MBBS - HLA and Transplantation.ppt
- Количество слайдов: 43

MAJOR HISTO-COMPATIBILITY TRANSPLANTATION
OBJECTIVES • HLA & MHC • STRUCTURE OF HLA CLASSES • ROLE / FUNCTION OF HLA IN IMMUNOLOGICAL REACTION • TRANSPLANTATION • TISSUE TYPING – LABORATORY TESTS
HLA & MHC • HLA: Human Leukocyte Antigen • MHC: Major Histocompability Complex HLA is also called histocompatibility antigens are cell surface antigens that induce an immune response leading to rejection of allografts. MHC is a complex of genes on a segment of chromosome pair coding for 3 different classes of protiens. The major antigens determining histocompatibility in humans are characteristically found on the surface of leukocytes. Human MHC antigens are synonymous with HLA and the MHC complex of genes with HLA complex.
What is HLA? • Human Leukocyte Antigen (HLA) – Gene product of the HLA region on chromosome 6 that encodes for cell surface antigen-presenting proteins • HLA region is classified into 3 parts: – MHC Class III
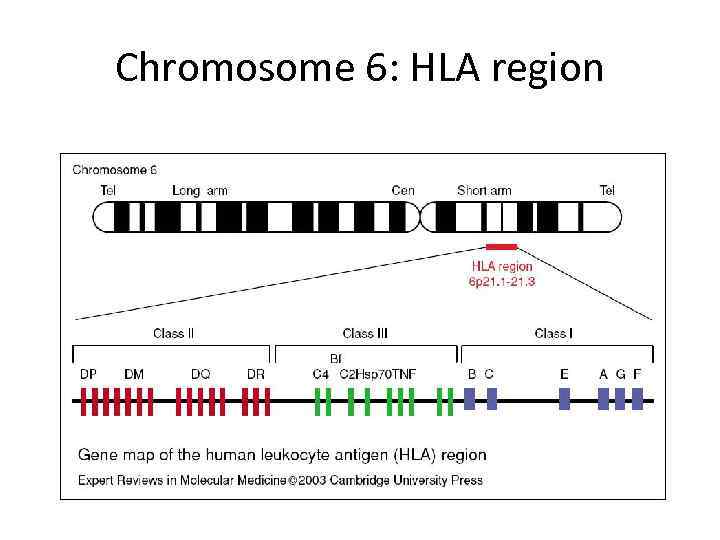
Chromosome 6: HLA region
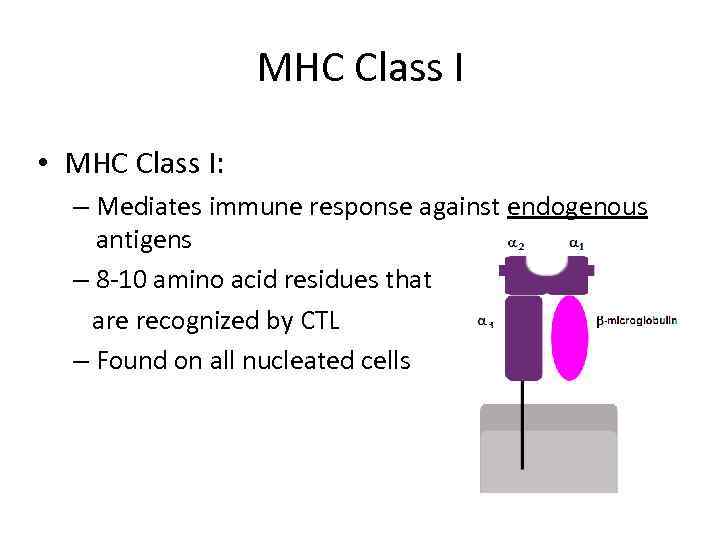
MHC Class I • MHC Class I: – Mediates immune response against endogenous antigens – 8 -10 amino acid residues that are recognized by CTL – Found on all nucleated cells
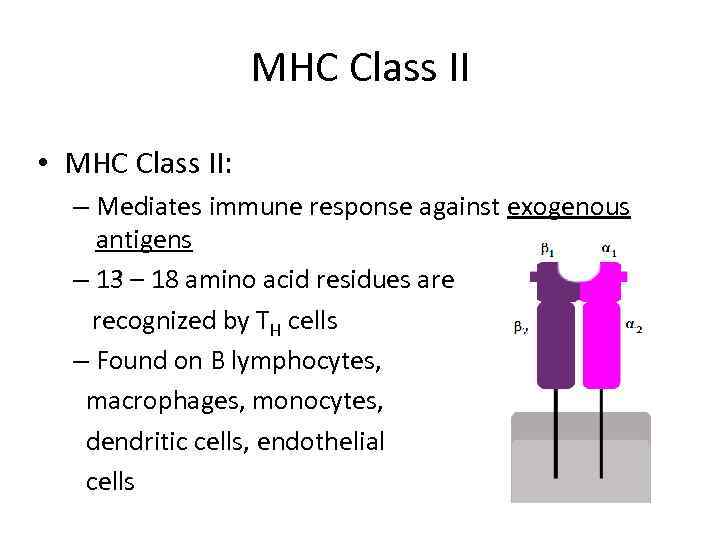
MHC Class II • MHC Class II: – Mediates immune response against exogenous antigens – 13 – 18 amino acid residues are recognized by TH cells – Found on B lymphocytes, macrophages, monocytes, dendritic cells, endothelial cells
MHC Class III • MHC Class III: – Codes for genes unrelated to cell-mediated immunity – Codes for components such as TNF, Hsp, complement proteins (C 2, C 4, BF)
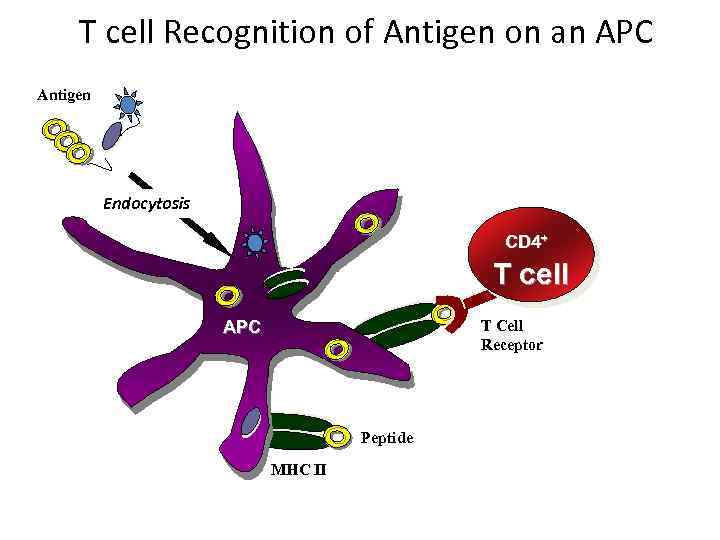
T cell Recognition of Antigen on an APC Antigen Endocytosis T cell CD 4+ T Cell Receptor APC Peptide MHC II
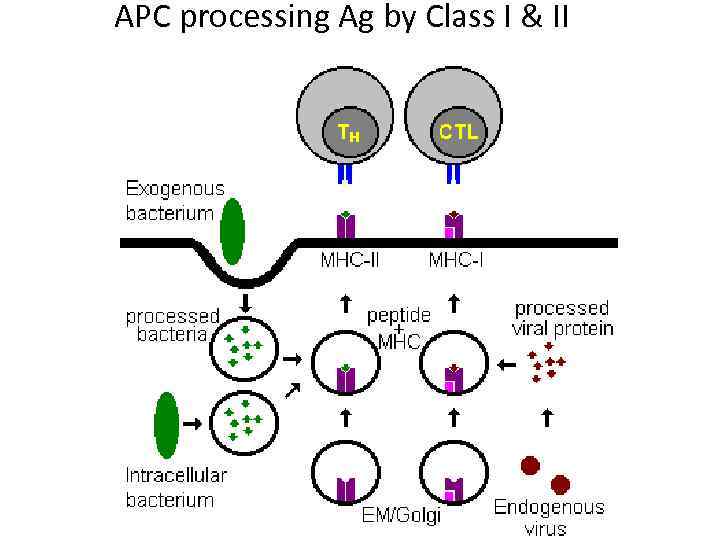
APC processing Ag by Class I & II
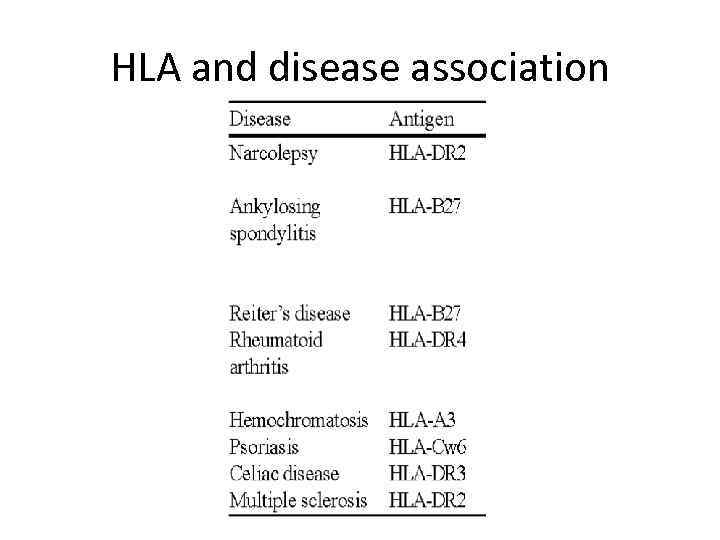
HLA and disease association © Ranjith’s
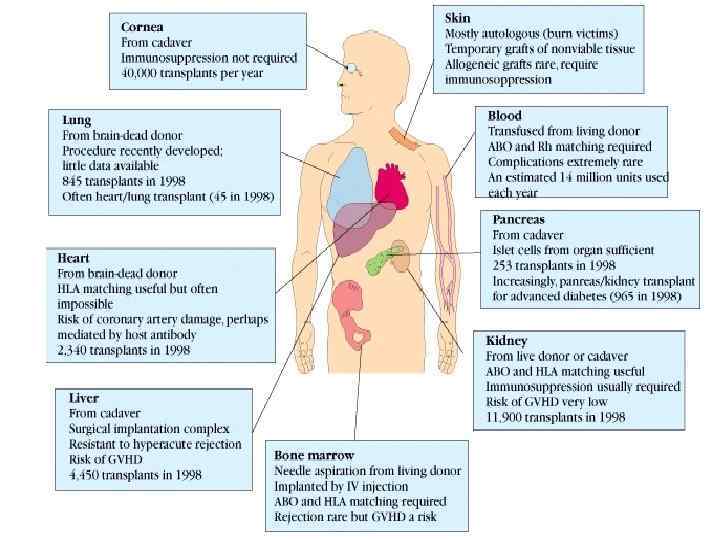
TRANSPLANTATION Replacement of a diseased or damaged organ or tissue by healthy organ or tissue for the restoration of function is known as transplantation. Donor: individual from whom the transplant is obtained. Recipient: individual to whom it is applied.
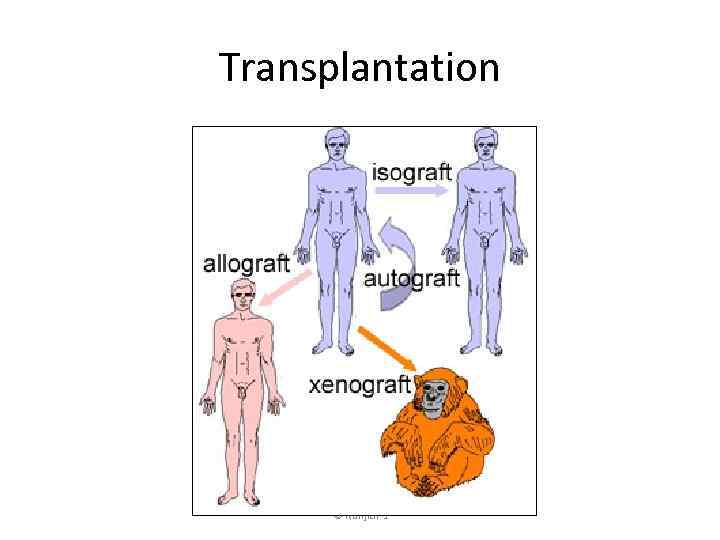
Transplantation © Ranjith’s
Levels of Rejection • • Hyper Acute Rejection Chronic Rejection Graft Versus Host Rejection
© Ranjith’s
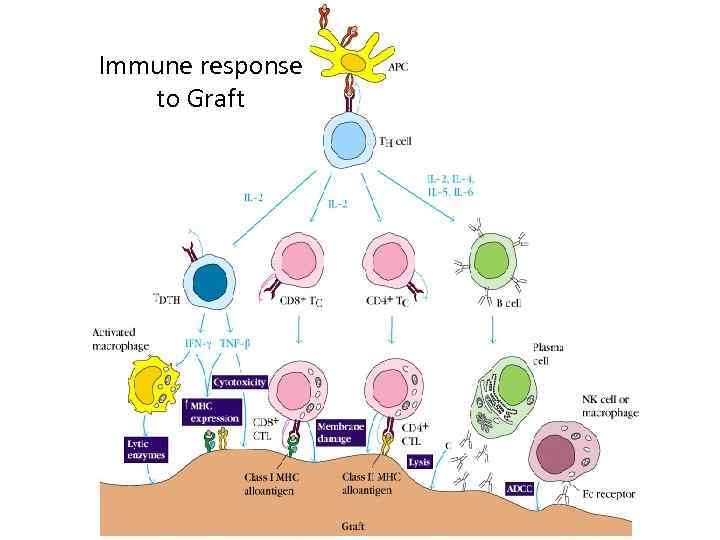
Immune response to Graft © Ranjith’s
HYPERACUTE REJECTION • Minutes - hours • Existing recipient alloantibodies • Attacks donor vascular endothelial cells • Rapid thrombotic occlusion of graft vasculature • Tissue ischemia, inflammation, cell death
Hyper Acute Rejection Mechanism: Much of the damage results from release of lysosomal enzymes by PMNs that accumulate in response to the release of C 5 a. This leads to thrombosis and endothelial cell injury. Fibroid necrosis is also often seen.
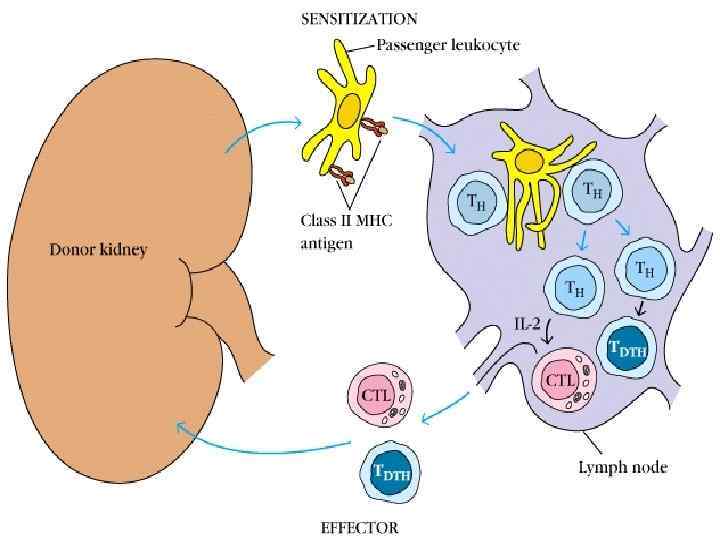
HYPERACUTE RX • Avoidance of high-risk donor/recipient combinations • HLA, ABO matching • Pretransplant cross-match tests
Acute rejection • Occurs between 7 and 21 days after the transplant • It is due to induction of T cell reactions against the graft, leading to direct cytotoxicity of the cells and massive mononuclear cell infiltration. • Mechanism: The lymphokines result in a massive mononuclear cell infiltrate into the cortical interstitium which become so large that the pressure closes the arterioles. Most damage to the cells of the graft is from hypoxia (lack of oxygen) due to the interrupted blood flow. The damage causes a rapid decrease in renal failure with resultant decrease in urine output, rise in serum creatinine levels, and the presence of proteins and blood cells in the urine.
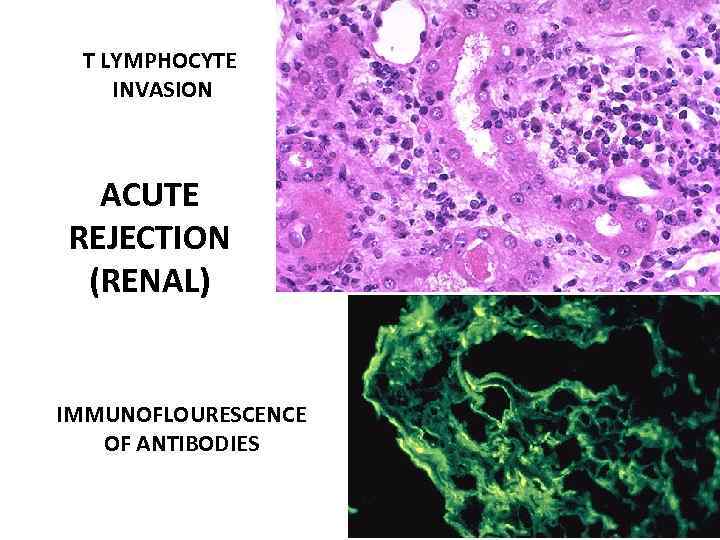
T LYMPHOCYTE INVASION ACUTE REJECTION (RENAL) IMMUNOFLOURESCENCE OF ANTIBODIES
ACUTE RX • Steroids • T cell inhibition • B cell inhibition • Cytokine blockers
CHRONIC REJECTION • Persistent alloimmunity to donor antigens plus poor transplant organ function • Develops after weeks to years • Risks include peritransplant injury, acute rejection episodes and chronic infection • Inflammation, smooth muscle proliferation, fibrosis • Tissue ischemia
Chronic rejection In kidneys -vproliferative inflammatory lesions of the small arterioles vthickening of the glomerular basement membrane vinterstitial fibrosis • Most of the damage occur at the time of diagnosis, immunosuppression is of little use and the graft probably cannot be saved
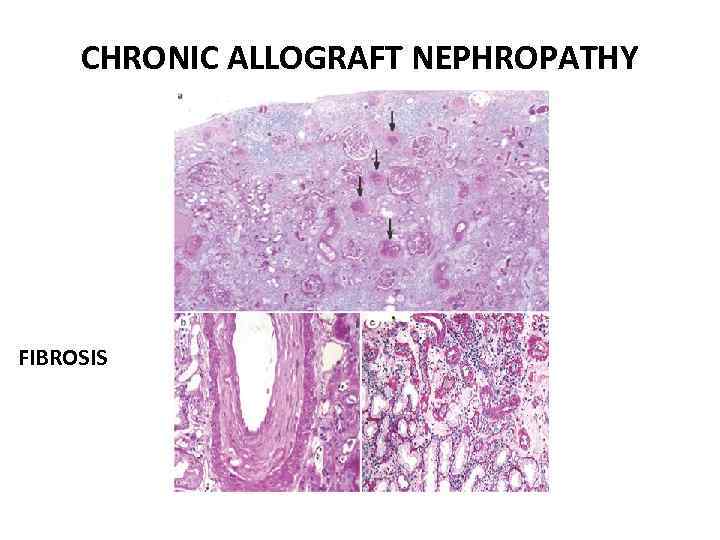
CHRONIC ALLOGRAFT NEPHROPATHY FIBROSIS
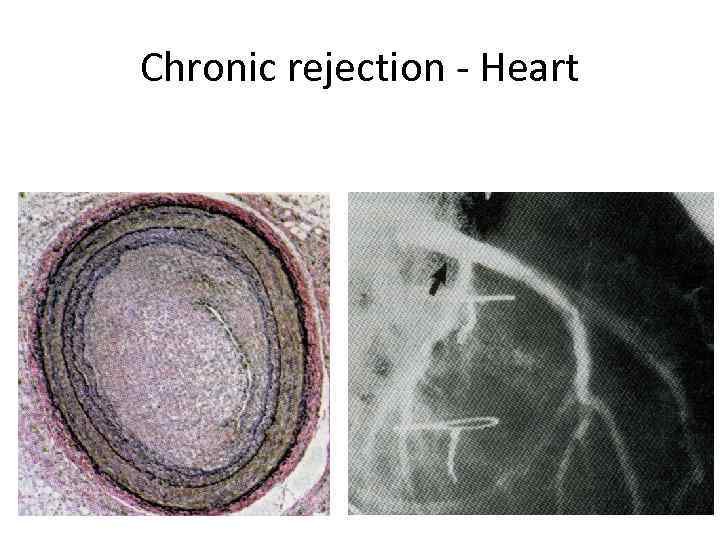
Chronic rejection - Heart
CHRONIC RX • Prevention of peritransplant ischemia and reperfusion injury
Effect of Matching • The three class I genes (HLA-A, B & C) serve as the main targets of graft rejection A mismatch in these genes stimulates production of the cytokines, which in turn, enhance all immune responses in the area including the ones to HLA-B and -A. There is a strong synergy between mismatches in both class II and class I genes
Tissue typing: Micro/Lympho Cytotoxicity Assay • A panel of HLA specific antibodies is used to determine the phenotype of MHC Ag expressed on the cells • Phenotypic assays include – Immunoflouresence staining – Fluorescence-activated cell sorting FACS – Microcytotoxicity Assay (or) Lymphocytotoxicity Assay
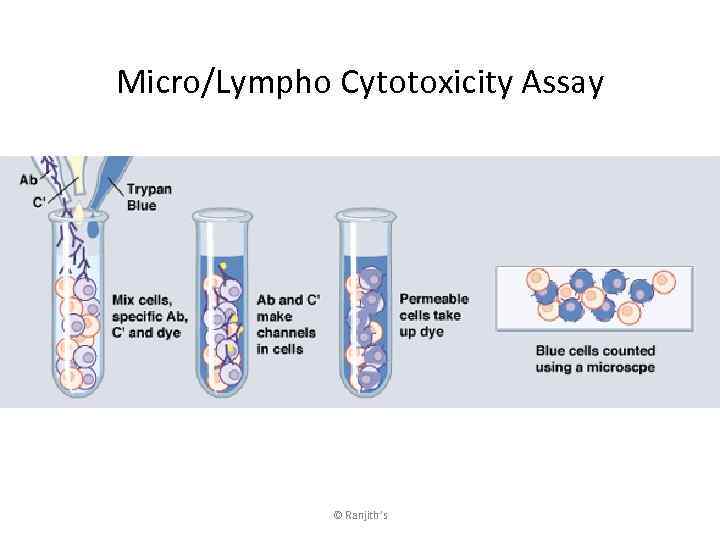
Micro/Lympho Cytotoxicity Assay © Ranjith’s
Micro/Lympho Cytotoxicity Assay • MHC specific Abs in presence of complement destroys the lymphocytes • Donor and recipient lymphocytes are reacted with a panel of Abs with specificity for wide range of MHC I and II alleles • Complement mediated killing of lymphocytes indicates that the Ab has reacted with cellsurface MHC, thus the cells are positive for that MHC allele
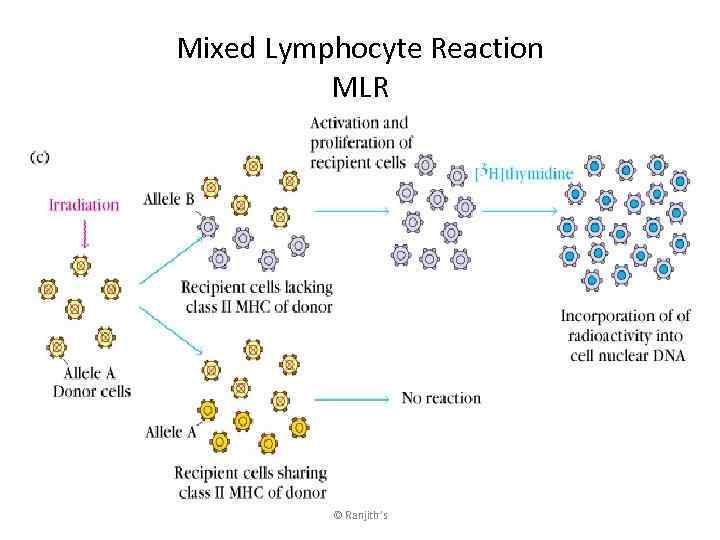
Mixed Lymphocyte Reaction MLR © Ranjith’s
MLR 1. The MLR is an in vitro reaction used to analyze the response of a patient’s Tcells to foreign MHC molecules, and thus predict the likelihood of T-cell mediated graft rejection. 2. To set up a MLR, mononuclear leukocytes (e. g. T-cells, B-cells, NK-cells, DCs) isolated from the peripheral blood of both donor and host are cultured together. If donor and host have different MHC alleles, the mononuclear cells will proliferate in 4 -7 days. This proliferation response is the so-called MLR 3. However, if donor and host mononuclear cells were simply cultured together (a ‘twoway’ MLR), there would be proliferation of both cell populations, thus confusing results. Instead, a ‘one-way’ MLR is typically performed – cells from the donor are irradiated, rendering them incapable of mitosis. Thus, in a one-way MLR, only host cells can proliferate in the co-culture. 4. In the one-way MLR, T-cells from the host will recognize allogenic MHC molecules on the donor cells, and begin to proliferate. This proliferation can be measured, and can reveal whether MHC class I or II from the donor is involved. © Ranjith’s
© Ranjith’s
Graft versus Host Disease • Graft Vs Host rejection is life threatening complication • Donor T cells recognize recipient MHC Ag (Minor Histocompatibility Ag) as foreign and reject • This reaction particularly important in cases in which immunocompetent lymphoid cells are transplanted into immunologically incompetent or immunosupressed and therefore cannot reject the transplanted tissue e. g - Bone marrow transplantation • Can occur even when HLA are perfectly matched between donor and recipient • Donor lymphocytes recruit recipient inflammatory cells – chiefly responsible for destruction of tissue
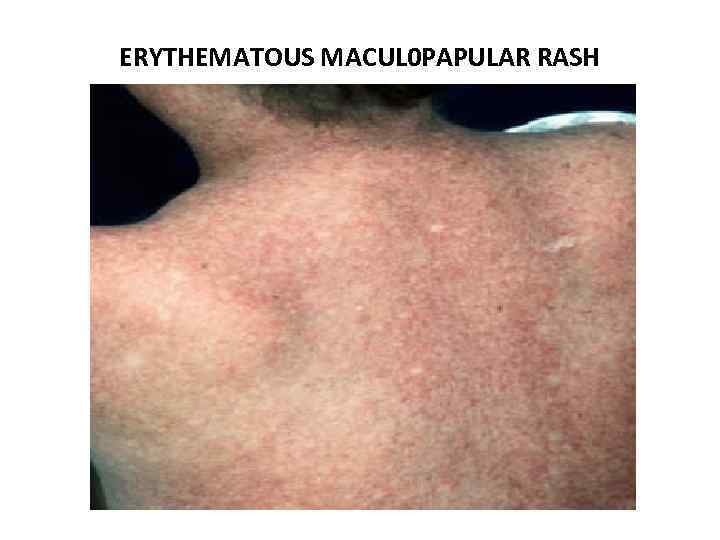
ERYTHEMATOUS MACUL 0 PAPULAR RASH

BULLAE FORMATION
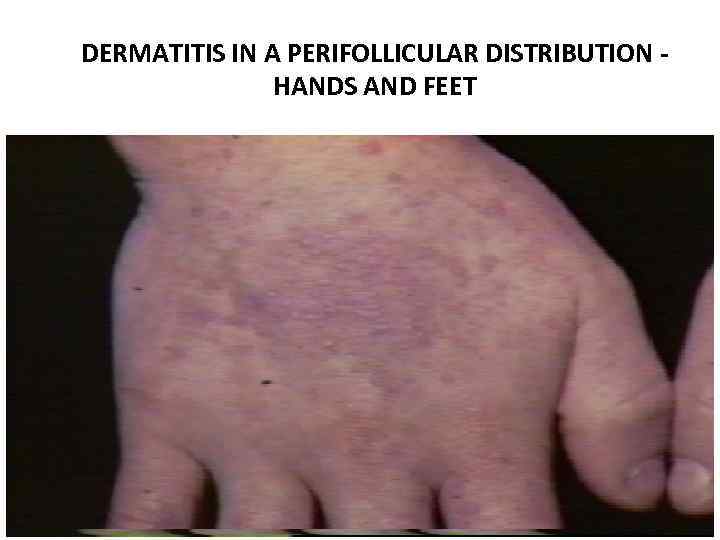
DERMATITIS IN A PERIFOLLICULAR DISTRIBUTION HANDS AND FEET
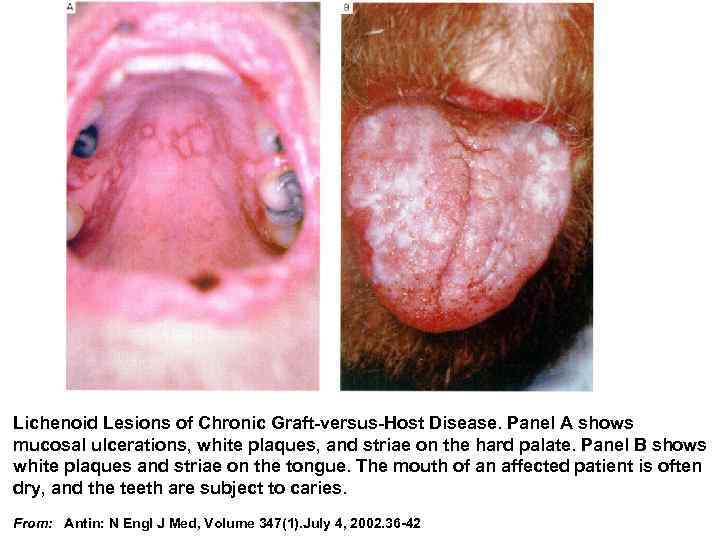
Lichenoid Lesions of Chronic Graft-versus-Host Disease. Panel A shows mucosal ulcerations, white plaques, and striae on the hard palate. Panel B shows white plaques and striae on the tongue. The mouth of an affected patient is often dry, and the teeth are subject to caries. From: Antin: N Engl J Med, Volume 347(1). July 4, 2002. 36 -42
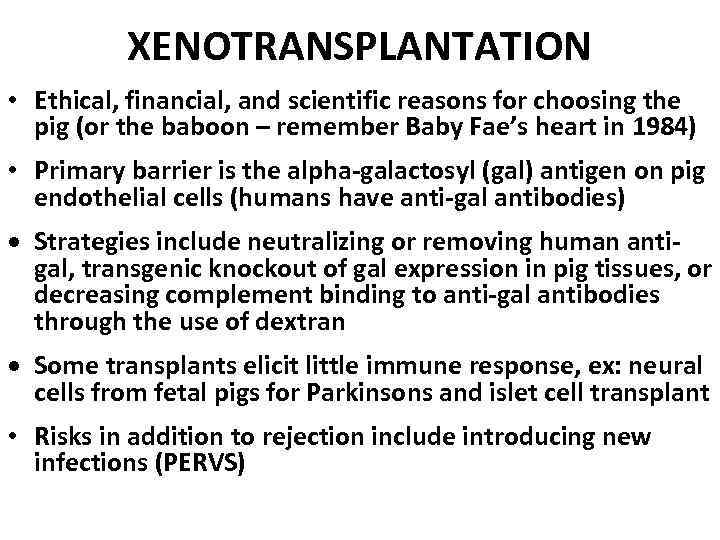
XENOTRANSPLANTATION • Ethical, financial, and scientific reasons for choosing the pig (or the baboon – remember Baby Fae’s heart in 1984) • Primary barrier is the alpha-galactosyl (gal) antigen on pig endothelial cells (humans have anti-gal antibodies) Strategies include neutralizing or removing human antigal, transgenic knockout of gal expression in pig tissues, or decreasing complement binding to anti-gal antibodies through the use of dextran Some transplants elicit little immune response, ex: neural cells from fetal pigs for Parkinsons and islet cell transplant • Risks in addition to rejection include introducing new infections (PERVS)
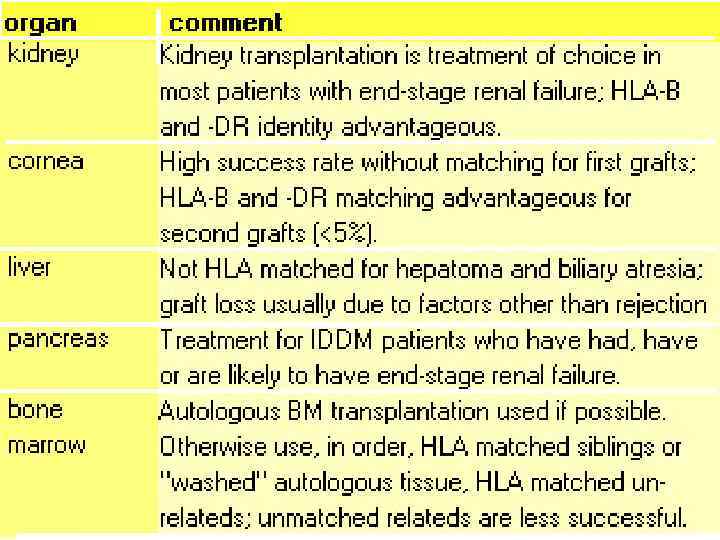
© Ranjith’s
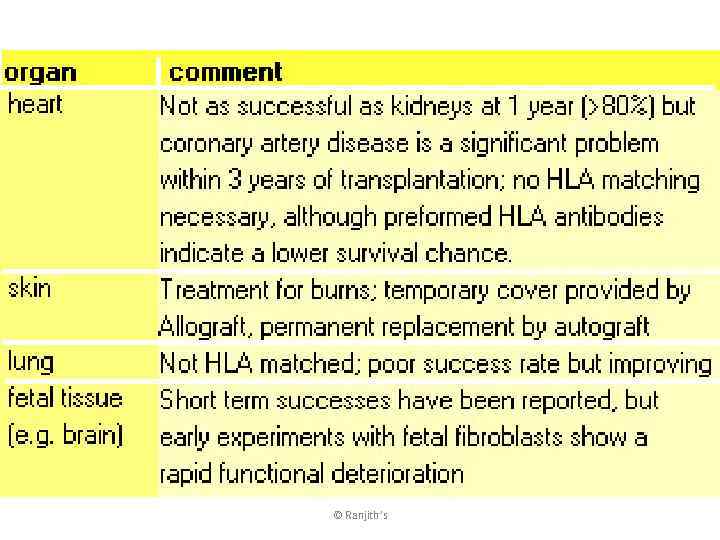
© Ranjith’s

THANK YOU
MBBS - HLA and Transplantation.ppt