e118df11f3ad018a9043366fe6f301f3.ppt
- Количество слайдов: 34
 Long-Term Care Insurance The Missing Link in Retirement Planning Presented by www. CTpartnership. org
Long-Term Care Insurance The Missing Link in Retirement Planning Presented by www. CTpartnership. org
 What is Long-Term Care? A wide range of services designed to manage limitations caused by a chronic condition and to minimize further deterioration of physical and mental health.
What is Long-Term Care? A wide range of services designed to manage limitations caused by a chronic condition and to minimize further deterioration of physical and mental health.
 THE RISK FOR LONG-TERM CARE
THE RISK FOR LONG-TERM CARE
 THE COST OF LONG-TERM CARE
THE COST OF LONG-TERM CARE
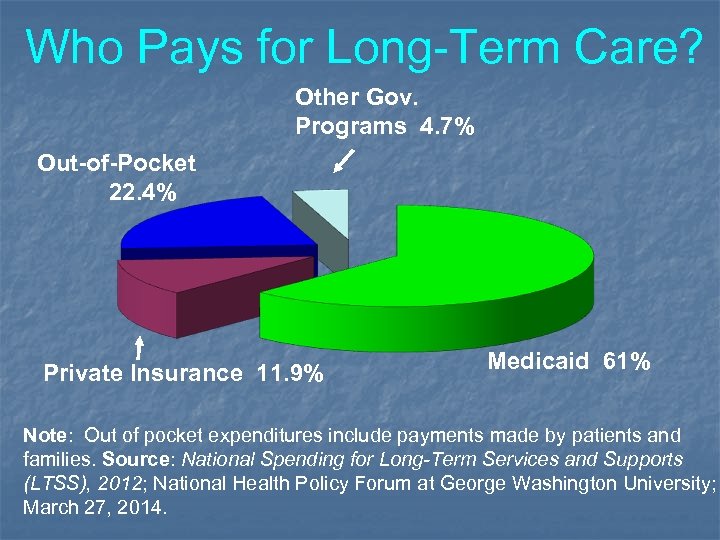 Who Pays for Long-Term Care? Other Gov. Programs 4. 7% Out-of-Pocket 22. 4% Private Insurance 11. 9% Medicaid 61% Note: Out of pocket expenditures include payments made by patients and families. Source: National Spending for Long-Term Services and Supports (LTSS), 2012; National Health Policy Forum at George Washington University; March 27, 2014.
Who Pays for Long-Term Care? Other Gov. Programs 4. 7% Out-of-Pocket 22. 4% Private Insurance 11. 9% Medicaid 61% Note: Out of pocket expenditures include payments made by patients and families. Source: National Spending for Long-Term Services and Supports (LTSS), 2012; National Health Policy Forum at George Washington University; March 27, 2014.
 WHY LONG-TERM CARE INSURANCE?
WHY LONG-TERM CARE INSURANCE?
 (1) Risk is high (2) Cost is high (3) Medi. CARE and health insurance do not pay for long-term care (4) While Medic. AID pays for long-term care, you have to be poor and eligibility rules are restrictive (5) Partnership for Long-Term Care
(1) Risk is high (2) Cost is high (3) Medi. CARE and health insurance do not pay for long-term care (4) While Medic. AID pays for long-term care, you have to be poor and eligibility rules are restrictive (5) Partnership for Long-Term Care
 (800) 547 -3443 www. ctpartnership. org
(800) 547 -3443 www. ctpartnership. org
 Program Goals n. Provide individuals a way to plan for their long-term care needs n. Enhance standards of long-term care insurance n. Provide public education n. Conserve State Medicaid funds
Program Goals n. Provide individuals a way to plan for their long-term care needs n. Enhance standards of long-term care insurance n. Provide public education n. Conserve State Medicaid funds
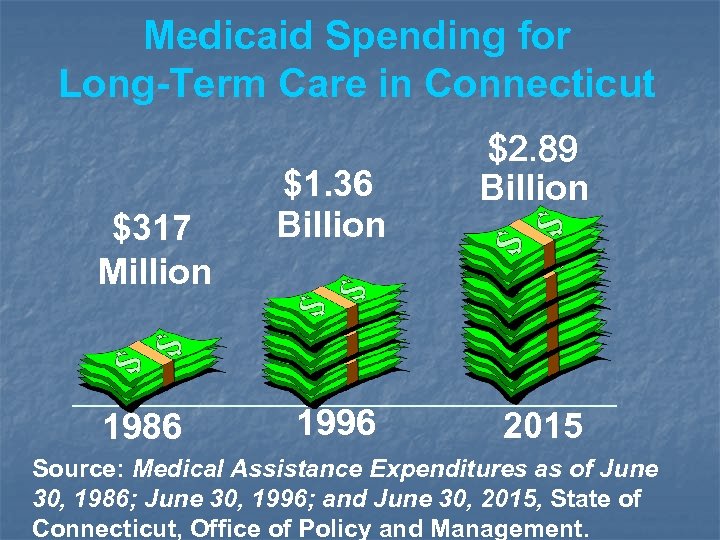 Medicaid Spending for Long-Term Care in Connecticut $317 Million 1986 $1. 36 Billion 1996 $2. 89 Billion 2015 Source: Medical Assistance Expenditures as of June 30, 1986; June 30, 1996; and June 30, 2015, State of Connecticut, Office of Policy and Management.
Medicaid Spending for Long-Term Care in Connecticut $317 Million 1986 $1. 36 Billion 1996 $2. 89 Billion 2015 Source: Medical Assistance Expenditures as of June 30, 1986; June 30, 1996; and June 30, 2015, State of Connecticut, Office of Policy and Management.
 DECISION CHECKLIST FOR A POLICY ü ü ü Where Will Benefits Be Paid Daily/Weekly/Monthly Benefit Lifetime Benefit Inflation Protection Elimination Period (deductible)
DECISION CHECKLIST FOR A POLICY ü ü ü Where Will Benefits Be Paid Daily/Weekly/Monthly Benefit Lifetime Benefit Inflation Protection Elimination Period (deductible)
 PARTNERSHIP CHECKLIST ü State Endorsement ü Medicaid Asset Protection ü Strict Consumer Standards ü Nursing Facility Discount
PARTNERSHIP CHECKLIST ü State Endorsement ü Medicaid Asset Protection ü Strict Consumer Standards ü Nursing Facility Discount
 ü State Endorsement Only Partnership long-term care coverage carries the State’s special endorsement for meeting strict consumer standards.
ü State Endorsement Only Partnership long-term care coverage carries the State’s special endorsement for meeting strict consumer standards.
 How Asset Protection Works n. If you continue to need care after your Partnership policy has paid benefits, you may apply for assistance from Medicaid. n. When determining eligibility, the Dept. of Social Services will disregard or ignore any assets you have up to the amount the Partnership policy has paid in benefits.
How Asset Protection Works n. If you continue to need care after your Partnership policy has paid benefits, you may apply for assistance from Medicaid. n. When determining eligibility, the Dept. of Social Services will disregard or ignore any assets you have up to the amount the Partnership policy has paid in benefits.
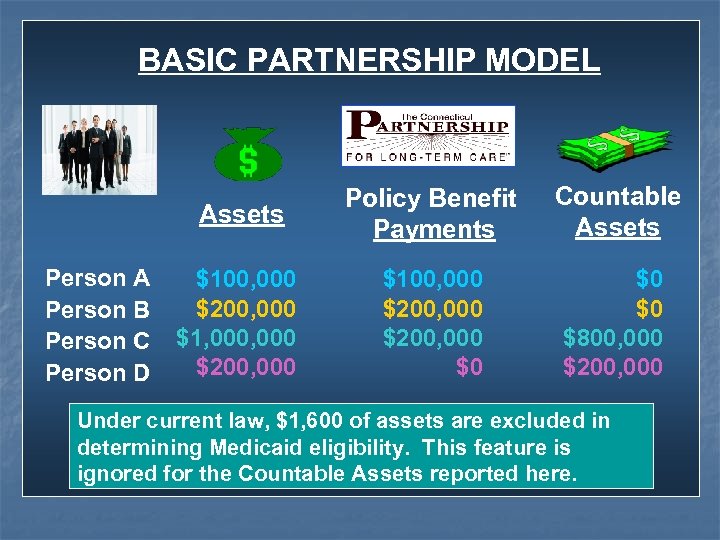 BASIC PARTNERSHIP MODEL Assets Person A Person B Person C Person D Policy Benefit Payments Countable Assets $100, 000 $200, 000 $1, 000 $200, 000 $100, 000 $200, 000 $0 $800, 000 $200, 000 Under current law, $1, 600 of assets are excluded in determining Medicaid eligibility. This feature is ignored for the Countable Assets reported here.
BASIC PARTNERSHIP MODEL Assets Person A Person B Person C Person D Policy Benefit Payments Countable Assets $100, 000 $200, 000 $1, 000 $200, 000 $100, 000 $200, 000 $0 $800, 000 $200, 000 Under current law, $1, 600 of assets are excluded in determining Medicaid eligibility. This feature is ignored for the Countable Assets reported here.
 Medicaid Asset Protection is free. Premiums for comparable Partnership and non-Partnership plans from the same company are identical. n Assets protected through the Partnership will not be recovered by Medicaid. n
Medicaid Asset Protection is free. Premiums for comparable Partnership and non-Partnership plans from the same company are identical. n Assets protected through the Partnership will not be recovered by Medicaid. n
 Must Reside In CT (or any reciprocal state*) n At purchase and issue of Partnership policy n When applying for and receiving Medicaid Dollar-for-dollar reciprocity between CT and other states CT has a reciprocal agreement with (*see notes for additional information).
Must Reside In CT (or any reciprocal state*) n At purchase and issue of Partnership policy n When applying for and receiving Medicaid Dollar-for-dollar reciprocity between CT and other states CT has a reciprocal agreement with (*see notes for additional information).
 Reciprocity Compact n n Dollar for dollar Medicaid Asset Protection between all states in Compact. States can opt out of Compact with 60 days notice to the Federal Government. Reciprocity is important when applying to Medicaid. All Partnership policyholders have reciprocity regardless of when the Partnership policy was purchased.
Reciprocity Compact n n Dollar for dollar Medicaid Asset Protection between all states in Compact. States can opt out of Compact with 60 days notice to the Federal Government. Reciprocity is important when applying to Medicaid. All Partnership policyholders have reciprocity regardless of when the Partnership policy was purchased.
 Use of Nursing Facility and Home Care* ð ð Average length of stay in a nursing facility is approximately 2 1/2 years (for individuals 65 years of age and older) Average length of time receiving home care services is 4. 1 years About half transition from home care to a nursing facility *(see notes for additional information)
Use of Nursing Facility and Home Care* ð ð Average length of stay in a nursing facility is approximately 2 1/2 years (for individuals 65 years of age and older) Average length of time receiving home care services is 4. 1 years About half transition from home care to a nursing facility *(see notes for additional information)
 Greater Affordability n. You need only buy an amount of insurance equal to the amount of assets you wish to protect n. Greater rationale for purchase of shorter coverage
Greater Affordability n. You need only buy an amount of insurance equal to the amount of assets you wish to protect n. Greater rationale for purchase of shorter coverage
 ü Strict Consumer Standards 1. Must offer option to purchase wide array of home and community-based services. Must include homemaker and other support services.
ü Strict Consumer Standards 1. Must offer option to purchase wide array of home and community-based services. Must include homemaker and other support services.
 2. Extensive care management services must be part of the home care benefit v Assessment v Plan of Care v Coordination of Services v Monitoring of Services.
2. Extensive care management services must be part of the home care benefit v Assessment v Plan of Care v Coordination of Services v Monitoring of Services.
 3. Minimum Daily Benefit Amount Policies applied for in: 2016 2017 Nursing Facility $256 $265 Home Care $128 $132. 50
3. Minimum Daily Benefit Amount Policies applied for in: 2016 2017 Nursing Facility $256 $265 Home Care $128 $132. 50
 4. Must provide automatic, compounded inflation protection on an annual basis without increases in premium.
4. Must provide automatic, compounded inflation protection on an annual basis without increases in premium.
 5. Must offer shorter term coverage to those in danger of lapsing policy 6. Producers complete special training.
5. Must offer shorter term coverage to those in danger of lapsing policy 6. Producers complete special training.
 Guaranteed Discount Only Partnership policyholders are guaranteed a 5% discount on nursing home rates in Connecticut.
Guaranteed Discount Only Partnership policyholders are guaranteed a 5% discount on nursing home rates in Connecticut.
 Premiums § § Premium Increases Payment Modes: § § Lifetime Waiver of Premium
Premiums § § Premium Increases Payment Modes: § § Lifetime Waiver of Premium
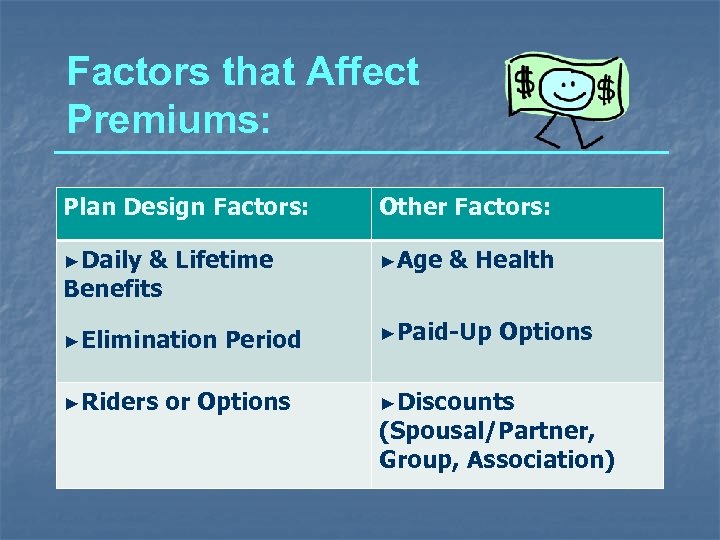 Factors that Affect Premiums: Plan Design Factors: Other Factors: ►Daily & Lifetime Benefits ►Age ►Elimination ►Paid-Up ►Riders Period or Options & Health Options ►Discounts (Spousal/Partner, Group, Association)
Factors that Affect Premiums: Plan Design Factors: Other Factors: ►Daily & Lifetime Benefits ►Age ►Elimination ►Paid-Up ►Riders Period or Options & Health Options ►Discounts (Spousal/Partner, Group, Association)
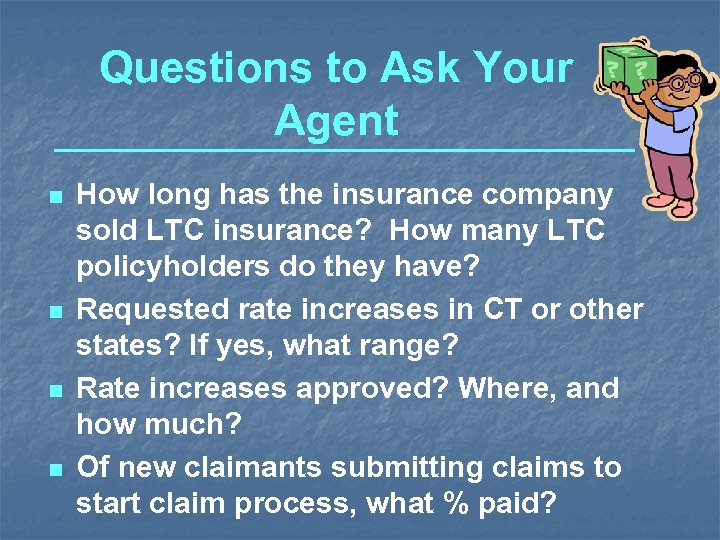 Questions to Ask Your Agent n n How long has the insurance company sold LTC insurance? How many LTC policyholders do they have? Requested rate increases in CT or other states? If yes, what range? Rate increases approved? Where, and how much? Of new claimants submitting claims to start claim process, what % paid?
Questions to Ask Your Agent n n How long has the insurance company sold LTC insurance? How many LTC policyholders do they have? Requested rate increases in CT or other states? If yes, what range? Rate increases approved? Where, and how much? Of new claimants submitting claims to start claim process, what % paid?
 Free Services Available from the State n Easy to read publications Trained staff and volunteers for individual assistance n Toll-free number to access services (1 -800 -547 -3443) n Website – www. ctpartnership. org n
Free Services Available from the State n Easy to read publications Trained staff and volunteers for individual assistance n Toll-free number to access services (1 -800 -547 -3443) n Website – www. ctpartnership. org n
 (800) 547 -3443 www. ctpartnership. org
(800) 547 -3443 www. ctpartnership. org
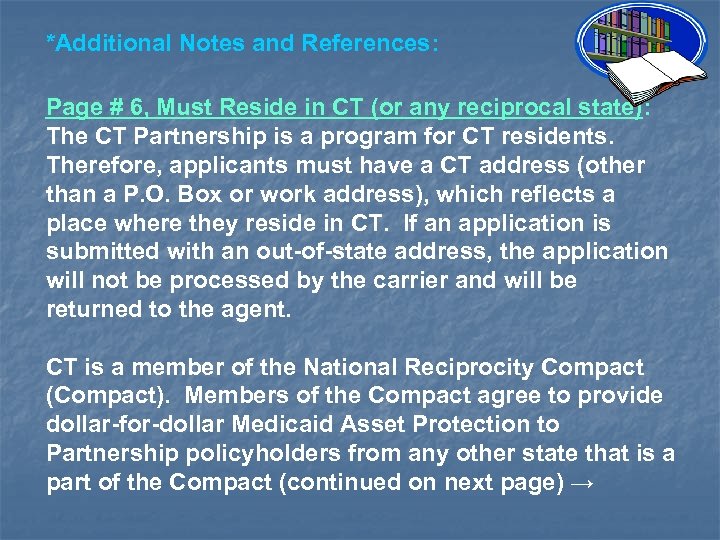 *Additional Notes and References: Page # 6, Must Reside in CT (or any reciprocal state): The CT Partnership is a program for CT residents. Therefore, applicants must have a CT address (other than a P. O. Box or work address), which reflects a place where they reside in CT. If an application is submitted with an out-of-state address, the application will not be processed by the carrier and will be returned to the agent. CT is a member of the National Reciprocity Compact (Compact). Members of the Compact agree to provide dollar-for-dollar Medicaid Asset Protection to Partnership policyholders from any other state that is a part of the Compact (continued on next page) →
*Additional Notes and References: Page # 6, Must Reside in CT (or any reciprocal state): The CT Partnership is a program for CT residents. Therefore, applicants must have a CT address (other than a P. O. Box or work address), which reflects a place where they reside in CT. If an application is submitted with an out-of-state address, the application will not be processed by the carrier and will be returned to the agent. CT is a member of the National Reciprocity Compact (Compact). Members of the Compact agree to provide dollar-for-dollar Medicaid Asset Protection to Partnership policyholders from any other state that is a part of the Compact (continued on next page) →
 *Additional Notes and References: Page # 6, Must Reside in CT (or any reciprocal state) cont’d: Therefore, CT Partnership policyholders will be able to receive Medicaid Asset Protection in any other state that at the time they apply to Medicaid that state and CT are members of the Compact, and vice versa for Partnership policyholders applying to CT’s Medicaid program. In addition, CT and Indiana have a separate reciprocal agreement to honor Medicaid Asset Protection. The reciprocal agreement means that CT Partnership policyholders who apply to Indiana’s Medicaid program will have dollar-for-dollar Medicaid Asset Protection recognized by the State of Indiana and vice versa for Indiana policyholders who apply to CT’s Medicaid Program.
*Additional Notes and References: Page # 6, Must Reside in CT (or any reciprocal state) cont’d: Therefore, CT Partnership policyholders will be able to receive Medicaid Asset Protection in any other state that at the time they apply to Medicaid that state and CT are members of the Compact, and vice versa for Partnership policyholders applying to CT’s Medicaid program. In addition, CT and Indiana have a separate reciprocal agreement to honor Medicaid Asset Protection. The reciprocal agreement means that CT Partnership policyholders who apply to Indiana’s Medicaid program will have dollar-for-dollar Medicaid Asset Protection recognized by the State of Indiana and vice versa for Indiana policyholders who apply to CT’s Medicaid Program.
 Additional Notes and References (cont’d): Page # 7, Use of Nursing Facility and Home Care: Congressional Budget Office based on Celia S. Gabrel, Characteristics of Elderly Nursing Home Current Residents and Discharges: Data from the 1997 National Nursing Home Survey, Advance Data no. 312 (Centers for Disease Control and Prevention, National Center for Health Statistics, April 25, 2000). CT Home Care Program for Elders: SFY 2010 Annual Report to the Legislature (July 2009 – June 2010), State of Connecticut, Department of Social Services, November 2011.
Additional Notes and References (cont’d): Page # 7, Use of Nursing Facility and Home Care: Congressional Budget Office based on Celia S. Gabrel, Characteristics of Elderly Nursing Home Current Residents and Discharges: Data from the 1997 National Nursing Home Survey, Advance Data no. 312 (Centers for Disease Control and Prevention, National Center for Health Statistics, April 25, 2000). CT Home Care Program for Elders: SFY 2010 Annual Report to the Legislature (July 2009 – June 2010), State of Connecticut, Department of Social Services, November 2011.


