e1ecda9301e3f7bce9945d377b74ba29.ppt
- Количество слайдов: 60
 Lower Urinary Tract & Sexual Function Following Pelvic Surgery “The Vulnerable Pelvis” Patricia A. Wallace M. D. Assistant Professor, UCIMC Female Pelvic Medicine & Reconstructive Surgery The Incontinence & Support Institute
Lower Urinary Tract & Sexual Function Following Pelvic Surgery “The Vulnerable Pelvis” Patricia A. Wallace M. D. Assistant Professor, UCIMC Female Pelvic Medicine & Reconstructive Surgery The Incontinence & Support Institute
 Objectives u Definitions: – Lower urinary tract symptoms (LUTS) – Female sexual dysfunction u Prevalence of LUTS & sexual dysfunction in general population u Pelvic anatomy & vulnerable areas
Objectives u Definitions: – Lower urinary tract symptoms (LUTS) – Female sexual dysfunction u Prevalence of LUTS & sexual dysfunction in general population u Pelvic anatomy & vulnerable areas
 Objectives u Effects of pelvic surgery – General gyn surgery – Incontinence & prolapse surgery – Surgery for gyn malignancy – Surgery for colorectal disorders u Multidisciplinary & recovery approach to surgery
Objectives u Effects of pelvic surgery – General gyn surgery – Incontinence & prolapse surgery – Surgery for gyn malignancy – Surgery for colorectal disorders u Multidisciplinary & recovery approach to surgery
 Lower Urinary Tract Symptoms (LUTS) Symptom-subjective indicator of a change in condition as perceived by patient, caregiver, or partner and may lead to the person seeking health care u Storage symptoms u – Urgency, frequency, nocturia, incontinence, abnormal bladder sensation u Voiding symptoms – Slow stream, hesitancy, split stream, intermittent stream u Post micturition symptoms – Postvoid fullness or dribbling
Lower Urinary Tract Symptoms (LUTS) Symptom-subjective indicator of a change in condition as perceived by patient, caregiver, or partner and may lead to the person seeking health care u Storage symptoms u – Urgency, frequency, nocturia, incontinence, abnormal bladder sensation u Voiding symptoms – Slow stream, hesitancy, split stream, intermittent stream u Post micturition symptoms – Postvoid fullness or dribbling
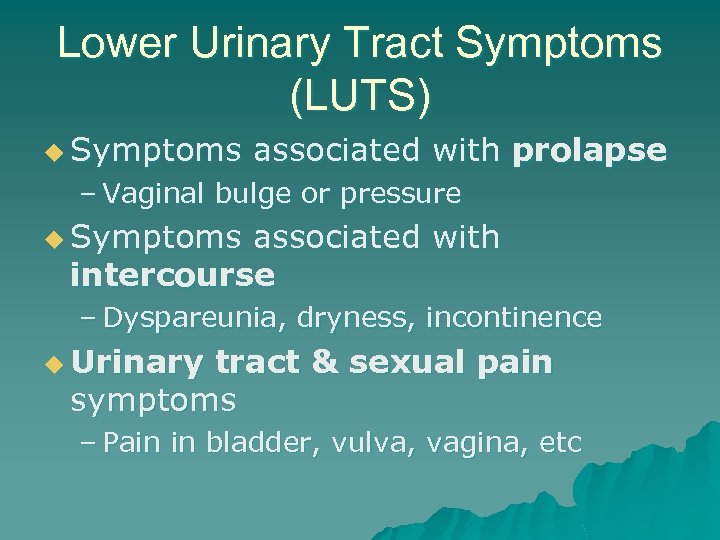 Lower Urinary Tract Symptoms (LUTS) u Symptoms associated with prolapse – Vaginal bulge or pressure u Symptoms associated with intercourse – Dyspareunia, dryness, incontinence u Urinary tract & sexual pain symptoms – Pain in bladder, vulva, vagina, etc
Lower Urinary Tract Symptoms (LUTS) u Symptoms associated with prolapse – Vaginal bulge or pressure u Symptoms associated with intercourse – Dyspareunia, dryness, incontinence u Urinary tract & sexual pain symptoms – Pain in bladder, vulva, vagina, etc
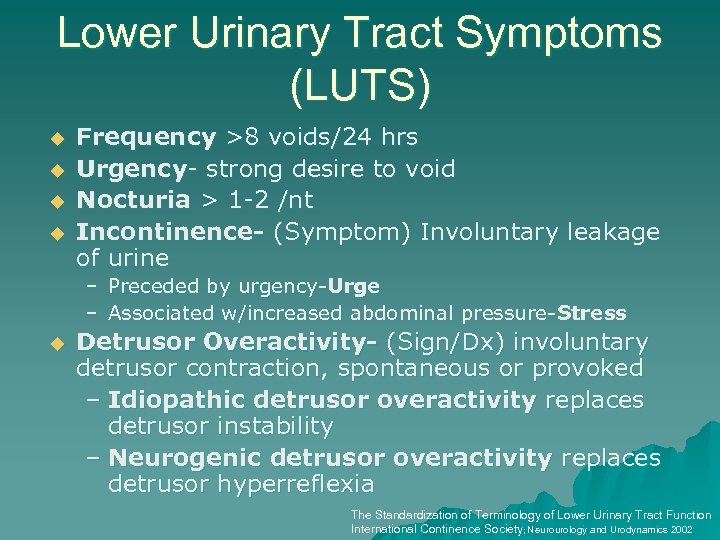 Lower Urinary Tract Symptoms (LUTS) u u Frequency >8 voids/24 hrs Urgency- strong desire to void Nocturia > 1 -2 /nt Incontinence- (Symptom) Involuntary leakage of urine – Preceded by urgency-Urge – Associated w/increased abdominal pressure-Stress u Detrusor Overactivity- (Sign/Dx) involuntary detrusor contraction, spontaneous or provoked – Idiopathic detrusor overactivity replaces detrusor instability – Neurogenic detrusor overactivity replaces detrusor hyperreflexia The Standardization of Terminology of Lower Urinary Tract Function International Continence Society; Neurourology and Urodynamics 2002
Lower Urinary Tract Symptoms (LUTS) u u Frequency >8 voids/24 hrs Urgency- strong desire to void Nocturia > 1 -2 /nt Incontinence- (Symptom) Involuntary leakage of urine – Preceded by urgency-Urge – Associated w/increased abdominal pressure-Stress u Detrusor Overactivity- (Sign/Dx) involuntary detrusor contraction, spontaneous or provoked – Idiopathic detrusor overactivity replaces detrusor instability – Neurogenic detrusor overactivity replaces detrusor hyperreflexia The Standardization of Terminology of Lower Urinary Tract Function International Continence Society; Neurourology and Urodynamics 2002
 Overactive Bladder u. A collection of symptoms consisting of urgency, frequency, nocturia, with and without incontinence u No identifiable pathologic or metabolic condition to explain symptoms
Overactive Bladder u. A collection of symptoms consisting of urgency, frequency, nocturia, with and without incontinence u No identifiable pathologic or metabolic condition to explain symptoms
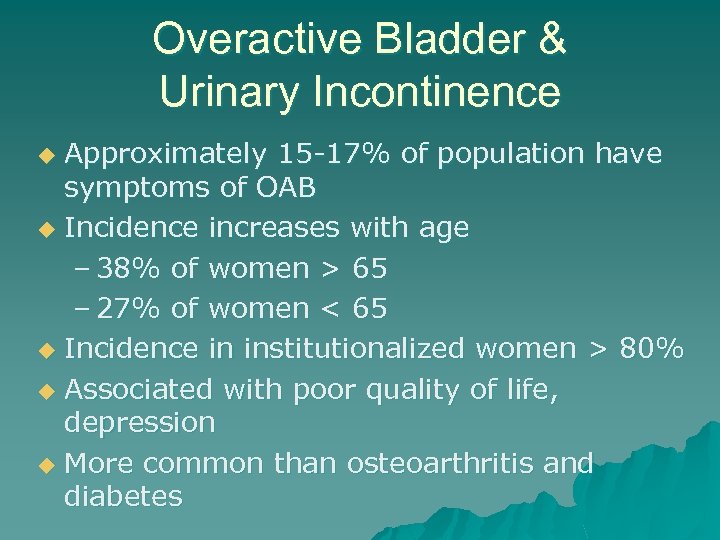 Overactive Bladder & Urinary Incontinence Approximately 15 -17% of population have symptoms of OAB u Incidence increases with age – 38% of women > 65 – 27% of women < 65 u Incidence in institutionalized women > 80% u Associated with poor quality of life, depression u More common than osteoarthritis and diabetes u
Overactive Bladder & Urinary Incontinence Approximately 15 -17% of population have symptoms of OAB u Incidence increases with age – 38% of women > 65 – 27% of women < 65 u Incidence in institutionalized women > 80% u Associated with poor quality of life, depression u More common than osteoarthritis and diabetes u
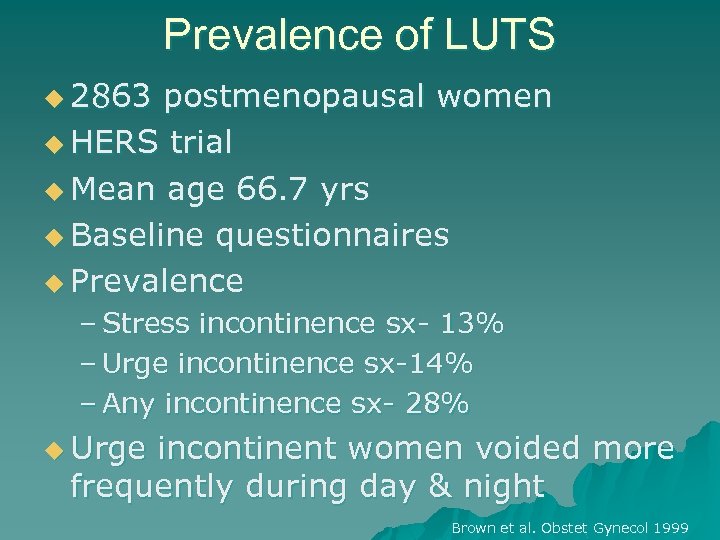 Prevalence of LUTS u 2863 postmenopausal women u HERS trial u Mean age 66. 7 yrs u Baseline questionnaires u Prevalence – Stress incontinence sx- 13% – Urge incontinence sx-14% – Any incontinence sx- 28% u Urge incontinent women voided more frequently during day & night Brown et al. Obstet Gynecol 1999
Prevalence of LUTS u 2863 postmenopausal women u HERS trial u Mean age 66. 7 yrs u Baseline questionnaires u Prevalence – Stress incontinence sx- 13% – Urge incontinence sx-14% – Any incontinence sx- 28% u Urge incontinent women voided more frequently during day & night Brown et al. Obstet Gynecol 1999
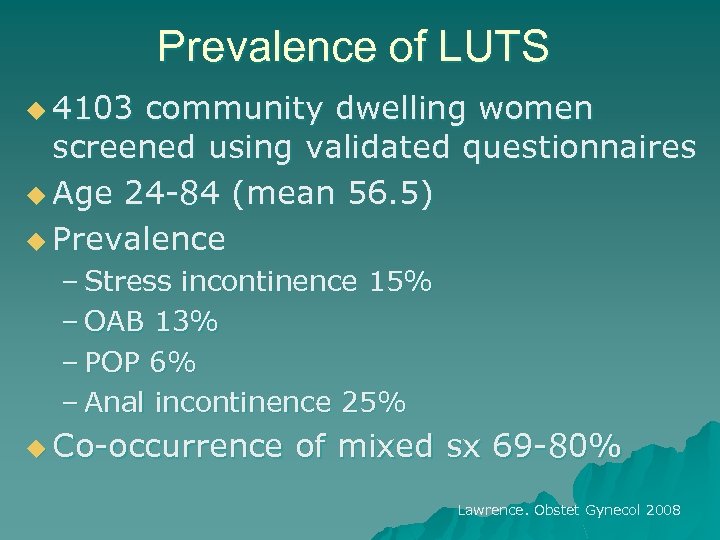 Prevalence of LUTS u 4103 community dwelling women screened using validated questionnaires u Age 24 -84 (mean 56. 5) u Prevalence – Stress incontinence 15% – OAB 13% – POP 6% – Anal incontinence 25% u Co-occurrence of mixed sx 69 -80% Lawrence. Obstet Gynecol 2008
Prevalence of LUTS u 4103 community dwelling women screened using validated questionnaires u Age 24 -84 (mean 56. 5) u Prevalence – Stress incontinence 15% – OAB 13% – POP 6% – Anal incontinence 25% u Co-occurrence of mixed sx 69 -80% Lawrence. Obstet Gynecol 2008
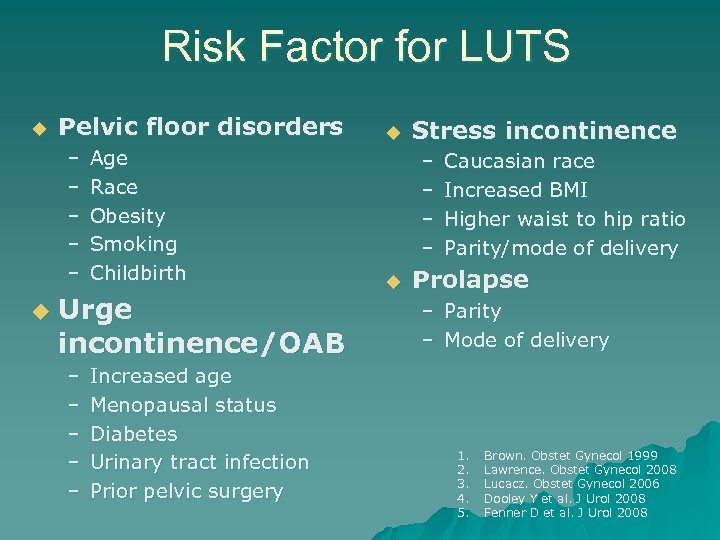 Risk Factor for LUTS u Pelvic floor disorders – – – u Age Race Obesity Smoking Childbirth Urge incontinence/OAB – – – Increased age Menopausal status Diabetes Urinary tract infection Prior pelvic surgery u Stress incontinence – – u Caucasian race Increased BMI Higher waist to hip ratio Parity/mode of delivery Prolapse – Parity – Mode of delivery 1. 2. 3. 4. 5. Brown. Obstet Gynecol 1999 Lawrence. Obstet Gynecol 2008 Lucacz. Obstet Gynecol 2006 Dooley Y et al. J Urol 2008 Fenner D et al. J Urol 2008
Risk Factor for LUTS u Pelvic floor disorders – – – u Age Race Obesity Smoking Childbirth Urge incontinence/OAB – – – Increased age Menopausal status Diabetes Urinary tract infection Prior pelvic surgery u Stress incontinence – – u Caucasian race Increased BMI Higher waist to hip ratio Parity/mode of delivery Prolapse – Parity – Mode of delivery 1. 2. 3. 4. 5. Brown. Obstet Gynecol 1999 Lawrence. Obstet Gynecol 2008 Lucacz. Obstet Gynecol 2006 Dooley Y et al. J Urol 2008 Fenner D et al. J Urol 2008
 Santa makes a pit stop!
Santa makes a pit stop!
 Sexual Function vs Dysfunction u Highly variable u Life cycle & age u Sexual response cycle in women u Personal distress caused by symptoms related to sexual response cycle
Sexual Function vs Dysfunction u Highly variable u Life cycle & age u Sexual response cycle in women u Personal distress caused by symptoms related to sexual response cycle
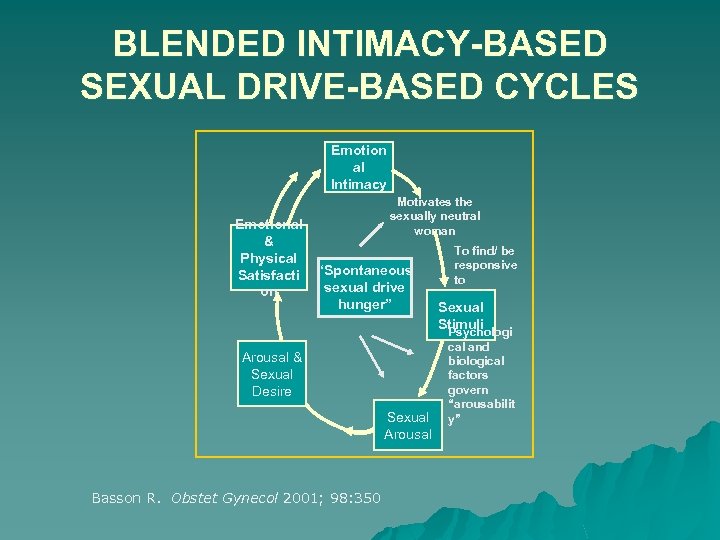 BLENDED INTIMACY-BASED SEXUAL DRIVE-BASED CYCLES Emotion al Intimacy Emotional & Physical Satisfacti on Motivates the sexually neutral woman “Spontaneous sexual drive hunger” Arousal & Sexual Desire Sexual Arousal Basson R. Obstet Gynecol 2001; 98: 350 To find/ be responsive to Sexual Stimuli Psychologi cal and biological factors govern “arousabilit y”
BLENDED INTIMACY-BASED SEXUAL DRIVE-BASED CYCLES Emotion al Intimacy Emotional & Physical Satisfacti on Motivates the sexually neutral woman “Spontaneous sexual drive hunger” Arousal & Sexual Desire Sexual Arousal Basson R. Obstet Gynecol 2001; 98: 350 To find/ be responsive to Sexual Stimuli Psychologi cal and biological factors govern “arousabilit y”
 Prevalence of Sexual Dysfunction u Affects 25%-43% of women 1 u Multidimensional and multicausal combining biological, psychological, and interpersonal factors 1, 2 u Physically and emotionally distressing u Increases with age 1 1. Bancroft j. Arch Sex Behav. 2003; In Press 2. Laumann EO, et al. JAMA. 1999; 281: 537
Prevalence of Sexual Dysfunction u Affects 25%-43% of women 1 u Multidimensional and multicausal combining biological, psychological, and interpersonal factors 1, 2 u Physically and emotionally distressing u Increases with age 1 1. Bancroft j. Arch Sex Behav. 2003; In Press 2. Laumann EO, et al. JAMA. 1999; 281: 537
 Risk Factors for Sexual Dysfunction Aging and menopause u Chronic medical conditions: DM, HTN, Depression, CAD u Pelvic surgery* u Neurological disorders: MS, epilepsy, paralysis u Endocrine disorders: Addisons disease, hypothyroidism u Medications: SSRIs, antihypertensives, steroids, statins, other psychotropics u Infection: STDs or condyloma u
Risk Factors for Sexual Dysfunction Aging and menopause u Chronic medical conditions: DM, HTN, Depression, CAD u Pelvic surgery* u Neurological disorders: MS, epilepsy, paralysis u Endocrine disorders: Addisons disease, hypothyroidism u Medications: SSRIs, antihypertensives, steroids, statins, other psychotropics u Infection: STDs or condyloma u
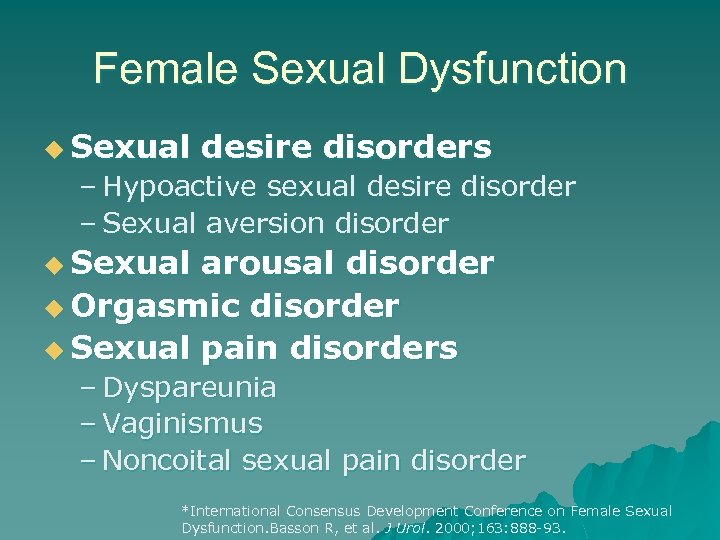 Female Sexual Dysfunction u Sexual desire disorders – Hypoactive sexual desire disorder – Sexual aversion disorder u Sexual arousal disorder u Orgasmic disorder u Sexual pain disorders – Dyspareunia – Vaginismus – Noncoital sexual pain disorder *International Consensus Development Conference on Female Sexual Dysfunction. Basson R, et al. J Urol. 2000; 163: 888 -93.
Female Sexual Dysfunction u Sexual desire disorders – Hypoactive sexual desire disorder – Sexual aversion disorder u Sexual arousal disorder u Orgasmic disorder u Sexual pain disorders – Dyspareunia – Vaginismus – Noncoital sexual pain disorder *International Consensus Development Conference on Female Sexual Dysfunction. Basson R, et al. J Urol. 2000; 163: 888 -93.
 LUTS & Sexual Dysfunction u 25 -50% women with pelvic floor disorders u Most common – Decreased libido – Dyspareunia – Decreased orgasm u Urinary incontinence independently associated with worse sexual function Handa. AJOG 2004
LUTS & Sexual Dysfunction u 25 -50% women with pelvic floor disorders u Most common – Decreased libido – Dyspareunia – Decreased orgasm u Urinary incontinence independently associated with worse sexual function Handa. AJOG 2004
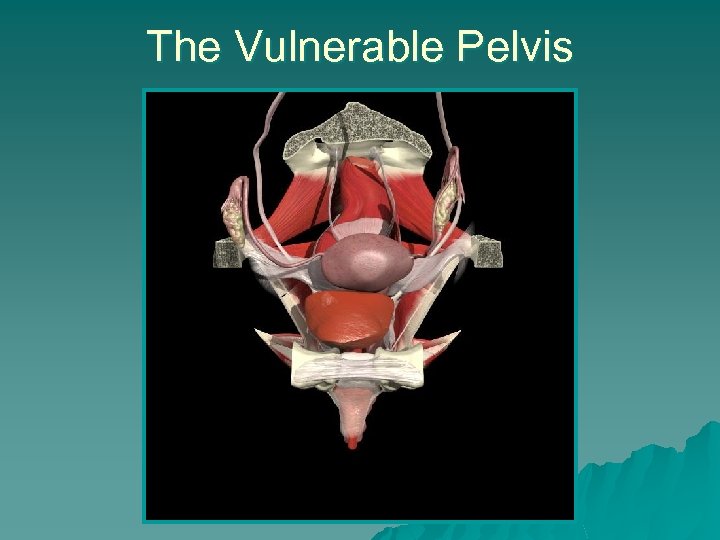 The Vulnerable Pelvis
The Vulnerable Pelvis
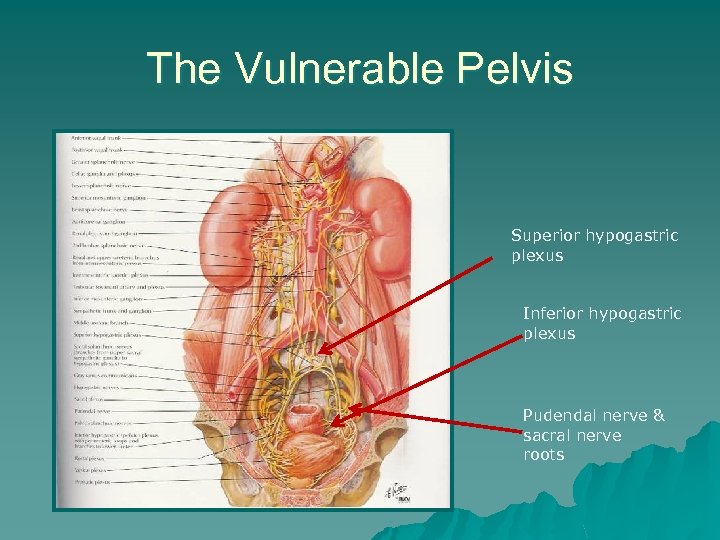 The Vulnerable Pelvis Superior hypogastric plexus Inferior hypogastric plexus Pudendal nerve & sacral nerve roots
The Vulnerable Pelvis Superior hypogastric plexus Inferior hypogastric plexus Pudendal nerve & sacral nerve roots
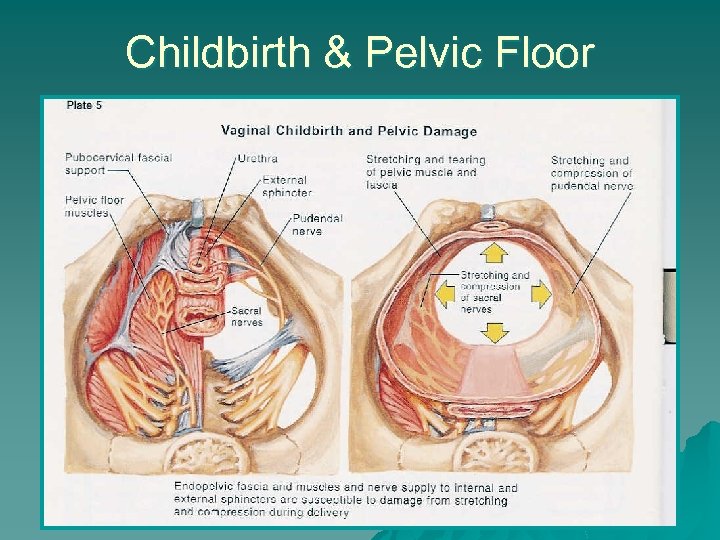 Childbirth & Pelvic Floor
Childbirth & Pelvic Floor
 Surgery & The Pelvis
Surgery & The Pelvis
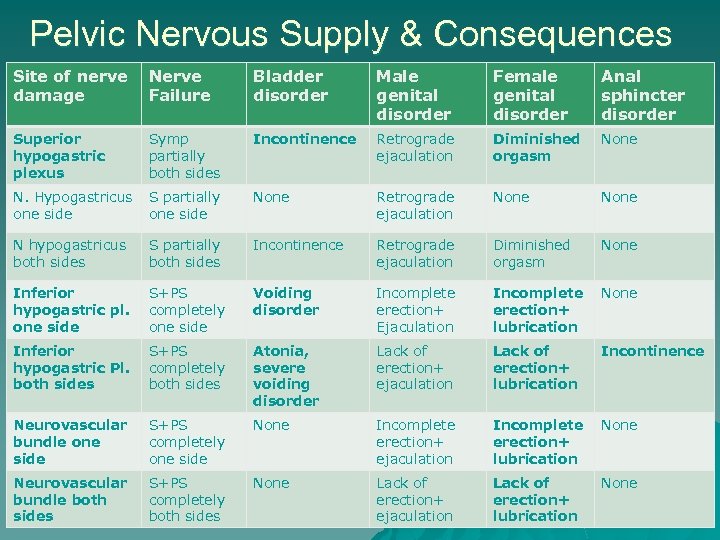 Pelvic Nervous Supply & Consequences Site of nerve damage Nerve Failure Bladder disorder Male genital disorder Female genital disorder Anal sphincter disorder Superior hypogastric plexus Symp partially both sides Incontinence Retrograde ejaculation Diminished orgasm None N. Hypogastricus one side S partially one side None Retrograde ejaculation None N hypogastricus both sides S partially both sides Incontinence Retrograde ejaculation Diminished orgasm None Inferior hypogastric pl. one side S+PS completely one side Voiding disorder Incomplete erection+ Ejaculation Incomplete erection+ lubrication None Inferior hypogastric Pl. both sides S+PS completely both sides Atonia, severe voiding disorder Lack of erection+ ejaculation Lack of erection+ lubrication Incontinence Neurovascular bundle one side S+PS completely one side None Incomplete erection+ ejaculation Incomplete erection+ lubrication None Neurovascular bundle both sides S+PS completely both sides None Lack of erection+ ejaculation Lack of erection+ lubrication None
Pelvic Nervous Supply & Consequences Site of nerve damage Nerve Failure Bladder disorder Male genital disorder Female genital disorder Anal sphincter disorder Superior hypogastric plexus Symp partially both sides Incontinence Retrograde ejaculation Diminished orgasm None N. Hypogastricus one side S partially one side None Retrograde ejaculation None N hypogastricus both sides S partially both sides Incontinence Retrograde ejaculation Diminished orgasm None Inferior hypogastric pl. one side S+PS completely one side Voiding disorder Incomplete erection+ Ejaculation Incomplete erection+ lubrication None Inferior hypogastric Pl. both sides S+PS completely both sides Atonia, severe voiding disorder Lack of erection+ ejaculation Lack of erection+ lubrication Incontinence Neurovascular bundle one side S+PS completely one side None Incomplete erection+ ejaculation Incomplete erection+ lubrication None Neurovascular bundle both sides S+PS completely both sides None Lack of erection+ ejaculation Lack of erection+ lubrication None
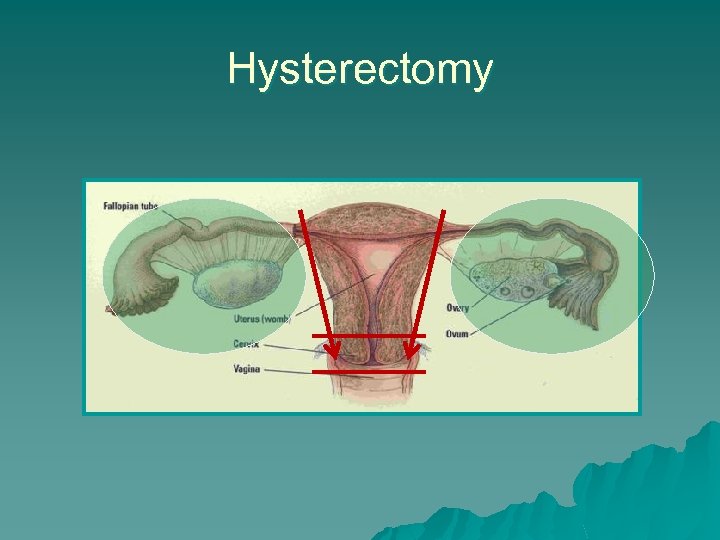 Hysterectomy
Hysterectomy
 General Gynecology u Hysterectomy- any route – Mild improvement in LUTS 1, 2 – Improvement in sexual function 3 u Postmenopausal status, severity of gynecologic complaints, & preop frequency predictors of sexual outcomes u Abdominal scar/pain short term impact – Supracervical & abdominal hysterectomy -similar outcomes 4 1. 2. 3. 4. El-Touky. J Obstet Gynecol 2004 Kluviers. J Minim Invasive Gynecol 2007 Gutl. J Psychosom Obstet Gynecol 2002 Kupperman et al. Obstet Gynecol 2005
General Gynecology u Hysterectomy- any route – Mild improvement in LUTS 1, 2 – Improvement in sexual function 3 u Postmenopausal status, severity of gynecologic complaints, & preop frequency predictors of sexual outcomes u Abdominal scar/pain short term impact – Supracervical & abdominal hysterectomy -similar outcomes 4 1. 2. 3. 4. El-Touky. J Obstet Gynecol 2004 Kluviers. J Minim Invasive Gynecol 2007 Gutl. J Psychosom Obstet Gynecol 2002 Kupperman et al. Obstet Gynecol 2005
 Oophorectomy u Premenopausal woman – Worse body image – Poor sleep – Decreased overall quality of life SF-36 – No difference in sexual scores, urinary complaints – At 2 years-Equivalent! – Improvement in gynecologic condition & postoperative well-being 1. Teplin. Obstet Gynecol 2007 2. Aziz. Maturitas 2005
Oophorectomy u Premenopausal woman – Worse body image – Poor sleep – Decreased overall quality of life SF-36 – No difference in sexual scores, urinary complaints – At 2 years-Equivalent! – Improvement in gynecologic condition & postoperative well-being 1. Teplin. Obstet Gynecol 2007 2. Aziz. Maturitas 2005
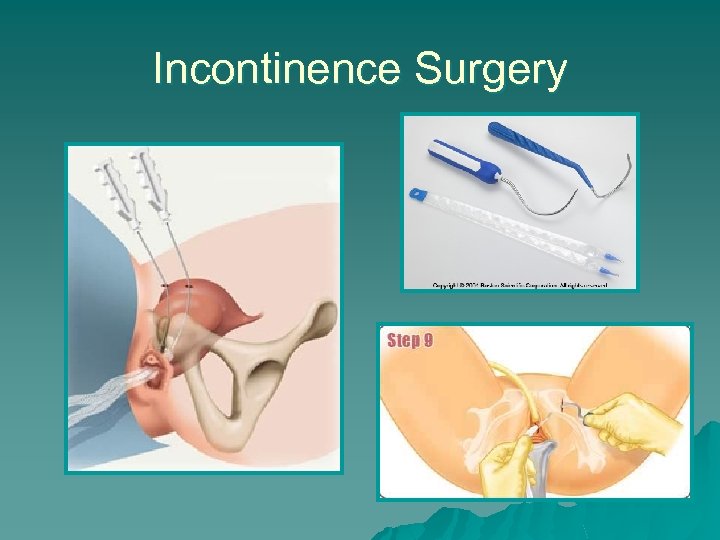 Incontinence Surgery
Incontinence Surgery
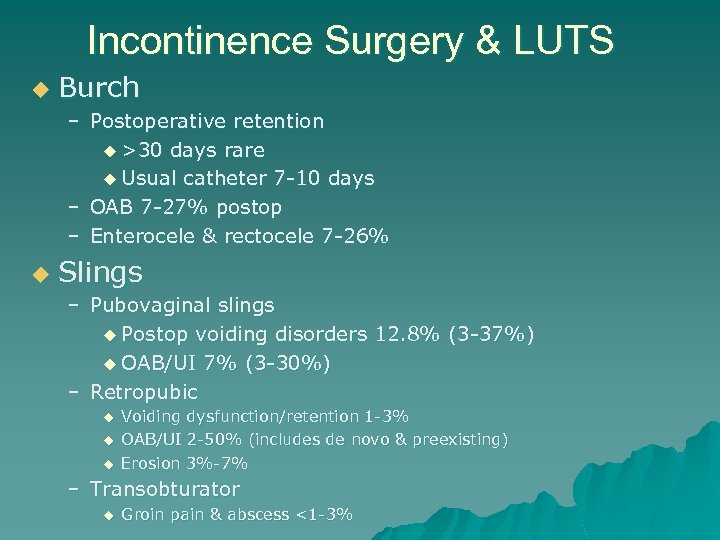 Incontinence Surgery & LUTS u Burch – Postoperative retention u >30 days rare u Usual catheter 7 -10 days – OAB 7 -27% postop – Enterocele & rectocele 7 -26% u Slings – Pubovaginal slings u Postop voiding disorders 12. 8% (3 -37%) u OAB/UI 7% (3 -30%) – Retropubic u u u Voiding dysfunction/retention 1 -3% OAB/UI 2 -50% (includes de novo & preexisting) Erosion 3%-7% – Transobturator u Groin pain & abscess <1 -3%
Incontinence Surgery & LUTS u Burch – Postoperative retention u >30 days rare u Usual catheter 7 -10 days – OAB 7 -27% postop – Enterocele & rectocele 7 -26% u Slings – Pubovaginal slings u Postop voiding disorders 12. 8% (3 -37%) u OAB/UI 7% (3 -30%) – Retropubic u u u Voiding dysfunction/retention 1 -3% OAB/UI 2 -50% (includes de novo & preexisting) Erosion 3%-7% – Transobturator u Groin pain & abscess <1 -3%
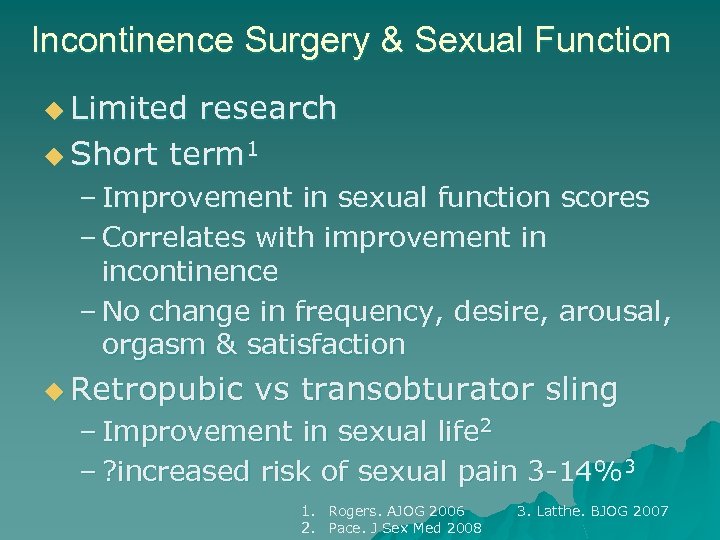 Incontinence Surgery & Sexual Function u Limited research u Short term 1 – Improvement in sexual function scores – Correlates with improvement in incontinence – No change in frequency, desire, arousal, orgasm & satisfaction u Retropubic vs transobturator sling – Improvement in sexual life 2 – ? increased risk of sexual pain 3 -14%3 1. Rogers. AJOG 2006 2. Pace. J Sex Med 2008 3. Latthe. BJOG 2007
Incontinence Surgery & Sexual Function u Limited research u Short term 1 – Improvement in sexual function scores – Correlates with improvement in incontinence – No change in frequency, desire, arousal, orgasm & satisfaction u Retropubic vs transobturator sling – Improvement in sexual life 2 – ? increased risk of sexual pain 3 -14%3 1. Rogers. AJOG 2006 2. Pace. J Sex Med 2008 3. Latthe. BJOG 2007
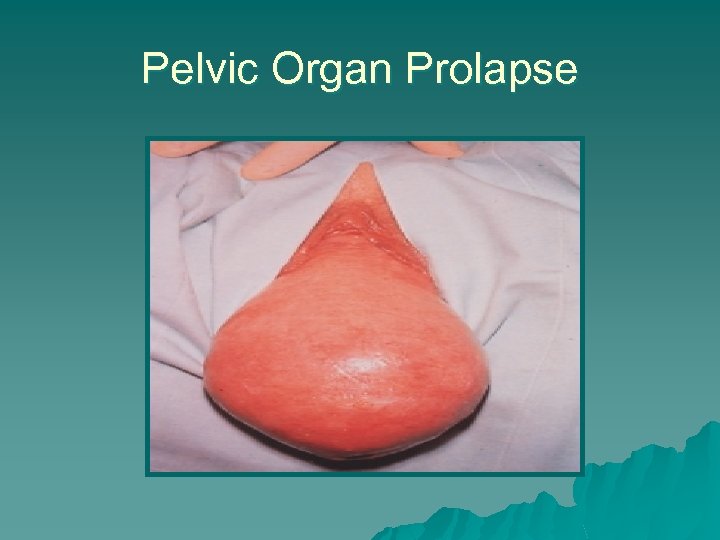 Pelvic Organ Prolapse
Pelvic Organ Prolapse
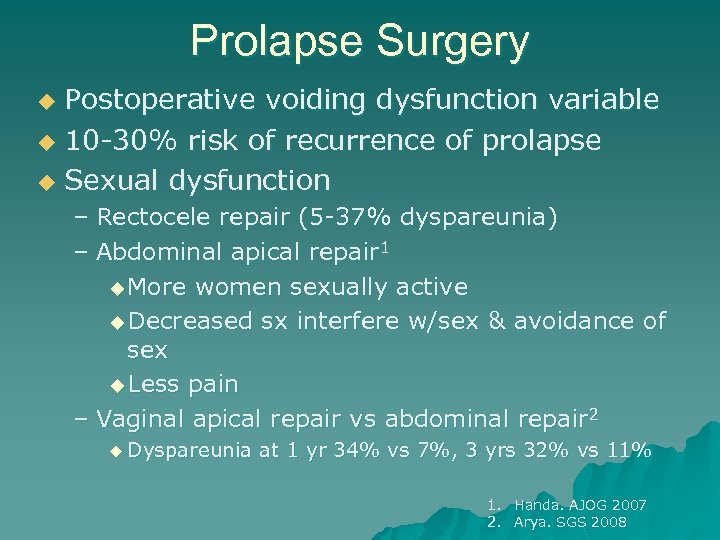 Prolapse Surgery Postoperative voiding dysfunction variable u 10 -30% risk of recurrence of prolapse u Sexual dysfunction u – Rectocele repair (5 -37% dyspareunia) – Abdominal apical repair 1 u More women sexually active u Decreased sx interfere w/sex & avoidance of sex u Less pain – Vaginal apical repair vs abdominal repair 2 u Dyspareunia at 1 yr 34% vs 7%, 3 yrs 32% vs 11% 1. Handa. AJOG 2007 2. Arya. SGS 2008
Prolapse Surgery Postoperative voiding dysfunction variable u 10 -30% risk of recurrence of prolapse u Sexual dysfunction u – Rectocele repair (5 -37% dyspareunia) – Abdominal apical repair 1 u More women sexually active u Decreased sx interfere w/sex & avoidance of sex u Less pain – Vaginal apical repair vs abdominal repair 2 u Dyspareunia at 1 yr 34% vs 7%, 3 yrs 32% vs 11% 1. Handa. AJOG 2007 2. Arya. SGS 2008
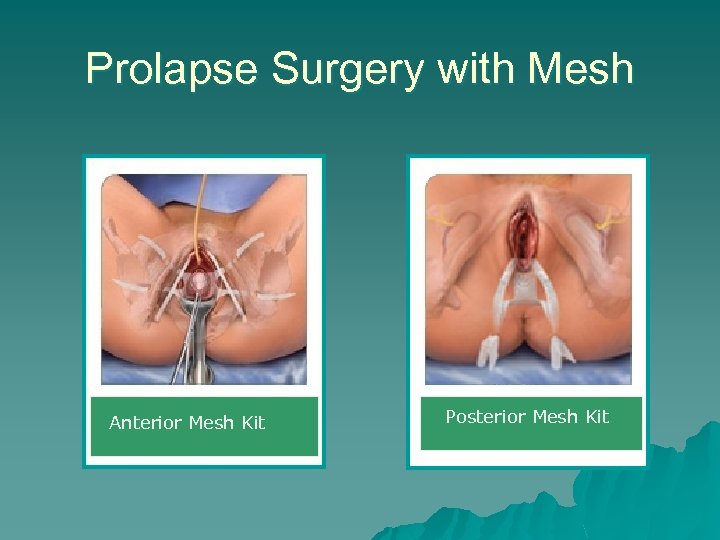 Prolapse Surgery with Mesh Anterior Mesh Kit Posterior Mesh Kit
Prolapse Surgery with Mesh Anterior Mesh Kit Posterior Mesh Kit
 Prolapse Repair with Mesh u 8 papers/presentations at AUGS Oct 2007 u 10 papers/ presentations at SGS April 2008 u Erosion rates 2 -13% u Reoperation rates for erosion, fistula, or pain 20% u Dyspareunia 38 -41%
Prolapse Repair with Mesh u 8 papers/presentations at AUGS Oct 2007 u 10 papers/ presentations at SGS April 2008 u Erosion rates 2 -13% u Reoperation rates for erosion, fistula, or pain 20% u Dyspareunia 38 -41%
 SGS Guidelines for Use of Graft In Prolapse Surgery Systematic review u Medline 1950 -2007 u Publications on comparative studies using vaginal grafts u Adverse events of non-comparative studies u
SGS Guidelines for Use of Graft In Prolapse Surgery Systematic review u Medline 1950 -2007 u Publications on comparative studies using vaginal grafts u Adverse events of non-comparative studies u
 How to GRADE the evidence… u Quality of Evidence – High-more research unlikely to change confidence in effect – Moderate-more research likely to change confidence in effect & may change estimate of effect – Low-very likely to change confidence in effect & likely change estimate of effect – Very Low- any estimate of effect is uncertain u Recommendations – Strong- high quality evidence &/or other considerations support strong recommendation – Moderate-high or moderate evidence &/or other considerations support moderate recommendations – Weak-low or very low evidence support weak recommendation, based mostly on expert opinion
How to GRADE the evidence… u Quality of Evidence – High-more research unlikely to change confidence in effect – Moderate-more research likely to change confidence in effect & may change estimate of effect – Low-very likely to change confidence in effect & likely change estimate of effect – Very Low- any estimate of effect is uncertain u Recommendations – Strong- high quality evidence &/or other considerations support strong recommendation – Moderate-high or moderate evidence &/or other considerations support moderate recommendations – Weak-low or very low evidence support weak recommendation, based mostly on expert opinion
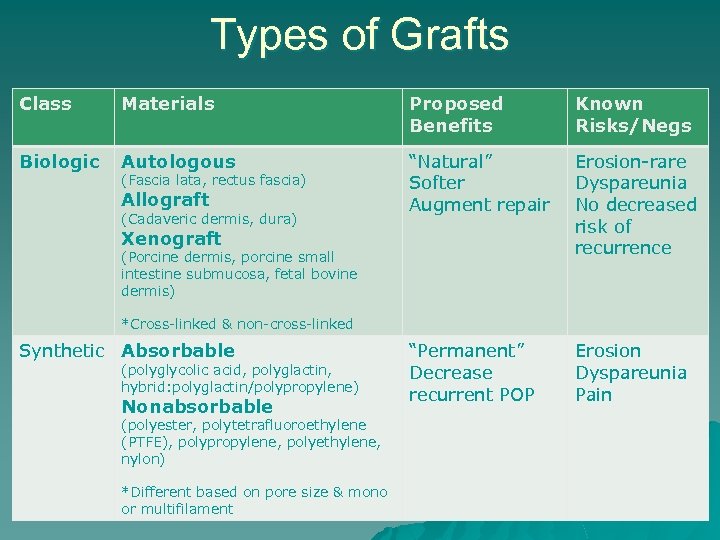 Types of Grafts Class Materials Proposed Benefits Known Risks/Negs Biologic Autologous “Natural” Softer Augment repair Erosion-rare Dyspareunia No decreased risk of recurrence “Permanent” Decrease recurrent POP Erosion Dyspareunia Pain (Fascia lata, rectus fascia) Allograft (Cadaveric dermis, dura) Xenograft (Porcine dermis, porcine small intestine submucosa, fetal bovine dermis) *Cross-linked & non-cross-linked Synthetic Absorbable (polyglycolic acid, polyglactin, hybrid: polyglactin/polypropylene) Nonabsorbable (polyester, polytetrafluoroethylene (PTFE), polypropylene, polyethylene, nylon) *Different based on pore size & mono or multifilament
Types of Grafts Class Materials Proposed Benefits Known Risks/Negs Biologic Autologous “Natural” Softer Augment repair Erosion-rare Dyspareunia No decreased risk of recurrence “Permanent” Decrease recurrent POP Erosion Dyspareunia Pain (Fascia lata, rectus fascia) Allograft (Cadaveric dermis, dura) Xenograft (Porcine dermis, porcine small intestine submucosa, fetal bovine dermis) *Cross-linked & non-cross-linked Synthetic Absorbable (polyglycolic acid, polyglactin, hybrid: polyglactin/polypropylene) Nonabsorbable (polyester, polytetrafluoroethylene (PTFE), polypropylene, polyethylene, nylon) *Different based on pore size & mono or multifilament
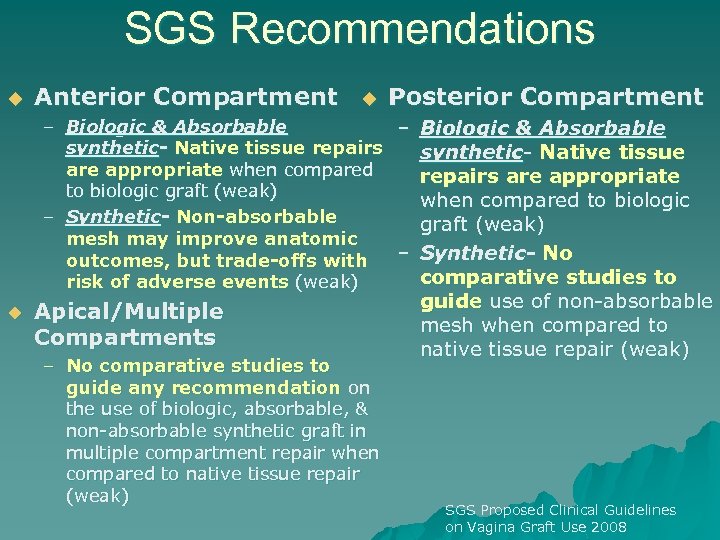 SGS Recommendations u Anterior Compartment u Posterior Compartment – Biologic & Absorbable synthetic- Native tissue repairs synthetic- Native tissue are appropriate when compared repairs are appropriate to biologic graft (weak) when compared to biologic – Synthetic- Non-absorbable graft (weak) mesh may improve anatomic – Synthetic- No outcomes, but trade-offs with comparative studies to risk of adverse events (weak) u Apical/Multiple Compartments – No comparative studies to guide any recommendation on the use of biologic, absorbable, & non-absorbable synthetic graft in multiple compartment repair when compared to native tissue repair (weak) guide use of non-absorbable mesh when compared to native tissue repair (weak) SGS Proposed Clinical Guidelines on Vagina Graft Use 2008
SGS Recommendations u Anterior Compartment u Posterior Compartment – Biologic & Absorbable synthetic- Native tissue repairs synthetic- Native tissue are appropriate when compared repairs are appropriate to biologic graft (weak) when compared to biologic – Synthetic- Non-absorbable graft (weak) mesh may improve anatomic – Synthetic- No outcomes, but trade-offs with comparative studies to risk of adverse events (weak) u Apical/Multiple Compartments – No comparative studies to guide any recommendation on the use of biologic, absorbable, & non-absorbable synthetic graft in multiple compartment repair when compared to native tissue repair (weak) guide use of non-absorbable mesh when compared to native tissue repair (weak) SGS Proposed Clinical Guidelines on Vagina Graft Use 2008
 Surgery for Gynecologic Malignancy: Radical Hysterectomy
Surgery for Gynecologic Malignancy: Radical Hysterectomy
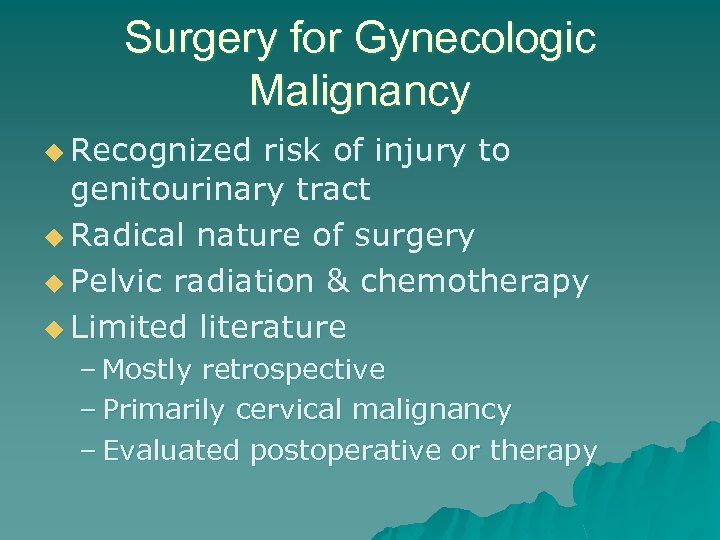 Surgery for Gynecologic Malignancy u Recognized risk of injury to genitourinary tract u Radical nature of surgery u Pelvic radiation & chemotherapy u Limited literature – Mostly retrospective – Primarily cervical malignancy – Evaluated postoperative or therapy
Surgery for Gynecologic Malignancy u Recognized risk of injury to genitourinary tract u Radical nature of surgery u Pelvic radiation & chemotherapy u Limited literature – Mostly retrospective – Primarily cervical malignancy – Evaluated postoperative or therapy
 Effects of Radical Hysterectomy u Hypertonicity-early u Voiding & transient dysfunction – Abdominal straining – Decreased compliance u Stress incontinence u Detrusor overactivity
Effects of Radical Hysterectomy u Hypertonicity-early u Voiding & transient dysfunction – Abdominal straining – Decreased compliance u Stress incontinence u Detrusor overactivity
 Gynecologic Malignancy & LUTS u Farquharson et al 1986 – 15% baseline report urinary incontinence – Stress incontinence more common in surgery alone group-26% (10 -52%) – Urgency, mixed incontinence >RT group – 63% incidence of incontinence following radical hysterectomy + radiation – No difference in bladder sensation – RH + RT less bladder compliance
Gynecologic Malignancy & LUTS u Farquharson et al 1986 – 15% baseline report urinary incontinence – Stress incontinence more common in surgery alone group-26% (10 -52%) – Urgency, mixed incontinence >RT group – 63% incidence of incontinence following radical hysterectomy + radiation – No difference in bladder sensation – RH + RT less bladder compliance
 Gynecologic Malignancy & LUTS Lin et al 2000 u 210 women w/cervical CA plan RH u Preoperative urodynamics u Mean age 49 u 42% menopausal w/o HRT u 17% had NORMAL preop urodynamics u 83% at least one type of LUTD u 73% storage dysfcn u 51% urinary incontinence (37% stress, DO 8%, mixed 6%) u No difference in age, parity, or stage u
Gynecologic Malignancy & LUTS Lin et al 2000 u 210 women w/cervical CA plan RH u Preoperative urodynamics u Mean age 49 u 42% menopausal w/o HRT u 17% had NORMAL preop urodynamics u 83% at least one type of LUTD u 73% storage dysfcn u 51% urinary incontinence (37% stress, DO 8%, mixed 6%) u No difference in age, parity, or stage u
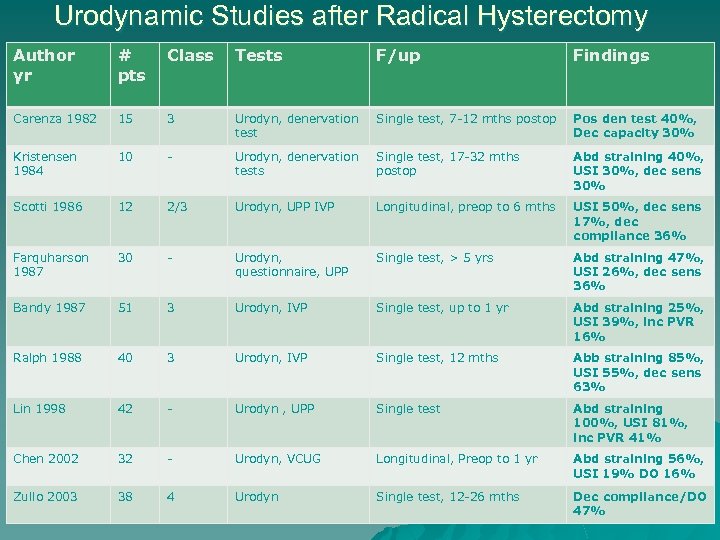 Urodynamic Studies after Radical Hysterectomy Author yr # pts Class Tests F/up Findings Carenza 1982 15 3 Urodyn, denervation test Single test, 7 -12 mths postop Pos den test 40%, Dec capacity 30% Kristensen 1984 10 - Urodyn, denervation tests Single test, 17 -32 mths postop Abd straining 40%, USI 30%, dec sens 30% Scotti 1986 12 2/3 Urodyn, UPP IVP Longitudinal, preop to 6 mths USI 50%, dec sens 17%, dec compliance 36% Farquharson 1987 30 - Urodyn, questionnaire, UPP Single test, > 5 yrs Abd straining 47%, USI 26%, dec sens 36% Bandy 1987 51 3 Urodyn, IVP Single test, up to 1 yr Abd straining 25%, USI 39%, inc PVR 16% Ralph 1988 40 3 Urodyn, IVP Single test, 12 mths Abb straining 85%, USI 55%, dec sens 63% Lin 1998 42 - Urodyn , UPP Single test Abd straining 100%, USI 81%, inc PVR 41% Chen 2002 32 - Urodyn, VCUG Longitudinal, Preop to 1 yr Abd straining 56%, USI 19% DO 16% Zullo 2003 38 4 Urodyn Single test, 12 -26 mths Dec compliance/DO 47%
Urodynamic Studies after Radical Hysterectomy Author yr # pts Class Tests F/up Findings Carenza 1982 15 3 Urodyn, denervation test Single test, 7 -12 mths postop Pos den test 40%, Dec capacity 30% Kristensen 1984 10 - Urodyn, denervation tests Single test, 17 -32 mths postop Abd straining 40%, USI 30%, dec sens 30% Scotti 1986 12 2/3 Urodyn, UPP IVP Longitudinal, preop to 6 mths USI 50%, dec sens 17%, dec compliance 36% Farquharson 1987 30 - Urodyn, questionnaire, UPP Single test, > 5 yrs Abd straining 47%, USI 26%, dec sens 36% Bandy 1987 51 3 Urodyn, IVP Single test, up to 1 yr Abd straining 25%, USI 39%, inc PVR 16% Ralph 1988 40 3 Urodyn, IVP Single test, 12 mths Abb straining 85%, USI 55%, dec sens 63% Lin 1998 42 - Urodyn , UPP Single test Abd straining 100%, USI 81%, inc PVR 41% Chen 2002 32 - Urodyn, VCUG Longitudinal, Preop to 1 yr Abd straining 56%, USI 19% DO 16% Zullo 2003 38 4 Urodyn Single test, 12 -26 mths Dec compliance/DO 47%
 Gynecologic Malignancy & Sexual Function u u u Retrospective & limited to postoperative evaluation Interruption in sexual activity common leading up to diagnosis Surgery impacts frequency of intercourse & dyspareunia Radiation more effect locally Most common effects: – Loss of desire, sensation, & increased pain Different cancers pose different problems
Gynecologic Malignancy & Sexual Function u u u Retrospective & limited to postoperative evaluation Interruption in sexual activity common leading up to diagnosis Surgery impacts frequency of intercourse & dyspareunia Radiation more effect locally Most common effects: – Loss of desire, sensation, & increased pain Different cancers pose different problems
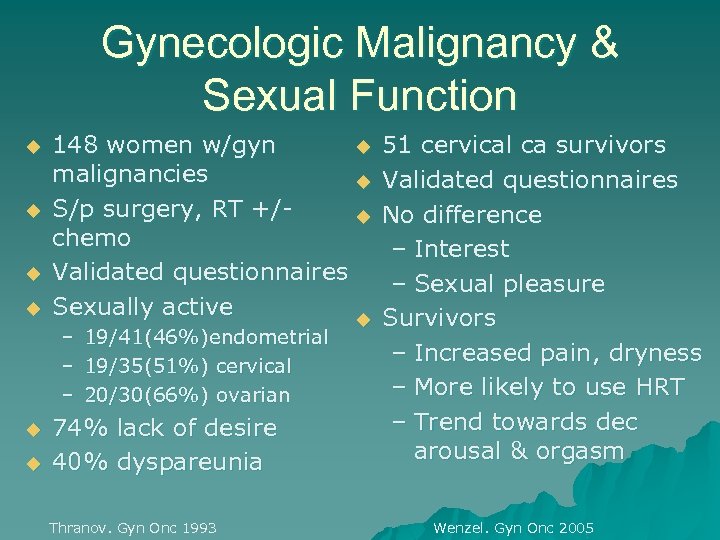 Gynecologic Malignancy & Sexual Function u u 148 women w/gyn u malignancies u S/p surgery, RT +/u chemo Validated questionnaires Sexually active u – 19/41(46%)endometrial – 19/35(51%) cervical – 20/30(66%) ovarian u u 74% lack of desire 40% dyspareunia Thranov. Gyn Onc 1993 51 cervical ca survivors Validated questionnaires No difference – Interest – Sexual pleasure Survivors – Increased pain, dryness – More likely to use HRT – Trend towards dec arousal & orgasm Wenzel. Gyn Onc 2005
Gynecologic Malignancy & Sexual Function u u 148 women w/gyn u malignancies u S/p surgery, RT +/u chemo Validated questionnaires Sexually active u – 19/41(46%)endometrial – 19/35(51%) cervical – 20/30(66%) ovarian u u 74% lack of desire 40% dyspareunia Thranov. Gyn Onc 1993 51 cervical ca survivors Validated questionnaires No difference – Interest – Sexual pleasure Survivors – Increased pain, dryness – More likely to use HRT – Trend towards dec arousal & orgasm Wenzel. Gyn Onc 2005
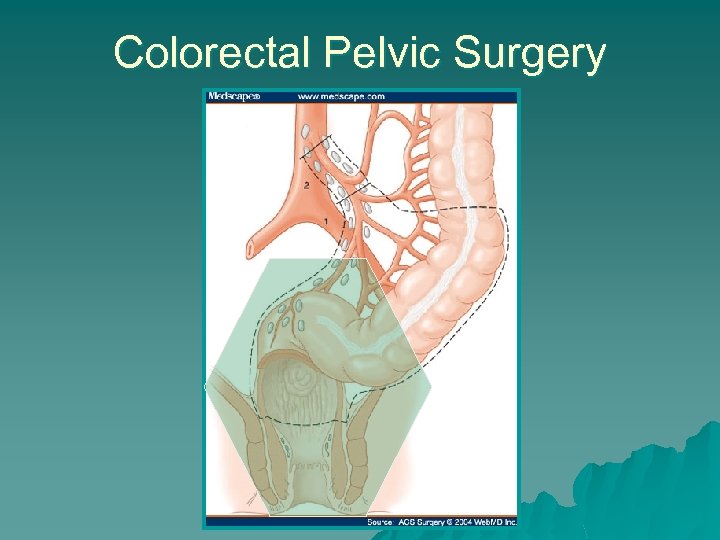 Colorectal Pelvic Surgery
Colorectal Pelvic Surgery
 Colorectal Surgery u Sigmoid & rectal cancer patients most vulnerable u Similar risk to adjacent organs & nerves u Most studies retrospective or descriptive, done postoperatively u Men studied more than women u Combined LUTS & sexual function u Improvement in outcomes with evolution of nerve sparing techniques
Colorectal Surgery u Sigmoid & rectal cancer patients most vulnerable u Similar risk to adjacent organs & nerves u Most studies retrospective or descriptive, done postoperatively u Men studied more than women u Combined LUTS & sexual function u Improvement in outcomes with evolution of nerve sparing techniques
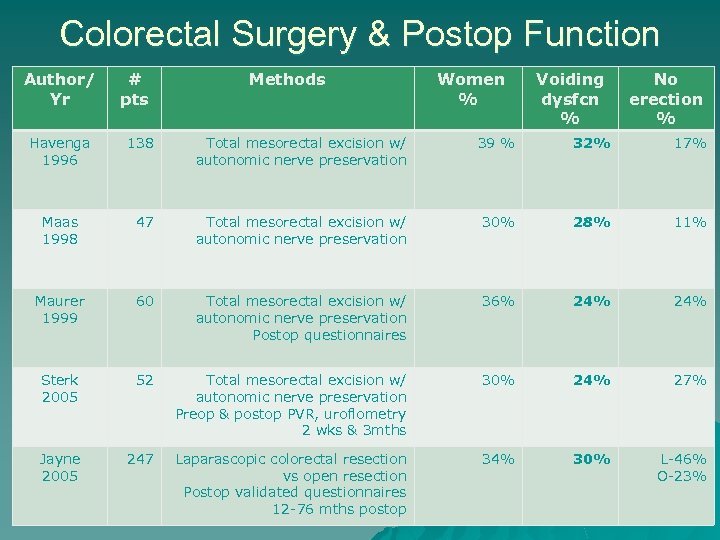 Colorectal Surgery & Postop Function Author/ Yr Havenga 1996 # pts Methods Women % Voiding dysfcn % No erection % 138 Total mesorectal excision w/ autonomic nerve preservation 39 % 32% 17% Maas 1998 47 Total mesorectal excision w/ autonomic nerve preservation 30% 28% 11% Maurer 1999 60 Total mesorectal excision w/ autonomic nerve preservation Postop questionnaires 36% 24% Sterk 2005 52 Total mesorectal excision w/ autonomic nerve preservation Preop & postop PVR, uroflometry 2 wks & 3 mths 30% 24% 27% Jayne 2005 247 Laparascopic colorectal resection vs open resection Postop validated questionnaires 12 -76 mths postop 34% 30% L-46% O-23%
Colorectal Surgery & Postop Function Author/ Yr Havenga 1996 # pts Methods Women % Voiding dysfcn % No erection % 138 Total mesorectal excision w/ autonomic nerve preservation 39 % 32% 17% Maas 1998 47 Total mesorectal excision w/ autonomic nerve preservation 30% 28% 11% Maurer 1999 60 Total mesorectal excision w/ autonomic nerve preservation Postop questionnaires 36% 24% Sterk 2005 52 Total mesorectal excision w/ autonomic nerve preservation Preop & postop PVR, uroflometry 2 wks & 3 mths 30% 24% 27% Jayne 2005 247 Laparascopic colorectal resection vs open resection Postop validated questionnaires 12 -76 mths postop 34% 30% L-46% O-23%
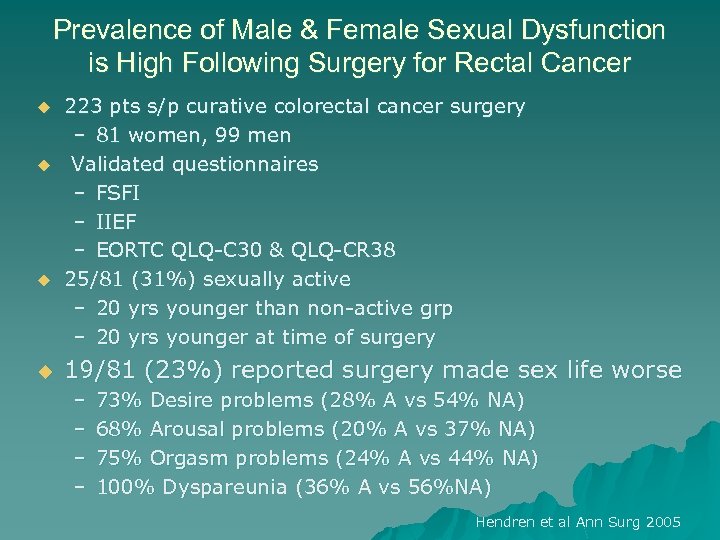 Prevalence of Male & Female Sexual Dysfunction is High Following Surgery for Rectal Cancer u u 223 pts s/p curative colorectal cancer surgery – 81 women, 99 men Validated questionnaires – FSFI – IIEF – EORTC QLQ-C 30 & QLQ-CR 38 25/81 (31%) sexually active – 20 yrs younger than non-active grp – 20 yrs younger at time of surgery 19/81 (23%) reported surgery made sex life worse – – 73% Desire problems (28% A vs 54% NA) 68% Arousal problems (20% A vs 37% NA) 75% Orgasm problems (24% A vs 44% NA) 100% Dyspareunia (36% A vs 56%NA) Hendren et al Ann Surg 2005
Prevalence of Male & Female Sexual Dysfunction is High Following Surgery for Rectal Cancer u u 223 pts s/p curative colorectal cancer surgery – 81 women, 99 men Validated questionnaires – FSFI – IIEF – EORTC QLQ-C 30 & QLQ-CR 38 25/81 (31%) sexually active – 20 yrs younger than non-active grp – 20 yrs younger at time of surgery 19/81 (23%) reported surgery made sex life worse – – 73% Desire problems (28% A vs 54% NA) 68% Arousal problems (20% A vs 37% NA) 75% Orgasm problems (24% A vs 44% NA) 100% Dyspareunia (36% A vs 56%NA) Hendren et al Ann Surg 2005
 Goals of Surgery u Remove pathology u Restore anatomy u Improve function u Extend survival u …. DO NO HARM!
Goals of Surgery u Remove pathology u Restore anatomy u Improve function u Extend survival u …. DO NO HARM!
 What we know… u Lower urinary tract symptoms are common u Sexual function is complex – Sexual dysfunction is difficult to measure – Common in our patients – Coincides with LUTS often u Pelvic surgery impacts the genitourinary tract, often adversely u Radical pelvic surgery & radiation have unique risks
What we know… u Lower urinary tract symptoms are common u Sexual function is complex – Sexual dysfunction is difficult to measure – Common in our patients – Coincides with LUTS often u Pelvic surgery impacts the genitourinary tract, often adversely u Radical pelvic surgery & radiation have unique risks
 Moving Forward…. u Establish prevalence of these symptoms in specific populations u Evaluate patients for LUTS & sexual dysfunction before pelvic surgery u Give better informed consent & counseling of postoperative expectations/functional changes u Offer treatment or concomitant surgery, when appropriate
Moving Forward…. u Establish prevalence of these symptoms in specific populations u Evaluate patients for LUTS & sexual dysfunction before pelvic surgery u Give better informed consent & counseling of postoperative expectations/functional changes u Offer treatment or concomitant surgery, when appropriate
 Evaluation for Sexual Pain Following Surgery u Careful History – Attention to any grafts, complications, pre -existing pain issues (Fibromyalgia, IBS, Endometriosis, IC, Vulvodynia) u Careful exam – Abdominal trigger points, psoas, iliacus – Musculoskeletal restrictions – Pelvic exam u Vaginal length, caliber, scarring, ridges, palpable grafts/sutures u Atrophy u Levator tenderness
Evaluation for Sexual Pain Following Surgery u Careful History – Attention to any grafts, complications, pre -existing pain issues (Fibromyalgia, IBS, Endometriosis, IC, Vulvodynia) u Careful exam – Abdominal trigger points, psoas, iliacus – Musculoskeletal restrictions – Pelvic exam u Vaginal length, caliber, scarring, ridges, palpable grafts/sutures u Atrophy u Levator tenderness
 Tests u Cystoscopy u Colonoscopy u Urinalysis, urine & vaginal cultures u +/- uroflow or urodynamics
Tests u Cystoscopy u Colonoscopy u Urinalysis, urine & vaginal cultures u +/- uroflow or urodynamics
 Treatment u Aimed at physical & emotional findings u Establish short & long term goals u Multidisciplinary – Physician, PT, Psych, Pain Management, Sexual Therapy
Treatment u Aimed at physical & emotional findings u Establish short & long term goals u Multidisciplinary – Physician, PT, Psych, Pain Management, Sexual Therapy
 u Physician Treatment – Surgical revision, removal of mesh, etc – Dilators – Trigger point/pudendal injections u Kenalog 10 mg/ml, 0. 25% marcaine, sodium bicarbonate – RX: compounded medications for vagina/vulva u Baclofen, ketamine/lidocaine/gabapentin, amitriptyline/baclofen/gabapentin, cyclobenzaprine, estradiol, testosterone, etc. – Botox injections 20 -40 units levators – Inter. Stim
u Physician Treatment – Surgical revision, removal of mesh, etc – Dilators – Trigger point/pudendal injections u Kenalog 10 mg/ml, 0. 25% marcaine, sodium bicarbonate – RX: compounded medications for vagina/vulva u Baclofen, ketamine/lidocaine/gabapentin, amitriptyline/baclofen/gabapentin, cyclobenzaprine, estradiol, testosterone, etc. – Botox injections 20 -40 units levators – Inter. Stim
 Current Research u Prevalence of Lower Urinary Tract Symptoms in Women with Gynecologic Malignancy planning to Undergo Surgery u Lower Urinary Tract and Sexual Function in Women following Surgery for Colorectal Disorders u Trigger Point Injections with Manual Physical Therapy for Treatment of Pelvic Muscle Tension Myalgia
Current Research u Prevalence of Lower Urinary Tract Symptoms in Women with Gynecologic Malignancy planning to Undergo Surgery u Lower Urinary Tract and Sexual Function in Women following Surgery for Colorectal Disorders u Trigger Point Injections with Manual Physical Therapy for Treatment of Pelvic Muscle Tension Myalgia
 Questions?
Questions?


