b31ad04ac2f9d965340db00f14f2afdd.ppt
- Количество слайдов: 33
 Managed Care and Homeless Populations: Linking the HCH Community and MCO Partners April 5, 2016
Managed Care and Homeless Populations: Linking the HCH Community and MCO Partners April 5, 2016
 Welcome Speakers: Learning Objectives: • Catherine Anderson, Vice President, Positioning and Strategy, United. Healthcare Community & State • Understand the factors influencing Medicaid managed care plans and their approach to serving people experiencing homelessness and how they are seeking opportunities to partner with providers serving the population • Understand how the HCH Community can maximize common goals with managed care plans • Describe how two Health Care for the Homeless projects in Washington State (one urban and one rural) are partnering with a managed care plan for medical respite services. • Barbara Di. Pietro, Senior Director of Policy, National HCH Council • Doug Bowes, CEO, United. Healthcare Community Plan of Washington • Edward Dwyer-O'Connor, BS, RN, Senior Manager, Downtown Programs, Harborview Medical Center, Seattle, WA • Matt Lund, Director of Contracting, UW Medicine at Harborview Medical Center, Seattle, WA • Rhonda Hauff, COO/Deputy CEO, Yakima Neighborhood Health, Yakima, WA 2
Welcome Speakers: Learning Objectives: • Catherine Anderson, Vice President, Positioning and Strategy, United. Healthcare Community & State • Understand the factors influencing Medicaid managed care plans and their approach to serving people experiencing homelessness and how they are seeking opportunities to partner with providers serving the population • Understand how the HCH Community can maximize common goals with managed care plans • Describe how two Health Care for the Homeless projects in Washington State (one urban and one rural) are partnering with a managed care plan for medical respite services. • Barbara Di. Pietro, Senior Director of Policy, National HCH Council • Doug Bowes, CEO, United. Healthcare Community Plan of Washington • Edward Dwyer-O'Connor, BS, RN, Senior Manager, Downtown Programs, Harborview Medical Center, Seattle, WA • Matt Lund, Director of Contracting, UW Medicine at Harborview Medical Center, Seattle, WA • Rhonda Hauff, COO/Deputy CEO, Yakima Neighborhood Health, Yakima, WA 2
 Background on Initiative • • 2015 Healthcare for the Homeless Annual Conference • Began conversations • Co-wrote the white paper and developed today’s webinar • 3 Recognized Interest Beginning to an on-going conversation
Background on Initiative • • 2015 Healthcare for the Homeless Annual Conference • Began conversations • Co-wrote the white paper and developed today’s webinar • 3 Recognized Interest Beginning to an on-going conversation
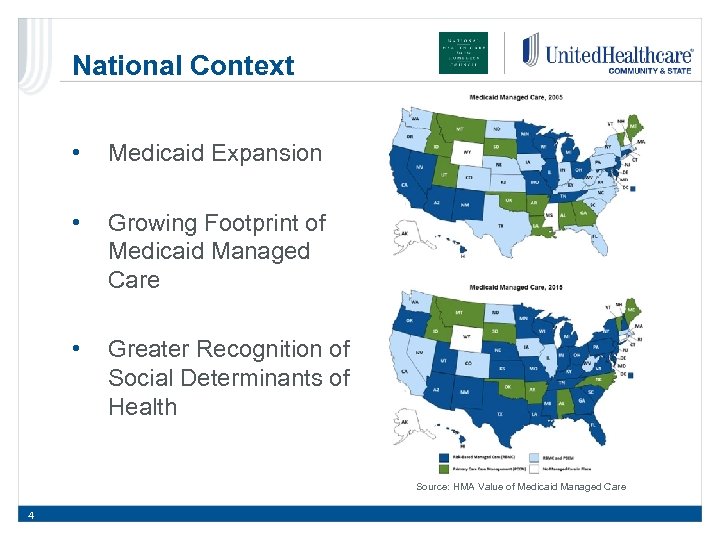 National Context • Medicaid Expansion • Growing Footprint of Medicaid Managed Care • Greater Recognition of Social Determinants of Health Source: HMA Value of Medicaid Managed Care 4
National Context • Medicaid Expansion • Growing Footprint of Medicaid Managed Care • Greater Recognition of Social Determinants of Health Source: HMA Value of Medicaid Managed Care 4
 Medicaid Managed Care Source: Architect of the Capitol Federal Government • Establishes basic rules and criteria States must follow in the design and operation of a Medicaid program • Covers a significant portion of the costs of Medicaid (varies by state and population) • Approves contracts and rates between states and managed care entities State Governments • Establish program rules, benefits, eligibility, contract provisions and the rates health plans will be paid to administer the Medicaid program • Compensates the health plans using a per member per month capitated rate Health Plans • Administer the Medicaid program according to the terms of the contract with the state for their assigned Medicaid beneficiaries • Measured on ability to support their members in receiving preventive treatment, achieving state goals, and meeting other quality metrics established by the state • Established contracts with providers 5 Proprietary Information of United. Health Group. Do not distribute or reproduce without express permission of United. Health Group.
Medicaid Managed Care Source: Architect of the Capitol Federal Government • Establishes basic rules and criteria States must follow in the design and operation of a Medicaid program • Covers a significant portion of the costs of Medicaid (varies by state and population) • Approves contracts and rates between states and managed care entities State Governments • Establish program rules, benefits, eligibility, contract provisions and the rates health plans will be paid to administer the Medicaid program • Compensates the health plans using a per member per month capitated rate Health Plans • Administer the Medicaid program according to the terms of the contract with the state for their assigned Medicaid beneficiaries • Measured on ability to support their members in receiving preventive treatment, achieving state goals, and meeting other quality metrics established by the state • Established contracts with providers 5 Proprietary Information of United. Health Group. Do not distribute or reproduce without express permission of United. Health Group.
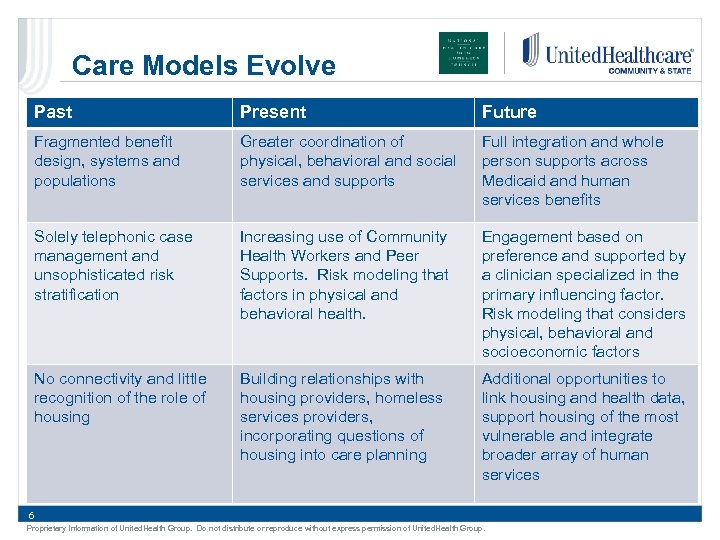 Care Models Evolve Past Present Future Fragmented benefit design, systems and populations Greater coordination of physical, behavioral and social services and supports Full integration and whole person supports across Medicaid and human services benefits Solely telephonic case management and unsophisticated risk stratification Increasing use of Community Health Workers and Peer Supports. Risk modeling that factors in physical and behavioral health. Engagement based on preference and supported by a clinician specialized in the primary influencing factor. Risk modeling that considers physical, behavioral and socioeconomic factors No connectivity and little recognition of the role of housing Building relationships with housing providers, homeless services providers, incorporating questions of housing into care planning Additional opportunities to link housing and health data, support housing of the most vulnerable and integrate broader array of human services 6 Proprietary Information of United. Health Group. Do not distribute or reproduce without express permission of United. Health Group.
Care Models Evolve Past Present Future Fragmented benefit design, systems and populations Greater coordination of physical, behavioral and social services and supports Full integration and whole person supports across Medicaid and human services benefits Solely telephonic case management and unsophisticated risk stratification Increasing use of Community Health Workers and Peer Supports. Risk modeling that factors in physical and behavioral health. Engagement based on preference and supported by a clinician specialized in the primary influencing factor. Risk modeling that considers physical, behavioral and socioeconomic factors No connectivity and little recognition of the role of housing Building relationships with housing providers, homeless services providers, incorporating questions of housing into care planning Additional opportunities to link housing and health data, support housing of the most vulnerable and integrate broader array of human services 6 Proprietary Information of United. Health Group. Do not distribute or reproduce without express permission of United. Health Group.
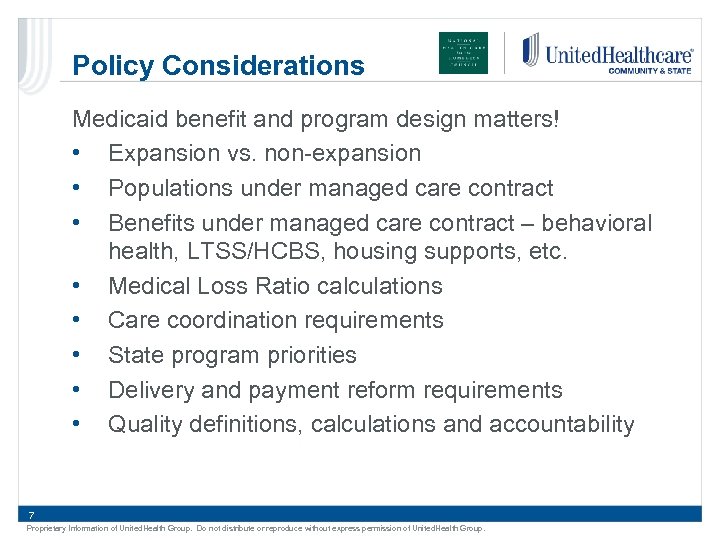 Policy Considerations Medicaid benefit and program design matters! • Expansion vs. non-expansion • Populations under managed care contract • Benefits under managed care contract – behavioral health, LTSS/HCBS, housing supports, etc. • Medical Loss Ratio calculations • Care coordination requirements • State program priorities • Delivery and payment reform requirements • Quality definitions, calculations and accountability 7 Proprietary Information of United. Health Group. Do not distribute or reproduce without express permission of United. Health Group.
Policy Considerations Medicaid benefit and program design matters! • Expansion vs. non-expansion • Populations under managed care contract • Benefits under managed care contract – behavioral health, LTSS/HCBS, housing supports, etc. • Medical Loss Ratio calculations • Care coordination requirements • State program priorities • Delivery and payment reform requirements • Quality definitions, calculations and accountability 7 Proprietary Information of United. Health Group. Do not distribute or reproduce without express permission of United. Health Group.
 Needed for Success • Countless opportunities to collaborate exist, but resources and capacity on both sides are limited • Evaluating opportunities: • • Members impacted Opportunity to improve quality Opportunity to improve utilization Data available to support the decision to invest, track and demonstrate impact • Presence of trusted partners willing to innovate with unique skills and expertise 8 Proprietary Information of United. Health Group. Do not distribute or reproduce without express permission of United. Health Group.
Needed for Success • Countless opportunities to collaborate exist, but resources and capacity on both sides are limited • Evaluating opportunities: • • Members impacted Opportunity to improve quality Opportunity to improve utilization Data available to support the decision to invest, track and demonstrate impact • Presence of trusted partners willing to innovate with unique skills and expertise 8 Proprietary Information of United. Health Group. Do not distribute or reproduce without express permission of United. Health Group.
 Washington Panel on MCO & HCH Collaborations 9
Washington Panel on MCO & HCH Collaborations 9
 Washington Panel • Doug Bowes, CEO, United. Healthcare Community Plan of Washington • Edward Dwyer-O'Connor, BS, RN, Senior Manager, Downtown Programs, Harborview Medical Center, Seattle, WA • Matt Lund, Director of Contracting, UW Medicine at Harborview Medical Center, Seattle, WA • Rhonda Hauff, COO/Deputy CEO, Yakima Neighborhood Health, Yakima, WA 10 Proprietary Information of United. Health Group. Do not distribute or reproduce without express permission of United. Health Group.
Washington Panel • Doug Bowes, CEO, United. Healthcare Community Plan of Washington • Edward Dwyer-O'Connor, BS, RN, Senior Manager, Downtown Programs, Harborview Medical Center, Seattle, WA • Matt Lund, Director of Contracting, UW Medicine at Harborview Medical Center, Seattle, WA • Rhonda Hauff, COO/Deputy CEO, Yakima Neighborhood Health, Yakima, WA 10 Proprietary Information of United. Health Group. Do not distribute or reproduce without express permission of United. Health Group.
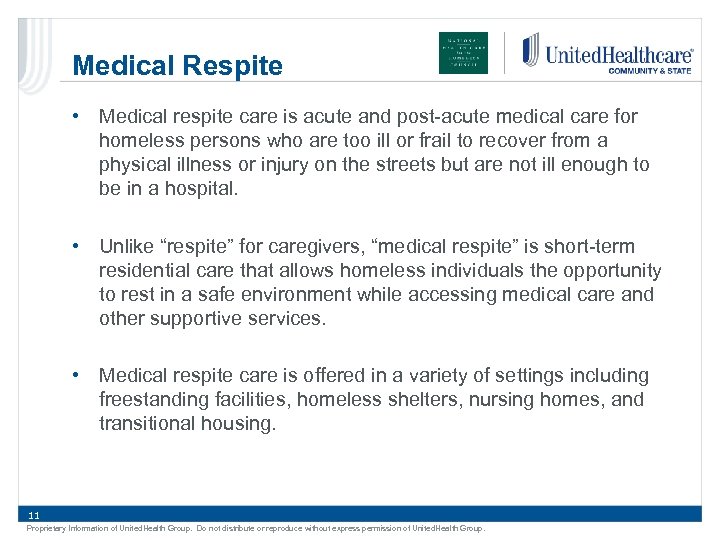 Medical Respite • Medical respite care is acute and post-acute medical care for homeless persons who are too ill or frail to recover from a physical illness or injury on the streets but are not ill enough to be in a hospital. • Unlike “respite” for caregivers, “medical respite” is short-term residential care that allows homeless individuals the opportunity to rest in a safe environment while accessing medical care and other supportive services. • Medical respite care is offered in a variety of settings including freestanding facilities, homeless shelters, nursing homes, and transitional housing. 11 Proprietary Information of United. Health Group. Do not distribute or reproduce without express permission of United. Health Group.
Medical Respite • Medical respite care is acute and post-acute medical care for homeless persons who are too ill or frail to recover from a physical illness or injury on the streets but are not ill enough to be in a hospital. • Unlike “respite” for caregivers, “medical respite” is short-term residential care that allows homeless individuals the opportunity to rest in a safe environment while accessing medical care and other supportive services. • Medical respite care is offered in a variety of settings including freestanding facilities, homeless shelters, nursing homes, and transitional housing. 11 Proprietary Information of United. Health Group. Do not distribute or reproduce without express permission of United. Health Group.
 Washington Context • United. Healthcare Community Plan is the third largest Medicaid managed care plan in Washington State providing physical health benefits and services to more than 210, 000 members • We provide face-to-face and telephonic care coordination services for our most complex members, including many that are homeless • Washington Medicaid program has continually sought significant reforms and modernization including: o Medicaid Expansion o State Innovation Model o 1115 waiver with Movement toward Grant significant delivery integrated physical and o Accountable system reforms behavioral health Communities of Health o 12 Proprietary Information of United. Health Group. Do not distribute or reproduce without express permission of United. Health Group.
Washington Context • United. Healthcare Community Plan is the third largest Medicaid managed care plan in Washington State providing physical health benefits and services to more than 210, 000 members • We provide face-to-face and telephonic care coordination services for our most complex members, including many that are homeless • Washington Medicaid program has continually sought significant reforms and modernization including: o Medicaid Expansion o State Innovation Model o 1115 waiver with Movement toward Grant significant delivery integrated physical and o Accountable system reforms behavioral health Communities of Health o 12 Proprietary Information of United. Health Group. Do not distribute or reproduce without express permission of United. Health Group.
 Health Plan Journey • Recognized need • Built off Established Relationships • Learned about Jefferson Terrace Program • Made the case internally • Worked out the details and executed contract • Replicated with Yakima Neighborhood Health Services • Continuing to look for ways to improve coordination, care transition and evaluation 13 Proprietary Information of United. Health Group. Do not distribute or reproduce without express permission of United. Health Group.
Health Plan Journey • Recognized need • Built off Established Relationships • Learned about Jefferson Terrace Program • Made the case internally • Worked out the details and executed contract • Replicated with Yakima Neighborhood Health Services • Continuing to look for ways to improve coordination, care transition and evaluation 13 Proprietary Information of United. Health Group. Do not distribute or reproduce without express permission of United. Health Group.
 Value of Collaboration • We were interested in seeing to it that our members were able to access the care and recovery environment they needed and to keep them from facing recovery and recuperation on the streets or in a shelter. o Reducing hospital readmissions o Improving the health of the member • Partnering with medical respite helps to create an essential care linkage opening the door to additional physical and behavioral health care coordination and holistic social support services, all of which uphold our driving goal of the Triple Aim. 14 Proprietary Information of United. Health Group. Do not distribute or reproduce without express permission of United. Health Group.
Value of Collaboration • We were interested in seeing to it that our members were able to access the care and recovery environment they needed and to keep them from facing recovery and recuperation on the streets or in a shelter. o Reducing hospital readmissions o Improving the health of the member • Partnering with medical respite helps to create an essential care linkage opening the door to additional physical and behavioral health care coordination and holistic social support services, all of which uphold our driving goal of the Triple Aim. 14 Proprietary Information of United. Health Group. Do not distribute or reproduce without express permission of United. Health Group.
 Edward Thomas House • • Respite history in Seattle Free-standing unit in Jefferson Terrace/SHA/HUD Harm Reduction Program/34 beds Designed for high medical and behavioral acuity Braided funding; money from 6 hospitals, Public Health – HUD, HRSA, local MIDD funding and MCOs. Hospitals needed IV antibiotic treatment for IVDU 475 patients/year. LOS 21 days. 15 Proprietary Information of United. Health Group. Do not distribute or reproduce without express permission of United. Health Group.
Edward Thomas House • • Respite history in Seattle Free-standing unit in Jefferson Terrace/SHA/HUD Harm Reduction Program/34 beds Designed for high medical and behavioral acuity Braided funding; money from 6 hospitals, Public Health – HUD, HRSA, local MIDD funding and MCOs. Hospitals needed IV antibiotic treatment for IVDU 475 patients/year. LOS 21 days. 15 Proprietary Information of United. Health Group. Do not distribute or reproduce without express permission of United. Health Group.
 WHO DOES RESPITE SERVE? • • • Homeless men and women with complex needs [too sick for the streets, not sick enough for the hospital] Acute medical issues; often abscesses and infections R/T IVDU IV antibiotics often 4 -6 weeks Multiple chronic conditions Preponderance of chemical dependency plus mental illness Patients must be independent in mobility [wheelchair OK] Behavior must be safe for the setting [no threats, violence, weapons] Cannot use drugs on the unit Able to serve much higher acuity [staff includes MD, ARNPs, RNs, MHPs, MHSs, Mas, custodial and data manager] Goals for care include; access to entitlements, primary care, case management services, housing, opiate replacement therapy, chemical dependency treatment Client story
WHO DOES RESPITE SERVE? • • • Homeless men and women with complex needs [too sick for the streets, not sick enough for the hospital] Acute medical issues; often abscesses and infections R/T IVDU IV antibiotics often 4 -6 weeks Multiple chronic conditions Preponderance of chemical dependency plus mental illness Patients must be independent in mobility [wheelchair OK] Behavior must be safe for the setting [no threats, violence, weapons] Cannot use drugs on the unit Able to serve much higher acuity [staff includes MD, ARNPs, RNs, MHPs, MHSs, Mas, custodial and data manager] Goals for care include; access to entitlements, primary care, case management services, housing, opiate replacement therapy, chemical dependency treatment Client story
 APPROACH • Risk sharing and collaboration • Search for innovative ways to provide care for underserved, high cost patients • Manage the whole person • Look for leverage points in the Triple Aim • Reduce costa • Improve outcomes • Find data to support outcomes and decreased costs [EDH study of 69 patients showed 70% reduction in hospital days 6 months post respite compared to 6 months pre-respite, a 57% reduction in inpatient admissions also decrease ED visits by 10%] • MCOs could not pay for respite stay, needed Health Care Authority to allow payment
APPROACH • Risk sharing and collaboration • Search for innovative ways to provide care for underserved, high cost patients • Manage the whole person • Look for leverage points in the Triple Aim • Reduce costa • Improve outcomes • Find data to support outcomes and decreased costs [EDH study of 69 patients showed 70% reduction in hospital days 6 months post respite compared to 6 months pre-respite, a 57% reduction in inpatient admissions also decrease ED visits by 10%] • MCOs could not pay for respite stay, needed Health Care Authority to allow payment
 Path to a Contract • Gained authorization from state Medicaid agency to bill/reimburse for respite care • Directed to bill and reimburse under G 9006 “Coordinated Care Fee, Home Monitoring” • Determined how and how much to charge • Consulted revenue cycle, contracting, utilization management, and social work departments to ensure full understanding of work flows • Assembled helpful data and analysis demonstrating efficacy and cost effectiveness of program • Hosted tours of facility for managed Medicaid plan reps • Approached managed Medicaid plans with pitch to contract for respite services
Path to a Contract • Gained authorization from state Medicaid agency to bill/reimburse for respite care • Directed to bill and reimburse under G 9006 “Coordinated Care Fee, Home Monitoring” • Determined how and how much to charge • Consulted revenue cycle, contracting, utilization management, and social work departments to ensure full understanding of work flows • Assembled helpful data and analysis demonstrating efficacy and cost effectiveness of program • Hosted tours of facility for managed Medicaid plan reps • Approached managed Medicaid plans with pitch to contract for respite services
 Contract • Coverage and reimbursement established through amendment to existing agreements • Discussed possible models for reimbursement (per diem, case rate, etc. ) • Discussed: concurrent review/UM needs, program definitions, scope of services, other expectations • Negotiated key terms, executed amendments, and monitored events (care delivered, charges issued, reimbursements paid, problems solved, lessons learned) • Agreement to meet and discuss specs, successes/challenges, and needs on a regular basis • Recognition of cost savings and improvement of individual and population health
Contract • Coverage and reimbursement established through amendment to existing agreements • Discussed possible models for reimbursement (per diem, case rate, etc. ) • Discussed: concurrent review/UM needs, program definitions, scope of services, other expectations • Negotiated key terms, executed amendments, and monitored events (care delivered, charges issued, reimbursements paid, problems solved, lessons learned) • Agreement to meet and discuss specs, successes/challenges, and needs on a regular basis • Recognition of cost savings and improvement of individual and population health
 YNHS Mission To provide accessible, affordable, quality health care, promote learning opportunities for students of health professions, end homelessness and improve quality of life in our communities. 20
YNHS Mission To provide accessible, affordable, quality health care, promote learning opportunities for students of health professions, end homelessness and improve quality of life in our communities. 20
 Satellites Serve Special Populations Homeless Respite - Recuperative Housing for those not sick enough to be in the hospital, and those discharged from the hospital but not well enough to go back to the streets 21
Satellites Serve Special Populations Homeless Respite - Recuperative Housing for those not sick enough to be in the hospital, and those discharged from the hospital but not well enough to go back to the streets 21
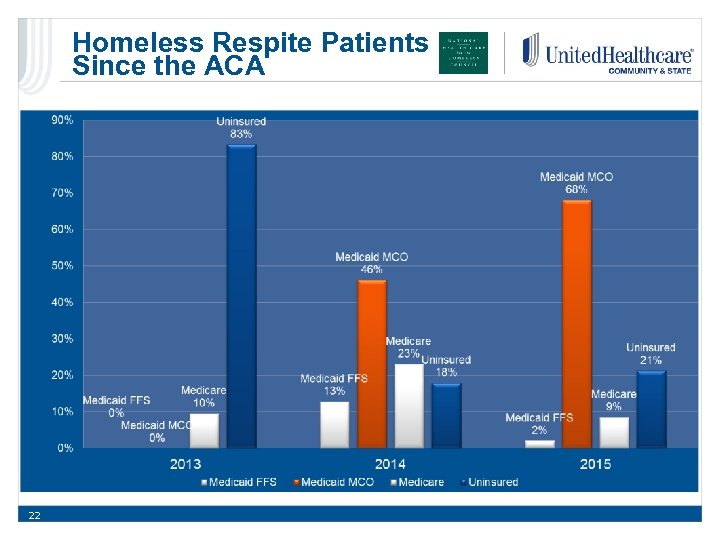 Homeless Respite Patients Since the ACA 22
Homeless Respite Patients Since the ACA 22
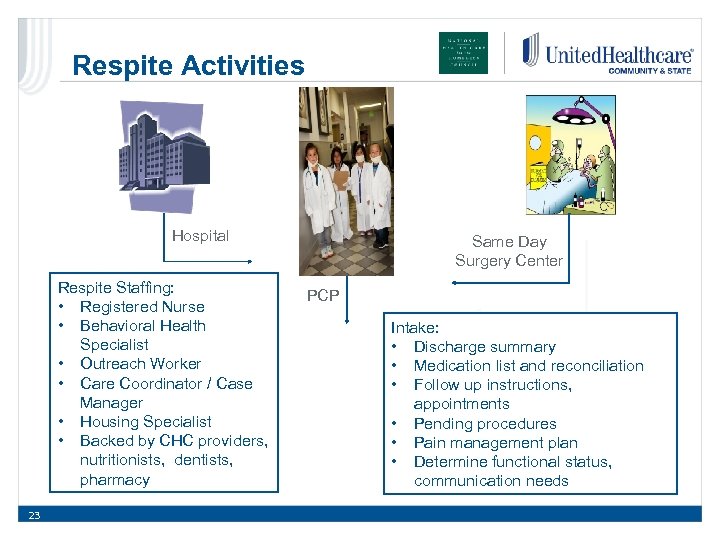 Respite Activities Hospital Respite Staffing: • Registered Nurse • Behavioral Health Specialist • Outreach Worker • Care Coordinator / Case Manager • Housing Specialist • Backed by CHC providers, nutritionists, dentists, pharmacy 23 Same Day Surgery Center PCP Intake: • Discharge summary • Medication list and reconciliation • Follow up instructions, appointments • Pending procedures • Pain management plan • Determine functional status, communication needs
Respite Activities Hospital Respite Staffing: • Registered Nurse • Behavioral Health Specialist • Outreach Worker • Care Coordinator / Case Manager • Housing Specialist • Backed by CHC providers, nutritionists, dentists, pharmacy 23 Same Day Surgery Center PCP Intake: • Discharge summary • Medication list and reconciliation • Follow up instructions, appointments • Pending procedures • Pain management plan • Determine functional status, communication needs
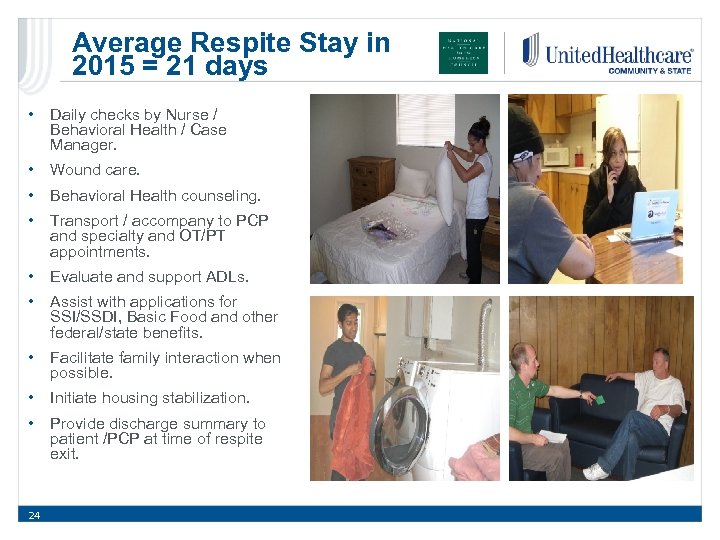 Average Respite Stay in 2015 = 21 days • Daily checks by Nurse / Behavioral Health / Case Manager. • Wound care. • Behavioral Health counseling. • Transport / accompany to PCP and specialty and OT/PT appointments. • Evaluate and support ADLs. • Assist with applications for SSI/SSDI, Basic Food and other federal/state benefits. • Facilitate family interaction when possible. • Initiate housing stabilization. • Provide discharge summary to patient /PCP at time of respite exit. 24
Average Respite Stay in 2015 = 21 days • Daily checks by Nurse / Behavioral Health / Case Manager. • Wound care. • Behavioral Health counseling. • Transport / accompany to PCP and specialty and OT/PT appointments. • Evaluate and support ADLs. • Assist with applications for SSI/SSDI, Basic Food and other federal/state benefits. • Facilitate family interaction when possible. • Initiate housing stabilization. • Provide discharge summary to patient /PCP at time of respite exit. 24
 Help is On the Way… SIESTAS Serving Individuals to End Serious Trouble through Agencies’ Support 25 Who do we SIESTA: • Chronic medical or social needs • Cause upheaval in the social service system • Seen by multiple service providers • Use a LOT of resources - repeatedly
Help is On the Way… SIESTAS Serving Individuals to End Serious Trouble through Agencies’ Support 25 Who do we SIESTA: • Chronic medical or social needs • Cause upheaval in the social service system • Seen by multiple service providers • Use a LOT of resources - repeatedly
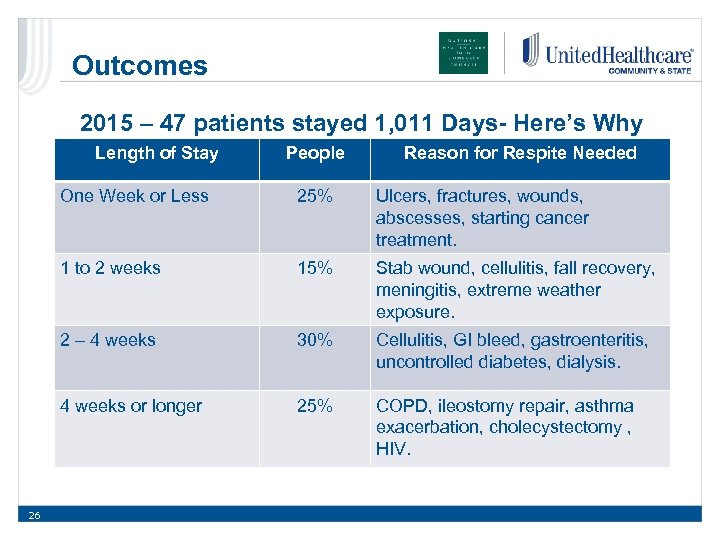 Outcomes 2015 – 47 patients stayed 1, 011 Days- Here’s Why Length of Stay People Reason for Respite Needed One Week or Less Ulcers, fractures, wounds, abscesses, starting cancer treatment. 1 to 2 weeks 15% Stab wound, cellulitis, fall recovery, meningitis, extreme weather exposure. 2 – 4 weeks 30% Cellulitis, GI bleed, gastroenteritis, uncontrolled diabetes, dialysis. 4 weeks or longer 26 25% COPD, ileostomy repair, asthma exacerbation, cholecystectomy , HIV.
Outcomes 2015 – 47 patients stayed 1, 011 Days- Here’s Why Length of Stay People Reason for Respite Needed One Week or Less Ulcers, fractures, wounds, abscesses, starting cancer treatment. 1 to 2 weeks 15% Stab wound, cellulitis, fall recovery, meningitis, extreme weather exposure. 2 – 4 weeks 30% Cellulitis, GI bleed, gastroenteritis, uncontrolled diabetes, dialysis. 4 weeks or longer 26 25% COPD, ileostomy repair, asthma exacerbation, cholecystectomy , HIV.
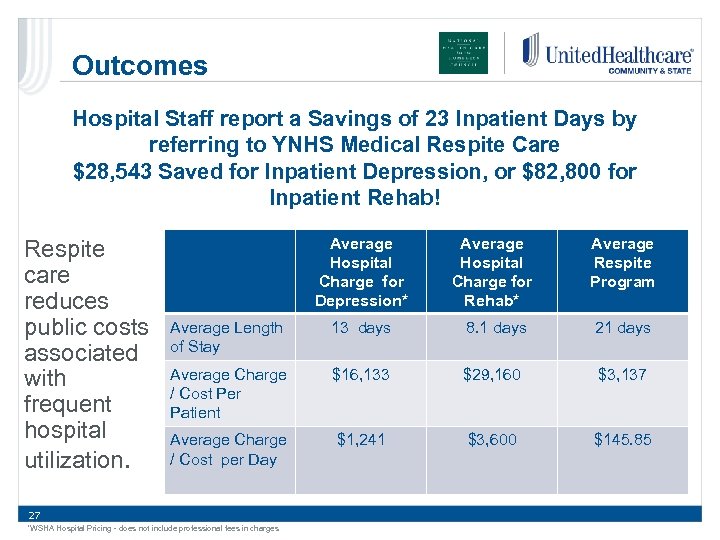 Outcomes Hospital Staff report a Savings of 23 Inpatient Days by referring to YNHS Medical Respite Care $28, 543 Saved for Inpatient Depression, or $82, 800 for Inpatient Rehab! Respite care reduces public costs associated with frequent hospital utilization. Average Hospital Charge for Depression* Average Hospital Charge for Rehab* Average Respite Program Average Length of Stay 13 days 8. 1 days 21 days Average Charge / Cost Per Patient $16, 133 $29, 160 $3, 137 Average Charge / Cost per Day $1, 241 $3, 600 $145. 85 27 *WSHA Hospital Pricing - does not include professional fees in charges
Outcomes Hospital Staff report a Savings of 23 Inpatient Days by referring to YNHS Medical Respite Care $28, 543 Saved for Inpatient Depression, or $82, 800 for Inpatient Rehab! Respite care reduces public costs associated with frequent hospital utilization. Average Hospital Charge for Depression* Average Hospital Charge for Rehab* Average Respite Program Average Length of Stay 13 days 8. 1 days 21 days Average Charge / Cost Per Patient $16, 133 $29, 160 $3, 137 Average Charge / Cost per Day $1, 241 $3, 600 $145. 85 27 *WSHA Hospital Pricing - does not include professional fees in charges
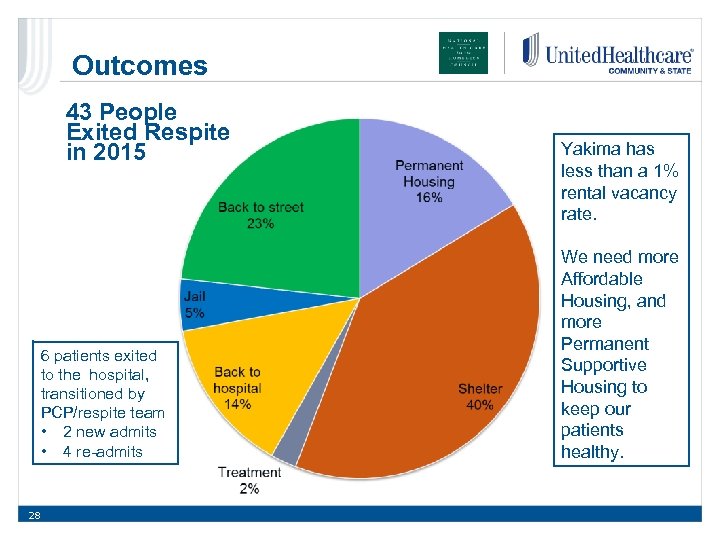 Outcomes 43 People Exited Respite in 2015 6 patients exited to the hospital, transitioned by PCP/respite team • 2 new admits • 4 re-admits 28 Yakima has less than a 1% rental vacancy rate. We need more Affordable Housing, and more Permanent Supportive Housing to keep our patients healthy.
Outcomes 43 People Exited Respite in 2015 6 patients exited to the hospital, transitioned by PCP/respite team • 2 new admits • 4 re-admits 28 Yakima has less than a 1% rental vacancy rate. We need more Affordable Housing, and more Permanent Supportive Housing to keep our patients healthy.
 “I am not a Homeless Guy Any More…” 29
“I am not a Homeless Guy Any More…” 29
 Health Home Services YNHS works with 3 MCOs providing Health Home Services • Targets high cost Medicaid and Dual Eligible clients. • Provides intense care coordination and support for high needs patients. • Sounds like our homeless population! • HCH staff certified as Health Home Care Coordinators • Last year YNHS staff provided Health Home Care Coordination to 230 unduplicated patients through our CHC – 55 (23%) were homeless. 30
Health Home Services YNHS works with 3 MCOs providing Health Home Services • Targets high cost Medicaid and Dual Eligible clients. • Provides intense care coordination and support for high needs patients. • Sounds like our homeless population! • HCH staff certified as Health Home Care Coordinators • Last year YNHS staff provided Health Home Care Coordination to 230 unduplicated patients through our CHC – 55 (23%) were homeless. 30
 Discussion/Q&A Speakers: • Catherine Anderson, Vice President, Positioning and Strategy, United. Healthcare Community & State • Barbara Di. Pietro, Senior Director of Policy, National HCH Council • Doug Bowes, CEO, United. Healthcare Community Plan of Washington • Edward Dwyer-O'Connor, BS, RN, Senior Manager, Downtown Programs, Harborview Medical Center, Seattle, WA • Matt Lund, Director of Contracting, UW Medicine at Harborview Medical Center, Seattle, WA • Rhonda Hauff, COO/Deputy CEO, Yakima Neighborhood Health, Yakima, WA 31
Discussion/Q&A Speakers: • Catherine Anderson, Vice President, Positioning and Strategy, United. Healthcare Community & State • Barbara Di. Pietro, Senior Director of Policy, National HCH Council • Doug Bowes, CEO, United. Healthcare Community Plan of Washington • Edward Dwyer-O'Connor, BS, RN, Senior Manager, Downtown Programs, Harborview Medical Center, Seattle, WA • Matt Lund, Director of Contracting, UW Medicine at Harborview Medical Center, Seattle, WA • Rhonda Hauff, COO/Deputy CEO, Yakima Neighborhood Health, Yakima, WA 31
 Additional Resources Policy Brief: Managed Care & Homeless Populations: Linking the HCH Community and MCO Partners Medical Respite Tool Kit: Available at: https: //www. nhchc. org/wpcontent/uploads/2016/03/mco-hch-policybrief. pdf https: //www. nhchc. org/resources/clinical/ medical-respite/tool-kit/ • • Intro & overview Development & finance Collaborating with hospitals Operations & clinical care 32 Proprietary Information of United. Health Group. Do not distribute or reproduce without express permission of United. Health Group.
Additional Resources Policy Brief: Managed Care & Homeless Populations: Linking the HCH Community and MCO Partners Medical Respite Tool Kit: Available at: https: //www. nhchc. org/wpcontent/uploads/2016/03/mco-hch-policybrief. pdf https: //www. nhchc. org/resources/clinical/ medical-respite/tool-kit/ • • Intro & overview Development & finance Collaborating with hospitals Operations & clinical care 32 Proprietary Information of United. Health Group. Do not distribute or reproduce without express permission of United. Health Group.
 Thank you for attending this webinar on Managed Care and Homeless Populations: Linking the HCH Community and MCO Partners! This project is/was supported by the Health Resources and Services Administration (HRSA) of the U. S. Department of Health and Human Services (HHS) under grant number U 30 CS 09746, a National Training and Technical Assistance Cooperative Agreement for $1, 625, 741, with 0% match from nongovernmental sources. This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U. S. Government. 33 Proprietary Information of United. Health Group. Do not distribute or reproduce without express permission of United. Health Group.
Thank you for attending this webinar on Managed Care and Homeless Populations: Linking the HCH Community and MCO Partners! This project is/was supported by the Health Resources and Services Administration (HRSA) of the U. S. Department of Health and Human Services (HHS) under grant number U 30 CS 09746, a National Training and Technical Assistance Cooperative Agreement for $1, 625, 741, with 0% match from nongovernmental sources. This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U. S. Government. 33 Proprietary Information of United. Health Group. Do not distribute or reproduce without express permission of United. Health Group.


