92fa8a2a4a3b09ef2c113e81618b27a5.ppt
- Количество слайдов: 85
Lessons from Recent Trials Thrombolysis the Choice for Reperfusion Dr. Vinod Sharma M. D. , D. M, FIMSA, FACC, MBA (HCA) National Heart Institute (All India Heart Foundation) New Delhi
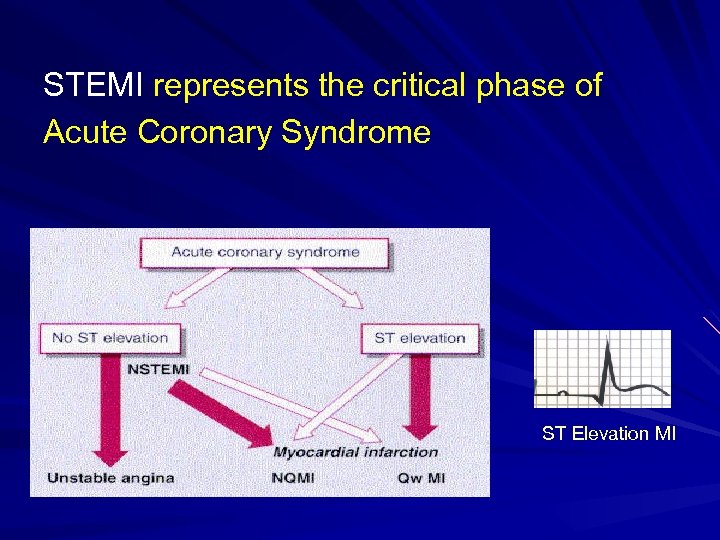
STEMI represents the critical phase of Acute Coronary Syndrome ST Elevation MI
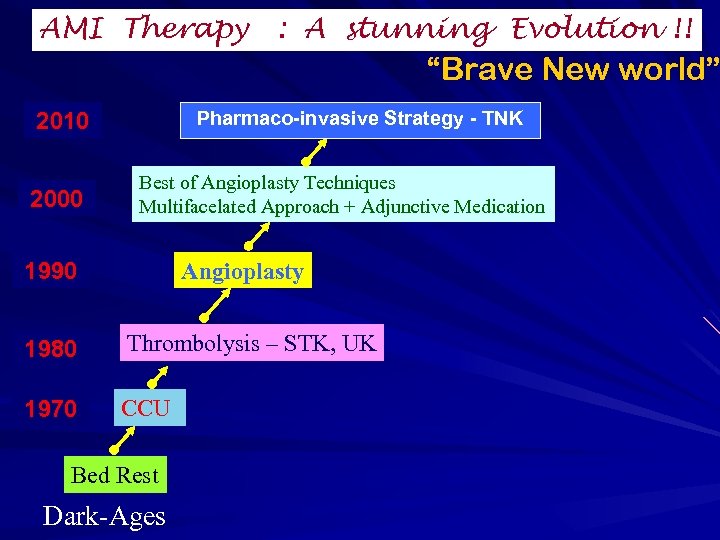
AMI Therapy : A stunning Evolution !! “Brave New world” Pharmaco-invasive Strategy - TNK 2010 2000 Best of Angioplasty Techniques Multifacelated Approach + Adjunctive Medication 1990 Angioplasty 1980 Thrombolysis – STK, UK 1970 CCU Bed Rest Dark-Ages
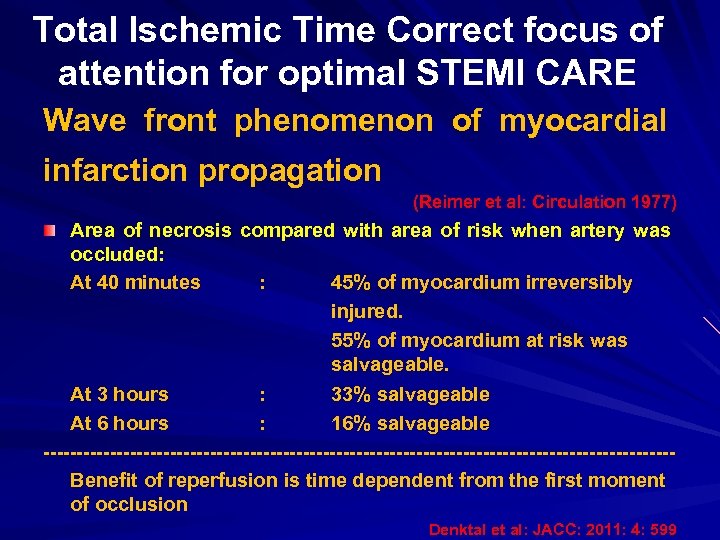
Total Ischemic Time Correct focus of attention for optimal STEMI CARE Wave front phenomenon of myocardial infarction propagation (Reimer et al: Circulation 1977) Area of necrosis compared with area of risk when artery was occluded: At 40 minutes : 45% of myocardium irreversibly injured. 55% of myocardium at risk was salvageable. At 3 hours : 33% salvageable At 6 hours : 16% salvageable -----------------------------------------------Benefit of reperfusion is time dependent from the first moment of occlusion Denktal et al: JACC: 2011: 4: 599
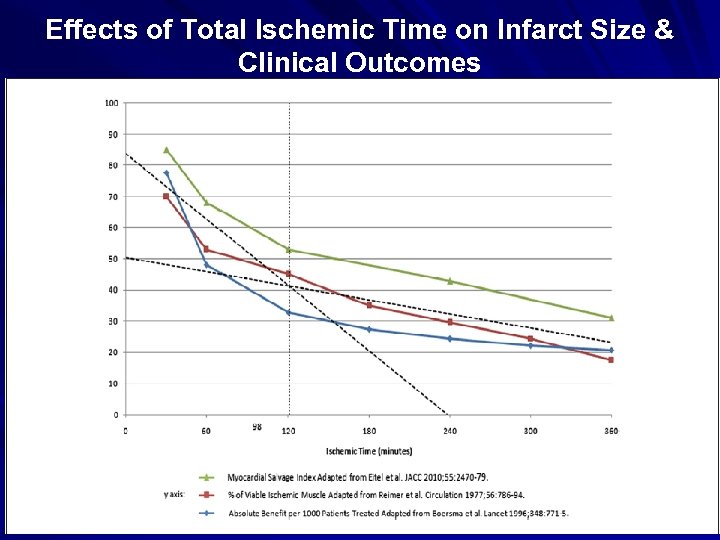
Effects of Total Ischemic Time on Infarct Size & Clinical Outcomes
Reperfusion is the key to save myocardium and life…. Aim is to open the blocked I. R. A. and Re -establish the coronary blood flow 1. Rapid 2. Early 3. Complete 4. Sustained

Time is essence ……
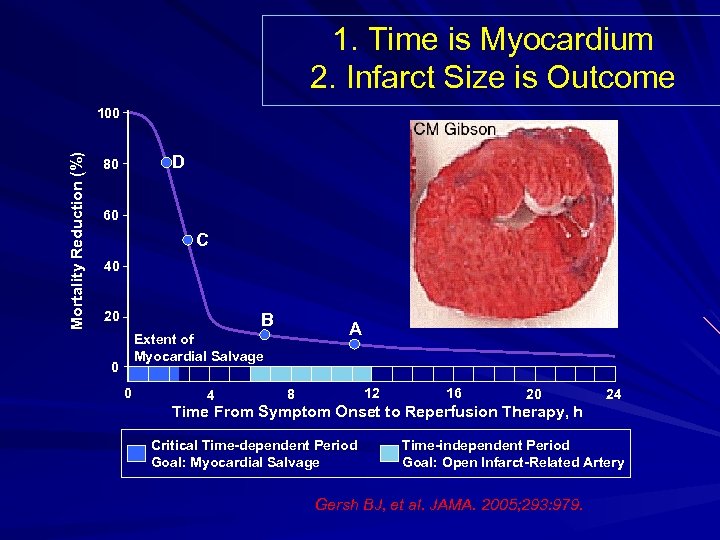
1. Time is Myocardium 2. Infarct Size is Outcome Mortality Reduction (%) 100 D 80 60 C 40 20 B A Extent of Myocardial Salvage 0 0 4 12 8 16 20 Time From Symptom Onset to Reperfusion Therapy, h Critical Time-dependent Period Goal: Myocardial Salvage 24 Time-independent Period Goal: Open Infarct-Related Artery Gersh BJ, et al. JAMA. 2005; 293: 979.
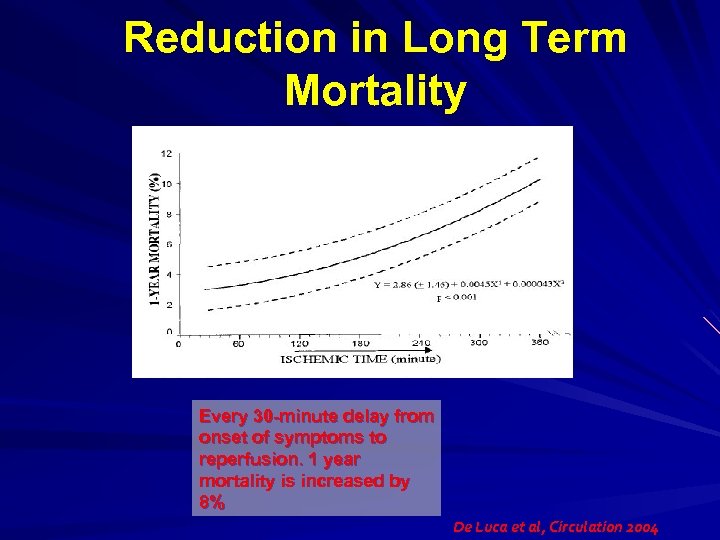
Reduction in Long Term Mortality Every 30 -minute delay from onset of symptoms to reperfusion. 1 year mortality is increased by 8% De Luca et al, Circulation 2004
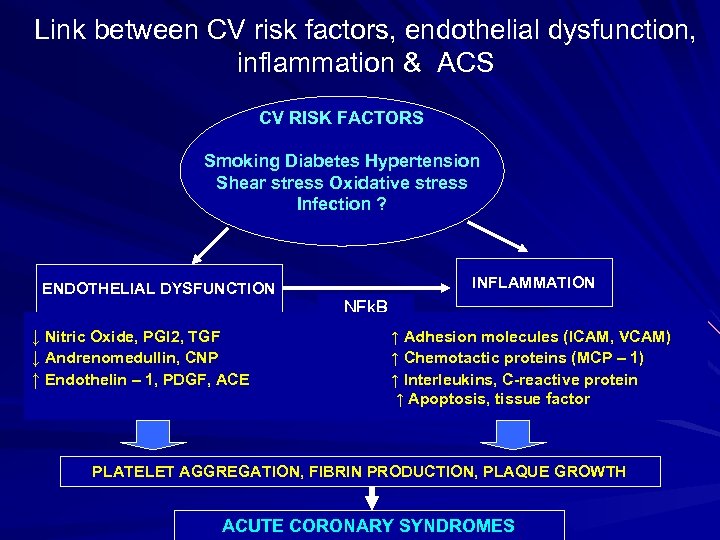
Link between CV risk factors, endothelial dysfunction, inflammation & ACS CV RISK FACTORS Smoking Diabetes Hypertension Shear stress Oxidative stress Infection ? ENDOTHELIAL DYSFUNCTION ↓ Nitric Oxide, PGI 2, TGF ↓ Andrenomedullin, CNP ↑ Endothelin – 1, PDGF, ACE INFLAMMATION NFk. B ↑ Adhesion molecules (ICAM, VCAM) ↑ Chemotactic proteins (MCP – 1) ↑ Interleukins, C-reactive protein ↑ Apoptosis, tissue factor PLATELET AGGREGATION, FIBRIN PRODUCTION, PLAQUE GROWTH ACUTE CORONARY SYNDROMES
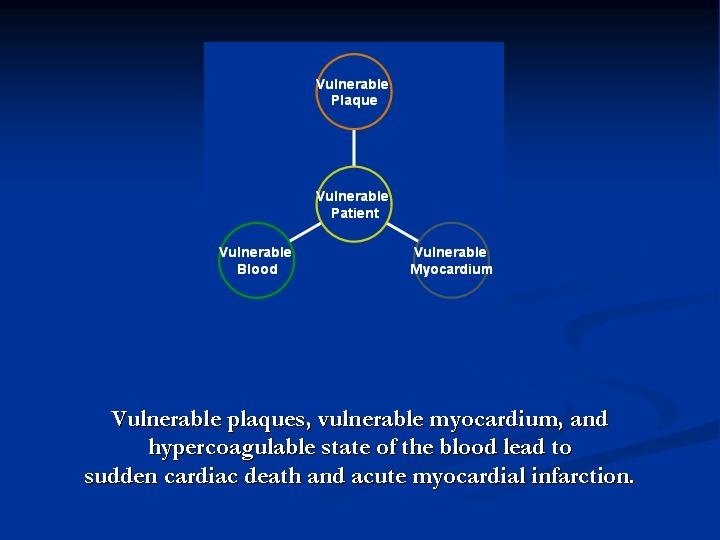
Acute Coronary Syndrome a “PANCORONITIS” ? Local manifestation of systemic disease
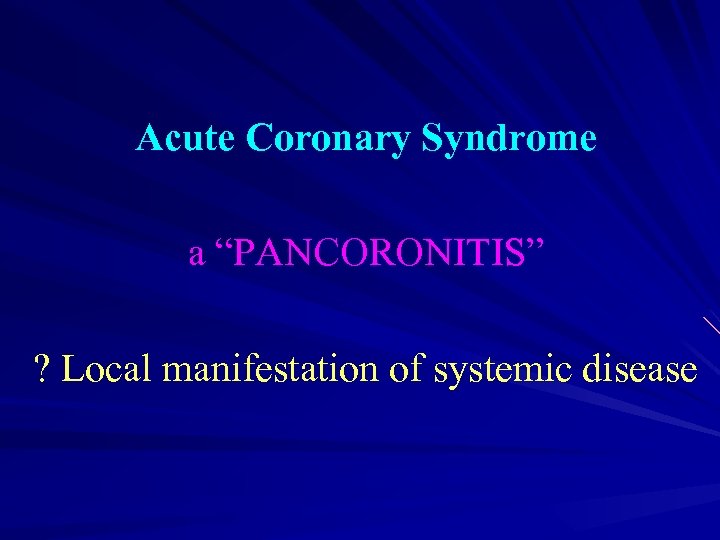
Evidence of multiple “vulnerable” plaques in acute coronary syndrome
Plaque Rupture – Clinical Manifestation People who died due to ACS, harbour both thrombosed & non thrombosed ruptured plaques in their coronary arteries. Goldstein JA et al: NEJM 2000 Additional plaques are frequently found adjacent to the culprit lesions in patients undergoing PTCA. Schoenhager Petal: 2003
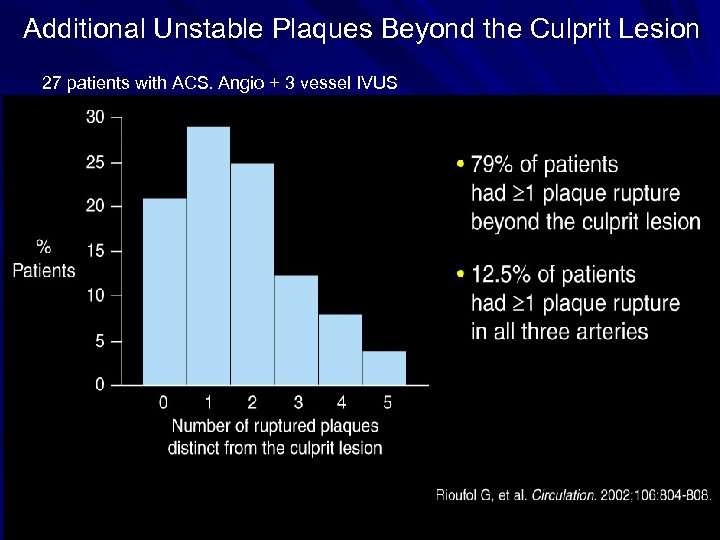
Additional Unstable Plaques Beyond the Culprit Lesion 27 patients with ACS. Angio + 3 vessel IVUS
Reperfusion Strategy in Acute STEMI Thrombolysis Primary Angioplasty Pharmaco-invasive strategy
Selection of Reperfusion Strategy in STEMI Time since the onset of symptoms Risk of Mortality from STEMI Availability of skilled PCI Laboratory Time required for Transport Any contraindication to thrombolysis including bleeding, ICH Patient preference ACC/AHA STEMI Guidelines 2013
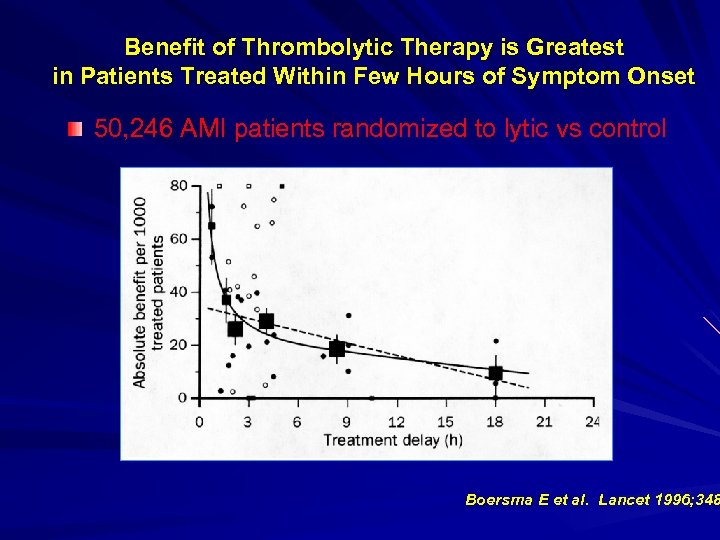
Benefit of Thrombolytic Therapy is Greatest in Patients Treated Within Few Hours of Symptom Onset 50, 246 AMI patients randomized to lytic vs control Boersma E et al. Lancet 1996; 348
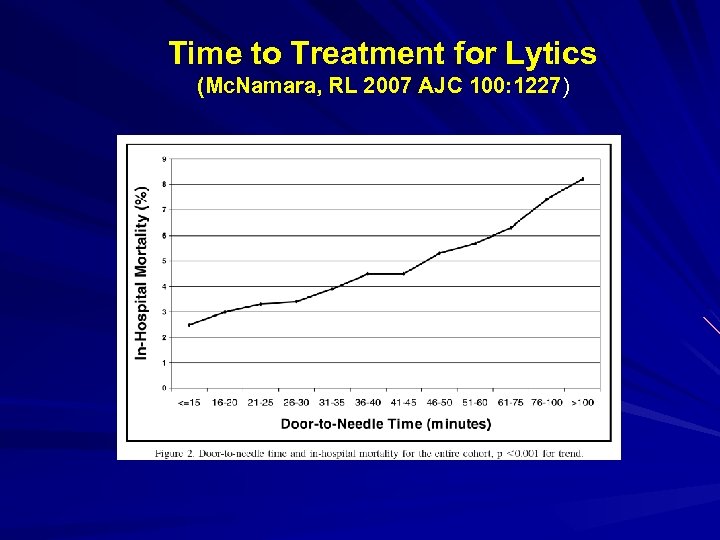
Time to Treatment for Lytics (Mc. Namara, RL 2007 AJC 100: 1227)
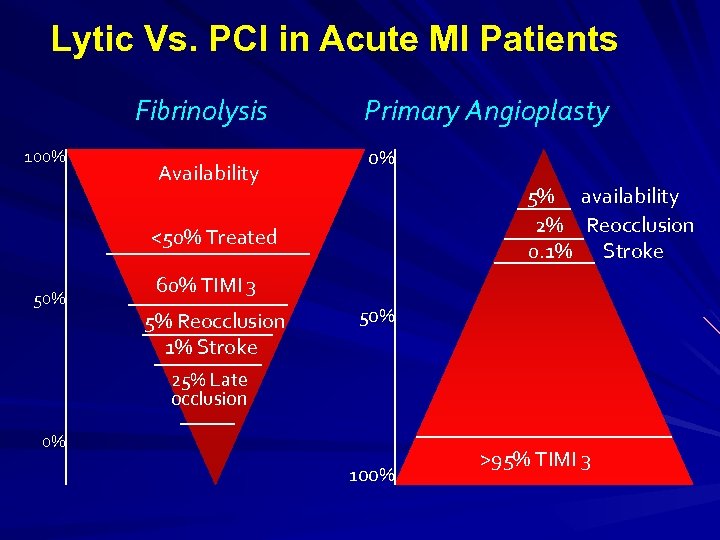
Lytic Vs. PCI in Acute MI Patients Fibrinolysis 100% Availability Primary Angioplasty 0% 5% availability 2% Reocclusion 0. 1% Stroke <50% Treated 50% 60% TIMI 3 5% Reocclusion 1% Stroke 50% 25% Late occlusion 0% 100% >95% TIMI 3
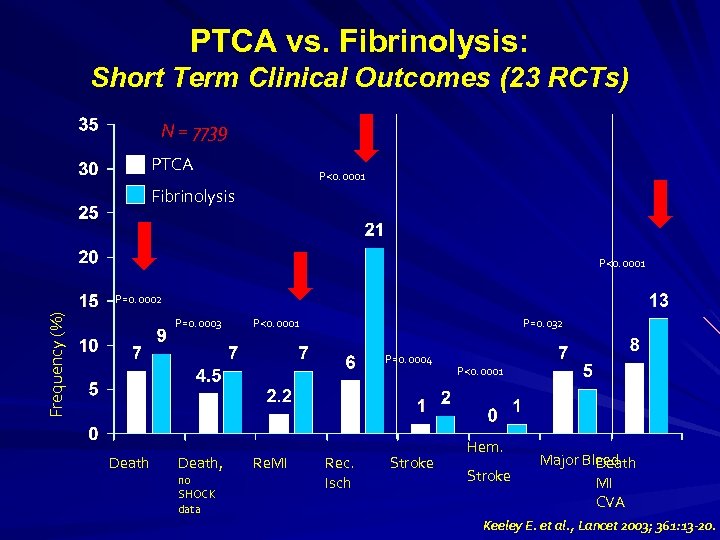
PTCA vs. Fibrinolysis: Short Term Clinical Outcomes (23 RCTs) N = 7739 PTCA P<0. 0001 Fibrinolysis P<0. 0001 Frequency (%) P=0. 0002 P=0. 0003 P<0. 0001 P=0. 032 P=0. 0004 Death, no SHOCK data Re. MI Rec. Isch Stroke P<0. 0001 Hem. Stroke Major Bleed Death MI CVA Keeley E. et al. , Lancet 2003; 361: 13 -20.
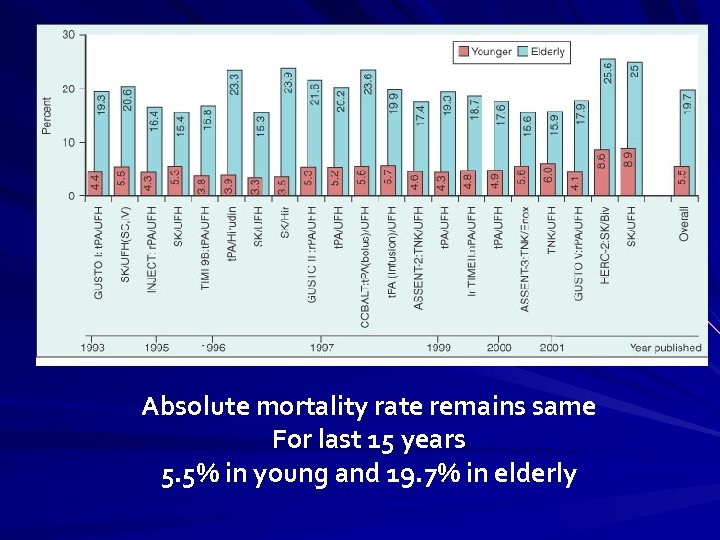
Absolute mortality rate remains same For last 15 years 5. 5% in young and 19. 7% in elderly
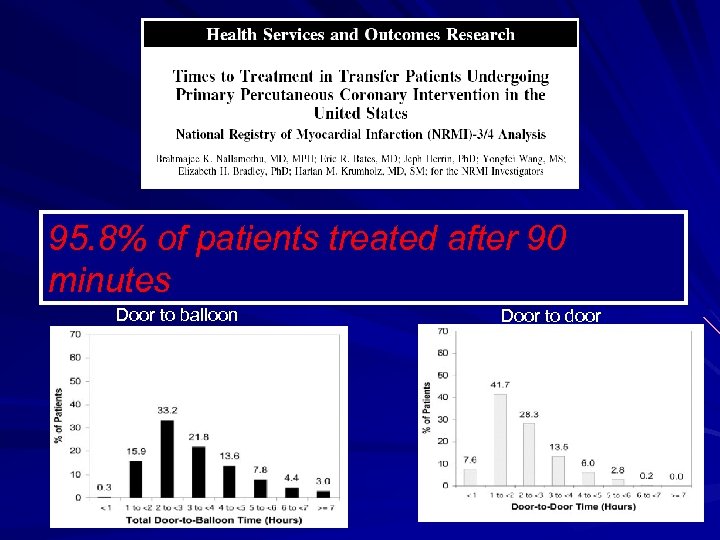
95. 8% of patients treated after 90 minutes Door to balloon Door to door
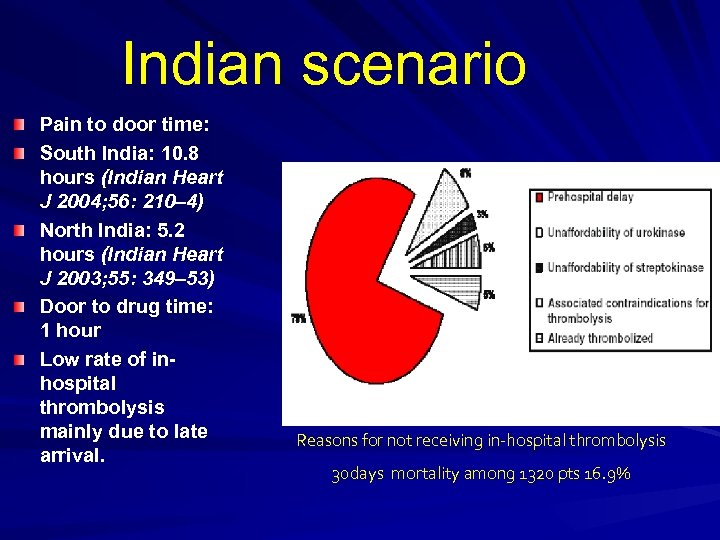
Indian scenario Pain to door time: South India: 10. 8 hours (Indian Heart J 2004; 56: 210– 4) North India: 5. 2 hours (Indian Heart J 2003; 55: 349– 53) Door to drug time: 1 hour Low rate of inhospital thrombolysis mainly due to late arrival. Reasons for not receiving in-hospital thrombolysis 30 days mortality among 1320 pts 16. 9%
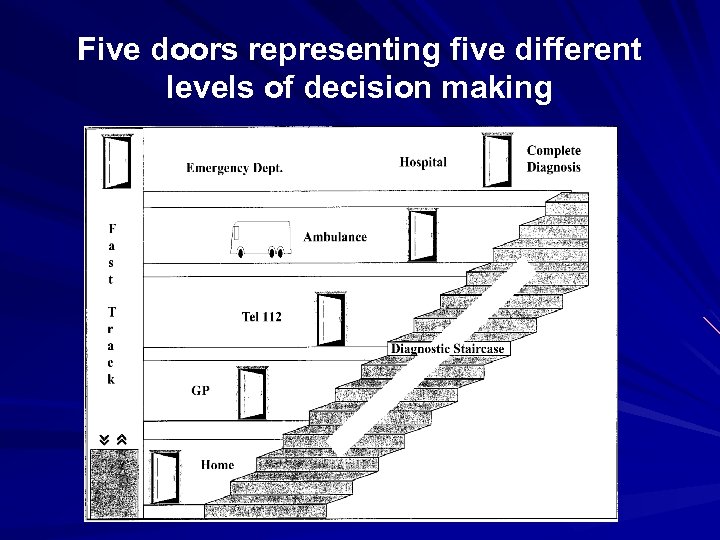
Five doors representing five different levels of decision making
Selection of Reperfusion Strategy in STEMI Majority of the hospitals are not PCI enabled. most of PCI enabled hospitals do not have inhouse interventional Cardiologists & paramedics to carry out interventional procedures round the clock. Availability of transport, long transportation time, traffic congestion & weather condition affects access to the PCI enabled centre.

Accounts / Billing section From where, I get 2. 0 lacs at this time in night !!! Your patient needs PPCI. Deposit Rs. 2. 0 lacs immediately for PCI
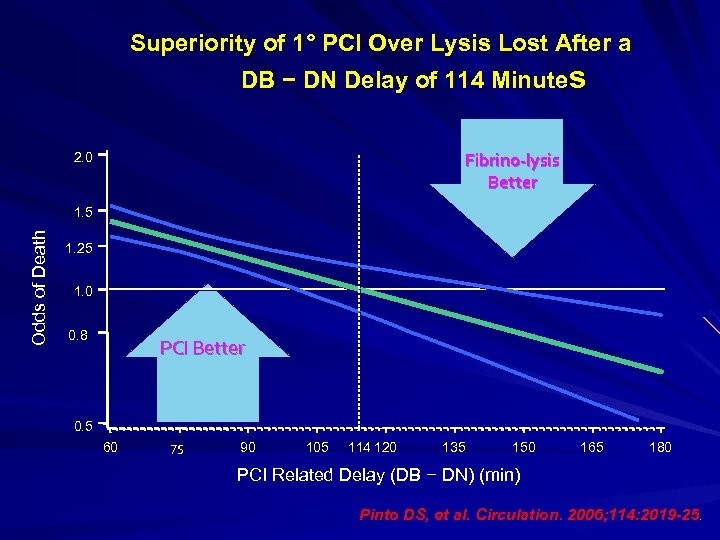
Superiority of 1° PCI Over Lysis Lost After a DB − DN Delay of 114 Minutes Fibrino-lysis Better 2. 0 O dds of Deat h 1. 5 1. 25 1. 0 0. 8 PCI Better 0. 5 60 75 90 105 114 120 135 150 165 180 PCI Related Delay (DB − DN) (min) Pinto DS, et al. Circulation. 2006; 114: 2019 -25.
Myocardial perfusion, not the epicardial perfusion is the final determinants……
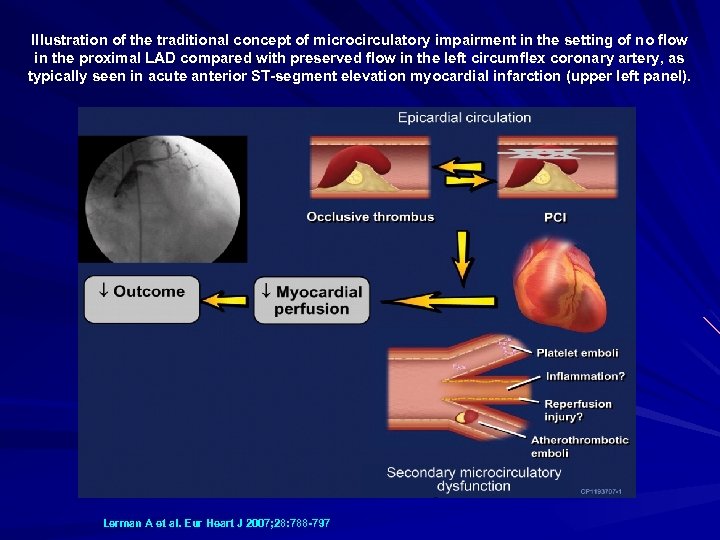
Illustration of the traditional concept of microcirculatory impairment in the setting of no flow in the proximal LAD compared with preserved flow in the left circumflex coronary artery, as typically seen in acute anterior ST-segment elevation myocardial infarction (upper left panel). Lerman A et al. Eur Heart J 2007; 28: 788 -797
“Despite the proven success of restoration of epicardial coronary blood flow in a reasonably timely fashion, reperfusion on the myocardial level is not accomplished in ~50% of patients with STEMI and is of negative prognostic implication” Lerman et al; European Heart Journal 2007
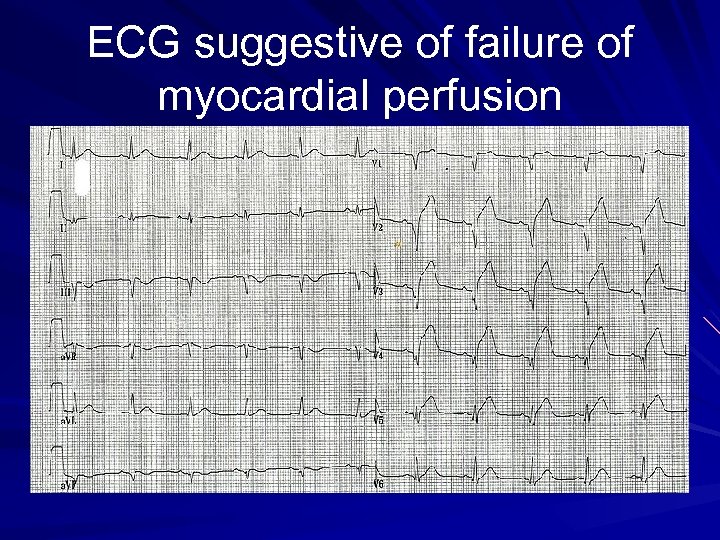
ECG suggestive of failure of myocardial perfusion
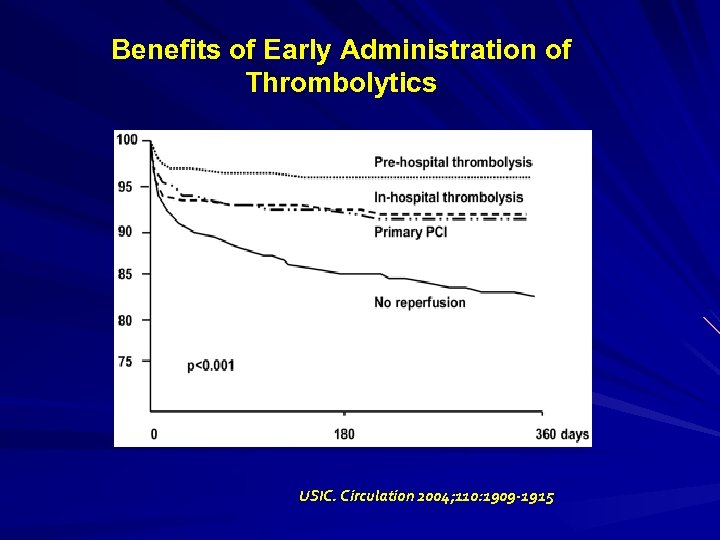
Benefits of Early Administration of Thrombolytics n = 1, 922 USIC. Circulation 2004; 110: 1909 -1915
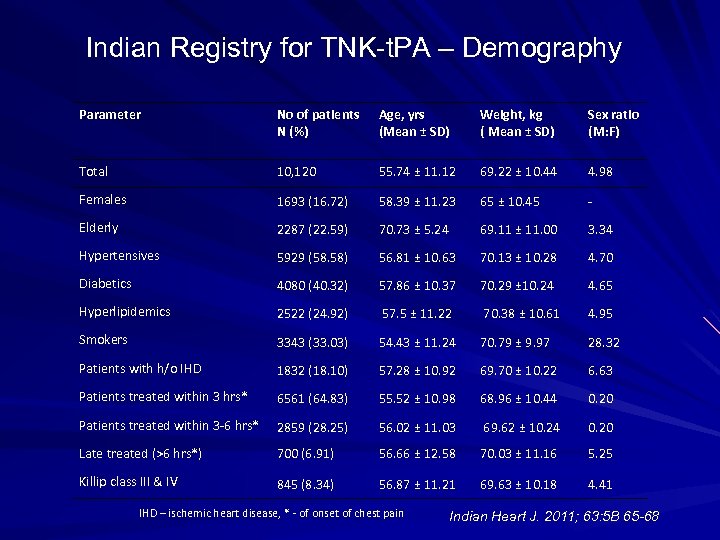
Indian Registry for TNK-t. PA – Demography Parameter No of patients N (%) Age, yrs (Mean ± SD) Weight, kg ( Mean ± SD) Sex ratio (M: F) Total 10, 120 55. 74 ± 11. 12 69. 22 ± 10. 44 4. 98 Females 1693 (16. 72) 58. 39 ± 11. 23 65 ± 10. 45 - Elderly 2287 (22. 59) 70. 73 ± 5. 24 69. 11 ± 11. 00 3. 34 Hypertensives 5929 (58. 58) 56. 81 ± 10. 63 70. 13 ± 10. 28 4. 70 Diabetics 4080 (40. 32) 57. 86 ± 10. 37 70. 29 ± 10. 24 4. 65 Hyperlipidemics 2522 (24. 92) 57. 5 ± 11. 22 70. 38 ± 10. 61 4. 95 Smokers 3343 (33. 03) 54. 43 ± 11. 24 70. 79 ± 9. 97 28. 32 Patients with h/o IHD 1832 (18. 10) 57. 28 ± 10. 92 69. 70 ± 10. 22 6. 63 Patients treated within 3 hrs* 6561 (64. 83) 55. 52 ± 10. 98 68. 96 ± 10. 44 0. 20 Patients treated within 3 -6 hrs* 2859 (28. 25) 56. 02 ± 11. 03 69. 62 ± 10. 24 0. 20 Late treated (>6 hrs*) 700 (6. 91) 56. 66 ± 12. 58 70. 03 ± 11. 16 5. 25 Killip class III & IV 845 (8. 34) 56. 87 ± 11. 21 69. 63 ± 10. 18 4. 41 IHD – ischemic heart disease, * - of onset of chest pain Indian Heart J. 2011; 63: 5 B 65 -68
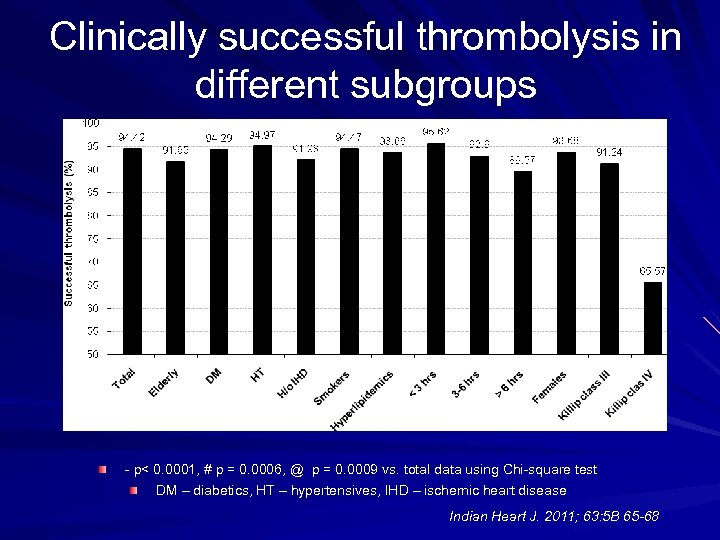
Clinically successful thrombolysis in different subgroups * # * * @ * * - p< 0. 0001, # p = 0. 0006, @ p = 0. 0009 vs. total data using Chi-square test DM – diabetics, HT – hypertensives, IHD – ischemic heart disease Indian Heart J. 2011; 63: 5 B 65 -68
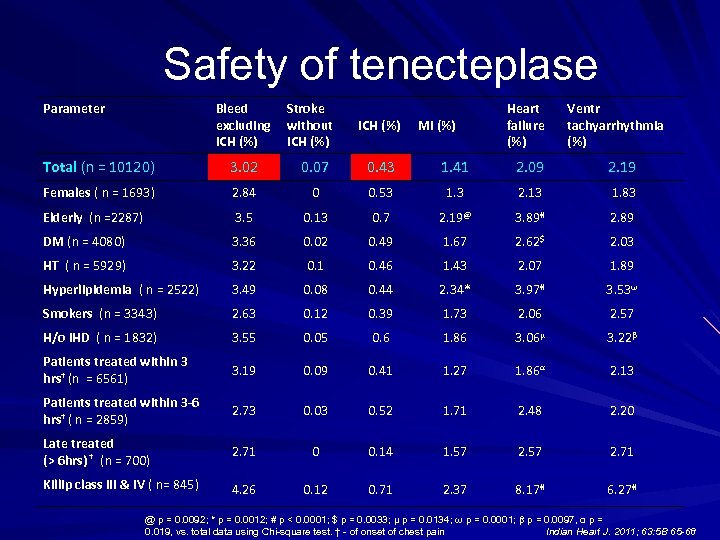
Safety of tenecteplase Parameter Bleed excluding ICH (%) Stroke without ICH (%) MI (%) Heart failure (%) Ventr tachyarrhythmia (%) Total (n = 10120) 3. 02 0. 07 0. 43 1. 41 2. 09 2. 19 Females ( n = 1693) 2. 84 0 0. 53 1. 3 2. 13 1. 83 Elderly (n =2287) 3. 5 0. 13 0. 7 2. 19@ 3. 89# 2. 89 DM (n = 4080) 3. 36 0. 02 0. 49 1. 67 2. 62$ 2. 03 HT ( n = 5929) 3. 22 0. 1 0. 46 1. 43 2. 07 1. 89 Hyperlipidemia ( n = 2522) 3. 49 0. 08 0. 44 2. 34* 3. 97# 3. 53ω Smokers (n = 3343) 2. 63 0. 12 0. 39 1. 73 2. 06 2. 57 H/o IHD ( n = 1832) 3. 55 0. 05 0. 6 1. 86 3. 06μ 3. 22β Patients treated within 3 hrs† (n = 6561) 3. 19 0. 09 0. 41 1. 27 1. 86α 2. 13 Patients treated within 3 -6 hrs† ( n = 2859) 2. 73 0. 03 0. 52 1. 71 2. 48 2. 20 Late treated (> 6 hrs) † (n = 700) 2. 71 0 0. 14 1. 57 2. 71 Killip class III & IV ( n= 845) 4. 26 0. 12 0. 71 2. 37 8. 17# 6. 27# @ p = 0. 0092; * p = 0. 0012; # p < 0. 0001; $ p = 0. 0033; μ p = 0. 0134; ω p = 0. 0001; β p = 0. 0097, α p = Indian Heart J. 2011; 63: 5 B 65 -68 0. 019, vs. total data using Chi-square test. † - of onset of chest pain
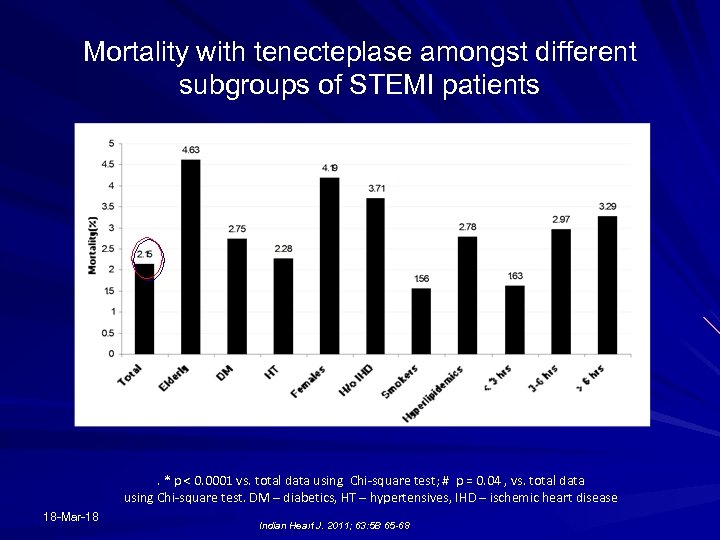
Mortality with tenecteplase amongst different subgroups of STEMI patients * * * # . * p < 0. 0001 vs. total data using Chi-square test; # p = 0. 04 , vs. total data using Chi-square test. DM – diabetics, HT – hypertensives, IHD – ischemic heart disease 18 -Mar-18 Indian Heart J. 2011; 63: 5 B 65 -68
Conclusion The results of this large observational study in clinical practice, in 10, 120 patients of STEMI, confirm safety and efficacy of indigenous tenecteplase in Indian STEMI patients including high-risk subgroups. This study reiterates the importance of early thrombolysis for better success rates and highlights the recognition of high-risk subgroups of STEMI patients who may have higher mortality and adverse outcomes compared to others. Indian Heart J. 2011; 63: 5 B 65 -68
Despite the clinical superiority of PAMI, thrombolytic therapy is the default treatment in many countries due to the practical limitations of PAMI
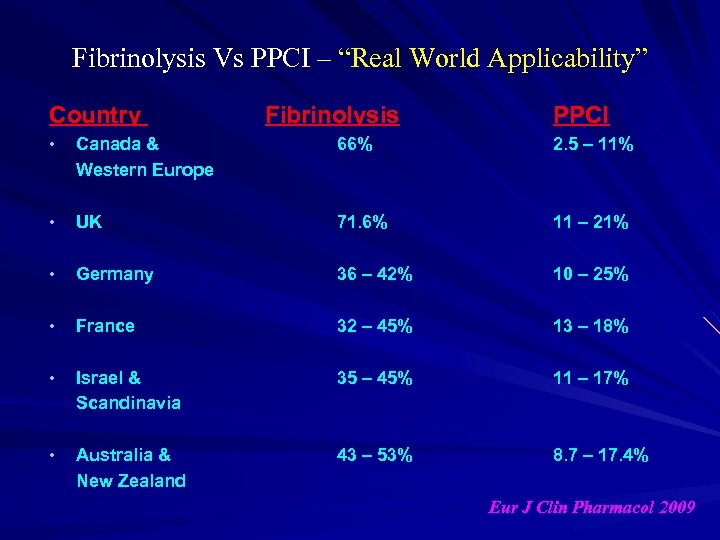
Fibrinolysis Vs PPCI – “Real World Applicability” Country Fibrinolysis PPCI • Canada & Western Europe 66% 2. 5 – 11% • UK 71. 6% 11 – 21% • Germany 36 – 42% 10 – 25% • France 32 – 45% 13 – 18% • Israel & Scandinavia 35 – 45% 11 – 17% • Australia & New Zealand 43 – 53% 8. 7 – 17. 4% Eur J Clin Pharmacol 2009
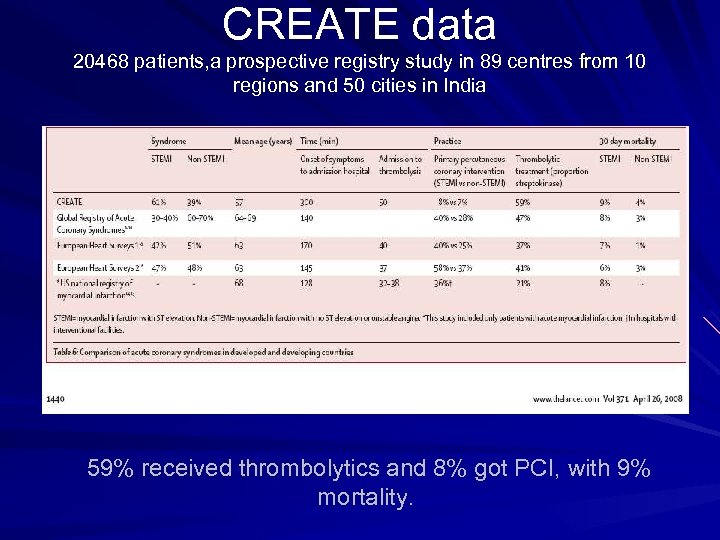
CREATE data 20468 patients, a prospective registry study in 89 centres from 10 regions and 50 cities in India 59% received thrombolytics and 8% got PCI, with 9% mortality.
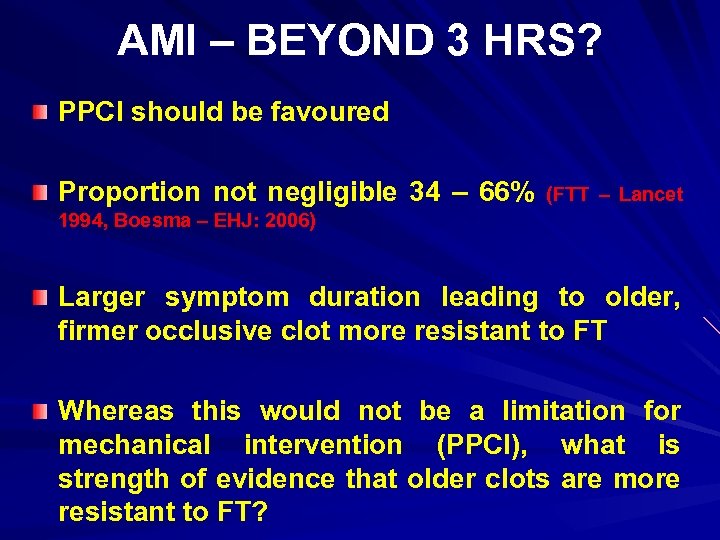
AMI – BEYOND 3 HRS? PPCI should be favoured Proportion not negligible 34 – 66% (FTT – Lancet 1994, Boesma – EHJ: 2006) Larger symptom duration leading to older, firmer occlusive clot more resistant to FT Whereas this would not be a limitation for mechanical intervention (PPCI), what is strength of evidence that older clots are more resistant to FT?
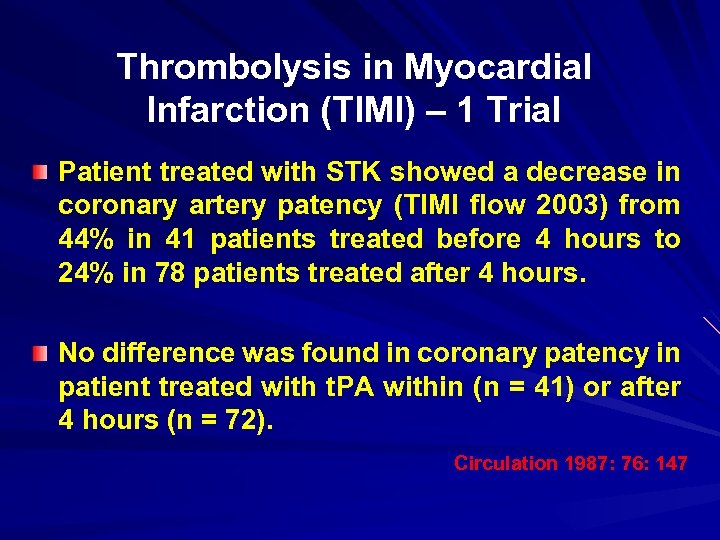
Thrombolysis in Myocardial Infarction (TIMI) – 1 Trial Patient treated with STK showed a decrease in coronary artery patency (TIMI flow 2003) from 44% in 41 patients treated before 4 hours to 24% in 78 patients treated after 4 hours. No difference was found in coronary patency in patient treated with t. PA within (n = 41) or after 4 hours (n = 72). Circulation 1987: 76: 147
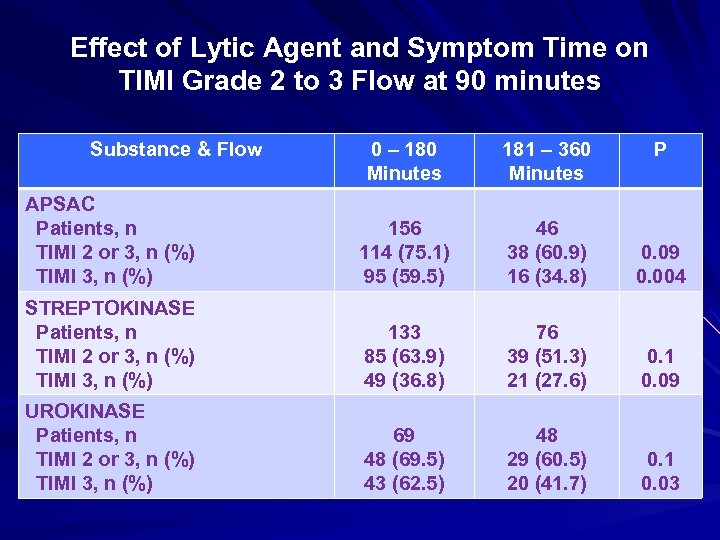
Effect of Lytic Agent and Symptom Time on TIMI Grade 2 to 3 Flow at 90 minutes Substance & Flow 0 – 180 Minutes 181 – 360 Minutes P APSAC Patients, n TIMI 2 or 3, n (%) TIMI 3, n (%) 156 114 (75. 1) 95 (59. 5) 46 38 (60. 9) 16 (34. 8) 0. 09 0. 004 STREPTOKINASE Patients, n TIMI 2 or 3, n (%) TIMI 3, n (%) 133 85 (63. 9) 49 (36. 8) 76 39 (51. 3) 21 (27. 6) 0. 1 0. 09 UROKINASE Patients, n TIMI 2 or 3, n (%) TIMI 3, n (%) 69 48 (69. 5) 43 (62. 5) 48 29 (60. 5) 20 (41. 7) 0. 1 0. 03
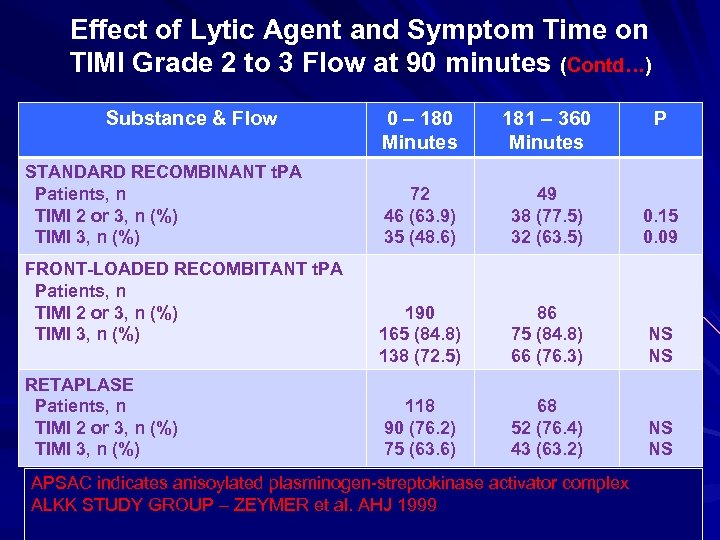
Effect of Lytic Agent and Symptom Time on TIMI Grade 2 to 3 Flow at 90 minutes (Contd…) Substance & Flow STANDARD RECOMBINANT t. PA Patients, n TIMI 2 or 3, n (%) TIMI 3, n (%) FRONT-LOADED RECOMBITANT t. PA Patients, n TIMI 2 or 3, n (%) TIMI 3, n (%) RETAPLASE Patients, n TIMI 2 or 3, n (%) TIMI 3, n (%) 0 – 180 Minutes 181 – 360 Minutes 72 46 (63. 9) 35 (48. 6) 49 38 (77. 5) 32 (63. 5) 0. 15 0. 09 190 165 (84. 8) 138 (72. 5) 86 75 (84. 8) 66 (76. 3) NS NS 118 90 (76. 2) 75 (63. 6) 68 52 (76. 4) 43 (63. 2) NS NS APSAC indicates anisoylated plasminogen-streptokinase activator complex ALKK STUDY GROUP – ZEYMER et al. AHJ 1999 P
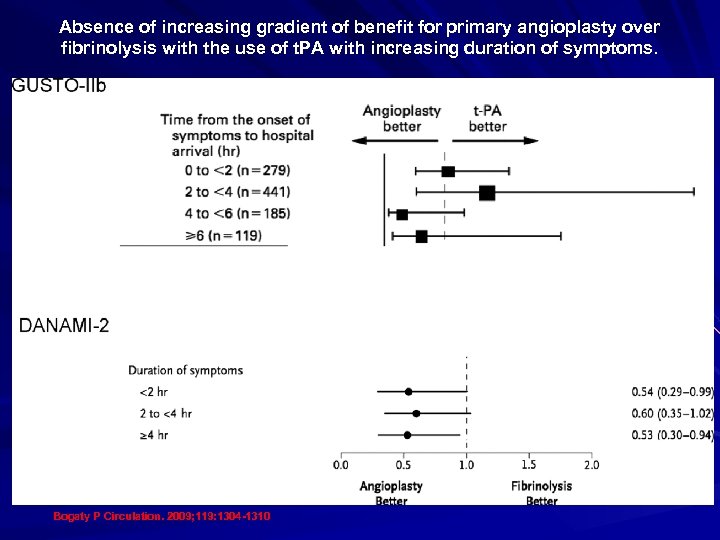
Absence of increasing gradient of benefit for primary angioplasty over fibrinolysis with the use of t. PA with increasing duration of symptoms. Bogaty P Circulation. 2009; 119: 1304 -1310
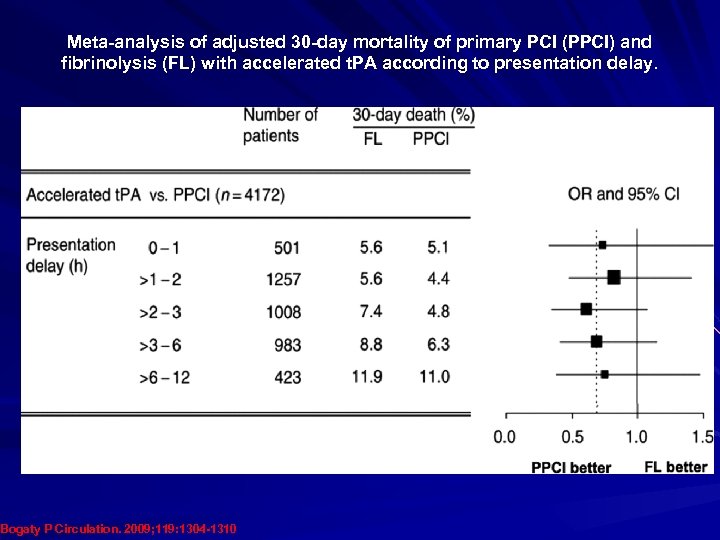
Meta-analysis of adjusted 30 -day mortality of primary PCI (PPCI) and fibrinolysis (FL) with accelerated t. PA according to presentation delay. Bogaty P Circulation. 2009; 119: 1304 -1310
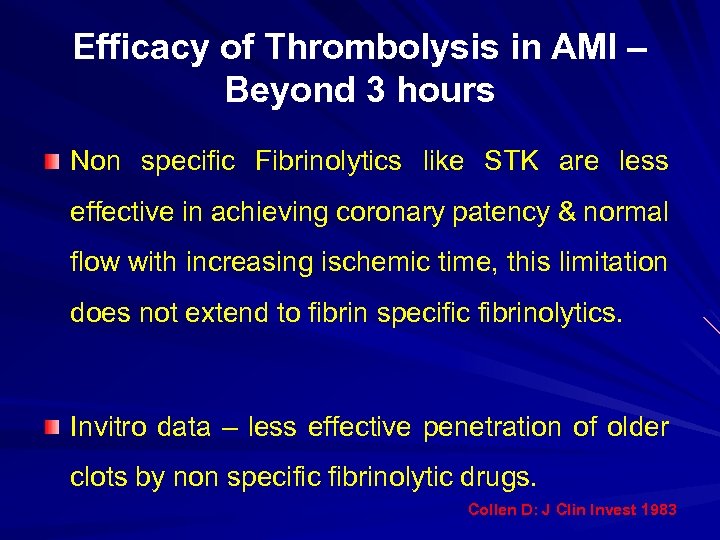
Efficacy of Thrombolysis in AMI – Beyond 3 hours Non specific Fibrinolytics like STK are less effective in achieving coronary patency & normal flow with increasing ischemic time, this limitation does not extend to fibrin specific fibrinolytics. Invitro data – less effective penetration of older clots by non specific fibrinolytic drugs. Collen D: J Clin Invest 1983
Total Ischemic Time (The Correct Focus of Attention for Optimal STEMI Care) “Just as with FT, mortality with primary PCI is indeed Ischemic time dependent” Luca et al: Circulation 2004 Boersma et al: EHJ 2006
“Beyond consideration of relative efficacies of FT & PPCI in “opening up” of acutely occluded coronary arteries, larger ischemic time lessen the chances for successful myocardial reperfusion, as evaluated by ST segment resolution or myocardial blush grade, whether the method of reperfusion is FT or PPCI”. Luca et al: Circulation 2004 Coustantini et al: JACC 2004 Gibbon et al: Circulation 2004
Should Symptom duration Intervene in the choice of Reperfusion Therapy in STEMI? “In the golden hour, when symptom duration is within 1 to 2 hours, prompt FT may provide clinical benefit compared with primary PCI & should be considered as a potentially preferable option”. “Beyond this critical time window, the available data suggest that symptoms duration need not guide the choice of reperfusion therapy, provided that the Fibrinolytic drug considered for use is fibrin specific”. Peter Bogaty: Circulation 2009
Pharmaco-Invasive Strategy Rationale Local rapid, cheap thrombolysis PCI routinely – thrombolysis (1/3) Non responder to
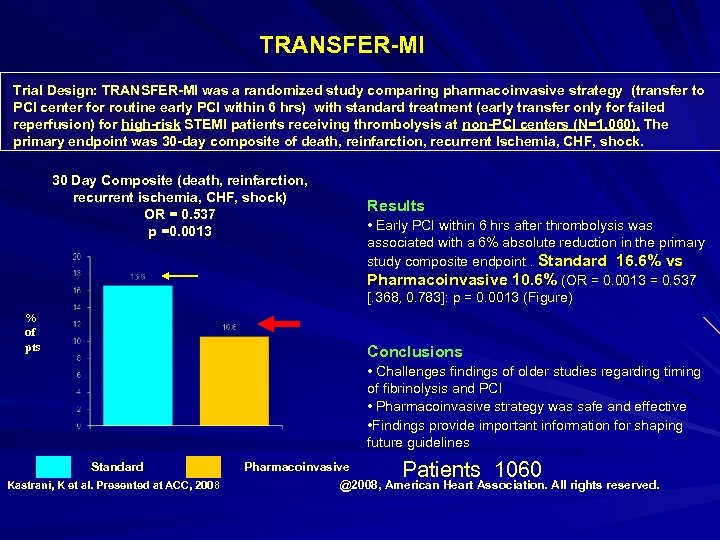
TRANSFER-MI Trial Design: TRANSFER-MI was a randomized study comparing pharmacoinvasive strategy (transfer to PCI center for routine early PCI within 6 hrs) with standard treatment (early transfer only for failed reperfusion) for high-risk STEMI patients receiving thrombolysis at non-PCI centers (N=1, 060). The primary endpoint was 30 -day composite of death, reinfarction, recurrent Ischemia, CHF, shock. 30 Day Composite (death, reinfarction, recurrent ischemia, CHF, shock) OR = 0. 537 p =0. 0013 % of pts Results • Early PCI within 6 hrs after thrombolysis was associated with a 6% absolute reduction in the primary study composite endpoint. Standard 16. 6% vs Pharmacoinvasive 10. 6% (OR = 0. 0013 = 0. 537 [. 368, 0. 783]: p = 0. 0013 (Figure) Conclusions • Challenges findings of older studies regarding timing of fibrinolysis and PCI • Pharmacoinvasive strategy was safe and effective • Findings provide important information for shaping future guidelines Standard Kastrani, K et al. Presented at ACC, 2008 Patients 1060 Pharmacoinvasive @2008, American Heart Association. All rights reserved.
NORDISTEMI Objective : To compare a strategy of immediate transfer for percutaneous coronary intervention (PCI) with an ischemia-guided approach after thrombolysis in patients with very long transfer distances to PCI. (J Am Coll Cardiol 2010; 55: 102– 10)
Methods NORDISTEMI A total of 266 patients with acute STEMI living in rural areas with more than 90 -min transfer delays to PCI were treated with tenecteplase, aspirin, enoxaparin, and clopidogrel and randomized to immediate transfer for PCI or to standard management in the local hospitals with early transfer, only if indicated for rescue or clinical deterioration. The primary outcome was a composite of death, reinfarction, stroke, or new ischemia at 12 months, and analysis was by intention to treat. (J Am Coll Cardiol 2010; 55: 102– 10)
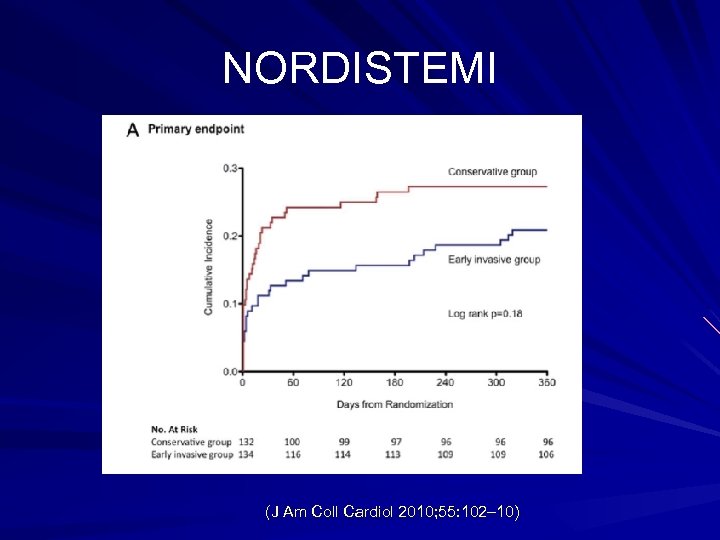
NORDISTEMI (J Am Coll Cardiol 2010; 55: 102– 10)
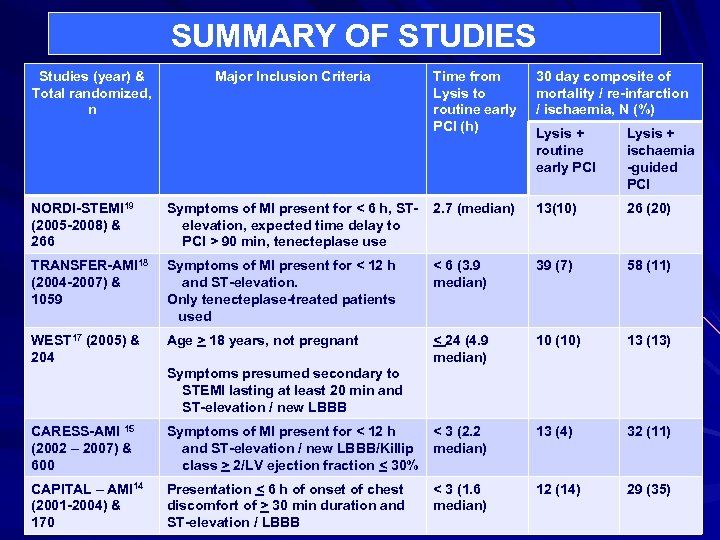
SUMMARY OF STUDIES Studies (year) & Total randomized, n Major Inclusion Criteria Time from Lysis to routine early PCI (h) 30 day composite of mortality / re-infarction / ischaemia, N (%) Lysis + routine early PCI Lysis + ischaemia -guided PCI NORDI-STEMI 19 (2005 -2008) & 266 Symptoms of MI present for < 6 h, STelevation, expected time delay to PCI > 90 min, tenecteplase use 2. 7 (median) 13(10) 26 (20) TRANSFER-AMI 18 (2004 -2007) & 1059 Symptoms of MI present for < 12 h and ST-elevation. Only tenecteplase-treated patients used < 6 (3. 9 median) 39 (7) 58 (11) WEST 17 (2005) & 204 Age > 18 years, not pregnant < 24 (4. 9 median) 10 (10) 13 (13) Symptoms presumed secondary to STEMI lasting at least 20 min and ST-elevation / new LBBB CARESS-AMI 15 (2002 – 2007) & 600 Symptoms of MI present for < 12 h and ST-elevation / new LBBB/Killip class > 2/LV ejection fraction < 30% < 3 (2. 2 median) 13 (4) 32 (11) CAPITAL – AMI 14 (2001 -2004) & 170 Presentation < 6 h of onset of chest discomfort of > 30 min duration and ST-elevation / LBBB < 3 (1. 6 median) 12 (14) 29 (35)
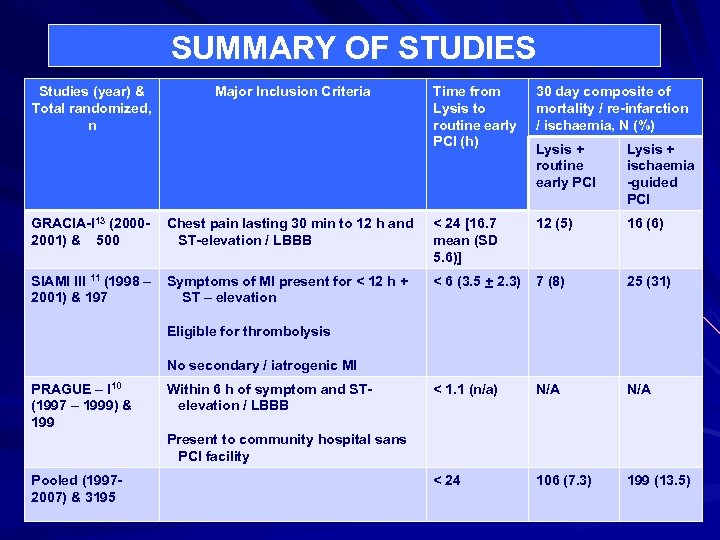
SUMMARY OF STUDIES Studies (year) & Total randomized, n Major Inclusion Criteria Time from Lysis to routine early PCI (h) 30 day composite of mortality / re-infarction / ischaemia, N (%) Lysis + routine early PCI Lysis + ischaemia -guided PCI GRACIA-I 13 (20002001) & 500 Chest pain lasting 30 min to 12 h and ST-elevation / LBBB < 24 [16. 7 mean (SD 5. 6)] 12 (5) 16 (6) SIAMI III 11 (1998 – 2001) & 197 Symptoms of MI present for < 12 h + ST – elevation < 6 (3. 5 + 2. 3) 7 (8) 25 (31) < 1. 1 (n/a) N/A < 24 106 (7. 3) 199 (13. 5) Eligible for thrombolysis No secondary / iatrogenic MI PRAGUE – I 10 (1997 – 1999) & 199 Within 6 h of symptom and STelevation / LBBB Present to community hospital sans PCI facility Pooled (19972007) & 3195
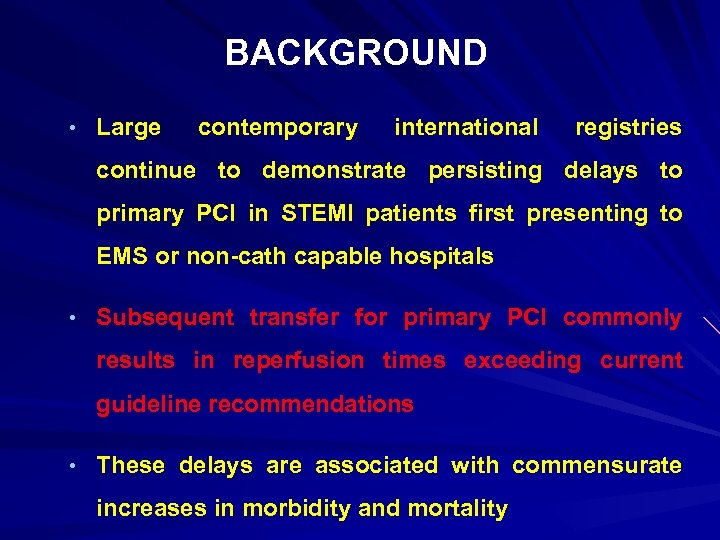
BACKGROUND • Large contemporary international registries continue to demonstrate persisting delays to primary PCI in STEMI patients first presenting to EMS or non-cath capable hospitals • Subsequent transfer for primary PCI commonly results in reperfusion times exceeding current guideline recommendations • These delays are associated with commensurate increases in morbidity and mortality
STREAM STRATEGIC REPERFUSION EARLY AFTER MYOCARDIAL INFARCTION ACC 2013
Dr. Lekha Adik Pathak
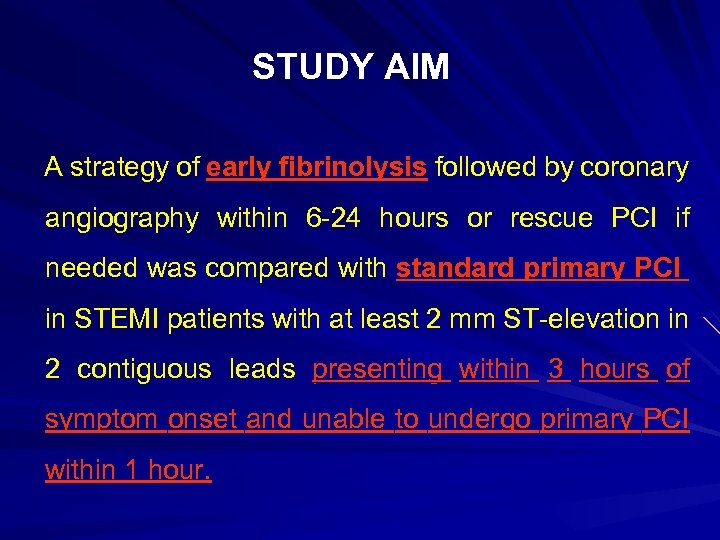
STUDY AIM A strategy of early fibrinolysis followed by coronary angiography within 6 -24 hours or rescue PCI if needed was compared with standard primary PCI in STEMI patients with at least 2 mm ST-elevation in 2 contiguous leads presenting within 3 hours of symptom onset and unable to undergo primary PCI within 1 hour.
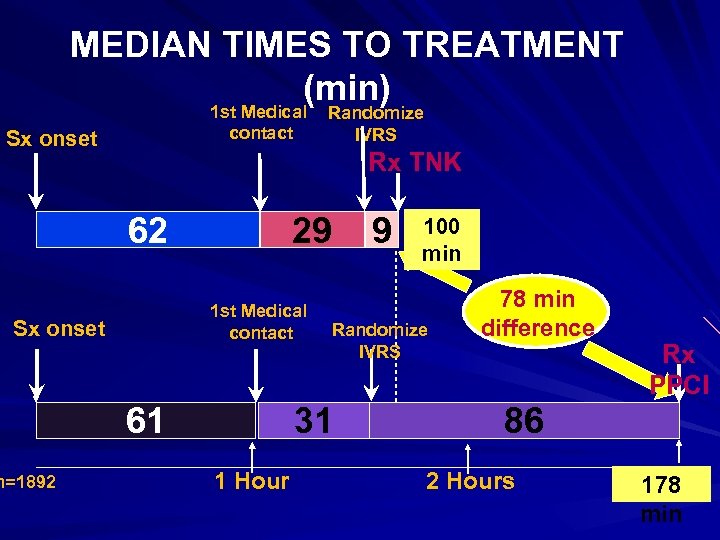
MEDIAN TIMES TO TREATMENT (min) 1 st Medical contact Sx onset Rx TNK 62 29 1 st Medical contact Sx onset n=1892 Randomize IVRS 61 100 min Randomize IVRS 31 1 Hour 9 78 min difference Rx PPCI 86 2 Hours 178 min
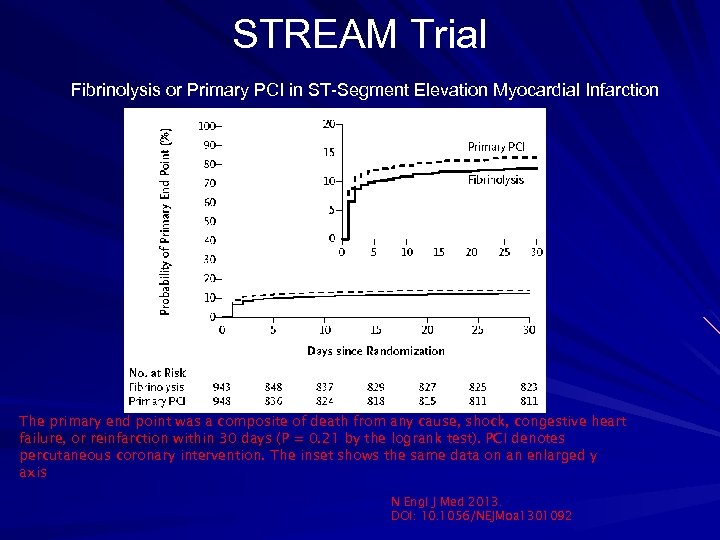
STREAM Trial Fibrinolysis or Primary PCI in ST-Segment Elevation Myocardial Infarction The primary end point was a composite of death from any cause, shock, congestive heart failure, or reinfarction within 30 days (P = 0. 21 by the logrank test). PCI denotes percutaneous coronary intervention. The inset shows the same data on an enlarged y axis N Engl J Med 2013. DOI: 10. 1056/NEJMoa 1301092
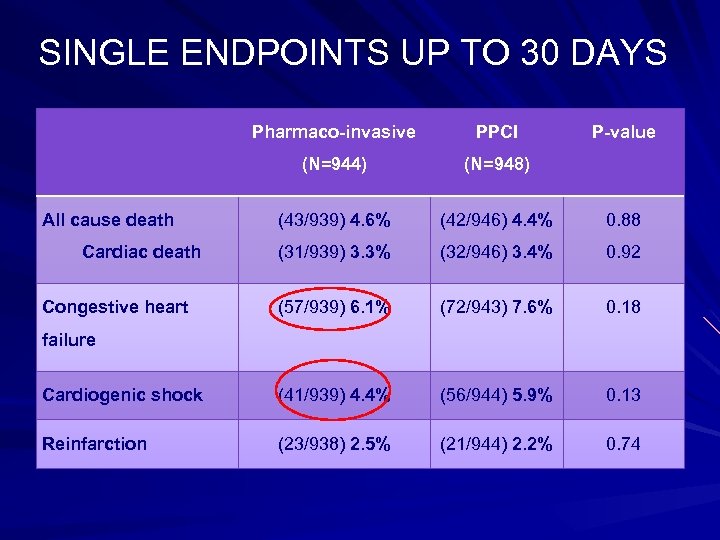
SINGLE ENDPOINTS UP TO 30 DAYS Pharmaco-invasive PPCI (N=944) (N=948) (43/939) 4. 6% (42/946) 4. 4% 0. 88 (31/939) 3. 3% (32/946) 3. 4% 0. 92 (57/939) 6. 1% (72/943) 7. 6% 0. 18 Cardiogenic shock (41/939) 4. 4% (56/944) 5. 9% 0. 13 Reinfarction (23/938) 2. 5% (21/944) 2. 2% 0. 74 All cause death Cardiac death Congestive heart P-value failure
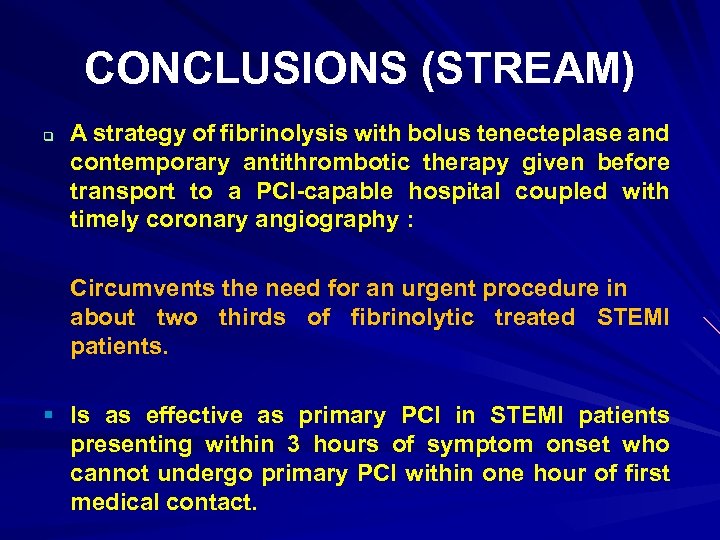
CONCLUSIONS (STREAM) q A strategy of fibrinolysis with bolus tenecteplase and contemporary antithrombotic therapy given before transport to a PCI-capable hospital coupled with timely coronary angiography : Circumvents the need for an urgent procedure in about two thirds of fibrinolytic treated STEMI patients. § Is as effective as primary PCI in STEMI patients presenting within 3 hours of symptom onset who cannot undergo primary PCI within one hour of first medical contact.
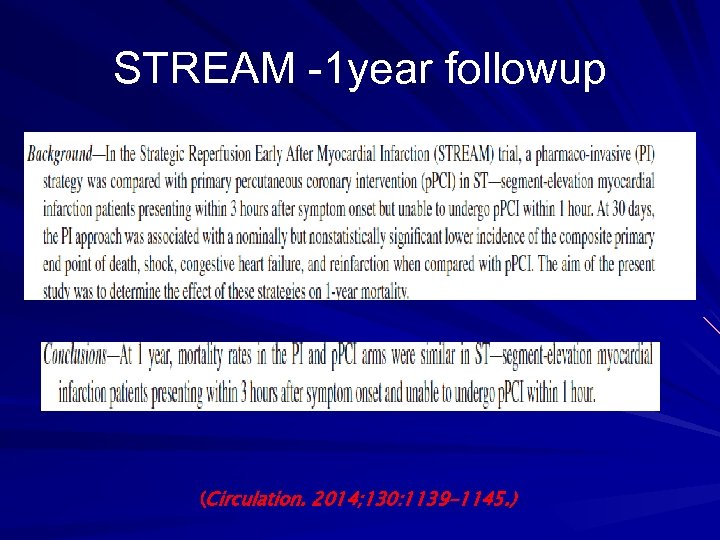
STREAM -1 year followup (Circulation. 2014; 130: 1139 -1145. )
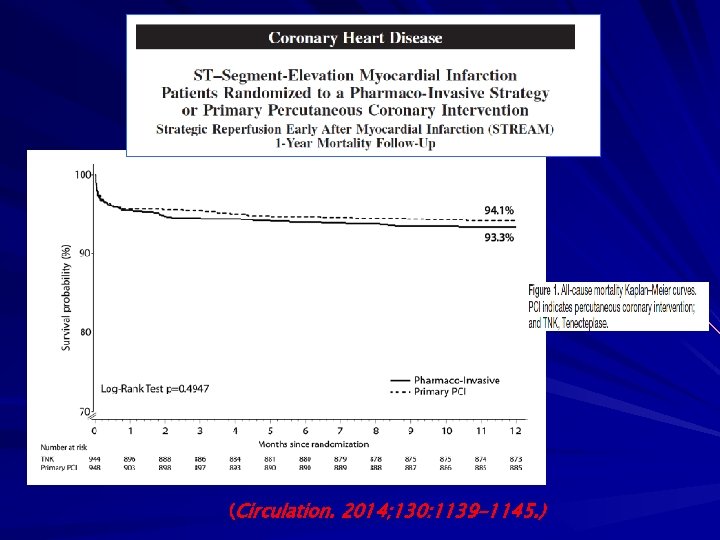
(Circulation. 2014; 130: 1139 -1145. )
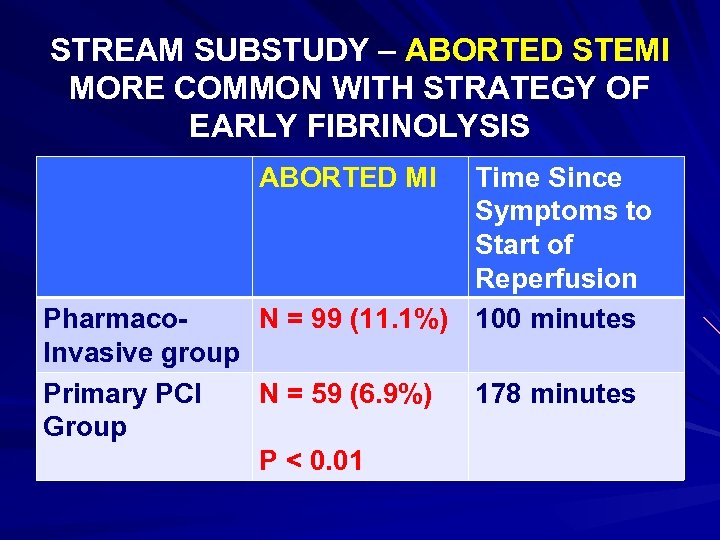
STREAM SUBSTUDY – ABORTED STEMI MORE COMMON WITH STRATEGY OF EARLY FIBRINOLYSIS ABORTED MI Time Since Symptoms to Start of Reperfusion N = 99 (11. 1%) 100 minutes Pharmaco. Invasive group Primary PCI N = 59 (6. 9%) Group P < 0. 01 178 minutes
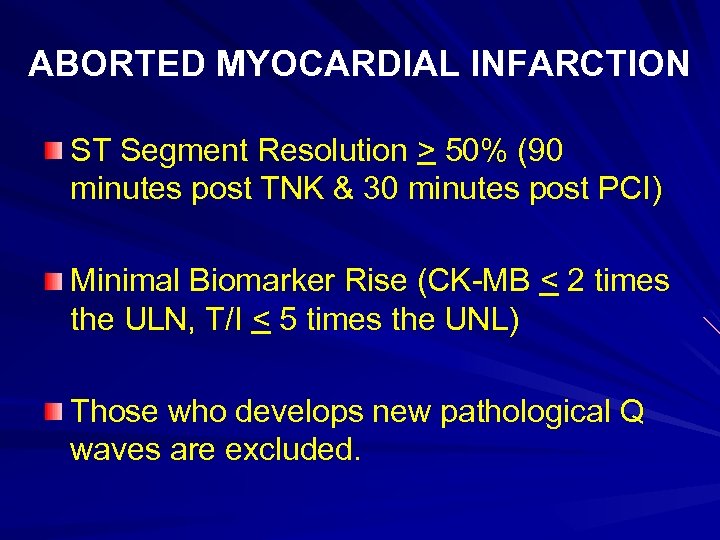
ABORTED MYOCARDIAL INFARCTION ST Segment Resolution > 50% (90 minutes post TNK & 30 minutes post PCI) Minimal Biomarker Rise (CK-MB < 2 times the ULN, T/I < 5 times the UNL) Those who develops new pathological Q waves are excluded.
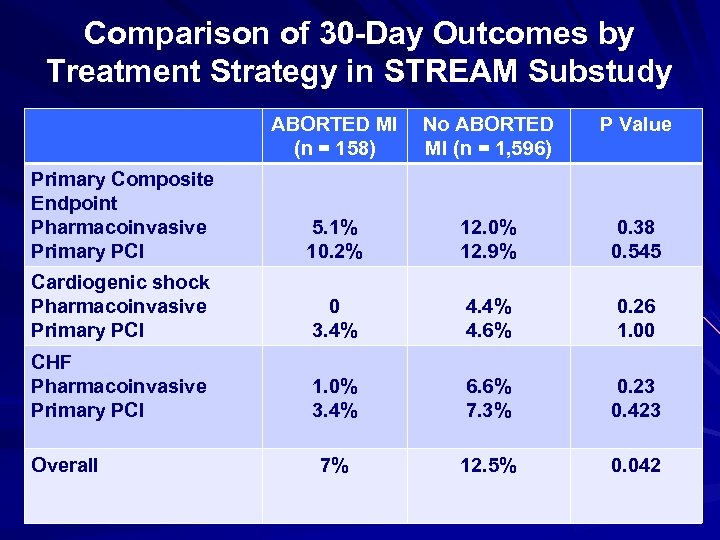
Comparison of 30 -Day Outcomes by Treatment Strategy in STREAM Substudy ABORTED MI (n = 158) No ABORTED MI (n = 1, 596) P Value Primary Composite Endpoint Pharmacoinvasive Primary PCI 5. 1% 10. 2% 12. 0% 12. 9% 0. 38 0. 545 Cardiogenic shock Pharmacoinvasive Primary PCI 0 3. 4% 4. 6% 0. 26 1. 00 CHF Pharmacoinvasive Primary PCI 1. 0% 3. 4% 6. 6% 7. 3% 0. 23 0. 423 7% 12. 5% 0. 042 Overall
STREAM SUBSTUDY: ABORTION OF STEMI ONE YEAR FOLLOW UP All Cause Mortality Aborted MI Vs Non-aborted MI 3. 1% Vs 4. 5% (P =. 818)
Can we Extrapolate these results to our Healthcare System? STREAM STUDY – Included patients with a symptom onset to FMC < 3 hours FAST MI – Two third received prehospital thrombolysis -----------------------------Whether these findings are also applicable to late presenters?
FIBRINOLYTICS in all these trials was Tenecteplase (TNK): - extended half life allowing single bolus administration - more fibrin specific - associated with less intra cranial bleeding - higher rate of infarct artery patency compared to streptokinase which is more frequently used fibrinolytic worldwide. q It is unknown whether a pharmaco-invasive approach utilizing streptokinase would yield similar results.
Well Established EMS in France & Countries Conducted Trials, had higher prehospital Fibrinolysis. This set up and high rate of prehospital fibrinolysis is clearly difficult to reproduce in many countries / regions.
WHAT HAVE WE LEARNED? Timely PPCI remains preferred the reperfusion strategy of choice in patients with acute STEMI, but it is not advisable. Findings from STREAM, FAST MI & other studies lend further support to the adoption of a pharmaco-invasive approach in areas where timely PPCI is not achievable. q Effort should be made to strengthen EMS Prehospital thrombolysis - Wireless transmission of 12 lead ECG to an offsite cardiologist Standardized inter hospital transfer protocols to allow for routine post-fibrinolysis angiography & rescue PCI within recommended time in case of failed thrombolysis.
Ultimate objective in setting of Acute STEMI is reducing “Total Ischemic Time” which includes time delay to FMC (It is approximately 30 -60% of total ischemic time). - EMS strengthening Public awareness / Education so as to have effective reduction of patient related delays.
CHHATTISGARH MAP Model Healthcare Accessibility Affordability Availability Applicability
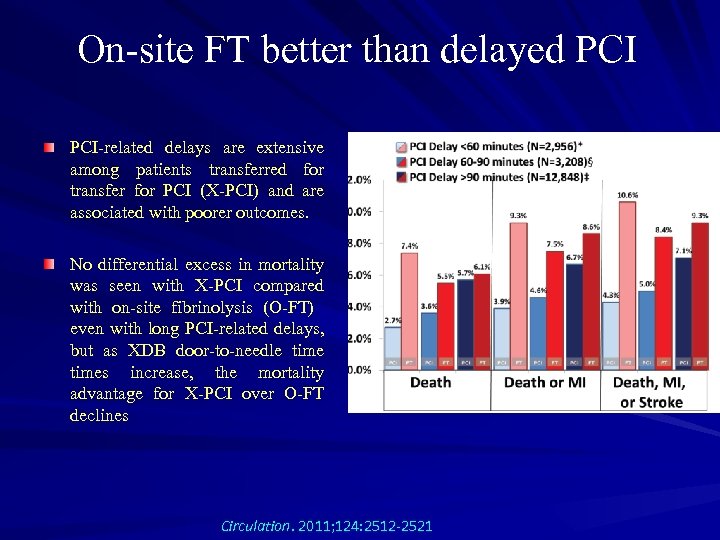
On-site FT better than delayed PCI-related delays are extensive among patients transferred for transfer for PCI (X-PCI) and are associated with poorer outcomes. No differential excess in mortality was seen with X-PCI compared with on-site fibrinolysis (O-FT) even with long PCI-related delays, but as XDB door-to-needle times increase, the mortality advantage for X-PCI over O-FT declines Circulation. 2011; 124: 2512 -2521
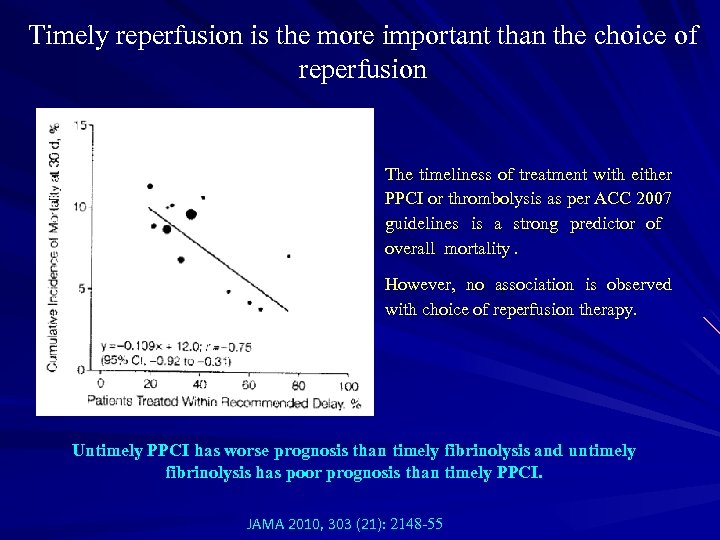
Timely reperfusion is the more important than the choice of reperfusion The timeliness of treatment with either PPCI or thrombolysis as per ACC 2007 guidelines is a strong predictor of overall mortality. However, no association is observed with choice of reperfusion therapy. Untimely PPCI has worse prognosis than timely fibrinolysis and untimely fibrinolysis has poor prognosis than timely PPCI. JAMA 2010, 303 (21): 2148 -55
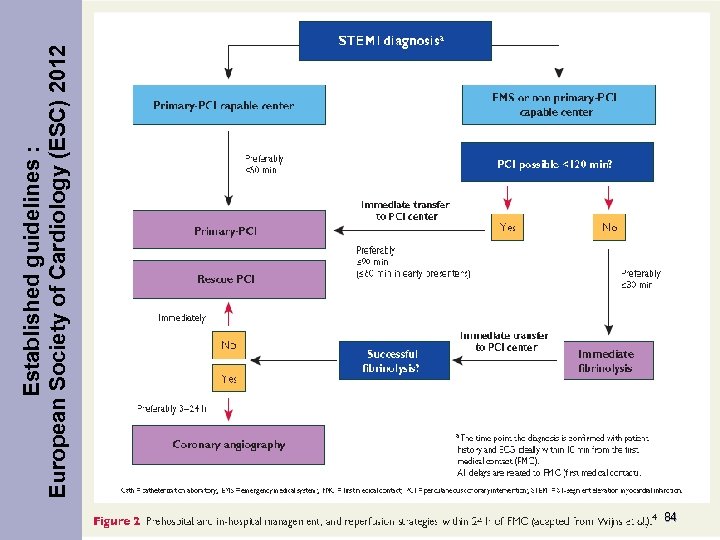
84 Established guidelines : European Society of Cardiology (ESC) 2012
THANK YOU
92fa8a2a4a3b09ef2c113e81618b27a5.ppt