2a51f2e24088be5f11cd7fe9e3994d22.ppt
- Количество слайдов: 43
 Management of Cervical Cancer Chu-Ling Wang 4/19/2006
Management of Cervical Cancer Chu-Ling Wang 4/19/2006
 Outline • • • Epidemiology Risk factors of cervical cancer Role of human papillomavirus Clinical manifestations Management of cervical cancer Human papillomavirus vaccine
Outline • • • Epidemiology Risk factors of cervical cancer Role of human papillomavirus Clinical manifestations Management of cervical cancer Human papillomavirus vaccine
 Cervical cancer • In the United States – 10, 370 new cases are diagnosed annually – 3, 710 deaths (1. 3% of cancer deaths in women) • Incidence – – Mean age at diagnosis of 47 years 0/100, 000/year in women under age 20 1. 7/100, 000/year in women aged 20 - 24 years Peaking at 16. 5/100, 000/year in women aged 45 to 49 years – Only 10% of cases occurred in women age 75 or more
Cervical cancer • In the United States – 10, 370 new cases are diagnosed annually – 3, 710 deaths (1. 3% of cancer deaths in women) • Incidence – – Mean age at diagnosis of 47 years 0/100, 000/year in women under age 20 1. 7/100, 000/year in women aged 20 - 24 years Peaking at 16. 5/100, 000/year in women aged 45 to 49 years – Only 10% of cases occurred in women age 75 or more
 Cervical cancer • In Taiwan (2002) – 5, 725 new cases are diagnosed (8. 98% of cancer) – 941 deaths (2. 74% of cancer deaths) • Incidence – Mean age at diagnosis of 49 years
Cervical cancer • In Taiwan (2002) – 5, 725 new cases are diagnosed (8. 98% of cancer) – 941 deaths (2. 74% of cancer deaths) • Incidence – Mean age at diagnosis of 49 years
 Risk factors of cervical cancer • Early onset of sexual activity • Multiple sexual partners • High-risk sexual partner – eg, promiscuous sexual activity, sexual exposure to a partner with human papillomavirus infection • Other risk factors: – History of sexually transmitted diseases (eg, herpes simplex virus) – Smoking, immunosuppression, low socioeconomic status, and previous history of vulvar or vaginal squamous dysplasia
Risk factors of cervical cancer • Early onset of sexual activity • Multiple sexual partners • High-risk sexual partner – eg, promiscuous sexual activity, sexual exposure to a partner with human papillomavirus infection • Other risk factors: – History of sexually transmitted diseases (eg, herpes simplex virus) – Smoking, immunosuppression, low socioeconomic status, and previous history of vulvar or vaginal squamous dysplasia
 Role of human papillomavirus • The human papillomavirus (HPV) is central to the development of cervical neoplasia and can be detected in almost all cervical cancers. • Most HPV infections are transient, not all HPVs are oncogenic, and the virus alone is not sufficient to cause cervical neoplasia. • The most prevalent HPV types associated with cervical cancer are HPV-16 (60%) and HPV-18 (10%).
Role of human papillomavirus • The human papillomavirus (HPV) is central to the development of cervical neoplasia and can be detected in almost all cervical cancers. • Most HPV infections are transient, not all HPVs are oncogenic, and the virus alone is not sufficient to cause cervical neoplasia. • The most prevalent HPV types associated with cervical cancer are HPV-16 (60%) and HPV-18 (10%).
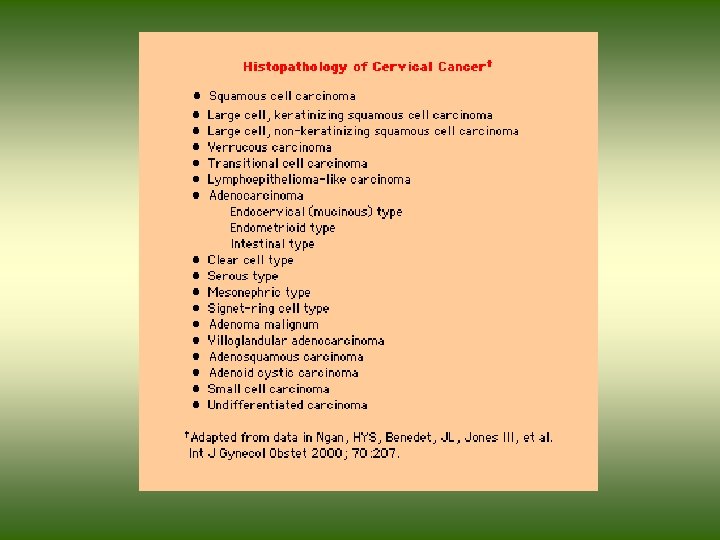
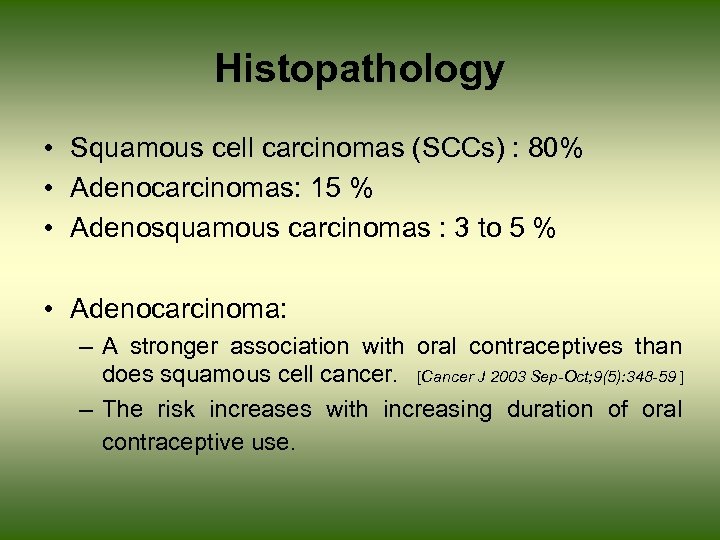 Histopathology • Squamous cell carcinomas (SCCs) : 80% • Adenocarcinomas: 15 % • Adenosquamous carcinomas : 3 to 5 % • Adenocarcinoma: – A stronger association with oral contraceptives than does squamous cell cancer. [Cancer J 2003 Sep-Oct; 9(5): 348 -59 ] – The risk increases with increasing duration of oral contraceptive use.
Histopathology • Squamous cell carcinomas (SCCs) : 80% • Adenocarcinomas: 15 % • Adenosquamous carcinomas : 3 to 5 % • Adenocarcinoma: – A stronger association with oral contraceptives than does squamous cell cancer. [Cancer J 2003 Sep-Oct; 9(5): 348 -59 ] – The risk increases with increasing duration of oral contraceptive use.
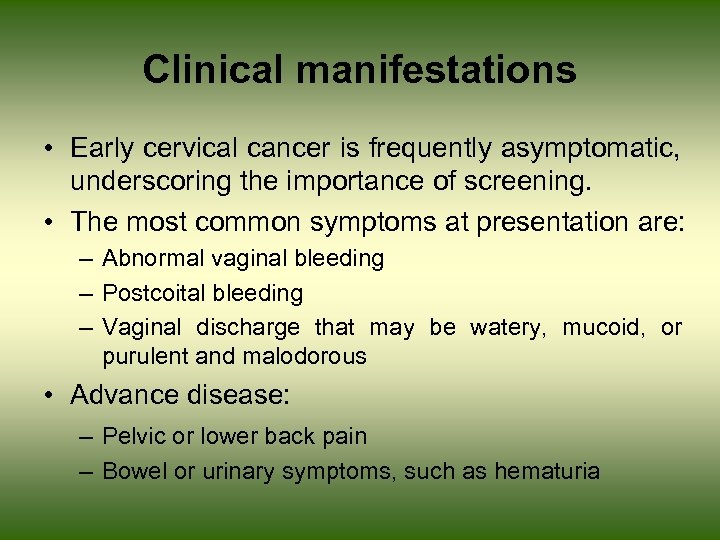 Clinical manifestations • Early cervical cancer is frequently asymptomatic, underscoring the importance of screening. • The most common symptoms at presentation are: – Abnormal vaginal bleeding – Postcoital bleeding – Vaginal discharge that may be watery, mucoid, or purulent and malodorous • Advance disease: – Pelvic or lower back pain – Bowel or urinary symptoms, such as hematuria
Clinical manifestations • Early cervical cancer is frequently asymptomatic, underscoring the importance of screening. • The most common symptoms at presentation are: – Abnormal vaginal bleeding – Postcoital bleeding – Vaginal discharge that may be watery, mucoid, or purulent and malodorous • Advance disease: – Pelvic or lower back pain – Bowel or urinary symptoms, such as hematuria
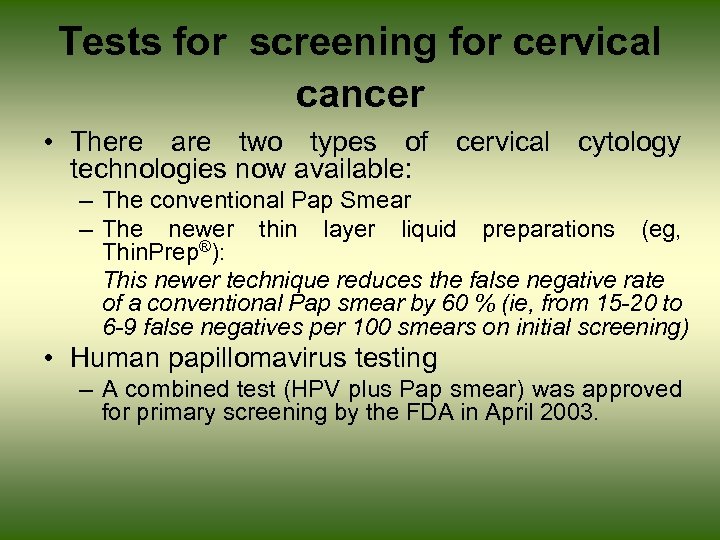 Tests for screening for cervical cancer • There are two types of cervical cytology technologies now available: – The conventional Pap Smear – The newer thin layer liquid preparations (eg, Thin. Prep®): This newer technique reduces the false negative rate of a conventional Pap smear by 60 % (ie, from 15 -20 to 6 -9 false negatives per 100 smears on initial screening) • Human papillomavirus testing – A combined test (HPV plus Pap smear) was approved for primary screening by the FDA in April 2003.
Tests for screening for cervical cancer • There are two types of cervical cytology technologies now available: – The conventional Pap Smear – The newer thin layer liquid preparations (eg, Thin. Prep®): This newer technique reduces the false negative rate of a conventional Pap smear by 60 % (ie, from 15 -20 to 6 -9 false negatives per 100 smears on initial screening) • Human papillomavirus testing – A combined test (HPV plus Pap smear) was approved for primary screening by the FDA in April 2003.
 Human papillomavirus testing • A combination of HPV DNA testing and cervical cytology in women over age 30 who are being screened for cervical cancer is another option for primary screening. • The rationale is to take advantage of the high sensitivity of HPV DNA testing and the high specificity of cervical cytology to increase the screening interval in women who test negative for HPV DNA and negative for cytological abnormalities.
Human papillomavirus testing • A combination of HPV DNA testing and cervical cytology in women over age 30 who are being screened for cervical cancer is another option for primary screening. • The rationale is to take advantage of the high sensitivity of HPV DNA testing and the high specificity of cervical cytology to increase the screening interval in women who test negative for HPV DNA and negative for cytological abnormalities.
 Examinations • • • Palpation and inspection of the primary tumor Colposcopy (陰道鏡檢查 ) Endocervical curettage (子宮內頸搔刮術 ) Conization (錐狀切片 ) Hysteroscopy (子宮腔鏡 ) Cystoscopy (膀胱鏡 ) Proctoscopy (直腸鏡 ) Intravenous pyelogram (IVP) (靜脈腎盂攝影 ) Radiography of the lungs and skeleton
Examinations • • • Palpation and inspection of the primary tumor Colposcopy (陰道鏡檢查 ) Endocervical curettage (子宮內頸搔刮術 ) Conization (錐狀切片 ) Hysteroscopy (子宮腔鏡 ) Cystoscopy (膀胱鏡 ) Proctoscopy (直腸鏡 ) Intravenous pyelogram (IVP) (靜脈腎盂攝影 ) Radiography of the lungs and skeleton
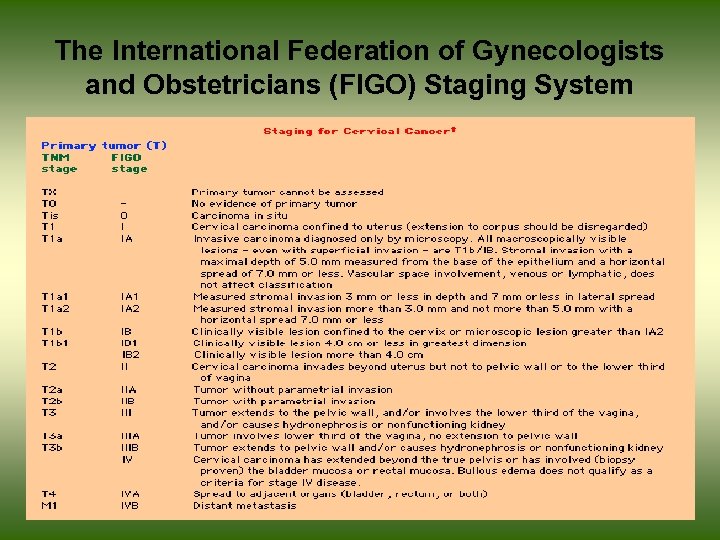 The International Federation of Gynecologists and Obstetricians (FIGO) Staging System
The International Federation of Gynecologists and Obstetricians (FIGO) Staging System
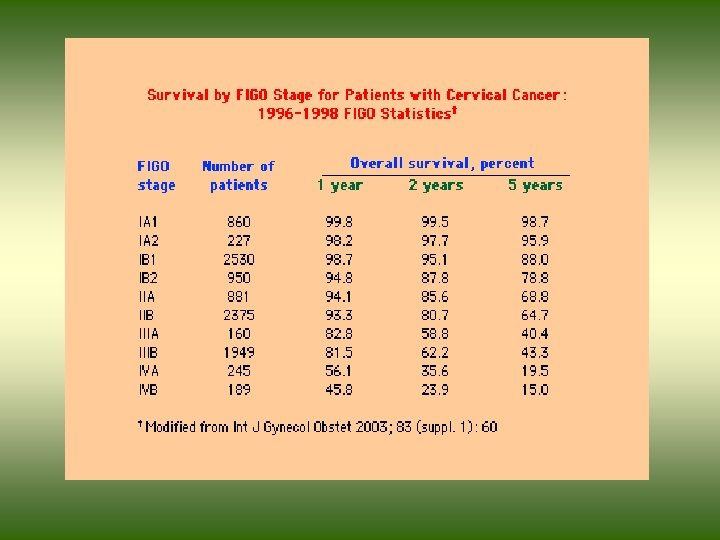
 FIGO Stage • • 0 : Carcinoma in situ IA : Microinvasive (IA 1, IA 2) IB : Invasive (>5 mm FIGO) IIA : Upper 2/3 of vagina IIB : Parametrial involvement IIIA: Involves lower 1/3 of vagina IIIB: Extends to pelvic and/or caused hydronephrosis/ nonfunctional kidney • IVA: Spread to bladder or rectum • IVB: Distant metastasis
FIGO Stage • • 0 : Carcinoma in situ IA : Microinvasive (IA 1, IA 2) IB : Invasive (>5 mm FIGO) IIA : Upper 2/3 of vagina IIB : Parametrial involvement IIIA: Involves lower 1/3 of vagina IIIB: Extends to pelvic and/or caused hydronephrosis/ nonfunctional kidney • IVA: Spread to bladder or rectum • IVB: Distant metastasis
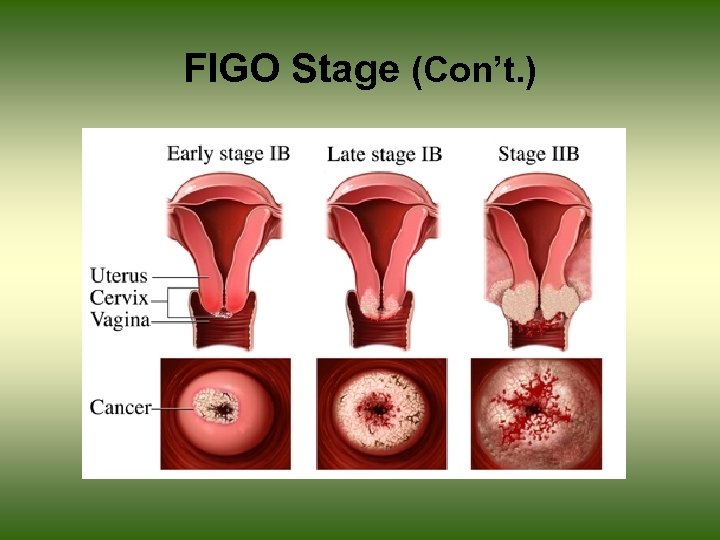 FIGO Stage (Con’t. )
FIGO Stage (Con’t. )
 Optional evaluation procedures • Although they are not used to assign disease stage in the FIGO classification, optional staging examinations, including CT, MRI, PET, lymphangiography (LAG), or ultrasonography may be of value for planning treatment, particularly the extent of the radiation therapy field or scope of surgery.
Optional evaluation procedures • Although they are not used to assign disease stage in the FIGO classification, optional staging examinations, including CT, MRI, PET, lymphangiography (LAG), or ultrasonography may be of value for planning treatment, particularly the extent of the radiation therapy field or scope of surgery.
 MRI vs. CT • Detection of nodal disease – Sensitivity: MRI 60% vs. CT 43% • Detection of parametrial invasion – Sensitivity: MRI 74% vs. CT 55% – MRI showed a trend toward better assessment of bladder and rectal involvement. • Positive findings by either imaging modality should be histologically confirmed by fine needle aspiration under CT guidance. Gynecol Oncol 2003 Oct; 91(1): 59 -66.
MRI vs. CT • Detection of nodal disease – Sensitivity: MRI 60% vs. CT 43% • Detection of parametrial invasion – Sensitivity: MRI 74% vs. CT 55% – MRI showed a trend toward better assessment of bladder and rectal involvement. • Positive findings by either imaging modality should be histologically confirmed by fine needle aspiration under CT guidance. Gynecol Oncol 2003 Oct; 91(1): 59 -66.
 PET scan • PET scanning may provide a better assessment of the presence of extrapelvic metastases than other imaging modalities.
PET scan • PET scanning may provide a better assessment of the presence of extrapelvic metastases than other imaging modalities.
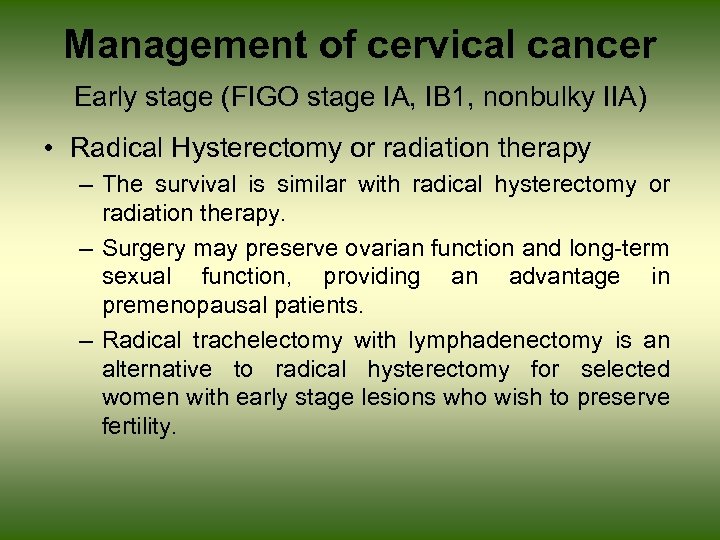 Management of cervical cancer Early stage (FIGO stage IA, IB 1, nonbulky IIA) • Radical Hysterectomy or radiation therapy – The survival is similar with radical hysterectomy or radiation therapy. – Surgery may preserve ovarian function and long-term sexual function, providing an advantage in premenopausal patients. – Radical trachelectomy with lymphadenectomy is an alternative to radical hysterectomy for selected women with early stage lesions who wish to preserve fertility.
Management of cervical cancer Early stage (FIGO stage IA, IB 1, nonbulky IIA) • Radical Hysterectomy or radiation therapy – The survival is similar with radical hysterectomy or radiation therapy. – Surgery may preserve ovarian function and long-term sexual function, providing an advantage in premenopausal patients. – Radical trachelectomy with lymphadenectomy is an alternative to radical hysterectomy for selected women with early stage lesions who wish to preserve fertility.
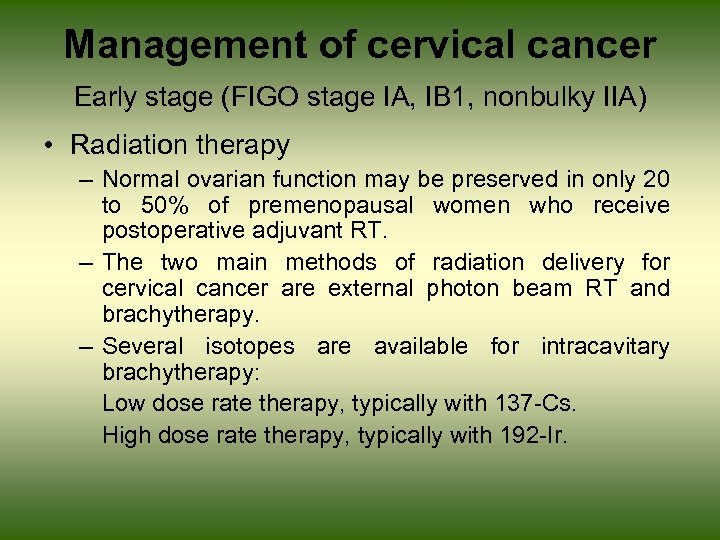 Management of cervical cancer Early stage (FIGO stage IA, IB 1, nonbulky IIA) • Radiation therapy – Normal ovarian function may be preserved in only 20 to 50% of premenopausal women who receive postoperative adjuvant RT. – The two main methods of radiation delivery for cervical cancer are external photon beam RT and brachytherapy. – Several isotopes are available for intracavitary brachytherapy: Low dose rate therapy, typically with 137 -Cs. High dose rate therapy, typically with 192 -Ir.
Management of cervical cancer Early stage (FIGO stage IA, IB 1, nonbulky IIA) • Radiation therapy – Normal ovarian function may be preserved in only 20 to 50% of premenopausal women who receive postoperative adjuvant RT. – The two main methods of radiation delivery for cervical cancer are external photon beam RT and brachytherapy. – Several isotopes are available for intracavitary brachytherapy: Low dose rate therapy, typically with 137 -Cs. High dose rate therapy, typically with 192 -Ir.
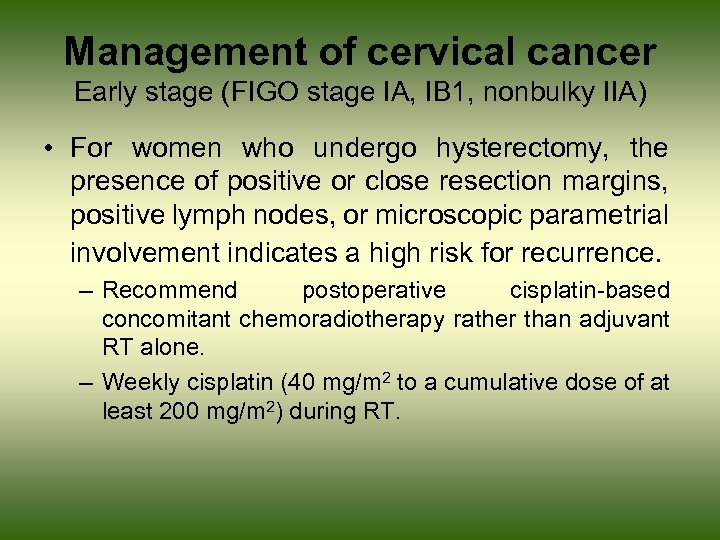 Management of cervical cancer Early stage (FIGO stage IA, IB 1, nonbulky IIA) • For women who undergo hysterectomy, the presence of positive or close resection margins, positive lymph nodes, or microscopic parametrial involvement indicates a high risk for recurrence. – Recommend postoperative cisplatin-based concomitant chemoradiotherapy rather than adjuvant RT alone. – Weekly cisplatin (40 mg/m 2 to a cumulative dose of at least 200 mg/m 2) during RT.
Management of cervical cancer Early stage (FIGO stage IA, IB 1, nonbulky IIA) • For women who undergo hysterectomy, the presence of positive or close resection margins, positive lymph nodes, or microscopic parametrial involvement indicates a high risk for recurrence. – Recommend postoperative cisplatin-based concomitant chemoradiotherapy rather than adjuvant RT alone. – Weekly cisplatin (40 mg/m 2 to a cumulative dose of at least 200 mg/m 2) during RT.
 Management of cervical cancer Early stage (FIGO stage IA, IB 1, nonbulky IIA) • Compared to RT alone, chemoradiotherapy was associated with a significant 29% reduction in the risk of death [absolute improvement in overall survival of 12 % (from 40 to 52%)]; and a 39% improvement in PFS [16% absolute improvement (from 47 to 63%)]. • Concomitant chemoradiotherapy was associated with a significant decrease in both local and distant recurrence compared with RT alone. Lancet 2001 Sep 8; 358(9284): 781 -6.
Management of cervical cancer Early stage (FIGO stage IA, IB 1, nonbulky IIA) • Compared to RT alone, chemoradiotherapy was associated with a significant 29% reduction in the risk of death [absolute improvement in overall survival of 12 % (from 40 to 52%)]; and a 39% improvement in PFS [16% absolute improvement (from 47 to 63%)]. • Concomitant chemoradiotherapy was associated with a significant decrease in both local and distant recurrence compared with RT alone. Lancet 2001 Sep 8; 358(9284): 781 -6.
 Quality of Life • Quality of life after RT or surgery: – Both hysterectomy and RT can lead to changes such as vaginal shortening and decreased vaginal lubrication, which adversely influence sexual function, overall quality of life.
Quality of Life • Quality of life after RT or surgery: – Both hysterectomy and RT can lead to changes such as vaginal shortening and decreased vaginal lubrication, which adversely influence sexual function, overall quality of life.
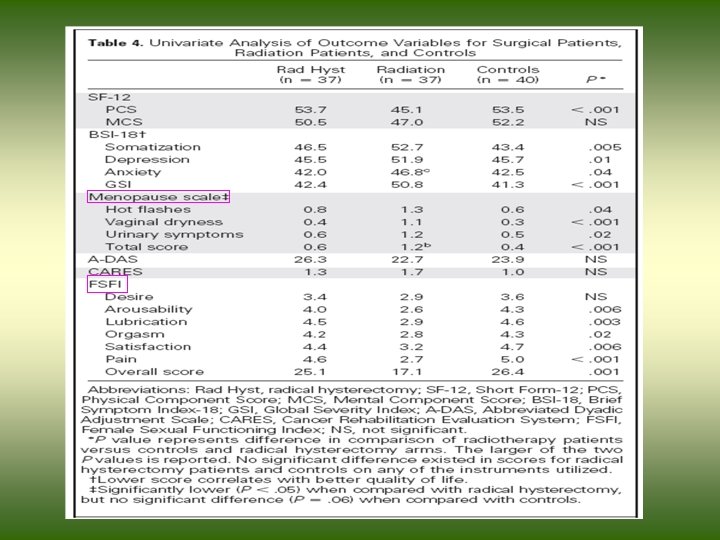
 Quality of Life (Con’t. ) • Women were at least 5 years after initial treatment for cervical cancer. Eligible women had squamous cell tumors smaller than 6 cm (stage I) at diagnosis, were currently disease-free, and had either undergone surgery or radiotherapy, but not both. • 114 patients (37 surgery, 37 radiotherapy, 40 controls) were included for analysis. J Clin Oncol 23: 7428 -7436.
Quality of Life (Con’t. ) • Women were at least 5 years after initial treatment for cervical cancer. Eligible women had squamous cell tumors smaller than 6 cm (stage I) at diagnosis, were currently disease-free, and had either undergone surgery or radiotherapy, but not both. • 114 patients (37 surgery, 37 radiotherapy, 40 controls) were included for analysis. J Clin Oncol 23: 7428 -7436.
 Quality of Life (Con’t. ) • Cervical cancer survivors treated primarily with radical hysterectomy have less sexual dysfunction than patients treated with radiotherapy. • Authors strongly recommend either the use of a vaginal dilator or the engagement in sexual intercourse frequently after completion of radiotherapy for cervical cancer in an effort to maintain the length, width, and elasticity of the vaginal canal. J Clin Oncol 23: 7428 -7436.
Quality of Life (Con’t. ) • Cervical cancer survivors treated primarily with radical hysterectomy have less sexual dysfunction than patients treated with radiotherapy. • Authors strongly recommend either the use of a vaginal dilator or the engagement in sexual intercourse frequently after completion of radiotherapy for cervical cancer in an effort to maintain the length, width, and elasticity of the vaginal canal. J Clin Oncol 23: 7428 -7436.
 Management of cervical cancer Bulky stage IB 2 and IIA disease • Women with bulky early stage cervical cancer (ie, stage IB 2 and IIA) have a higher local failure rate. After surgery alone, the rate of relapse is as high as 30%.
Management of cervical cancer Bulky stage IB 2 and IIA disease • Women with bulky early stage cervical cancer (ie, stage IB 2 and IIA) have a higher local failure rate. After surgery alone, the rate of relapse is as high as 30%.
 Management of cervical cancer Bulky stage IB 2 and IIA disease • There are three options for treating women with stage IB 2 or IIA disease: 1. Chemoradiotherapy alone 2. Surgery followed by chemoradiotherapy – For patient with high or intermediate risk factors for recurrence 3. Chemoradiotherapy followed by hysterectomy – Reduction in pelvic recurrence rates (from 15 to 20 % to 2 to 5%)
Management of cervical cancer Bulky stage IB 2 and IIA disease • There are three options for treating women with stage IB 2 or IIA disease: 1. Chemoradiotherapy alone 2. Surgery followed by chemoradiotherapy – For patient with high or intermediate risk factors for recurrence 3. Chemoradiotherapy followed by hysterectomy – Reduction in pelvic recurrence rates (from 15 to 20 % to 2 to 5%)
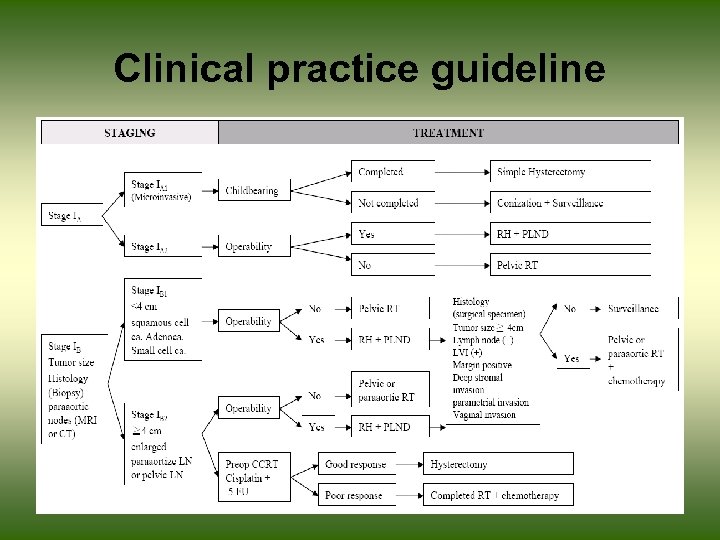 Clinical practice guideline
Clinical practice guideline
 Management of cervical cancer Locally advanced disease • For women with stages IIB, III, and IVA cervical SCC, primary chemoradiotherapy is recommended over RT alone. • Suggest weekly cisplatin (40 mg/m 2 to a cumulative dose of at least 200 mg/m 2) during RT.
Management of cervical cancer Locally advanced disease • For women with stages IIB, III, and IVA cervical SCC, primary chemoradiotherapy is recommended over RT alone. • Suggest weekly cisplatin (40 mg/m 2 to a cumulative dose of at least 200 mg/m 2) during RT.
 Management of cervical cancer Locally advanced disease • The previously meta-analysis included trials that randomly assigned patients with FIGO stage IB to IVA disease to concomitant chemoradiotherapy vs. RT with or without surgery, and with or without additional adjuvant chemotherapy • Compared to RT alone, concomitant chemoradiotherapy was associated with a significant 29% reduction in the risk of death, a 39% improvement in PFS, and a significant decrease in both local and distant recurrence. Lancet 2001 Sep 8; 358(9284): 781 -6.
Management of cervical cancer Locally advanced disease • The previously meta-analysis included trials that randomly assigned patients with FIGO stage IB to IVA disease to concomitant chemoradiotherapy vs. RT with or without surgery, and with or without additional adjuvant chemotherapy • Compared to RT alone, concomitant chemoradiotherapy was associated with a significant 29% reduction in the risk of death, a 39% improvement in PFS, and a significant decrease in both local and distant recurrence. Lancet 2001 Sep 8; 358(9284): 781 -6.
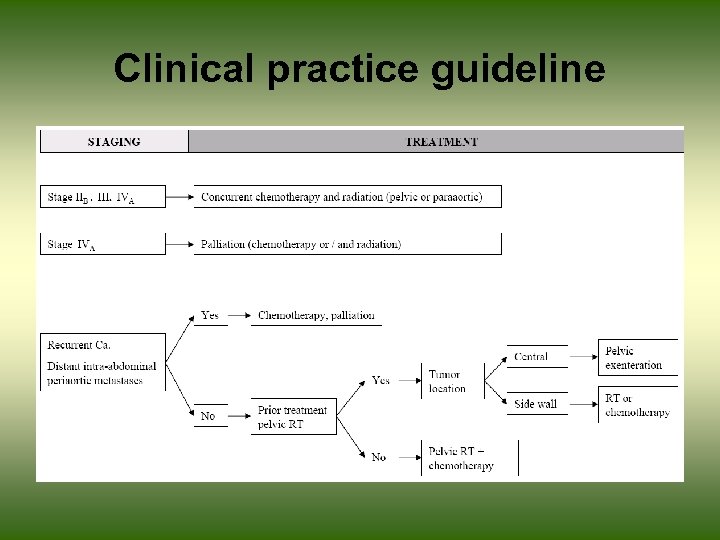 Clinical practice guideline
Clinical practice guideline
 HPV Vaccine • A randomised, double-blind, controlled trial to assess the efficacy, safety, and immunogenicity of a bivalent HPV-16/18 L 1 virus-like particle vaccine. • 1113 women between 15– 25 years of age to receive three doses of either the vaccine formulated with AS 04 adjuvant or placebo on a 0 month, 1 month, and 6 month schedule. (followup 27 months) Lancet 2004; 364: 1757– 65
HPV Vaccine • A randomised, double-blind, controlled trial to assess the efficacy, safety, and immunogenicity of a bivalent HPV-16/18 L 1 virus-like particle vaccine. • 1113 women between 15– 25 years of age to receive three doses of either the vaccine formulated with AS 04 adjuvant or placebo on a 0 month, 1 month, and 6 month schedule. (followup 27 months) Lancet 2004; 364: 1757– 65
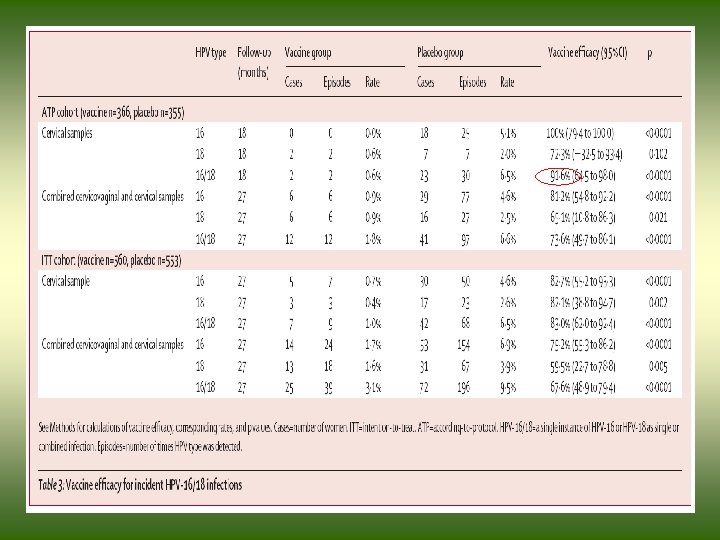
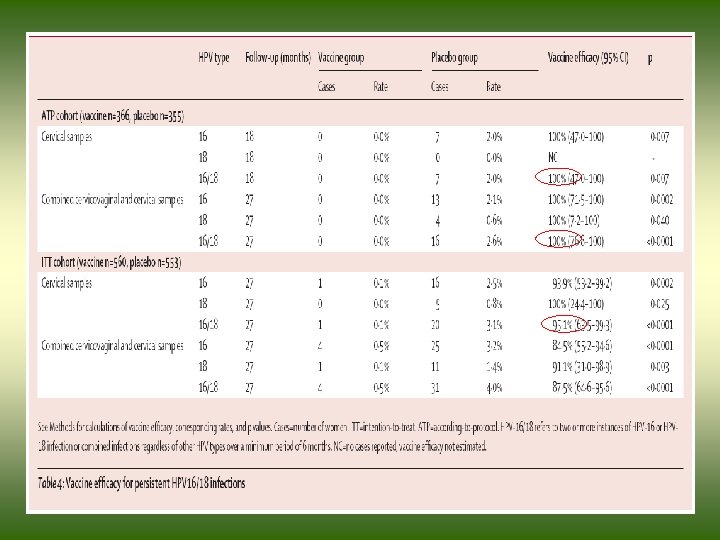
 HPV Vaccine (Con’t. ) • In the according-to-protocol analyses: – Vaccine efficacy was 91. 6% against incident infection and 100% against persistent infection with HPV-16/18. • In the intention-to-treat analyses: – vaccine efficacy was 95. 1% against persistent cervical infection with HPV-16/18 and 92. 9% against cytological abnormalities associated with HPV-16/18 infection. Lancet 2004; 364: 1757– 65
HPV Vaccine (Con’t. ) • In the according-to-protocol analyses: – Vaccine efficacy was 91. 6% against incident infection and 100% against persistent infection with HPV-16/18. • In the intention-to-treat analyses: – vaccine efficacy was 95. 1% against persistent cervical infection with HPV-16/18 and 92. 9% against cytological abnormalities associated with HPV-16/18 infection. Lancet 2004; 364: 1757– 65
 HPV Vaccine (Con’t. ) • The vaccine targets HPV types 16 and 18. Women were followed for up to 4. 5 years: – More than 98% of women had antibodies against HPV 16 and HPV 18. – Vaccine efficacy was 97% against incident infection with HPV-16/18. – Protection against HPV 16 - or HPV 18 -related precancerous changes to the cervix was 100%. Lancet. Early Online Publication April 6, 2006.
HPV Vaccine (Con’t. ) • The vaccine targets HPV types 16 and 18. Women were followed for up to 4. 5 years: – More than 98% of women had antibodies against HPV 16 and HPV 18. – Vaccine efficacy was 97% against incident infection with HPV-16/18. – Protection against HPV 16 - or HPV 18 -related precancerous changes to the cervix was 100%. Lancet. Early Online Publication April 6, 2006.
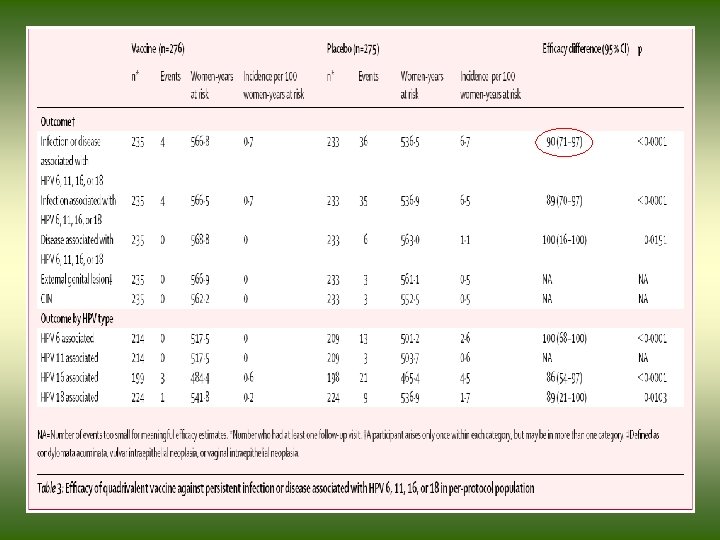
 HPV Vaccine (Con’t. ) • A randomised double-blind placebo-controlled phase II trial was done to assess the efficacy of a prophylactic quadrivalent vaccine targeting the HPV types associated with 70% of cervical cancers (HPV 16 and 18) and with 90% of genital warts (HPV 6 and 11). • Women between 16– 23 years of age to receive three doses of HPV vaccine (n=277) or placebo (n= 275) on a day 1, month 1, and month 6. (follow-up 36 months) Lancet Oncology 2005; 6: 271– 278
HPV Vaccine (Con’t. ) • A randomised double-blind placebo-controlled phase II trial was done to assess the efficacy of a prophylactic quadrivalent vaccine targeting the HPV types associated with 70% of cervical cancers (HPV 16 and 18) and with 90% of genital warts (HPV 6 and 11). • Women between 16– 23 years of age to receive three doses of HPV vaccine (n=277) or placebo (n= 275) on a day 1, month 1, and month 6. (follow-up 36 months) Lancet Oncology 2005; 6: 271– 278
 HPV Vaccine (Con’t. ) • Combined incidence of persistent infection or disease with HPV 6, 11, 16, or 18 fell by 90% ( p<0. 0001) in those assigned vaccine compared with those assigned placebo. Lancet Oncology 2005; 6: 271– 278
HPV Vaccine (Con’t. ) • Combined incidence of persistent infection or disease with HPV 6, 11, 16, or 18 fell by 90% ( p<0. 0001) in those assigned vaccine compared with those assigned placebo. Lancet Oncology 2005; 6: 271– 278