leprosy.ppt
- Количество слайдов: 47
LEPROSY Hansen`s disease
Cause • Mycobacterium leprae (Hansen, 1874) • Straight or slightly curved, acid-fast rod, Gr+ • M. leprae cannot be cultured in vitro
HOST • Main reservoir – Humans • Additional reservoir – wild armadillos, chimpanzees, mangabey monkeys.
Transmission • Mode of transmission is uncertain • Human-to-human transmission • The source of dissemination is multibacillary-type infection • Portals of entry are ingestion (food and drink), inoculation (bites, scratches, small wounds, tattoos), inhalation (nasal passages or lungs)
Pathogenesis • Immune response of the patient (high resistance, low resistance) • Host`s immunologic response • Cell-mediated immunity to M. leprae
Clinicopathologic classification - lepromatous (LL) - low or abcentresistance - tuberculoid (TT) - high resistance - borderline (or “dimorphic”) (BB) - borderline lepromatous (BL) - borderline tuberculoid (BT)
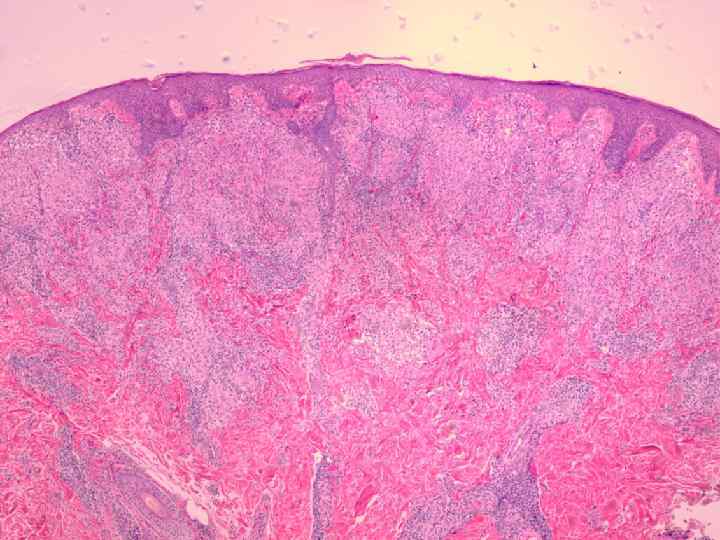
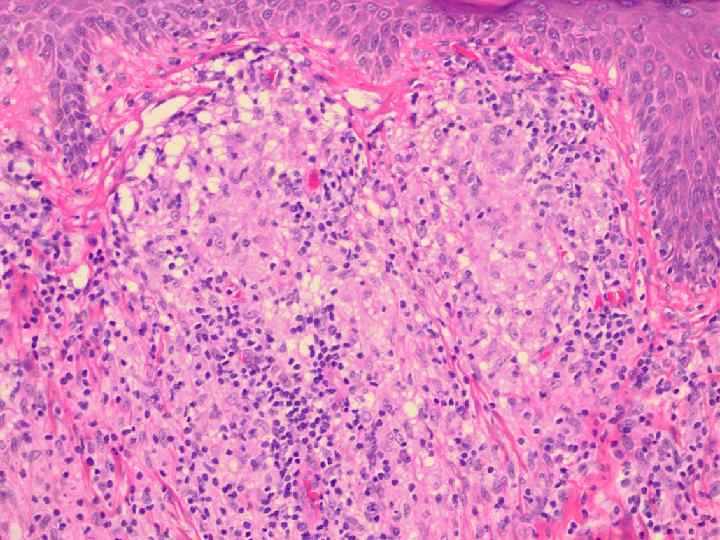
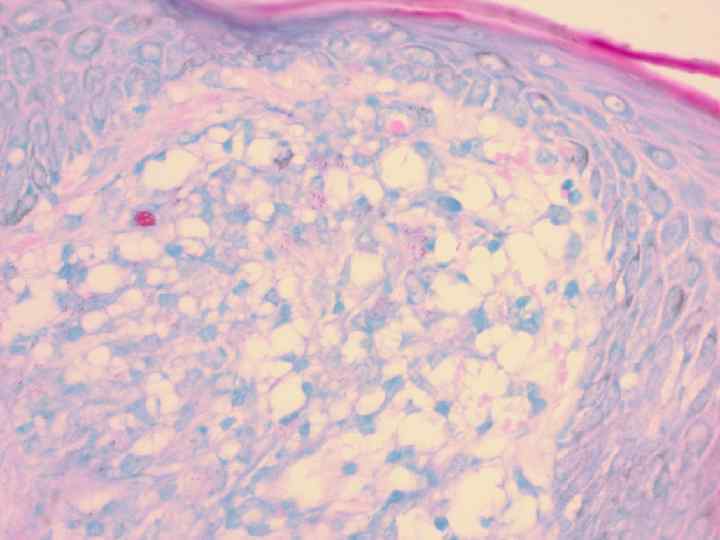
Dermatopathology 1. 2. 3. 4. 5. The type of granuloma (epithelioid cell granulomas-TL, extensive cellular infiltrate – LL) Bacterial index (BI) The number and distribution of lymphocytes Nerves thickened Lepra cells (Virchow cells)
• Multibacillary types (LL, BB) • Paucibacillary types (TT, BT)

Geography Hot and humid climates 53 countries report endemic leprosy 12 million in the world 5. 5 million are receiving chemotherapy 2 -3 million have disabilities 4 million cases – India 2500 patients in US 500 in Russia
Predisposing factors 1) residence in an endemic area 2)Having a blood relative with leprosy 3) Poverty (malnutrition) 4) Contact with affected armadillos
Differential diagnosis • TL- tinea corporis, pityriasis versicolor, seborrheic dermatitis, vitiligo and etc. • LL – cutaneous TBS, dermal leishmaniasis, neurofibromatosis and etc. • BL – late syphilis, lupus erythematosus, cutaneous leishmaniasis • Peripheral neuropathy – tabes dorsalis, peroneal muscular atrophy, syringomyelia, peripheral atrophy of varied etiology

• Lucio`s leprae • LL patients • Large poligonal sloughing ulcerations • Generalized distribution • Secondary bactetrial infection and sepsis
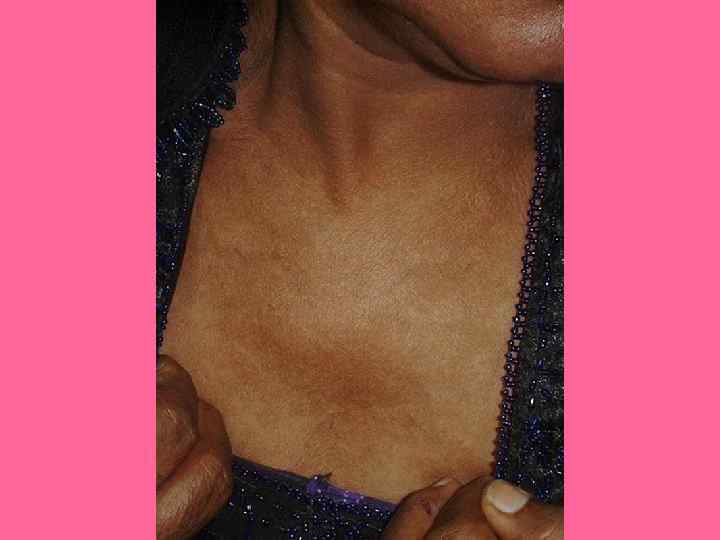
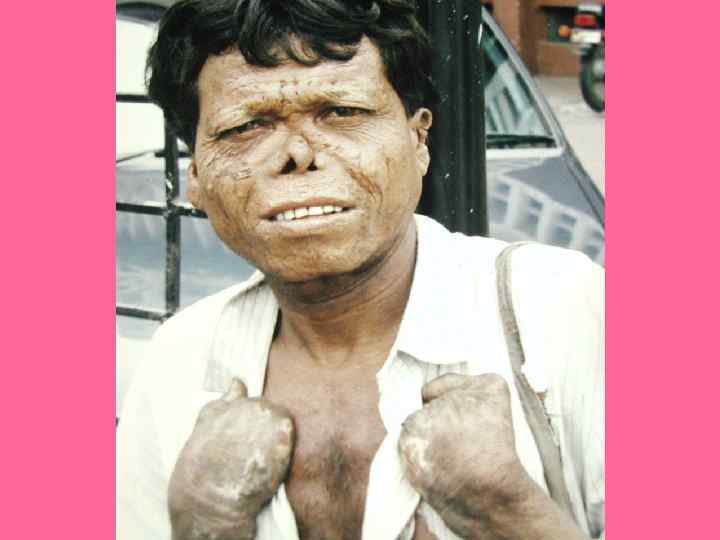
Lepromatous type (clinical appearance) • Macules, papules, nodules, plaques (innumerable, widespread) • Impairment of functions of skin adnexes (glove and stocking anaesthesia, trophic ulcers of periphery, muscle paralysis) • Involvement of many tissues (early involvement of mucosa, internal organs) • Most peripheral nerves thickened (late involvement of nervous system) • Resistant to treatment • Infectious form • Negative lepromin test
Tuberculoid leprosy (clinical appearance) • Early skin manifestations (one or two only) • Sharply marginated macules and plaques • Early affection of peripheral nerves • Non-infectious • Histological investigations only • Positive lepromin test (Page 199)

























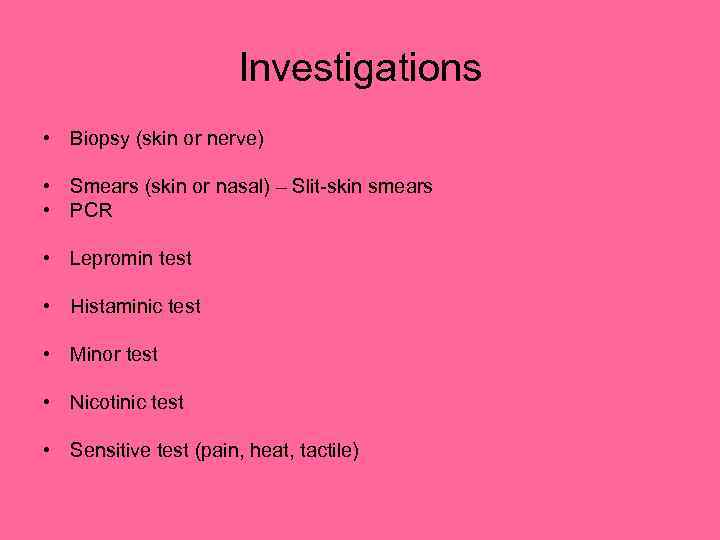
Investigations • Biopsy (skin or nerve) • Smears (skin or nasal) – Slit-skin smears • PCR • Lepromin test • Histaminic test • Minor test • Nicotinic test • Sensitive test (pain, heat, tactile)

Treatment Dapson Rifampicin Clofazimine Antimicrobal agents Orthopedic care_____________ Tuberculoid forms – 6 -12 months Lepromatous form – 2 years
Leprous reactions Type 1 downgrading or reversal reactions (red lesions, pain and paralysis) in BT and BL patients. Type 2 reactions - (erythema nodosum leprosum) nerve palsies, lymphadenopathy, arthritis, iridocyclitis, epididimoorchitis , proteinuria in LL patients. Treatment (steroids, NSAID, antimalarials, salicylates, thalidomide)
leprosy.ppt