508f3c3140d5f77e3702ec0d59c65a21.ppt
- Количество слайдов: 33
Lumbar Spinal Stenosis Decompression Prof. Dr. R. Kemal Koç Department of Neurosurgery Erciyes University, Faculty of Medicine Kayseri, Turkey
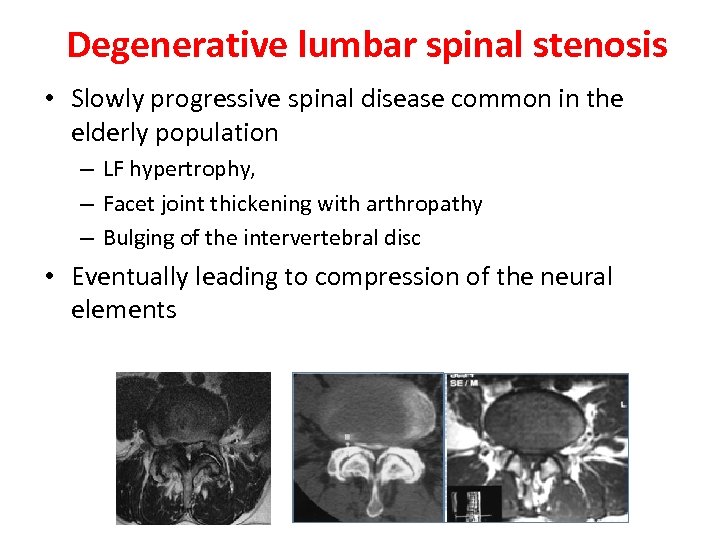
Degenerative lumbar spinal stenosis • Slowly progressive spinal disease common in the elderly population – LF hypertrophy, – Facet joint thickening with arthropathy – Bulging of the intervertebral disc • Eventually leading to compression of the neural elements
Indications for surgery • Neurogenic claudication or radiculopathy • Failure of conservative treatment – nonsteroidal antiinflammatory drugs – corticosteroids – physiotherapy • Patient selection criteria • CT or MR imaging evidence of lumbar degenerative stenosis
Surgical technique for DLS • The chosen technique inherently depends on the stability of the DLS. • The following preoperative parameters are predictors of stability in DLS – the absence of low-back pain, – no facet joint effusions on MR, – restabilization signs (disc height loss, osteophyte formation, vertebral endplate sclerosis, and ligament ossification), – no disc angle change or less than 3 mm of translation on dynamic radiographs. • Decompression alone is sufficient in the stable cases Simmonds AM. Defining the inherent stability of degenerative spondylolisthesis: a systematic review. J Neurosurg Spine 23: 178– 189, 2015
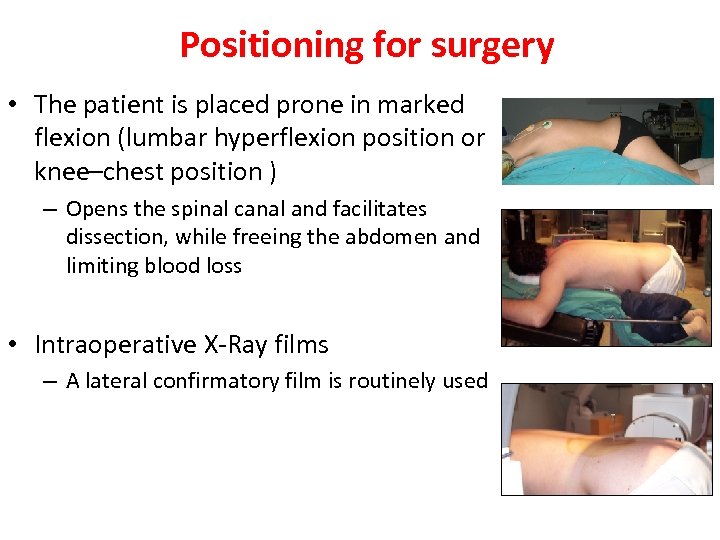
Positioning for surgery • The patient is placed prone in marked flexion (lumbar hyperflexion position or knee–chest position ) – Opens the spinal canal and facilitates dissection, while freeing the abdomen and limiting blood loss • Intraoperative X-Ray films – A lateral confirmatory film is routinely used
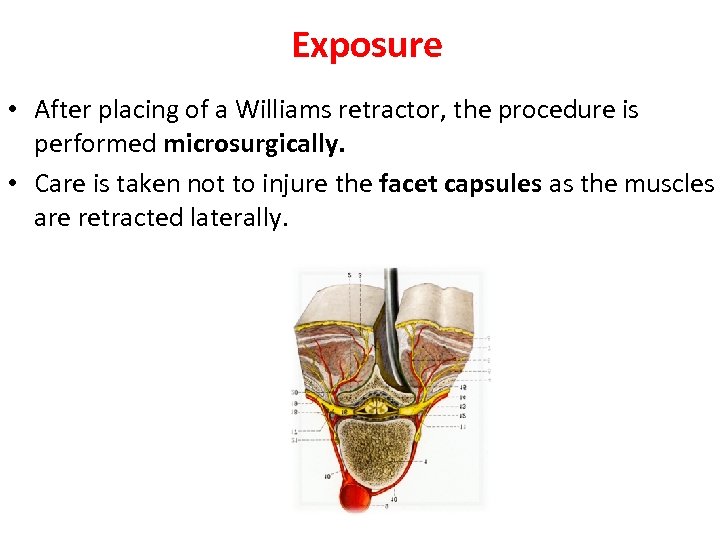
Exposure • After placing of a Williams retractor, the procedure is performed microsurgically. • Care is taken not to injure the facet capsules as the muscles are retracted laterally.
Basic principles of decompression technique • The intraoperative complication of an incidental durotomy can be markedly decreased – Thinning of the lamina and hypertrophic bone with a high-speed burr – The use of a blunt dissector or nerve hook to release adhesions – A small punch used to remove the last little pieces of bone – Performing the decompression in caudal to cephalad direction – The usage of microscope and microsurgery tool.
Basic principles of decompression technique • Spinal stability should be protected during decompression – More than 50% of the facet joints should not be removed. – Nerve root can be decompressed by removal of the medial 1/3 of superior articular process. – Pars interarticularis should be protected at least 5 mm wide. • Dissector must be easily moved throughout the course of decompressed nerve root after decompression
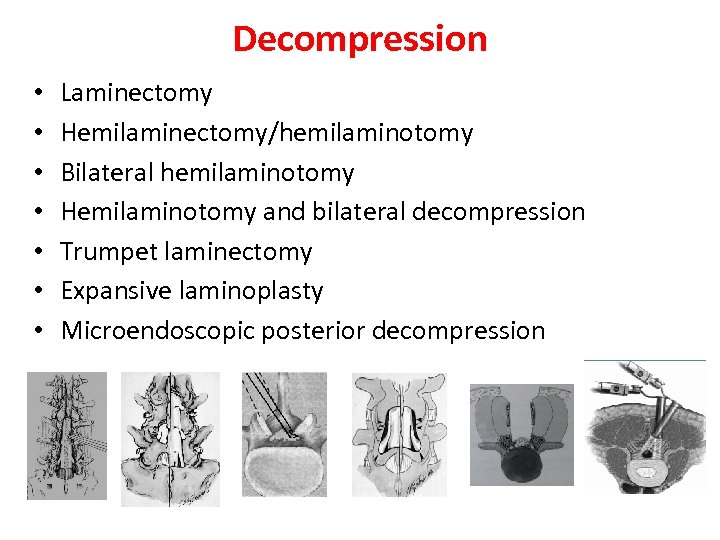
Decompression • • Laminectomy Hemilaminectomy/hemilaminotomy Bilateral hemilaminotomy Hemilaminotomy and bilateral decompression Trumpet laminectomy Expansive laminoplasty Microendoscopic posterior decompression
Laminectomy • Traditional surgery is wide laminectomy, which allows decompression of the neural structures by unroofing the spinal canal. • The success rate of this procedure varies from 62 to 70%, • Frequent surgical failures are generally related to postoperative iatrogenic spinal instability. Airaksinen O, Spine 22: 2278– 2282, 1997 Javid MJ, J Neurosurg 89: 1– 7, 1998 Silvers HR, J Neurosurg 78: 695– 701, 1993 Turner JA, Spine 17: 1– 8, 1992
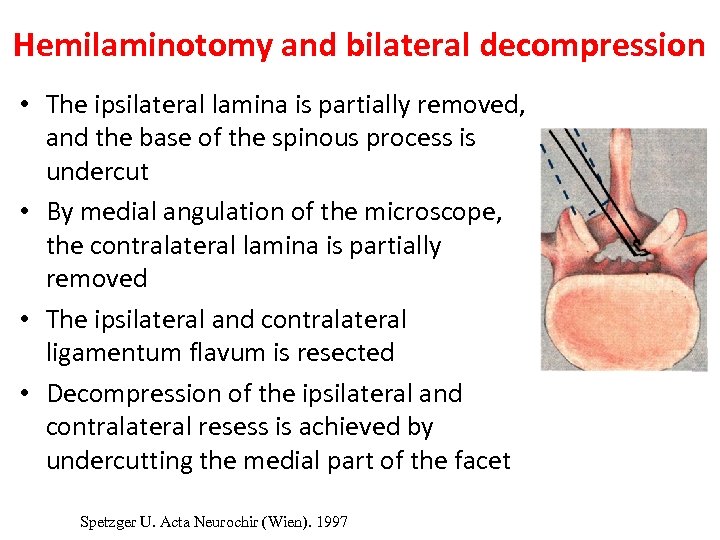
Hemilaminotomy and bilateral decompression • The ipsilateral lamina is partially removed, and the base of the spinous process is undercut • By medial angulation of the microscope, the contralateral lamina is partially removed • The ipsilateral and contralateral ligamentum flavum is resected • Decompression of the ipsilateral and contralateral resess is achieved by undercutting the medial part of the facet Spetzger U. Acta Neurochir (Wien). 1997
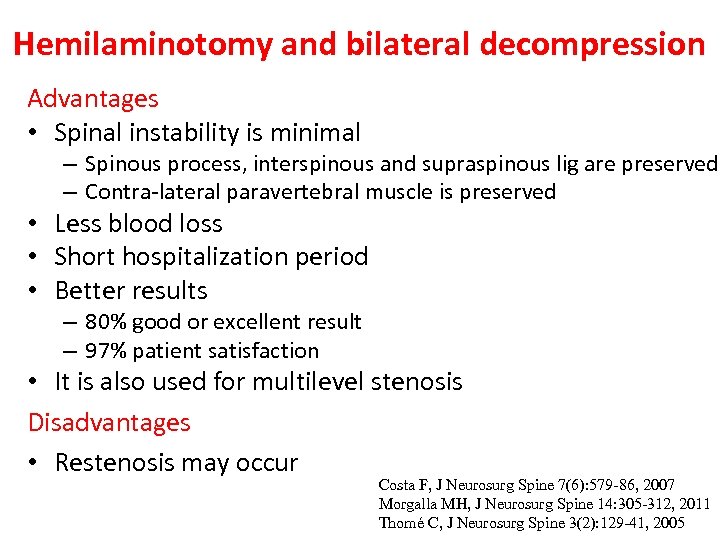
Hemilaminotomy and bilateral decompression Advantages • Spinal instability is minimal – Spinous process, interspinous and supraspinous lig are preserved – Contra-lateral paravertebral muscle is preserved • Less blood loss • Short hospitalization period • Better results – 80% good or excellent result – 97% patient satisfaction • It is also used for multilevel stenosis Disadvantages • Restenosis may occur Costa F, J Neurosurg Spine 7(6): 579 -86, 2007 Morgalla MH, J Neurosurg Spine 14: 305 -312, 2011 Thomé C, J Neurosurg Spine 3(2): 129 -41, 2005
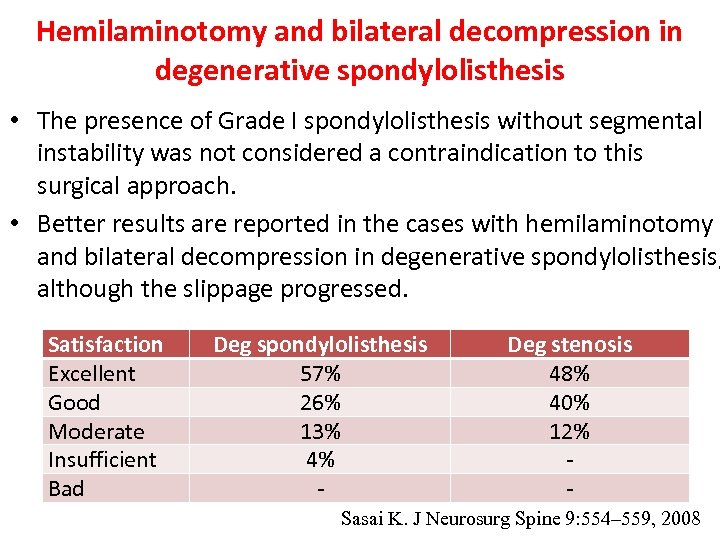
Hemilaminotomy and bilateral decompression in degenerative spondylolisthesis • The presence of Grade I spondylolisthesis without segmental instability was not considered a contraindication to this surgical approach. • Better results are reported in the cases with hemilaminotomy and bilateral decompression in degenerative spondylolisthesis, although the slippage progressed. Satisfaction Excellent Good Moderate Insufficient Bad Deg spondylolisthesis 57% 26% 13% 4% - Deg stenosis 48% 40% 12% - Sasai K. J Neurosurg Spine 9: 554– 559, 2008
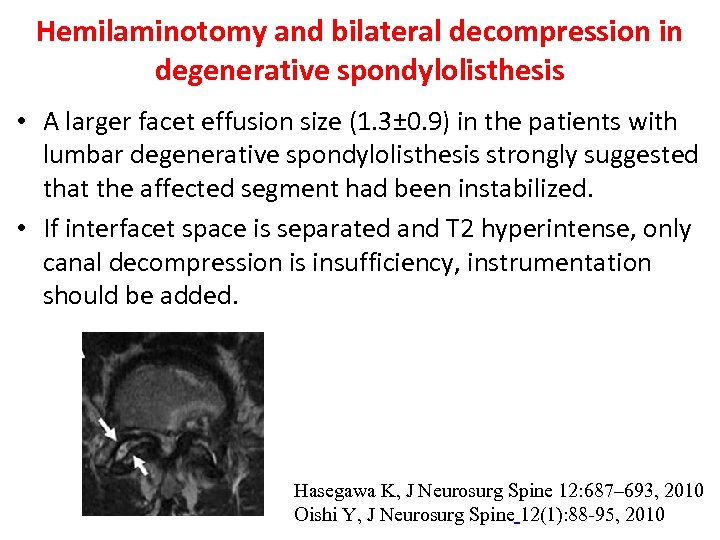
Hemilaminotomy and bilateral decompression in degenerative spondylolisthesis • A larger facet effusion size (1. 3± 0. 9) in the patients with lumbar degenerative spondylolisthesis strongly suggested that the affected segment had been instabilized. • If interfacet space is separated and T 2 hyperintense, only canal decompression is insufficiency, instrumentation should be added. Hasegawa K, J Neurosurg Spine 12: 687– 693, 2010 Oishi Y, J Neurosurg Spine 12(1): 88 -95, 2010
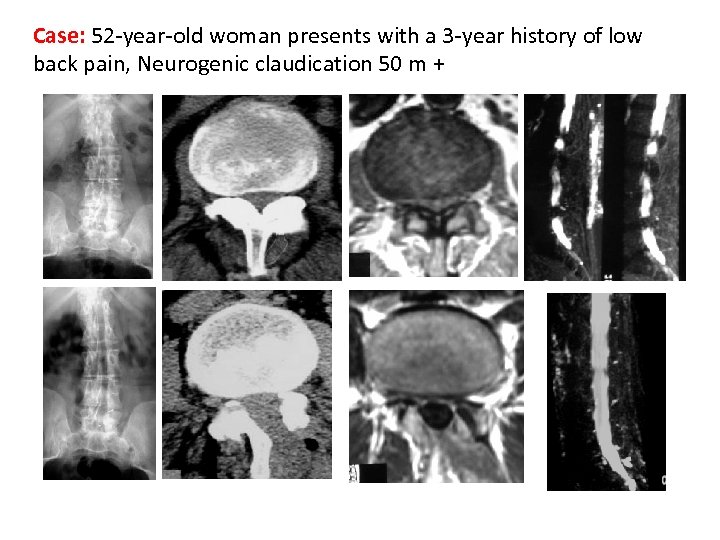
Case: 52 -year-old woman presents with a 3 -year history of low back pain, Neurogenic claudication 50 m +
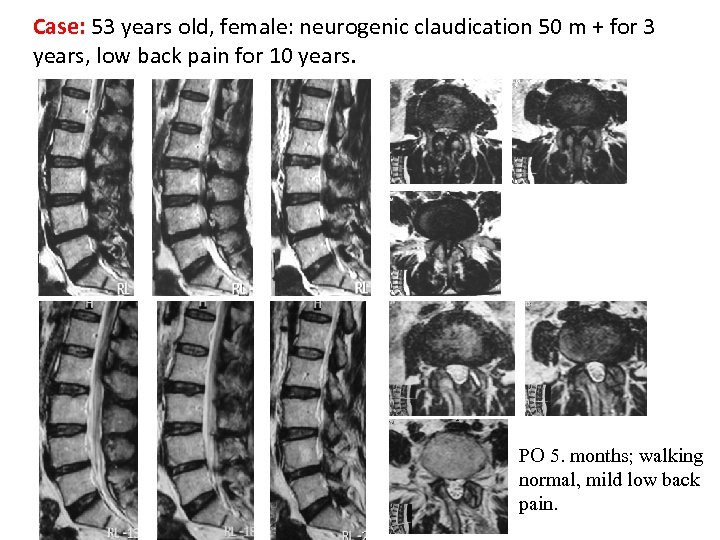
Case: 53 years old, female: neurogenic claudication 50 m + for 3 years, low back pain for 10 years. PO 5. months; walking normal, mild low back pain.
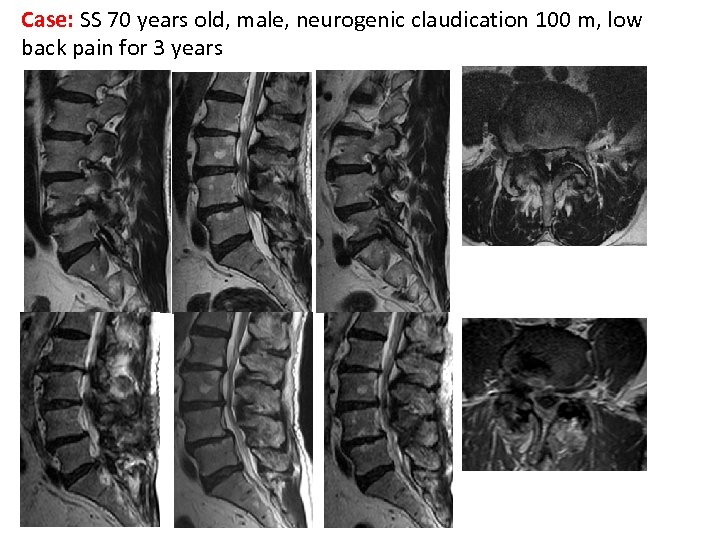
Case: SS 70 years old, male, neurogenic claudication 100 m, low back pain for 3 years
Recurrence of stenosis after surgery • • No regrowth Mild regrowth Moderate regrowth Marked regrowth 12% 48% 28% 12% • Of the patients with marked regrowth, 60% had a unsatisfactory clinical result Postacchini F, J Bone Joint Surg, 1992
Indications of instrumentation • • • Instability Progressive deformity (scoliosis, kyphosis) Resection of more than 50% of facet Extensive decompression with an underlying deformity Significant loss of lordosis Stenosis develops at a previously decompressed segment
Complications • • • Dural tear Cauda equina syndrome Nerve root injury Epidural hematoma Infection Delayed complications • Segmental instability • Epidural scar formation
CONCLUSION • Microsurgical bilateral decompression via unilateral approach is a useful and safe operative procedure for LSS patients. • Sufficient clinical results is obtained even in the patients with multiple-level LSS, if the patient is correctly selected and the microsurgical decompression surgery is carefully performed.

THANK YOU
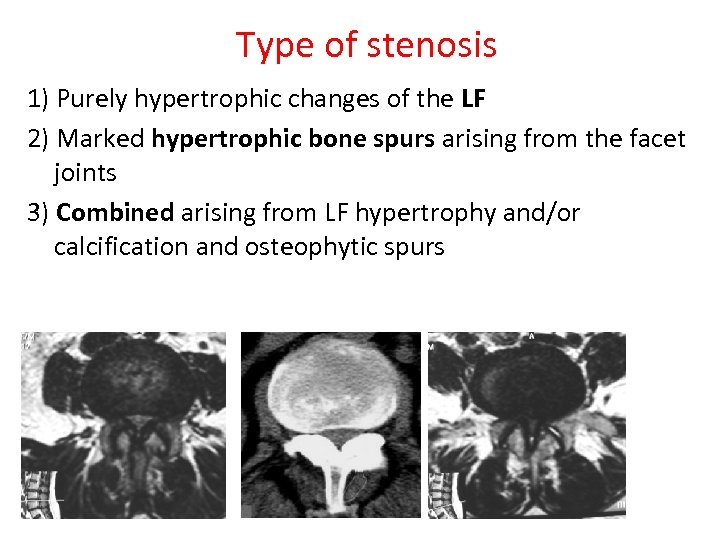
Type of stenosis 1) Purely hypertrophic changes of the LF 2) Marked hypertrophic bone spurs arising from the facet joints 3) Combined arising from LF hypertrophy and/or calcification and osteophytic spurs
Clinical presentation • Bilateral neurogenic claudication • Intermittent pain radiating to the thigh and/or leg, which is – aggravated by prolonged standing or lumbar extension – relieved by sitting or flexing the lumbar spine • Radicular deficits are sometimes present
Prognosis • Many variables (due to type of stenosis, number of stenosis, applied surgical method, etc. ). • Overall, good or excellent result is 82%. • Good or excellent result is 96% in non-related symptoms with posture. • Low back pain is more likely to continue after the decompression. Granz JC. J Neurosurg 72: 71 -74, 1990
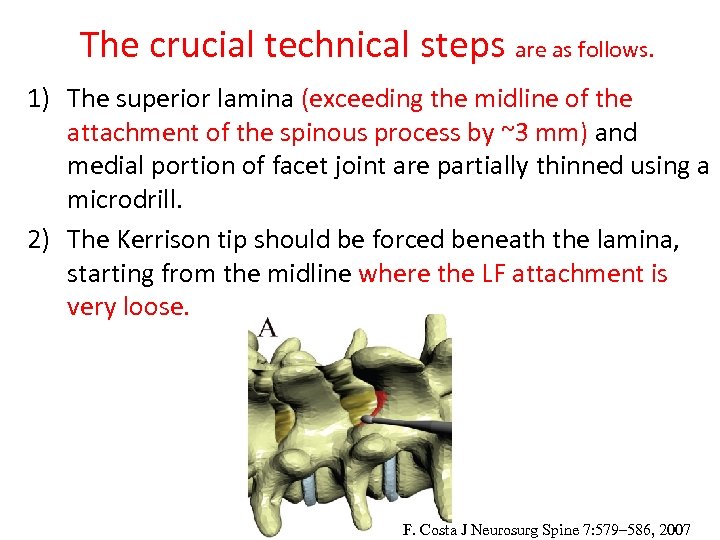
The crucial technical steps are as follows. 1) The superior lamina (exceeding the midline of the attachment of the spinous process by ~3 mm) and medial portion of facet joint are partially thinned using a microdrill. 2) The Kerrison tip should be forced beneath the lamina, starting from the midline where the LF attachment is very loose. F. Costa J Neurosurg Spine 7: 579– 586, 2007
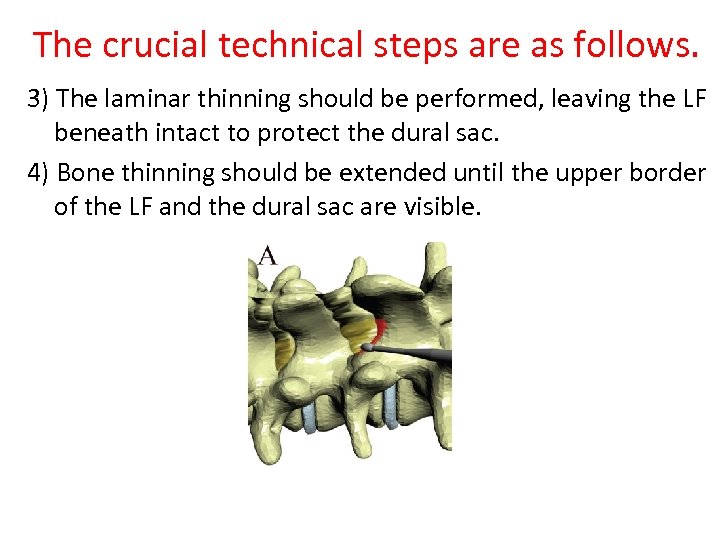
The crucial technical steps are as follows. 3) The laminar thinning should be performed, leaving the LF beneath intact to protect the dural sac. 4) Bone thinning should be extended until the upper border of the LF and the dural sac are visible.
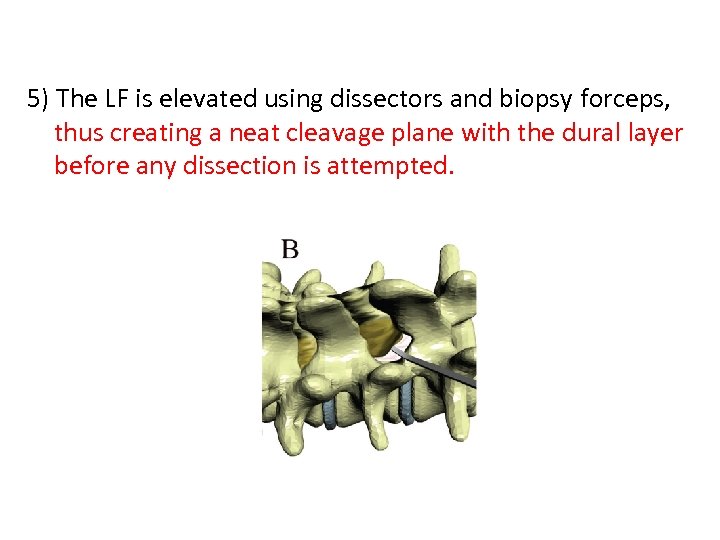
5) The LF is elevated using dissectors and biopsy forceps, thus creating a neat cleavage plane with the dural layer before any dissection is attempted.
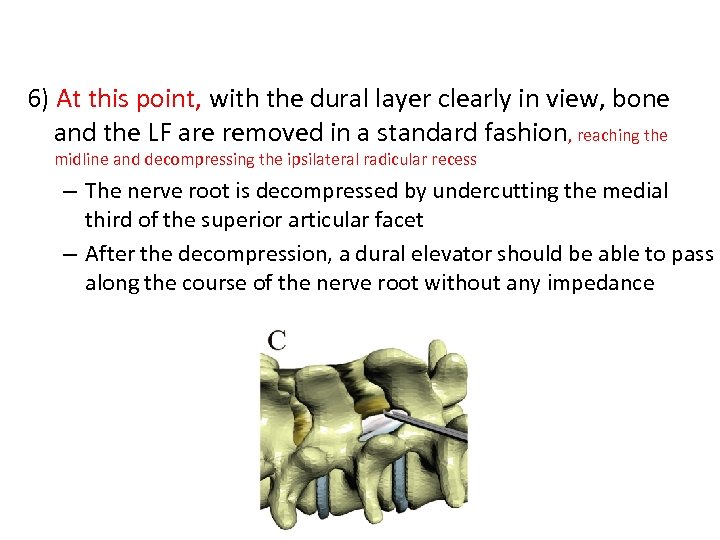
6) At this point, with the dural layer clearly in view, bone and the LF are removed in a standard fashion, reaching the midline and decompressing the ipsilateral radicular recess – The nerve root is decompressed by undercutting the medial third of the superior articular facet – After the decompression, a dural elevator should be able to pass along the course of the nerve root without any impedance
7) Finally, the operating table is elevated, and the operative microscope is gradually tilted toward the opposite side at the proper angle, thus allowing as much of the contralateral LF as possible to be removed using the small Kerrison rongeurs.
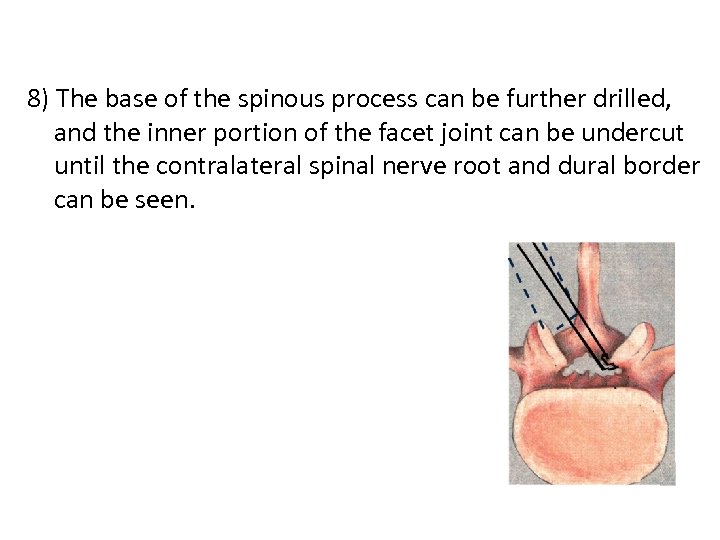
8) The base of the spinous process can be further drilled, and the inner portion of the facet joint can be undercut until the contralateral spinal nerve root and dural border can be seen.
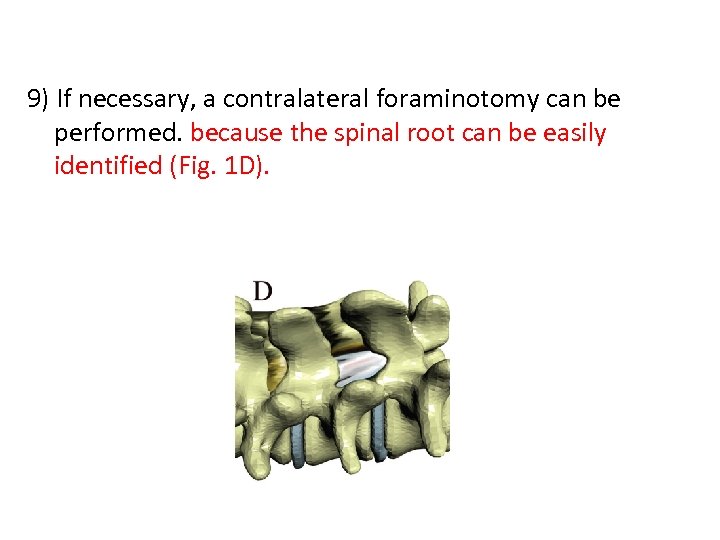
9) If necessary, a contralateral foraminotomy can be performed. because the spinal root can be easily identified (Fig. 1 D).
10) Obviously, in cases of tight adhesions, some small pieces of the LF can be left in place.
508f3c3140d5f77e3702ec0d59c65a21.ppt