4f5d3271c142118bad1e391733d577be.ppt
- Количество слайдов: 62

Management of severe burns
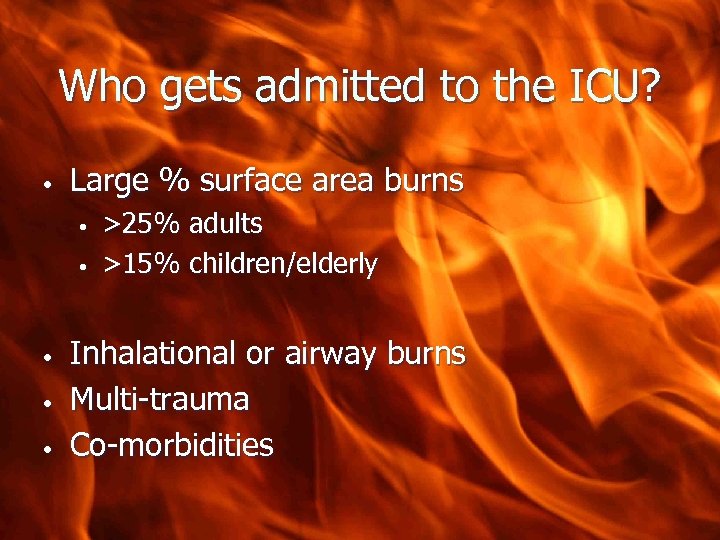
Who gets admitted to the ICU? • Large % surface area burns • • • >25% adults >15% children/elderly Inhalational or airway burns Multi-trauma Co-morbidities
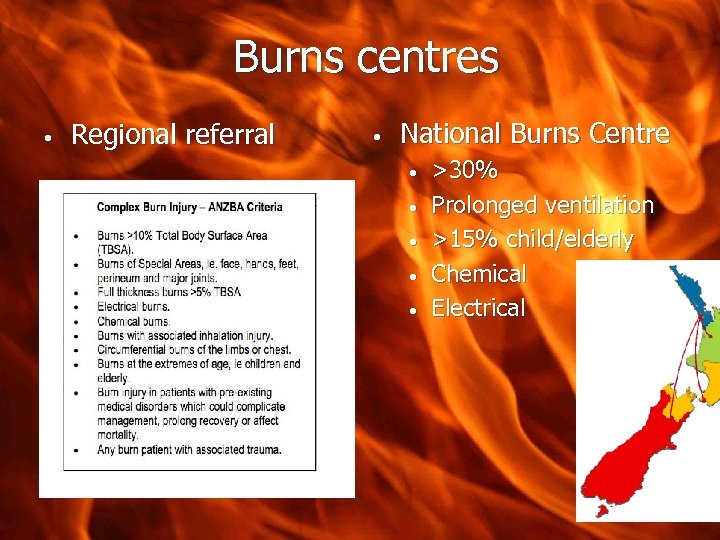
Burns centres • Regional referral • National Burns Centre • • • >30% Prolonged ventilation >15% child/elderly Chemical Electrical

BURN=TRAUMA ultimate distracting injury RX as trauma EMST approach EMSB www. anzba. org. au www. vicburns. org. au • Burn specific care
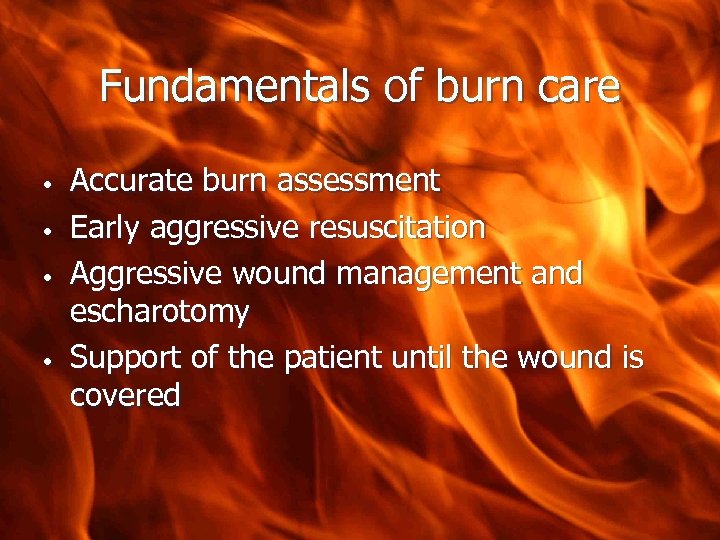
Fundamentals of burn care • • Accurate burn assessment Early aggressive resuscitation Aggressive wound management and escharotomy Support of the patient until the wound is covered
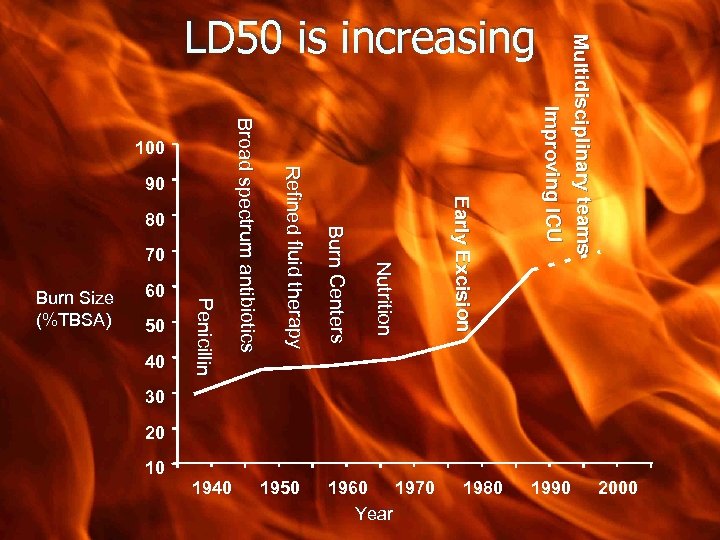
100 Nut r t on Nutriitiion 70 2000 1990 1980 1960 1970 Year E arl y E xci si o n 80 1950 B u rn C e n t e rs 40 1940 R e f n e d f u d t h e ra p y Refiined flluiid therapy 90 Broad spectrum ant b ot cs Broad spectrum antiibiiotiics 50 P en c n Peniiciilllliin 60 Burn Size (%TBSA) 10 Mu l ti d i s c i p l i n a r y te a m s I mp ro vi n g I CU LD 50 is increasing 30 20
Basic First Aid • STOP THE BURNING PROCESS • COOL-running tap water, 20 minutes not of value >3 hours post burn minimise hypothermia • COVER • •
What are the key determinants of burn severity? • Depth Size • Other very important factors • • • Age Co-morbidities First aid Inhalation injury Other injuries
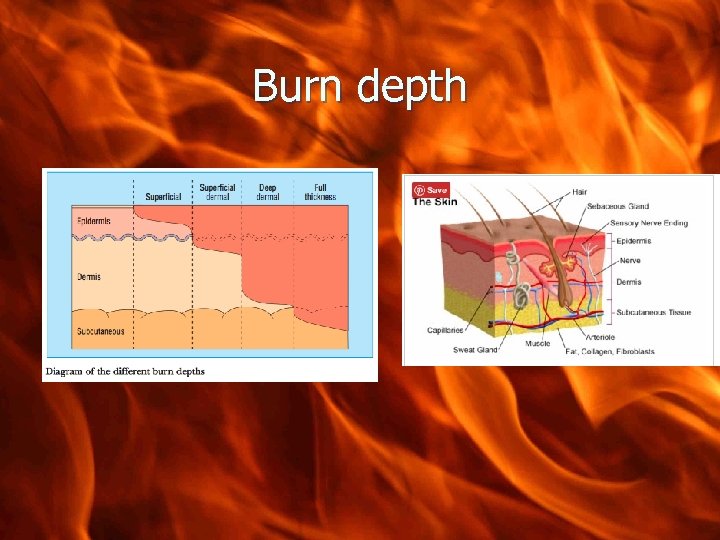
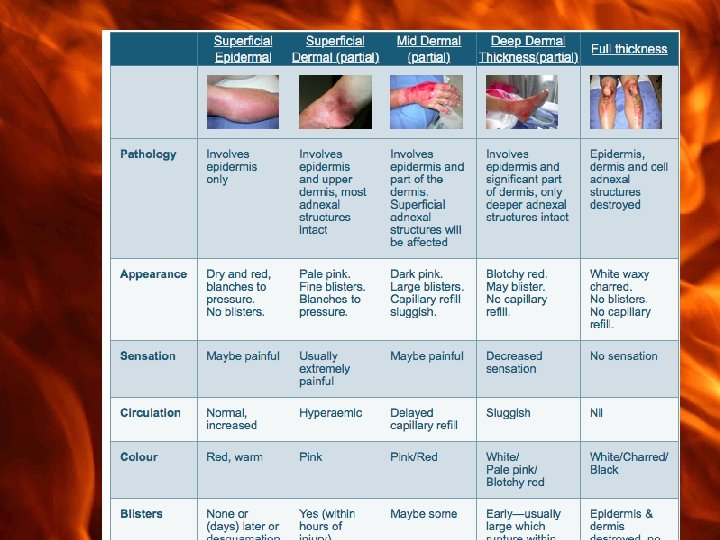
Burn depth
How do you assess burn area? • Rule of 1’s Rule of 9’s Charts • Only count dermal and full thickness burns • •
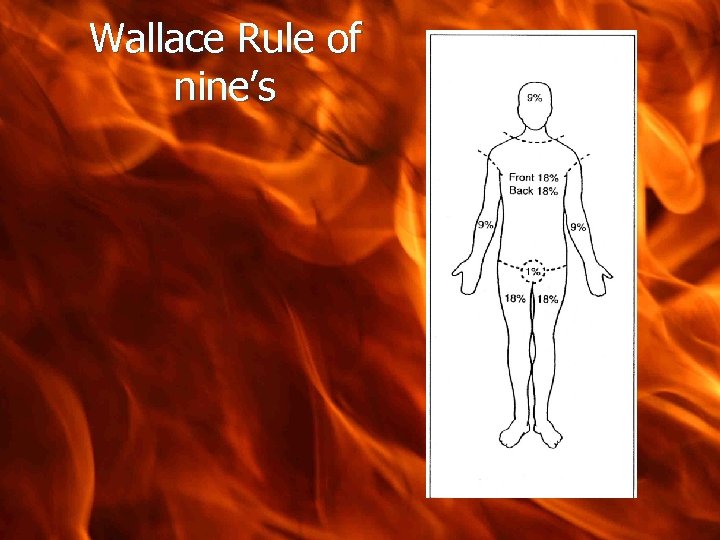
Wallace Rule of nine’s
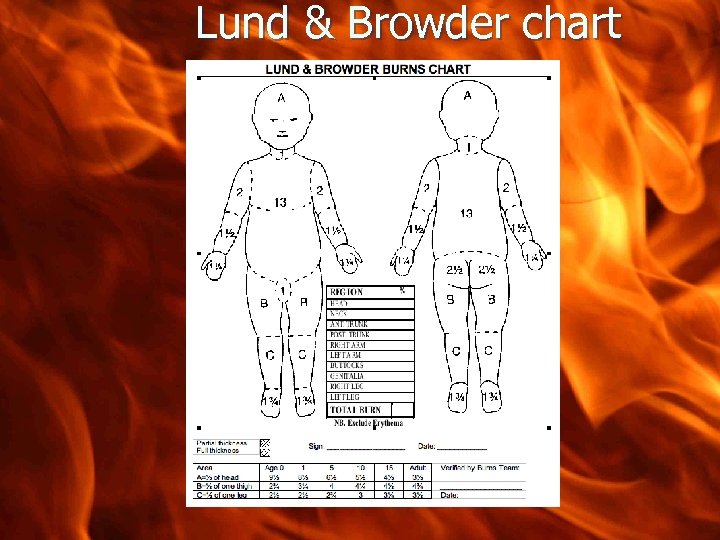
Lund & Browder chart
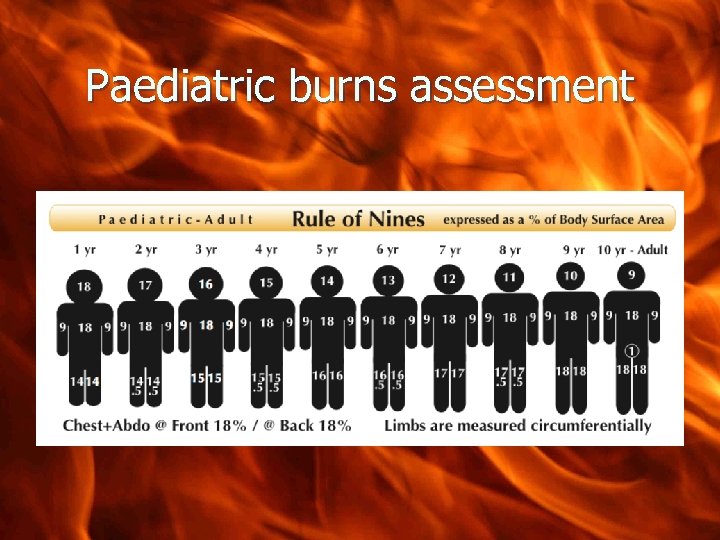
Paediatric burns assessment
Resuscitation Goals • • • Minimise burn shock Maintain perfusion without fluid overload Fluids • • • Adults >20% Paeds >10% Delay in fluid resus • Inc mortality
Burn Shock • • ”The burn wound is a 3 -dimensional mass of damaged tissue” Loss of fluid/electrolytes and proteins into interstitium WCC release of vasoactive substrances Microthrombi
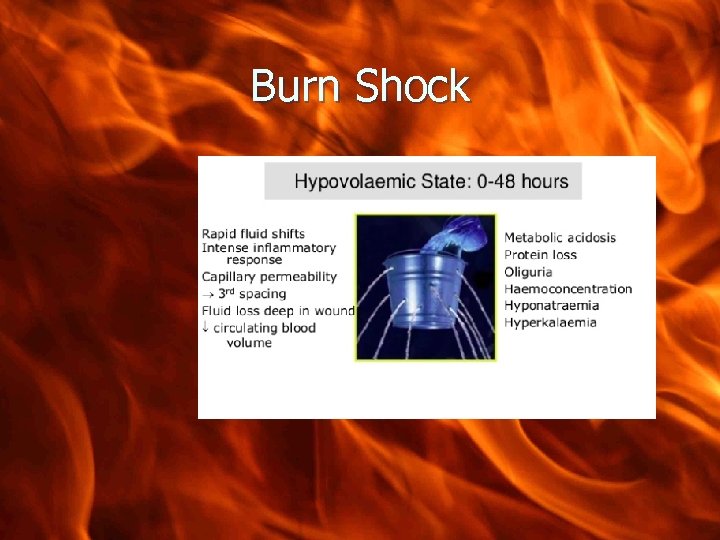
Burn Shock
How do we see this clinically? ? • Hypovolaemia • • Reduced UO, BP High Hct Oedema Low CO • • • Lactate Other end organ injury Major burns non burnt tissue becomes oedematous
Fluid resuscitation- the formulae • Modified Parkland formula • • • 4 ml/kg/%TBSA burned/first 24 hours 50% over first 8 hours from injury 50% over next 16 hours • MANY others e. g Brooke uses 2 ml/kg/%SA Galveston & Shriners calc SA Military I: O ratio • Required in adult >20% kid>10% • •
Fluid Therapy in burns- Monitoring response • • Invasive BP, pulse rate and pressure, cap refill Urine output • • • Adults UO 0. 5 ml/kg/hr Kids <30 kg 1 ml/kg/hr Lactate Haematocrit Na- useful >24 hr
Must not “set and forget” • • The minute by minute, hour by hour titration of volume to effect Resuscitation endpoints: • BP, urine, capillary refill, lactate, Hb, sodium • • Scv. O 2, Pi. CCO, echocardiography Avoid boluses if possible
Which fluid? • First 24 hours • Buffered isotonic crystalloid • • Plasmalyte (WARMED!) Colloid- NOT synthetic! • 4% albumin • • • Transfuse RBC as needed • • Cochrane review 2011 – no reduction mortality ? after 24 hr ? 12 hr Significant blood loss when debriding Enteral
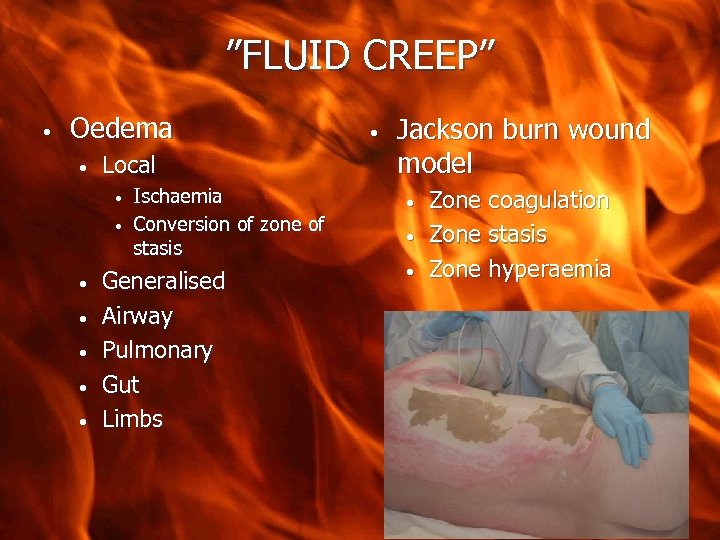
”FLUID CREEP” • Oedema • Local • • Ischaemia Conversion of zone of stasis Generalised Airway Pulmonary Gut Limbs • Jackson burn wound model • • • Zone coagulation Zone stasis Zone hyperaemia
Complications of fluid resuscitation • • Limb ischaemia/ compartment syndrome Abdominal compartment syndrome • • Gut oedema Abdominal wall burns • • Very poor outcome especially if laparostomy is required May occur within 24 hours
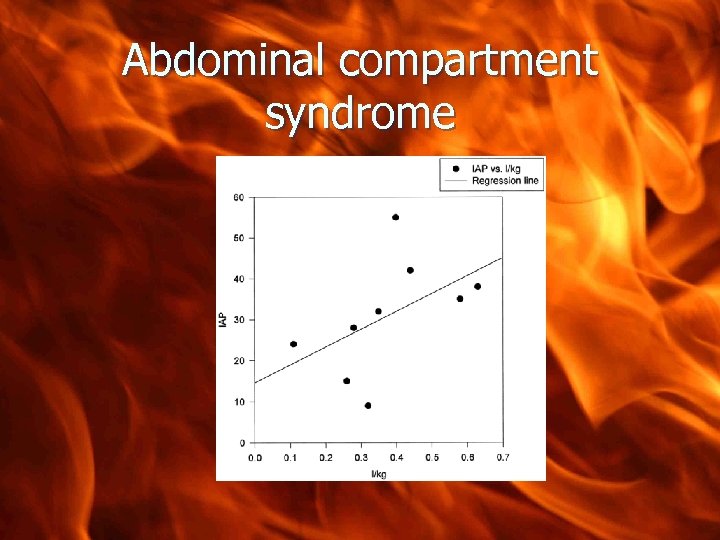
Abdominal compartment syndrome
Airway • Major burns • • • Swelling 1 -3 hr post injury and continues normal tissue swell Intubate early Avoid suxamethonium >24 hr post injury Beware “cuff leak” Secure- screw or wire
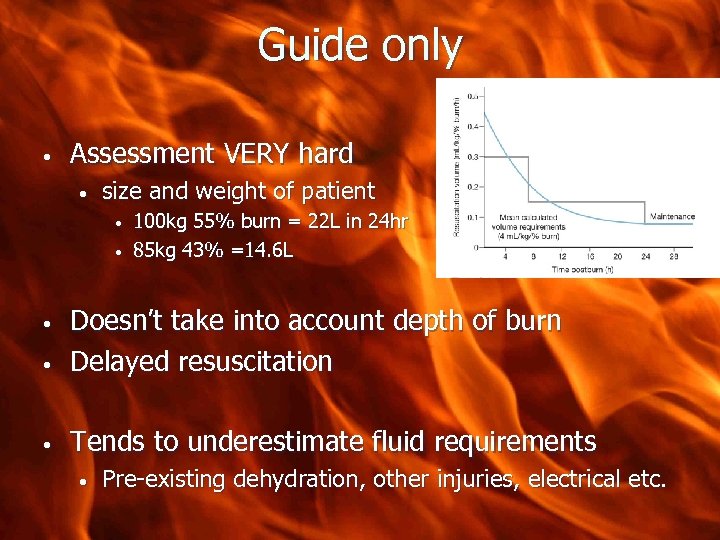
Guide only • Assessment VERY hard • size and weight of patient • • 100 kg 55% burn = 22 L in 24 hr 85 kg 43% =14. 6 L • Doesn’t take into account depth of burn Delayed resuscitation • Tends to underestimate fluid requirements • • Pre-existing dehydration, other injuries, electrical etc.
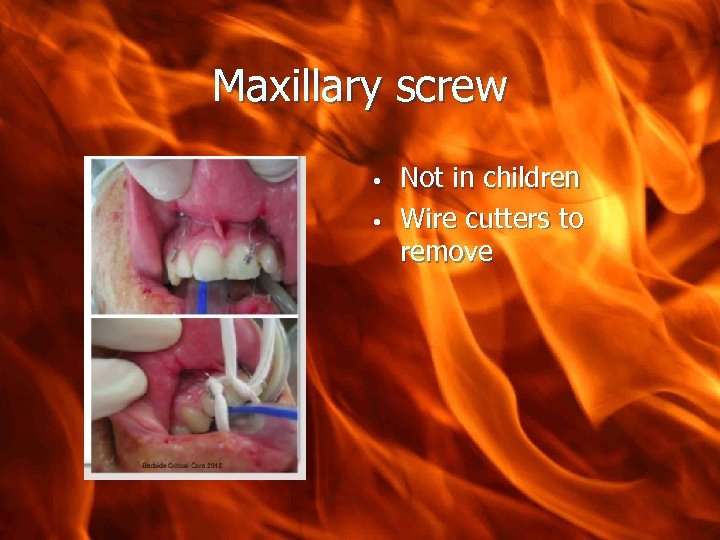
Maxillary screw • • Not in children Wire cutters to remove
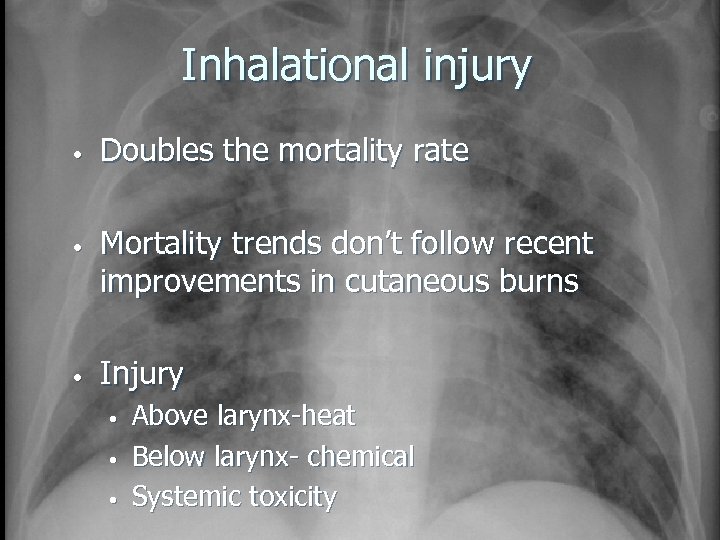
Inhalational injury • • • Doubles the mortality rate Mortality trends don’t follow recent improvements in cutaneous burns Injury • • • Above larynx-heat Below larynx- chemical Systemic toxicity
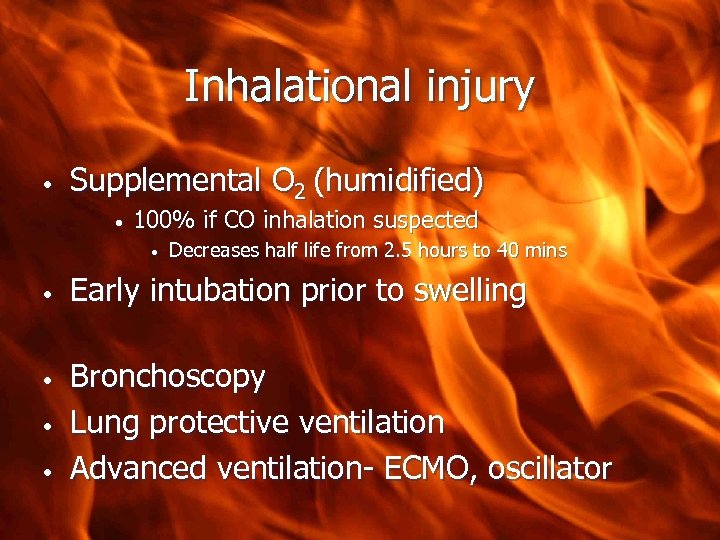
Inhalational injury • Supplemental O 2 (humidified) • 100% if CO inhalation suspected • • • Decreases half life from 2. 5 hours to 40 mins Early intubation prior to swelling Bronchoscopy Lung protective ventilation Advanced ventilation- ECMO, oscillator
Exam question • Outline the pathophysiology and clinical features of a smoke inhalation injury in a patient with major burns
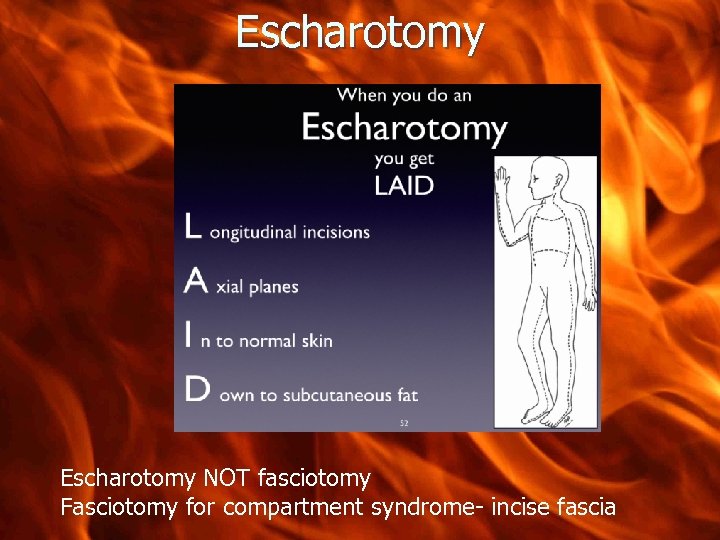
Escharotomy NOT fasciotomy Fasciotomy for compartment syndrome- incise fascia

Escharotomy
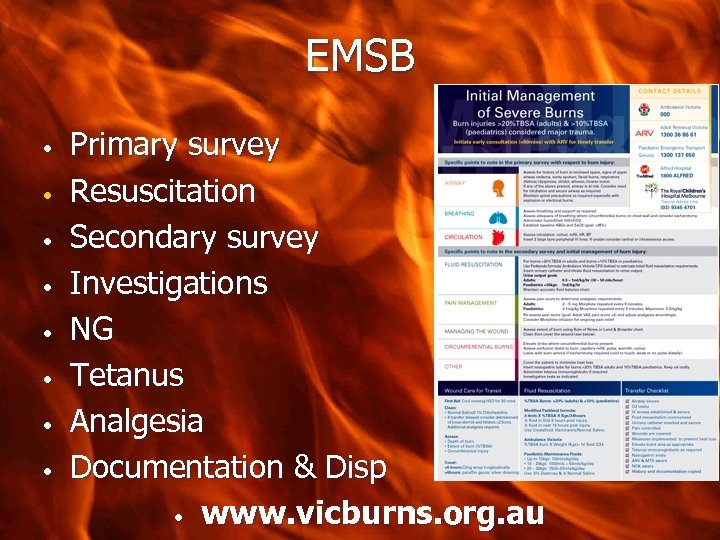
EMSB • • Primary survey Resuscitation Secondary survey Investigations NG Tetanus Analgesia Documentation & Disp • www. vicburns. org. au
Complications • • Cover • • • AVOID HYPOTHERMIA Clean dressing SSD-discuss Heated rooms and fluids

Most important issue in burn care • DEBRIDEMENT AND EARLY COVERAGE
OR • • Scrub down Debridement Grafting Dressing changes
The Function of a burn dressing • • • Comfort Metabolic Protective • IDEAL DRESSING • • Facilitate wound healing Acceptable appearance Promote comfort & function Cheap & easy to handle
Basic Principals • There is NO ‘perfect’ dressing • • different dressings achieve different things The ‘ultimate’ dressing is the patient’s own skin… via spontaneous healing or via grafting •
Aggressive wound care • Cut off the eschar as early as possible and close the wound • • Issues surround coverage of wounds • • • Improved mortality and length of stay Ideally with autograft Not usually possible with large burns ……. Skin substitutes • Buy time until grafting or healing occurs
Wound care • • Topical agents Compresses • • gauze, silver containing (Acticoat) Biosynthetics Dermal replacement/Biologics Barrier • Waterproof and breathable

SSD • Silver sulphadiazine • • • Delivers silver to the wound Antiimicrobial and inflammatory Messy Forms pseudoeschar CI- pregnancy, <2/12 old
Nomenclature of dermal replacements • • Allograft = cadaver = homograft Autograft = patients own skin • • Increases burn area = donor site Xenograft = pig Synthetic skin substitutes Cultured epithelial autograft
Biobrane • 2 layer membrane • • • Inner- allows nylon allows fibrovascular ingrowth Outer silastic- barrier to fluid and bacteria Uses Typically used • • • Donor site Dressing over autograft / allograft Toxic epidermal necrolysis
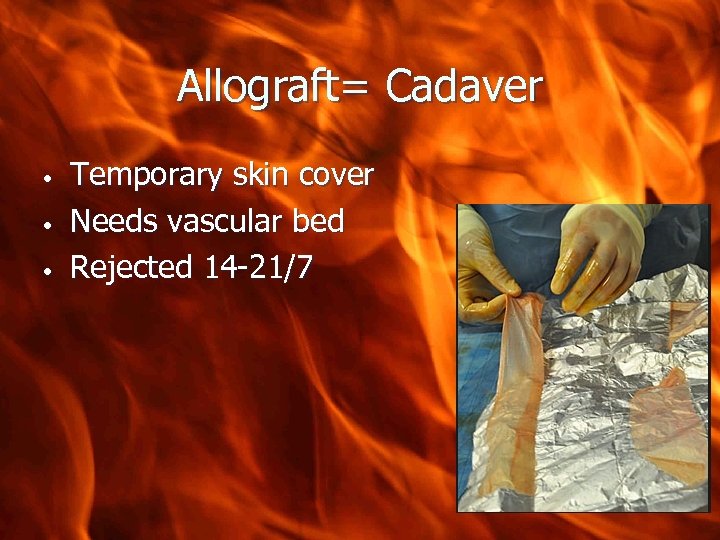
Allograft= Cadaver • • • Temporary skin cover Needs vascular bed Rejected 14 -21/7
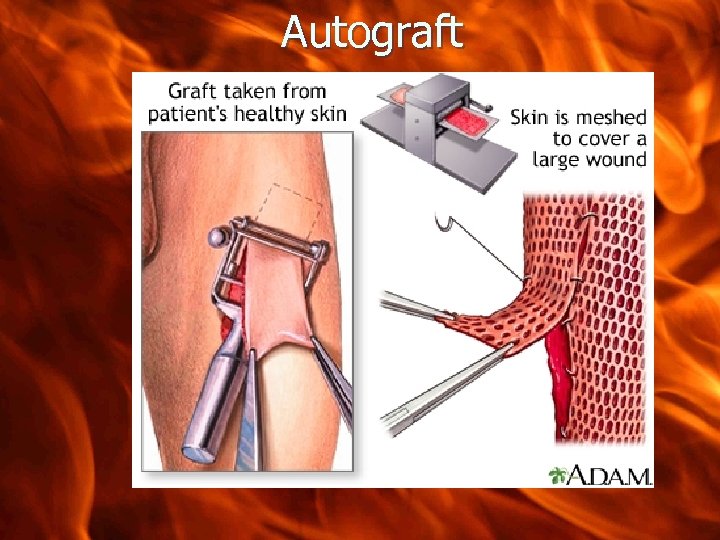
Autograft

Integra ™ • Bilaminar dermal replacement • • Silicone, collagen & glycosaminoglycans Creates a ‘neodermis’ • • Infiltration by host fibroblasts & neovascularisation Thin split skin graft over • Intolerant of wound infection • Expensive
Skin Culture • • • Autograft Epidermal cells are replicated But…. . • • No dermis Fragile graft Approx 50% ‘take’ Cost

Support until wound coverage • Organ support • Analgesia • • Background Cover procedures • Temperature • Nutrition
Prevent infection • • Nurse in isolation Aggressive infection surveillance Early wound care Prophylactic antibiotics • • • No evidence unless contaminated Rectal tube Antibiotic impregnated lines
Infection • • • GNB wound infection can kill in hours Vigilant Early signs • • • Gut distension/ng asps Loss of glucose control UO tails off Inotropes “whiff” Low temp-consider what’s normal
Infection • • Theatre for review- don’t delay Antibiotics • • • Previous micro Gram negative cover Consider other source once wounds excluded
Hypermetabolic response to burns • • • BSA >25% Begins within 5/7 lasts upto 12 months Ebb phase • • • <48 hr Low CO, metabolic rate, glucose intolerance Flow phase • • Within 5/7 Hyperdynamic and hypermetabolic • Oxandrolone, Bblockers, rhgh
Analgesic agents • Opioids • • Anaesthetic agents • • Morphine, methadone, fentanyl Ketamine, benzodiazepines Non opioids • Paracetamol, Gabapentin, NSAIDs
Nutrition • • • NJ tube Supplements- zinc, folate, multivits REE
With respect to the clinical assessment of a patient presenting with a severe burn injury sustained in a house fire: a) Outline how burns are classified. b) List three methods for estimating the total body surface area affected by a burn injury. c)Other than the burn type and extent, list the other important features of the physical examination that should be noted as part of the initial clinical assessment of the patient described above.
55 yo 60% burn some debridement and grafting Returns from OR following further debridement BP 85/50 Outline causes and Mx of his hypotension •
Other considerations • • • DVT prophylaxis Control of bowels Ulcer prophylaxis Eye care Family
Burns hot case • • Exam limited! If early <48 hr • • • Resus Other traumatic injuries Toxins –CO ARDS ventilation Escharotomies • Later • • • Infection Oedema Nutrition
Anabolic agents • Human Growth Hormone • • Accelerate donor healing Restore nitrogen balance Oxandrolone Beta- blocking agents • Anti catabolic agent
Key points • Burns=trauma • • • Look for other injuries First aid vital Assess size and depth Fluid formulas a guide only Circumferential burns Prevent hypothermia
Summary • • The severely burned patient is a trauma patient Challenging • • • Time and resource consuming Early aggressive resuscitation, and definitive wound care defines outcome Requires a multi-disciplinary team approach
4f5d3271c142118bad1e391733d577be.ppt