ddd958376076789ef014b4ecfe0fbe5e.ppt
- Количество слайдов: 55
 Managing Differences and Difficult Populations Glenn Duncan LPC, LCADC, CCS, ACS Copyright © 2017, Advanced Counselor Training Do not reproduce any workshop materials without express written consent.
Managing Differences and Difficult Populations Glenn Duncan LPC, LCADC, CCS, ACS Copyright © 2017, Advanced Counselor Training Do not reproduce any workshop materials without express written consent.
 From Differences to Similarities Exercise n n There are certain core tasks that each therapist must learn to master in order to be effective with clients. Supervisors must help each supervisee progress towards mastery of these tasks. What similar tasks must therapists master in order to a level of expertise when working with their clients? In a small group, brainstorm and come up with as many core tasks (e. g. , the ability to establish a therapeutic relationship with a client) that you feel are needed for therapists to master, in order to be the most effective when working with clients.
From Differences to Similarities Exercise n n There are certain core tasks that each therapist must learn to master in order to be effective with clients. Supervisors must help each supervisee progress towards mastery of these tasks. What similar tasks must therapists master in order to a level of expertise when working with their clients? In a small group, brainstorm and come up with as many core tasks (e. g. , the ability to establish a therapeutic relationship with a client) that you feel are needed for therapists to master, in order to be the most effective when working with clients.
 From Differences to Similarities n Develop a Therapeutic Alliance n Nurture Hope n n Understand & Implement Best Practices in Theory and Application – knowledge of the best, evidence based therapeutic paradigms when working with clients individually, in group settings and with their families. Be able to properly assess individual client problems and needs and tailor theory and techniques that best suite individual client needs. Pharmacological interventions/interactions should also be known and taught to supervisees and known by supervisors, without prejudice (e. g. , methadone prejudice). Teach Skills – emotional regulation, relaxation, problem-solving, cognitive restructuring skills, interpersonal skills, tolerance and acceptance skills.
From Differences to Similarities n Develop a Therapeutic Alliance n Nurture Hope n n Understand & Implement Best Practices in Theory and Application – knowledge of the best, evidence based therapeutic paradigms when working with clients individually, in group settings and with their families. Be able to properly assess individual client problems and needs and tailor theory and techniques that best suite individual client needs. Pharmacological interventions/interactions should also be known and taught to supervisees and known by supervisors, without prejudice (e. g. , methadone prejudice). Teach Skills – emotional regulation, relaxation, problem-solving, cognitive restructuring skills, interpersonal skills, tolerance and acceptance skills.
 From Differences to Similarities n n Provide Ongoing Education to the Client – the ability to conduct accurate assessments, working with the client towards individualized, behavioral treatment planning, having the client engaged in self-monitoring of thoughts, feelings and behaviors, enhance client awareness of the addition process. Build in Generalization and Maintenance Procedures – understand the concept of skill generalization to the target problem, involve significant others as allies in obtaining generalization of targeted positive behaviors, feelings and thoughts, and helping with the maintenance of them.
From Differences to Similarities n n Provide Ongoing Education to the Client – the ability to conduct accurate assessments, working with the client towards individualized, behavioral treatment planning, having the client engaged in self-monitoring of thoughts, feelings and behaviors, enhance client awareness of the addition process. Build in Generalization and Maintenance Procedures – understand the concept of skill generalization to the target problem, involve significant others as allies in obtaining generalization of targeted positive behaviors, feelings and thoughts, and helping with the maintenance of them.
 From Differences to Similarities n n Assess/Treat/Refer Co-occurring Problems – be able to accurately identify possible Co-occurring problems and treat (if education and training ethically provides the ability to do so), or refer client to have Co-occurring problems addressed with specialist. Assess For & Conduct Relapse Prevention – assess and work with relapse triggers and high risk situations that will occur for the client. Ensure Clients “Take Credit” and “Ownership” for Their Changes – foster independence and client ownership of the changes made. Other important clinician factors include: experience, personal characteristics of the client, therapist and supervisor, cultural competence, and comfort with ambiguity.
From Differences to Similarities n n Assess/Treat/Refer Co-occurring Problems – be able to accurately identify possible Co-occurring problems and treat (if education and training ethically provides the ability to do so), or refer client to have Co-occurring problems addressed with specialist. Assess For & Conduct Relapse Prevention – assess and work with relapse triggers and high risk situations that will occur for the client. Ensure Clients “Take Credit” and “Ownership” for Their Changes – foster independence and client ownership of the changes made. Other important clinician factors include: experience, personal characteristics of the client, therapist and supervisor, cultural competence, and comfort with ambiguity.
 Uniqueness of Individuals n n Client uniqueness can include, but is not limited to, race, ethnicity, culture, subculture, age, sexual orientation, gender, physical and psychological limitations, and geographic location. Uniqueness should be assessed: 1. 2. 3. 4. In the context of identifying the difference(s); Developing an understanding of the interactional nature of many differences that exist within one client. Once identified, these differences should be interpreted in the context of their contribution to current functioning of the client. In the case of more than one unique quality, supervisors must continue to assess and make sure supervisees are not focusing on uniqueness at the expense of another.
Uniqueness of Individuals n n Client uniqueness can include, but is not limited to, race, ethnicity, culture, subculture, age, sexual orientation, gender, physical and psychological limitations, and geographic location. Uniqueness should be assessed: 1. 2. 3. 4. In the context of identifying the difference(s); Developing an understanding of the interactional nature of many differences that exist within one client. Once identified, these differences should be interpreted in the context of their contribution to current functioning of the client. In the case of more than one unique quality, supervisors must continue to assess and make sure supervisees are not focusing on uniqueness at the expense of another.
 Cultural Issues in Supervision n n Supervisors increasingly will have to monitor practitioners’ sensitivity to the beliefs, attitudes, behaviors, and needs of clients who are different from the practitioners. Key factors supervisors need to monitor: 1. Differing perceptions of the meaning of functions, expectations, explanations, and the behaviors of the client, practitioner, and supervisor whenever such differences are part of the client/supervisee/supervisor interactions. 2. Ensuring that respect and acceptance are shown for religious, spiritual, political, age, gender, and lifestyle differences.
Cultural Issues in Supervision n n Supervisors increasingly will have to monitor practitioners’ sensitivity to the beliefs, attitudes, behaviors, and needs of clients who are different from the practitioners. Key factors supervisors need to monitor: 1. Differing perceptions of the meaning of functions, expectations, explanations, and the behaviors of the client, practitioner, and supervisor whenever such differences are part of the client/supervisee/supervisor interactions. 2. Ensuring that respect and acceptance are shown for religious, spiritual, political, age, gender, and lifestyle differences.
 Cultural Issues in Supervision n Key factors supervisors need to monitor (continued): 3. 4. n Cultural explanations of illness. Supervisor must be able to help a practitioner accurately identify the meaning and severity of symptoms in relation to the cultural group, or individual members within that cultural group. Overall cultural assessment related to diagnosis and care. Supervisee assessment of client perceptions may be impeded by differing views of language, styles of communication, valuing of socioeconomic and other statuses, acceptance of direct questioning, use of storytelling, role of privacy, boundary regulations, role of authority, and the importance of age. Any generalizations about the clients in regards to culture have the potential to produce bias in the clinician and resistance in the client.
Cultural Issues in Supervision n Key factors supervisors need to monitor (continued): 3. 4. n Cultural explanations of illness. Supervisor must be able to help a practitioner accurately identify the meaning and severity of symptoms in relation to the cultural group, or individual members within that cultural group. Overall cultural assessment related to diagnosis and care. Supervisee assessment of client perceptions may be impeded by differing views of language, styles of communication, valuing of socioeconomic and other statuses, acceptance of direct questioning, use of storytelling, role of privacy, boundary regulations, role of authority, and the importance of age. Any generalizations about the clients in regards to culture have the potential to produce bias in the clinician and resistance in the client.
 Organizational Culture n 1. 2. 3. 4. 5. 6. 7. 8. The clinical supervisor cannot manage without some rudimentary understanding of the organizational context, or culture, within which the supervisor must function. The following are questions you can ask in order to ascertain the nature of the organizational culture: Does the staff have a set of common goals, and are those goals appropriate to the setting? What does the administration model to the rest of the staff, what message does the administration send about itself? Does the organization promote professional development? Are, and if so, how are progress towards organizational goals monitored? Is there support for clinical supervision? What is management style within the organization? How does change and decision making occur within the organization? How political is the organization and its players, who are the key players that make policy change decisions?
Organizational Culture n 1. 2. 3. 4. 5. 6. 7. 8. The clinical supervisor cannot manage without some rudimentary understanding of the organizational context, or culture, within which the supervisor must function. The following are questions you can ask in order to ascertain the nature of the organizational culture: Does the staff have a set of common goals, and are those goals appropriate to the setting? What does the administration model to the rest of the staff, what message does the administration send about itself? Does the organization promote professional development? Are, and if so, how are progress towards organizational goals monitored? Is there support for clinical supervision? What is management style within the organization? How does change and decision making occur within the organization? How political is the organization and its players, who are the key players that make policy change decisions?
 Ethnicity vs. Organizational Culture Exercise You have entered into an mental health/substance abuse outpatient treatment organization as the new director of outpatient/intensive outpatient substance abuse treatment services. This is a mid sized organization that specializes in 3 distinct departments: mental health services, substance abuse services, and a specialized case management department for working with HIV+ clients. This outpatient facility states that it does short-medium term outpatient care for clients. During your second week in the organization, you attend your first bi-weekly, interdepartmental group supervision meeting. In this meeting the head of the outpatient mental health department presents a case. This is a case of a Colombian female in her 40’s who was referred for treatment due to depression. She had been in treatment for approximately 9 months, and shared some news with her therapist (the outpatient director).
Ethnicity vs. Organizational Culture Exercise You have entered into an mental health/substance abuse outpatient treatment organization as the new director of outpatient/intensive outpatient substance abuse treatment services. This is a mid sized organization that specializes in 3 distinct departments: mental health services, substance abuse services, and a specialized case management department for working with HIV+ clients. This outpatient facility states that it does short-medium term outpatient care for clients. During your second week in the organization, you attend your first bi-weekly, interdepartmental group supervision meeting. In this meeting the head of the outpatient mental health department presents a case. This is a case of a Colombian female in her 40’s who was referred for treatment due to depression. She had been in treatment for approximately 9 months, and shared some news with her therapist (the outpatient director).
 Ethnicity vs. Organizational Culture Exercise The news the client presented was the happy news (according to the client) that her daughter was pregnant. The client was ecstatic over the news and delighted in sharing with her therapist. The therapist asked pointed questions, such as asking what the daughter will do about her college career (she is a Sophomore). The client stated that the daughter would drop out and return “eventually”, but the important thing would be focusing on her child, not her own education. The therapist then asked if the daughter would need help in rearing the child, the client responded “oh it will be great, I’ll mother her, her mother will mother her, her aunt will mother her, the baby will be well taken care of. ” One last question therapist put forth was a question concerning the father of the child. The client stated the father was not involved, nor was it necessary to have a male in the picture. “The baby will be more than cared for by us all, and my oldest son (14) will be a male role model for the baby. ”
Ethnicity vs. Organizational Culture Exercise The news the client presented was the happy news (according to the client) that her daughter was pregnant. The client was ecstatic over the news and delighted in sharing with her therapist. The therapist asked pointed questions, such as asking what the daughter will do about her college career (she is a Sophomore). The client stated that the daughter would drop out and return “eventually”, but the important thing would be focusing on her child, not her own education. The therapist then asked if the daughter would need help in rearing the child, the client responded “oh it will be great, I’ll mother her, her mother will mother her, her aunt will mother her, the baby will be well taken care of. ” One last question therapist put forth was a question concerning the father of the child. The client stated the father was not involved, nor was it necessary to have a male in the picture. “The baby will be more than cared for by us all, and my oldest son (14) will be a male role model for the baby. ”
 Ethnicity vs. Organizational Culture Exercise The therapist then described how upset she was about this, and was at a loss as to how to convey to the client that while this is a blessed event, it is also a bit of a crisis given the fact that the daughter will drop out of school and no man is involved in the picture. This therapist (the mental health outpatient director) is a white woman in her mid 50’s, and in the past 5 years made a career change from working in New York City in the fashion industry (making well into the 6 figures per year), to becoming a therapist. This fact alone makes you question her sanity, which you do so quietly to yourself, not daring to state it in the meeting. However, the thought did cross your mind to just skip this woman’s treatment “crisis” and make the meeting interesting by asking her the reason for making the switch. The therapist then asked the team for guidance on how to best handle the situation. Thinking to yourself that this therapist was biased in her view of the client and not taking her culture into account when viewing the problem, you were sure others would give her this feedback. What ensued became a bizarre interaction of suggestions for therapist to help “the client realize the crisis she was in” by other staff members. Not one other member suggested that this is not a crisis at all.
Ethnicity vs. Organizational Culture Exercise The therapist then described how upset she was about this, and was at a loss as to how to convey to the client that while this is a blessed event, it is also a bit of a crisis given the fact that the daughter will drop out of school and no man is involved in the picture. This therapist (the mental health outpatient director) is a white woman in her mid 50’s, and in the past 5 years made a career change from working in New York City in the fashion industry (making well into the 6 figures per year), to becoming a therapist. This fact alone makes you question her sanity, which you do so quietly to yourself, not daring to state it in the meeting. However, the thought did cross your mind to just skip this woman’s treatment “crisis” and make the meeting interesting by asking her the reason for making the switch. The therapist then asked the team for guidance on how to best handle the situation. Thinking to yourself that this therapist was biased in her view of the client and not taking her culture into account when viewing the problem, you were sure others would give her this feedback. What ensued became a bizarre interaction of suggestions for therapist to help “the client realize the crisis she was in” by other staff members. Not one other member suggested that this is not a crisis at all.
 Ethnicity vs. Organization Culture Exercise You begin thinking to yourself how bizarre this set of transactions just was, though thinking to yourself how useful this could be in some future workshop exercise. Since nobody in the room seemed to be responding to reality, you decide to dissociate and let your mind continue to wander away from the content of the meeting and drift towards thoughts of the group makeup. Thinking first about the fact that you’re the only male member, to how one therapist’s hair has surely taken on the unintended tint of blue, and then finally drifting to remind yourself to search the employment section of Star Ledger this Sunday. Suddenly, and quite rudely, you’re awakened from what appeared to you as a more useful pursuit of your mental energies, as the focus of the group has turned to you. The director has asked you specifically to give some feedback on this issue to the group. 1. 2. What feedback do you give to the director? Give reasons why you decided to say what you said. What organization cultural issues exist in this program (that we know of)? How do these issues impact our decision making for question 1?
Ethnicity vs. Organization Culture Exercise You begin thinking to yourself how bizarre this set of transactions just was, though thinking to yourself how useful this could be in some future workshop exercise. Since nobody in the room seemed to be responding to reality, you decide to dissociate and let your mind continue to wander away from the content of the meeting and drift towards thoughts of the group makeup. Thinking first about the fact that you’re the only male member, to how one therapist’s hair has surely taken on the unintended tint of blue, and then finally drifting to remind yourself to search the employment section of Star Ledger this Sunday. Suddenly, and quite rudely, you’re awakened from what appeared to you as a more useful pursuit of your mental energies, as the focus of the group has turned to you. The director has asked you specifically to give some feedback on this issue to the group. 1. 2. What feedback do you give to the director? Give reasons why you decided to say what you said. What organization cultural issues exist in this program (that we know of)? How do these issues impact our decision making for question 1?
 Treatment vs. Organization Culture Exercise Two weeks pass, and you’re back in the room that you’ve dubbed “the outer limits” and set yourself mentally to prepare for another case presentation. This case is presented of elderly woman with no real social supports, depressed, whose case has been transferred 5 months ago from anotherapist who left the agency. The woman has been in outpatient treatment during her entire stay at the agency. This therapist is asking the group for help with treatment goals for this client, and concern over a direction to go with when working with the client for the next upcoming months. You’re handed the genogram, which has been passed to each member of the supervision meeting. As you’re perusing the genogram, you come to see the date this genogram was done and it says 2007. You do a double take, out of shock, look on the back to make sure this isn’t some kind of joke shop gag gift. But, alas, it isn’t and this woman has been coming weekly to outpatient for the past 9 years.
Treatment vs. Organization Culture Exercise Two weeks pass, and you’re back in the room that you’ve dubbed “the outer limits” and set yourself mentally to prepare for another case presentation. This case is presented of elderly woman with no real social supports, depressed, whose case has been transferred 5 months ago from anotherapist who left the agency. The woman has been in outpatient treatment during her entire stay at the agency. This therapist is asking the group for help with treatment goals for this client, and concern over a direction to go with when working with the client for the next upcoming months. You’re handed the genogram, which has been passed to each member of the supervision meeting. As you’re perusing the genogram, you come to see the date this genogram was done and it says 2007. You do a double take, out of shock, look on the back to make sure this isn’t some kind of joke shop gag gift. But, alas, it isn’t and this woman has been coming weekly to outpatient for the past 9 years.
 Treatment vs. Organization Culture Exercise What you’ve come to learn about the organizational milieu in the now month that you’ve been working there is that E. D. is a micro-manager, but with no real clinical background, at least not enough to question the need for 9 years of supportive counseling which appears to have been downgraded to social hour for this woman (as she is stabilized on her medication, has been so for years, refuses to engage in activities to help with support networks in the community, has never been in any real crisis in the entire 9 years she’s been coming, and appears her only need to continue in “treatment” is that of her need to have an hour where she can talk to an adult who will listen). The organizational style of this meeting is one in which a person does not question the technique or decision making of another, but only provides (psychotic) advice for the continuation of something you’re sure everyone else in the room feels are salient “treatment recommendations”.
Treatment vs. Organization Culture Exercise What you’ve come to learn about the organizational milieu in the now month that you’ve been working there is that E. D. is a micro-manager, but with no real clinical background, at least not enough to question the need for 9 years of supportive counseling which appears to have been downgraded to social hour for this woman (as she is stabilized on her medication, has been so for years, refuses to engage in activities to help with support networks in the community, has never been in any real crisis in the entire 9 years she’s been coming, and appears her only need to continue in “treatment” is that of her need to have an hour where she can talk to an adult who will listen). The organizational style of this meeting is one in which a person does not question the technique or decision making of another, but only provides (psychotic) advice for the continuation of something you’re sure everyone else in the room feels are salient “treatment recommendations”.
 Treatment vs. Organization Culture Exercise But being the eternal optimist that you are, and filling in the textbook definition of insanity (i. e. , expecting different results when using the same ingredients in exactly the same way), you hope beyond hope that somebody will question why this woman has been in treatment for 9 years, or at least what the need is for continued treatment when therapist herself can’t even come up with a goal. With toes and fingers crossed, you are of course let down by the koolaid drinking mantra of each participant as they help try to brainstorm some new treatment goal for this therapist. Shaking your head and cursing yourself internally forgetting to pick up the Star Ledger last week, therapist notices your visible “slip” and questions the “negative vibe” she is receiving from you. 1. 2. What feedback do you give to this therapist? Do you question the group in their apparent inability to question the current effectiveness of treatment at this point? Give reasons why you decided to say what you said. Given that we know more about the organizational culture, does this affect our decision making for question 1?
Treatment vs. Organization Culture Exercise But being the eternal optimist that you are, and filling in the textbook definition of insanity (i. e. , expecting different results when using the same ingredients in exactly the same way), you hope beyond hope that somebody will question why this woman has been in treatment for 9 years, or at least what the need is for continued treatment when therapist herself can’t even come up with a goal. With toes and fingers crossed, you are of course let down by the koolaid drinking mantra of each participant as they help try to brainstorm some new treatment goal for this therapist. Shaking your head and cursing yourself internally forgetting to pick up the Star Ledger last week, therapist notices your visible “slip” and questions the “negative vibe” she is receiving from you. 1. 2. What feedback do you give to this therapist? Do you question the group in their apparent inability to question the current effectiveness of treatment at this point? Give reasons why you decided to say what you said. Given that we know more about the organizational culture, does this affect our decision making for question 1?
 Self Disclosure n n Therapists should generally disclose infrequently. The most appropriate topic for therapist self-disclosure involves professional background, whereas the least appropriate topics include sexual practices and beliefs. Therapists generally use disclosures to validate reality, normalize client experiences, model appropriate behavior, strengthen therapeutic alliance, or offer alternative ways to think or act. Therapists should generally avoid using disclosures that are chiefly for their own needs (e. g. , of this can occur with strengthening therapeutic alliance), disclosures that remove the focus from the client, that interfere with the flow of the session, that burden or confuse the client, that are intrusive, that blur the boundaries, or that over-stimulate the client.
Self Disclosure n n Therapists should generally disclose infrequently. The most appropriate topic for therapist self-disclosure involves professional background, whereas the least appropriate topics include sexual practices and beliefs. Therapists generally use disclosures to validate reality, normalize client experiences, model appropriate behavior, strengthen therapeutic alliance, or offer alternative ways to think or act. Therapists should generally avoid using disclosures that are chiefly for their own needs (e. g. , of this can occur with strengthening therapeutic alliance), disclosures that remove the focus from the client, that interfere with the flow of the session, that burden or confuse the client, that are intrusive, that blur the boundaries, or that over-stimulate the client.
 Self Disclosure n n n Therapist self-disclosure in response to client self-disclosure seems to be particularly effective in eliciting client disclosure. Therapists should observe carefully how clients respond to therapist disclosures, ask about client reactions, and use the information to conceptualize the clients and decide how to intervene next. It may be especially important to therapists to disclose with clients who have difficulty forming relationships in therapeutic setting. The clinical use of intentional self-disclosure requires thoughtful and judicious application. The use of self-disclosure can also vary depending on the treatment setting (e. g. , outpatient vs. milieu based treatment settings).
Self Disclosure n n n Therapist self-disclosure in response to client self-disclosure seems to be particularly effective in eliciting client disclosure. Therapists should observe carefully how clients respond to therapist disclosures, ask about client reactions, and use the information to conceptualize the clients and decide how to intervene next. It may be especially important to therapists to disclose with clients who have difficulty forming relationships in therapeutic setting. The clinical use of intentional self-disclosure requires thoughtful and judicious application. The use of self-disclosure can also vary depending on the treatment setting (e. g. , outpatient vs. milieu based treatment settings).
 Difficulties in Supervision n 1. 2. 3. 4. Problematic supervision has been found to be characterized by: Confrontational criticism Direct attribution of blame Unclear agendas Instructive rather than interactive learning processes
Difficulties in Supervision n 1. 2. 3. 4. Problematic supervision has been found to be characterized by: Confrontational criticism Direct attribution of blame Unclear agendas Instructive rather than interactive learning processes
 Critical Incidents in Supervision n 1. 2. 3. 4. 5. 6. 7. Difficulties, and in more pronounced terms, critical incidents reported by supervisors includes issues in the following: Supervisee competence Multicultural issues Role conflicts Sexual attraction Gender-related misunderstandings Ethical issues Supervisee characteristics
Critical Incidents in Supervision n 1. 2. 3. 4. 5. 6. 7. Difficulties, and in more pronounced terms, critical incidents reported by supervisors includes issues in the following: Supervisee competence Multicultural issues Role conflicts Sexual attraction Gender-related misunderstandings Ethical issues Supervisee characteristics
 Critical Incidents in Supervision n 1. 2. 3. 4. 5. 6. 7. Supervisee characteristics that can interfere in the resolution of critical incidents include the following: Low emotional awareness Problems with autonomy Personal issues Professional identity Respect for client difference Personal motivation Supervise resistance, defensiveness, and negative transferences
Critical Incidents in Supervision n 1. 2. 3. 4. 5. 6. 7. Supervisee characteristics that can interfere in the resolution of critical incidents include the following: Low emotional awareness Problems with autonomy Personal issues Professional identity Respect for client difference Personal motivation Supervise resistance, defensiveness, and negative transferences
 Critical Incidents and Countertransference n 1. 2. 3. 4. 5. 6. 7. 8. 9. The supervisory relationship, and the issues raised in the past 3 slides, can also raise strong countertransference feelings in supervisors. Sources of supervisor countertransference include: Supervisee interpersonal style The supervision context Unresolved supervisor issues Problematic supervisee–client or supervisee–supervisor interactions Supervisee oppositional behavior Supervisee passivity Supervisee self-aggrandizement Supervisee personal behaviors and/or manners Erotic attraction
Critical Incidents and Countertransference n 1. 2. 3. 4. 5. 6. 7. 8. 9. The supervisory relationship, and the issues raised in the past 3 slides, can also raise strong countertransference feelings in supervisors. Sources of supervisor countertransference include: Supervisee interpersonal style The supervision context Unresolved supervisor issues Problematic supervisee–client or supervisee–supervisor interactions Supervisee oppositional behavior Supervisee passivity Supervisee self-aggrandizement Supervisee personal behaviors and/or manners Erotic attraction
 How Supervisors Resolve Difficulties n n 1. 2. 3. 4. 5. 6. 7. 8. Research has shown 4 basic interaction styles when dealing with difficult supervisees: relational, reflective, confrontational, and avoidant. Relational approaches to supervision explore difficulties and included those focused on the supervisory relationship, the supervisee relationship with client, and the supervisee relationship with self. Name the difficulty Validate and normalize Attune to supervisee needs Support Anticipate Explore parallel process Acknowledge mistakes Modeling
How Supervisors Resolve Difficulties n n 1. 2. 3. 4. 5. 6. 7. 8. Research has shown 4 basic interaction styles when dealing with difficult supervisees: relational, reflective, confrontational, and avoidant. Relational approaches to supervision explore difficulties and included those focused on the supervisory relationship, the supervisee relationship with client, and the supervisee relationship with self. Name the difficulty Validate and normalize Attune to supervisee needs Support Anticipate Explore parallel process Acknowledge mistakes Modeling
 How Supervisors Resolve Difficulties Reflective n. Reflective interventions focused on endeavors to think deeply about and understand difficult supervisee processes with clients and supervisors. n. Reflective interventions were centered predominantly on assisting the supervisee to case conceptualize more deeply and to reflect more profoundly on therapeutic processes or their internal responses. 1. Facilitate reflectivity 2. Remain mindful and monitor 3. Remain patient and transparent 4. Process countertransference 5. Seek supervision on supervision 6. Case conceptualize
How Supervisors Resolve Difficulties Reflective n. Reflective interventions focused on endeavors to think deeply about and understand difficult supervisee processes with clients and supervisors. n. Reflective interventions were centered predominantly on assisting the supervisee to case conceptualize more deeply and to reflect more profoundly on therapeutic processes or their internal responses. 1. Facilitate reflectivity 2. Remain mindful and monitor 3. Remain patient and transparent 4. Process countertransference 5. Seek supervision on supervision 6. Case conceptualize
 How Supervisors Resolve Difficulties Confrontation n. When attempts to address difficulties through reflective or relational strategies were unsuccessful, supervisors typically progressed to more direct and confrontative strategies. n. Confrontative interventions involve challenging the supervisee about some aspect of his or her therapeutic practice or professional behavior. n. Confront tentatively (how do I say this in a way that they can hear it? ) n. Confront directly Withdraw, deny, avoid and then confront q Assess level of directness before confronting (e. g. , developmental level) q Confront but recognize limits of supervision q Use immediacy to confront (what is happening in the moment) n. Refuse or terminate supervision n. Take formal action (progressive discipline) n. Refer to personal therapy n. Become directive (the less competent, the more directive) q
How Supervisors Resolve Difficulties Confrontation n. When attempts to address difficulties through reflective or relational strategies were unsuccessful, supervisors typically progressed to more direct and confrontative strategies. n. Confrontative interventions involve challenging the supervisee about some aspect of his or her therapeutic practice or professional behavior. n. Confront tentatively (how do I say this in a way that they can hear it? ) n. Confront directly Withdraw, deny, avoid and then confront q Assess level of directness before confronting (e. g. , developmental level) q Confront but recognize limits of supervision q Use immediacy to confront (what is happening in the moment) n. Refuse or terminate supervision n. Take formal action (progressive discipline) n. Refer to personal therapy n. Become directive (the less competent, the more directive) q
 How Supervisors Resolve Difficulties Avoidant Strategies n. Avoidant strategies are usually the least frequently reported approach, where supervisors refrained from raising difficult issues. n. Avoidance was mainly used to manage unhelpful supervisee characteristics and professional issues that were deemed too entrenched to change. n. Another example was when time for supervision was very limited, supervisors avoided difficult issues because they did not believe the supervisee could “hear” or benefit from such discussion; 1. “Struggle on” and await external intervention 2. Withhold 3. Withdraw, ignore, or deny
How Supervisors Resolve Difficulties Avoidant Strategies n. Avoidant strategies are usually the least frequently reported approach, where supervisors refrained from raising difficult issues. n. Avoidance was mainly used to manage unhelpful supervisee characteristics and professional issues that were deemed too entrenched to change. n. Another example was when time for supervision was very limited, supervisors avoided difficult issues because they did not believe the supervisee could “hear” or benefit from such discussion; 1. “Struggle on” and await external intervention 2. Withhold 3. Withdraw, ignore, or deny
 Managing Difficult Staff 1. Don't generalize – be very clear about what the problems and symptoms are. Some individuals simply aren't up to the job, and would benefit from being helped to find a position that better suits their talents. Others may have a clash of personalities with an immediate superior. The first response to a troublemaker has to be, "I need more information". Use cost-benefit analysis - take the time to assess just what are the costs to the organization of this individual, including the cost of any trouble caused. Weigh this up against the benefits brought to the organization by that individual. Only then can you decide on the appropriate course to take.
Managing Difficult Staff 1. Don't generalize – be very clear about what the problems and symptoms are. Some individuals simply aren't up to the job, and would benefit from being helped to find a position that better suits their talents. Others may have a clash of personalities with an immediate superior. The first response to a troublemaker has to be, "I need more information". Use cost-benefit analysis - take the time to assess just what are the costs to the organization of this individual, including the cost of any trouble caused. Weigh this up against the benefits brought to the organization by that individual. Only then can you decide on the appropriate course to take.
 Managing Difficult Staff 2. Don't try to change Inherent behavior. Assuming that giving a difficult staff member more attention would change deeply rooted behavior. If someone is persistently cynical, negative and disruptive in their job, it is more helpful to them, to you and to their colleagues if you help them to find a different role. 3. See the problem through their eyes-people are often called troublemakers because their reactions seem unreasonable. Take the time to see the problem through their eyes. You might not change things, but you will often find that they are reasonable people with a real concern that needs addressing.
Managing Difficult Staff 2. Don't try to change Inherent behavior. Assuming that giving a difficult staff member more attention would change deeply rooted behavior. If someone is persistently cynical, negative and disruptive in their job, it is more helpful to them, to you and to their colleagues if you help them to find a different role. 3. See the problem through their eyes-people are often called troublemakers because their reactions seem unreasonable. Take the time to see the problem through their eyes. You might not change things, but you will often find that they are reasonable people with a real concern that needs addressing.
 Managing Difficult Staff 4. Don't confuse Input and output. It is easy to push highly talented people into troublemaker mode by trying to control the way they do their jobs. If you focus on micro-managing style, timekeeping, looking neat and having tidy desks rather than quality and timeliness of output, it is easy to alienate staff members who are often hugely productive. Make it clear when you expect specific standards (being on time for meetings, need for paperwork being finished), but then give supervisees as much leeway as you can in day-to-day work practices. Focus on what they produce, not how they produce it (as long as how they produce it is ethical and legal). This approach can transform some troublemakers into top workers.
Managing Difficult Staff 4. Don't confuse Input and output. It is easy to push highly talented people into troublemaker mode by trying to control the way they do their jobs. If you focus on micro-managing style, timekeeping, looking neat and having tidy desks rather than quality and timeliness of output, it is easy to alienate staff members who are often hugely productive. Make it clear when you expect specific standards (being on time for meetings, need for paperwork being finished), but then give supervisees as much leeway as you can in day-to-day work practices. Focus on what they produce, not how they produce it (as long as how they produce it is ethical and legal). This approach can transform some troublemakers into top workers.
 Managing Difficult Staff Exercise n n n In small groups, I would like you to come up with a problem case that somebody is currently dealing with regarding a difficult staff. If no current problem exists, then make it a previous problem. I would like you to then brainstorm for this person as to the possibilities for resolving this situation. Have one person act as the secretary and write down brainstorming ideas. This person will describe the current (or recent past) problem (changing the names to protect the stupid), and this person will describe the solutions that the group came up with in the brainstorming section.
Managing Difficult Staff Exercise n n n In small groups, I would like you to come up with a problem case that somebody is currently dealing with regarding a difficult staff. If no current problem exists, then make it a previous problem. I would like you to then brainstorm for this person as to the possibilities for resolving this situation. Have one person act as the secretary and write down brainstorming ideas. This person will describe the current (or recent past) problem (changing the names to protect the stupid), and this person will describe the solutions that the group came up with in the brainstorming section.
 The Impaired Clinician n n Although the emotional functioning of a clinician should be a concern for all disciplines, the impaired clinician is a particular concern in all counseling related fields. The supervisor plays a critical role in the identification and referral of the impaired professional. Yet all too often the helping professions deny it when their own peers act in an impaired manner. This downward spiral can be averted if the supervisor intervenes in the early phases of the noticed impairment(s), identifying job performance impairment as it evolves. The final stage of discipline and potential termination is often used as one of the first intervention methods, this is due to poor supervision of the impaired employee and/or anxiety surrounding dealing with the issue when it first came up.
The Impaired Clinician n n Although the emotional functioning of a clinician should be a concern for all disciplines, the impaired clinician is a particular concern in all counseling related fields. The supervisor plays a critical role in the identification and referral of the impaired professional. Yet all too often the helping professions deny it when their own peers act in an impaired manner. This downward spiral can be averted if the supervisor intervenes in the early phases of the noticed impairment(s), identifying job performance impairment as it evolves. The final stage of discipline and potential termination is often used as one of the first intervention methods, this is due to poor supervision of the impaired employee and/or anxiety surrounding dealing with the issue when it first came up.
 The Impaired Clinician n n Impairment may involve failure to provide competent care or violation of a licensee’s ethical standards. It also may take such forms as providing flawed or inferior services, sexual involvement with a client, or failure to carry out professional duties as a result of substance abuse or mental illness (Lamb et al. , 1987). Such impairment may be the result of a wide range of factors, such as employment stress, illness or death of family members, marital or relationship problems, financial difficulties, midlife crises, personal physical or mental health problems, legal problems, and substance abuse.
The Impaired Clinician n n Impairment may involve failure to provide competent care or violation of a licensee’s ethical standards. It also may take such forms as providing flawed or inferior services, sexual involvement with a client, or failure to carry out professional duties as a result of substance abuse or mental illness (Lamb et al. , 1987). Such impairment may be the result of a wide range of factors, such as employment stress, illness or death of family members, marital or relationship problems, financial difficulties, midlife crises, personal physical or mental health problems, legal problems, and substance abuse.
 The Impaired Clinician – Substance Use n One of the most common impairment issues that is dealt with supervisees is impairment due to substance abuse. What should the agency and supervisor do if a clinician is thought to be abusing substances? n n n First, the agency should have a substance abuse policy in place. This policy, developed in consultation with legal counsel, should specify what substances it covers, what the policy is on substance use, and what the progressive disciplinary response will be to substance abuse on the job. The policy must not discriminate against the practitioner in recovery by imposing a stricter standard on those who have disclosed their recovery history. If abuse is found, as soon as the problem is identified, the practitioner should be taken out of counseling functions immediately. However, how long should they stay out of counseling functions?
The Impaired Clinician – Substance Use n One of the most common impairment issues that is dealt with supervisees is impairment due to substance abuse. What should the agency and supervisor do if a clinician is thought to be abusing substances? n n n First, the agency should have a substance abuse policy in place. This policy, developed in consultation with legal counsel, should specify what substances it covers, what the policy is on substance use, and what the progressive disciplinary response will be to substance abuse on the job. The policy must not discriminate against the practitioner in recovery by imposing a stricter standard on those who have disclosed their recovery history. If abuse is found, as soon as the problem is identified, the practitioner should be taken out of counseling functions immediately. However, how long should they stay out of counseling functions?
 Title 45 – Uniform Enforcement Act – Duty to Report n 45: 1 -37 Notification to division of impairment of health care professional. A health care professional shall promptly notify the division if that health care professional is in possession of information which reasonably indicates that another health care professional has demonstrated an impairment, gross incompetence or unprofessional conduct which would present an imminent danger to an individual patient or to the public health, safety or welfare. A health care professional who fails to so notify the division is subject to disciplinary action and civil penalties pursuant to sections 8, 9 and 12 of P. L. 1978, c. 73 (C. 45: 1 -21, 45: 1 -22 and 45: 1 -25). B. A health care professional shall be deemed to have satisfied the reporting requirement concerning another health care professional's impairment by promptly providing notice to the division, the board or a professional assistance or intervention program approved or designated by the division or a board to provide confidential oversight of the licensee.
Title 45 – Uniform Enforcement Act – Duty to Report n 45: 1 -37 Notification to division of impairment of health care professional. A health care professional shall promptly notify the division if that health care professional is in possession of information which reasonably indicates that another health care professional has demonstrated an impairment, gross incompetence or unprofessional conduct which would present an imminent danger to an individual patient or to the public health, safety or welfare. A health care professional who fails to so notify the division is subject to disciplinary action and civil penalties pursuant to sections 8, 9 and 12 of P. L. 1978, c. 73 (C. 45: 1 -21, 45: 1 -22 and 45: 1 -25). B. A health care professional shall be deemed to have satisfied the reporting requirement concerning another health care professional's impairment by promptly providing notice to the division, the board or a professional assistance or intervention program approved or designated by the division or a board to provide confidential oversight of the licensee.
 Title 45 – Uniform Enforcement Act – Duty to Report n C. 45: 1 -37 Notification to division of impairment of health care professional. (1) There shall be no private right of action against a health care professional for failure to comply with the notification requirements of this section. (2) There shall be no private right of action against a health care entity if a health care professional who is employed by, under contract to render professional services to, or has privileges granted by, that health care entity, or who provides such services pursuant to an agreement with a health care services firm or staffing registry, fails to comply with the notification requirements of this section. D. A health care professional who provides notification to the division, board or review panel, in good faith and without malice, about a health care professional who is impaired or grossly incompetent or who has demonstrated unprofessional conduct, pursuant to this section, is not liable for civil damages to any person in any cause of action arising out of the notification.
Title 45 – Uniform Enforcement Act – Duty to Report n C. 45: 1 -37 Notification to division of impairment of health care professional. (1) There shall be no private right of action against a health care professional for failure to comply with the notification requirements of this section. (2) There shall be no private right of action against a health care entity if a health care professional who is employed by, under contract to render professional services to, or has privileges granted by, that health care entity, or who provides such services pursuant to an agreement with a health care services firm or staffing registry, fails to comply with the notification requirements of this section. D. A health care professional who provides notification to the division, board or review panel, in good faith and without malice, about a health care professional who is impaired or grossly incompetent or who has demonstrated unprofessional conduct, pursuant to this section, is not liable for civil damages to any person in any cause of action arising out of the notification.
 Title 45 – Uniform Enforcement Act – Duty to Report n E. 45: 1 -37 Notification to division of impairment of health care professional. Notwithstanding the provisions of this section to the contrary, a health care professional is not required to provide notification pursuant to this section about an impaired or incompetent health care professional if the health care professional's knowledge of the other health care professional's impairment or incompetence was obtained as a result of rendering treatment to that health care professional.
Title 45 – Uniform Enforcement Act – Duty to Report n E. 45: 1 -37 Notification to division of impairment of health care professional. Notwithstanding the provisions of this section to the contrary, a health care professional is not required to provide notification pursuant to this section about an impaired or incompetent health care professional if the health care professional's knowledge of the other health care professional's impairment or incompetence was obtained as a result of rendering treatment to that health care professional.
 Title 45 – Uniform Enforcement Act – Acts which could cause Committee action n n A. B. C. D. 45: 1 -21 Refusal to license or renew, grounds. A board may refuse to admit a person to an examination or may refuse to issue or may suspend or revoke any certificate, registration or license issued by the board upon proof that the applicant or holder of such certificate, registration or license: Has obtained a certificate, registration, license or authorization to sit for an examination, as the case may be, through fraud, deception, or misrepresentation; Has engaged in the use or employment of dishonesty, fraud, deception, misrepresentation, false promise or false pretense; Has engaged in gross negligence, gross malpractice or gross incompetence which damaged or endangered the life, health, welfare, safety or property of any person; Has engaged in repeated acts of negligence, malpractice or incompetence;
Title 45 – Uniform Enforcement Act – Acts which could cause Committee action n n A. B. C. D. 45: 1 -21 Refusal to license or renew, grounds. A board may refuse to admit a person to an examination or may refuse to issue or may suspend or revoke any certificate, registration or license issued by the board upon proof that the applicant or holder of such certificate, registration or license: Has obtained a certificate, registration, license or authorization to sit for an examination, as the case may be, through fraud, deception, or misrepresentation; Has engaged in the use or employment of dishonesty, fraud, deception, misrepresentation, false promise or false pretense; Has engaged in gross negligence, gross malpractice or gross incompetence which damaged or endangered the life, health, welfare, safety or property of any person; Has engaged in repeated acts of negligence, malpractice or incompetence;
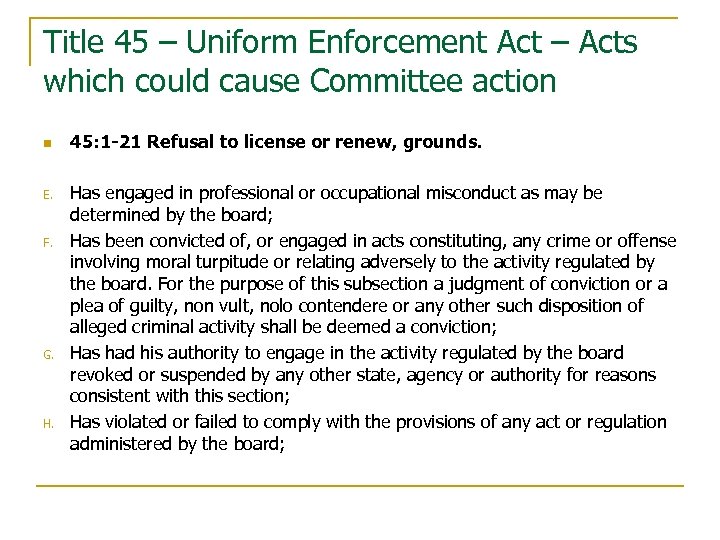 Title 45 – Uniform Enforcement Act – Acts which could cause Committee action n E. F. G. H. 45: 1 -21 Refusal to license or renew, grounds. Has engaged in professional or occupational misconduct as may be determined by the board; Has been convicted of, or engaged in acts constituting, any crime or offense involving moral turpitude or relating adversely to the activity regulated by the board. For the purpose of this subsection a judgment of conviction or a plea of guilty, non vult, nolo contendere or any other such disposition of alleged criminal activity shall be deemed a conviction; Has had his authority to engage in the activity regulated by the board revoked or suspended by any other state, agency or authority for reasons consistent with this section; Has violated or failed to comply with the provisions of any act or regulation administered by the board;
Title 45 – Uniform Enforcement Act – Acts which could cause Committee action n E. F. G. H. 45: 1 -21 Refusal to license or renew, grounds. Has engaged in professional or occupational misconduct as may be determined by the board; Has been convicted of, or engaged in acts constituting, any crime or offense involving moral turpitude or relating adversely to the activity regulated by the board. For the purpose of this subsection a judgment of conviction or a plea of guilty, non vult, nolo contendere or any other such disposition of alleged criminal activity shall be deemed a conviction; Has had his authority to engage in the activity regulated by the board revoked or suspended by any other state, agency or authority for reasons consistent with this section; Has violated or failed to comply with the provisions of any act or regulation administered by the board;
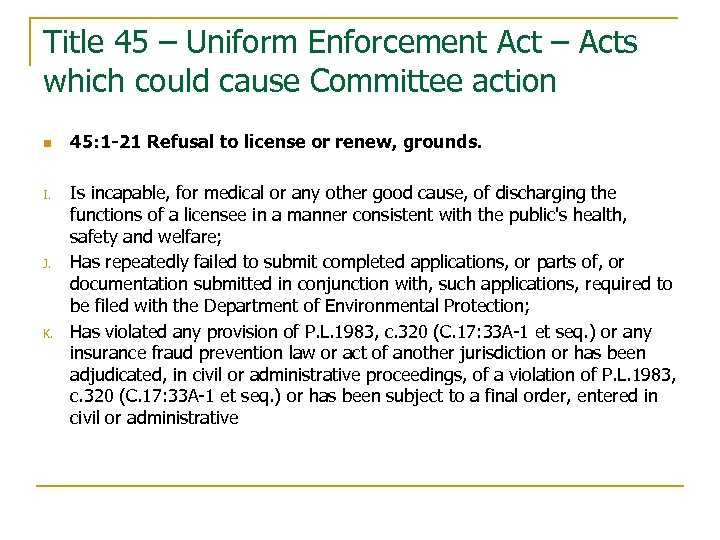 Title 45 – Uniform Enforcement Act – Acts which could cause Committee action n I. J. K. 45: 1 -21 Refusal to license or renew, grounds. Is incapable, for medical or any other good cause, of discharging the functions of a licensee in a manner consistent with the public's health, safety and welfare; Has repeatedly failed to submit completed applications, or parts of, or documentation submitted in conjunction with, such applications, required to be filed with the Department of Environmental Protection; Has violated any provision of P. L. 1983, c. 320 (C. 17: 33 A-1 et seq. ) or any insurance fraud prevention law or act of another jurisdiction or has been adjudicated, in civil or administrative proceedings, of a violation of P. L. 1983, c. 320 (C. 17: 33 A-1 et seq. ) or has been subject to a final order, entered in civil or administrative
Title 45 – Uniform Enforcement Act – Acts which could cause Committee action n I. J. K. 45: 1 -21 Refusal to license or renew, grounds. Is incapable, for medical or any other good cause, of discharging the functions of a licensee in a manner consistent with the public's health, safety and welfare; Has repeatedly failed to submit completed applications, or parts of, or documentation submitted in conjunction with, such applications, required to be filed with the Department of Environmental Protection; Has violated any provision of P. L. 1983, c. 320 (C. 17: 33 A-1 et seq. ) or any insurance fraud prevention law or act of another jurisdiction or has been adjudicated, in civil or administrative proceedings, of a violation of P. L. 1983, c. 320 (C. 17: 33 A-1 et seq. ) or has been subject to a final order, entered in civil or administrative
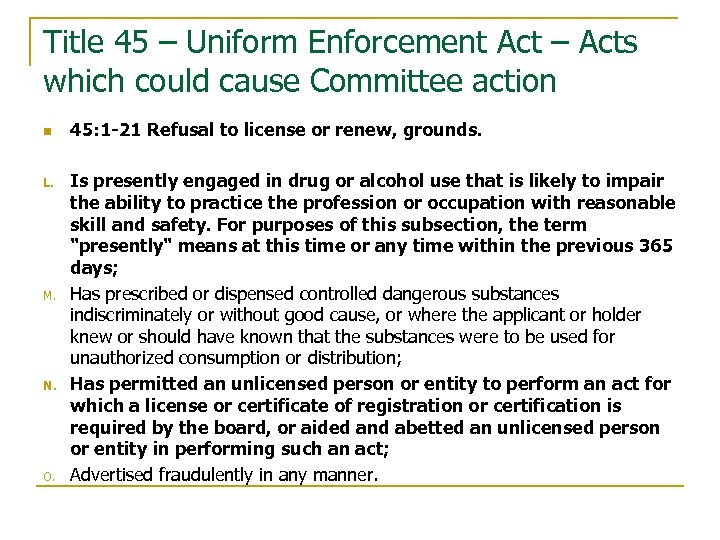 Title 45 – Uniform Enforcement Act – Acts which could cause Committee action n L. M. N. O. 45: 1 -21 Refusal to license or renew, grounds. Is presently engaged in drug or alcohol use that is likely to impair the ability to practice the profession or occupation with reasonable skill and safety. For purposes of this subsection, the term "presently" means at this time or any time within the previous 365 days; Has prescribed or dispensed controlled dangerous substances indiscriminately or without good cause, or where the applicant or holder knew or should have known that the substances were to be used for unauthorized consumption or distribution; Has permitted an unlicensed person or entity to perform an act for which a license or certificate of registration or certification is required by the board, or aided and abetted an unlicensed person or entity in performing such an act; Advertised fraudulently in any manner.
Title 45 – Uniform Enforcement Act – Acts which could cause Committee action n L. M. N. O. 45: 1 -21 Refusal to license or renew, grounds. Is presently engaged in drug or alcohol use that is likely to impair the ability to practice the profession or occupation with reasonable skill and safety. For purposes of this subsection, the term "presently" means at this time or any time within the previous 365 days; Has prescribed or dispensed controlled dangerous substances indiscriminately or without good cause, or where the applicant or holder knew or should have known that the substances were to be used for unauthorized consumption or distribution; Has permitted an unlicensed person or entity to perform an act for which a license or certificate of registration or certification is required by the board, or aided and abetted an unlicensed person or entity in performing such an act; Advertised fraudulently in any manner.
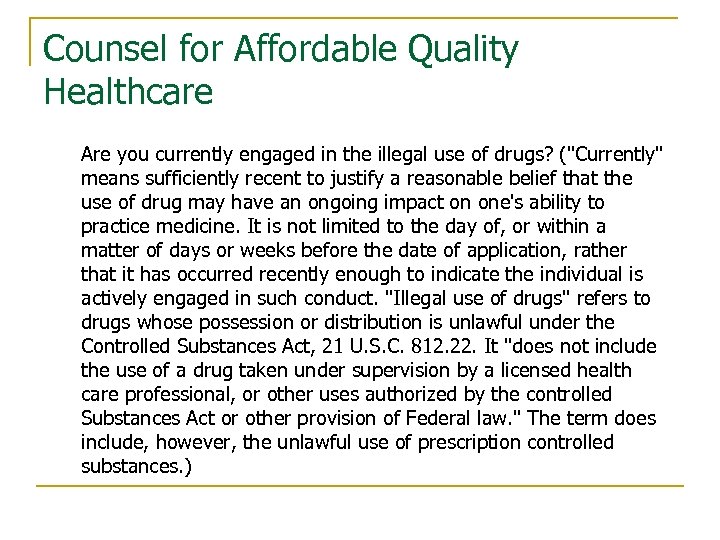 Counsel for Affordable Quality Healthcare Are you currently engaged in the illegal use of drugs? ("Currently" means sufficiently recent to justify a reasonable belief that the use of drug may have an ongoing impact on one's ability to practice medicine. It is not limited to the day of, or within a matter of days or weeks before the date of application, rather that it has occurred recently enough to indicate the individual is actively engaged in such conduct. "Illegal use of drugs" refers to drugs whose possession or distribution is unlawful under the Controlled Substances Act, 21 U. S. C. 812. 22. It "does not include the use of a drug taken under supervision by a licensed health care professional, or other uses authorized by the controlled Substances Act or other provision of Federal law. " The term does include, however, the unlawful use of prescription controlled substances. )
Counsel for Affordable Quality Healthcare Are you currently engaged in the illegal use of drugs? ("Currently" means sufficiently recent to justify a reasonable belief that the use of drug may have an ongoing impact on one's ability to practice medicine. It is not limited to the day of, or within a matter of days or weeks before the date of application, rather that it has occurred recently enough to indicate the individual is actively engaged in such conduct. "Illegal use of drugs" refers to drugs whose possession or distribution is unlawful under the Controlled Substances Act, 21 U. S. C. 812. 22. It "does not include the use of a drug taken under supervision by a licensed health care professional, or other uses authorized by the controlled Substances Act or other provision of Federal law. " The term does include, however, the unlawful use of prescription controlled substances. )
 What constitutes supervisee impairment? “Impairment refers to the inability of professionals to fulfill the minimal responsibilities of their profession because of a mental or physical disability. ” (Knapp & Vandecreek, 1997). 3 broad aspects of professional functioning that constitute competence as professional functioning that include: 1) competence 2) knowledge and skill 3) personal suitability to maintain a mental health role 1. An inability or unwillingness to acquire and integrate professional standards into one’s repertoire of professional behavior. 2. An inability to acquire professional skills and reach an accepted level of competency. 3. An inability to control personal stress, psychological dysfunction, or emotional reactions that may affect professional functioning.
What constitutes supervisee impairment? “Impairment refers to the inability of professionals to fulfill the minimal responsibilities of their profession because of a mental or physical disability. ” (Knapp & Vandecreek, 1997). 3 broad aspects of professional functioning that constitute competence as professional functioning that include: 1) competence 2) knowledge and skill 3) personal suitability to maintain a mental health role 1. An inability or unwillingness to acquire and integrate professional standards into one’s repertoire of professional behavior. 2. An inability to acquire professional skills and reach an accepted level of competency. 3. An inability to control personal stress, psychological dysfunction, or emotional reactions that may affect professional functioning.
 Impaired Employee Vignette Mark is an LCSW and works for you as your per diem counselor, seeing clients individually and in group every Monday and Wednesday nights. It has been brought to your attention by other staff that Mark has been smelling of alcohol over the past week. You then check this out for yourself on Wednesday when Mark comes in and there is a distinct smell … of something. You’re unsure as to whether or not the smell is alcohol or mouthwash, or some evil concoction of both. Work performance has been relatively steady, except with paperwork being more behind than usual. Mark is about to start a group therapy session in 1 hour, but his client that was due in now has called to cancel. What do you do immediately? If you decide to take action, how do you handle Mark’s suspected drinking? What things shouldn’t you say?
Impaired Employee Vignette Mark is an LCSW and works for you as your per diem counselor, seeing clients individually and in group every Monday and Wednesday nights. It has been brought to your attention by other staff that Mark has been smelling of alcohol over the past week. You then check this out for yourself on Wednesday when Mark comes in and there is a distinct smell … of something. You’re unsure as to whether or not the smell is alcohol or mouthwash, or some evil concoction of both. Work performance has been relatively steady, except with paperwork being more behind than usual. Mark is about to start a group therapy session in 1 hour, but his client that was due in now has called to cancel. What do you do immediately? If you decide to take action, how do you handle Mark’s suspected drinking? What things shouldn’t you say?
 Impaired Employee Vignette You’ve made all the right choices, Mark admits to his drinking problem, decides to go to inpatient treatment, which his insurance will allow 14 days of inpatient treatment. Those two weeks have passed, and Mark is now back at your doorstep, wanting to come back to work. He stated he is going to AA meetings, and is now reengaged in outpatient counseling. Can Mark come back to work, and if so, in what capacity? If you determine he cannot come back and counsel right away, what do you do with Mark, and more importantly, what are your determining criteria for his being able to go back into a counseling role? What are your rights as an employer to monitor his treatment compliance?
Impaired Employee Vignette You’ve made all the right choices, Mark admits to his drinking problem, decides to go to inpatient treatment, which his insurance will allow 14 days of inpatient treatment. Those two weeks have passed, and Mark is now back at your doorstep, wanting to come back to work. He stated he is going to AA meetings, and is now reengaged in outpatient counseling. Can Mark come back to work, and if so, in what capacity? If you determine he cannot come back and counsel right away, what do you do with Mark, and more importantly, what are your determining criteria for his being able to go back into a counseling role? What are your rights as an employer to monitor his treatment compliance?
 Impaired Employee Vignette Mark appears to not be drinking, however his work performance is suffering in many areas. As part of your EAP monitoring of Mark, he admits to you that he also suffers from clinical depression, is under psychiatric care, and is compliant with his medication regime. His work has been sloppy in many areas, and he has caused others to do extra work because of this poor performance. What is your next step with Mark?
Impaired Employee Vignette Mark appears to not be drinking, however his work performance is suffering in many areas. As part of your EAP monitoring of Mark, he admits to you that he also suffers from clinical depression, is under psychiatric care, and is compliant with his medication regime. His work has been sloppy in many areas, and he has caused others to do extra work because of this poor performance. What is your next step with Mark?
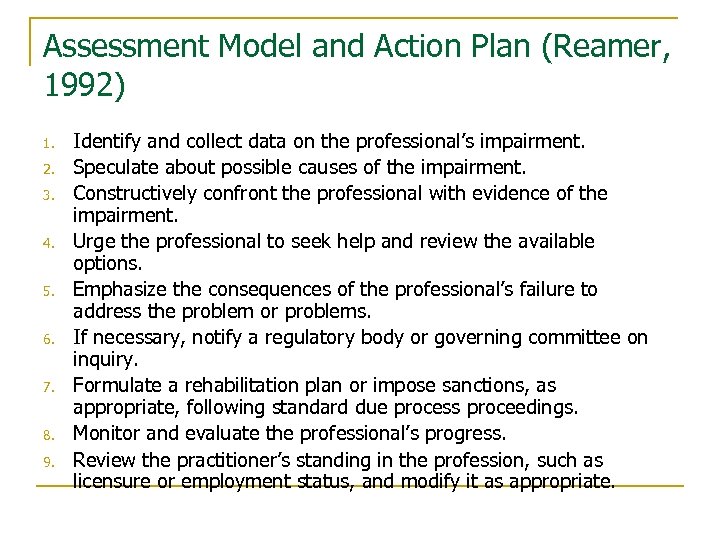 Assessment Model and Action Plan (Reamer, 1992) 1. 2. 3. 4. 5. 6. 7. 8. 9. Identify and collect data on the professional’s impairment. Speculate about possible causes of the impairment. Constructively confront the professional with evidence of the impairment. Urge the professional to seek help and review the available options. Emphasize the consequences of the professional’s failure to address the problem or problems. If necessary, notify a regulatory body or governing committee on inquiry. Formulate a rehabilitation plan or impose sanctions, as appropriate, following standard due process proceedings. Monitor and evaluate the professional’s progress. Review the practitioner’s standing in the profession, such as licensure or employment status, and modify it as appropriate.
Assessment Model and Action Plan (Reamer, 1992) 1. 2. 3. 4. 5. 6. 7. 8. 9. Identify and collect data on the professional’s impairment. Speculate about possible causes of the impairment. Constructively confront the professional with evidence of the impairment. Urge the professional to seek help and review the available options. Emphasize the consequences of the professional’s failure to address the problem or problems. If necessary, notify a regulatory body or governing committee on inquiry. Formulate a rehabilitation plan or impose sanctions, as appropriate, following standard due process proceedings. Monitor and evaluate the professional’s progress. Review the practitioner’s standing in the profession, such as licensure or employment status, and modify it as appropriate.
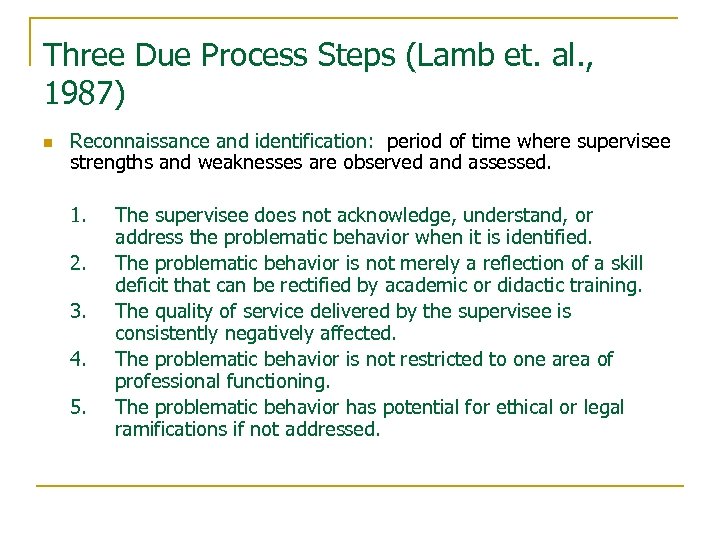 Three Due Process Steps (Lamb et. al. , 1987) n Reconnaissance and identification: period of time where supervisee strengths and weaknesses are observed and assessed. 1. 2. 3. 4. 5. The supervisee does not acknowledge, understand, or address the problematic behavior when it is identified. The problematic behavior is not merely a reflection of a skill deficit that can be rectified by academic or didactic training. The quality of service delivered by the supervisee is consistently negatively affected. The problematic behavior is not restricted to one area of professional functioning. The problematic behavior has potential for ethical or legal ramifications if not addressed.
Three Due Process Steps (Lamb et. al. , 1987) n Reconnaissance and identification: period of time where supervisee strengths and weaknesses are observed and assessed. 1. 2. 3. 4. 5. The supervisee does not acknowledge, understand, or address the problematic behavior when it is identified. The problematic behavior is not merely a reflection of a skill deficit that can be rectified by academic or didactic training. The quality of service delivered by the supervisee is consistently negatively affected. The problematic behavior is not restricted to one area of professional functioning. The problematic behavior has potential for ethical or legal ramifications if not addressed.
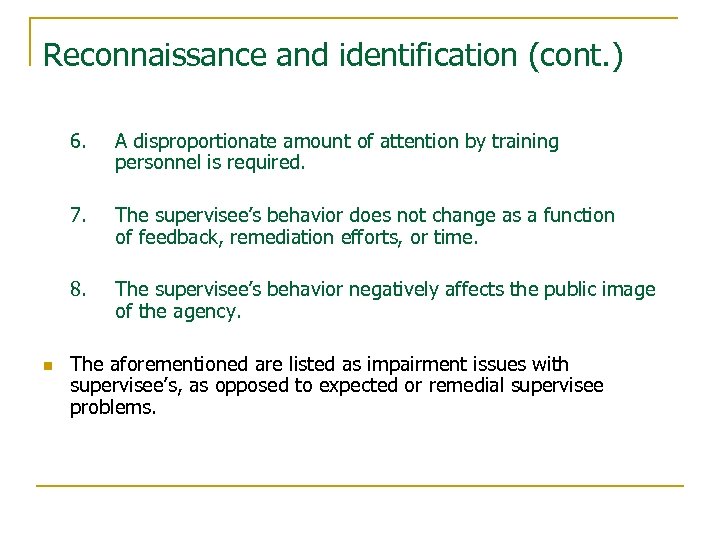 Reconnaissance and identification (cont. ) 6. 7. The supervisee’s behavior does not change as a function of feedback, remediation efforts, or time. 8. n A disproportionate amount of attention by training personnel is required. The supervisee’s behavior negatively affects the public image of the agency. The aforementioned are listed as impairment issues with supervisee’s, as opposed to expected or remedial supervisee problems.
Reconnaissance and identification (cont. ) 6. 7. The supervisee’s behavior does not change as a function of feedback, remediation efforts, or time. 8. n A disproportionate amount of attention by training personnel is required. The supervisee’s behavior negatively affects the public image of the agency. The aforementioned are listed as impairment issues with supervisee’s, as opposed to expected or remedial supervisee problems.
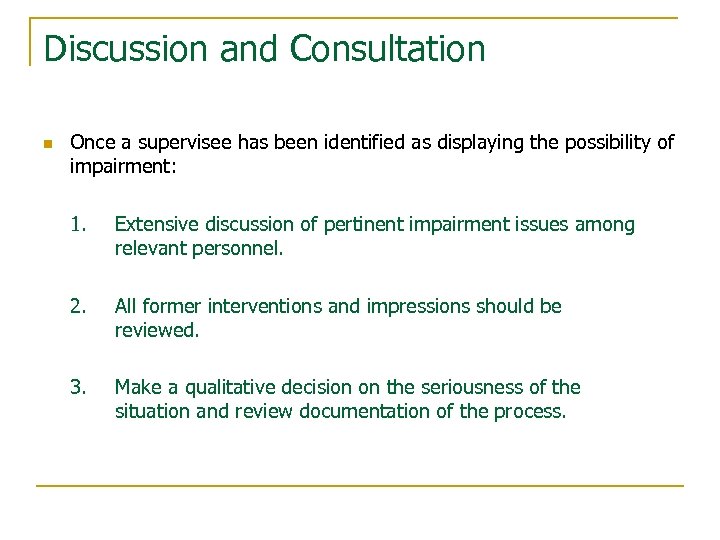 Discussion and Consultation n Once a supervisee has been identified as displaying the possibility of impairment: 1. Extensive discussion of pertinent impairment issues among relevant personnel. 2. All former interventions and impressions should be reviewed. 3. Make a qualitative decision on the seriousness of the situation and review documentation of the process.
Discussion and Consultation n Once a supervisee has been identified as displaying the possibility of impairment: 1. Extensive discussion of pertinent impairment issues among relevant personnel. 2. All former interventions and impressions should be reviewed. 3. Make a qualitative decision on the seriousness of the situation and review documentation of the process.
 Implementation and Review n This is the point of action taken on the supervisee due to behavior and discussion of that behavior. If termination isn’t decided and some probation is mandated, here are some guidelines for what should be included to the supervisee: 1. 2. 3. Identify the specific behaviors or areas of professional functioning that are of concern. Directly relate these behaviors to the written evaluation or written report (e. g. , not showing up for group sessions). Provide several specific ways that these deficiencies can be remediated (e. g. , from additional training to personal therapy).
Implementation and Review n This is the point of action taken on the supervisee due to behavior and discussion of that behavior. If termination isn’t decided and some probation is mandated, here are some guidelines for what should be included to the supervisee: 1. 2. 3. Identify the specific behaviors or areas of professional functioning that are of concern. Directly relate these behaviors to the written evaluation or written report (e. g. , not showing up for group sessions). Provide several specific ways that these deficiencies can be remediated (e. g. , from additional training to personal therapy).
 Probation Guidelines (continued) 4. 5. n Stipulate, if appropriate, how the supervisee’s functioning in the agency will change during the probation period. 6. n Identify a specific probation period after which the performance of the supervisee will be reviewed. Reiterate the due process procedures available to challenge the decision. Anticipating and responding to organizational reaction. Checking with any licensing body as to whether or not this action is reportable.
Probation Guidelines (continued) 4. 5. n Stipulate, if appropriate, how the supervisee’s functioning in the agency will change during the probation period. 6. n Identify a specific probation period after which the performance of the supervisee will be reviewed. Reiterate the due process procedures available to challenge the decision. Anticipating and responding to organizational reaction. Checking with any licensing body as to whether or not this action is reportable.
 Due Process – Staff Grievances n n Supervisors must follow due process guidelines when responding to grievances. Those guidelines are usually found in an organization’s policy and procedure (P&P) manual. Clinical supervisors should ensure the P&P manual complies with both Division of Mental Health standards of care, and licensure standards of care. Supervisors must ensure that supervisees know their rights as employees and understand the organization’s employee grievance procedures. If your organization has an employee handbook, there should be written documentation that the supervisee has received a copy. There should be written documentation that the supervisee has read and understood the organization’s employee grievance P&P.
Due Process – Staff Grievances n n Supervisors must follow due process guidelines when responding to grievances. Those guidelines are usually found in an organization’s policy and procedure (P&P) manual. Clinical supervisors should ensure the P&P manual complies with both Division of Mental Health standards of care, and licensure standards of care. Supervisors must ensure that supervisees know their rights as employees and understand the organization’s employee grievance procedures. If your organization has an employee handbook, there should be written documentation that the supervisee has received a copy. There should be written documentation that the supervisee has read and understood the organization’s employee grievance P&P.
 Bibliography n n n n Bernard, J. M. & Goodyear, R. K. (2013). Fundamentals of Clinical Supervision, 5 th Ed. Allyn and Bacon, Boston, MA. Falvey, J. E. (2002). Managing clinical supervision: Ethical practice and legal risk management. Pacific Groove: Wadsworth Flinders, C. A. & Shafranske, E. P. (2004). Clinical Supervision: A Competency-Based Approach. American Psychological Association, Washington, DC. Glegg, B. (2002). Diffusing the troublemakers, Director, 56(4), 38. Grant, J. , Schofield, M. J. & Crawford, S. (2012). Managing Difficulties in Supervision: Supervisors’ Perspectives. Journal of Counseling Psychology, 59(4), pp. 528 -541. Lamb, D. , Presser, N. , Pfost, K. , Baum, M. , Jackson, R. , & Jarvis, P. (1987). Confronting Professional Impairment During the Internship: Identification, Due Process, and Remediation. Professional Psychology: Research and Practice, 18, pp. 597 -603. Meichenbaum, D. (2001). Treatment of Individuals with Anger-Control Problems and Aggressive Behaviors: A Clinical Handbook. Clearwater, Fl: Institute Press.
Bibliography n n n n Bernard, J. M. & Goodyear, R. K. (2013). Fundamentals of Clinical Supervision, 5 th Ed. Allyn and Bacon, Boston, MA. Falvey, J. E. (2002). Managing clinical supervision: Ethical practice and legal risk management. Pacific Groove: Wadsworth Flinders, C. A. & Shafranske, E. P. (2004). Clinical Supervision: A Competency-Based Approach. American Psychological Association, Washington, DC. Glegg, B. (2002). Diffusing the troublemakers, Director, 56(4), 38. Grant, J. , Schofield, M. J. & Crawford, S. (2012). Managing Difficulties in Supervision: Supervisors’ Perspectives. Journal of Counseling Psychology, 59(4), pp. 528 -541. Lamb, D. , Presser, N. , Pfost, K. , Baum, M. , Jackson, R. , & Jarvis, P. (1987). Confronting Professional Impairment During the Internship: Identification, Due Process, and Remediation. Professional Psychology: Research and Practice, 18, pp. 597 -603. Meichenbaum, D. (2001). Treatment of Individuals with Anger-Control Problems and Aggressive Behaviors: A Clinical Handbook. Clearwater, Fl: Institute Press.
 Bibliography n n Munson, C. E. (2002). Handbook of Clinical Social Work Supervision, 3 rd Ed. New York, Haworth Press, Inc. National Association of Alcoholism and Drug Abuse Counselors. (2011). NAADAC Internet Code of Ethics. http: //www. naadac. org/resources/codeofethics (Accessed on September 6, 2011). New Jersey Uniform Enforcement Act (2005) Printed on the Internet on June, 2011. http: //www. nj. gov/lps/ca/laws/uniformact. pdf (Accessed on September 1, 2001). Powell, D. J. & Brodsky, A. (2004). Clinical Supervision in Alcohol and Drug Abuse Counseling. Jossey-Bass Publishers, San Francisco, CA. n Reamer, F. G. (2000). The social work ethics audit: A risk-management strategy. Social Work. 45(4), 355 -366. n Reamer, F. G. (1992). The impaired social worker. Social Work. 37(2), 165 -170. n Stoltenberg, C. D. , Mc. Neil, B. , & Delworth, U. (1998). IDM Supervision: An Integrated Developmental Model for Supervising Counselors and Therapists. Jossey-Bass Publishers, San Francisco, CA.
Bibliography n n Munson, C. E. (2002). Handbook of Clinical Social Work Supervision, 3 rd Ed. New York, Haworth Press, Inc. National Association of Alcoholism and Drug Abuse Counselors. (2011). NAADAC Internet Code of Ethics. http: //www. naadac. org/resources/codeofethics (Accessed on September 6, 2011). New Jersey Uniform Enforcement Act (2005) Printed on the Internet on June, 2011. http: //www. nj. gov/lps/ca/laws/uniformact. pdf (Accessed on September 1, 2001). Powell, D. J. & Brodsky, A. (2004). Clinical Supervision in Alcohol and Drug Abuse Counseling. Jossey-Bass Publishers, San Francisco, CA. n Reamer, F. G. (2000). The social work ethics audit: A risk-management strategy. Social Work. 45(4), 355 -366. n Reamer, F. G. (1992). The impaired social worker. Social Work. 37(2), 165 -170. n Stoltenberg, C. D. , Mc. Neil, B. , & Delworth, U. (1998). IDM Supervision: An Integrated Developmental Model for Supervising Counselors and Therapists. Jossey-Bass Publishers, San Francisco, CA.
 Bibliography n n Ethical Guidelines - National Association of Social Workers: http: //www. socialworkers. org/pubs/code. asp Ethical Guidelines - LSW/LCSW Code of Ethics: http: //www. state. nj. us/lps/ca/social. pdf Webster. com for the definitions of misfeasance, malfeasance or nonfeasance.
Bibliography n n Ethical Guidelines - National Association of Social Workers: http: //www. socialworkers. org/pubs/code. asp Ethical Guidelines - LSW/LCSW Code of Ethics: http: //www. state. nj. us/lps/ca/social. pdf Webster. com for the definitions of misfeasance, malfeasance or nonfeasance.


