859347f61261b7381f0ed030c04d14a6.ppt
- Количество слайдов: 61
 Malnutrition among children in Gujarat Health & family Welfare Department GOG
Malnutrition among children in Gujarat Health & family Welfare Department GOG
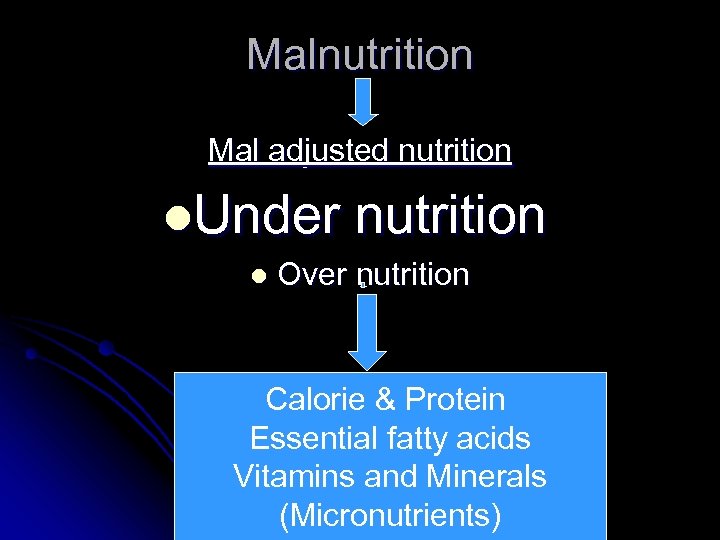 Malnutrition Mal adjusted nutrition l. Under l nutrition Over nutrition Calorie & Protein Essential fatty acids Vitamins and Minerals (Micronutrients)
Malnutrition Mal adjusted nutrition l. Under l nutrition Over nutrition Calorie & Protein Essential fatty acids Vitamins and Minerals (Micronutrients)
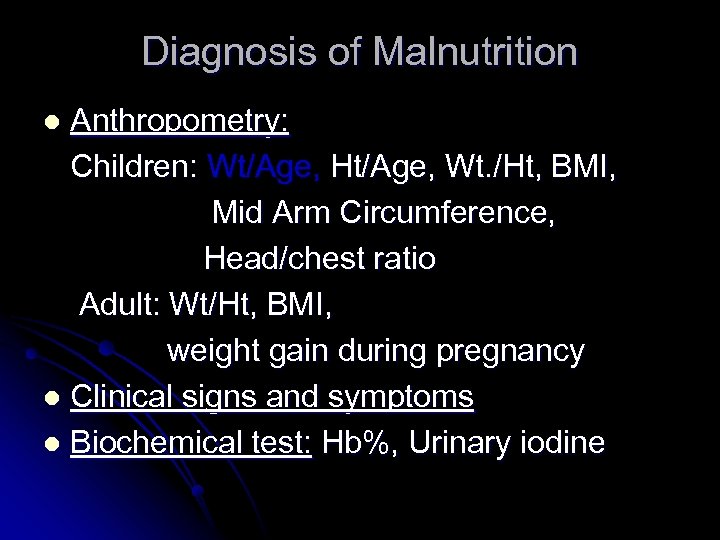 Diagnosis of Malnutrition Anthropometry: Children: Wt/Age, Ht/Age, Wt. /Ht, BMI, Mid Arm Circumference, Head/chest ratio Adult: Wt/Ht, BMI, weight gain during pregnancy l Clinical signs and symptoms l Biochemical test: Hb%, Urinary iodine l
Diagnosis of Malnutrition Anthropometry: Children: Wt/Age, Ht/Age, Wt. /Ht, BMI, Mid Arm Circumference, Head/chest ratio Adult: Wt/Ht, BMI, weight gain during pregnancy l Clinical signs and symptoms l Biochemical test: Hb%, Urinary iodine l
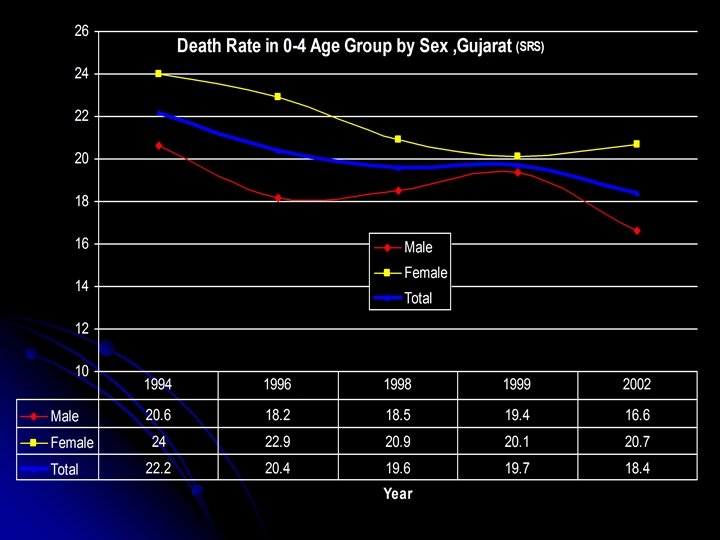
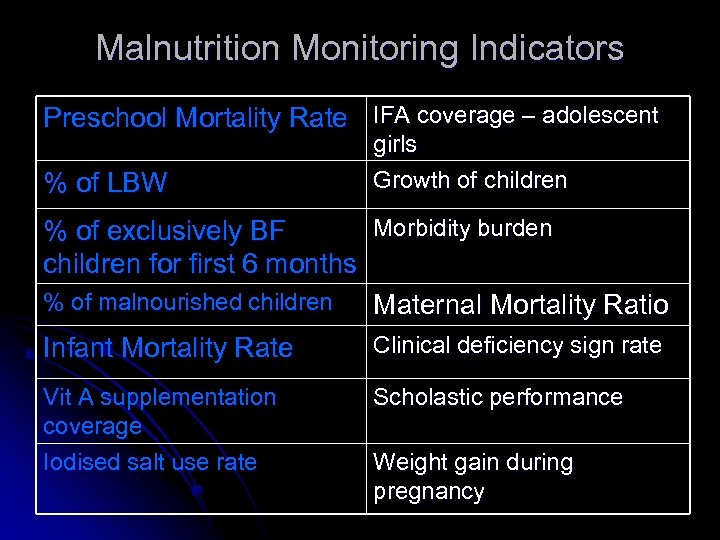 Malnutrition Monitoring Indicators Preschool Mortality Rate IFA coverage – adolescent % of LBW girls Growth of children Morbidity burden % of exclusively BF children for first 6 months % of malnourished children Maternal Mortality Ratio Clinical deficiency sign rate Infant Mortality Rate Vit A supplementation coverage Iodised salt use rate Scholastic performance Weight gain during pregnancy
Malnutrition Monitoring Indicators Preschool Mortality Rate IFA coverage – adolescent % of LBW girls Growth of children Morbidity burden % of exclusively BF children for first 6 months % of malnourished children Maternal Mortality Ratio Clinical deficiency sign rate Infant Mortality Rate Vit A supplementation coverage Iodised salt use rate Scholastic performance Weight gain during pregnancy
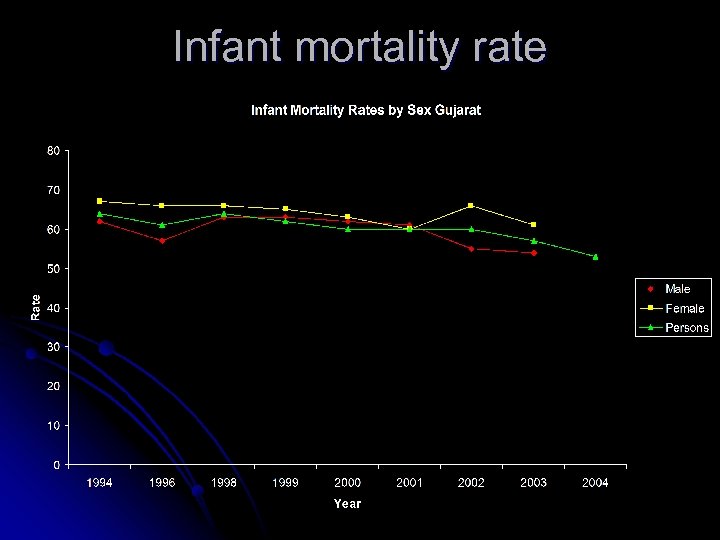 Infant mortality rate
Infant mortality rate
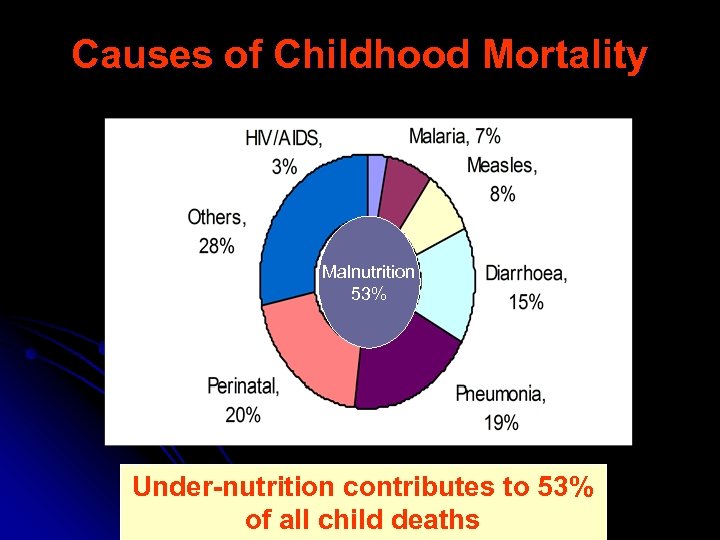 Causes of Childhood Mortality Malnutrition 53% Under-nutrition contributes to 53% of all child deaths
Causes of Childhood Mortality Malnutrition 53% Under-nutrition contributes to 53% of all child deaths
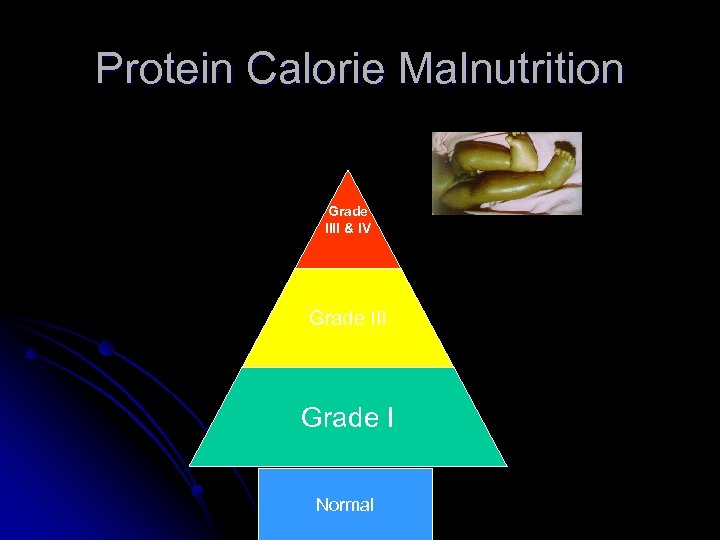 Protein Calorie Malnutrition Grade IIII & IV Grade III Grade I Normal
Protein Calorie Malnutrition Grade IIII & IV Grade III Grade I Normal
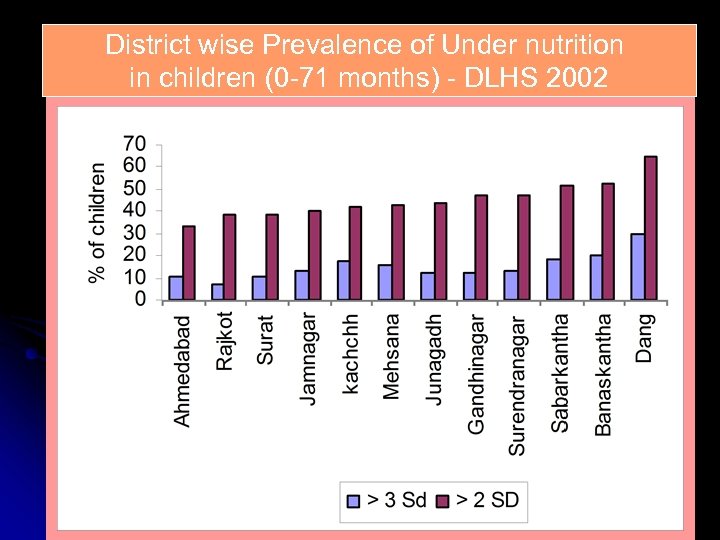 District wise Prevalence of Under nutrition in children (0 -71 months) - DLHS 2002
District wise Prevalence of Under nutrition in children (0 -71 months) - DLHS 2002
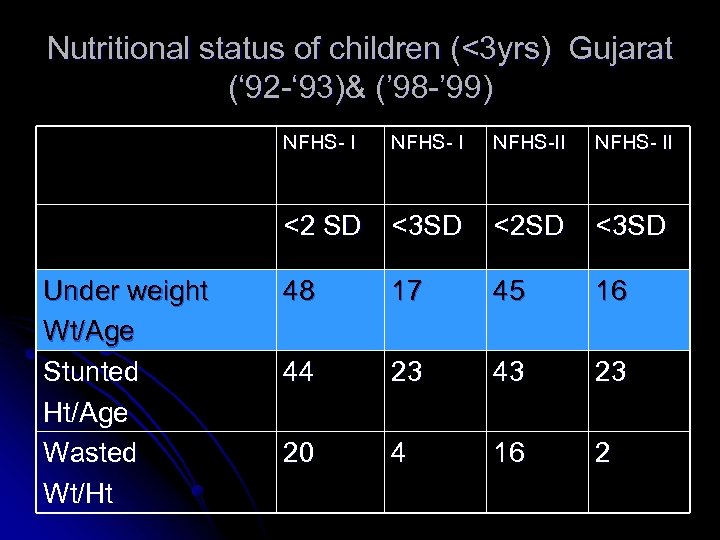 Nutritional status of children (<3 yrs) Gujarat (‘ 92 -‘ 93)& (’ 98 -’ 99) NFHS- I NFHS-II NFHS- II <2 SD Under weight Wt/Age Stunted Ht/Age Wasted Wt/Ht NFHS- I <3 SD <2 SD <3 SD 48 17 45 16 44 23 43 23 20 4 16 2
Nutritional status of children (<3 yrs) Gujarat (‘ 92 -‘ 93)& (’ 98 -’ 99) NFHS- I NFHS-II NFHS- II <2 SD Under weight Wt/Age Stunted Ht/Age Wasted Wt/Ht NFHS- I <3 SD <2 SD <3 SD 48 17 45 16 44 23 43 23 20 4 16 2
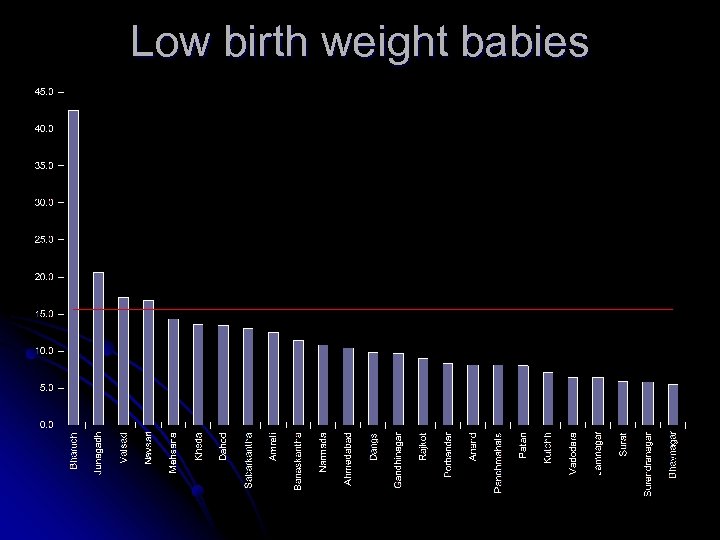 Low birth weight babies
Low birth weight babies
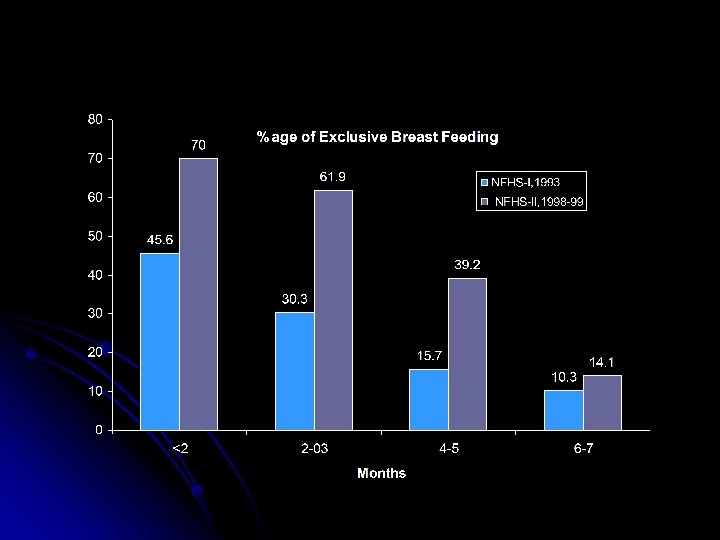
 % of women who gave exclusive Breast milk up to 4 months (DLHS, 2002 & 2004)
% of women who gave exclusive Breast milk up to 4 months (DLHS, 2002 & 2004)
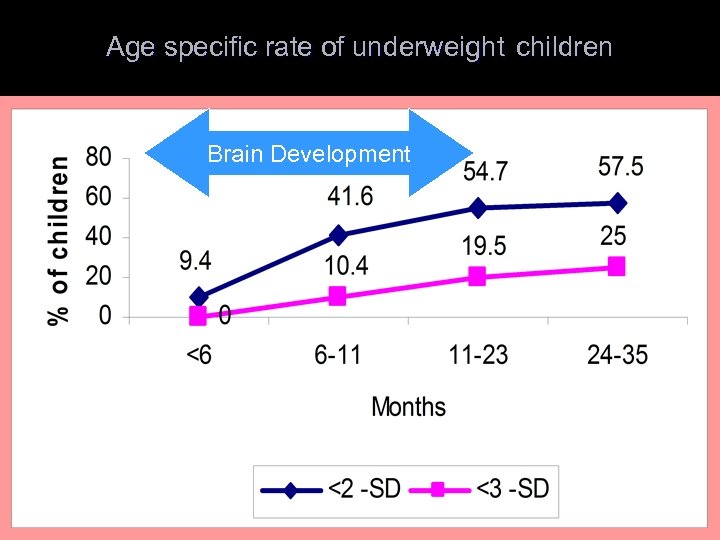 Age specific rate of underweight children Brain Development
Age specific rate of underweight children Brain Development
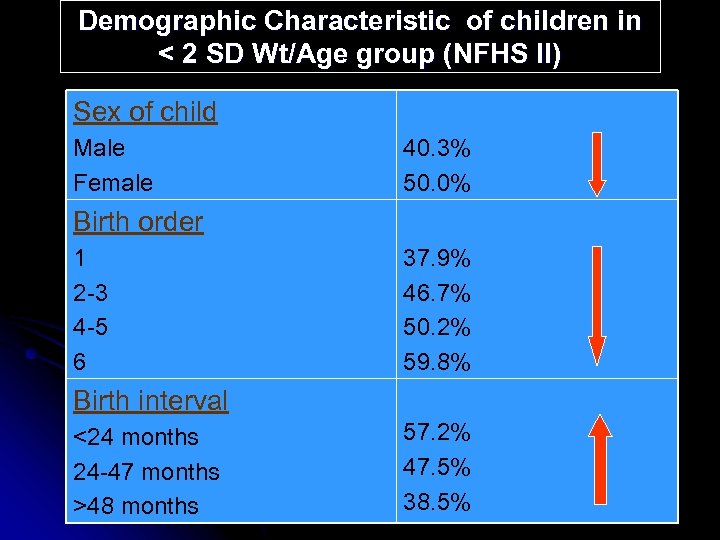 Demographic Characteristic of children in < 2 SD Wt/Age group (NFHS II) Sex of child Male Female 40. 3% 50. 0% Birth order 1 2 -3 4 -5 6 37. 9% 46. 7% 50. 2% 59. 8% Birth interval <24 months 24 -47 months >48 months 57. 2% 47. 5% 38. 5%
Demographic Characteristic of children in < 2 SD Wt/Age group (NFHS II) Sex of child Male Female 40. 3% 50. 0% Birth order 1 2 -3 4 -5 6 37. 9% 46. 7% 50. 2% 59. 8% Birth interval <24 months 24 -47 months >48 months 57. 2% 47. 5% 38. 5%
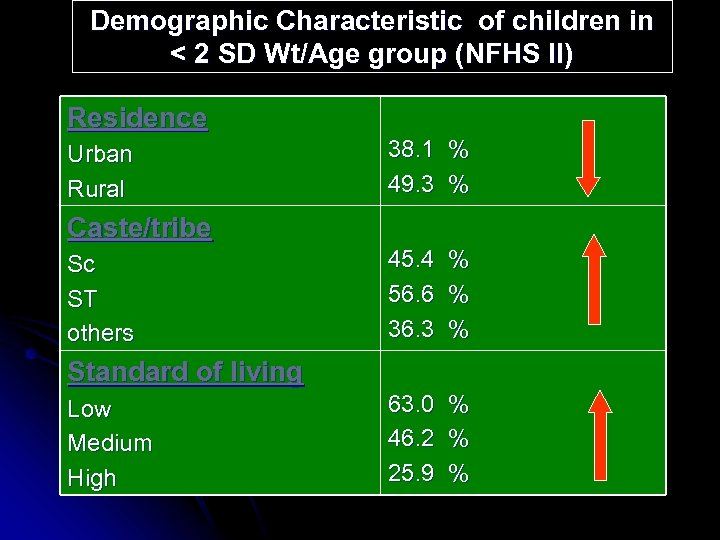 Demographic Characteristic of children in < 2 SD Wt/Age group (NFHS II) Residence Urban Rural 38. 1 % 49. 3 % Caste/tribe Sc ST others 45. 4 56. 6 36. 3 % % % 63. 0 46. 2 25. 9 % % % Standard of living Low Medium High
Demographic Characteristic of children in < 2 SD Wt/Age group (NFHS II) Residence Urban Rural 38. 1 % 49. 3 % Caste/tribe Sc ST others 45. 4 56. 6 36. 3 % % % 63. 0 46. 2 25. 9 % % % Standard of living Low Medium High
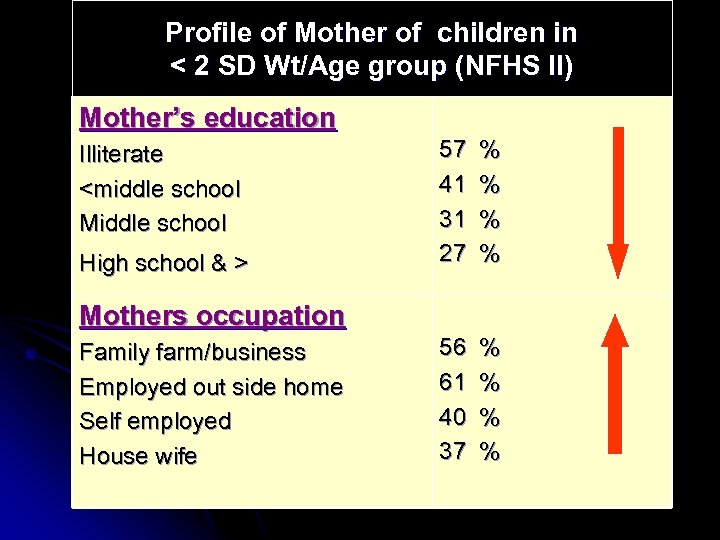 Profile of Mother of children in < 2 SD Wt/Age group (NFHS II) Mother’s education Illiterate
Profile of Mother of children in < 2 SD Wt/Age group (NFHS II) Mother’s education Illiterate
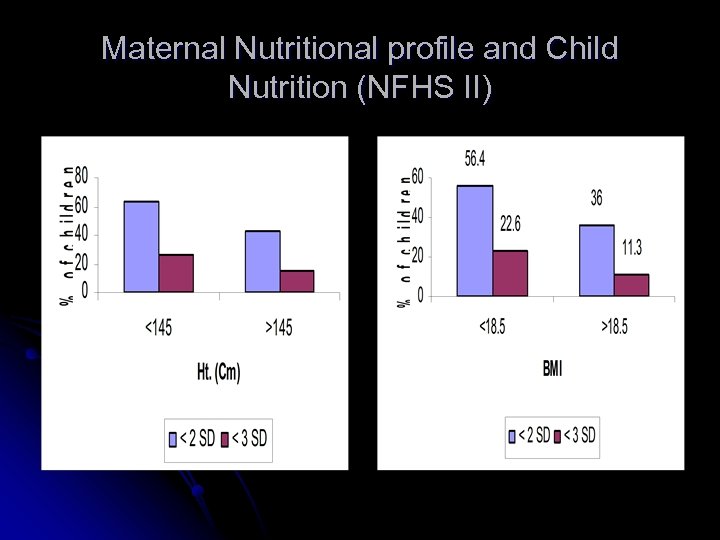 Maternal Nutritional profile and Child Nutrition (NFHS II)
Maternal Nutritional profile and Child Nutrition (NFHS II)
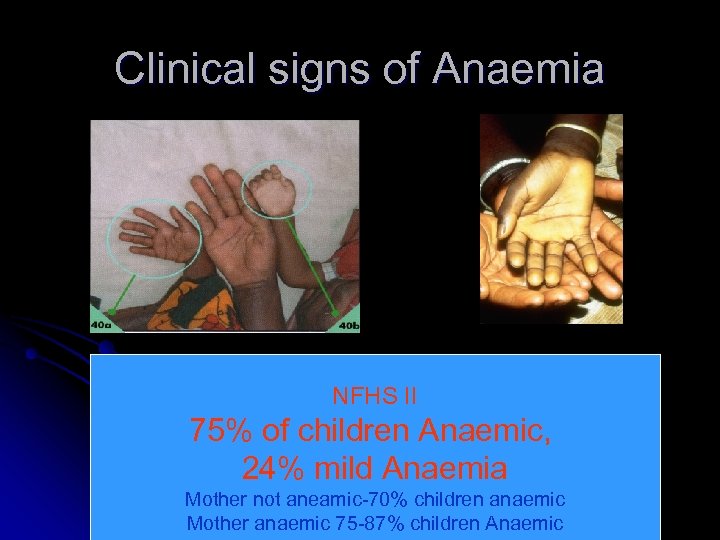 Clinical signs of Anaemia NFHS II 75% of children Anaemic, 24% mild Anaemia Mother not aneamic-70% children anaemic Mother anaemic 75 -87% children Anaemic
Clinical signs of Anaemia NFHS II 75% of children Anaemic, 24% mild Anaemia Mother not aneamic-70% children anaemic Mother anaemic 75 -87% children Anaemic
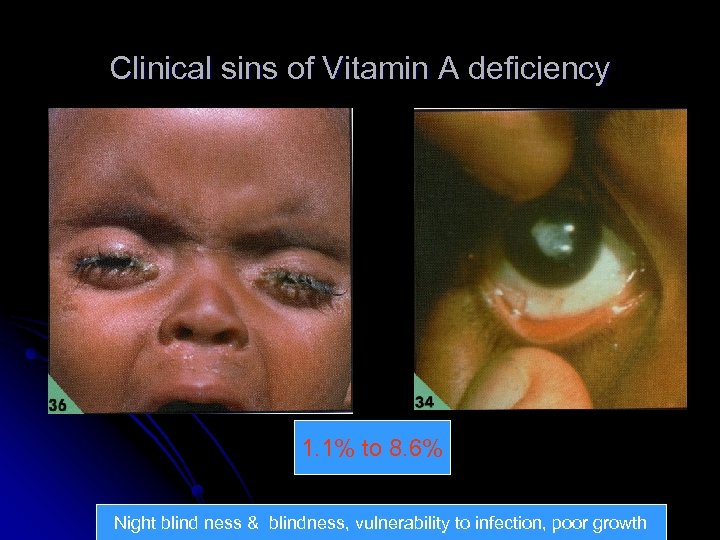 Clinical sins of Vitamin A deficiency 1. 1% to 8. 6% Night blind ness & blindness, vulnerability to infection, poor growth
Clinical sins of Vitamin A deficiency 1. 1% to 8. 6% Night blind ness & blindness, vulnerability to infection, poor growth
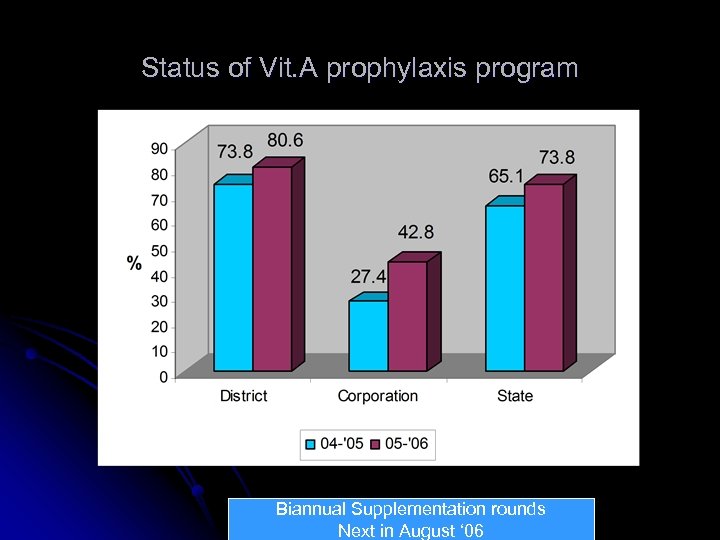 Status of Vit. A prophylaxis program Biannual Supplementation rounds Next in August ‘ 06
Status of Vit. A prophylaxis program Biannual Supplementation rounds Next in August ‘ 06
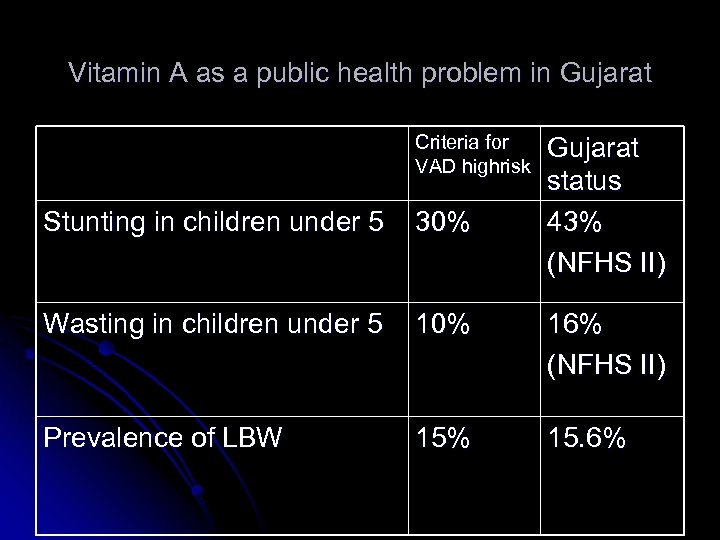 Vitamin A as a public health problem in Gujarat Criteria for VAD highrisk Gujarat status 43% (NFHS II) Stunting in children under 5 30% Wasting in children under 5 10% 16% (NFHS II) Prevalence of LBW 15% 15. 6%
Vitamin A as a public health problem in Gujarat Criteria for VAD highrisk Gujarat status 43% (NFHS II) Stunting in children under 5 30% Wasting in children under 5 10% 16% (NFHS II) Prevalence of LBW 15% 15. 6%
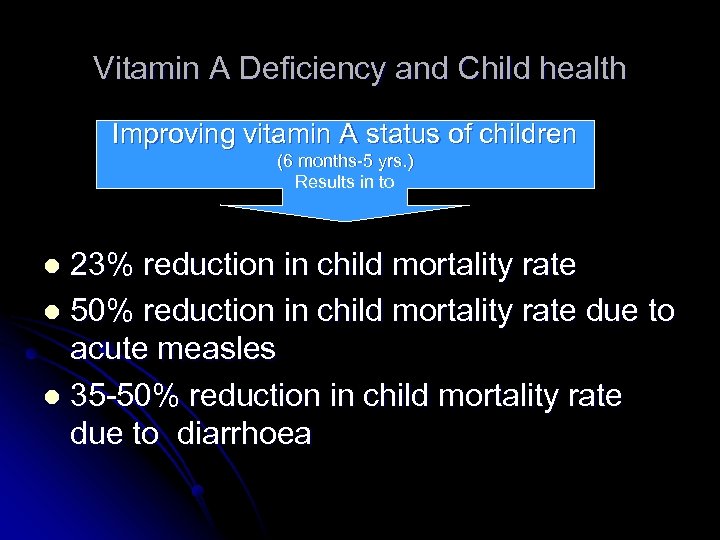 Vitamin A Deficiency and Child health Improving vitamin A status of children (6 months-5 yrs. ) Results in to 23% reduction in child mortality rate l 50% reduction in child mortality rate due to acute measles l 35 -50% reduction in child mortality rate due to diarrhoea l
Vitamin A Deficiency and Child health Improving vitamin A status of children (6 months-5 yrs. ) Results in to 23% reduction in child mortality rate l 50% reduction in child mortality rate due to acute measles l 35 -50% reduction in child mortality rate due to diarrhoea l
 Clinical signs of Iodine deficiency disorders
Clinical signs of Iodine deficiency disorders
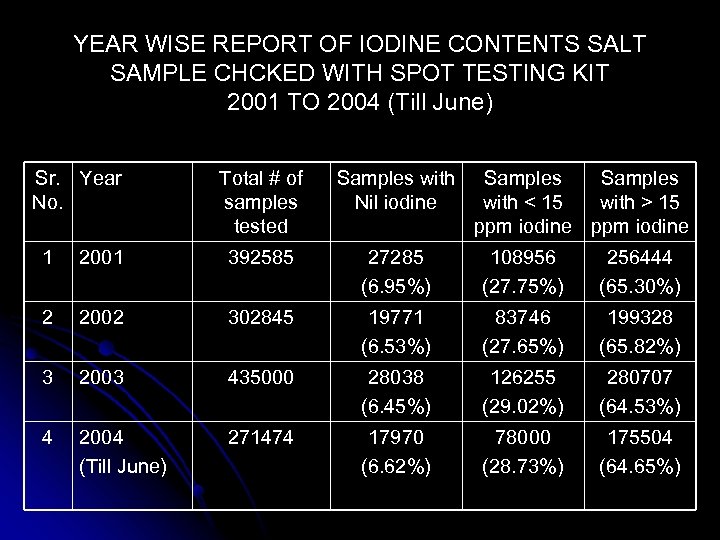 YEAR WISE REPORT OF IODINE CONTENTS SALT SAMPLE CHCKED WITH SPOT TESTING KIT 2001 TO 2004 (Till June) Sr. Year No. Total # of samples tested Samples with Nil iodine Samples with < 15 with > 15 ppm iodine 1 2001 392585 27285 (6. 95%) 108956 (27. 75%) 256444 (65. 30%) 2 2002 302845 19771 (6. 53%) 83746 (27. 65%) 199328 (65. 82%) 3 2003 435000 28038 (6. 45%) 126255 (29. 02%) 280707 (64. 53%) 4 2004 (Till June) 271474 17970 (6. 62%) 78000 (28. 73%) 175504 (64. 65%)
YEAR WISE REPORT OF IODINE CONTENTS SALT SAMPLE CHCKED WITH SPOT TESTING KIT 2001 TO 2004 (Till June) Sr. Year No. Total # of samples tested Samples with Nil iodine Samples with < 15 with > 15 ppm iodine 1 2001 392585 27285 (6. 95%) 108956 (27. 75%) 256444 (65. 30%) 2 2002 302845 19771 (6. 53%) 83746 (27. 65%) 199328 (65. 82%) 3 2003 435000 28038 (6. 45%) 126255 (29. 02%) 280707 (64. 53%) 4 2004 (Till June) 271474 17970 (6. 62%) 78000 (28. 73%) 175504 (64. 65%)
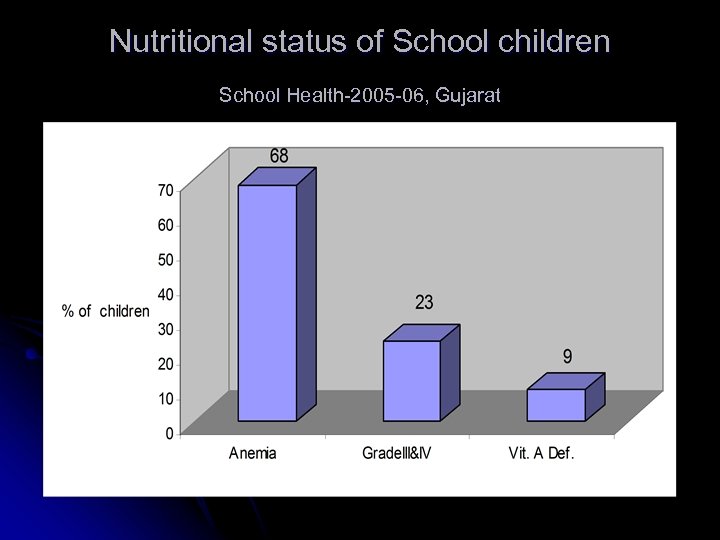 Nutritional status of School children School Health-2005 -06, Gujarat
Nutritional status of School children School Health-2005 -06, Gujarat
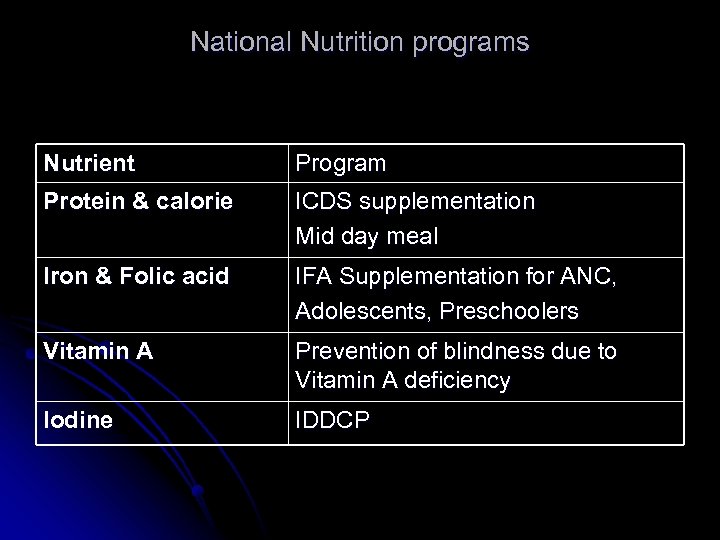 National Nutrition programs Nutrient Program Protein & calorie ICDS supplementation Mid day meal Iron & Folic acid IFA Supplementation for ANC, Adolescents, Preschoolers Vitamin A Prevention of blindness due to Vitamin A deficiency Iodine IDDCP
National Nutrition programs Nutrient Program Protein & calorie ICDS supplementation Mid day meal Iron & Folic acid IFA Supplementation for ANC, Adolescents, Preschoolers Vitamin A Prevention of blindness due to Vitamin A deficiency Iodine IDDCP
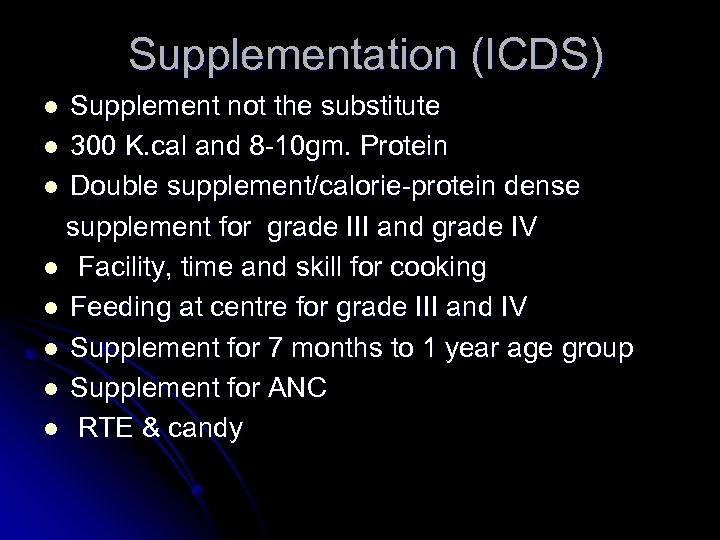 Supplementation (ICDS) Supplement not the substitute l 300 K. cal and 8 -10 gm. Protein l Double supplement/calorie-protein dense supplement for grade III and grade IV l Facility, time and skill for cooking l Feeding at centre for grade III and IV l Supplement for 7 months to 1 year age group l Supplement for ANC l RTE & candy l
Supplementation (ICDS) Supplement not the substitute l 300 K. cal and 8 -10 gm. Protein l Double supplement/calorie-protein dense supplement for grade III and grade IV l Facility, time and skill for cooking l Feeding at centre for grade III and IV l Supplement for 7 months to 1 year age group l Supplement for ANC l RTE & candy l
 Special care of Grade III & IV Problems: Loss of appetite, high calorie protein need, Infection proneness, restriction of food, digestion Solution: Frequent feeding Calorie protein dense supplement Easily digestible food Animal/ First class protein Vitamin and Mineral supplement Treatment of infection Mother’s involvement in care of the child
Special care of Grade III & IV Problems: Loss of appetite, high calorie protein need, Infection proneness, restriction of food, digestion Solution: Frequent feeding Calorie protein dense supplement Easily digestible food Animal/ First class protein Vitamin and Mineral supplement Treatment of infection Mother’s involvement in care of the child
 MDM supplement 300 k. cal. And 8 -10 gm. Protein l Supplement not substitute l Children attending school / Child’s attention in school l In built Diet education l In built equity education l
MDM supplement 300 k. cal. And 8 -10 gm. Protein l Supplement not substitute l Children attending school / Child’s attention in school l In built Diet education l In built equity education l
 GUJARAT INITIATIVES
GUJARAT INITIATIVES
 Adolescent Girls Anaemia Control Programme 2001 pilot project in Vadodara district (UNICEF) l Anaemia reduction from 74% to 53% in 17 months l Project is operationalised in all districts (UNICEF & MI) l Convergence between Health and Education department l
Adolescent Girls Anaemia Control Programme 2001 pilot project in Vadodara district (UNICEF) l Anaemia reduction from 74% to 53% in 17 months l Project is operationalised in all districts (UNICEF & MI) l Convergence between Health and Education department l
 RTE Ready to Eat fortified with micronutrients l Operationalised in four districts (Mehsana, Patan, Panchmahal, Dahod) in 2001 l MI project l High level of micronutrient deficiency recorded in baseline study l Acceptability was high l Bulk was a limiting factor l Convergence between Health and ICDS(DWCD) l
RTE Ready to Eat fortified with micronutrients l Operationalised in four districts (Mehsana, Patan, Panchmahal, Dahod) in 2001 l MI project l High level of micronutrient deficiency recorded in baseline study l Acceptability was high l Bulk was a limiting factor l Convergence between Health and ICDS(DWCD) l
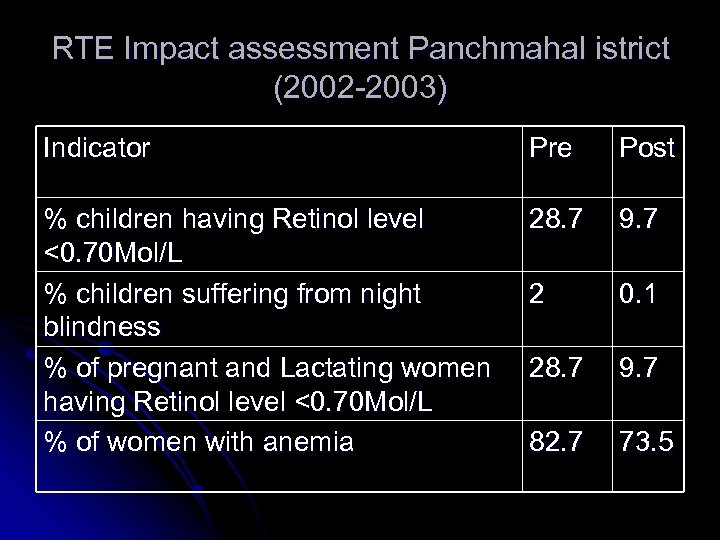 RTE Impact assessment Panchmahal istrict (2002 -2003) Indicator Pre Post % children having Retinol level <0. 70 Mol/L % children suffering from night blindness % of pregnant and Lactating women having Retinol level <0. 70 Mol/L % of women with anemia 28. 7 9. 7 2 0. 1 28. 7 9. 7 82. 7 73. 5
RTE Impact assessment Panchmahal istrict (2002 -2003) Indicator Pre Post % children having Retinol level <0. 70 Mol/L % children suffering from night blindness % of pregnant and Lactating women having Retinol level <0. 70 Mol/L % of women with anemia 28. 7 9. 7 2 0. 1 28. 7 9. 7 82. 7 73. 5
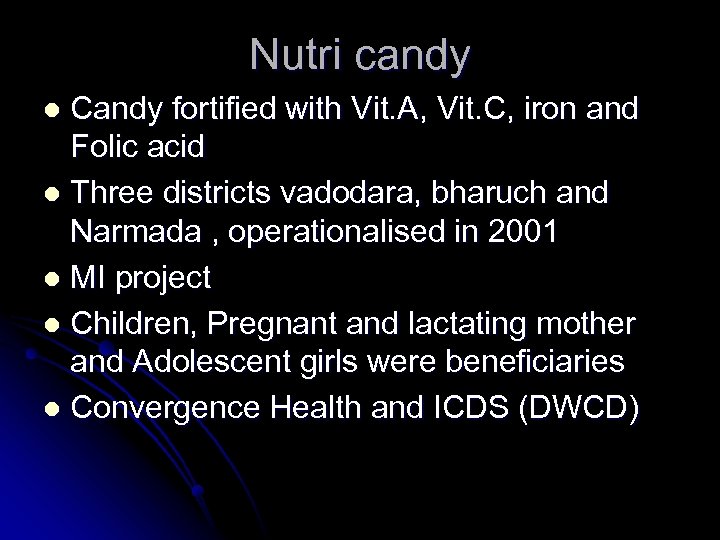 Nutri candy Candy fortified with Vit. A, Vit. C, iron and Folic acid l Three districts vadodara, bharuch and Narmada , operationalised in 2001 l MI project l Children, Pregnant and lactating mother and Adolescent girls were beneficiaries l Convergence Health and ICDS (DWCD) l
Nutri candy Candy fortified with Vit. A, Vit. C, iron and Folic acid l Three districts vadodara, bharuch and Narmada , operationalised in 2001 l MI project l Children, Pregnant and lactating mother and Adolescent girls were beneficiaries l Convergence Health and ICDS (DWCD) l
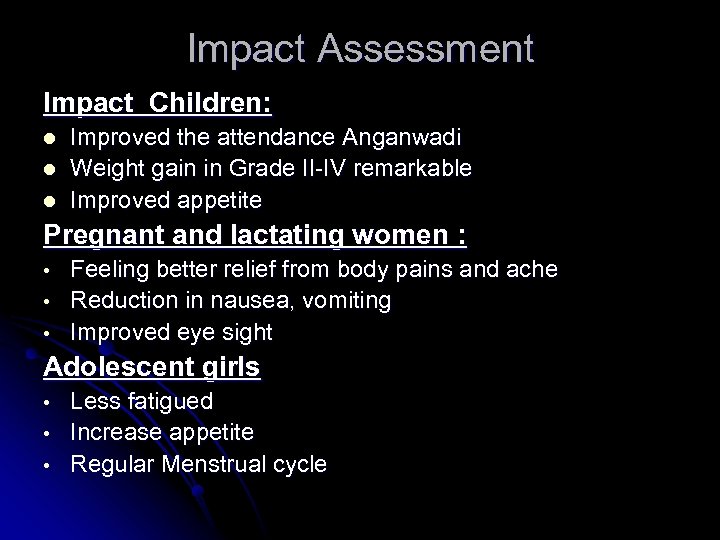 Impact Assessment Impact Children: l l l Improved the attendance Anganwadi Weight gain in Grade II-IV remarkable Improved appetite Pregnant and lactating women : • • • Feeling better relief from body pains and ache Reduction in nausea, vomiting Improved eye sight Adolescent girls • • • Less fatigued Increase appetite Regular Menstrual cycle
Impact Assessment Impact Children: l l l Improved the attendance Anganwadi Weight gain in Grade II-IV remarkable Improved appetite Pregnant and lactating women : • • • Feeling better relief from body pains and ache Reduction in nausea, vomiting Improved eye sight Adolescent girls • • • Less fatigued Increase appetite Regular Menstrual cycle
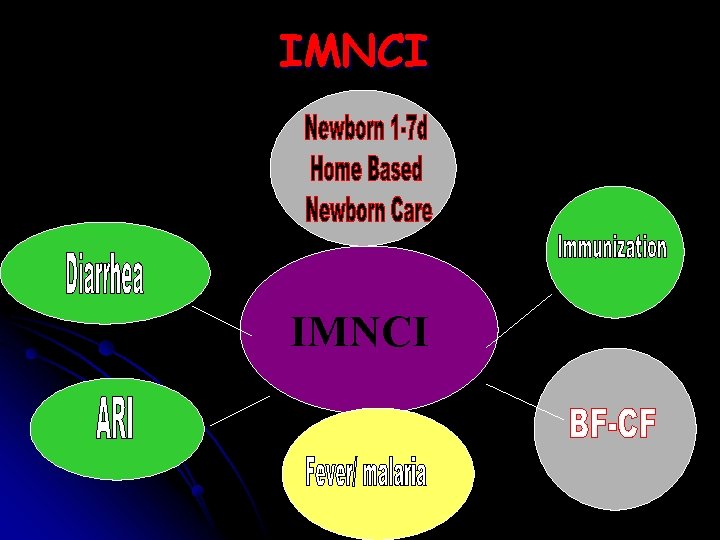 IMNCI
IMNCI
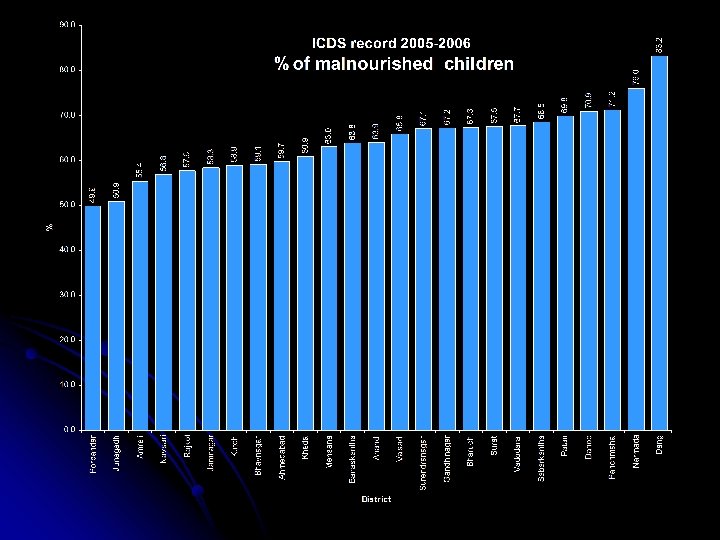
 Mapping & Monitoring Malnutrition ICDS special round of weighing the children with inbuilt quality check process May-June 2006 l Routine monthly assessment l Health facility assessment and support as well as regular monitoring record in health worker’s register l Inbuilt assessment through monthly reporting system l
Mapping & Monitoring Malnutrition ICDS special round of weighing the children with inbuilt quality check process May-June 2006 l Routine monthly assessment l Health facility assessment and support as well as regular monitoring record in health worker’s register l Inbuilt assessment through monthly reporting system l
 Field level Functional Convergence Fix day ‘ Health and Nutrition Day’ Session at SC Planning and Implementation in progress v Improve quality and coverage of RCH services v Mainstreaming of Nutrition care and support v Improve quality and coverage of monitoring data v Improve Accessibility of Health and Nutrition services v Improve Maternal and Child health status v
Field level Functional Convergence Fix day ‘ Health and Nutrition Day’ Session at SC Planning and Implementation in progress v Improve quality and coverage of RCH services v Mainstreaming of Nutrition care and support v Improve quality and coverage of monitoring data v Improve Accessibility of Health and Nutrition services v Improve Maternal and Child health status v
 Minimum need Supply Monitor ing Integrat ion Community Awareness and Involvement Care and Support For Health & Nutrition workers
Minimum need Supply Monitor ing Integrat ion Community Awareness and Involvement Care and Support For Health & Nutrition workers
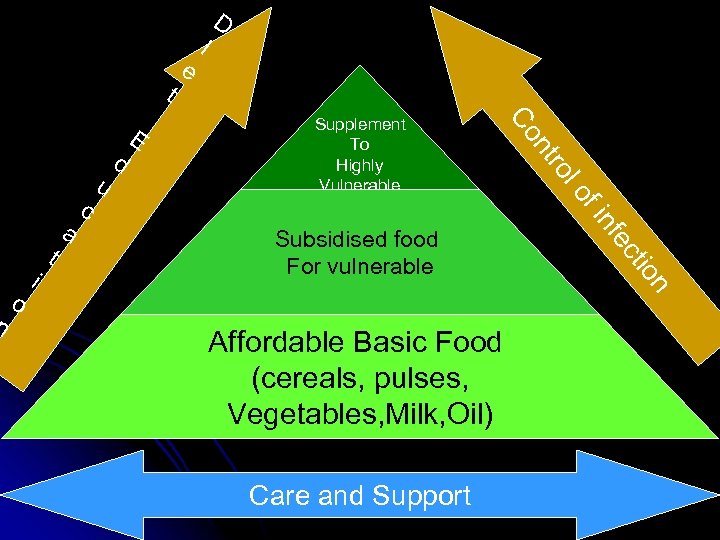 lo f in fe o cti Subsidised food For vulnerable ro Supplement To Highly Vulnerable nt n o i t a c u d E Co n t e I D Affordable Basic Food (cereals, pulses, Vegetables, Milk, Oil) Care and Support
lo f in fe o cti Subsidised food For vulnerable ro Supplement To Highly Vulnerable nt n o i t a c u d E Co n t e I D Affordable Basic Food (cereals, pulses, Vegetables, Milk, Oil) Care and Support
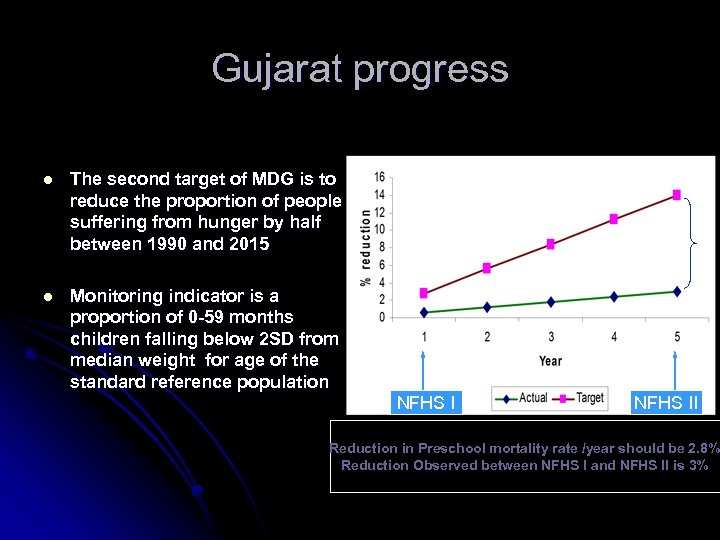 Gujarat progress l The second target of MDG is to reduce the proportion of people suffering from hunger by half between 1990 and 2015 l Monitoring indicator is a proportion of 0 -59 months children falling below 2 SD from median weight for age of the standard reference population NFHS II Reduction in Preschool mortality rate /year should be 2. 8% Reduction Observed between NFHS I and NFHS II is 3%
Gujarat progress l The second target of MDG is to reduce the proportion of people suffering from hunger by half between 1990 and 2015 l Monitoring indicator is a proportion of 0 -59 months children falling below 2 SD from median weight for age of the standard reference population NFHS II Reduction in Preschool mortality rate /year should be 2. 8% Reduction Observed between NFHS I and NFHS II is 3%

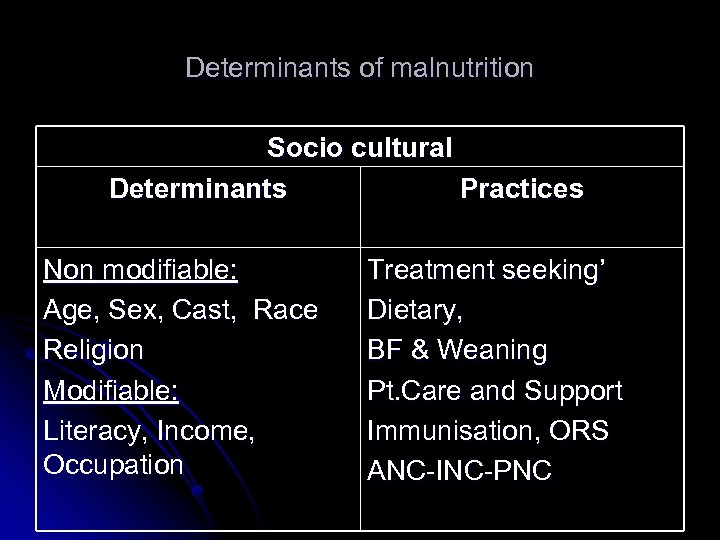 Determinants of malnutrition Socio cultural Determinants Practices Non modifiable: Age, Sex, Cast, Race Religion Modifiable: Literacy, Income, Occupation Treatment seeking’ Dietary, BF & Weaning Pt. Care and Support Immunisation, ORS ANC-INC-PNC
Determinants of malnutrition Socio cultural Determinants Practices Non modifiable: Age, Sex, Cast, Race Religion Modifiable: Literacy, Income, Occupation Treatment seeking’ Dietary, BF & Weaning Pt. Care and Support Immunisation, ORS ANC-INC-PNC
 Nutrition care of Community l Nutrition care of vulnerable l School age group Adolescent l Nutrition care of highly vulnerable Pregnant woman Breast feeding woman Preschool children Infants
Nutrition care of Community l Nutrition care of vulnerable l School age group Adolescent l Nutrition care of highly vulnerable Pregnant woman Breast feeding woman Preschool children Infants
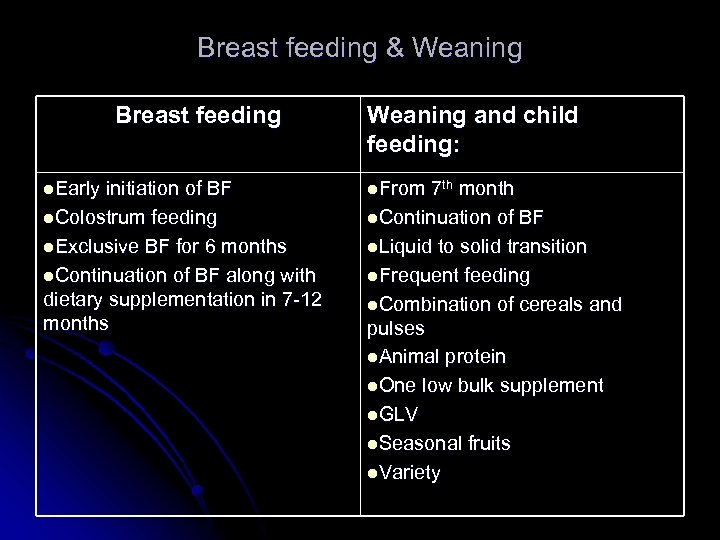 Breast feeding & Weaning Breast feeding l. Early initiation of BF l. Colostrum feeding l. Exclusive BF for 6 months l. Continuation of BF along with dietary supplementation in 7 -12 months Weaning and child feeding: l. From 7 th month l. Continuation of BF l. Liquid to solid transition l. Frequent feeding l. Combination of cereals and pulses l. Animal protein l. One low bulk supplement l. GLV l. Seasonal fruits l. Variety
Breast feeding & Weaning Breast feeding l. Early initiation of BF l. Colostrum feeding l. Exclusive BF for 6 months l. Continuation of BF along with dietary supplementation in 7 -12 months Weaning and child feeding: l. From 7 th month l. Continuation of BF l. Liquid to solid transition l. Frequent feeding l. Combination of cereals and pulses l. Animal protein l. One low bulk supplement l. GLV l. Seasonal fruits l. Variety
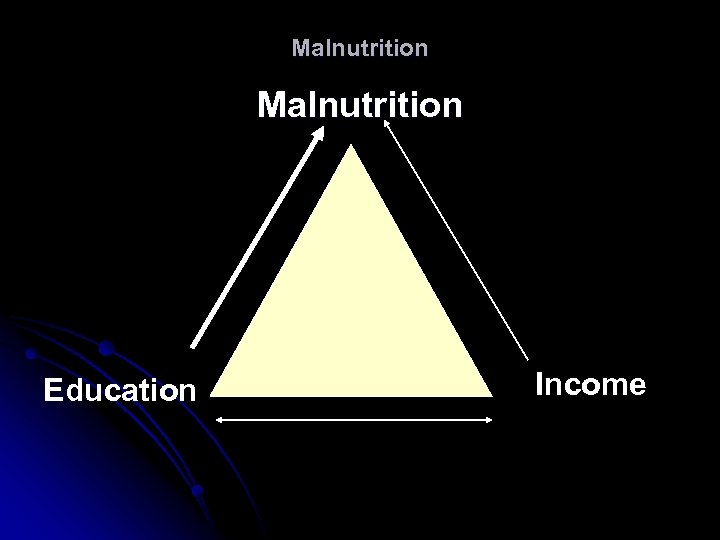 Malnutrition Education Income
Malnutrition Education Income
 Integrated care l l l l Maternal and Child nutrition Adolescent and Maternal Nutrition and Infection control/care- sanitation, hygiene, vaccination, early detection and treatment Nutrition and FP Macro and Micro nutrition Nutrition and --------Mental development Family nutrition and supplementary nutrition Nutrition supplement and Diet/ nutrition education
Integrated care l l l l Maternal and Child nutrition Adolescent and Maternal Nutrition and Infection control/care- sanitation, hygiene, vaccination, early detection and treatment Nutrition and FP Macro and Micro nutrition Nutrition and --------Mental development Family nutrition and supplementary nutrition Nutrition supplement and Diet/ nutrition education
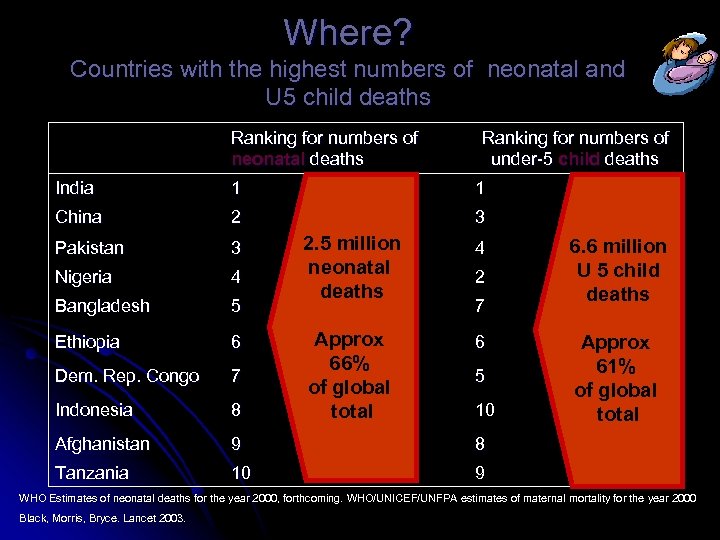 Where? Countries with the highest numbers of neonatal and U 5 child deaths Ranking for numbers of neonatal deaths Ranking for numbers of under-5 child deaths India 1 1 China 2 3 Pakistan 3 Nigeria 4 Bangladesh 5 Ethiopia 6 Dem. Rep. Congo 7 Indonesia 8 Afghanistan 9 8 Tanzania 10 9 2. 5 million neonatal deaths 4 Approx 66% of global total 6 2 7 5 10 6. 6 million U 5 child deaths Approx 61% of global total WHO Estimates of neonatal deaths for the year 2000, forthcoming. WHO/UNICEF/UNFPA estimates of maternal mortality for the year 2000 Black, Morris, Bryce. Lancet 2003.
Where? Countries with the highest numbers of neonatal and U 5 child deaths Ranking for numbers of neonatal deaths Ranking for numbers of under-5 child deaths India 1 1 China 2 3 Pakistan 3 Nigeria 4 Bangladesh 5 Ethiopia 6 Dem. Rep. Congo 7 Indonesia 8 Afghanistan 9 8 Tanzania 10 9 2. 5 million neonatal deaths 4 Approx 66% of global total 6 2 7 5 10 6. 6 million U 5 child deaths Approx 61% of global total WHO Estimates of neonatal deaths for the year 2000, forthcoming. WHO/UNICEF/UNFPA estimates of maternal mortality for the year 2000 Black, Morris, Bryce. Lancet 2003.
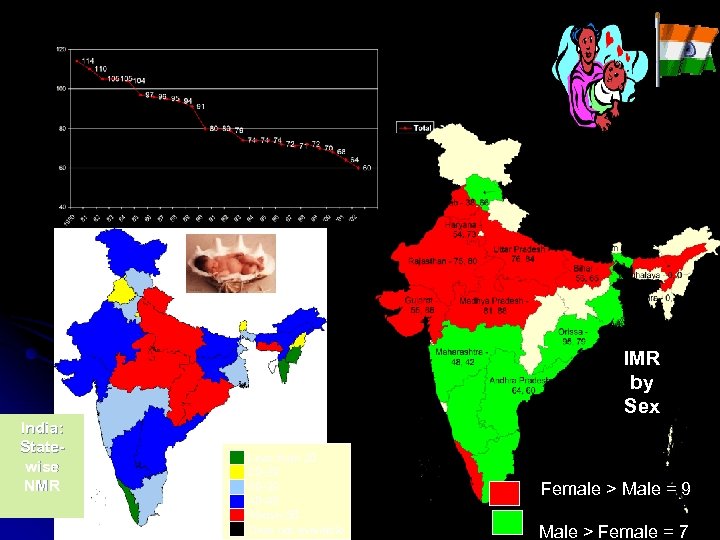 Infant Mortality Rates (India), Decline over the Years IMR by Sex India: Statewise NMR Less than 20 20 -29 30 -39 40 -49 Above 50 Data not available Female > Male = 9 Male > Female = 7
Infant Mortality Rates (India), Decline over the Years IMR by Sex India: Statewise NMR Less than 20 20 -29 30 -39 40 -49 Above 50 Data not available Female > Male = 9 Male > Female = 7
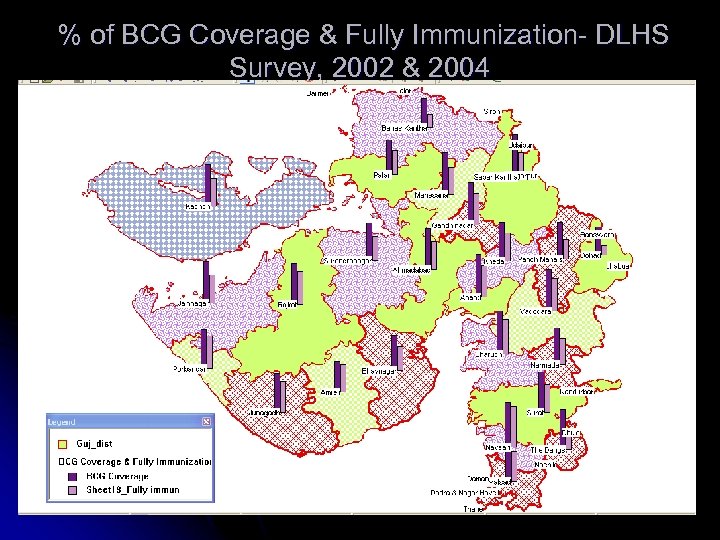 % of BCG Coverage & Fully Immunization- DLHS Survey, 2002 & 2004
% of BCG Coverage & Fully Immunization- DLHS Survey, 2002 & 2004
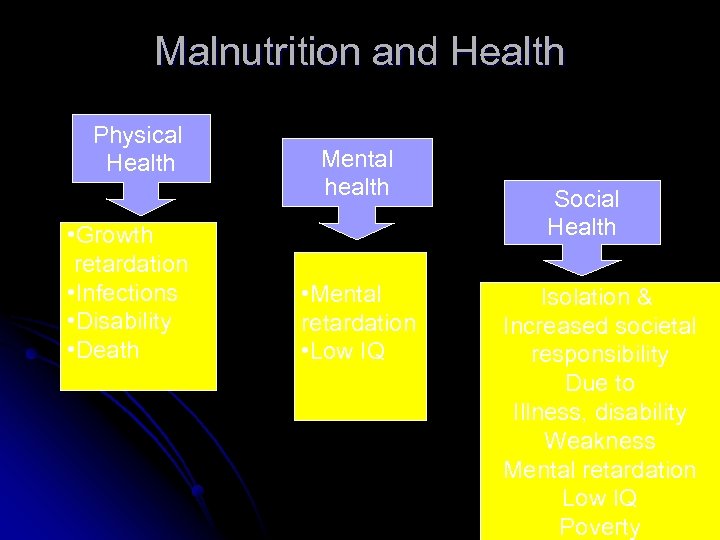 Malnutrition and Health Physical Health • Growth retardation • Infections • Disability • Death Mental health • Mental retardation • Low IQ Social Health Isolation & Increased societal responsibility Due to Illness, disability Weakness Mental retardation Low IQ Poverty
Malnutrition and Health Physical Health • Growth retardation • Infections • Disability • Death Mental health • Mental retardation • Low IQ Social Health Isolation & Increased societal responsibility Due to Illness, disability Weakness Mental retardation Low IQ Poverty
 What are the causes of death? Source: WHR 2005
What are the causes of death? Source: WHR 2005
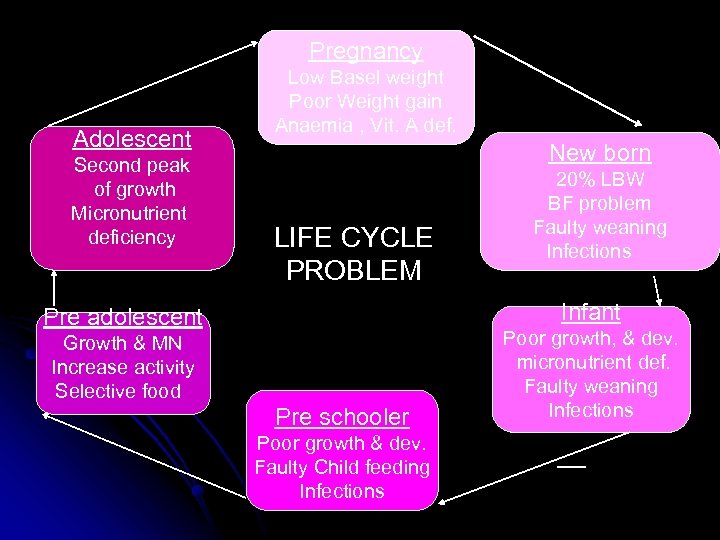 Pregnancy Adolescent Second peak of growth Micronutrient deficiency Low Basel weight Poor Weight gain Anaemia , Vit. A def. New born LIFE CYCLE PROBLEM 20% LBW BF problem Faulty weaning Infections Infant Pre adolescent Growth & MN Increase activity Selective food Pre schooler Poor growth & dev. Faulty Child feeding Infections Poor growth, & dev. micronutrient def. Faulty weaning Infections
Pregnancy Adolescent Second peak of growth Micronutrient deficiency Low Basel weight Poor Weight gain Anaemia , Vit. A def. New born LIFE CYCLE PROBLEM 20% LBW BF problem Faulty weaning Infections Infant Pre adolescent Growth & MN Increase activity Selective food Pre schooler Poor growth & dev. Faulty Child feeding Infections Poor growth, & dev. micronutrient def. Faulty weaning Infections
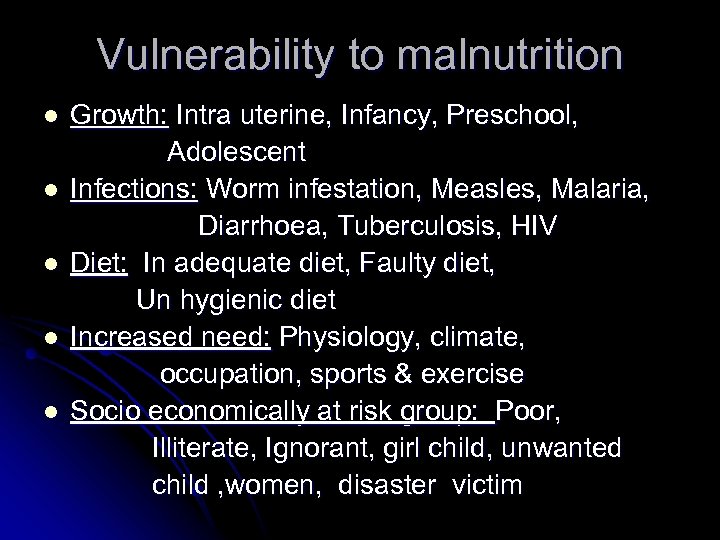 Vulnerability to malnutrition l l l Growth: Intra uterine, Infancy, Preschool, Adolescent Infections: Worm infestation, Measles, Malaria, Diarrhoea, Tuberculosis, HIV Diet: In adequate diet, Faulty diet, Un hygienic diet Increased need: Physiology, climate, occupation, sports & exercise Socio economically at risk group: Poor, Illiterate, Ignorant, girl child, unwanted child , women, disaster victim
Vulnerability to malnutrition l l l Growth: Intra uterine, Infancy, Preschool, Adolescent Infections: Worm infestation, Measles, Malaria, Diarrhoea, Tuberculosis, HIV Diet: In adequate diet, Faulty diet, Un hygienic diet Increased need: Physiology, climate, occupation, sports & exercise Socio economically at risk group: Poor, Illiterate, Ignorant, girl child, unwanted child , women, disaster victim
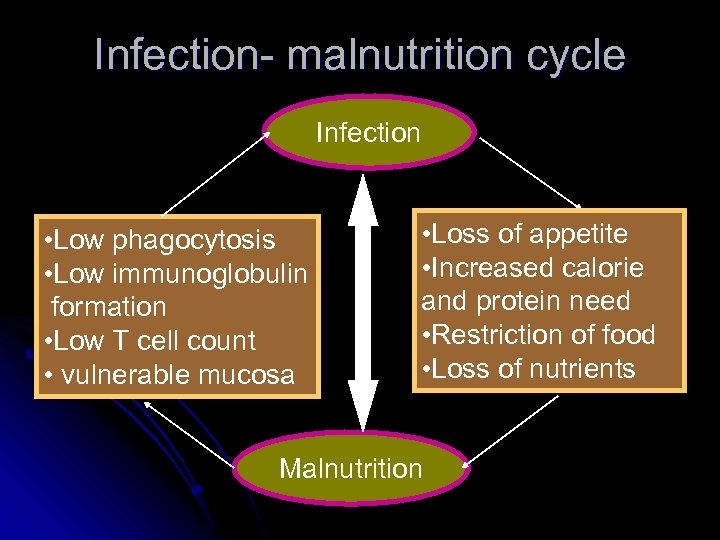 Infection- malnutrition cycle Infection • Low phagocytosis • Low immunoglobulin formation • Low T cell count • vulnerable mucosa • Loss of appetite • Increased calorie and protein need • Restriction of food • Loss of nutrients Malnutrition
Infection- malnutrition cycle Infection • Low phagocytosis • Low immunoglobulin formation • Low T cell count • vulnerable mucosa • Loss of appetite • Increased calorie and protein need • Restriction of food • Loss of nutrients Malnutrition
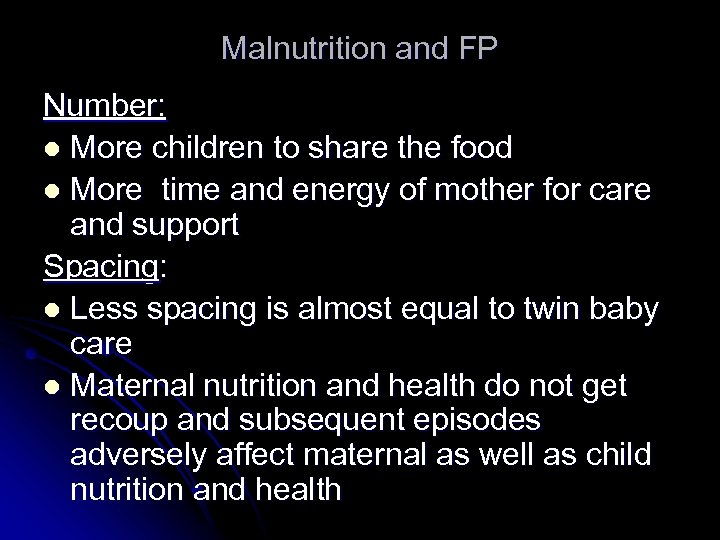 Malnutrition and FP Number: l More children to share the food l More time and energy of mother for care and support Spacing: l Less spacing is almost equal to twin baby care l Maternal nutrition and health do not get recoup and subsequent episodes adversely affect maternal as well as child nutrition and health
Malnutrition and FP Number: l More children to share the food l More time and energy of mother for care and support Spacing: l Less spacing is almost equal to twin baby care l Maternal nutrition and health do not get recoup and subsequent episodes adversely affect maternal as well as child nutrition and health
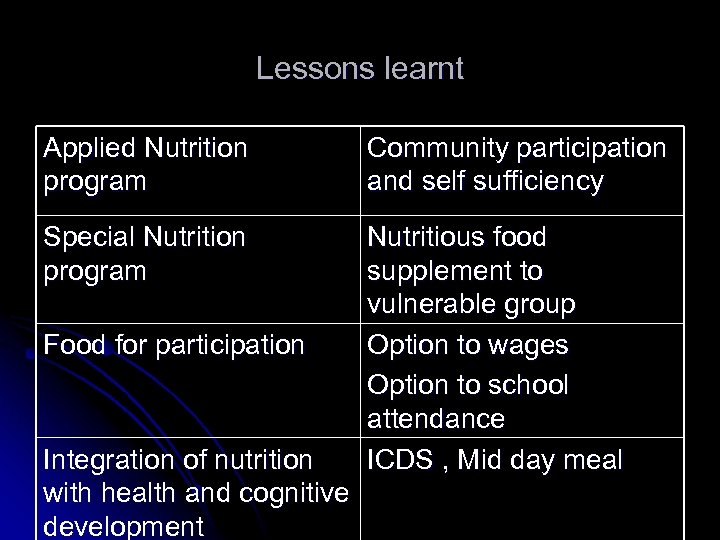 Lessons learnt Applied Nutrition program Community participation and self sufficiency Special Nutrition program Nutritious food supplement to vulnerable group Option to wages Option to school attendance ICDS , Mid day meal Food for participation Integration of nutrition with health and cognitive development
Lessons learnt Applied Nutrition program Community participation and self sufficiency Special Nutrition program Nutritious food supplement to vulnerable group Option to wages Option to school attendance ICDS , Mid day meal Food for participation Integration of nutrition with health and cognitive development
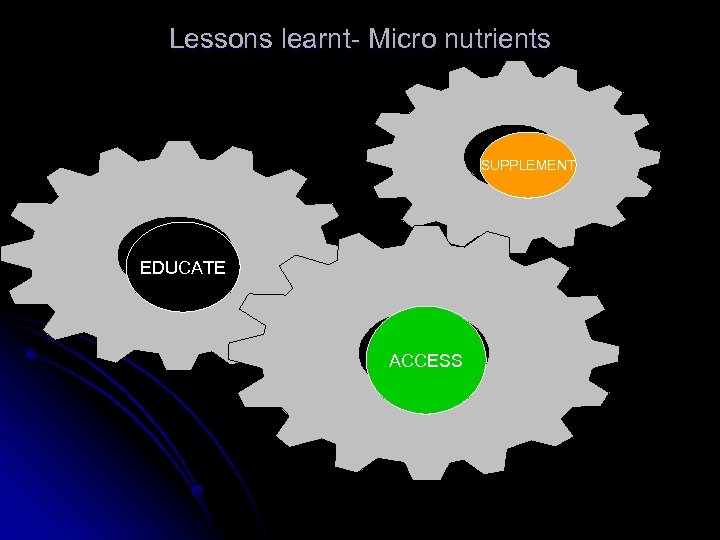 Lessons learnt- Micro nutrients SUPPLEMENT EDUCATE ACCESS
Lessons learnt- Micro nutrients SUPPLEMENT EDUCATE ACCESS
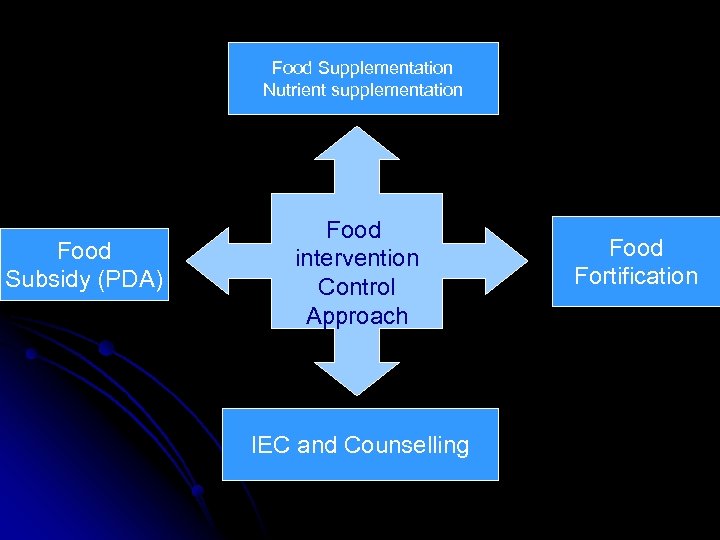 Food Supplementation Nutrient supplementation Food Subsidy (PDA) Food intervention Control Approach IEC and Counselling Food Fortification
Food Supplementation Nutrient supplementation Food Subsidy (PDA) Food intervention Control Approach IEC and Counselling Food Fortification


