1dcd490318f47844f35593d5340654f9.ppt
- Количество слайдов: 28
 Management of Severe Head Trauma in A&E Dr. David Tran A&E department FVHospital 17 mars 2010
Management of Severe Head Trauma in A&E Dr. David Tran A&E department FVHospital 17 mars 2010
 Management of head injury n Primary survey: ensure that airways, breathing, circulation and cervical spine are secure. n Assessment of mental state (glasgow score adapted to the age) n Alert (A), responds to voive (V), Responds to pain (P), unresponsive (U)
Management of head injury n Primary survey: ensure that airways, breathing, circulation and cervical spine are secure. n Assessment of mental state (glasgow score adapted to the age) n Alert (A), responds to voive (V), Responds to pain (P), unresponsive (U)
 Perform secondary survey n n n Neck & cervical spine (tenderness, muscle spasm) Head: scalp hematoma, laceration, swelling, tenderness… Eyes: pupils size, equality, reactivity Ears: otorrhage, hemotympan Nose, mouth, facial fractures Motor function: limbs, reflexes, lateralised weakness, Babinski’s sign.
Perform secondary survey n n n Neck & cervical spine (tenderness, muscle spasm) Head: scalp hematoma, laceration, swelling, tenderness… Eyes: pupils size, equality, reactivity Ears: otorrhage, hemotympan Nose, mouth, facial fractures Motor function: limbs, reflexes, lateralised weakness, Babinski’s sign.
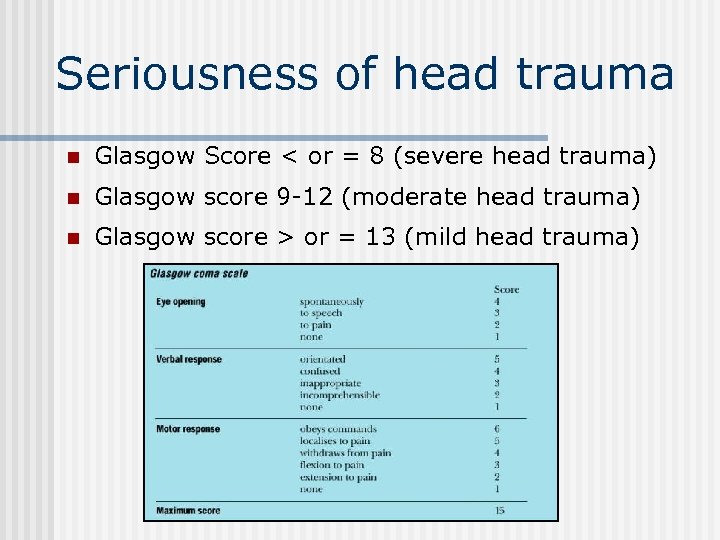 Seriousness of head trauma n Glasgow Score < or = 8 (severe head trauma) n Glasgow score 9 -12 (moderate head trauma) n Glasgow score > or = 13 (mild head trauma)
Seriousness of head trauma n Glasgow Score < or = 8 (severe head trauma) n Glasgow score 9 -12 (moderate head trauma) n Glasgow score > or = 13 (mild head trauma)
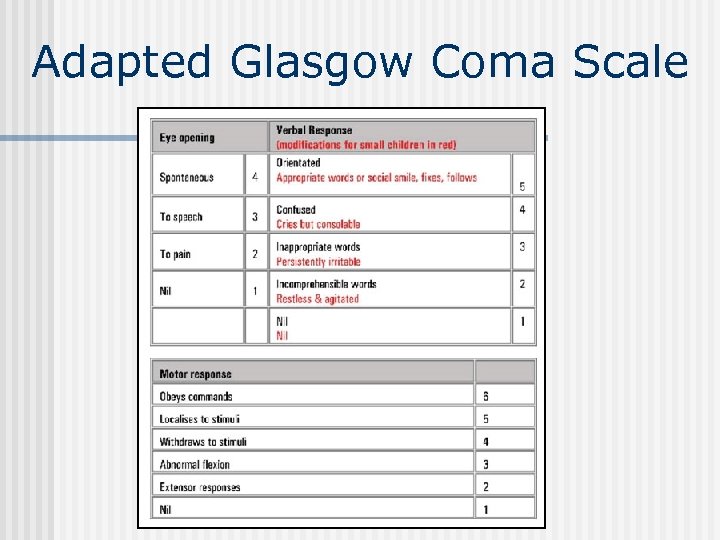 Adapted Glasgow Coma Scale
Adapted Glasgow Coma Scale
 Do not forget neck protection n Severe head trauma are frequently associated with neck injuries. n Those injuries often concern the cervicooccipital region (C 1/C 2) n Neck collar has to be put immediately at arrival in A&E and will be removed only after imaging.
Do not forget neck protection n Severe head trauma are frequently associated with neck injuries. n Those injuries often concern the cervicooccipital region (C 1/C 2) n Neck collar has to be put immediately at arrival in A&E and will be removed only after imaging.
 General management n IV line, use infusion of isotonic solutions* (Na. Cl 0. 9% is the most adapted) n Intubation: all patients with severe head trauma (Glasgow score < or =8) have to be intubated. n Crash induction is the gold standard for management of airways. * Avoid hypotonic solutions like G 5% or Ringer Lactate
General management n IV line, use infusion of isotonic solutions* (Na. Cl 0. 9% is the most adapted) n Intubation: all patients with severe head trauma (Glasgow score < or =8) have to be intubated. n Crash induction is the gold standard for management of airways. * Avoid hypotonic solutions like G 5% or Ringer Lactate
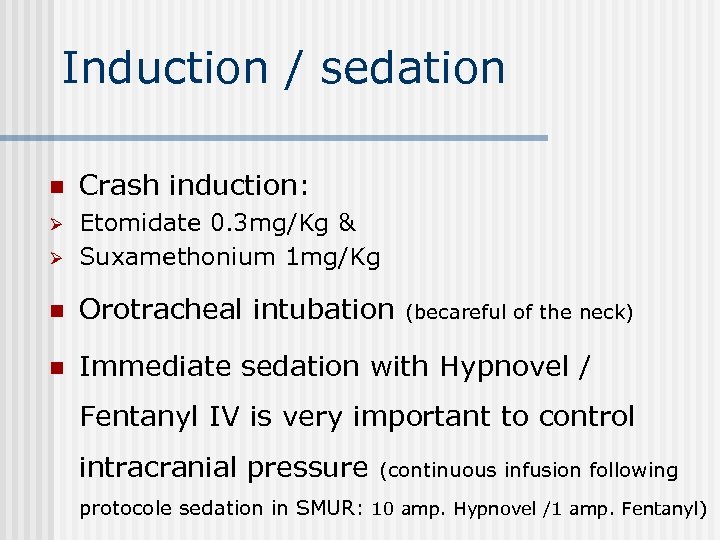 Induction / sedation n Crash induction: Ø Ø Etomidate 0. 3 mg/Kg & Suxamethonium 1 mg/Kg n Orotracheal intubation n Immediate sedation with Hypnovel / (becareful of the neck) Fentanyl IV is very important to control intracranial pressure (continuous infusion following protocole sedation in SMUR: 10 amp. Hypnovel /1 amp. Fentanyl)
Induction / sedation n Crash induction: Ø Ø Etomidate 0. 3 mg/Kg & Suxamethonium 1 mg/Kg n Orotracheal intubation n Immediate sedation with Hypnovel / (becareful of the neck) Fentanyl IV is very important to control intracranial pressure (continuous infusion following protocole sedation in SMUR: 10 amp. Hypnovel /1 amp. Fentanyl)
 Interest of early sedation in case of severe head trauma n Control agitation of the patient n Control of analgesia n Avoid or decrease intra-cranial hypertension. n Adaptation to mechanical ventilation
Interest of early sedation in case of severe head trauma n Control agitation of the patient n Control of analgesia n Avoid or decrease intra-cranial hypertension. n Adaptation to mechanical ventilation
 Monitoring head trauma in A&E n Non invasive blood pressure/15 min n Sp. O 2 n Pulse rate on scope n PCO 2 (if not available, blood gaz during mechanical ventilation)
Monitoring head trauma in A&E n Non invasive blood pressure/15 min n Sp. O 2 n Pulse rate on scope n PCO 2 (if not available, blood gaz during mechanical ventilation)
 Intracranial pressure monitoring (PPC= MAP-ICP) n Each time there is a severe traumatic brain injury (with GCS 3 -8) associated with CT scanner images of hematomas, contusions, swelling, herniation or compressed basal cisterns.
Intracranial pressure monitoring (PPC= MAP-ICP) n Each time there is a severe traumatic brain injury (with GCS 3 -8) associated with CT scanner images of hematomas, contusions, swelling, herniation or compressed basal cisterns.
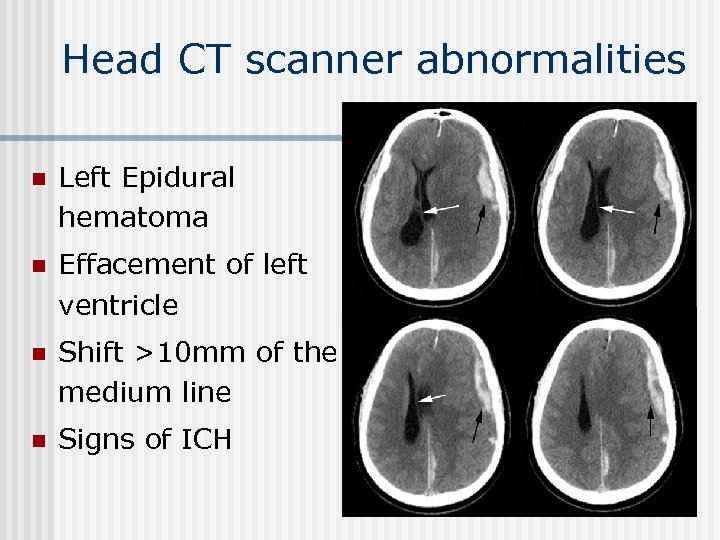 Head CT scanner abnormalities n Left Epidural hematoma n Effacement of left ventricle n Shift >10 mm of the medium line n Signs of ICH
Head CT scanner abnormalities n Left Epidural hematoma n Effacement of left ventricle n Shift >10 mm of the medium line n Signs of ICH
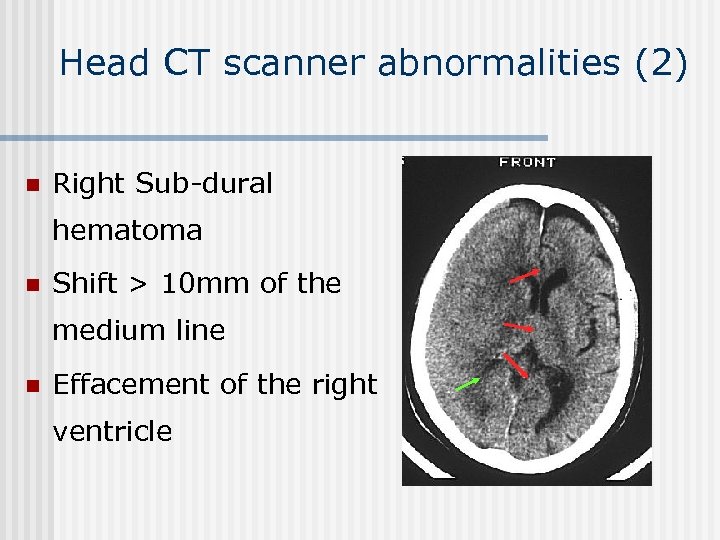 Head CT scanner abnormalities (2) n Right Sub-dural hematoma n Shift > 10 mm of the medium line n Effacement of the right ventricle
Head CT scanner abnormalities (2) n Right Sub-dural hematoma n Shift > 10 mm of the medium line n Effacement of the right ventricle
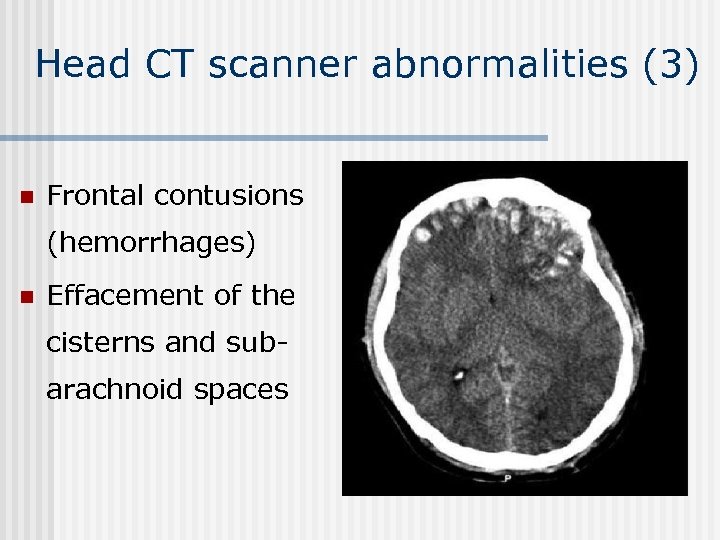 Head CT scanner abnormalities (3) n Frontal contusions (hemorrhages) n Effacement of the cisterns and subarachnoid spaces
Head CT scanner abnormalities (3) n Frontal contusions (hemorrhages) n Effacement of the cisterns and subarachnoid spaces
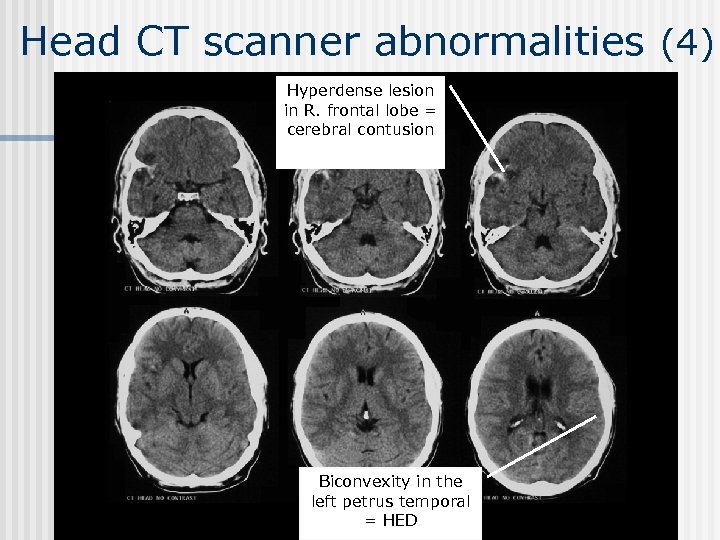 Head CT scanner abnormalities (4) Hyperdense lesion in R. frontal lobe = cerebral contusion Biconvexity in the left petrus temporal = HED
Head CT scanner abnormalities (4) Hyperdense lesion in R. frontal lobe = cerebral contusion Biconvexity in the left petrus temporal = HED
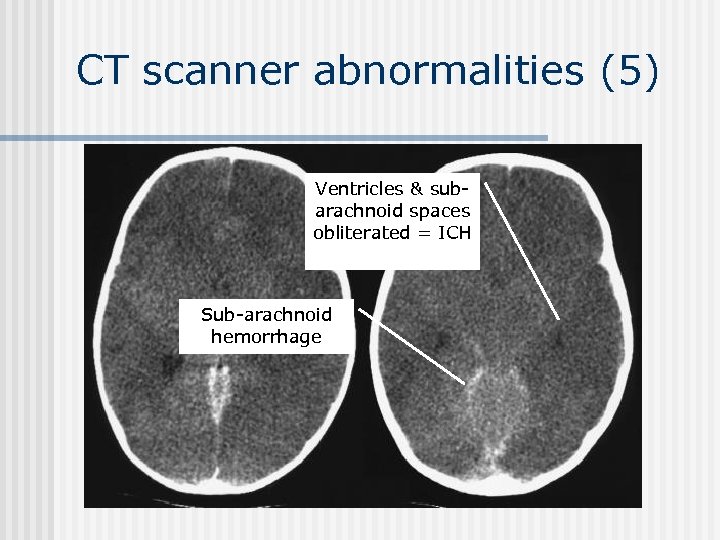 CT scanner abnormalities (5) Ventricles & subarachnoid spaces obliterated = ICH Sub-arachnoid hemorrhage
CT scanner abnormalities (5) Ventricles & subarachnoid spaces obliterated = ICH Sub-arachnoid hemorrhage
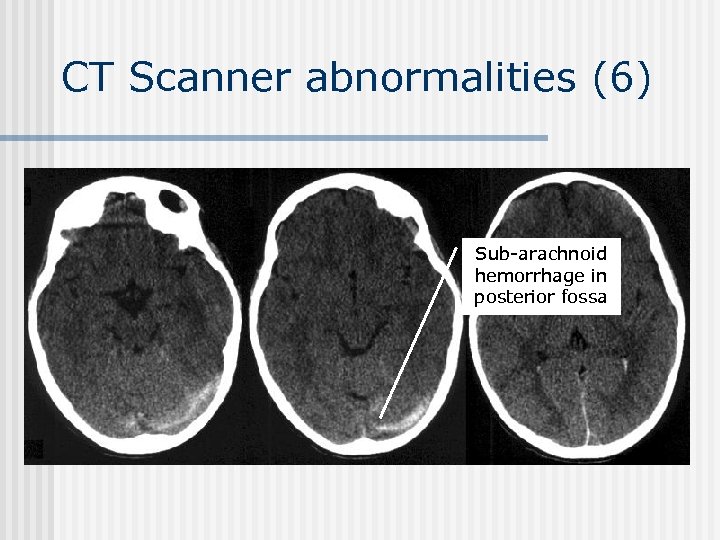 CT Scanner abnormalities (6) Sub-arachnoid hemorrhage in posterior fossa
CT Scanner abnormalities (6) Sub-arachnoid hemorrhage in posterior fossa
 Recommandations n Blood pressure should be monitored and hypotension avoided n (Pas > 90 mm. Hg) Oxygenation should be monitored and hypoxemia avoided (Pa O 2 > 60 mm. Hg Sp. O 2>90%) n Mannitol is effective for control of raised intra-cranial pressure (ICP)
Recommandations n Blood pressure should be monitored and hypotension avoided n (Pas > 90 mm. Hg) Oxygenation should be monitored and hypoxemia avoided (Pa O 2 > 60 mm. Hg Sp. O 2>90%) n Mannitol is effective for control of raised intra-cranial pressure (ICP)
 Signs of intra-cranial hypertension (ICH) n Signs of transtentorial herniation / ICH: anisocoria, mydriasis, neurological lateral signs, seizures, bradycardia, hypertension, bradypnea. n Progressive neurological deterioration not attributable to extra-cranial causes. n Those signs are an indication for immediate use of bolus of Mannitol (up to 1 mg/Kg/20 min. )
Signs of intra-cranial hypertension (ICH) n Signs of transtentorial herniation / ICH: anisocoria, mydriasis, neurological lateral signs, seizures, bradycardia, hypertension, bradypnea. n Progressive neurological deterioration not attributable to extra-cranial causes. n Those signs are an indication for immediate use of bolus of Mannitol (up to 1 mg/Kg/20 min. )
 Use of Mannitol n Indication: Signs of intra cranial hypertension n Mannitol 20 or 25% (20 g/100 ml or 25 g/100 ml) n Bolus 0. 25 to 1 g/Kg/20 min. n Exp: body weight 60 kgs > 15 g to 60 g IV in 20 min. = 100 to 300 ml Mannitol 20%
Use of Mannitol n Indication: Signs of intra cranial hypertension n Mannitol 20 or 25% (20 g/100 ml or 25 g/100 ml) n Bolus 0. 25 to 1 g/Kg/20 min. n Exp: body weight 60 kgs > 15 g to 60 g IV in 20 min. = 100 to 300 ml Mannitol 20%
 Administration of Mannitol n Mannitol is superior to Barbiturates for control of high ICP after TBI. n The osmotic effect of Mannitol is delayed for 15 -30 min. while gradients are established between plasma & cells. n Its effects persist for about 90 min. to several hours.
Administration of Mannitol n Mannitol is superior to Barbiturates for control of high ICP after TBI. n The osmotic effect of Mannitol is delayed for 15 -30 min. while gradients are established between plasma & cells. n Its effects persist for about 90 min. to several hours.
 Use of hypertonic Saline (HS) n Osmotic mobilization of water across blood brain-barrier. (Saline 7, 2% or 10%) n HS as a bolus infusion could be an effective adjuvant to Mannitol to treat ICH. n Potential side effects: central pontic myelinolysis in patient with chronic hyponatremia. n More studies are required to determine the place of HS in the treatment of ICH.
Use of hypertonic Saline (HS) n Osmotic mobilization of water across blood brain-barrier. (Saline 7, 2% or 10%) n HS as a bolus infusion could be an effective adjuvant to Mannitol to treat ICH. n Potential side effects: central pontic myelinolysis in patient with chronic hyponatremia. n More studies are required to determine the place of HS in the treatment of ICH.
 Goals for management of severe head trauma n Any episode of hypotension or hypoxia increases head injury mortality. n Systolic blood pressure > 90 mm. Hg (ideal = SBP 120 mm. Hg & MAP 85 mm. Hg ) n Sp. O 2 > 90% (Pa. O 2> 60 mm. Hg)
Goals for management of severe head trauma n Any episode of hypotension or hypoxia increases head injury mortality. n Systolic blood pressure > 90 mm. Hg (ideal = SBP 120 mm. Hg & MAP 85 mm. Hg ) n Sp. O 2 > 90% (Pa. O 2> 60 mm. Hg)
 Management of severe head trauma in A&E n Neck collar n Monitoring BP, pulse, Sa. O 2 n IV line and fluid infusion (Na. Cl 0. 9%) to restore systolic BP >90 mm. Hg n Intubation (crash induction) and mechanical ventilation. n Immediate sedation after intubation (hypnovel/fentanyl)
Management of severe head trauma in A&E n Neck collar n Monitoring BP, pulse, Sa. O 2 n IV line and fluid infusion (Na. Cl 0. 9%) to restore systolic BP >90 mm. Hg n Intubation (crash induction) and mechanical ventilation. n Immediate sedation after intubation (hypnovel/fentanyl)
 Interest of early CT scanner n CT scanner has to be performed before transfert to neurosurgical center. n The time you spend to perform CT in FVH (<15 min. ) is time you save for the patient later. (timing in CR is probably longer)
Interest of early CT scanner n CT scanner has to be performed before transfert to neurosurgical center. n The time you spend to perform CT in FVH (<15 min. ) is time you save for the patient later. (timing in CR is probably longer)
 Management of imaging n Head CT scanner without injection n Complete by images of cervico-occipital and cervical region. n Chest Xray and Pelvis Xray are systematic n Thorax, abdomen and dorso-lombar rachis CT scanner are requested according clinical signs.
Management of imaging n Head CT scanner without injection n Complete by images of cervico-occipital and cervical region. n Chest Xray and Pelvis Xray are systematic n Thorax, abdomen and dorso-lombar rachis CT scanner are requested according clinical signs.
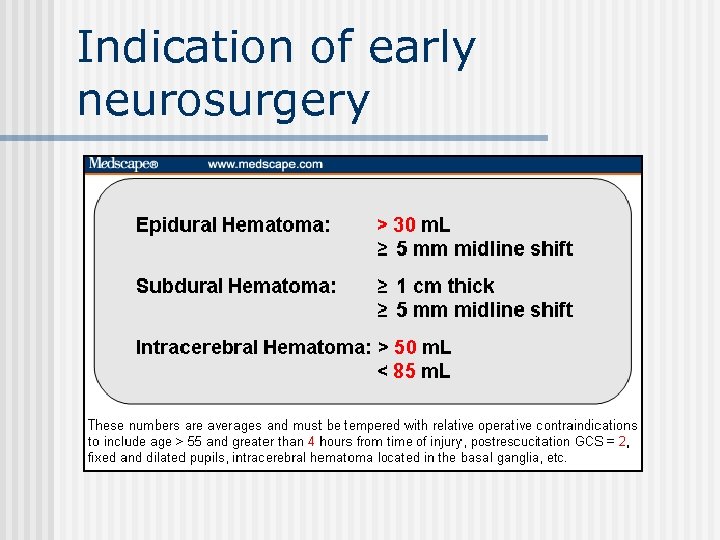 Indication of early neurosurgery
Indication of early neurosurgery
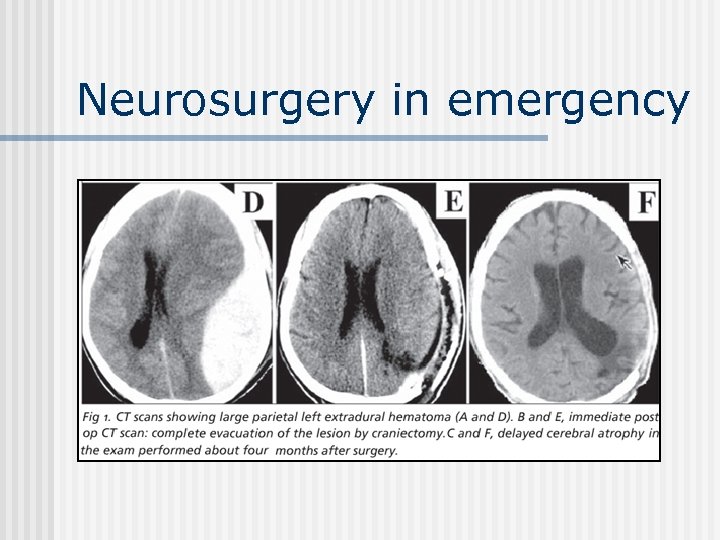 Neurosurgery in emergency
Neurosurgery in emergency


