1030f16a5e14e370a30bc1e526768133.ppt
- Количество слайдов: 31

Lessons From Top Down & Bottom up Health Care Change Paul Rafferty Berwick – Delivering Safer Care through growing HSC Organisations as learning organisations prafferty@stjames, ie

Objective & Introductions “Experience is merely the name men gave to their mistakes. ”

Session structure Part 1: The benefits and limits of Top Down Change Lessons learnt from establishing and managing the National Clinical Programmes National level Part 2: Relearning how to use improvement tools in health care Measurement: Hip Fracture Pathway & ECHO Utilisation Mapping patient flow: Dementia Pathway Influencing change: Chemo Drug Savings Patient level Part 3: Observations on teaching clinicians QI RCPI Diploma in Leadership & Quality Part 4: Sustaining change Building a Directorate Model that imbeds continuous improvement Close: 5 years “Learning” on a page Management level

Session structure Part 1: The benefits and limits of Top Down Change Lessons learnt from establishing and managing the National Clinical Programmes Part 2: Relearning how to use improvement tools in health care Measurement: Hip Fracture Pathway & ECHO Utilisation Mapping patient flow: Dementia Pathway Influencing change: Chemo Drug Savings Part 3: Observations on teaching clinicians QI RCPI Diploma in Leadership & Quality Part 4: Sustaining change Building a Directorate Model that imbeds continuous improvement Close: 5 years “Learning” on a page

Session structure Part 1: The benefits and limits of Top Down Change Lessons learnt from establishing and managing the National Clinical Programmes Part 2: Relearning how to use improvement tools in health care Measurement: Hip Fracture Pathway & ECHO Utilisation Mapping patient flow: Dementia Pathway Influencing change: Chemo Drug Savings 11 ish Part 3: Observations on teaching clinicians QI RCPI Diploma in Leadership & Quality Part 4: Sustaining change Building a Directorate Model that imbeds continuous improvement Close: 5 years “Learning” on a page 12: 30

Agenda Part 1: The benefits and limits of Top Down Change Lessons learnt from establishing and managing the National Clinical Programmes Part 2: Relearning how to use improvement tools in health care Measurement: Hip Fracture Pathway & ECHO Utilisation Mapping patient flow: Dementia Pathway Influencing change: Chemo Drug Savings Part 3: Observations on teaching clinicians QI RCPI Diploma in Leadership & Quality Part 4: Sustaining change Building a Directorate Model that imbeds continuous improvement Close: 5 years “Learning” on a page

The National Clinical Programmes Learning – Branding was important

National Clinical Programmes timeline Jan 2010 Sept 2009 Dr Barry White appointed National Director Clinical Strategy & programmes Jan 2011 Jan 2012 Jan 2013 Jan. Today 2014 Context • 30 + hospitals (6 Voluntary hospitals-funded by HSE but not managed Directly) • Fianna Fail Government – Brian Cowen-Taoiseach , Mary Harney-Mo. H • At Celtic Tiger budget levels but deep cuts beginning • HSE 4+ years old – CEO Brendan Drumm – but leaving • HSE new structures being implemented – Regional Directors of operation • Reconfiguration being discussed • No sign of Clinical Leaders in the HSE – high distrust • Clinical Directors initiative lacking sponsorship & leadership Role origins • National Director role for Quality and safety – part of original HSE design • Provided with an office & a secretary • Existing clinical programmes – Cancer Programme & Renal Office

Part 1: The benefits and limits of Top Down Change Lessons learnt from establishing and managing the National Clinical Programmes timeline Jan 2010 Sept 2009 Dr Barry White appointed National Director Clinical Strategy & programmes Oct ‘ 09 Principles & Approach designed Jan 2011 Jan 2012 Jan 2013 Jan. Today 2014
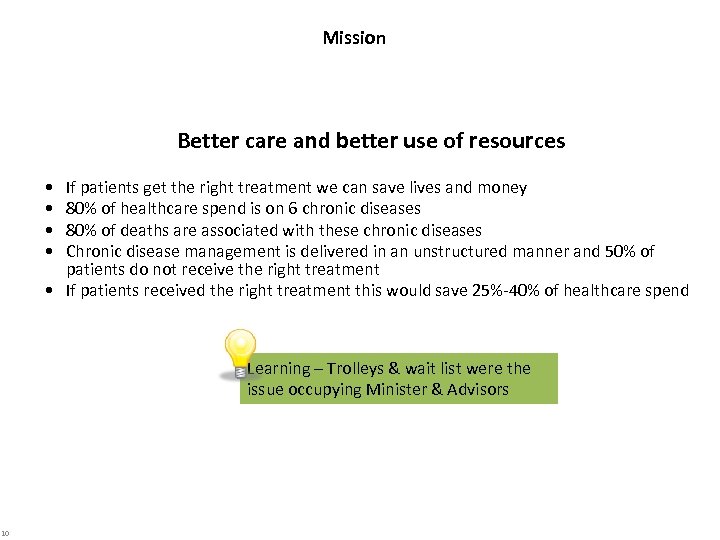
Mission Better care and better use of resources • • If patients get the right treatment we can save lives and money 80% of healthcare spend is on 6 chronic diseases 80% of deaths are associated with these chronic diseases Chronic disease management is delivered in an unstructured manner and 50% of patients do not receive the right treatment • If patients received the right treatment this would save 25%-40% of healthcare spend Learning – Trolleys & wait list were the issue occupying Minister & Advisors 10

What are the key metrics for measuring Programme Success Quality Reduction in mortality Reduction in morbidity Improved patient experience Improved quality of life Access Reduction in waiting time for admission Reduction in time for appointment with appropriate health care professional Cost Reduction in cost ( drugs, overtime, beds) Improved productivity Learning – Cost was the wrong label should have used “Waste” or “Efficiency” QAC 11

Don Berwick – the Ethics of Quality In hind sight this is what our aim was Types of Health Care waste • • • Over treatment Failures to co-ordinate care Failure in care delivery Excess Administration Excessive Health Care Prices Fraud & Abuse 158 25 102 107 84 82 -226 m -45 m -154 m – 389 m – 178 m – 272 m

Overall principles • • • Clinically led Multi-discipline team Set goals that achieve gains in Quality, Access & Cost Set goals that are simple and meaningful – e. g. prevent 300 stroke deaths Target what is achievable Nationalise existing local good practice - do not reinvent the wheel Ensure local ownership (authority, accountability and responsibility) Ensure patient involvement Trusted data informs our decisions Invest in selling the benefits of change and winning hearts and minds (90% of leads time) Detailed implementation and communication plans How success will be assessed ü 5% of marks for developing solutions ü 45% of marks for implementing solutions that deliver measurable improvement ü 50% of marks for putting in place the mechanisms to sustain continuous improvement 13 Learning – Principles were correct and helped to create momentum - 95% of marks were for implementation but locally the implementation skills not uniformly present and no “Change Management” infrastructure in the system through which change could be cascaded & protected from the impact of crisis management

Programme deliverables (1) Define scope , objectives, measures of success , stakeholders , Program Governance & Team (2) Baseline performance (3) Clinical Evidence based documentation Guidelines (4) Model of Care Pathway Infrastructure, Roles and Responsibilities, Governance (who does what) SLAs with related services - Rapid access to Clinics, consult services, diagnostics, and home/community services Metrics – Av. LOS, Morbidity, Mortality, Readmission Rates, Admission Rates (5) Decision making documentation Care Bundles Algorithm Patient Information GP/Clinician information Care Plans/Pathways (Respiratory Nurse and Self Care) (6) Gap analysis (7) Reconfiguration inputs (8) Business Case Learning – Every service (programme) is starting from a different point - Demand & capacity Data was key but data not trusted - (+/-) Didn’t standardise deliverables For the models of care Cost Benefit of implementing Forecast the usage Identify the current deficit i. e. in outreach and What is required to fill the deficit to deliver the model of care in terms of Governance, Roles, Processes, Funding (9) Implementation & Communication plan (10) Establish & mange implementation team & governance 14

Programme Team Governance • Clinical Advisory Group (College) Clinical Lead (Consultant ) Nurse Lead • Nurse Advisory Group Allied Health Professional (Physio, • AHP Advisory Group etc) • GP Advisory Group (ICGP) • GP Lead • Patient advisory group • Public Health Doctor Learning • Manager • Programme manager was key to managing the • Programme Manager team (Role descriptions for all roles) • There relationship with lead was key (partner& coach Vs personal assistant • Embedding programme managers in college had +/- benefits • College and other advisory groups key to ensuring (a) the leads had their authority & b) programme solutions had their sanction • Didn’t involve management in the teams early enough • • •
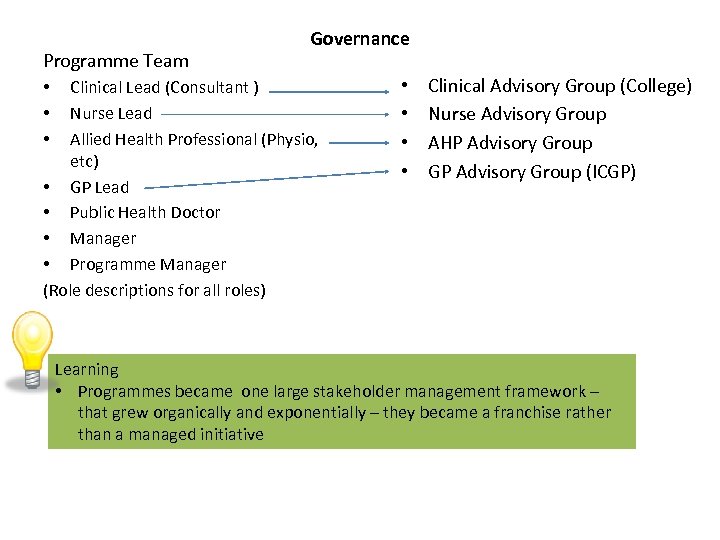
Programme Team Governance Clinical Lead (Consultant ) Nurse Lead Allied Health Professional (Physio, etc) • GP Lead • Public Health Doctor • Manager • Programme Manager (Role descriptions for all roles) • • Clinical Advisory Group (College) Nurse Advisory Group AHP Advisory Group GP Advisory Group (ICGP) Learning • Programmes became one large stakeholder management framework – that grew organically and exponentially – they became a franchise rather than a managed initiative

Programme approach? 1 2 Initiate program 3 Scope Set the Goals progra 1 Define key issues & solutions 4 5 Measure & analyse performance 6 Validate solutions 2 7 Detailed solution design 3 8 Sustain & Implement improve solutions performance 4 Learning – Right to have a structured approach but - Every service starting from a different place - Language got in the way – not clinically relevant enough - Got distracted by other approaches and confused people - Jumped the approach steps due to impatience or fear of running out – ran into problems Checkpoints with the Program Advisory Group, the Director of Quality & Clinical Care and Steering group

Example QACs COPD Programme Over arching aim: To save a life a week from COPD. Objectives Access • Implementation of COPD outreach program to decrease admissions • Implement COPD pulmonary rehabilitation program Diabetes Programme Over arching aim: Save the lives, eyes and limbs of patients with Diabetes Objectives Access • Everyone with Diabetes should access a structure program of care which covers all aspects of their Diabetic care. Quality • Decrease morbidity and mortality through: • Correct and early Diagnosis • Correct treatment based on best practice guidelines for treatment (self management, GP and Pharmacy management) Quality • Reduction in mortality by 10%. • Reduction in morbidity ( Reduce; Blindness by 40%, Amputations by 40%, Cardiovascular events by 20%. Cost • Reduce COPD admissions by 1, 500 a year. Cost • Reduction in overall bed days by 40, 000 per year. 18

How to get the specialities on-board Things Barry said: • I understand why you might not won’t to come on board • ………welcome to join phase two! • Backing of College • For key speciality engagement meetings let people vent but make sure you’re not the only persuading voice – make sure you have senior clinician support • Opportunity to disprove people that clinicians can’t lead change • I’m here to broker a deal not to tell you what to do – you have to give me a business case I can sell – What’s the gap between demand capacity to meet demand – What we will do to bridge the gap through change of practice and service delivery innovation that has a neutral cost Learning – You have got to be as – The deal is you (HSE/DOH) have to bridge the demand gap that remains interested in the implementation (95% of the marks) as the ideas (5% of the Marks) Value of a “ Barry: • Docs Invest trust in him not the “system” • Understands their business and world • Can challenge their facts • Interest goes beyond his speciality – stimulated by problem solving

Programmes & leads - PM Mairead Gleeson Diarmuid Smith 20 Learning – The problem was not too many programmes it was (a) Growing too quickly (b) Not building the team and infrastructure 1 st (c) Not recognising the systems capacity & capability to absorb & manage Medication Management change
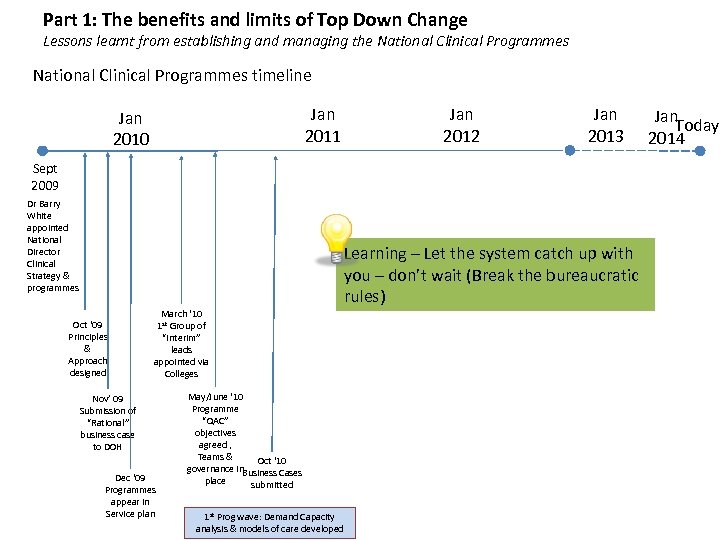
Part 1: The benefits and limits of Top Down Change Lessons learnt from establishing and managing the National Clinical Programmes timeline Jan 2011 Jan 2010 Jan 2012 Jan 2013 Sept 2009 Dr Barry White appointed National Director Clinical Strategy & programmes Learning – Let the system catch up with you – don’t wait (Break the bureaucratic rules) Oct ‘ 09 Principles & Approach designed March ‘ 10 1 st Group of “Interim” leads appointed via Colleges Nov’ 09 Submission of “Rational” business case to DOH Dec ‘ 09 Programmes appear in Service plan May/June ‘ 10 Programme “QAC” objectives agreed , Teams & Oct ‘ 10 governance in. Business Cases place submitted 1 st Prog wave: Demand Capacity analysis & models of care developed Jan. Today 2014

Business cases Learning – They didn’t read them – the fact we had them and had detailed data seemed enough

Part 1: The benefits and limits of Top Down Change Lessons learnt from establishing and managing the National Clinical Programmes timeline Jan 2011 Jan 2010 Sept 2009 Dr Barry White appointed National Director Clinical Strategy & programmes Oct ‘ 09 Principles & Approach designed March ‘ 10 1 st Group of “Interim” leads appointed via Colleges Nov’ 09 Submission of “Rational” business case to DOH Dec ‘ 09 Programmes appear in Service plan € 40 m Funding confirmed in service plan Service Implementation approach developed May/June ‘ 10 Programme “QAC” objectives agreed , Teams & Oct ‘ 10 governance in. Business Cases place submitted 1 st Prog wave: Demand Capacity analysis & models of care developed Jan 2012 Jan 2013 Jan. Today 2014

Framework for National Clinical Programmes Patient 1 Patient information web site Self Management 10 2 3 Chronic Disease watch 4 12 Initial Assessment Incl. AMAU/MAU Clinical Prioritisation: EWS 16 14 Surgical Assessment Unit 17 18 Out patients Elective Surgery Rapid Access Clinics Community Intervention Team & other home delivered services 26 Critical Care (ICU/CCU) 13 Acute Medical Unit (AMU) Outreach Service 7 19 Emergency Department Triage and/or EWS Ambulatory Care Service 6 25 9 Regional Patient Navigation Hub Ambulance Triage and/or EWS 11 Pharmacy 5 24 Walk-in 8 GP/Primary Care Team 23 Rehab services Learning Working Don’t manage the. Diagnosis programmes in Emergency • Surgery away that accentuates “Silo thinking” 15 • It’s a single patient pathway with. Units/Centres e. g. Specialist Care plan Stroke, multiple integrated solution areas. Heart Failure, Epilepsy, PCI, Diabetes • Its not Multiple programmes with multiple un integrated solutions 22 Discharge management 27 Community nursing Units/Homes Diagnostics AMU Short Stay Unit 20 Admission wards EWS Specialist Wards Home 29 Hospital retrieval Transfer 28 Hospice/ Palliative Care 1 4 21 3 2 Hospital Network Pathway enablement and sustainability 3/19/2018 Rafferty/Programmes/Implementation Strategy & Plan 24
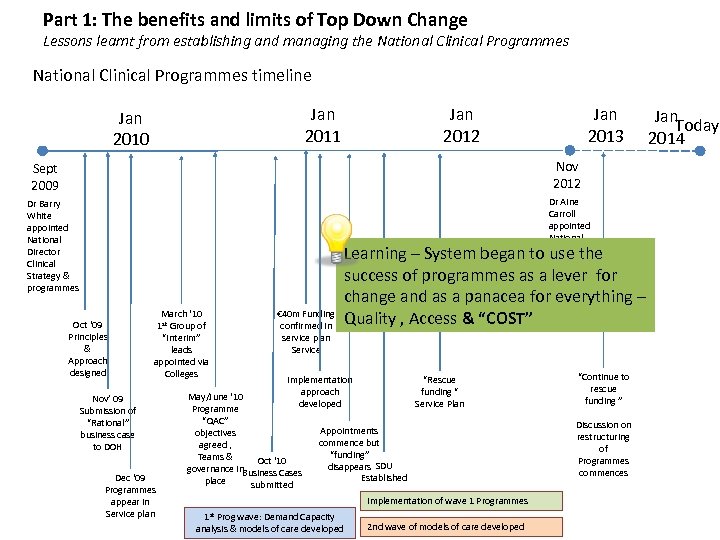
Part 1: The benefits and limits of Top Down Change Lessons learnt from establishing and managing the National Clinical Programmes timeline Jan 2011 Jan 2010 Jan 2013 Jan 2012 Nov 2012 Sept 2009 Dr Aine Carroll appointed National Director Clinical Strategy & programmes Dr Barry White appointed National Director Clinical Strategy & programmes Oct ‘ 09 Principles & Approach designed March ‘ 10 1 st Group of “Interim” leads appointed via Colleges Nov’ 09 Submission of “Rational” business case to DOH Dec ‘ 09 Programmes appear in Service plan € 40 m Funding confirmed in service plan Service Learning – System began to use the success of programmes as a lever for change and as a panacea for everything – Quality , Access & “COST” Implementation approach developed May/June ‘ 10 Programme “QAC” objectives agreed , Teams & Oct ‘ 10 governance in. Business Cases place submitted “Rescue funding “ Service Plan Appointments commence but “funding” disappears SDU Established Implementation of wave 1 Programmes 1 st Prog wave: Demand Capacity analysis & models of care developed 2 nd wave of models of care developed “Continue to rescue funding ” Discussion on restructuring of Programmes commences Jan. Today 2014

Part 1: The benefits and limits of Top Down Change Lessons learnt from establishing and managing the National Clinical Programmes timeline Jan 2011 Jan 2010 Jan 2013 Jan 2012 Nov 2012 Sept 2009 Dr Barry White appointed National Director Clinical Strategy & programmes Legacy serious incident reviews Oct ‘ 09 Principles & Approach designed Missdiagnosis Unopened referral letters March ‘ 10 1 st Group of “Interim” leads appointed via Colleges € 40 m Funding confirmed in service plan Service Learning Surgery safety • Clinical strategic improvement & Safety require clinical leadership Non reviewed x- “Rescue concern • ……. . but not the same person Implementation approach funding “ May/June ‘ 10 Nov’ 09 developedrays Service Plan Programme • Reactive of Submission Crisis/incident management with media / political “QAC” “Rational” Appointments implications will trump pro active change initiative objectives business case commence agreed , to • Need DOH separate National Oct ‘ 10 - but programme leads can cross to roles Teams & SDU governance between two areas place in. Business Cases Established Dec ‘ 09 Programmes appear in Service plan submitted Implementation of wave 1 Programmes 1 st Dr Aine Carroll appointed National Director Clinical Strategy & programmes Prog wave: Demand Capacity analysis & models of care developed 2 nd wave of models of care developed “Continue to rescue funding ” Discussion on restructuring of Programmes commences Jan. Today 2014
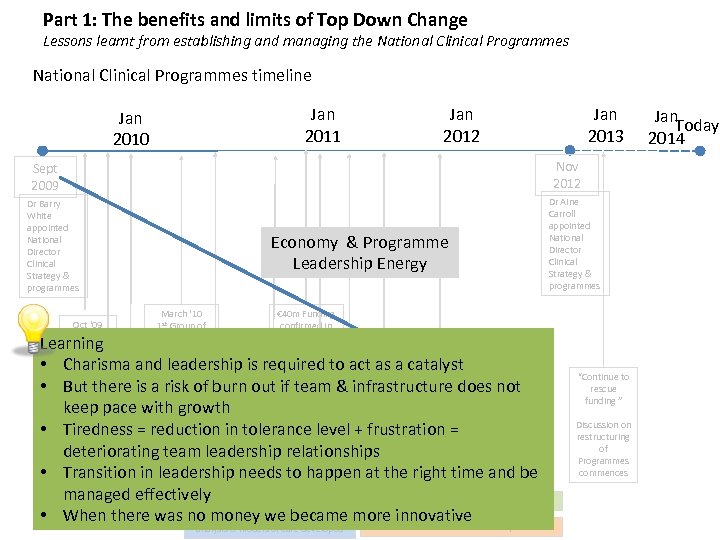
Part 1: The benefits and limits of Top Down Change Lessons learnt from establishing and managing the National Clinical Programmes timeline Jan 2011 Jan 2010 Jan 2013 Jan 2012 Nov 2012 Sept 2009 Dr Barry White appointed National Director Clinical Strategy & programmes Oct ‘ 09 Principles & Approach designed Economy & Programme Leadership Energy March ‘ 10 1 st Group of “Interim” leads appointed via Colleges Dr Aine Carroll appointed National Director Clinical Strategy & programmes € 40 m Funding confirmed in service plan Service Learning • Charisma and leadership is required to act as a catalyst “Rescue • But there is a risk. May/June ‘ 10 out if. Implementationinfrastructure “does not of burn team & approach funding Nov’ 09 developed Service Plan Programme keep pace with growth Submission of “QAC” “Rational” Appointments • Tiredness = reduction in tolerance level + frustration = objectives business case commence agreed , to DOH deteriorating team. Teams & Oct ‘ 10 relationships leadership SDU governance • Transition‘ 09 leadership in. Business Cases happen. Established right time and be needs to at the Dec in place submitted Programmes managed effectively Implementation of wave 1 Programmes appear in Service planwas no 1 money Demand Capacity Prog wave: we became more innovative • When there 2 nd wave of models of care developed st analysis & models of care developed “Continue to rescue funding ” Discussion on restructuring of Programmes commences Jan. Today 2014

Running cost • € 5 -8 m – – – Clinical lead back fills – 2. 5 days per week Programme Managers GP Compensation Central Programme management team Other running/operational costs
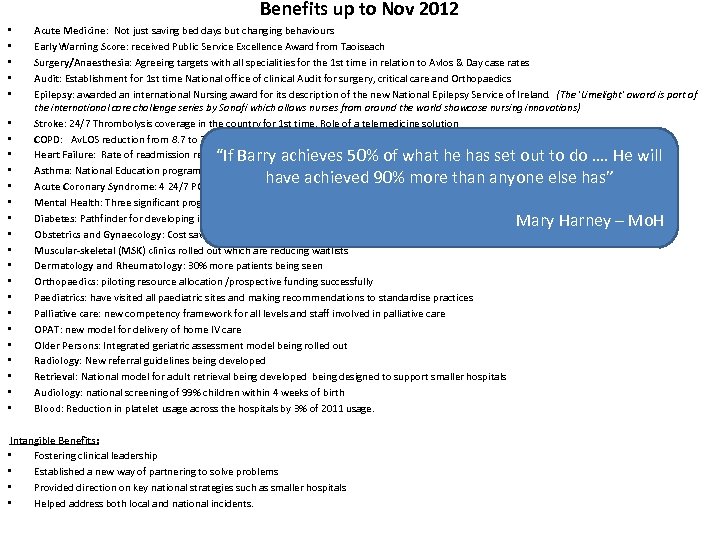
Benefits up to Nov 2012 • • • • • • Acute Medicine: Not just saving bed days but changing behaviours Early Warning Score: received Public Service Excellence Award from Taoiseach Surgery/Anaesthesia: Agreeing targets with all specialities for the 1 st time in relation to Avlos & Day case rates Audit: Establishment for 1 st time National office of clinical Audit for surgery, critical care and Orthopaedics Epilepsy: awarded an international Nursing award for its description of the new National Epilepsy Service of Ireland. (The 'Limelight' award is part of the international care challenge series by Sanofi which allows nurses from around the world showcase nursing innovations) Stroke: 24/7 Thrombolysis coverage in the country for 1 st time. Role of a telemedicine solution COPD: Av. LOS reduction from 8. 7 to 7. 9 day Heart Failure: Rate of readmission reduced from 27% to 6. 3% Asthma: National Education programme operational in primary and secondary care Acute Coronary Syndrome: 4 24/7 PCI centres operational Mental Health: Three significant programmes being designed in areas such as self harm and eating disorders Diabetes: Pathfinder for developing integrated care model and chronic disease management Obstetrics and Gynaecology: Cost savings from centralised procurement and no mis-scanning incidents since early pregnancy guidelines issued Muscular-skeletal (MSK) clinics rolled out which are reducing waitlists Dermatology and Rheumatology: 30% more patients being seen Orthopaedics: piloting resource allocation /prospective funding successfully Paediatrics: have visited all paediatric sites and making recommendations to standardise practices Palliative care: new competency framework for all levels and staff involved in palliative care OPAT: new model for delivery of home IV care Older Persons: Integrated geriatric assessment model being rolled out Radiology: New referral guidelines being developed Retrieval: National model for adult retrieval being developed being designed to support smaller hospitals Audiology: national screening of 99% children within 4 weeks of birth Blood: Reduction in platelet usage across the hospitals by 3% of 2011 usage. “If Barry achieves 50% of what he has set out to do …. He will have achieved 90% more than anyone else has” Intangible Benefits: • Fostering clinical leadership • Established a new way of partnering to solve problems • Provided direction on key national strategies such as smaller hospitals • Helped address both local and national incidents. Mary Harney – Mo. H

Part 1: The benefits and limits of Top Down Change RR WR RW WW Is was the right thing and we did it largely the right way except for • • Rate of growth - not saying No. Linking programmes to funding at time of economic crisis Programmes associated with an individual rather than being a sustainable entity Straying from the principles Drifting further from the colleges & closer to the political agenda Management of Primary Care engagement Performance management of leads Training?

Part 1: The benefits and limits of Top Down Change RR WR RW WW Discussion & Questions?
1030f16a5e14e370a30bc1e526768133.ppt