ab2a7818de85e32803a068ab4316f935.ppt
- Количество слайдов: 40
 Making the Right Thing Easier… Health Plan Initiatives in Quality Enhancement and Error Reducrion The Quality Colloquium August 23, 2004 Paul Wallace MD Care Management Insti Kaiser Permanente Paul. Wallace@kp. org
Making the Right Thing Easier… Health Plan Initiatives in Quality Enhancement and Error Reducrion The Quality Colloquium August 23, 2004 Paul Wallace MD Care Management Insti Kaiser Permanente Paul. Wallace@kp. org
 Kaiser Permanente g g g g America’s oldest and largest private, nonprofit, integrated health care delivery and financing system — Founded in 1945 Multi-specialty group practice prepayment program — Headquartered in Oakland, CA Operations in 9 states and Washington, D. C. with 29 Medical Centers and 423 Clinics KP Research Centers - $100, 000 in external funding in 2003 for Health Systems Research 8. 3 million members — 6. 1 million members in California Over 12, 000 physicians representing all specialties and 130, 000+ additional employees All employees and their families are KP members 2
Kaiser Permanente g g g g America’s oldest and largest private, nonprofit, integrated health care delivery and financing system — Founded in 1945 Multi-specialty group practice prepayment program — Headquartered in Oakland, CA Operations in 9 states and Washington, D. C. with 29 Medical Centers and 423 Clinics KP Research Centers - $100, 000 in external funding in 2003 for Health Systems Research 8. 3 million members — 6. 1 million members in California Over 12, 000 physicians representing all specialties and 130, 000+ additional employees All employees and their families are KP members 2
 The Pursuit of Value: Make the right thing easier. . . g g Identify the right thing • Evidence-based medicine • Measurement • Successful practices • Member centered and culturally competent care Make the right thing easier • Focus on the delivery system • Networks of individuals and groups • Technology to support effective work 3
The Pursuit of Value: Make the right thing easier. . . g g Identify the right thing • Evidence-based medicine • Measurement • Successful practices • Member centered and culturally competent care Make the right thing easier • Focus on the delivery system • Networks of individuals and groups • Technology to support effective work 3
 The Pursuit of Defect Free Care g Critical Design Considerations • The Clinician – Knowledge management – Information seeking behavior • The Patient – Who are these folks? – What else is likely going on? Co-morbidities – What is the patient’s role in their care? g System Support • A Model of Care – The Population View – The Chronic Condition Model • Leverage of Information Technologies – Support for Decision Making – Ongoing Care 4
The Pursuit of Defect Free Care g Critical Design Considerations • The Clinician – Knowledge management – Information seeking behavior • The Patient – Who are these folks? – What else is likely going on? Co-morbidities – What is the patient’s role in their care? g System Support • A Model of Care – The Population View – The Chronic Condition Model • Leverage of Information Technologies – Support for Decision Making – Ongoing Care 4
 Knowledge Management…One Approach 5
Knowledge Management…One Approach 5
 Common Threats to Safety • • • Interruptions Fatigue Poor communication Limited memory capacity Limited ability to multi-task 6
Common Threats to Safety • • • Interruptions Fatigue Poor communication Limited memory capacity Limited ability to multi-task 6
 Information-Seeking Activities of Kaiser Permanente Clinicians Holly Jimison, Ph. D, Mina Monroe, MPH, Mary-Anna Rae, Ph. D ABD, Aaron Snyder, MD g Methodology • Observed clinical day for 20 KP clinicians – – – 4 Regions (CO, NW, NC, SC) 1 Physician consultant in each region 1 expert computer user in each region 1 Physician novice computer user in each region 1 Physician Assistant or Nurse Practitioner in each region 1 Medical specialist in each region • Data – Ethnographic Notes – Pictures – Artifacts 7
Information-Seeking Activities of Kaiser Permanente Clinicians Holly Jimison, Ph. D, Mina Monroe, MPH, Mary-Anna Rae, Ph. D ABD, Aaron Snyder, MD g Methodology • Observed clinical day for 20 KP clinicians – – – 4 Regions (CO, NW, NC, SC) 1 Physician consultant in each region 1 expert computer user in each region 1 Physician novice computer user in each region 1 Physician Assistant or Nurse Practitioner in each region 1 Medical specialist in each region • Data – Ethnographic Notes – Pictures – Artifacts 7
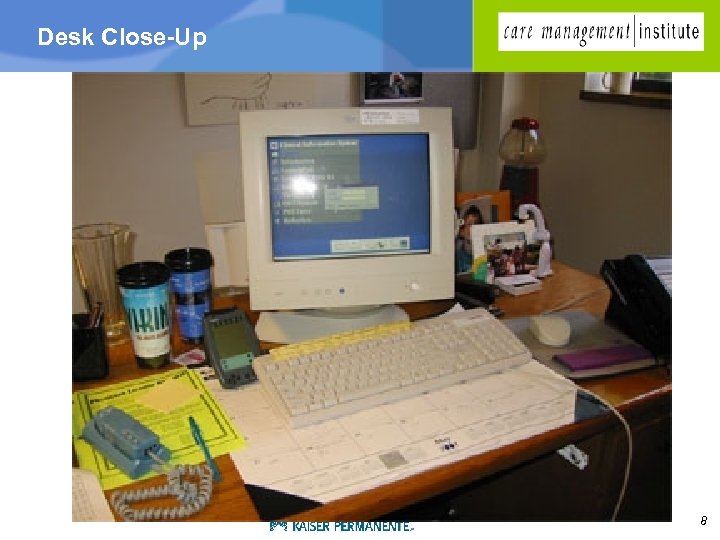 Desk Close-Up 8
Desk Close-Up 8
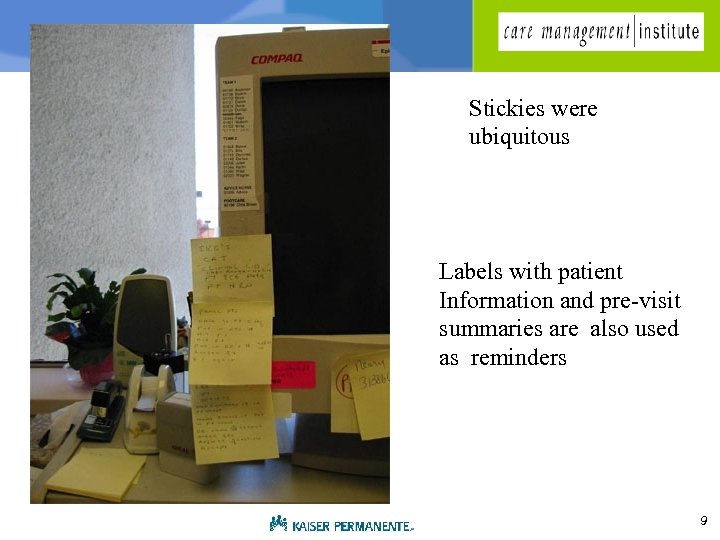 Stickies were ubiquitous Labels with patient Information and pre-visit summaries are also used as reminders 9
Stickies were ubiquitous Labels with patient Information and pre-visit summaries are also used as reminders 9
 Physicians Forget? 10
Physicians Forget? 10
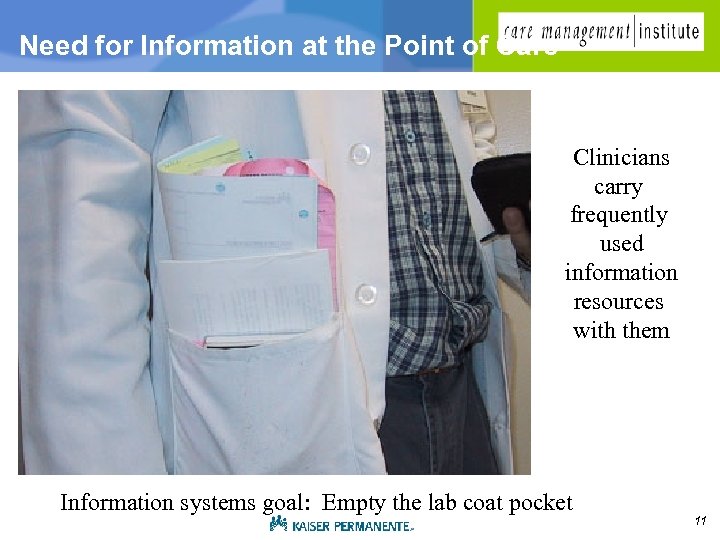 Need for Information at the Point of Care Clinicians carry frequently used information resources with them Information systems goal: Empty the lab coat pocket 11
Need for Information at the Point of Care Clinicians carry frequently used information resources with them Information systems goal: Empty the lab coat pocket 11
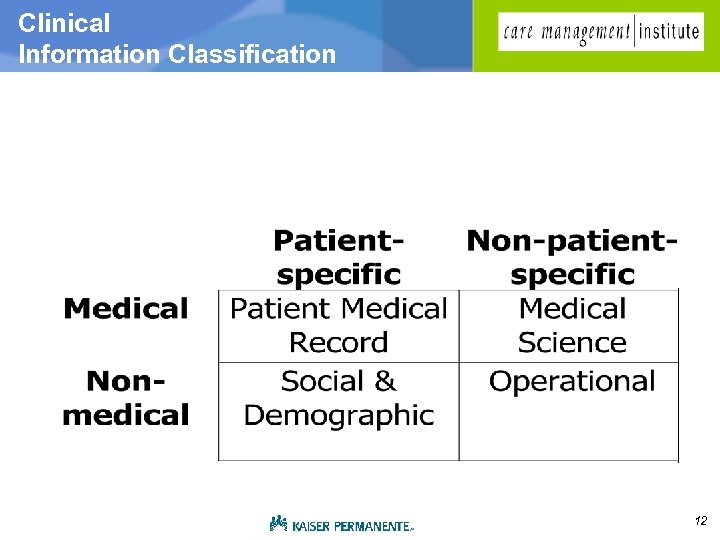 Clinical Information Classification 12
Clinical Information Classification 12
 Why Were Questions Unanswered? g Features of the environment • Time • Memory (short-term and long -term) • Pervasive irritation with handling information • Risk-aversion (economics of time invested) g Barriers • • • Design Incomplete Data Incomplete Access difficulties Time issues Communications 13
Why Were Questions Unanswered? g Features of the environment • Time • Memory (short-term and long -term) • Pervasive irritation with handling information • Risk-aversion (economics of time invested) g Barriers • • • Design Incomplete Data Incomplete Access difficulties Time issues Communications 13
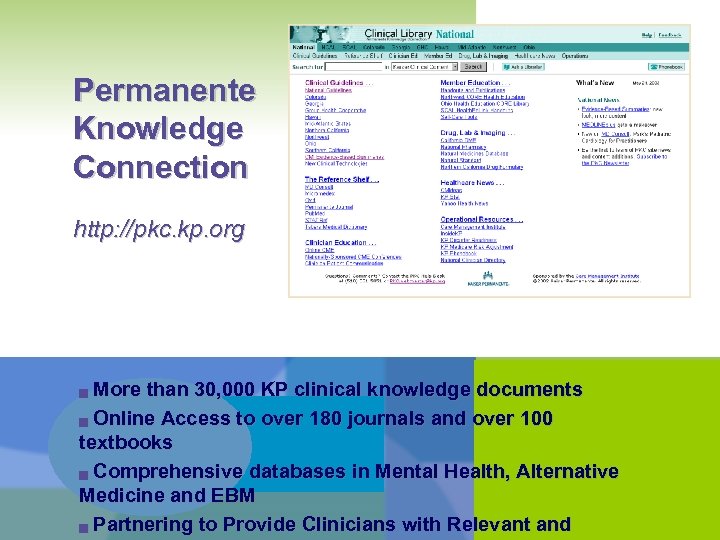 Permanente Knowledge Connection http: //pkc. kp. org More than 30, 000 KP clinical knowledge documents g Online Access to over 180 journals and over 100 textbooks g Comprehensive databases in Mental Health, Alternative Medicine and EBM g Partnering to Provide Clinicians with Relevant and g
Permanente Knowledge Connection http: //pkc. kp. org More than 30, 000 KP clinical knowledge documents g Online Access to over 180 journals and over 100 textbooks g Comprehensive databases in Mental Health, Alternative Medicine and EBM g Partnering to Provide Clinicians with Relevant and g
 15
15
 Making the right thing easier… Evidence in the exam room What’s wrong with this picture? 16
Making the right thing easier… Evidence in the exam room What’s wrong with this picture? 16
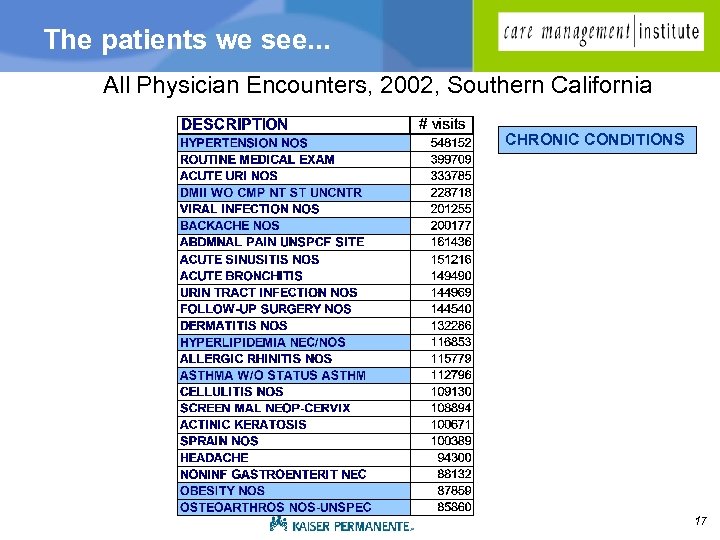 The patients we see. . . All Physician Encounters, 2002, Southern California CHRONIC CONDITIONS 17
The patients we see. . . All Physician Encounters, 2002, Southern California CHRONIC CONDITIONS 17
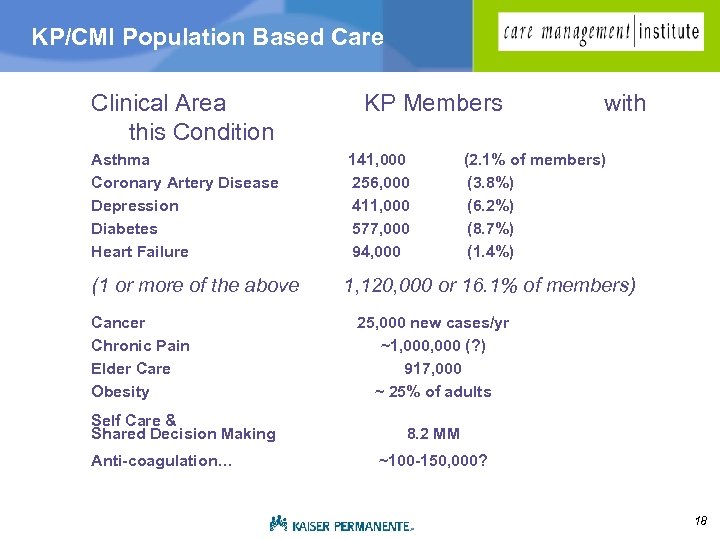 KP/CMI Population Based Care Clinical Area this Condition Asthma Coronary Artery Disease Depression Diabetes Heart Failure (1 or more of the above Cancer Chronic Pain Elder Care Obesity Self Care & Shared Decision Making Anti-coagulation… KP Members 141, 000 256, 000 411, 000 577, 000 94, 000 with (2. 1% of members) (3. 8%) (6. 2%) (8. 7%) (1. 4%) 1, 120, 000 or 16. 1% of members) 25, 000 new cases/yr ~1, 000 (? ) 917, 000 ~ 25% of adults 8. 2 MM ~100 -150, 000? 18
KP/CMI Population Based Care Clinical Area this Condition Asthma Coronary Artery Disease Depression Diabetes Heart Failure (1 or more of the above Cancer Chronic Pain Elder Care Obesity Self Care & Shared Decision Making Anti-coagulation… KP Members 141, 000 256, 000 411, 000 577, 000 94, 000 with (2. 1% of members) (3. 8%) (6. 2%) (8. 7%) (1. 4%) 1, 120, 000 or 16. 1% of members) 25, 000 new cases/yr ~1, 000 (? ) 917, 000 ~ 25% of adults 8. 2 MM ~100 -150, 000? 18
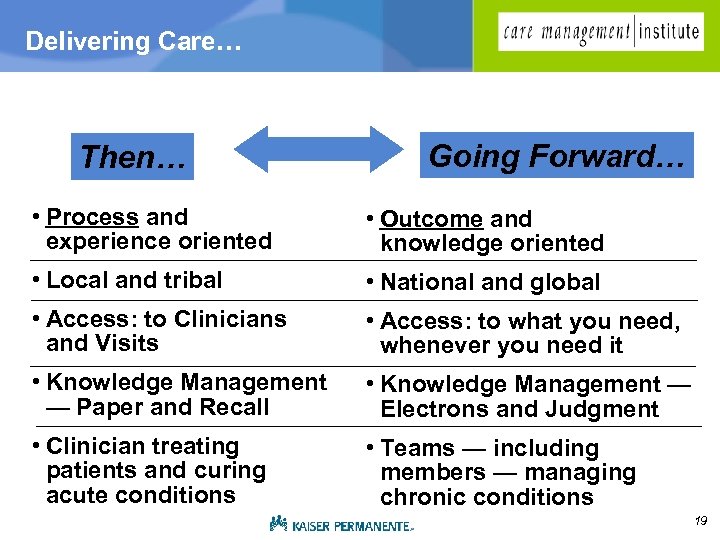 Delivering Care… Then… Going Forward… • Process and experience oriented • Outcome and knowledge oriented • Local and tribal • National and global • Access: to Clinicians and Visits • Access: to what you need, whenever you need it • Knowledge Management — Paper and Recall • Knowledge Management — Electrons and Judgment • Clinician treating patients and curing acute conditions • Teams — including members — managing chronic conditions 19
Delivering Care… Then… Going Forward… • Process and experience oriented • Outcome and knowledge oriented • Local and tribal • National and global • Access: to Clinicians and Visits • Access: to what you need, whenever you need it • Knowledge Management — Paper and Recall • Knowledge Management — Electrons and Judgment • Clinician treating patients and curing acute conditions • Teams — including members — managing chronic conditions 19
 20
20
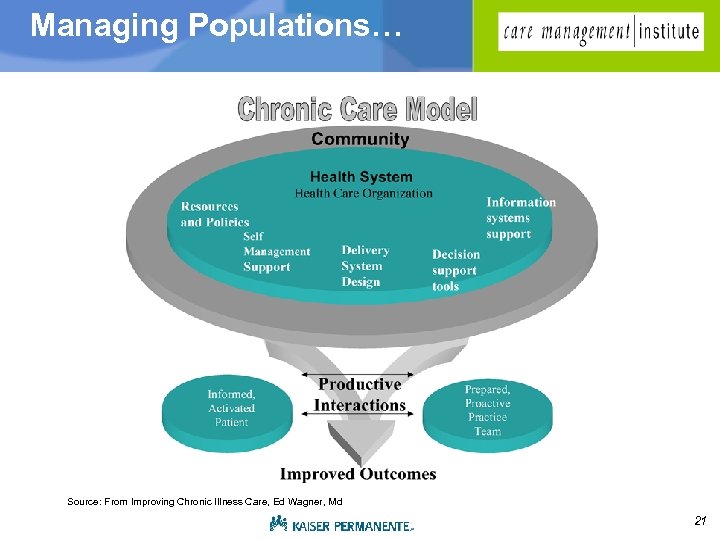 Managing Populations… Source: From Improving Chronic Illness Care, Ed Wagner, Md 21
Managing Populations… Source: From Improving Chronic Illness Care, Ed Wagner, Md 21
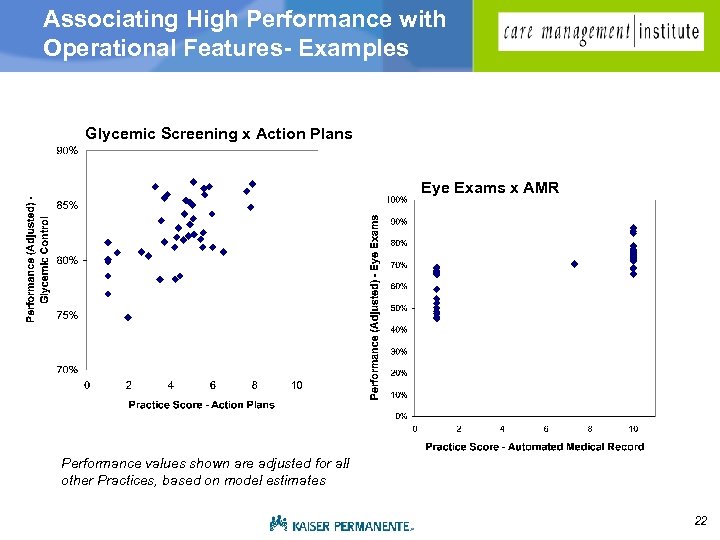 Associating High Performance with Operational Features- Examples Glycemic Screening x Action Plans Eye Exams x AMR Performance values shown are adjusted for all other Practices, based on model estimates 22
Associating High Performance with Operational Features- Examples Glycemic Screening x Action Plans Eye Exams x AMR Performance values shown are adjusted for all other Practices, based on model estimates 22
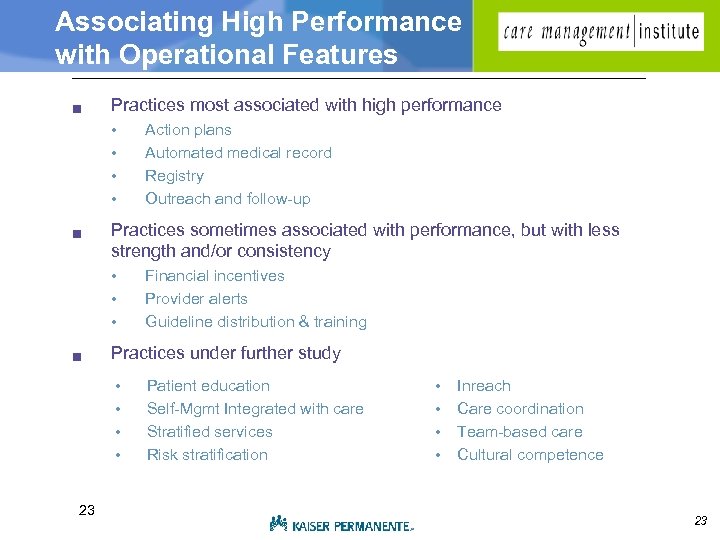 Associating High Performance with Operational Features g Practices most associated with high performance • • g Practices sometimes associated with performance, but with less strength and/or consistency • • • g Financial incentives Provider alerts Guideline distribution & training Practices under further study • • 23 Action plans Automated medical record Registry Outreach and follow-up Patient education Self-Mgmt Integrated with care Stratified services Risk stratification • • Inreach Care coordination Team-based care Cultural competence 23
Associating High Performance with Operational Features g Practices most associated with high performance • • g Practices sometimes associated with performance, but with less strength and/or consistency • • • g Financial incentives Provider alerts Guideline distribution & training Practices under further study • • 23 Action plans Automated medical record Registry Outreach and follow-up Patient education Self-Mgmt Integrated with care Stratified services Risk stratification • • Inreach Care coordination Team-based care Cultural competence 23
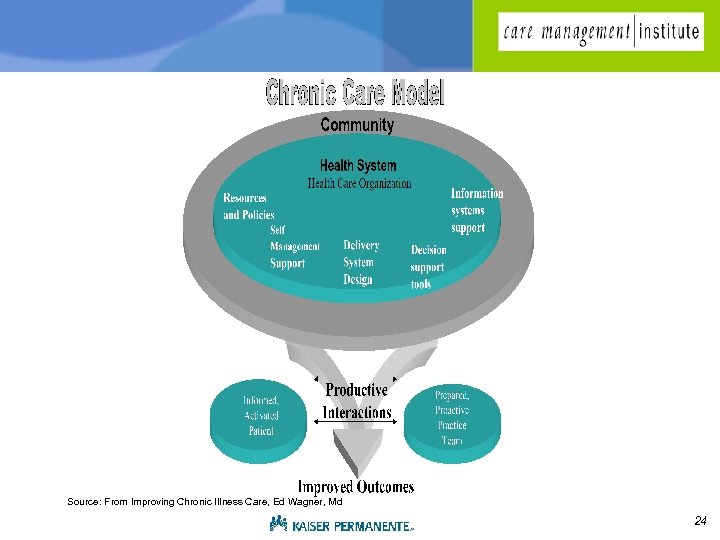 Source: From Improving Chronic Illness Care, Ed Wagner, Md 24
Source: From Improving Chronic Illness Care, Ed Wagner, Md 24
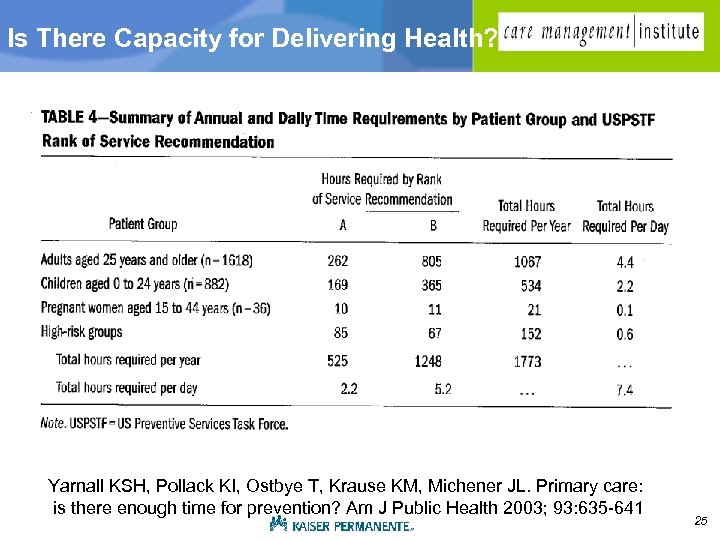 Is There Capacity for Delivering Health? Yarnall KSH, Pollack KI, Ostbye T, Krause KM, Michener JL. Primary care: is there enough time for prevention? Am J Public Health 2003; 93: 635 -641 25
Is There Capacity for Delivering Health? Yarnall KSH, Pollack KI, Ostbye T, Krause KM, Michener JL. Primary care: is there enough time for prevention? Am J Public Health 2003; 93: 635 -641 25
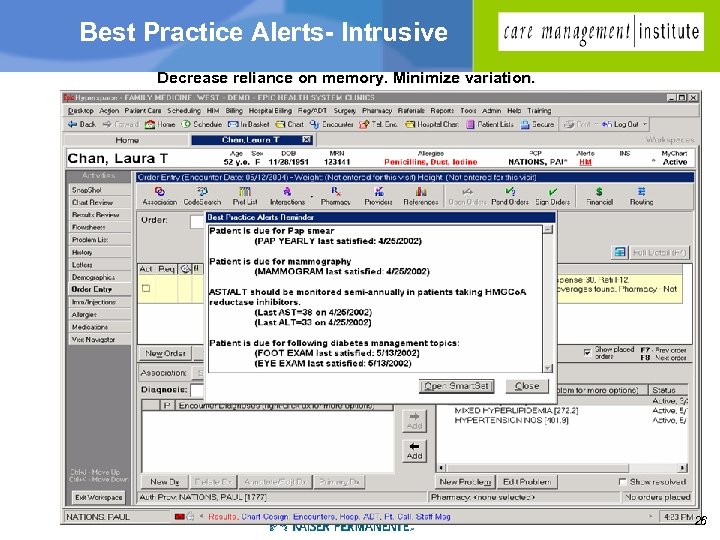 Best Practice Alerts- Intrusive Decrease reliance on memory. Minimize variation. 26
Best Practice Alerts- Intrusive Decrease reliance on memory. Minimize variation. 26
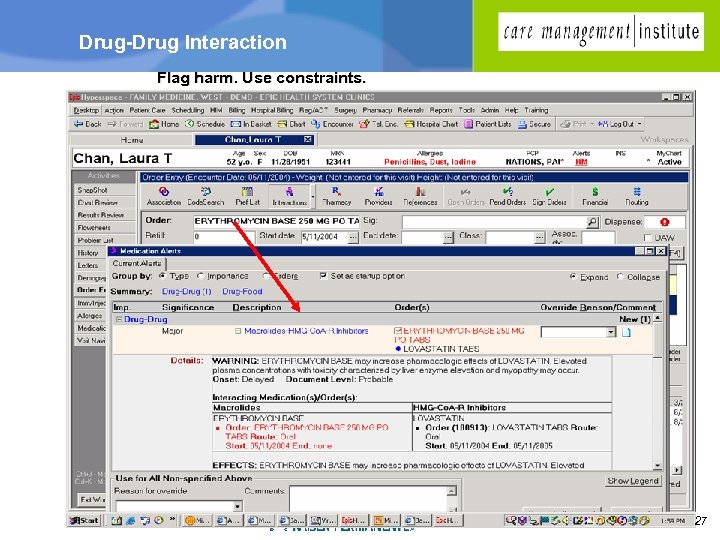 Drug-Drug Interaction Flag harm. Use constraints. 27
Drug-Drug Interaction Flag harm. Use constraints. 27
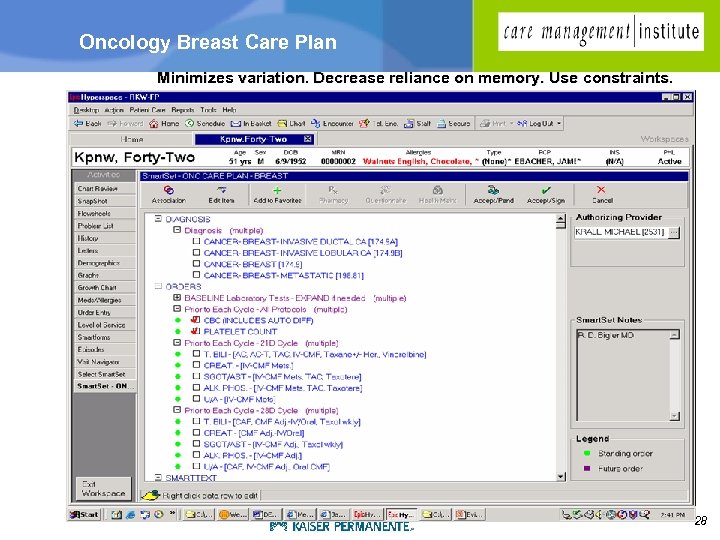 Oncology Breast Care Plan Minimizes variation. Decrease reliance on memory. Use constraints. 28
Oncology Breast Care Plan Minimizes variation. Decrease reliance on memory. Use constraints. 28
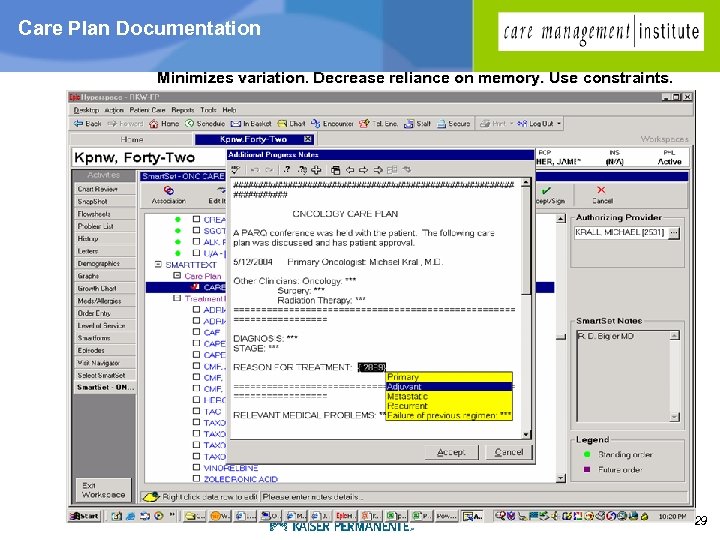 Care Plan Documentation Minimizes variation. Decrease reliance on memory. Use constraints. 29
Care Plan Documentation Minimizes variation. Decrease reliance on memory. Use constraints. 29
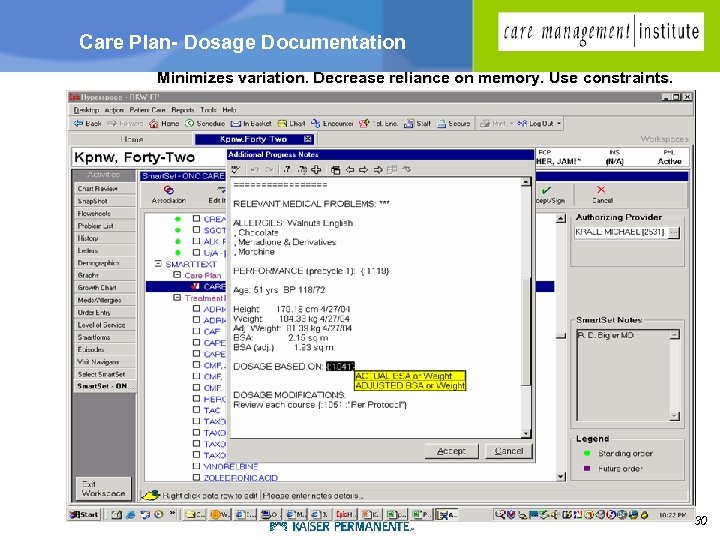 Care Plan- Dosage Documentation Minimizes variation. Decrease reliance on memory. Use constraints. 30
Care Plan- Dosage Documentation Minimizes variation. Decrease reliance on memory. Use constraints. 30
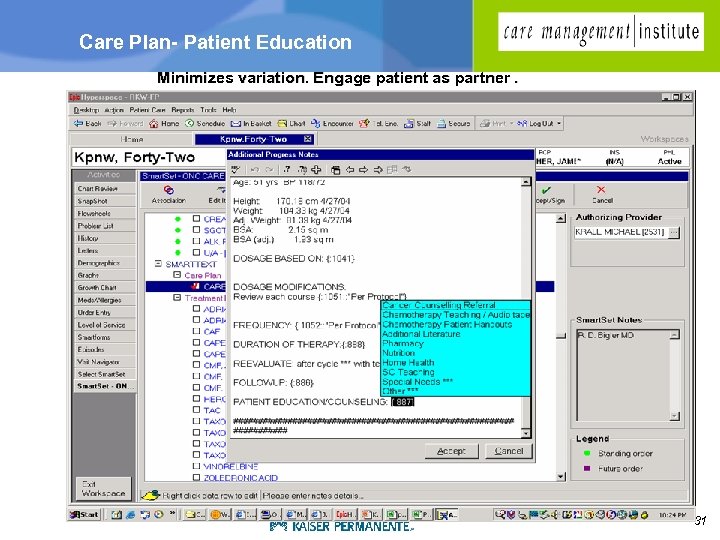 Care Plan- Patient Education Minimizes variation. Engage patient as partner. 31
Care Plan- Patient Education Minimizes variation. Engage patient as partner. 31
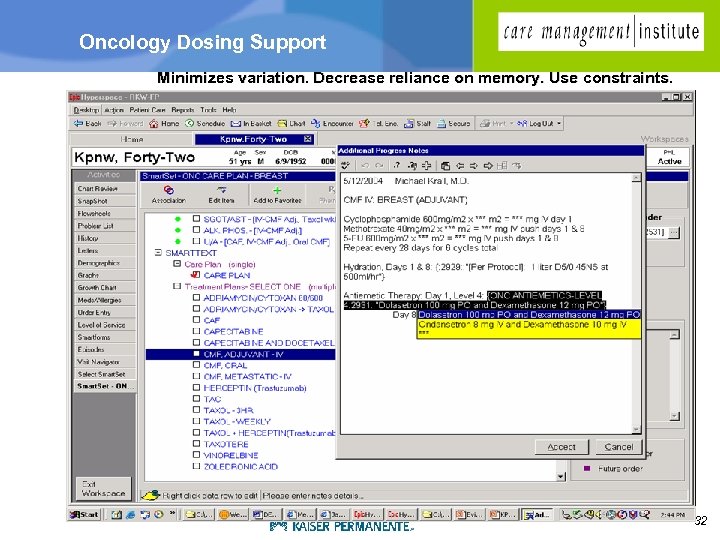 Oncology Dosing Support Minimizes variation. Decrease reliance on memory. Use constraints. 32
Oncology Dosing Support Minimizes variation. Decrease reliance on memory. Use constraints. 32
 Safe, Evidence-based Oncology Care g Treatment Plan Management • Oncologists g Treatment Administration • Treatment Nurses/Pharmacists g Infusion Center Management • Treatment Coordinators g Patient View of Treatment Plan • Patients Designed With Safety in Mind 33
Safe, Evidence-based Oncology Care g Treatment Plan Management • Oncologists g Treatment Administration • Treatment Nurses/Pharmacists g Infusion Center Management • Treatment Coordinators g Patient View of Treatment Plan • Patients Designed With Safety in Mind 33
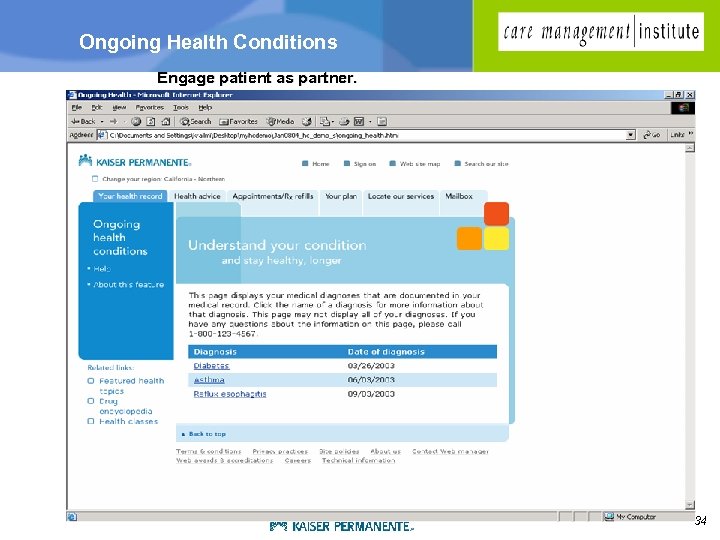 Ongoing Health Conditions Engage patient as partner. 34
Ongoing Health Conditions Engage patient as partner. 34
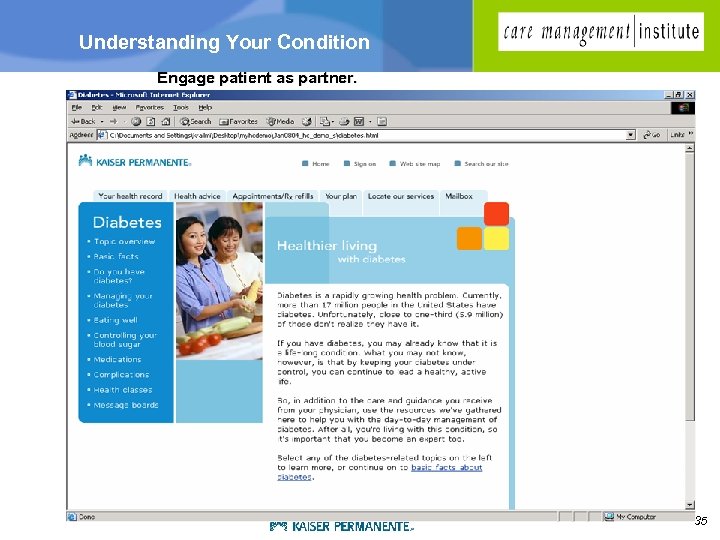 Understanding Your Condition Engage patient as partner. 35
Understanding Your Condition Engage patient as partner. 35
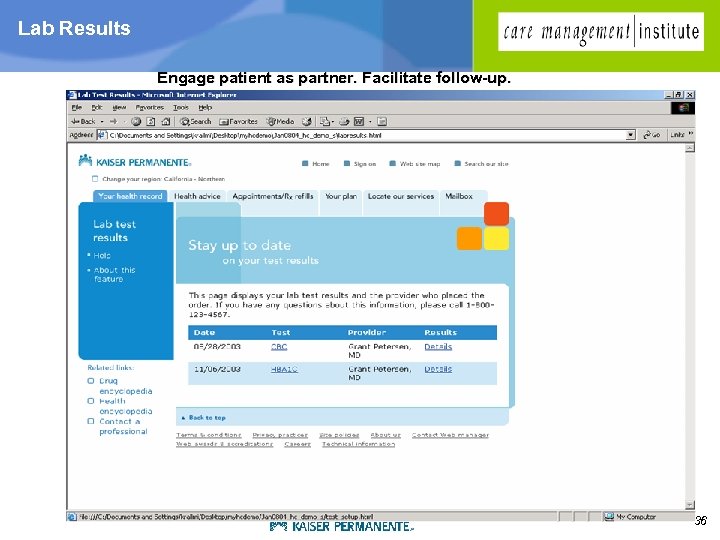 Lab Results Engage patient as partner. Facilitate follow-up. 36
Lab Results Engage patient as partner. Facilitate follow-up. 36
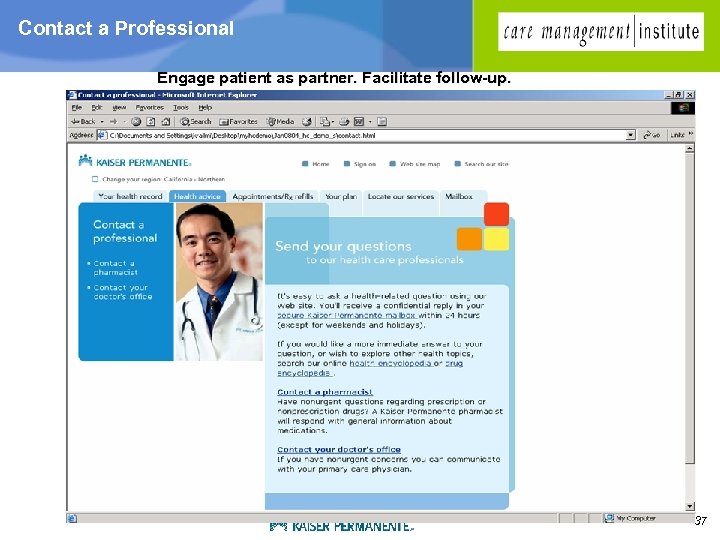 Contact a Professional Engage patient as partner. Facilitate follow-up. 37
Contact a Professional Engage patient as partner. Facilitate follow-up. 37
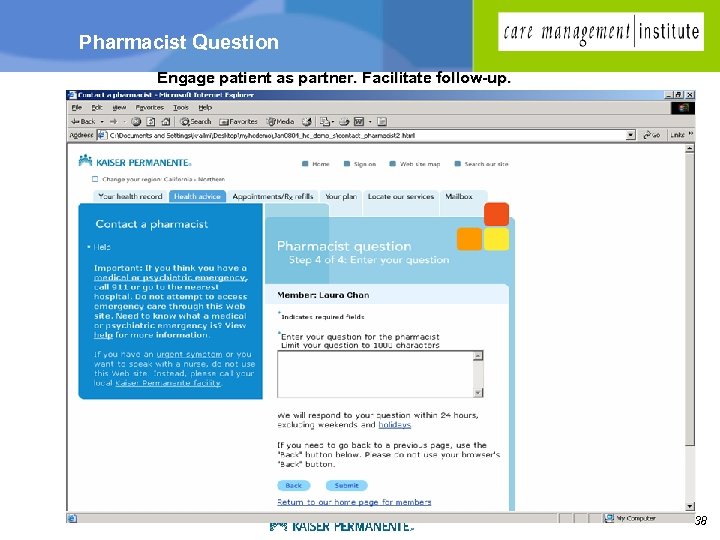 Pharmacist Question Engage patient as partner. Facilitate follow-up. 38
Pharmacist Question Engage patient as partner. Facilitate follow-up. 38
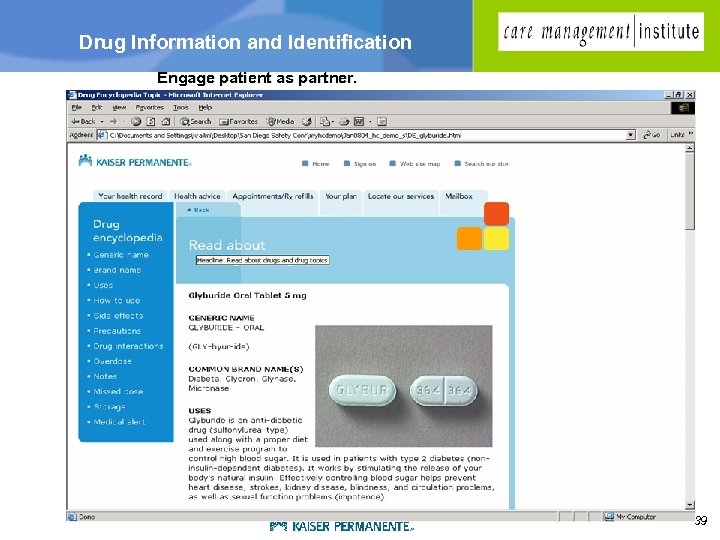 Drug Information and Identification Engage patient as partner. 39
Drug Information and Identification Engage patient as partner. 39
 If we can make the right thing easier… …it will likely happen Clinicians + Systems + Patients
If we can make the right thing easier… …it will likely happen Clinicians + Systems + Patients


