d33b86b1d30eb0ead7bea4ddffce4e6d.ppt
- Количество слайдов: 55
 MANAGEMENT OF ACUTE COPPER SULPHATE POISONING
MANAGEMENT OF ACUTE COPPER SULPHATE POISONING
 Synonyms of Copper sulphate • • • Copper (II) sulfate Cupric sulfate Bluestone Blue vitriol Roman vitriol Salzburg vitriol
Synonyms of Copper sulphate • • • Copper (II) sulfate Cupric sulfate Bluestone Blue vitriol Roman vitriol Salzburg vitriol
 Uses of Coppersulphate • In agriculture – fungicide, herbicide, algaecide and bactericide, and as a fertilizer additive. • In industry – textile dyeing; preserving hides and wood – tanning leather, electroplating, battery electrolyte; • In veterinary – anthelmintic, emetic and fungicide • Therapeutically – topical antifungal agent – antidote in phosphorus poisoning
Uses of Coppersulphate • In agriculture – fungicide, herbicide, algaecide and bactericide, and as a fertilizer additive. • In industry – textile dyeing; preserving hides and wood – tanning leather, electroplating, battery electrolyte; • In veterinary – anthelmintic, emetic and fungicide • Therapeutically – topical antifungal agent – antidote in phosphorus poisoning
 Role of Copper in Humans • Adult human content is 100 mg of copper • Co-factor in several metalloproteins, (cytochrome oxidase and superoxide dismutase) • Essential for the utilization of iron and haemoglobin formation
Role of Copper in Humans • Adult human content is 100 mg of copper • Co-factor in several metalloproteins, (cytochrome oxidase and superoxide dismutase) • Essential for the utilization of iron and haemoglobin formation
 Functions of Cuproenzymes electron transfer reactions in metabolic pathways involving • cellular respiration • iron homeostasis • pigment formation • neurotransmitter production • connective tissue biosyn-thesis • antioxidant defense.
Functions of Cuproenzymes electron transfer reactions in metabolic pathways involving • cellular respiration • iron homeostasis • pigment formation • neurotransmitter production • connective tissue biosyn-thesis • antioxidant defense.
 Acute Copper Sulphate poisoning
Acute Copper Sulphate poisoning
 Epidemiology • Particularly common in India • Cheap and do not have unpleasant smell or taste. • Common in North Chennai • Formed 2. 5% of poison cases at GSH(2005) • There is decline in the cuso 4 ingestion 1. 1%(2006) • Decline in the number of cases is possibly due to easy availability of less painful suicide substances
Epidemiology • Particularly common in India • Cheap and do not have unpleasant smell or taste. • Common in North Chennai • Formed 2. 5% of poison cases at GSH(2005) • There is decline in the cuso 4 ingestion 1. 1%(2006) • Decline in the number of cases is possibly due to easy availability of less painful suicide substances
 Absorption and Distribution • • • 40 to 70 % of ingested copper is absorped Transported across the intestinal mucosa Facilitated by enzyme cytosolic metallothionein Max. blood concentration in 2 hrs as albumin-bound In the liver it is incorporated into caeruloplasmin Can penetrate the erythrocyte membrane Can also absorbed through the skin and lung Copper can cross the placenta Highly concentrates in liver, heart, brain, kidneys and muscle
Absorption and Distribution • • • 40 to 70 % of ingested copper is absorped Transported across the intestinal mucosa Facilitated by enzyme cytosolic metallothionein Max. blood concentration in 2 hrs as albumin-bound In the liver it is incorporated into caeruloplasmin Can penetrate the erythrocyte membrane Can also absorbed through the skin and lung Copper can cross the placenta Highly concentrates in liver, heart, brain, kidneys and muscle
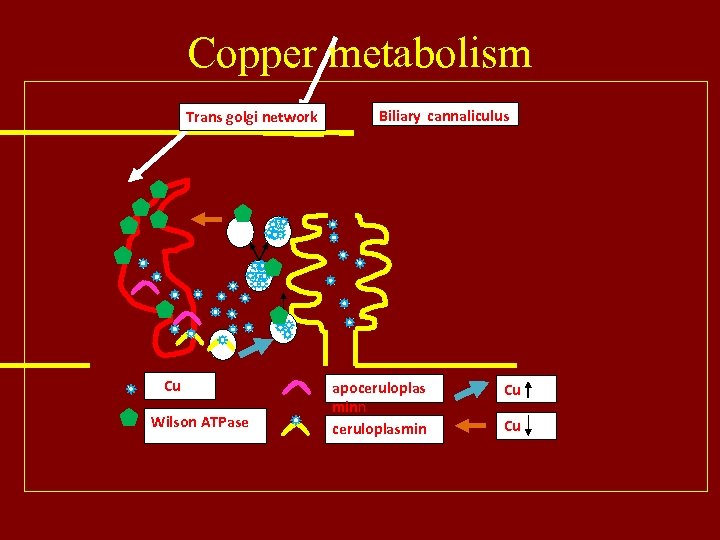 Copper metabolism Trans golgi network Cu Wilson ATPase Biliary cannaliculus apoceruloplas minn ceruloplasmin Cu Cu
Copper metabolism Trans golgi network Cu Wilson ATPase Biliary cannaliculus apoceruloplas minn ceruloplasmin Cu Cu
 Mechanism of Toxicity • Powerful oxidizing capacity and hence Corrosive to mucous membranes • Decreased copper-metallothionein binding and copper clearance from the cell ( se free Cu) results in cellular death • Inactivation of enzymes such as G 6 PD and Glutathione Reductase (GSH) by reduced Cu(I) that binds to SH groups • Production of reactive toxic hydroxyl radicals by copper interacting with oxygen species by catalyzing production hydroxyl ions (e. g. superoxide anions and hydrogen peroxide)
Mechanism of Toxicity • Powerful oxidizing capacity and hence Corrosive to mucous membranes • Decreased copper-metallothionein binding and copper clearance from the cell ( se free Cu) results in cellular death • Inactivation of enzymes such as G 6 PD and Glutathione Reductase (GSH) by reduced Cu(I) that binds to SH groups • Production of reactive toxic hydroxyl radicals by copper interacting with oxygen species by catalyzing production hydroxyl ions (e. g. superoxide anions and hydrogen peroxide)
 Mechanism of Hemolysis • Direct red cell membrane damage • Indirectly by inactivation of enzymes that protect against oxidative stress (including glutathione reductase)
Mechanism of Hemolysis • Direct red cell membrane damage • Indirectly by inactivation of enzymes that protect against oxidative stress (including glutathione reductase)
 Gastro Intestinal toxicity • Corrosive to mucous membranes • Ulceration of Gastric and duodenal mucosa • Haematemesis (frequently massive) and melaena • Vomiting, abdominal pain and diarrhoea • Hypersalivation and a metallic taste • Body secretions may be green or blue • Blue staining of the mouth, lips and oesophageal mucosa
Gastro Intestinal toxicity • Corrosive to mucous membranes • Ulceration of Gastric and duodenal mucosa • Haematemesis (frequently massive) and melaena • Vomiting, abdominal pain and diarrhoea • Hypersalivation and a metallic taste • Body secretions may be green or blue • Blue staining of the mouth, lips and oesophageal mucosa
 Hepatic toxicity • Excessive hepatic Cu produces cellular and obstructive damage. • 25 to 35% develop jaundice • Jaundice may be cholestatic, haemolytic or both • Jaundice, tender hepatomegaly with increased transaminase and alkaline phosphatase activities • Increase in serum caeruloplasmin concentrations until the third day post poisoning • There is decline in the ceruloplasmin level from 7 th day
Hepatic toxicity • Excessive hepatic Cu produces cellular and obstructive damage. • 25 to 35% develop jaundice • Jaundice may be cholestatic, haemolytic or both • Jaundice, tender hepatomegaly with increased transaminase and alkaline phosphatase activities • Increase in serum caeruloplasmin concentrations until the third day post poisoning • There is decline in the ceruloplasmin level from 7 th day
 Nephrotoxicity • Acute renal failure is a common complication • Secondary to – Hypovolaemic shock – Intravascular haemolysis. – Pigmentary nephropathy • Frequently occurs 3 to 4 days post poisoning • Dark-reddish coloured urine and oliguria. • Albuminuria, haematuria and haemoglobinuria
Nephrotoxicity • Acute renal failure is a common complication • Secondary to – Hypovolaemic shock – Intravascular haemolysis. – Pigmentary nephropathy • Frequently occurs 3 to 4 days post poisoning • Dark-reddish coloured urine and oliguria. • Albuminuria, haematuria and haemoglobinuria
 Hemotoxicity • Haemolytic anaemia is another common complication • Direct erythrocyte membrane damage • Indirectly by inhibition of enzymes protecting against oxidative stress, including G 6 PD and glutathione reductase • Hyperbilirubinaemia, reticulocytosis, haemoglobinaemia and a fall in haematocrit • Methaemoglobinaemia due to powerful oxidizing capacity
Hemotoxicity • Haemolytic anaemia is another common complication • Direct erythrocyte membrane damage • Indirectly by inhibition of enzymes protecting against oxidative stress, including G 6 PD and glutathione reductase • Hyperbilirubinaemia, reticulocytosis, haemoglobinaemia and a fall in haematocrit • Methaemoglobinaemia due to powerful oxidizing capacity
 Other toxicities • Pulmonary due to aspiration • Neurological due to hepatic or renal failure • Cardiac due to doubtful myocarditis Peripheral cyanosis, cardiac arrest • Rhabdomyolysis • Hyponatremia and hyperkalemia
Other toxicities • Pulmonary due to aspiration • Neurological due to hepatic or renal failure • Cardiac due to doubtful myocarditis Peripheral cyanosis, cardiac arrest • Rhabdomyolysis • Hyponatremia and hyperkalemia
 ACUTE COPPER SULPHATE POISON MANAGENENT
ACUTE COPPER SULPHATE POISON MANAGENENT
 Traditional Management • Gastric Lavage - Forced alkaline diuresis - D-Pencillamine (250 mg PO qid upto – 2 gms/ day) for 0 -7 days - Inj. Vitamin C 500 mgs 8 th hrly - H 2 Antagonist / PPI - Supportive measures for complications
Traditional Management • Gastric Lavage - Forced alkaline diuresis - D-Pencillamine (250 mg PO qid upto – 2 gms/ day) for 0 -7 days - Inj. Vitamin C 500 mgs 8 th hrly - H 2 Antagonist / PPI - Supportive measures for complications
 DISADVANTAGES OF TRADITIONAL MANAGEMENT
DISADVANTAGES OF TRADITIONAL MANAGEMENT
 Stomach in copper sulphate poisoning • Copper sulphate is a corrosive poisoning • Produces extensive ulceration and bleeding • Raw areas may hasten the absorption of cuso 4
Stomach in copper sulphate poisoning • Copper sulphate is a corrosive poisoning • Produces extensive ulceration and bleeding • Raw areas may hasten the absorption of cuso 4

 Sloughing of the mucosa
Sloughing of the mucosa
 Minimizing of corrosive injury of gastric mucosa • Avoidance of gastric lavage as in any corrosive poisons • Egg albumin to coat the mucosa and prevent injury
Minimizing of corrosive injury of gastric mucosa • Avoidance of gastric lavage as in any corrosive poisons • Egg albumin to coat the mucosa and prevent injury
 GASTROPROTECTIVE MEASURES • Stomach wash is to be avoided • Egg albumin to be used as demulcent • H 2 blockers or PPIs to hasten the healing of corrosive injury
GASTROPROTECTIVE MEASURES • Stomach wash is to be avoided • Egg albumin to be used as demulcent • H 2 blockers or PPIs to hasten the healing of corrosive injury
 Role of egg albumin in gastric protection • Coats the mucosa and protects further injury by the cuso 4 • Copper combine with albumin to form insoluble cupric albuminate • This reduces the corrosive effect of cuso 4
Role of egg albumin in gastric protection • Coats the mucosa and protects further injury by the cuso 4 • Copper combine with albumin to form insoluble cupric albuminate • This reduces the corrosive effect of cuso 4
 Egg albumin Cuso 4 absorption • Cupric albuminate is insoluble ( used for preserving paintings and photography) • Copper requires enzyme cytosolic methionine for its absorption • The enzyme may not act over insoluble Cupric albuminate poor absorption • Possibly by this mechanism systemic manifestations can be prevented
Egg albumin Cuso 4 absorption • Cupric albuminate is insoluble ( used for preserving paintings and photography) • Copper requires enzyme cytosolic methionine for its absorption • The enzyme may not act over insoluble Cupric albuminate poor absorption • Possibly by this mechanism systemic manifestations can be prevented
 Criteria for urinary alkalinization and forced diuresis • Should be predominantly eliminated unchanged by the kidney • Distributed primarily in the extracellular fluid compartment • Minimally protein-bound • Weak acids with p. H ranging from 3. 0 to 7. 5
Criteria for urinary alkalinization and forced diuresis • Should be predominantly eliminated unchanged by the kidney • Distributed primarily in the extracellular fluid compartment • Minimally protein-bound • Weak acids with p. H ranging from 3. 0 to 7. 5
 Forced alkaline diuresis • • • Copper sulphate does not fulfill the criteria Cycles to be properly monitored Close monitoring of the urine output is required Fluid overload may occur Studies indicate that there no advantage
Forced alkaline diuresis • • • Copper sulphate does not fulfill the criteria Cycles to be properly monitored Close monitoring of the urine output is required Fluid overload may occur Studies indicate that there no advantage
 Fluids in cuso 4 • • • Forced alkaline diuresis may be avoided Adequate replacement of fluids Close monitoring of the electrolytes Management of deficit Blood transfusion if there is hematemesis
Fluids in cuso 4 • • • Forced alkaline diuresis may be avoided Adequate replacement of fluids Close monitoring of the electrolytes Management of deficit Blood transfusion if there is hematemesis
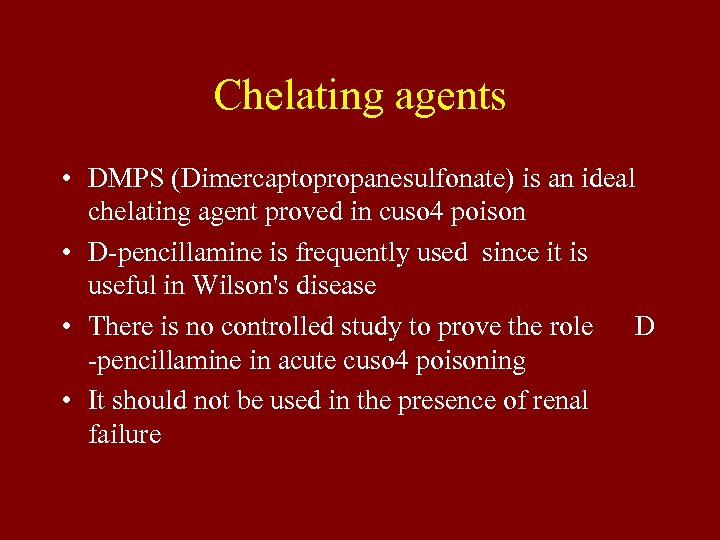 Chelating agents • DMPS (Dimercaptopropanesulfonate) is an ideal chelating agent proved in cuso 4 poison • D-pencillamine is frequently used since it is useful in Wilson's disease • There is no controlled study to prove the role D -pencillamine in acute cuso 4 poisoning • It should not be used in the presence of renal failure
Chelating agents • DMPS (Dimercaptopropanesulfonate) is an ideal chelating agent proved in cuso 4 poison • D-pencillamine is frequently used since it is useful in Wilson's disease • There is no controlled study to prove the role D -pencillamine in acute cuso 4 poisoning • It should not be used in the presence of renal failure
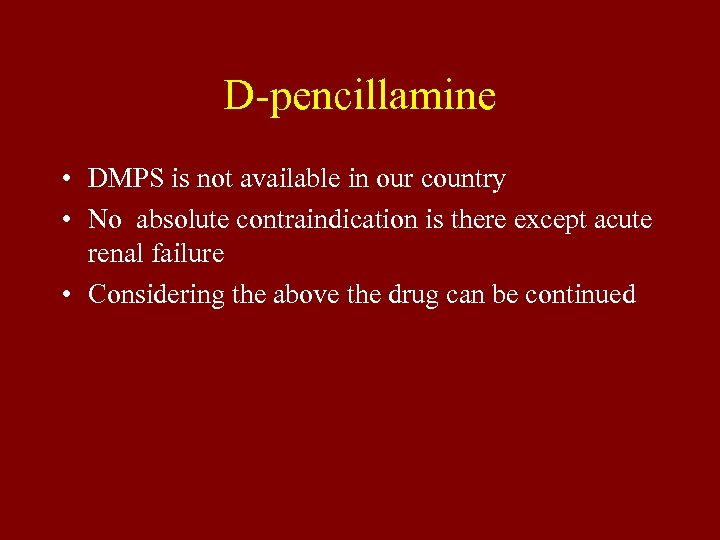 D-pencillamine • DMPS is not available in our country • No absolute contraindication is there except acute renal failure • Considering the above the drug can be continued
D-pencillamine • DMPS is not available in our country • No absolute contraindication is there except acute renal failure • Considering the above the drug can be continued
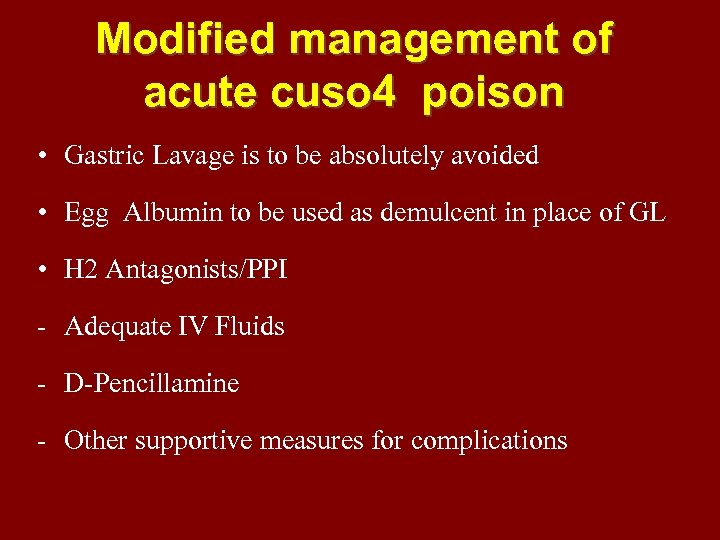 Modified management of acute cuso 4 poison • Gastric Lavage is to be absolutely avoided • Egg Albumin to be used as demulcent in place of GL • H 2 Antagonists/PPI - Adequate IV Fluids - D-Pencillamine - Other supportive measures for complications
Modified management of acute cuso 4 poison • Gastric Lavage is to be absolutely avoided • Egg Albumin to be used as demulcent in place of GL • H 2 Antagonists/PPI - Adequate IV Fluids - D-Pencillamine - Other supportive measures for complications
 ACUTE COPPER SULPHATE POISONING Comparative Study of the methods of treatment conducted at GOVERNMENT STANLEY MEDICAL COLLEGE 2004 TO 2006
ACUTE COPPER SULPHATE POISONING Comparative Study of the methods of treatment conducted at GOVERNMENT STANLEY MEDICAL COLLEGE 2004 TO 2006
 AIM To compare the mortality and morbidity of the traditional management protocol with modified protocol in acute copper sulphate poison
AIM To compare the mortality and morbidity of the traditional management protocol with modified protocol in acute copper sulphate poison
 Protocol-I Traditional Management • Gastric Lavage - Forced alkaline diuresis - D-Pencillamine (250 mg PO qid upto – 2 gms/ day) for 0 -7 days - Inj. Vitamin C 500 mgs 8 th hrly - H 2 Antagonist / PPI
Protocol-I Traditional Management • Gastric Lavage - Forced alkaline diuresis - D-Pencillamine (250 mg PO qid upto – 2 gms/ day) for 0 -7 days - Inj. Vitamin C 500 mgs 8 th hrly - H 2 Antagonist / PPI
 PROTOCOL – II Modified management • Gastric Lavage was Avoided - Egg Albumin was used as demulcent - Adequate IV Fluids - H 2 Antagonists/PPI - D-Pencillamine - Management of complications
PROTOCOL – II Modified management • Gastric Lavage was Avoided - Egg Albumin was used as demulcent - Adequate IV Fluids - H 2 Antagonists/PPI - D-Pencillamine - Management of complications
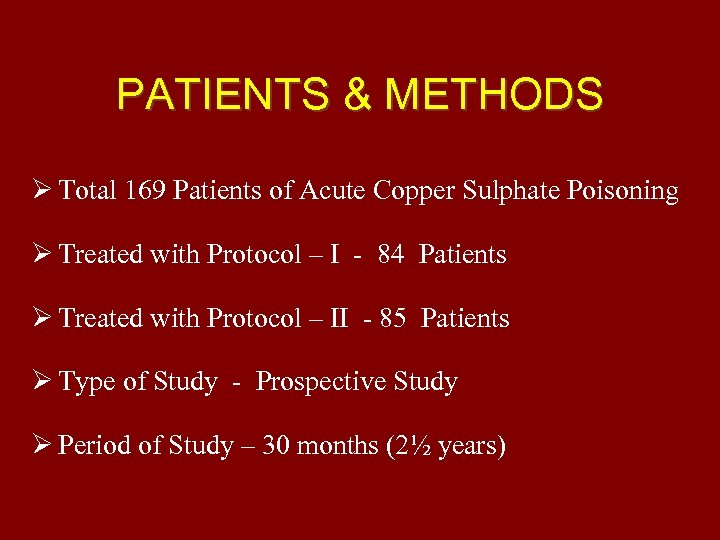 PATIENTS & METHODS Total 169 Patients of Acute Copper Sulphate Poisoning Treated with Protocol – I - 84 Patients Treated with Protocol – II - 85 Patients Type of Study - Prospective Study Period of Study – 30 months (2½ years)
PATIENTS & METHODS Total 169 Patients of Acute Copper Sulphate Poisoning Treated with Protocol – I - 84 Patients Treated with Protocol – II - 85 Patients Type of Study - Prospective Study Period of Study – 30 months (2½ years)
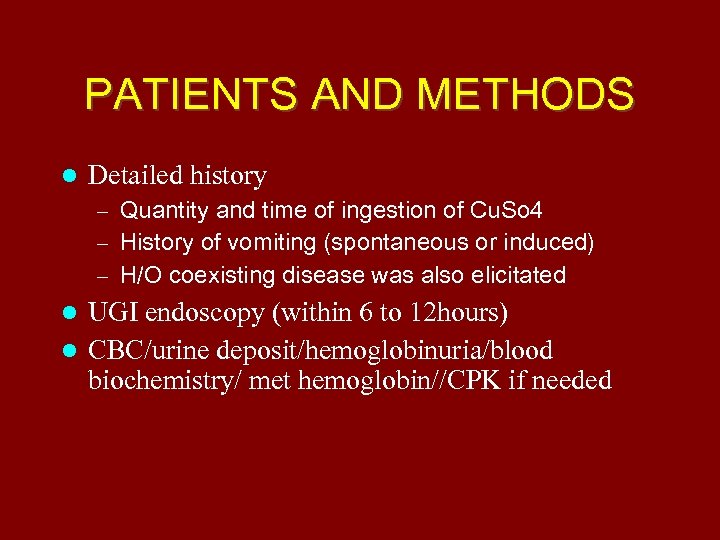 PATIENTS AND METHODS Detailed history – Quantity and time of ingestion of Cu. So 4 – History of vomiting (spontaneous or induced) – H/O coexisting disease was also elicitated UGI endoscopy (within 6 to 12 hours) CBC/urine deposit/hemoglobinuria/blood biochemistry/ met hemoglobin//CPK if needed
PATIENTS AND METHODS Detailed history – Quantity and time of ingestion of Cu. So 4 – History of vomiting (spontaneous or induced) – H/O coexisting disease was also elicitated UGI endoscopy (within 6 to 12 hours) CBC/urine deposit/hemoglobinuria/blood biochemistry/ met hemoglobin//CPK if needed
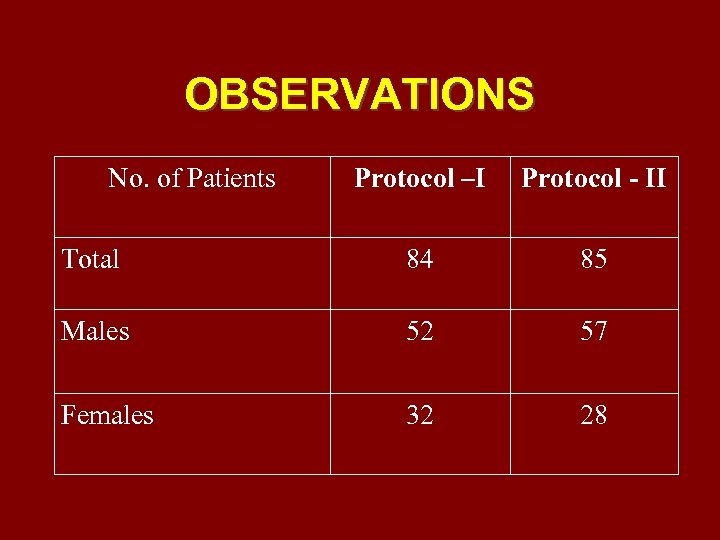 OBSERVATIONS No. of Patients Protocol –I Protocol - II Total 84 85 Males 52 57 Females 32 28
OBSERVATIONS No. of Patients Protocol –I Protocol - II Total 84 85 Males 52 57 Females 32 28
 Demographic data 84 85
Demographic data 84 85
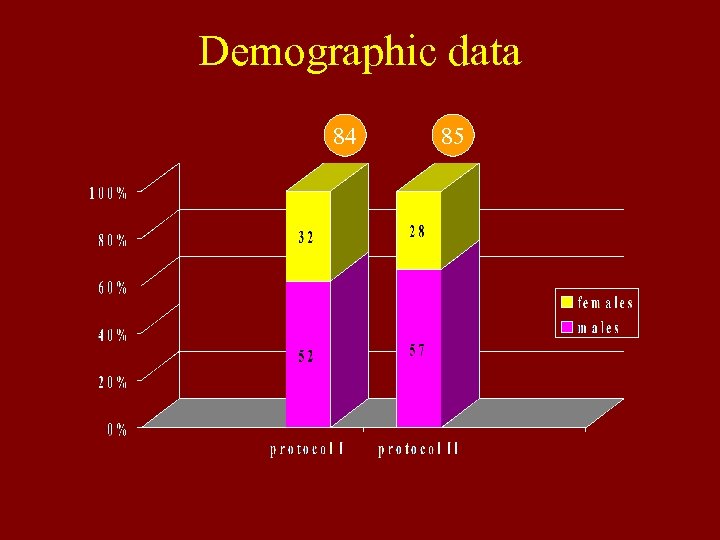
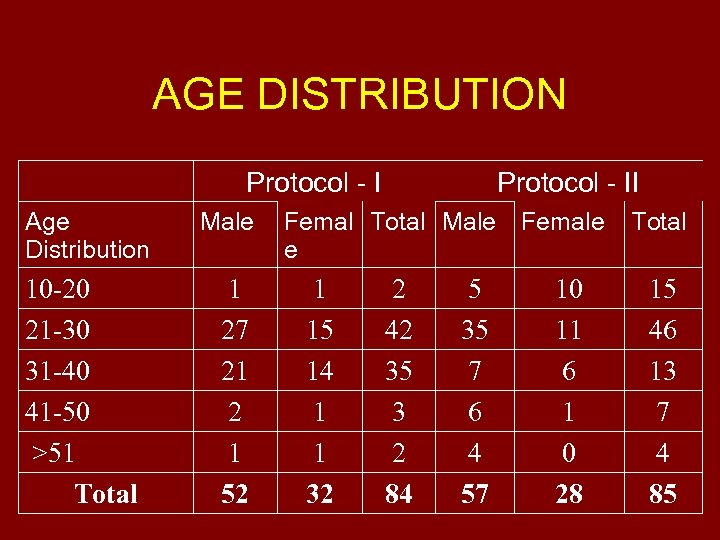 AGE DISTRIBUTION Protocol - I Age Distribution 10 -20 21 -30 31 -40 41 -50 >51 Total Male 1 27 21 2 1 52 Protocol - II Femal Total Male Female e 1 15 14 1 1 32 2 42 35 3 2 84 5 35 7 6 4 57 10 11 6 1 0 28 Total 15 46 13 7 4 85
AGE DISTRIBUTION Protocol - I Age Distribution 10 -20 21 -30 31 -40 41 -50 >51 Total Male 1 27 21 2 1 52 Protocol - II Femal Total Male Female e 1 15 14 1 1 32 2 42 35 3 2 84 5 35 7 6 4 57 10 11 6 1 0 28 Total 15 46 13 7 4 85
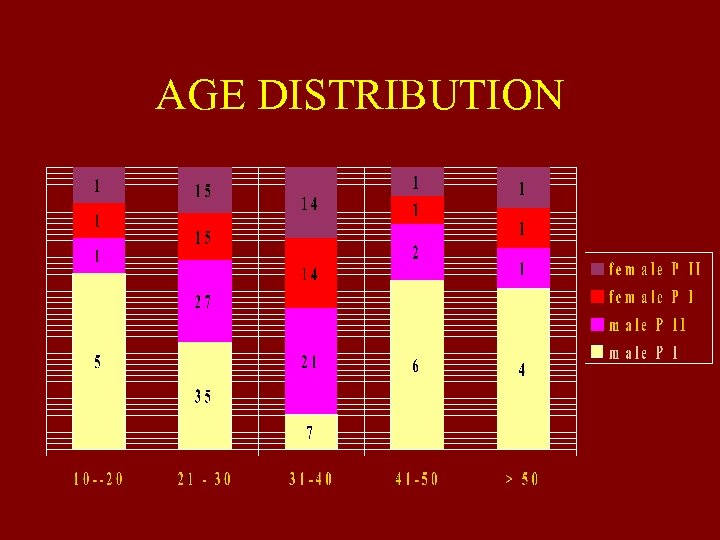 AGE DISTRIBUTION
AGE DISTRIBUTION
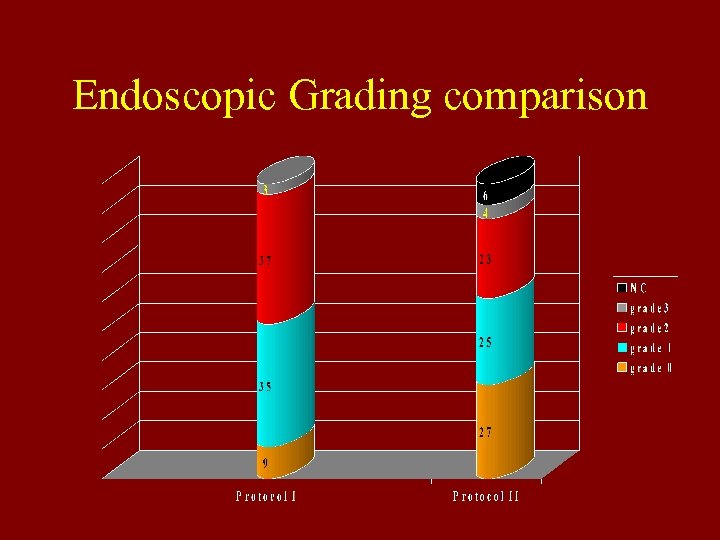 Endoscopic Grading comparison
Endoscopic Grading comparison
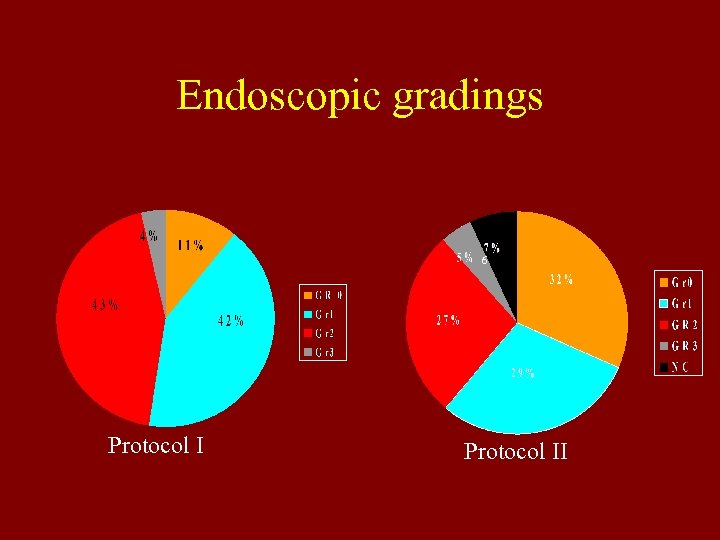 Endoscopic gradings 6 Protocol II
Endoscopic gradings 6 Protocol II
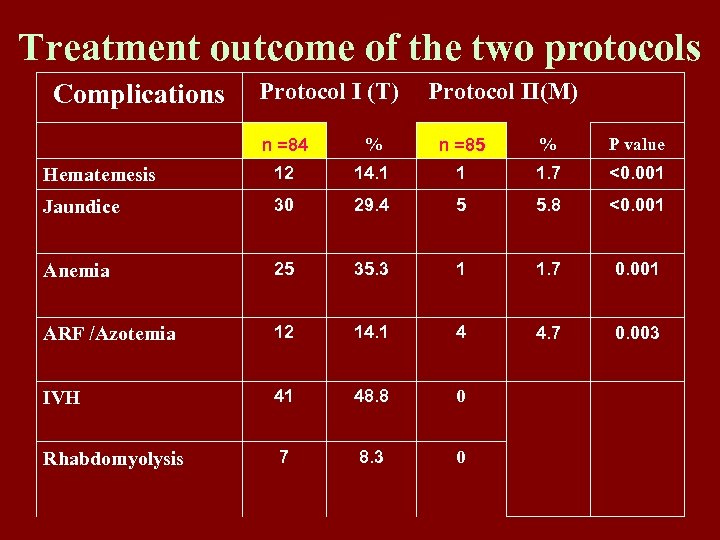 Treatment outcome of the two protocols Complications Protocol I (T) Protocol II(M) n =84 % n =85 % P value Hematemesis 12 14. 1 1 1. 7 <0. 001 Jaundice 30 29. 4 5 5. 8 <0. 001 Anemia 25 35. 3 1 1. 7 0. 001 ARF /Azotemia 12 14. 1 4 4. 7 0. 003 IVH 41 48. 8 0 Rhabdomyolysis 7 8. 3 0
Treatment outcome of the two protocols Complications Protocol I (T) Protocol II(M) n =84 % n =85 % P value Hematemesis 12 14. 1 1 1. 7 <0. 001 Jaundice 30 29. 4 5 5. 8 <0. 001 Anemia 25 35. 3 1 1. 7 0. 001 ARF /Azotemia 12 14. 1 4 4. 7 0. 003 IVH 41 48. 8 0 Rhabdomyolysis 7 8. 3 0
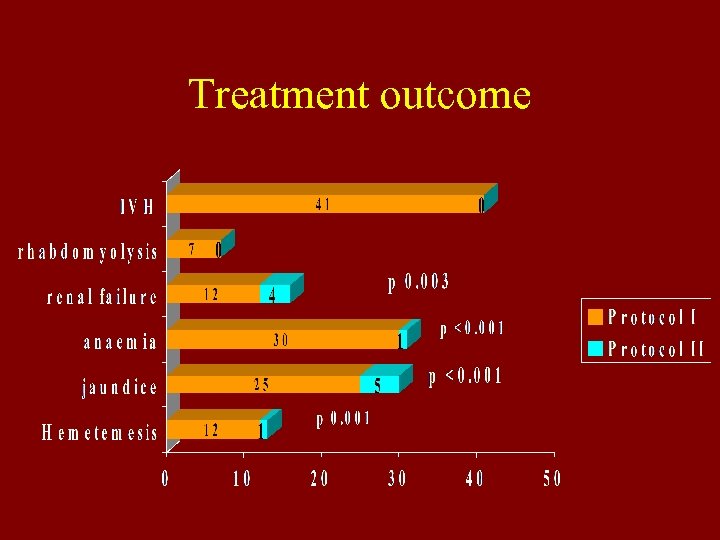 Treatment outcome
Treatment outcome
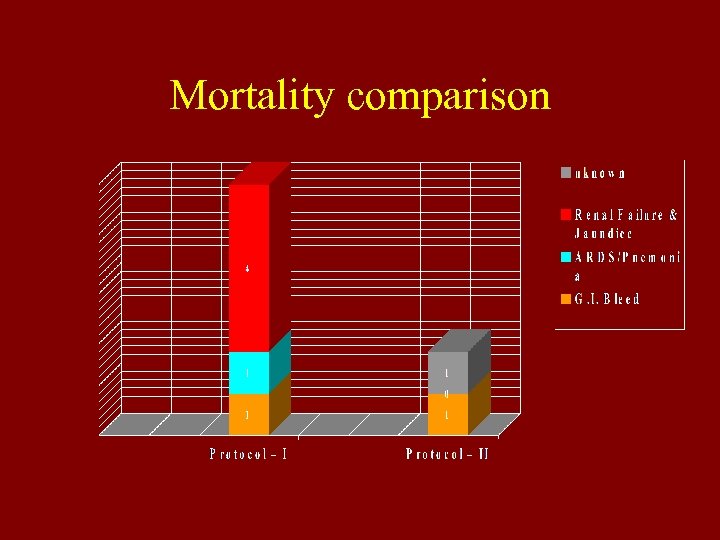 Mortality comparison
Mortality comparison
 AN ALTERNATE METHOD OF MANAGEMENT
AN ALTERNATE METHOD OF MANAGEMENT
 Recommendations • • • stomach wash to be deferred 6 – 8 raw egg white to be given orally H 2 blockers / PPIs to heal the corrosive injuries. Adequate fluid replacement D-Penicillamine if there is no contraindication Appropriate Management of complications
Recommendations • • • stomach wash to be deferred 6 – 8 raw egg white to be given orally H 2 blockers / PPIs to heal the corrosive injuries. Adequate fluid replacement D-Penicillamine if there is no contraindication Appropriate Management of complications
 ADVANTAGES OF THE MODIFIED TREATMENT • Management can start at the community level at the patient’s house (egg white) • Can be carried out by health worker (does not require instruments and equipments) • Can be managed at the primary care physicians (needs only adequate IV Fluids and observation) • Patients with complications only may require secondary or tertiary care
ADVANTAGES OF THE MODIFIED TREATMENT • Management can start at the community level at the patient’s house (egg white) • Can be carried out by health worker (does not require instruments and equipments) • Can be managed at the primary care physicians (needs only adequate IV Fluids and observation) • Patients with complications only may require secondary or tertiary care
 Training the community (health education) • Encourage the patient to vomit • Avoid inducing vomiting (may lead to aspiration into the lung) • Give patient 6 to 8 egg white provided the victim is conscious • Contact the health worker or shift to the nearest hospital
Training the community (health education) • Encourage the patient to vomit • Avoid inducing vomiting (may lead to aspiration into the lung) • Give patient 6 to 8 egg white provided the victim is conscious • Contact the health worker or shift to the nearest hospital
 Role of community health worker • To follow the instructions given to the community • Positioning the patient who is vomiting to avoid aspiration • Watch the patient the vital signs • Shift the victim to the PHC
Role of community health worker • To follow the instructions given to the community • Positioning the patient who is vomiting to avoid aspiration • Watch the patient the vital signs • Shift the victim to the PHC
 Role of the primary care physicians • Monitor the patient for the signs of shock and haematemesis • Use H 2 blockers or Proton pump inhibitors • Give adequate iv fluids to maintain the urinary output • Watch for hematuria and hemogloninuria • Follow up the patient especially from the third day for jaundice and renal failure
Role of the primary care physicians • Monitor the patient for the signs of shock and haematemesis • Use H 2 blockers or Proton pump inhibitors • Give adequate iv fluids to maintain the urinary output • Watch for hematuria and hemogloninuria • Follow up the patient especially from the third day for jaundice and renal failure
 Acknowledgement • Prof. Sivakumar Dept. of Medicine SMC • Prof. Natarajan HOD Dept. of Medicine SMC • Dr. Nambirajan/ Dr. Jayakumar/Dr. Chandrasekaran Asst. Professors of Medicine SMC • Dr. P. Senthilkumar MD Postgraduate SMC • All the staff of IMCW SMC • Prof. Thirumalaikolundu Subramanian Director of Internal Medicine MMC
Acknowledgement • Prof. Sivakumar Dept. of Medicine SMC • Prof. Natarajan HOD Dept. of Medicine SMC • Dr. Nambirajan/ Dr. Jayakumar/Dr. Chandrasekaran Asst. Professors of Medicine SMC • Dr. P. Senthilkumar MD Postgraduate SMC • All the staff of IMCW SMC • Prof. Thirumalaikolundu Subramanian Director of Internal Medicine MMC
 To agree or not
To agree or not


