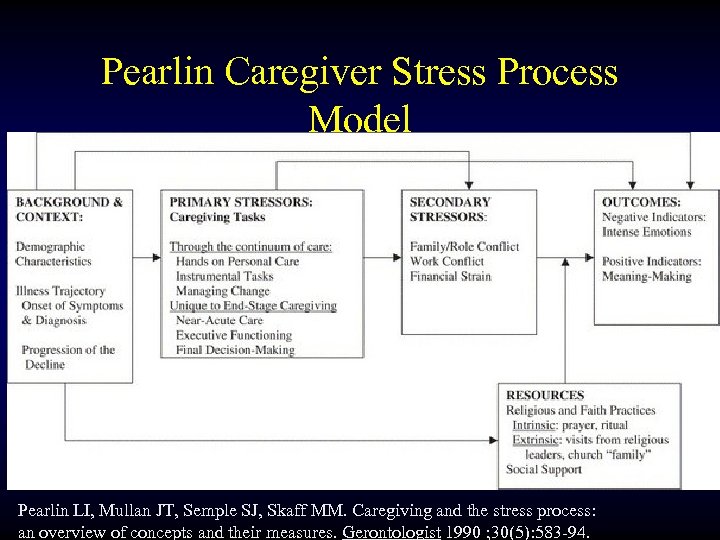 Pearlin Caregiver Stress Process Model Pearlin LI, Mullan JT, Semple SJ, Skaff MM. Caregiving and the stress process: an overview of concepts and their measures. Gerontologist 1990 ; 30(5): 583 -94.
Pearlin Caregiver Stress Process Model Pearlin LI, Mullan JT, Semple SJ, Skaff MM. Caregiving and the stress process: an overview of concepts and their measures. Gerontologist 1990 ; 30(5): 583 -94.
 Family Dysfunction predictors of negative outcomes • Caregivers who reported poor family functioning had higher ratings of strain and burden. • Family dysfunctions included: • • Negative expressed emotion (hostility, criticism, sadness…) Poor problem solving Impaired delegation of practical & emotional tasks Excessive emotional distance or closeness • Caution: cross sectional study • Corollary: These are red flags Heru AM, Ryan CE, Iqbal A. Family functioning in the caregivers of patients with dementia. Int J Geriatr Psychiatry 2004; 19(6): 533 -7.
Family Dysfunction predictors of negative outcomes • Caregivers who reported poor family functioning had higher ratings of strain and burden. • Family dysfunctions included: • • Negative expressed emotion (hostility, criticism, sadness…) Poor problem solving Impaired delegation of practical & emotional tasks Excessive emotional distance or closeness • Caution: cross sectional study • Corollary: These are red flags Heru AM, Ryan CE, Iqbal A. Family functioning in the caregivers of patients with dementia. Int J Geriatr Psychiatry 2004; 19(6): 533 -7.
 Structural Family Theory (Minuchin) • Family interactions are regulated predictable patterns that determine how family members: communicate, • manage disagreements, • distribute leadership roles, • form alliances, • negotiate distance or closeness. • Relatively stable and resistant to change. • Whereas healthy families adapt, others become rigid or disorganized under stress such as LTC placement.
Structural Family Theory (Minuchin) • Family interactions are regulated predictable patterns that determine how family members: communicate, • manage disagreements, • distribute leadership roles, • form alliances, • negotiate distance or closeness. • Relatively stable and resistant to change. • Whereas healthy families adapt, others become rigid or disorganized under stress such as LTC placement.
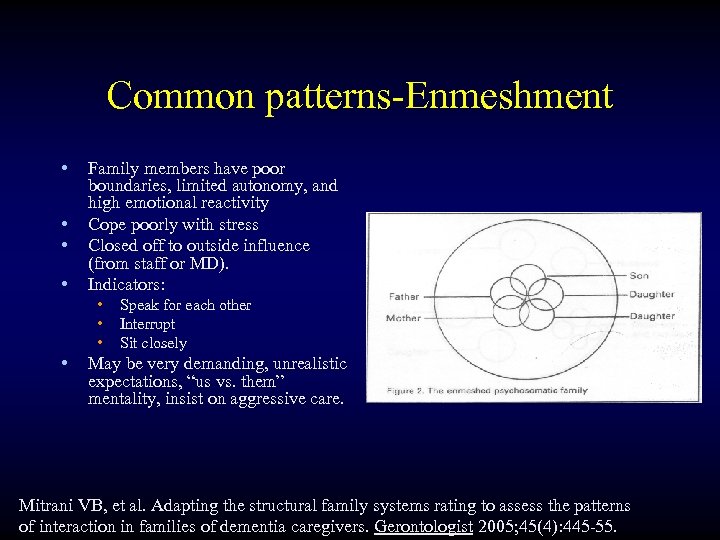 Common patterns-Enmeshment • Family members have poor • • boundaries, limited autonomy, and high emotional reactivity Cope poorly with stress Closed off to outside influence (from staff or MD). Indicators: • Speak for each other • Interrupt • Sit closely May be very demanding, unrealistic expectations, “us vs. them” mentality, insist on aggressive care. Mitrani VB, et al. Adapting the structural family systems rating to assess the patterns of interaction in families of dementia caregivers. Gerontologist 2005; 45(4): 445 -55.
Common patterns-Enmeshment • Family members have poor • • boundaries, limited autonomy, and high emotional reactivity Cope poorly with stress Closed off to outside influence (from staff or MD). Indicators: • Speak for each other • Interrupt • Sit closely May be very demanding, unrealistic expectations, “us vs. them” mentality, insist on aggressive care. Mitrani VB, et al. Adapting the structural family systems rating to assess the patterns of interaction in families of dementia caregivers. Gerontologist 2005; 45(4): 445 -55.
 Case • Ms B, aged 90, progressive dementia-Daughter from California (LCSW), calls daily, into “alternative medicine” , dislikes “chemicals” (but insists mom has bottle of scotch in her room) • Dtr looks like younger version of mom, speaks for her, answers questions for her.
Case • Ms B, aged 90, progressive dementia-Daughter from California (LCSW), calls daily, into “alternative medicine” , dislikes “chemicals” (but insists mom has bottle of scotch in her room) • Dtr looks like younger version of mom, speaks for her, answers questions for her.
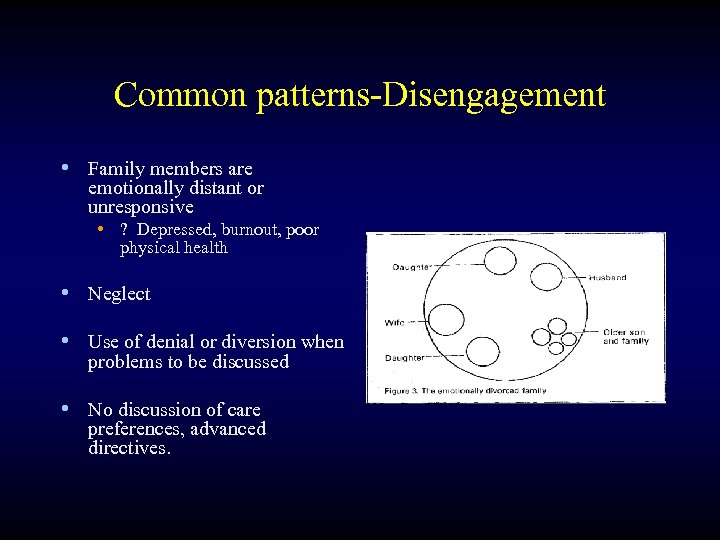 Common patterns-Disengagement • Family members are emotionally distant or unresponsive • ? Depressed, burnout, poor physical health • Neglect • Use of denial or diversion when problems to be discussed • No discussion of care preferences, advanced directives.
Common patterns-Disengagement • Family members are emotionally distant or unresponsive • ? Depressed, burnout, poor physical health • Neglect • Use of denial or diversion when problems to be discussed • No discussion of care preferences, advanced directives.
 Case Example-Disengagement • 79 yo Hispanic male in assisted living • Arthritis, anxiety & possible OCD, reflux, mild memory deficits, smokes. • Always dissatisfied, has demanded moves from several prior facilities • Life-long conflicted relationships with children • Lonely, high utilization of care, • Daughter lives 1 mile away, never visits, leading to increased isolation, somatization behavior. • Unwilling to transport to outside appointments • Feels father should be “no-code” despite mild degree of memory & physical impairment
Case Example-Disengagement • 79 yo Hispanic male in assisted living • Arthritis, anxiety & possible OCD, reflux, mild memory deficits, smokes. • Always dissatisfied, has demanded moves from several prior facilities • Life-long conflicted relationships with children • Lonely, high utilization of care, • Daughter lives 1 mile away, never visits, leading to increased isolation, somatization behavior. • Unwilling to transport to outside appointments • Feels father should be “no-code” despite mild degree of memory & physical impairment
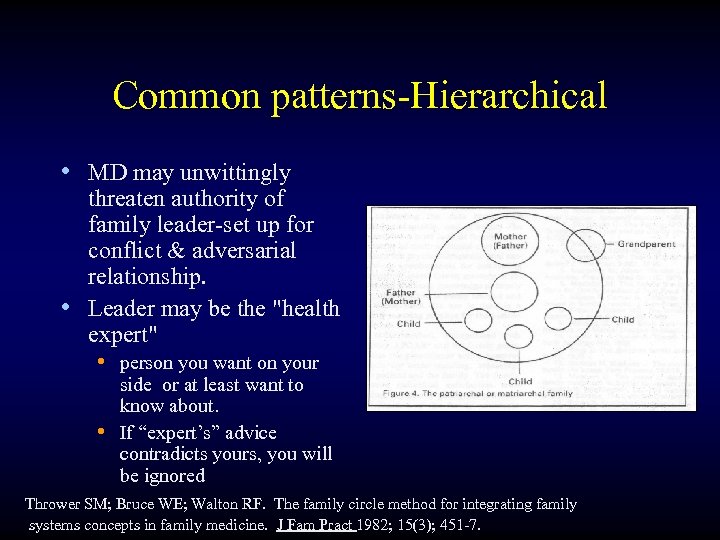 Common patterns-Hierarchical • MD may unwittingly threaten authority of family leader-set up for conflict & adversarial relationship. • Leader may be the "health expert" • person you want on your side or at least want to know about. • If “expert’s” advice contradicts yours, you will be ignored Thrower SM; Bruce WE; Walton RF. The family circle method for integrating family systems concepts in family medicine. J Fam Pract 1982; 15(3); 451 -7.
Common patterns-Hierarchical • MD may unwittingly threaten authority of family leader-set up for conflict & adversarial relationship. • Leader may be the "health expert" • person you want on your side or at least want to know about. • If “expert’s” advice contradicts yours, you will be ignored Thrower SM; Bruce WE; Walton RF. The family circle method for integrating family systems concepts in family medicine. J Fam Pract 1982; 15(3); 451 -7.
 Case Example-Hierarchical • 95 yo Caucasian woman with renal failure, DJD, dementia • Failing in her apartment, staff wishes her to move to long-term care. • Son, a physician, challenges her degree of cognitive decline, demands meeting with staff, critical of staff competence, when neuropsych testing recommended, brings her to his institution to use his “own” consultant • Agrees to placement thereafter
Case Example-Hierarchical • 95 yo Caucasian woman with renal failure, DJD, dementia • Failing in her apartment, staff wishes her to move to long-term care. • Son, a physician, challenges her degree of cognitive decline, demands meeting with staff, critical of staff competence, when neuropsych testing recommended, brings her to his institution to use his “own” consultant • Agrees to placement thereafter
 Other key concepts-Triangulation • Occurs when a 3 rd person is drawn into a 2–person system to diffuse anxiety or conflict or to communicate with each other through a 3 rd party. • Corollaries: • If the index pt buffers conflict among other family members, they may be unwilling to limit care. • May gang up on you
Other key concepts-Triangulation • Occurs when a 3 rd person is drawn into a 2–person system to diffuse anxiety or conflict or to communicate with each other through a 3 rd party. • Corollaries: • If the index pt buffers conflict among other family members, they may be unwilling to limit care. • May gang up on you
 Case-example, triangulation • 81 yo Caucasian woman, multiple hospitalizations related to cognitive impairment. • Daughter & son-in-law: argue when visiting. • Relate better & work as “team” when mom develops pressure ulcer, criticizing care.
Case-example, triangulation • 81 yo Caucasian woman, multiple hospitalizations related to cognitive impairment. • Daughter & son-in-law: argue when visiting. • Relate better & work as “team” when mom develops pressure ulcer, criticizing care.
 Coalitions • When 2 people collude against a 3 rd • May exclude other key family members. • Trap for MD-recognize and don’t take sides. There may be deliberate effort to draw you in
Coalitions • When 2 people collude against a 3 rd • May exclude other key family members. • Trap for MD-recognize and don’t take sides. There may be deliberate effort to draw you in
 Coalitions –case example • 90 yo man-PD, CHF, mild dementia. Family has received conflicting information about prognosis during recent hospitalization for CHF. Goals of care discussed /w wife (POA) & daughters. • Older Daughter calls you later to express her & her sister’s concerns, feels her mother is not acting in her father’s interest (e. g. , wife seeks conservative care) • Criticizes her mother as someone who never made a dime but happy to spend what dad earned, wants his $$ rather than spend on his care…
Coalitions –case example • 90 yo man-PD, CHF, mild dementia. Family has received conflicting information about prognosis during recent hospitalization for CHF. Goals of care discussed /w wife (POA) & daughters. • Older Daughter calls you later to express her & her sister’s concerns, feels her mother is not acting in her father’s interest (e. g. , wife seeks conservative care) • Criticizes her mother as someone who never made a dime but happy to spend what dad earned, wants his $$ rather than spend on his care…
 Overview • • Develop a baseline Crates positive 1 st impression of reaching out. Facilitates their understanding of this philosophy Creates alliances Enhances cultural competence Goal is to develop a win-win at the outset Environmental pre-assessment also important Identify family as experts about their loved one
Overview • • Develop a baseline Crates positive 1 st impression of reaching out. Facilitates their understanding of this philosophy Creates alliances Enhances cultural competence Goal is to develop a win-win at the outset Environmental pre-assessment also important Identify family as experts about their loved one
 Family meeting ≠ Family therapy session • • • Boundaries different Use of “I” different Don’t need to modify behavior as a rule Common ground established (pt) Different assessment measures Conducting supportive rather than therapeutic intervention
Family meeting ≠ Family therapy session • • • Boundaries different Use of “I” different Don’t need to modify behavior as a rule Common ground established (pt) Different assessment measures Conducting supportive rather than therapeutic intervention
 Planning the Family Meeting • • • Set goals Establish empathetic, common ground Elicit Family concerns Assess the family in relation to patient Provide overview of careplan Mc. Daniel S, Campbell TL, Seaburn DB. Family-Oriented Primary Care: a Manual for Medical Providers. Springer-Verlag, Inc. , New York: 1990. 73 -86.
Planning the Family Meeting • • • Set goals Establish empathetic, common ground Elicit Family concerns Assess the family in relation to patient Provide overview of careplan Mc. Daniel S, Campbell TL, Seaburn DB. Family-Oriented Primary Care: a Manual for Medical Providers. Springer-Verlag, Inc. , New York: 1990. 73 -86.
 Set goals • • Find out who the players are & how they interact Information & collateral history? Buy-in to treatment plan “Philosophy of care” (e. g. , code status, Aggressiveness of testing and therapeutic modalities) • Assistance-e. g. help overcome patient resistance, social support for depressed patients… • Support of caregivers • Avoid trouble
Set goals • • Find out who the players are & how they interact Information & collateral history? Buy-in to treatment plan “Philosophy of care” (e. g. , code status, Aggressiveness of testing and therapeutic modalities) • Assistance-e. g. help overcome patient resistance, social support for depressed patients… • Support of caregivers • Avoid trouble
 Set the stage • Thank them for coming • Review purpose of meeting • Elicit their expectations • What do you of your loved one’s condition & prognosis (what do you expect from here? ) • Functional assessment
Set the stage • Thank them for coming • Review purpose of meeting • Elicit their expectations • What do you of your loved one’s condition & prognosis (what do you expect from here? ) • Functional assessment
 Building partnership • What is your relationship to the patient? -e. g. , spouse, child, etc • How long have you been a caregiver? • What are things that have been most stressful to you with this transition, how can we most help you? • What concerns do you have for the future? • Acknowledge the ongoing stress of having family member in LTC
Building partnership • What is your relationship to the patient? -e. g. , spouse, child, etc • How long have you been a caregiver? • What are things that have been most stressful to you with this transition, how can we most help you? • What concerns do you have for the future? • Acknowledge the ongoing stress of having family member in LTC
 Patient Assessment, Basic • Geriatric • MMSE & Clock-draw • GDS • Basic & Instrumental ADLs. • Medical-what is the status and prognosis of the patient's various chronic illnesses: • • • CHF COPD Renal Failure Cancers Other
Patient Assessment, Basic • Geriatric • MMSE & Clock-draw • GDS • Basic & Instrumental ADLs. • Medical-what is the status and prognosis of the patient's various chronic illnesses: • • • CHF COPD Renal Failure Cancers Other
 Functional Assessment, family perspective& collateral History • Neuropsychiatric Inventory (10 minutes) • Behavior • Mood • Some cognition • Some functional • Clinical Dementia Rating Scale (10 minutes) • Cognition • ADLs • IADLS Have Family complete prior to visit if possible
Functional Assessment, family perspective& collateral History • Neuropsychiatric Inventory (10 minutes) • Behavior • Mood • Some cognition • Some functional • Clinical Dementia Rating Scale (10 minutes) • Cognition • ADLs • IADLS Have Family complete prior to visit if possible
 Facilitation techniques • Allow 1 person to speak at a time • Be sure everyone has a chance to say something if they choose • Use reflection for clarification • Normalizing (when faced with this situation, many people are [stressed/depressed/angry/guilty/etc. ]. Is this the case for you? ) • Emphasize strengths & positives (how have they coped successfully in the past)
Facilitation techniques • Allow 1 person to speak at a time • Be sure everyone has a chance to say something if they choose • Use reflection for clarification • Normalizing (when faced with this situation, many people are [stressed/depressed/angry/guilty/etc. ]. Is this the case for you? ) • Emphasize strengths & positives (how have they coped successfully in the past)
 Unobtrusive Assessment-verbal • • Who talks & who doesn't Who argues or agrees with whom Who is the leader or “health expert What they say, how they say it,
Unobtrusive Assessment-verbal • • Who talks & who doesn't Who argues or agrees with whom Who is the leader or “health expert What they say, how they say it,
 Unobtrusive Assessment-nonverbal • • Who’s there & who’s not Who sits near whom Body language How they act • Be ready for emotion • Have tissues handy
Unobtrusive Assessment-nonverbal • • Who’s there & who’s not Who sits near whom Body language How they act • Be ready for emotion • Have tissues handy
 Historical appraisal • Any other recent changes or stressors • How they have handled stressful situations in the past. • Where are they in terms of the “family lifecycle? ” • Are there prior medical experiences or medical beliefs that shape current situation
Historical appraisal • Any other recent changes or stressors • How they have handled stressful situations in the past. • Where are they in terms of the “family lifecycle? ” • Are there prior medical experiences or medical beliefs that shape current situation
 Presenting information • Present your assessment of patient's status • Goal setting & priorities-jointly establish ”philosophy of care” • Know what they already know or believe • Reconcile various sources of info (e. g. , “different” information from other physicians). • Are all family members “on the same page”?
Presenting information • Present your assessment of patient's status • Goal setting & priorities-jointly establish ”philosophy of care” • Know what they already know or believe • Reconcile various sources of info (e. g. , “different” information from other physicians). • Are all family members “on the same page”?
 What if you recognize dysfunction • Your goal is to assist the family in communicating or managing conflict sufficiently enough to address the immediate patient care issues, not "fix" family conflicts.
What if you recognize dysfunction • Your goal is to assist the family in communicating or managing conflict sufficiently enough to address the immediate patient care issues, not "fix" family conflicts.
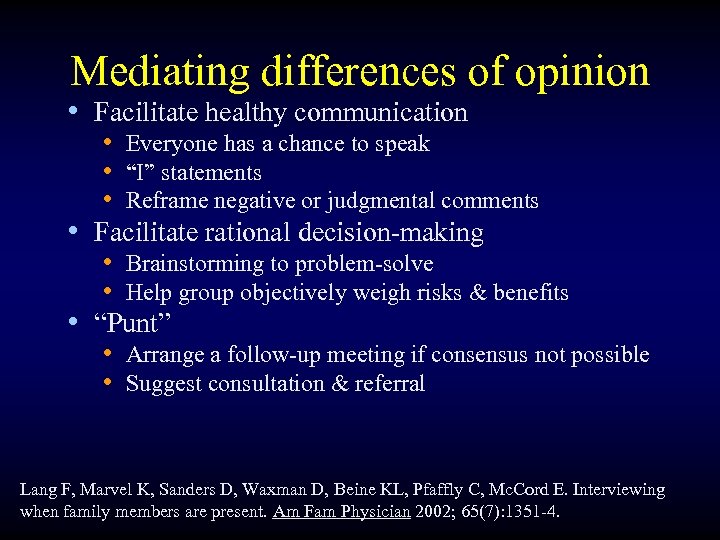 Mediating differences of opinion • Facilitate healthy communication • Everyone has a chance to speak • “I” statements • Reframe negative or judgmental comments • Facilitate rational decision-making • Brainstorming to problem-solve • Help group objectively weigh risks & benefits • “Punt” • Arrange a follow-up meeting if consensus not possible • Suggest consultation & referral Lang F, Marvel K, Sanders D, Waxman D, Beine KL, Pfaffly C, Mc. Cord E. Interviewing when family members are present. Am Fam Physician 2002; 65(7): 1351 -4.
Mediating differences of opinion • Facilitate healthy communication • Everyone has a chance to speak • “I” statements • Reframe negative or judgmental comments • Facilitate rational decision-making • Brainstorming to problem-solve • Help group objectively weigh risks & benefits • “Punt” • Arrange a follow-up meeting if consensus not possible • Suggest consultation & referral Lang F, Marvel K, Sanders D, Waxman D, Beine KL, Pfaffly C, Mc. Cord E. Interviewing when family members are present. Am Fam Physician 2002; 65(7): 1351 -4.
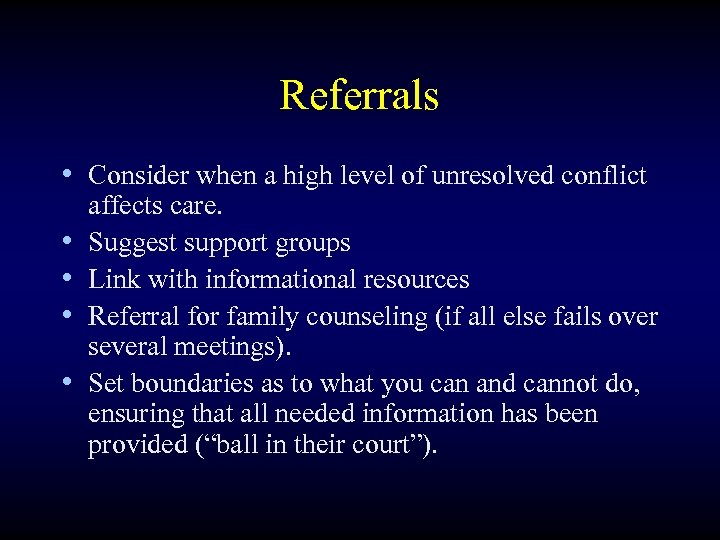 Referrals • Consider when a high level of unresolved conflict • • affects care. Suggest support groups Link with informational resources Referral for family counseling (if all else fails over several meetings). Set boundaries as to what you can and cannot do, ensuring that all needed information has been provided (“ball in their court”).
Referrals • Consider when a high level of unresolved conflict • • affects care. Suggest support groups Link with informational resources Referral for family counseling (if all else fails over several meetings). Set boundaries as to what you can and cannot do, ensuring that all needed information has been provided (“ball in their court”).
 When you are on shaky ground • Build trust • Get “the high ground” • Be informed • Be proactive • Project calm caring wisdom (don’t let frustration show) • It’s a process
When you are on shaky ground • Build trust • Get “the high ground” • Be informed • Be proactive • Project calm caring wisdom (don’t let frustration show) • It’s a process
 Pitfalls • Talking rather than listening • Being pulled into coalitions. • Not having a meeting • Excluding the patient (if lucid)
Pitfalls • Talking rather than listening • Being pulled into coalitions. • Not having a meeting • Excluding the patient (if lucid)
 Evaluating resistance & dissatisfaction • Caregiver not acting in patient’s best interest • Depressed • $$$ incentives • Conflictual relationship with patient • Covert or absent players-Are there conflicting views of the approach to care? • Disconnect between culture of medicine & family health beliefs?
Evaluating resistance & dissatisfaction • Caregiver not acting in patient’s best interest • Depressed • $$$ incentives • Conflictual relationship with patient • Covert or absent players-Are there conflicting views of the approach to care? • Disconnect between culture of medicine & family health beliefs?
 You are a part of the system (Like it or not) • Your own skills, attitudes & behavior reflect what you learned in your family of origin. Corollary: Understanding where you come from can make you more effective. • The clinician (and the facility and staff) are also now part of the index family’s system
You are a part of the system (Like it or not) • Your own skills, attitudes & behavior reflect what you learned in your family of origin. Corollary: Understanding where you come from can make you more effective. • The clinician (and the facility and staff) are also now part of the index family’s system
 Team-based approach • Geriatrics is a team sport. Players include but not limited to: • Psychologists, • Social workers /case-managers, • Nursing (RNs and CNAs), • Chaplains, • PT/OT • Dietician • Other team members will observe things you may not pick up on, ask questions in a different style. • “Good Cop/Bad Cop”
Team-based approach • Geriatrics is a team sport. Players include but not limited to: • Psychologists, • Social workers /case-managers, • Nursing (RNs and CNAs), • Chaplains, • PT/OT • Dietician • Other team members will observe things you may not pick up on, ask questions in a different style. • “Good Cop/Bad Cop”
 There is no 1 best way • Your approach will depend on time available, other team members, style… • Flexibility maximizes the possibilities of success. • No matter what you do, the return on your investment of effort & time is worth it.
There is no 1 best way • Your approach will depend on time available, other team members, style… • Flexibility maximizes the possibilities of success. • No matter what you do, the return on your investment of effort & time is worth it.
 Further reading • Mc. Goldrick M, Gerson R, Shellenberger S. Genograms: Assessment and Intervention (2 nd edition). New York, W. W. Norton & Co. 1999.
Further reading • Mc. Goldrick M, Gerson R, Shellenberger S. Genograms: Assessment and Intervention (2 nd edition). New York, W. W. Norton & Co. 1999.


