e5d26583c38298d496d46fc16019cdbf.ppt
- Количество слайдов: 65
Libby Zion’s Lesson: Serotonin Syndrome and P 450 Drug Interactions Laurence J. Kinsella, MD, FAAN SSM St Clare Neuroscience Institute Saint Louis University
Disclosures n Dr Kinsella is a consultant for Therapath laboratories and Cross Country Education. n No relationships with pharmaceutical industry n Stock ownership in Passnet Air Ambulance n 2009 Teacher of the Year, US Psychiatric Congress
You Should Know mechanism of drug-drug interactions (DDI) common DDIs in neurologic practice how to predict and manage interactions
Question 1 In 1984, a young woman died from a fatal drug interaction (DDI). Her death was blamed on poor judgment of sleep-deprived house staff, and led to the 80 hour work week restriction for residents. What was the DDI and the name of the syndrome? a. b. c. d. Haloperidol and Chlorpromazine - Neuroleptic malignant Syndrome Penicillamine and Gentamicin - Myasthenic Crisis Phenelzine and meperidine - Serotonin Syndrome Carbamazepine and acetaminophen - Stevens Johnson Syndrome
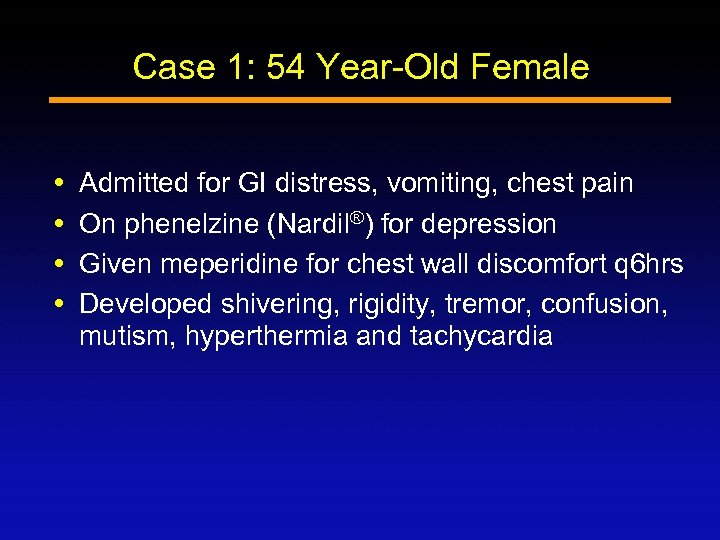
Case 1: 54 Year-Old Female Admitted for GI distress, vomiting, chest pain On phenelzine (Nardil®) for depression Given meperidine for chest wall discomfort q 6 hrs Developed shivering, rigidity, tremor, confusion, mutism, hyperthermia and tachycardia

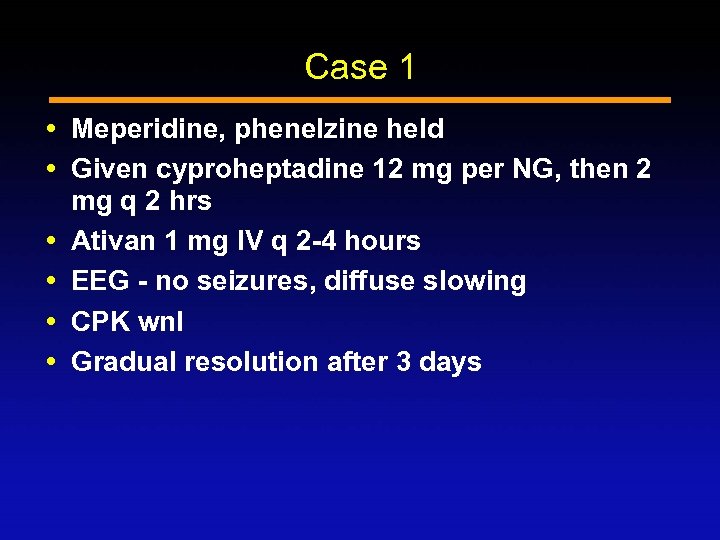
Case 1 Meperidine, phenelzine held Given cyproheptadine 12 mg per NG, then 2 mg q 2 hrs Ativan 1 mg IV q 2 -4 hours EEG - no seizures, diffuse slowing CPK wnl Gradual resolution after 3 days
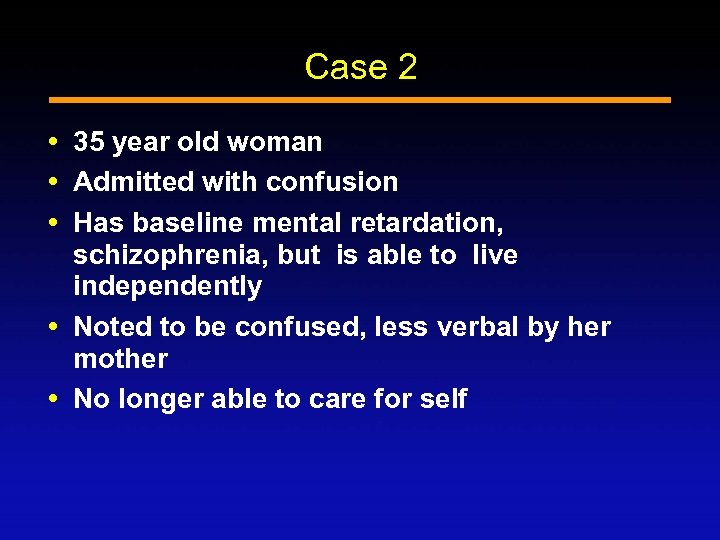
Case 2 35 year old woman Admitted with confusion Has baseline mental retardation, schizophrenia, but is able to live independently Noted to be confused, less verbal by her mother No longer able to care for self
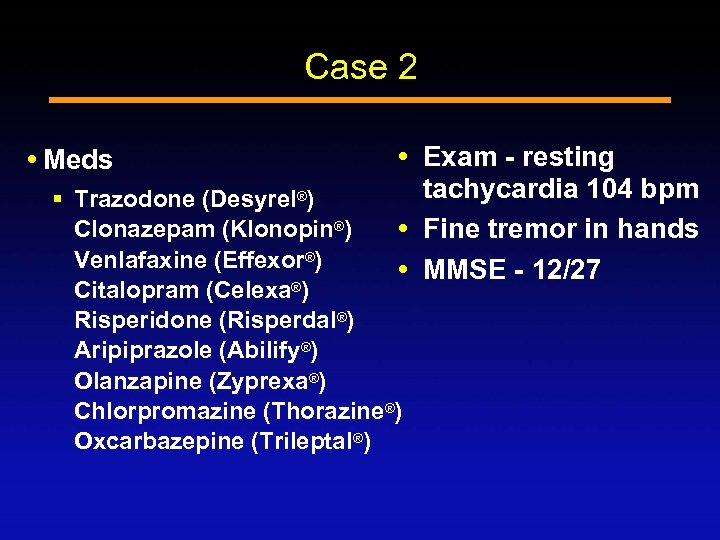
Case 2 Meds Exam - resting tachycardia 104 bpm Fine tremor in hands MMSE - 12/27 § Trazodone (Desyrel®) Clonazepam (Klonopin®) Venlafaxine (Effexor®) Citalopram (Celexa®) Risperidone (Risperdal®) Aripiprazole (Abilify®) Olanzapine (Zyprexa®) Chlorpromazine (Thorazine®) Oxcarbazepine (Trileptal®)
Case 2 Confusion and tremulousness resolved over 3 days when holding just 3 meds § Citalopram, venlafaxine and trazodone Mental status returned to baseline MMSE - 24/30 HR 81
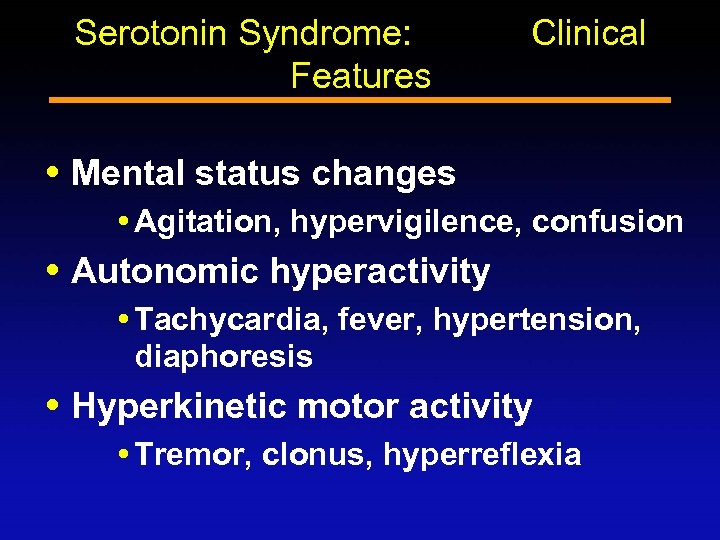
Serotonin Syndrome: Features Clinical Mental status changes Agitation, hypervigilence, confusion Autonomic hyperactivity Tachycardia, fever, hypertension, diaphoresis Hyperkinetic motor activity Tremor, clonus, hyperreflexia
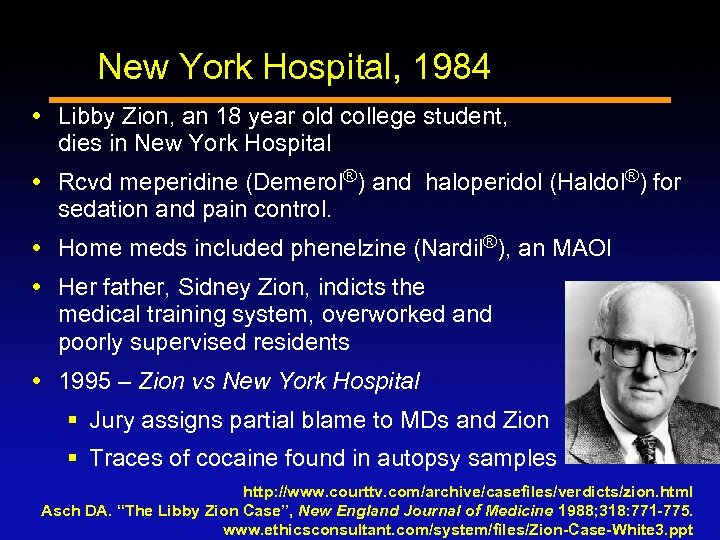
New York Hospital, 1984 Libby Zion, an 18 year old college student, dies in New York Hospital Rcvd meperidine (Demerol®) and haloperidol (Haldol®) for sedation and pain control. Home meds included phenelzine (Nardil®), an MAOI Her father, Sidney Zion, indicts the medical training system, overworked and poorly supervised residents 1995 – Zion vs New York Hospital § Jury assigns partial blame to MDs and Zion § Traces of cocaine found in autopsy samples http: //www. courttv. com/archive/casefiles/verdicts/zion. html Asch DA. “The Libby Zion Case”, New England Journal of Medicine 1988; 318: 771 -775. www. ethicsconsultant. com/system/files/Zion-Case-White 3. ppt
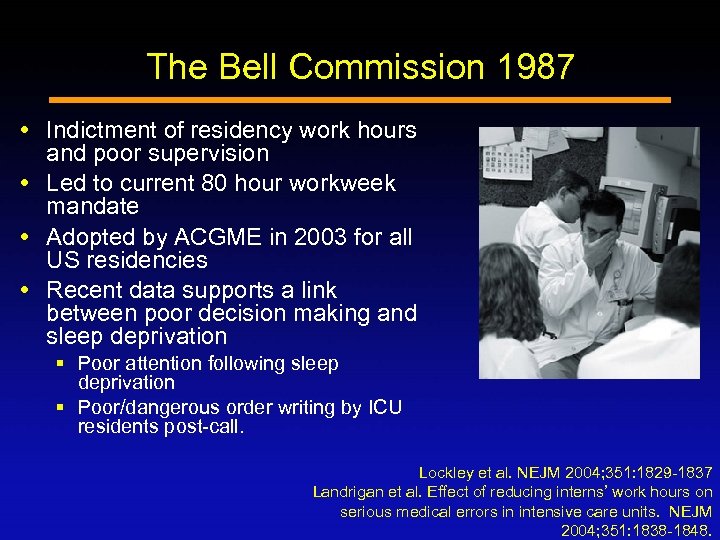
The Bell Commission 1987 Indictment of residency work hours and poor supervision Led to current 80 hour workweek mandate Adopted by ACGME in 2003 for all US residencies Recent data supports a link between poor decision making and sleep deprivation § Poor attention following sleep deprivation § Poor/dangerous order writing by ICU residents post-call. Lockley et al. NEJM 2004; 351: 1829 -1837 Landrigan et al. Effect of reducing interns’ work hours on serious medical errors in intensive care units. NEJM 2004; 351: 1838 -1848.
Libby Zion’s Lesson Would today’s well-rested resident have recognized the problem that killed Libby Zion?
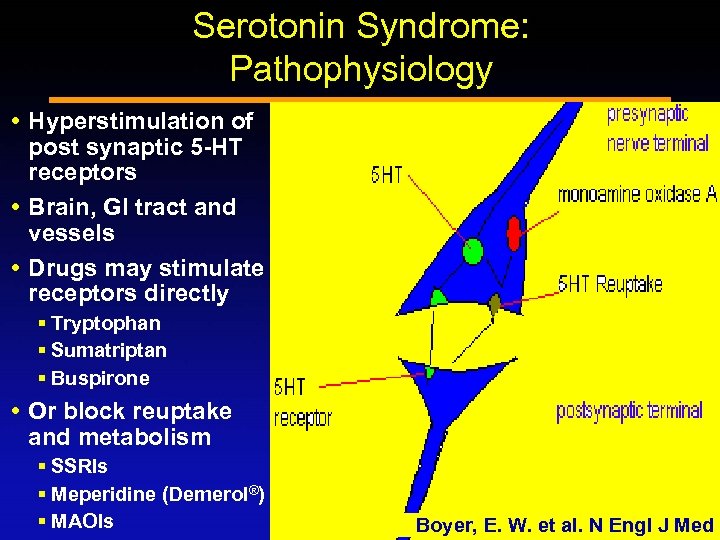
Serotonin Syndrome: Pathophysiology Hyperstimulation of post synaptic 5 -HT receptors Brain, GI tract and vessels Drugs may stimulate receptors directly § Tryptophan § Sumatriptan § Buspirone Or block reuptake and metabolism § SSRIs § Meperidine (Demerol®) § MAOIs Boyer, E. W. et al. N Engl J Med
Serotonin Syndrome 1960: tryptophan and MAOIs 1984: Libby Zion - Demerol and phenelzine (and cocaine? ) 15% incidence in patients overdosing SSRIs Toxic Exposure surveillance system 2002 § 7349 patients reported in 2002 § 93 deaths § 0. 4 cases/1, 000 patient-months on SSRIs Oates JA, Neurology, 1960; Asch DA, NEJM 1988
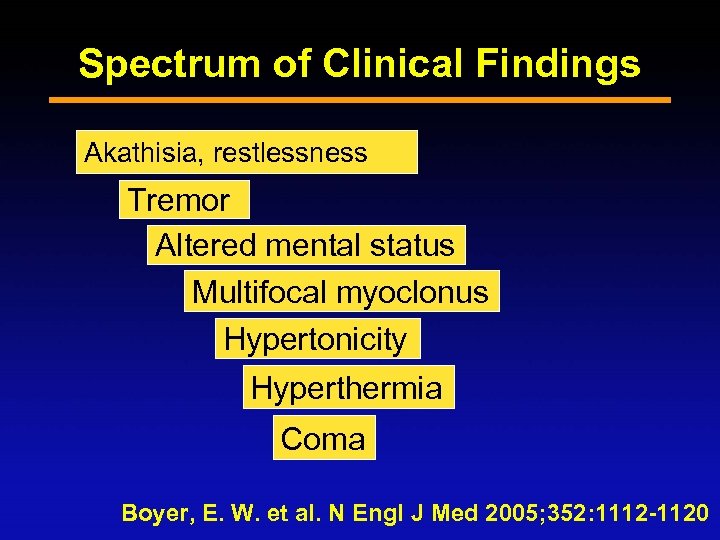
Spectrum of Clinical Findings Akathisia, restlessness Tremor Altered mental status Multifocal myoclonus Hypertonicity Hyperthermia Coma Boyer, E. W. et al. N Engl J Med 2005; 352: 1112 -1120
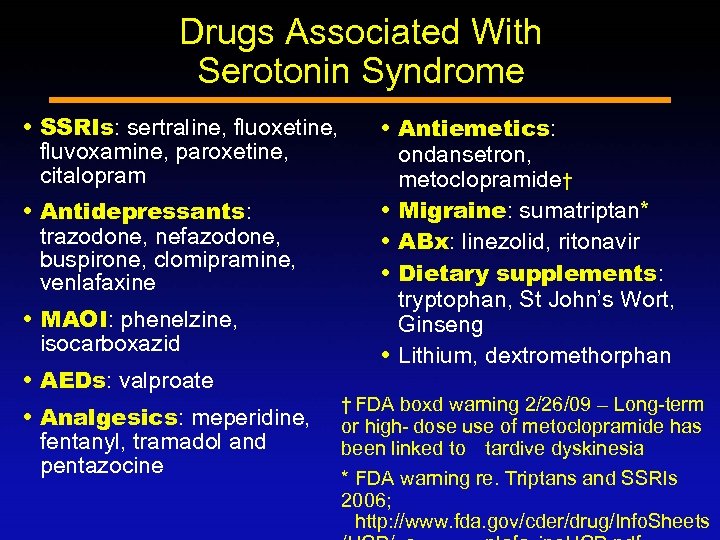
Drugs Associated With Serotonin Syndrome SSRIs: sertraline, fluoxetine, fluvoxamine, paroxetine, citalopram Antidepressants: trazodone, nefazodone, buspirone, clomipramine, venlafaxine MAOI: phenelzine, isocarboxazid AEDs: valproate Analgesics: meperidine, fentanyl, tramadol and pentazocine Antiemetics: ondansetron, metoclopramide† Migraine: sumatriptan* ABx: linezolid, ritonavir Dietary supplements: tryptophan, St John’s Wort, Ginseng Lithium, dextromethorphan † FDA boxd warning 2/26/09 – Long-term or high- dose use of metoclopramide has been linked to tardive dyskinesia * FDA warning re. Triptans and SSRIs 2006; http: //www. fda. gov/cder/drug/Info. Sheets
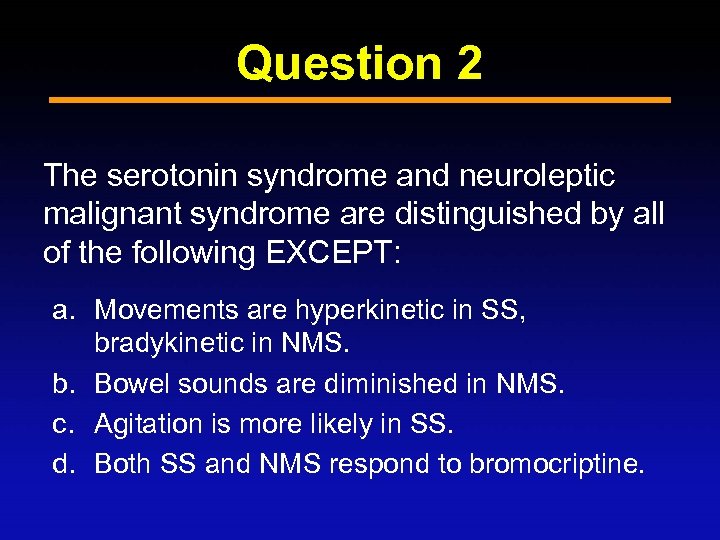
Question 2 The serotonin syndrome and neuroleptic malignant syndrome are distinguished by all of the following EXCEPT: a. Movements are hyperkinetic in SS, bradykinetic in NMS. b. Bowel sounds are diminished in NMS. c. Agitation is more likely in SS. d. Both SS and NMS respond to bromocriptine.
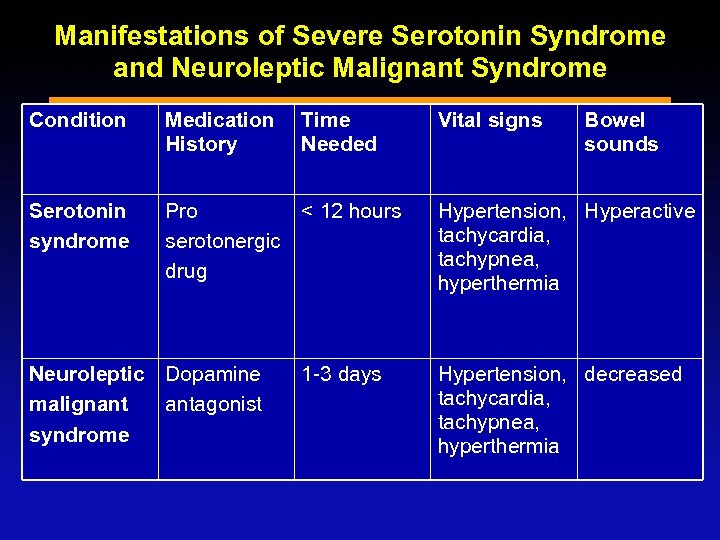
Manifestations of Severe Serotonin Syndrome and Neuroleptic Malignant Syndrome Condition Medication History Serotonin syndrome Pro < 12 hours serotonergic drug Neuroleptic Dopamine malignant antagonist syndrome Time Needed 1 -3 days Vital signs Bowel sounds Hypertension, Hyperactive tachycardia, tachypnea, hyperthermia Hypertension, decreased tachycardia, tachypnea, hyperthermia
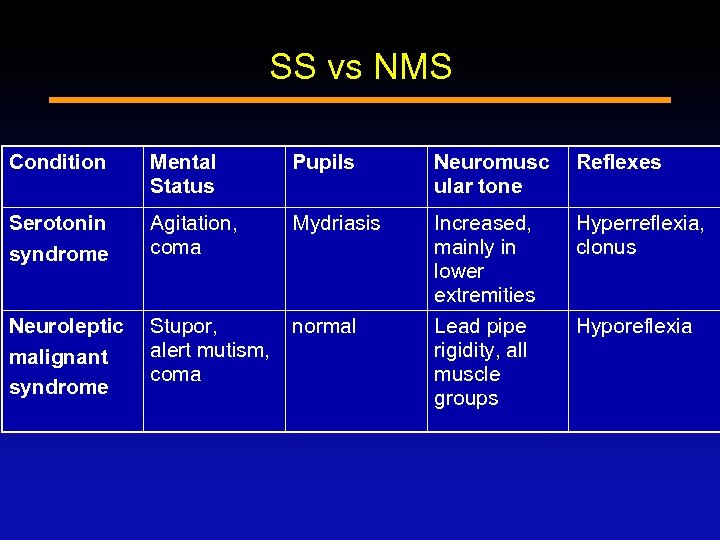
SS vs NMS Condition Mental Status Pupils Neuromusc ular tone Reflexes Serotonin syndrome Agitation, coma Mydriasis Hyperreflexia, clonus Neuroleptic malignant syndrome Stupor, alert mutism, coma normal Increased, mainly in lower extremities Lead pipe rigidity, all muscle groups Hyporeflexia
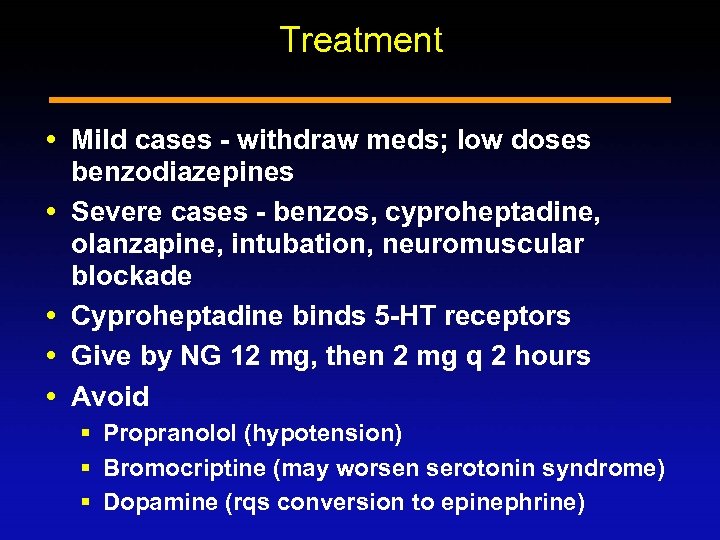
Treatment Mild cases - withdraw meds; low doses benzodiazepines Severe cases - benzos, cyproheptadine, olanzapine, intubation, neuromuscular blockade Cyproheptadine binds 5 -HT receptors Give by NG 12 mg, then 2 mg q 2 hours Avoid § Propranolol (hypotension) § Bromocriptine (may worsen serotonin syndrome) § Dopamine (rqs conversion to epinephrine)
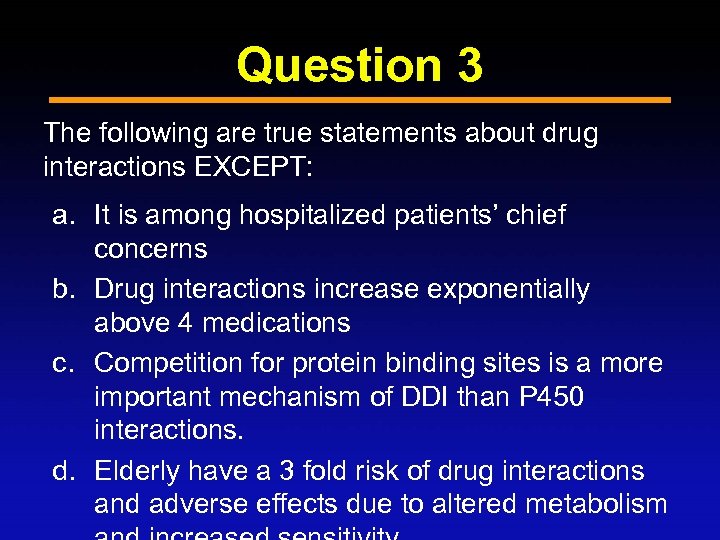
Question 3 The following are true statements about drug interactions EXCEPT: a. It is among hospitalized patients’ chief concerns b. Drug interactions increase exponentially above 4 medications c. Competition for protein binding sites is a more important mechanism of DDI than P 450 interactions. d. Elderly have a 3 fold risk of drug interactions and adverse effects due to altered metabolism
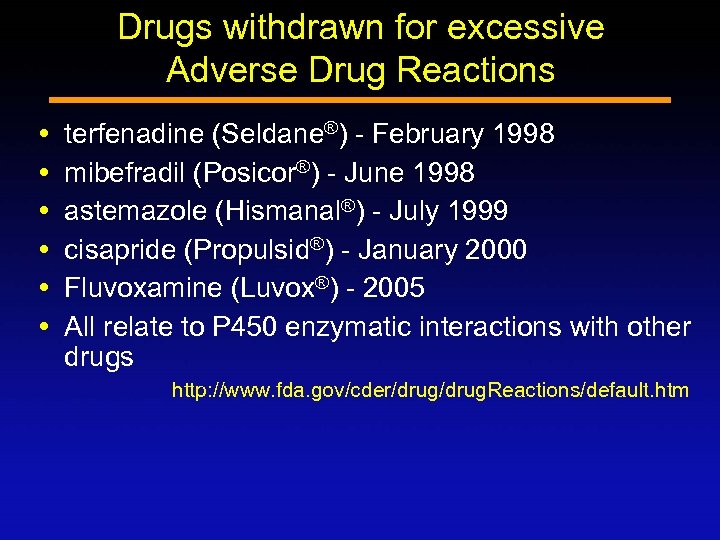
Drugs withdrawn for excessive Adverse Drug Reactions terfenadine (Seldane®) - February 1998 mibefradil (Posicor®) - June 1998 astemazole (Hismanal®) - July 1999 cisapride (Propulsid®) - January 2000 Fluvoxamine (Luvox®) - 2005 All relate to P 450 enzymatic interactions with other drugs http: //www. fda. gov/cder/drug. Reactions/default. htm
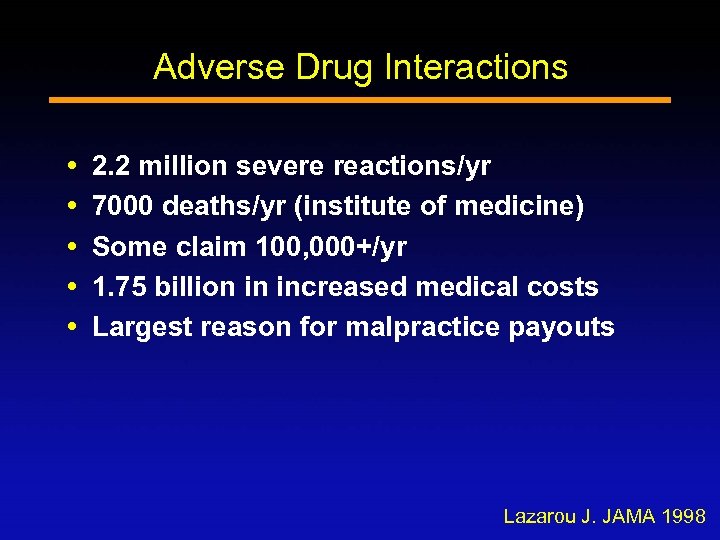
Adverse Drug Interactions 2. 2 million severe reactions/yr 7000 deaths/yr (institute of medicine) Some claim 100, 000+/yr 1. 75 billion in increased medical costs Largest reason for malpractice payouts Lazarou J. JAMA 1998
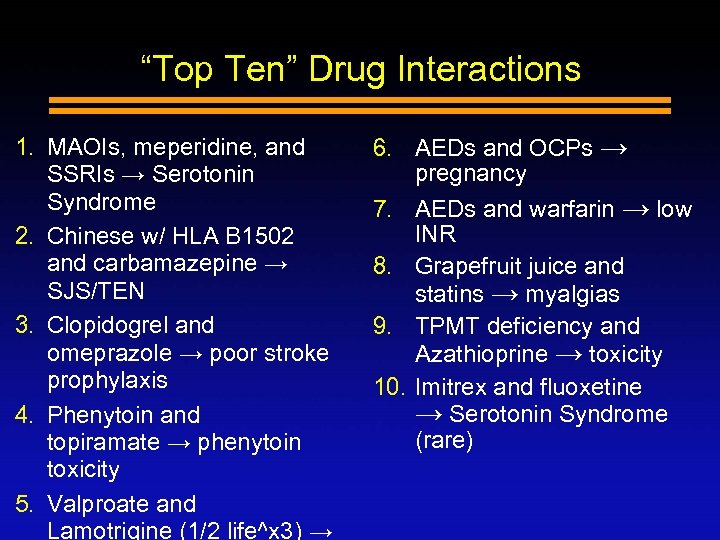
“Top Ten” Drug Interactions 1. MAOIs, meperidine, and SSRIs → Serotonin Syndrome 2. Chinese w/ HLA B 1502 and carbamazepine → SJS/TEN 3. Clopidogrel and omeprazole → poor stroke prophylaxis 4. Phenytoin and topiramate → phenytoin toxicity 5. Valproate and Lamotrigine (1/2 life^x 3) → 6. AEDs and OCPs → pregnancy 7. AEDs and warfarin → low INR 8. Grapefruit juice and statins → myalgias 9. TPMT deficiency and Azathioprine → toxicity 10. Imitrex and fluoxetine → Serotonin Syndrome (rare)
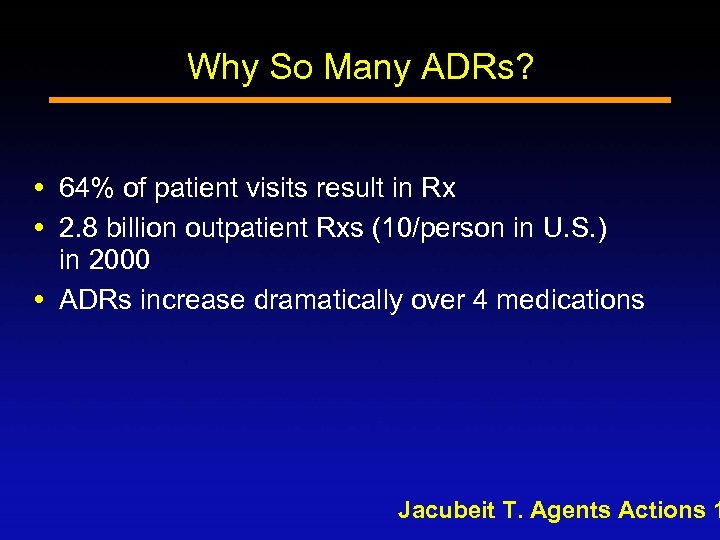
Why So Many ADRs? 64% of patient visits result in Rx 2. 8 billion outpatient Rxs (10/person in U. S. ) in 2000 ADRs increase dramatically over 4 medications Jacubeit T. Agents Actions 1
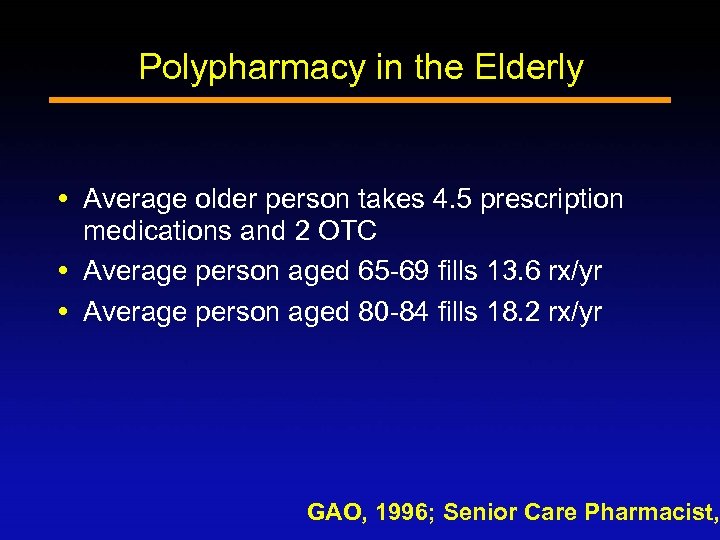
Polypharmacy in the Elderly Average older person takes 4. 5 prescription medications and 2 OTC Average person aged 65 -69 fills 13. 6 rx/yr Average person aged 80 -84 fills 18. 2 rx/yr GAO, 1996; Senior Care Pharmacist,
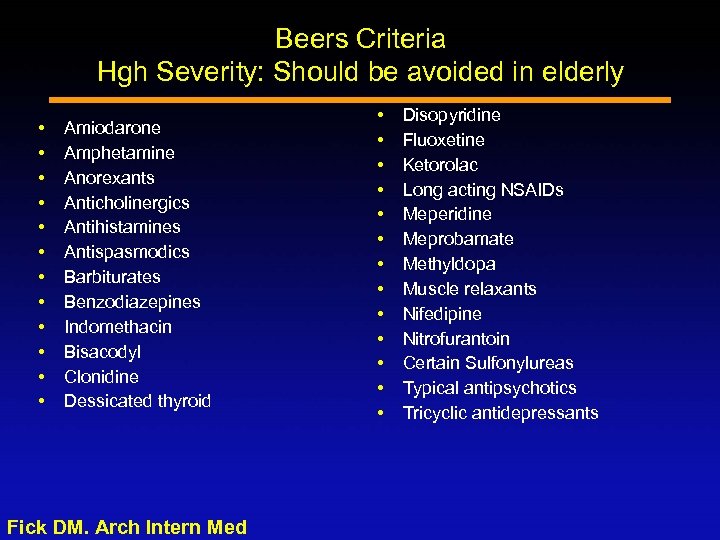
Beers Criteria Hgh Severity: Should be avoided in elderly Amiodarone Amphetamine Anorexants Anticholinergics Antihistamines Antispasmodics Barbiturates Benzodiazepines Indomethacin Bisacodyl Clonidine Dessicated thyroid Fick DM. Arch Intern Med Disopyridine Fluoxetine Ketorolac Long acting NSAIDs Meperidine Meprobamate Methyldopa Muscle relaxants Nifedipine Nitrofurantoin Certain Sulfonylureas Typical antipsychotics Tricyclic antidepressants
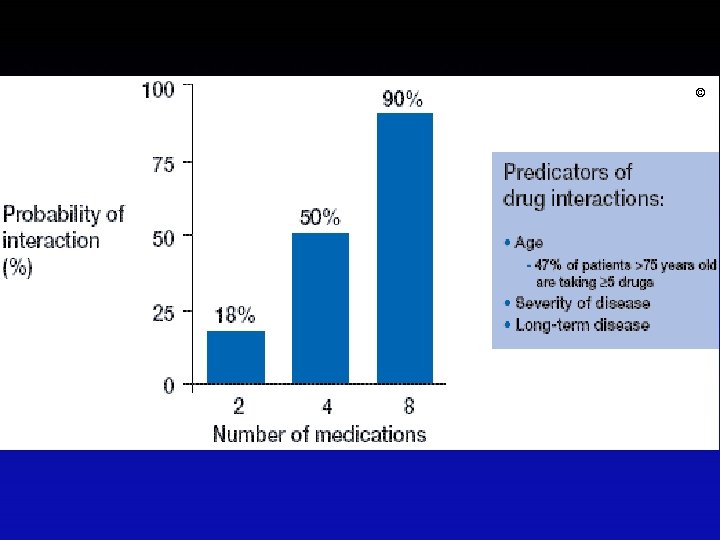
©
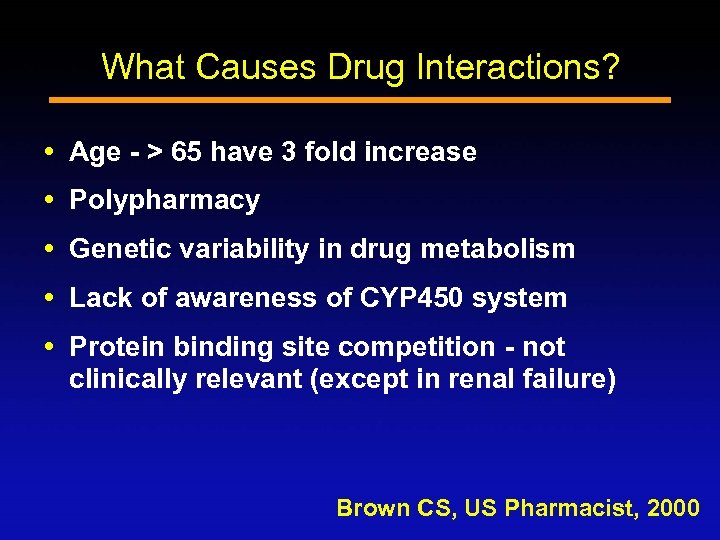
What Causes Drug Interactions? Age - > 65 have 3 fold increase Polypharmacy Genetic variability in drug metabolism Lack of awareness of CYP 450 system Protein binding site competition - not clinically relevant (except in renal failure) Brown CS, US Pharmacist, 2000
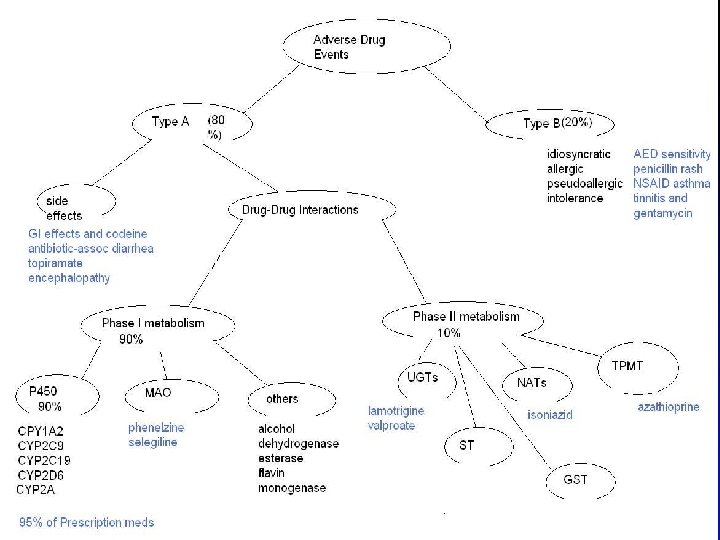
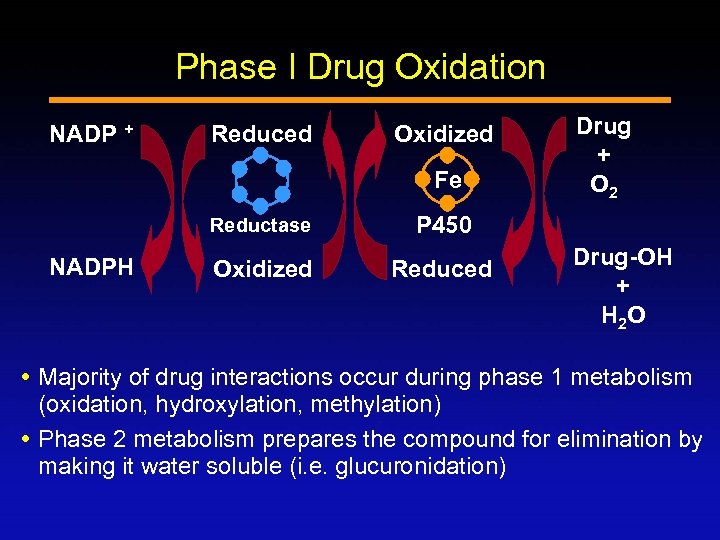
Phase I Drug Oxidation NADP + Reduced Oxidized Fe Reductase NADPH P 450 Oxidized Reduced Drug + O 2 Drug-OH + H 2 O Majority of drug interactions occur during phase 1 metabolism (oxidation, hydroxylation, methylation) Phase 2 metabolism prepares the compound for elimination by making it water soluble (i. e. glucuronidation)
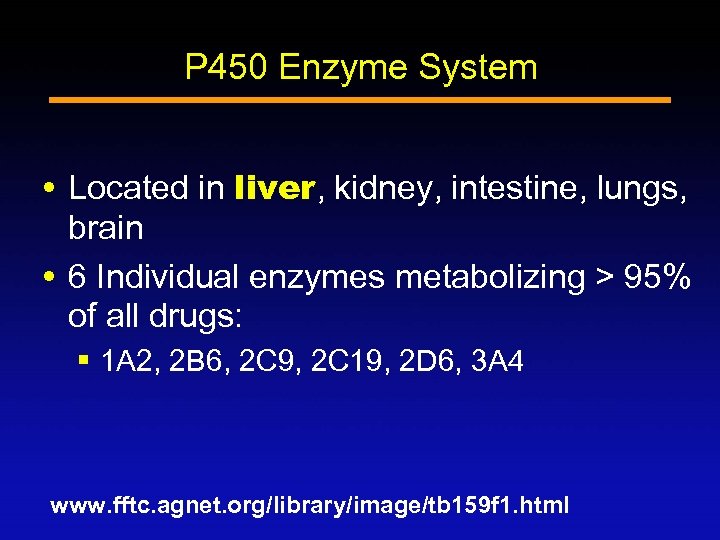
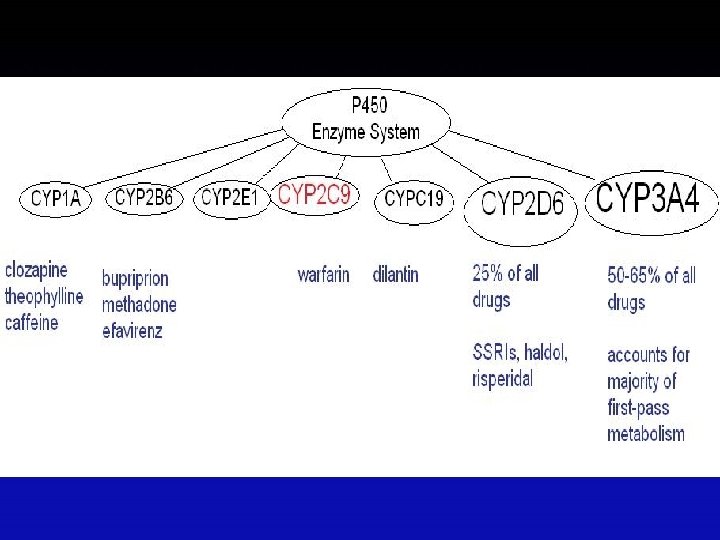
P 450 Enzyme System Located in liver, kidney, intestine, lungs, brain 6 Individual enzymes metabolizing > 95% of all drugs: § 1 A 2, 2 B 6, 2 C 9, 2 C 19, 2 D 6, 3 A 4 www. fftc. agnet. org/library/image/tb 159 f 1. html
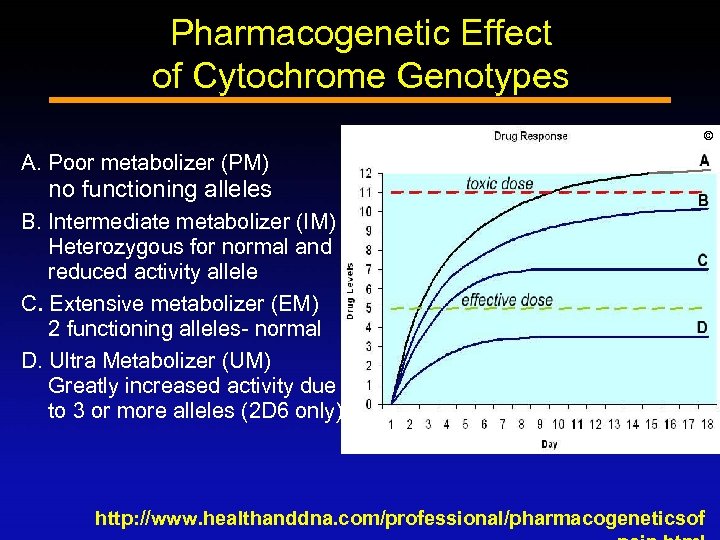
Pharmacogenetic Effect of Cytochrome Genotypes © A. Poor metabolizer (PM) no functioning alleles B. Intermediate metabolizer (IM) Heterozygous for normal and reduced activity allele C. Extensive metabolizer (EM) 2 functioning alleles- normal D. Ultra Metabolizer (UM) Greatly increased activity due to 3 or more alleles (2 D 6 only) http: //www. healthanddna. com/professional/pharmacogeneticsof
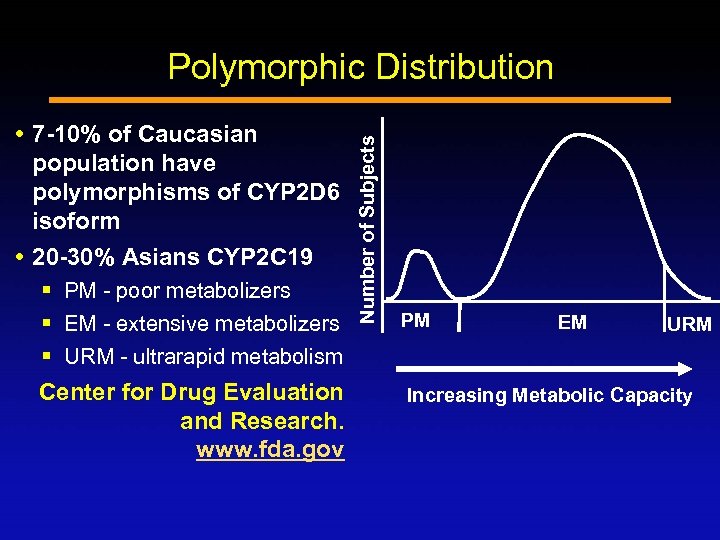
7 -10% of Caucasian population have polymorphisms of CYP 2 D 6 isoform 20 -30% Asians CYP 2 C 19 § PM - poor metabolizers § EM - extensive metabolizers § URM - ultrarapid metabolism Center for Drug Evaluation and Research. www. fda. gov Number of Subjects Polymorphic Distribution PM EM URM Increasing Metabolic Capacity
Question 4 Genetic variants increase the likelihood of drug toxicity. Which of the following drugs have clinically relevant genetic variations in metabolism? a) b) c) d) e) Warfarin Clopidogrel Carbamazepine Azathioprine All of the above
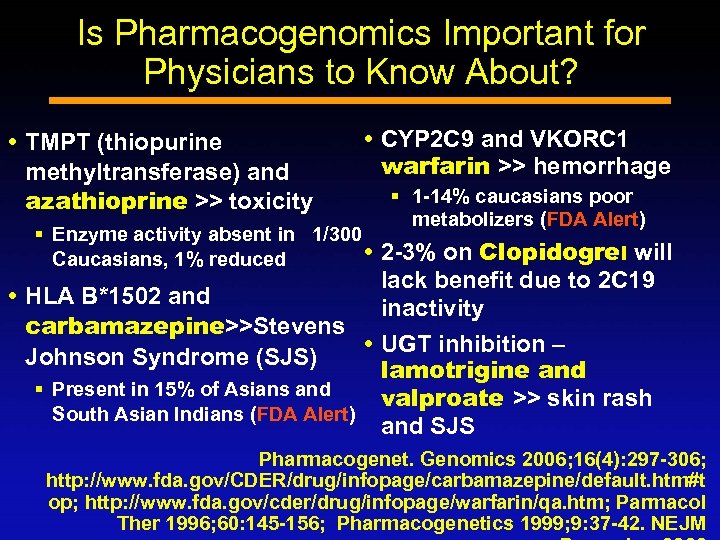
Is Pharmacogenomics Important for Physicians to Know About? TMPT (thiopurine methyltransferase) and azathioprine >> toxicity CYP 2 C 9 and VKORC 1 warfarin >> hemorrhage § 1 -14% caucasians poor metabolizers (FDA Alert) § Enzyme activity absent in 1/300 2 -3% on Clopidogrel will Caucasians, 1% reduced lack benefit due to 2 C 19 HLA B*1502 and inactivity carbamazepine>>Stevens UGT inhibition – Johnson Syndrome (SJS) lamotrigine and § Present in 15% of Asians and valproate >> skin rash South Asian Indians (FDA Alert) and SJS Pharmacogenet. Genomics 2006; 16(4): 297 -306; http: //www. fda. gov/CDER/drug/infopage/carbamazepine/default. htm#t op; http: //www. fda. gov/cder/drug/infopage/warfarin/qa. htm; Parmacol Ther 1996; 60: 145 -156; Pharmacogenetics 1999; 9: 37 -42. NEJM
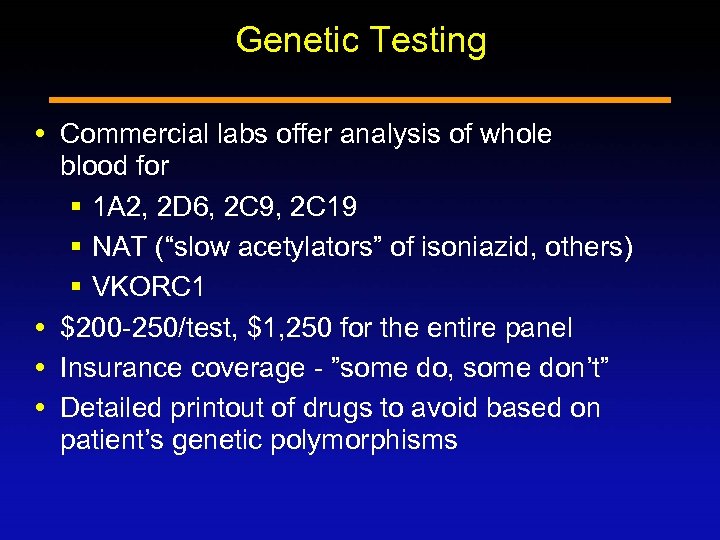
Genetic Testing Commercial labs offer analysis of whole blood for § 1 A 2, 2 D 6, 2 C 9, 2 C 19 § NAT (“slow acetylators” of isoniazid, others) § VKORC 1 $200 -250/test, $1, 250 for the entire panel Insurance coverage - ”some do, some don’t” Detailed printout of drugs to avoid based on patient’s genetic polymorphisms
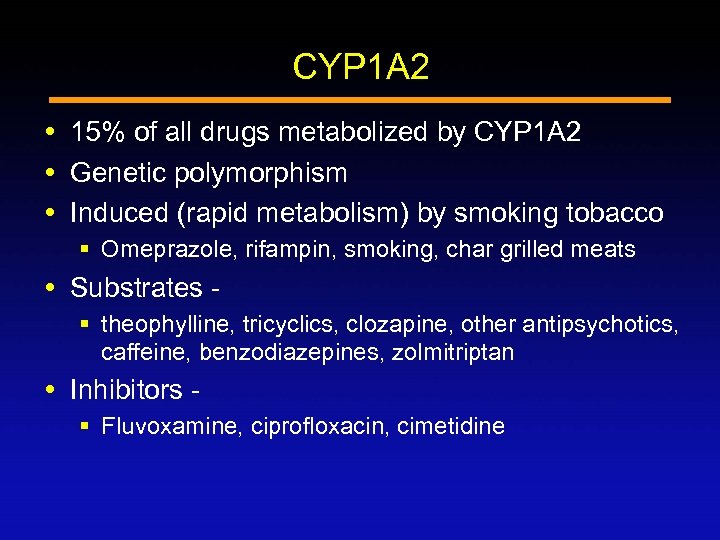
CYP 1 A 2 15% of all drugs metabolized by CYP 1 A 2 Genetic polymorphism Induced (rapid metabolism) by smoking tobacco § Omeprazole, rifampin, smoking, char grilled meats Substrates § theophylline, tricyclics, clozapine, other antipsychotics, caffeine, benzodiazepines, zolmitriptan Inhibitors § Fluvoxamine, ciprofloxacin, cimetidine
75 Year-Old Male With Seizures Admitted with COPD exacerbation Meds; theophylline 300 mg BID Begun on levaquin for pneumonia Developed confusion, ataxia, over next two days Seizure, encephalopathy 3 days after admission What caused the seizure?
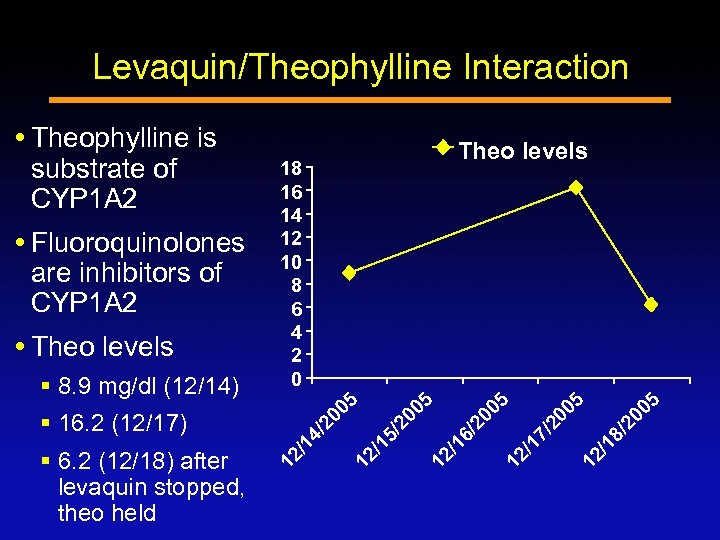
Levaquin/Theophylline Interaction /2 00 5 12 /1 8 /2 00 5 12 /1 7 § 6. 2 (12/18) after levaquin stopped, theo held 12 /1 6 § 16. 2 (12/17) /2 00 5 § 8. 9 mg/dl (12/14) 12 /1 5 Theo levels 18 16 14 12 10 8 6 4 2 0 /2 00 5 Fluoroquinolones are inhibitors of CYP 1 A 2 Theo levels 12 /1 4 Theophylline is substrate of CYP 1 A 2
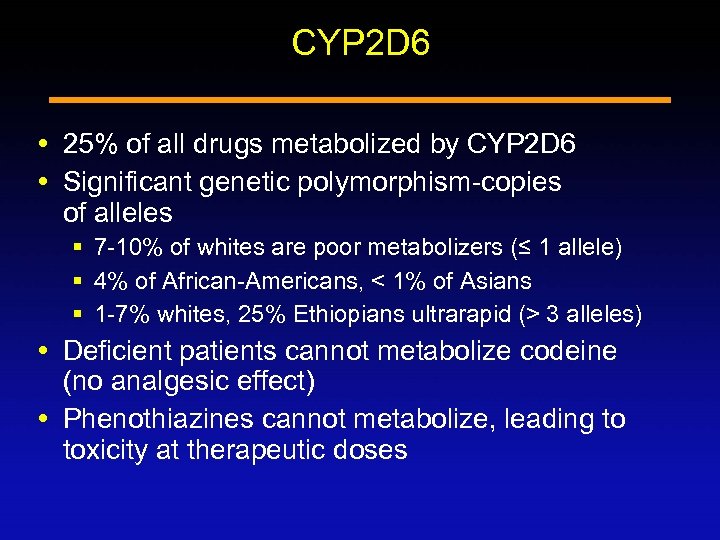
CYP 2 D 6 25% of all drugs metabolized by CYP 2 D 6 Significant genetic polymorphism-copies of alleles § 7 -10% of whites are poor metabolizers (≤ 1 allele) § 4% of African-Americans, < 1% of Asians § 1 -7% whites, 25% Ethiopians ultrarapid (> 3 alleles) Deficient patients cannot metabolize codeine (no analgesic effect) Phenothiazines cannot metabolize, leading to toxicity at therapeutic doses
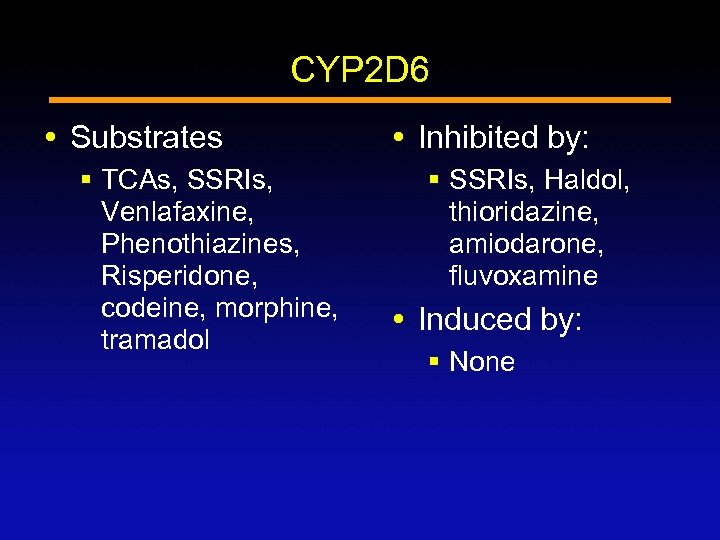
CYP 2 D 6 Substrates § TCAs, SSRIs, Venlafaxine, Phenothiazines, Risperidone, codeine, morphine, tramadol Inhibited by: § SSRIs, Haldol, thioridazine, amiodarone, fluvoxamine Induced by: § None
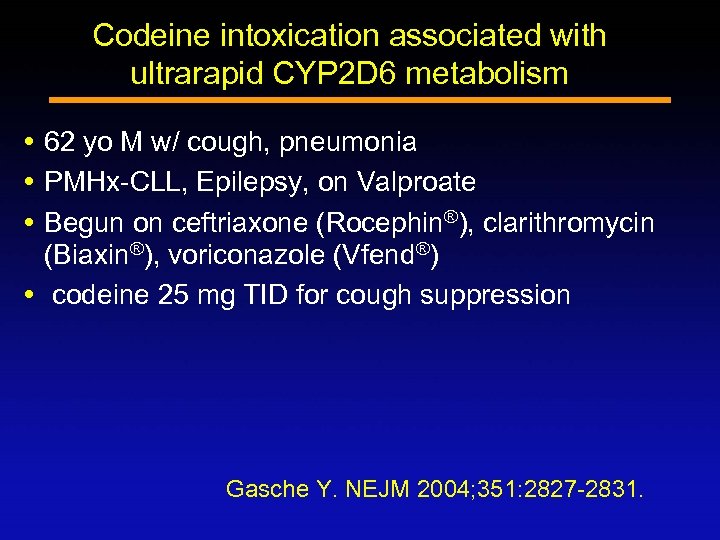
Codeine intoxication associated with ultrarapid CYP 2 D 6 metabolism 62 yo M w/ cough, pneumonia PMHx-CLL, Epilepsy, on Valproate Begun on ceftriaxone (Rocephin®), clarithromycin (Biaxin®), voriconazole (Vfend®) codeine 25 mg TID for cough suppression Gasche Y. NEJM 2004; 351: 2827 -2831.
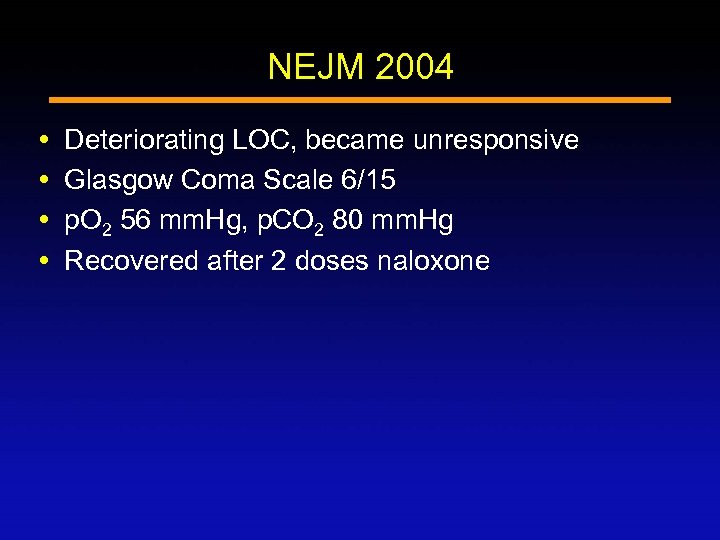
NEJM 2004 Deteriorating LOC, became unresponsive Glasgow Coma Scale 6/15 p. O 2 56 mm. Hg, p. CO 2 80 mm. Hg Recovered after 2 doses naloxone
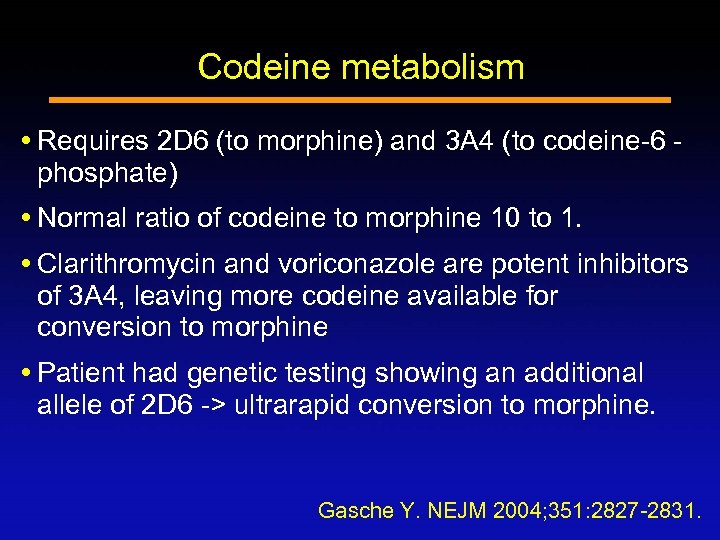
Codeine metabolism Requires 2 D 6 (to morphine) and 3 A 4 (to codeine-6 phosphate) Normal ratio of codeine to morphine 10 to 1. Clarithromycin and voriconazole are potent inhibitors of 3 A 4, leaving more codeine available for conversion to morphine Patient had genetic testing showing an additional allele of 2 D 6 -> ultrarapid conversion to morphine. Gasche Y. NEJM 2004; 351: 2827 -2831.
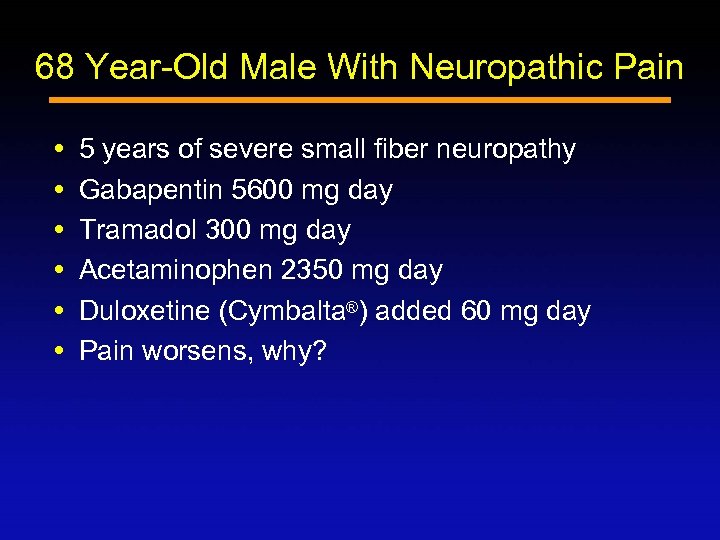
68 Year-Old Male With Neuropathic Pain 5 years of severe small fiber neuropathy Gabapentin 5600 mg day Tramadol 300 mg day Acetaminophen 2350 mg day Duloxetine (Cymbalta®) added 60 mg day Pain worsens, why?
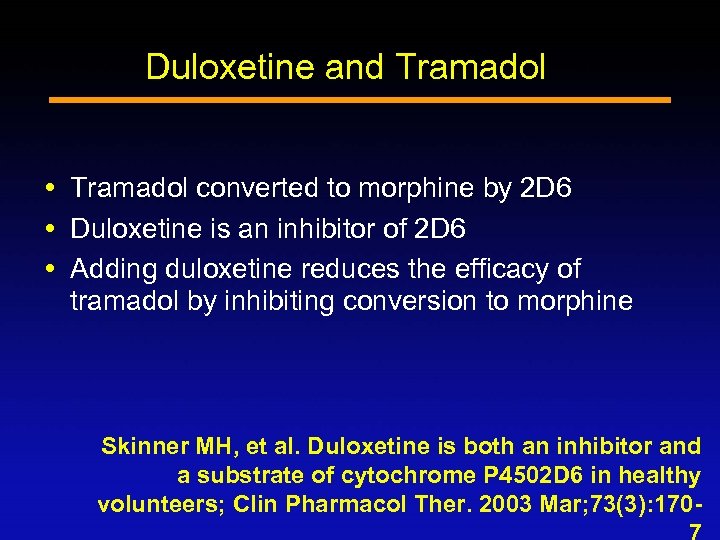
Duloxetine and Tramadol converted to morphine by 2 D 6 Duloxetine is an inhibitor of 2 D 6 Adding duloxetine reduces the efficacy of tramadol by inhibiting conversion to morphine Skinner MH, et al. Duloxetine is both an inhibitor and a substrate of cytochrome P 4502 D 6 in healthy volunteers; Clin Pharmacol Ther. 2003 Mar; 73(3): 170 -
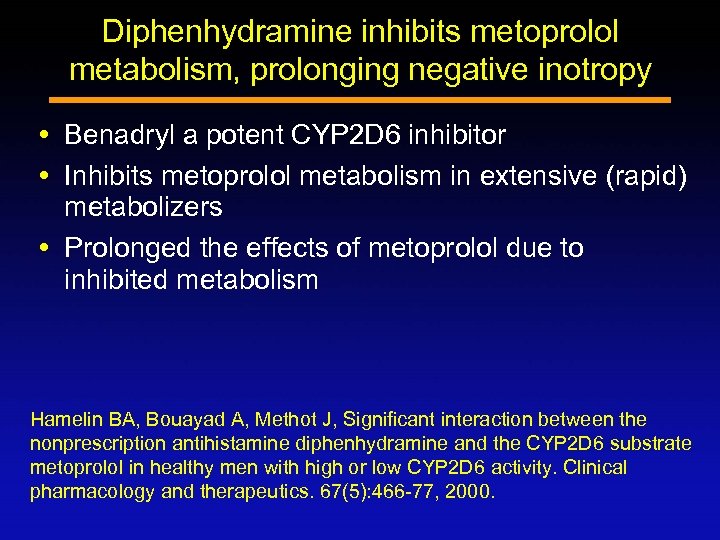
Diphenhydramine inhibits metoprolol metabolism, prolonging negative inotropy Benadryl a potent CYP 2 D 6 inhibitor Inhibits metoprolol metabolism in extensive (rapid) metabolizers Prolonged the effects of metoprolol due to inhibited metabolism Hamelin BA, Bouayad A, Methot J, Significant interaction between the nonprescription antihistamine diphenhydramine and the CYP 2 D 6 substrate metoprolol in healthy men with high or low CYP 2 D 6 activity. Clinical pharmacology and therapeutics. 67(5): 466 -77, 2000.
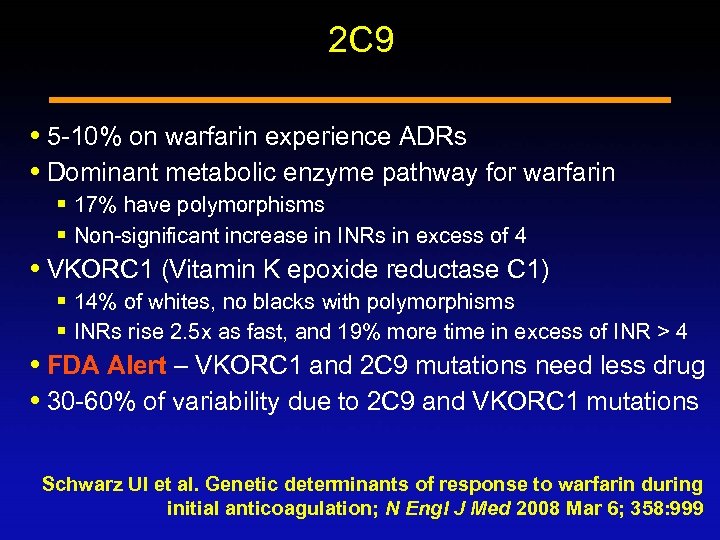
2 C 9 5 -10% on warfarin experience ADRs Dominant metabolic enzyme pathway for warfarin § 17% have polymorphisms § Non-significant increase in INRs in excess of 4 VKORC 1 (Vitamin K epoxide reductase C 1) § 14% of whites, no blacks with polymorphisms § INRs rise 2. 5 x as fast, and 19% more time in excess of INR > 4 FDA Alert – VKORC 1 and 2 C 9 mutations need less drug 30 -60% of variability due to 2 C 9 and VKORC 1 mutations Schwarz UI et al. Genetic determinants of response to warfarin during initial anticoagulation; N Engl J Med 2008 Mar 6; 358: 999
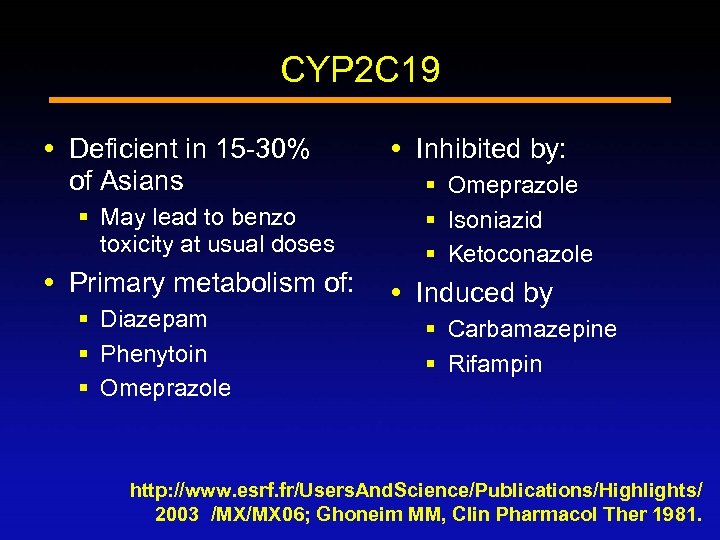
CYP 2 C 19 Deficient in 15 -30% of Asians § May lead to benzo toxicity at usual doses Primary metabolism of: § Diazepam § Phenytoin § Omeprazole Inhibited by: § Omeprazole § Isoniazid § Ketoconazole Induced by § Carbamazepine § Rifampin http: //www. esrf. fr/Users. And. Science/Publications/Highlights/ 2003 /MX/MX 06; Ghoneim MM, Clin Pharmacol Ther 1981.
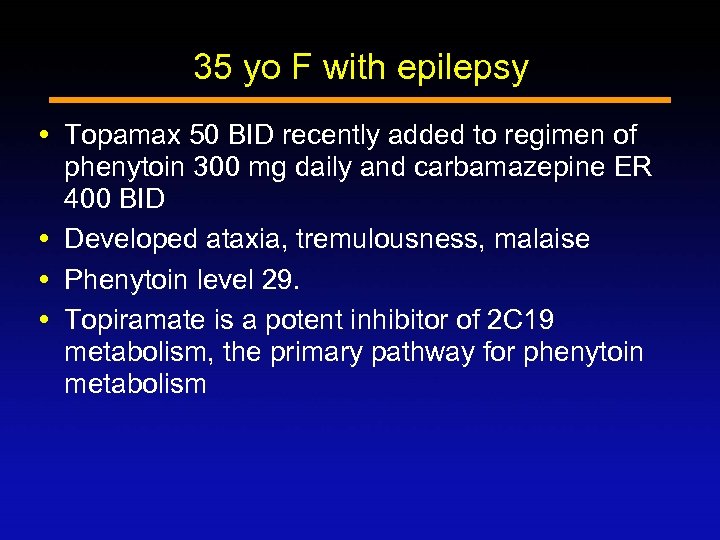
35 yo F with epilepsy Topamax 50 BID recently added to regimen of phenytoin 300 mg daily and carbamazepine ER 400 BID Developed ataxia, tremulousness, malaise Phenytoin level 29. Topiramate is a potent inhibitor of 2 C 19 metabolism, the primary pathway for phenytoin metabolism
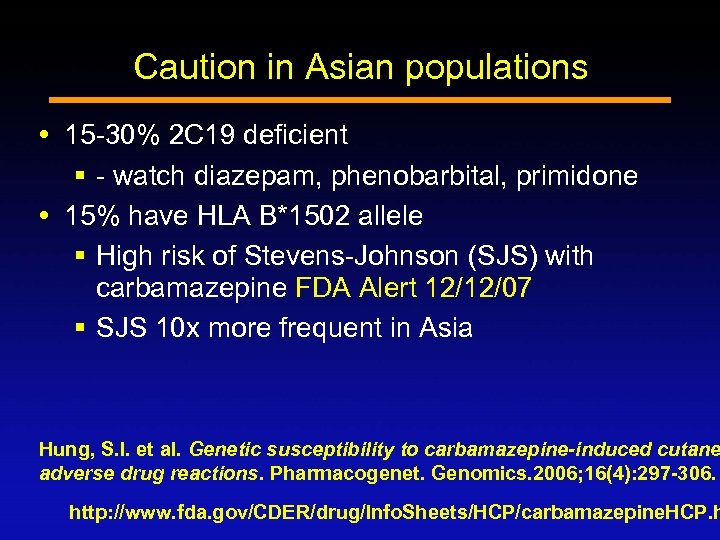
Caution in Asian populations 15 -30% 2 C 19 deficient § - watch diazepam, phenobarbital, primidone 15% have HLA B*1502 allele § High risk of Stevens-Johnson (SJS) with carbamazepine FDA Alert 12/12/07 § SJS 10 x more frequent in Asia Hung, S. I. et al. Genetic susceptibility to carbamazepine-induced cutane adverse drug reactions. Pharmacogenet. Genomics. 2006; 16(4): 297 -306. http: //www. fda. gov/CDER/drug/Info. Sheets/HCP/carbamazepine. HCP. h
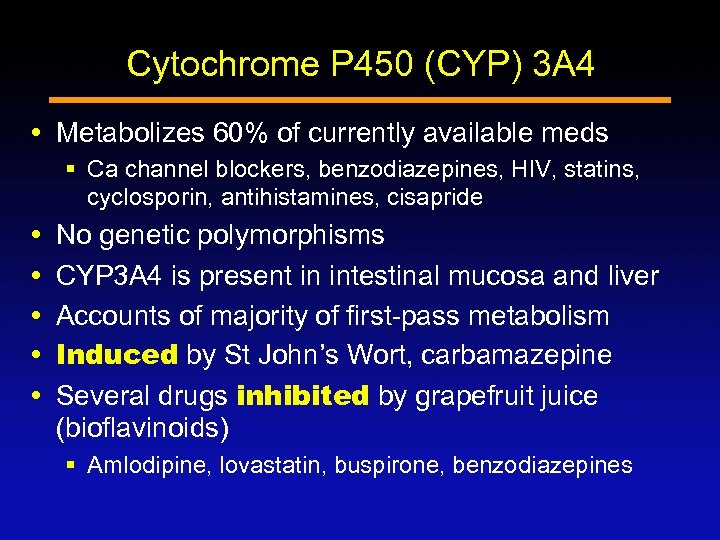
Cytochrome P 450 (CYP) 3 A 4 Metabolizes 60% of currently available meds § Ca channel blockers, benzodiazepines, HIV, statins, cyclosporin, antihistamines, cisapride No genetic polymorphisms CYP 3 A 4 is present in intestinal mucosa and liver Accounts of majority of first-pass metabolism Induced by St John’s Wort, carbamazepine Several drugs inhibited by grapefruit juice (bioflavinoids) § Amlodipine, lovastatin, buspirone, benzodiazepines
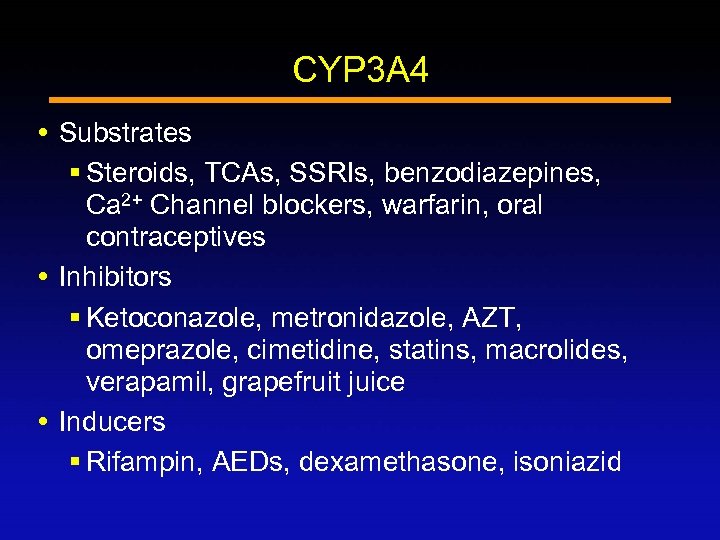
CYP 3 A 4 Substrates § Steroids, TCAs, SSRIs, benzodiazepines, Ca 2+ Channel blockers, warfarin, oral contraceptives Inhibitors § Ketoconazole, metronidazole, AZT, omeprazole, cimetidine, statins, macrolides, verapamil, grapefruit juice Inducers § Rifampin, AEDs, dexamethasone, isoniazid
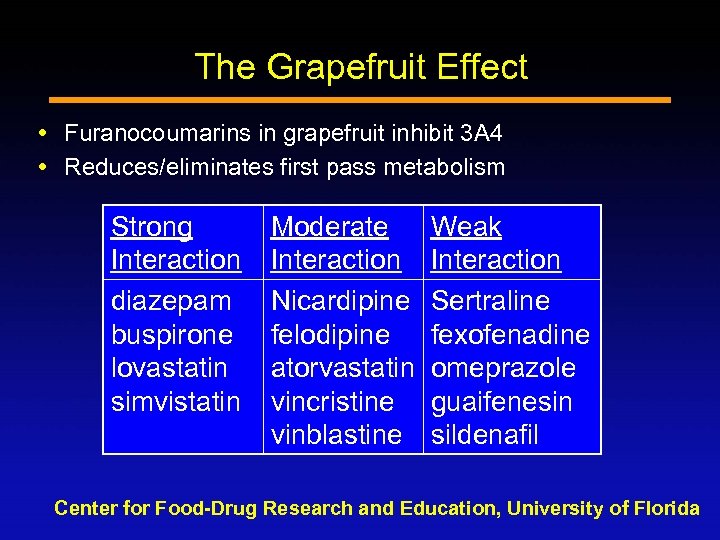
The Grapefruit Effect Furanocoumarins in grapefruit inhibit 3 A 4 Reduces/eliminates first pass metabolism Strong Interaction diazepam buspirone lovastatin simvistatin Moderate Interaction Nicardipine felodipine atorvastatin vincristine vinblastine Weak Interaction Sertraline fexofenadine omeprazole guaifenesin sildenafil Center for Food-Drug Research and Education, University of Florida
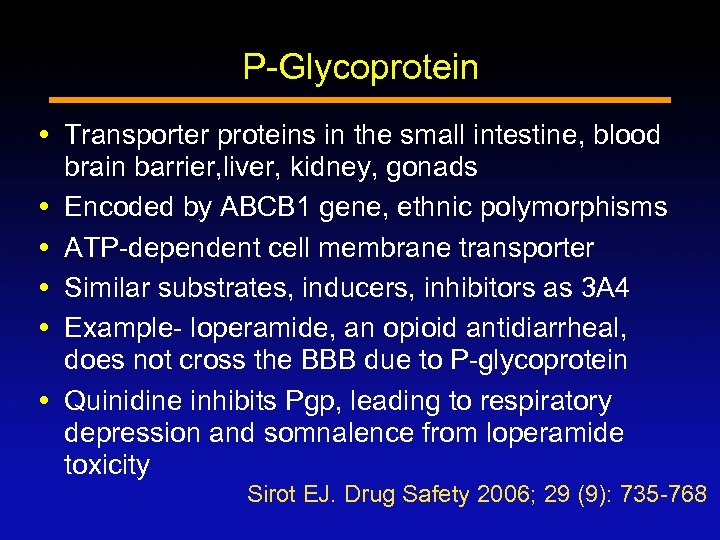
P-Glycoprotein Transporter proteins in the small intestine, blood brain barrier, liver, kidney, gonads Encoded by ABCB 1 gene, ethnic polymorphisms ATP-dependent cell membrane transporter Similar substrates, inducers, inhibitors as 3 A 4 Example- loperamide, an opioid antidiarrheal, does not cross the BBB due to P-glycoprotein Quinidine inhibits Pgp, leading to respiratory depression and somnalence from loperamide toxicity Sirot EJ. Drug Safety 2006; 29 (9): 735 -768
Question 5 Which statement is TRUE of the cytochrome P 450 system? a. Drug-drug interactions are likely to occur when a P 450 substrate is combined with a P 450 inhibitor b. Anticonvulsants tend to be P 450 inhibitors. c. P 450 enzymes are located primarily in the stomach and small intestine. d. Cigarette smoking has no effect on drug metabolism.
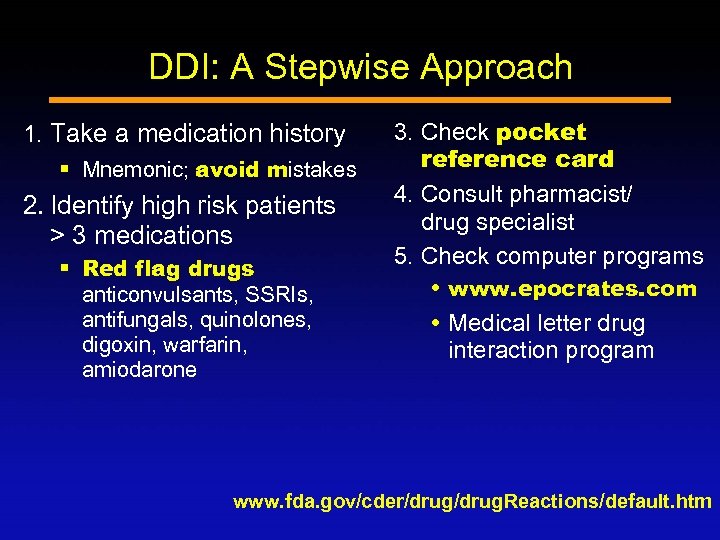
DDI: A Stepwise Approach 1. Take a medication history § Mnemonic; avoid mistakes 2. Identify high risk patients > 3 medications § Red flag drugs anticonvulsants, SSRIs, antifungals, quinolones, digoxin, warfarin, amiodarone 3. Check pocket reference card 4. Consult pharmacist/ drug specialist 5. Check computer programs www. epocrates. com Medical letter drug interaction program www. fda. gov/cder/drug. Reactions/default. htm
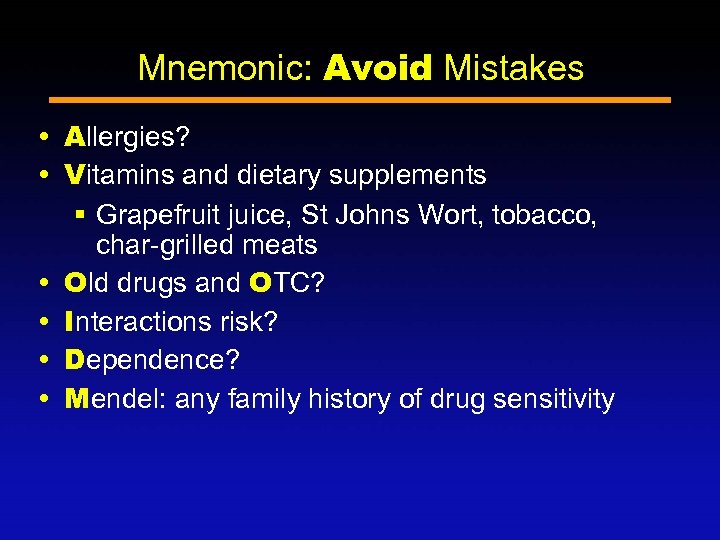
Mnemonic: Avoid Mistakes Allergies? Vitamins and dietary supplements § Grapefruit juice, St Johns Wort, tobacco, char-grilled meats Old drugs and OTC? Interactions risk? Dependence? Mendel: any family history of drug sensitivity
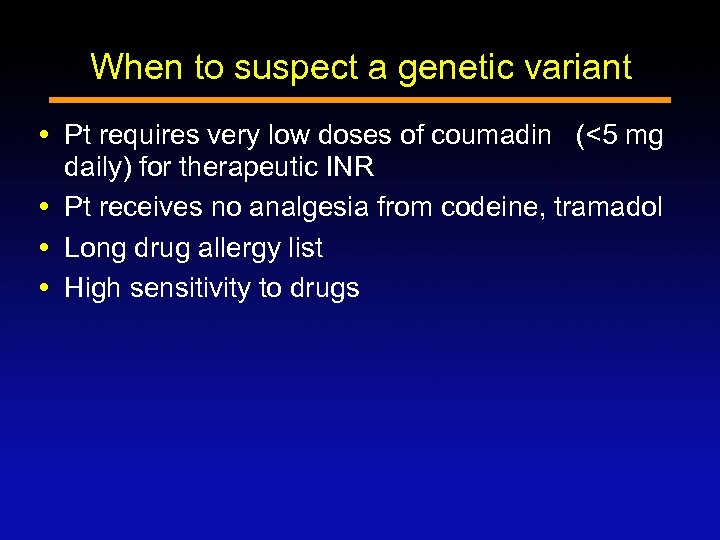
When to suspect a genetic variant Pt requires very low doses of coumadin (<5 mg daily) for therapeutic INR Pt receives no analgesia from codeine, tramadol Long drug allergy list High sensitivity to drugs
Websites on DDI, CYP 450, and drug transporting proteins http: //medicine. iupui. edu/flockhart www. epocrates. com http: //www. themedicalletter. com/ http: //www. druginteractioninfo. org/
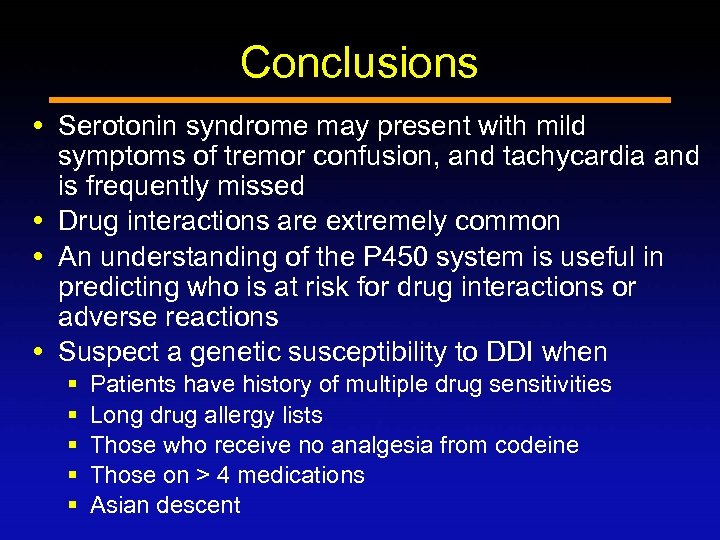
Conclusions Serotonin syndrome may present with mild symptoms of tremor confusion, and tachycardia and is frequently missed Drug interactions are extremely common An understanding of the P 450 system is useful in predicting who is at risk for drug interactions or adverse reactions Suspect a genetic susceptibility to DDI when § § § Patients have history of multiple drug sensitivities Long drug allergy lists Those who receive no analgesia from codeine Those on > 4 medications Asian descent
e5d26583c38298d496d46fc16019cdbf.ppt