c549ffbe7c800731e9255e61e0e87ff7.ppt
- Количество слайдов: 37

Mainstreaming telecare in the UK. Overcoming the barriers James Barlow Innovation Studies Centre Imperial College London Southern Institute for Health Informatics Conference University of Portsmouth 12 June 2003
Agenda § Background § Telecare services § Mainstreaming telecare § Conclusions
Agenda § Background § Telecare services § Mainstreaming telecare § Conclusions

Demands on care provision § Demographic and social change § Rising cost of care delivery § Demand for better quality services and improved access § Staff shortages
Government aspirations § The government wishes to see ‘home telemonitoring’ available in 20% of homes requiring it by December 2007 and 100% of homes requiring it by December 2010
Policy context § Information for Health (NHS Executive, 1998) § The Royal Commission on Long Term Care (1999) § Fully Equipped and Fully Equipped 2002 (Audit Commission, 2000, 2002) § Valuing People: A New Strategy for Learning Disability for the 21 st Century (DOH, 2001) § Integrating Community Equipment Services (ICES) (DOH, 2001) § National Service Framework for Older People (DOH, 2001) § Quality and Choice for Older People’s Housing – A Strategic Framework (DETR/Do. H, 2001) § The House of Commons Health Committee (2002) § National strategic programme for IT in the NHS (DOH, 2002)
Industry context § Telecoms – search for new services § Smart homes – emerging interest from some housing providers, consumer electronics and white goods companies § Digitalisation allows sensors/devices to be separated from transmission media so ‘technology silos’ can be broken § Sensors – developments in size, battery life, radio frequency
§ Within this context new telecare services are beginning to emerge …
Agenda § Background § Telecare services § Mainstreaming telecare § Conclusions
ICT enabled health care innovation § Innovation in administration and management (e. g. EPR) § Innovation in the delivery of care – Telecare is a ‘B 2 C’ service – between the patient / client and the care system – Telemedicine is a ‘B 2 B’ service – between health professionals
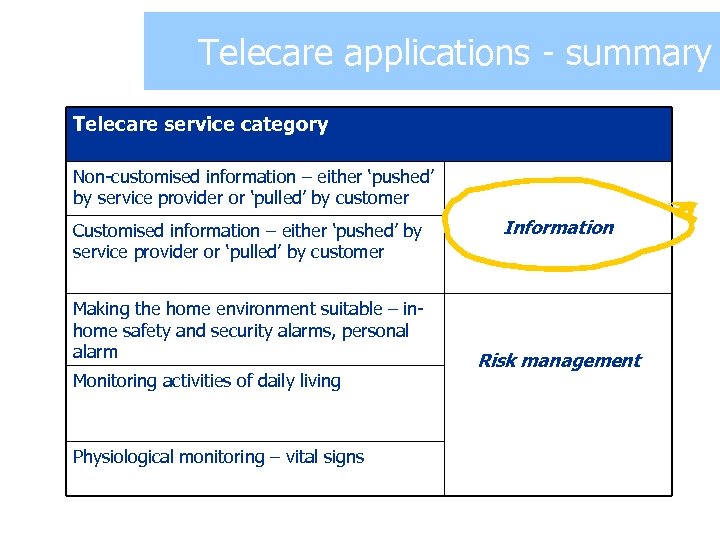
Examples summary Telecare applications - of telecare Telecare service category Non-customised information – either ‘pushed’ by service provider or ‘pulled’ by customer Customised information – either ‘pushed’ by service provider or ‘pulled’ by customer Making the home environment suitable – inhome safety and security alarms, personal alarm Monitoring activities of daily living Physiological monitoring – vital signs Information Risk management
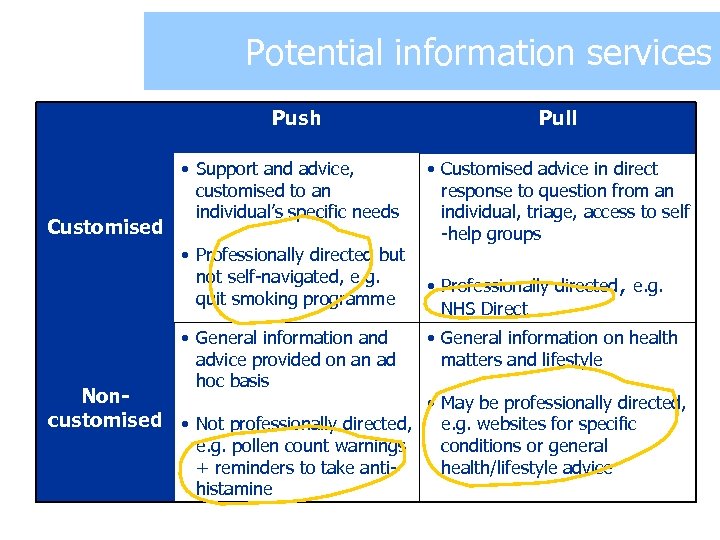
Potential information services Push Customised • Support and advice, customised to an individual’s specific needs • Professionally directed but not self-navigated, e. g. quit smoking programme • General information and advice provided on an ad hoc basis Pull • Customised advice in direct response to question from an individual, triage, access to self -help groups • Professionally directed, e. g. NHS Direct • General information on health matters and lifestyle Non • May be professionally directed, customised • Not professionally directed, e. g. websites for specific e. g. pollen count warnings + reminders to take antihistamine conditions or general health/lifestyle advice
Progress towards info. services § 40% of respondents (2001 MORI survey) identified the Internet as their preferred source of health information: § 500, 000+ hits per day on NHS Direct website; multiple delivery channels § 2%+ of the 1 bn+ www documents are health related (information on specific conditions and for informal carers)
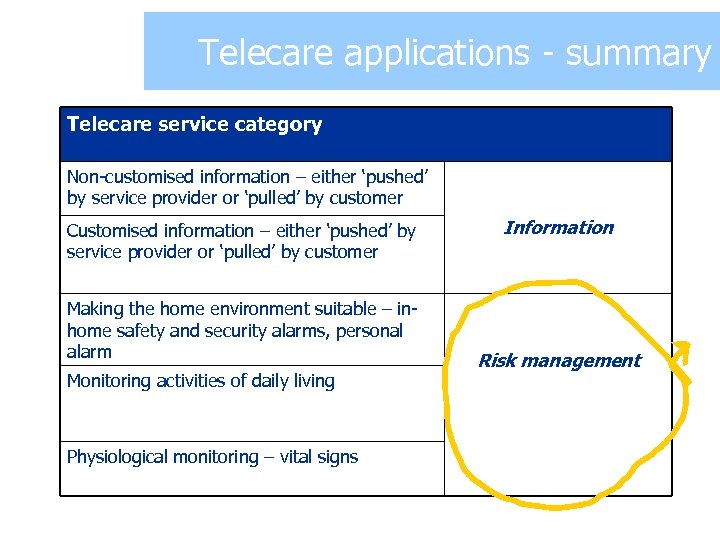
Examples summary Telecare applications - of telecare Telecare service category Non-customised information – either ‘pushed’ by service provider or ‘pulled’ by customer Customised information – either ‘pushed’ by service provider or ‘pulled’ by customer Making the home environment suitable – inhome safety and security alarms, personal alarm Monitoring activities of daily living Physiological monitoring – vital signs Information Risk management
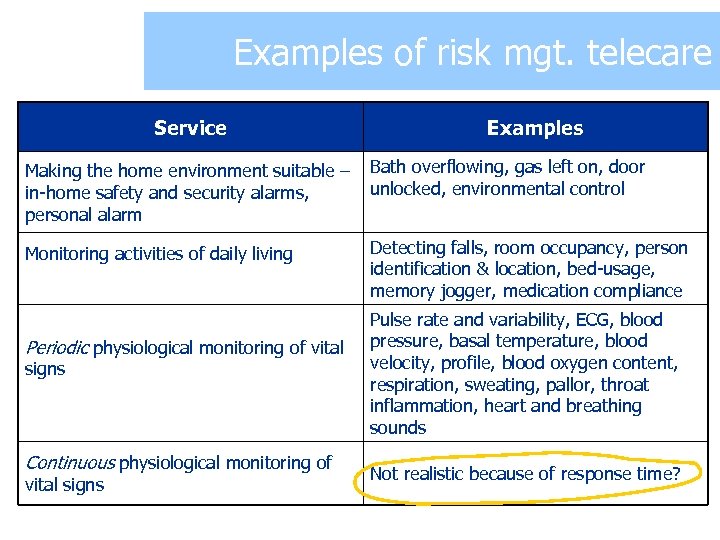
Examples of risk mgt. telecare Service Examples Making the home environment suitable – in-home safety and security alarms, personal alarm Bath overflowing, gas left on, door unlocked, environmental control Monitoring activities of daily living Detecting falls, room occupancy, person identification & location, bed-usage, memory jogger, medication compliance Periodic physiological monitoring of vital signs Continuous physiological monitoring of vital signs Pulse rate and variability, ECG, blood pressure, basal temperature, blood velocity, profile, blood oxygen content, respiration, sweating, pallor, throat inflammation, heart and breathing sounds Not realistic because of response time?
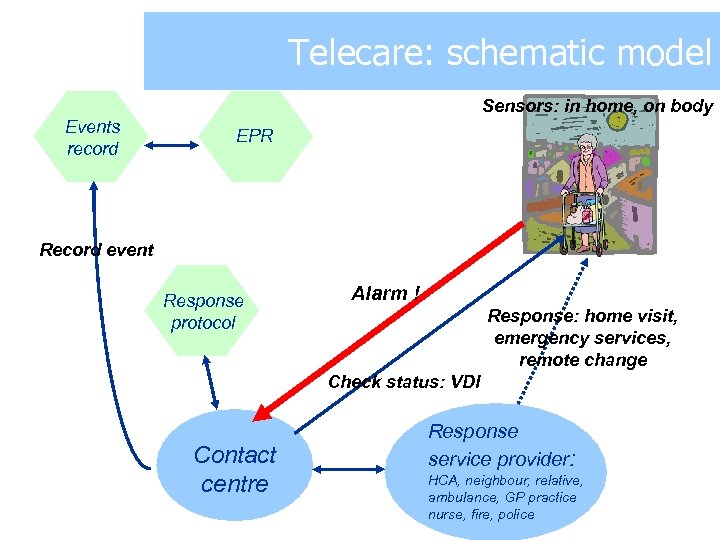
Telecare: schematic model Sensors: in home, on body Events record EPR Record event Response protocol Alarm ! Response: home visit, emergency services, remote change Check status: VDI Contact centre Response service provider: HCA, neighbour, relative, ambulance, GP practice nurse, fire, police

Telecare in the home
‘Thanks to the smarter home, a home help is required only once a year, to adjust the clock’
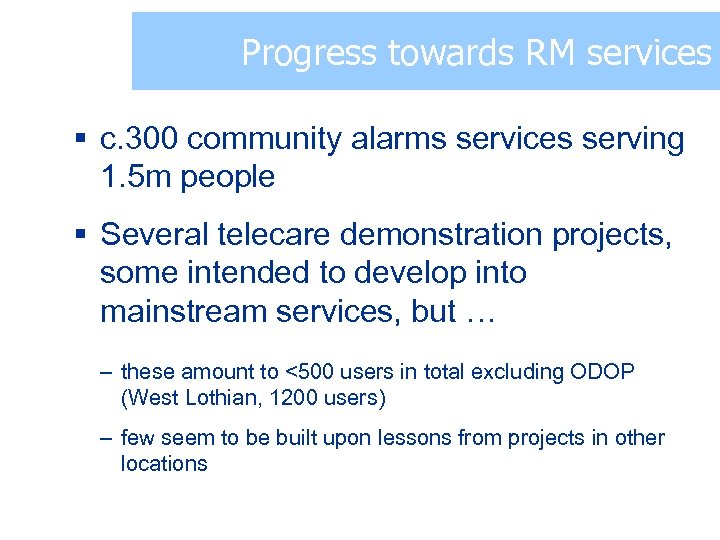
Progress towards RM services § c. 300 community alarms services serving 1. 5 m people § Several telecare demonstration projects, some intended to develop into mainstream services, but … – these amount to <500 users in total excluding ODOP (West Lothian, 1200 users) – few seem to be built upon lessons from projects in other locations
Agenda § Background § Telecare services § Mainstreaming telecare § Conclusions
Influences on implementation § Structural and operational complexity § Distribution of costs and benefits within the system § UK health system: policy innovation is faster than technology innovation, unlike many other sectors § Policy tension between modernisation (telecare) and evidence-based innovation (RCT as the ‘gold standard’)
Structural & operational complexity § Large number of stakeholders, incomplete understanding of care process by staff § Need to accommodate differing perceptions of risk and different value systems in different parts of the care system § Evolving policy priorities § (Generally much higher for telecare than telemedicine)
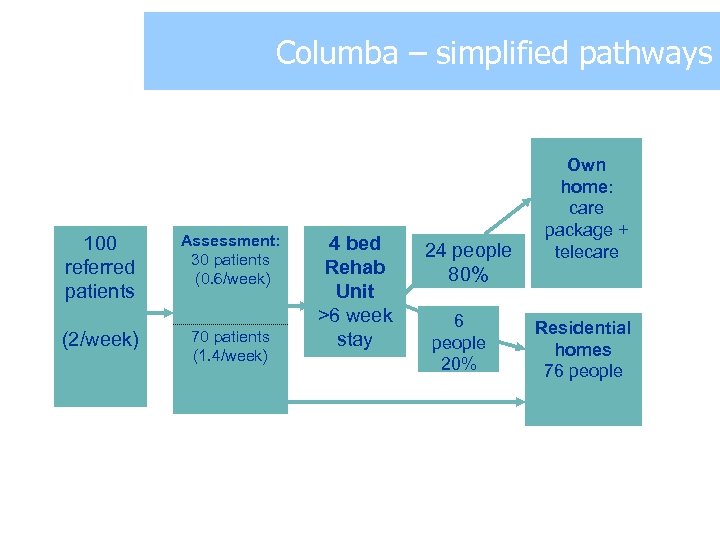
Columba – simplified pathways 100 referred patients (2/week) Assessment: 30 patients (0. 6/week) 70 patients (1. 4/week) 4 bed Rehab Unit >6 week stay 24 people 80% 6 people 20% Own home: care package + telecare Residential homes 76 people
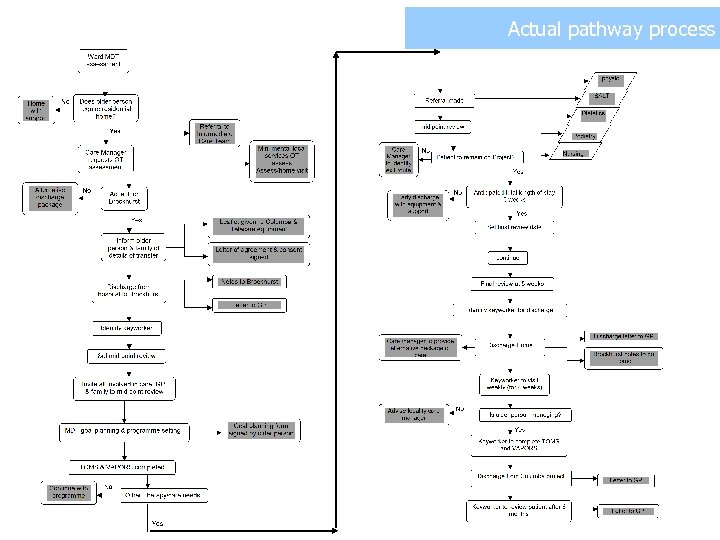
Actual pathway process
It’s not the technology!

Implications for mainstreaming § Integration with existing care services § Project design § Procurement § Supply chain § Business models
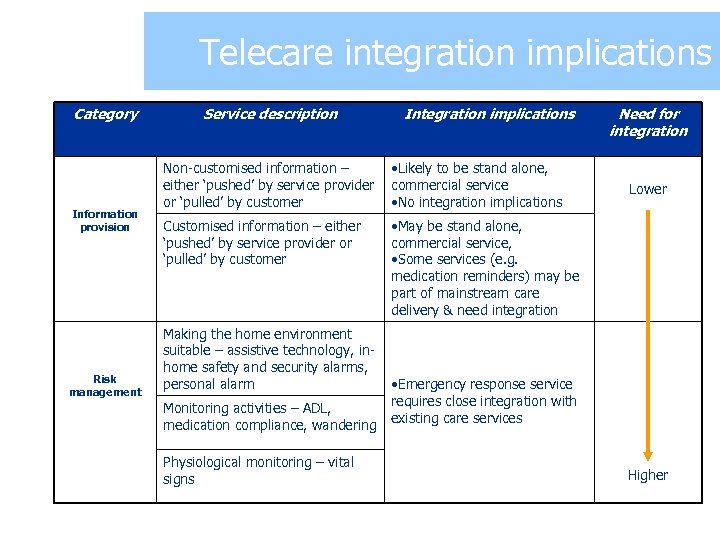
Examples of telecare Telecare integration implications Category Information provision Risk management Service description Integration implications Non-customised information – either ‘pushed’ by service provider or ‘pulled’ by customer • Likely to be stand alone, commercial service • No integration implications Customised information – either ‘pushed’ by service provider or ‘pulled’ by customer Need for integration • May be stand alone, commercial service, • Some services (e. g. medication reminders) may be part of mainstream care delivery & need integration Making the home environment suitable – assistive technology, inhome safety and security alarms, personal alarm Monitoring activities – ADL, medication compliance, wandering Physiological monitoring – vital signs Lower • Emergency response service requires close integration with existing care services Higher
Project design implications § Design must take into account requirements for future mainstream service delivery § Need for early involvement of all stakeholders in development phase, especially where integration needs are high § Need for clear ownership and leadership of the project § Telecare should become a focus for better integration of existing services and teams
Procurement implications § Start at the day to day operational level and then consider technology requirements § Mix and match approach – using beneficial technologies and systems to avoid technology silos § Care providers don’t have skills base for systems integration § Need for local single point responsibility for telecare procurement, working with systems integrators and within national framework
Supply chain implications § There are several possible ways of “cutting the stakeholders’ cake” – different supply chain models …
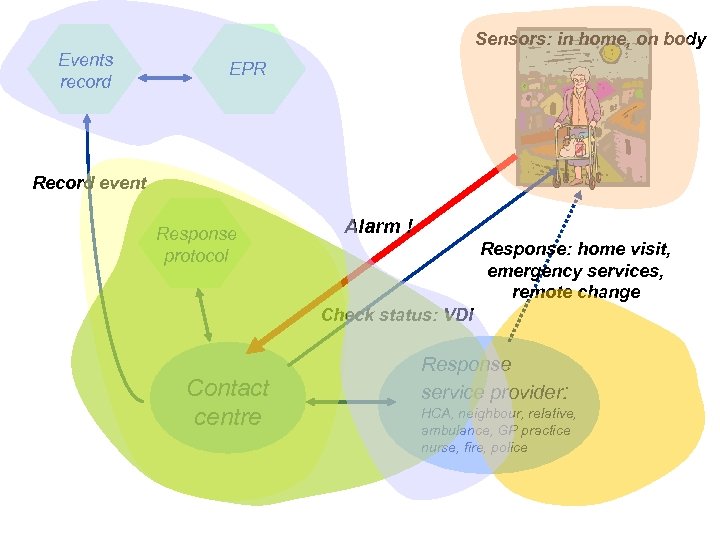
Sensors: in home, on body Events record EPR Record event Response protocol Alarm ! Response: home visit, emergency services, remote change Check status: VDI Contact centre Response service provider: HCA, neighbour, relative, ambulance, GP practice nurse, fire, police
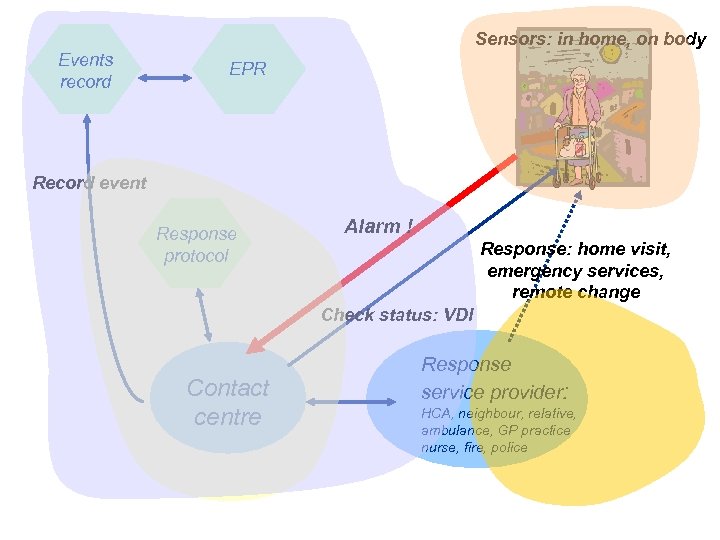
Sensors: in home, on body Events record EPR Record event Response protocol Alarm ! Response: home visit, emergency services, remote change Check status: VDI Contact centre Response service provider: HCA, neighbour, relative, ambulance, GP practice nurse, fire, police
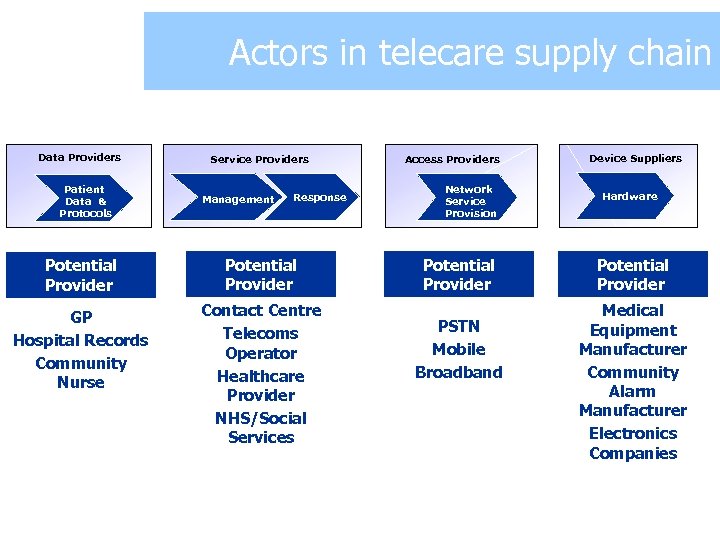
Actors in telecare supply chain Data Providers Patient Data & Protocols Service Providers Management Response Potential Provider GP Hospital Records Community Nurse Contact Centre Telecoms Operator Healthcare Provider NHS/Social Services Access Providers Network Service Provision Potential Provider PSTN Mobile Broadband Device Suppliers Hardware Potential Provider Medical Equipment Manufacturer Community Alarm Manufacturer Electronics Companies
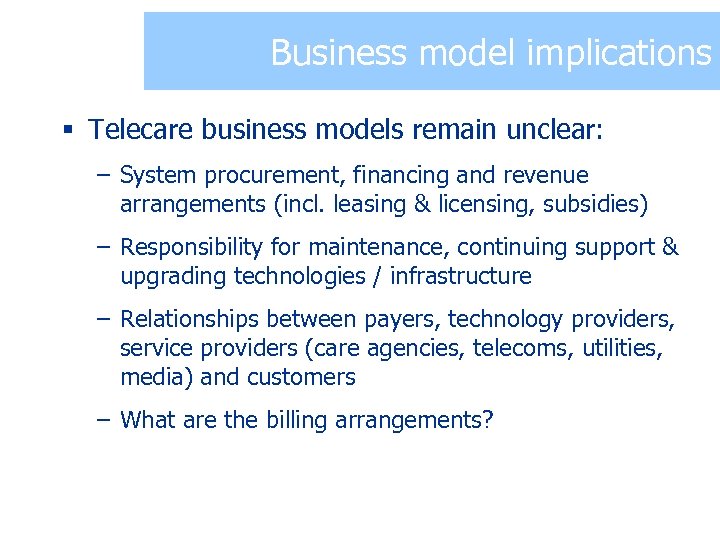
Business model implications § Telecare business models remain unclear: – System procurement, financing and revenue arrangements (incl. leasing & licensing, subsidies) – Responsibility for maintenance, continuing support & upgrading technologies / infrastructure – Relationships between payers, technology providers, service providers (care agencies, telecoms, utilities, media) and customers – What are the billing arrangements?
Agenda § Background § Telecare services § Implications for mainstreaming telecare § Conclusions
Conclusions § The future evolution of the care system needs to start from existing service delivery and a recognition of what telecare can achieve § The purpose and fit of telecare services in the wider care system should drive its introduction – not the technology § This will require a better understanding of telecare’s impact at the system-wide level and new approaches to evaluation

Thank you for listening! For further information: T 020 -7594 5936 F 020 -7823 7685 E j. barlow@imperial. ac. uk
c549ffbe7c800731e9255e61e0e87ff7.ppt