3bbb8b49ff94fb7e2de7fda5d5c1c111.ppt
- Количество слайдов: 40
 Lecture 7 Visual Perception (Dr Roger Newport) Hemianopia/Visual Field Cuts Blindsight u Akinetopsia u Achromatopsia u Agnosia Prosopagnosia Split Brain
Lecture 7 Visual Perception (Dr Roger Newport) Hemianopia/Visual Field Cuts Blindsight u Akinetopsia u Achromatopsia u Agnosia Prosopagnosia Split Brain
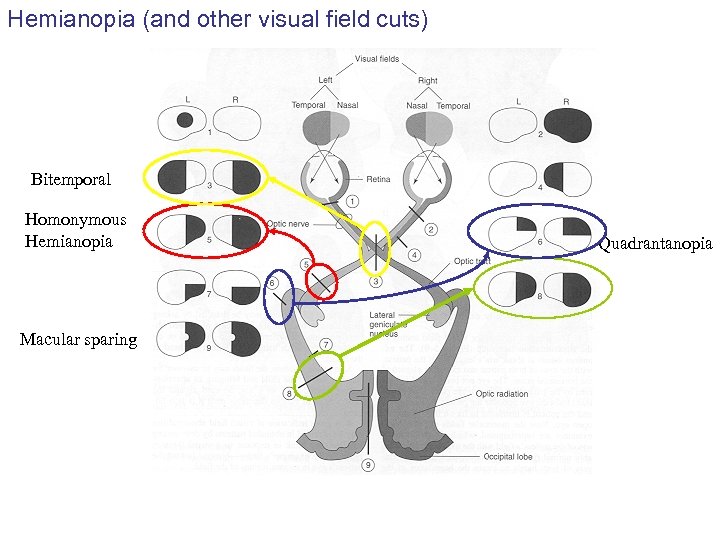 Hemianopia (and other visual field cuts) Bitemporal Homonymous Hemianopia Macular sparing Quadrantanopia
Hemianopia (and other visual field cuts) Bitemporal Homonymous Hemianopia Macular sparing Quadrantanopia
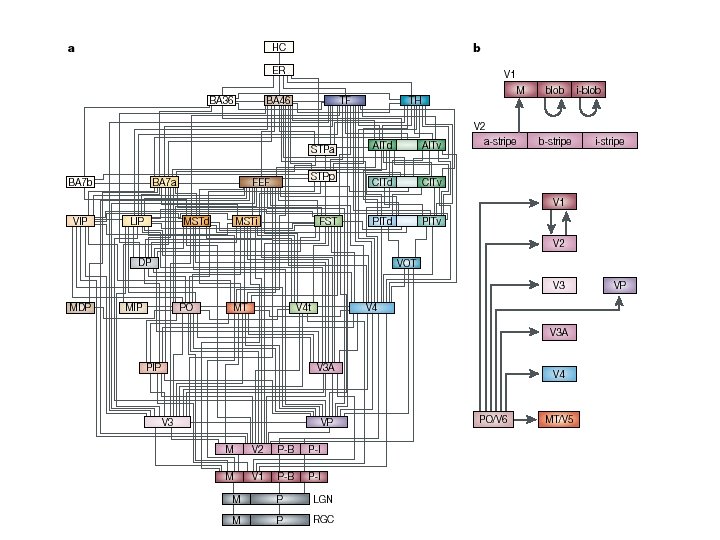
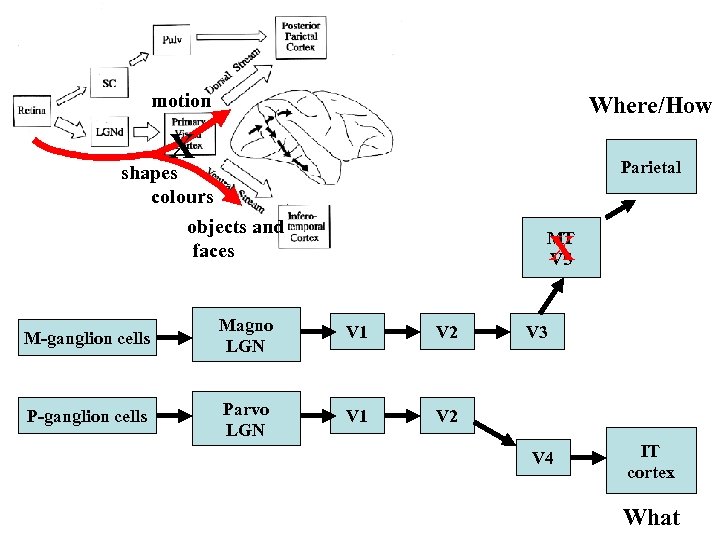
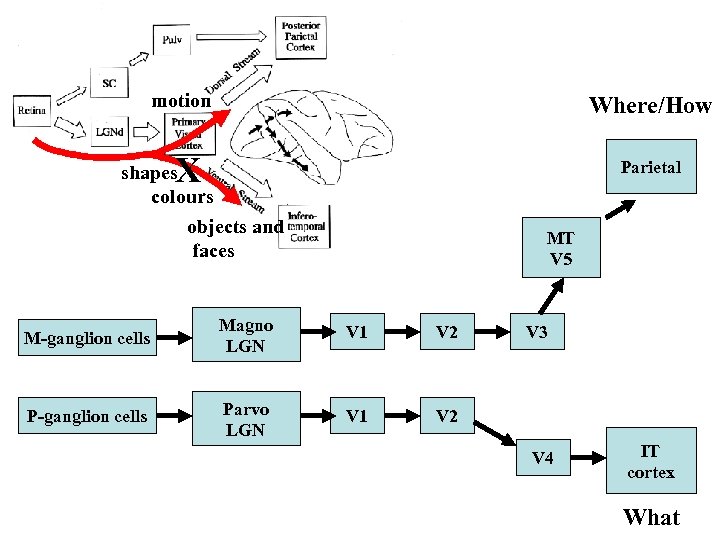
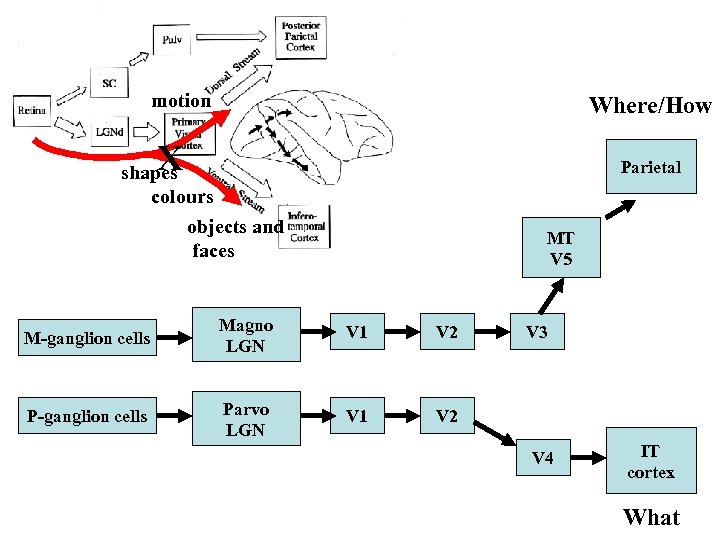 motion Where/How X Parietal shapes colours objects and faces MT V 5 M-ganglion cells Magno LGN V 1 V 2 P-ganglion cells Parvo LGN V 1 V 2 V 3 V 4 IT cortex What
motion Where/How X Parietal shapes colours objects and faces MT V 5 M-ganglion cells Magno LGN V 1 V 2 P-ganglion cells Parvo LGN V 1 V 2 V 3 V 4 IT cortex What
 Blindsight Clinical features • loss of half of the field of vision • can detect and discriminate visual stimuli in blind field without awareness (e. g. colour, luminance, motion, orientation) Neuropathology • striatal cortex (V 1) damage Diagnosis • forced choice reporting of ‘unseen’ stimuli
Blindsight Clinical features • loss of half of the field of vision • can detect and discriminate visual stimuli in blind field without awareness (e. g. colour, luminance, motion, orientation) Neuropathology • striatal cortex (V 1) damage Diagnosis • forced choice reporting of ‘unseen’ stimuli
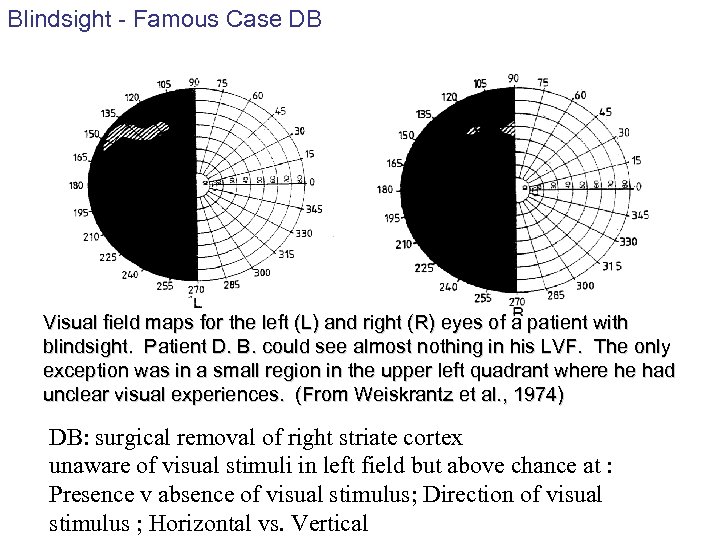 Blindsight - Famous Case DB Visual field maps for the left (L) and right (R) eyes of a patient with blindsight. Patient D. B. could see almost nothing in his LVF. The only exception was in a small region in the upper left quadrant where he had unclear visual experiences. (From Weiskrantz et al. , 1974) DB: surgical removal of right striate cortex unaware of visual stimuli in left field but above chance at : Presence v absence of visual stimulus; Direction of visual stimulus ; Horizontal vs. Vertical
Blindsight - Famous Case DB Visual field maps for the left (L) and right (R) eyes of a patient with blindsight. Patient D. B. could see almost nothing in his LVF. The only exception was in a small region in the upper left quadrant where he had unclear visual experiences. (From Weiskrantz et al. , 1974) DB: surgical removal of right striate cortex unaware of visual stimuli in left field but above chance at : Presence v absence of visual stimulus; Direction of visual stimulus ; Horizontal vs. Vertical
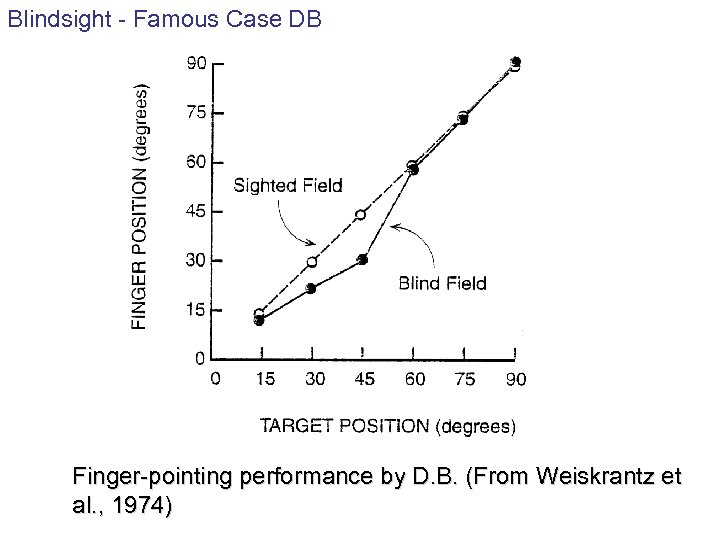 Blindsight - Famous Case DB Finger-pointing performance by D. B. (From Weiskrantz et al. , 1974)
Blindsight - Famous Case DB Finger-pointing performance by D. B. (From Weiskrantz et al. , 1974)
 Blindsight Clinical features • loss of half of the field of vision • can detect and discriminate visual stimuli in blind field without awareness (e. g. colour, luminance, motion, orientation) Neuropathology • striatal cortex (V 1) damage Diagnosis • forced choice reporting of ‘unseen’ stimuli Theories • stray light • islands of vision • primitive visual pathways stray light, but no blindsight at optic disc islands of vision: Friedrich patient, but GY primitive visual pathways - sparse, but widespread Retina - SC - Th - Cortex Retina - Pulvinar - Extrastriate cortex Retina - LGN - V 2/V 4/V 5/ TEO
Blindsight Clinical features • loss of half of the field of vision • can detect and discriminate visual stimuli in blind field without awareness (e. g. colour, luminance, motion, orientation) Neuropathology • striatal cortex (V 1) damage Diagnosis • forced choice reporting of ‘unseen’ stimuli Theories • stray light • islands of vision • primitive visual pathways stray light, but no blindsight at optic disc islands of vision: Friedrich patient, but GY primitive visual pathways - sparse, but widespread Retina - SC - Th - Cortex Retina - Pulvinar - Extrastriate cortex Retina - LGN - V 2/V 4/V 5/ TEO
 motion Where/How X Parietal shapes colours objects and faces MT V 5 X M-ganglion cells Magno LGN V 1 V 2 P-ganglion cells Parvo LGN V 1 V 2 V 3 V 4 IT cortex What
motion Where/How X Parietal shapes colours objects and faces MT V 5 X M-ganglion cells Magno LGN V 1 V 2 P-ganglion cells Parvo LGN V 1 V 2 V 3 V 4 IT cortex What
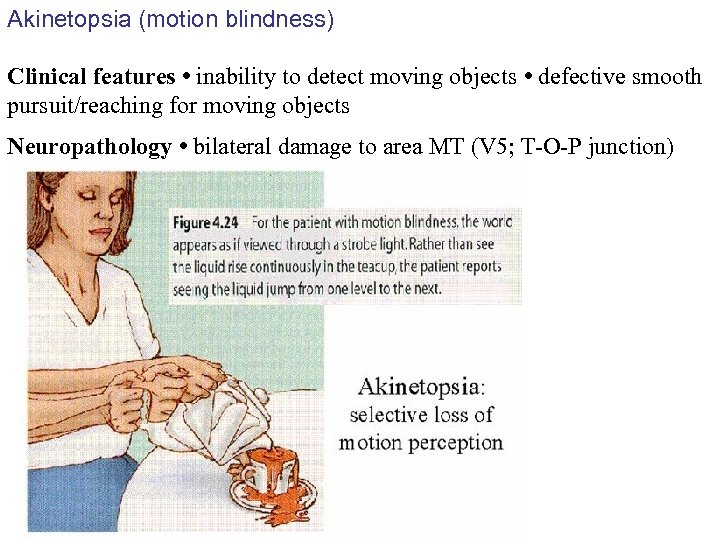 Akinetopsia (motion blindness) Clinical features • inability to detect moving objects • defective smooth pursuit/reaching for moving objects Neuropathology • bilateral damage to area MT (V 5; T-O-P junction)
Akinetopsia (motion blindness) Clinical features • inability to detect moving objects • defective smooth pursuit/reaching for moving objects Neuropathology • bilateral damage to area MT (V 5; T-O-P junction)
 Akinetopsia (motion blindness) - Famous case LM Case LM - akinetopsia 43 yr old. Sinus vein thrombosis V 5 damaged bilaterally - V 1 spared Could not see movement of objects but could see still objects. People would suddenly appear Diagnosed as agoraphobic o Can see movements/reach for/catch very slow moving objects (< 10 /s) LM could not speech read, but could tell forms of words from pictures Contrast HJA (ventral stream damage) who could speech read, but not tell forms of words from pictures
Akinetopsia (motion blindness) - Famous case LM Case LM - akinetopsia 43 yr old. Sinus vein thrombosis V 5 damaged bilaterally - V 1 spared Could not see movement of objects but could see still objects. People would suddenly appear Diagnosed as agoraphobic o Can see movements/reach for/catch very slow moving objects (< 10 /s) LM could not speech read, but could tell forms of words from pictures Contrast HJA (ventral stream damage) who could speech read, but not tell forms of words from pictures
 Akinetopsia (motion blindness) The consequences of inactivating areas V 1 and V 5 on visual motion perception G Beckers and S Zeki Brain 1995 118, 49 -60 TMS study - Stimulated V 1 and V 5 Motion perception disrupted most with V 5 stimulation up to 30 ms after visual stimulation onset V 1 stimulation also partially disrupts motion perception, but later (60 -70 ms after VS onset). Takes 30 -50 ms for signals to go from V 1 to V 5 Disruption of V 5 causes motion blindness more than V 1 Direct fast route from retina to V 5 via pulvinar bypassing V 1 Slower route to V 5 through V 1
Akinetopsia (motion blindness) The consequences of inactivating areas V 1 and V 5 on visual motion perception G Beckers and S Zeki Brain 1995 118, 49 -60 TMS study - Stimulated V 1 and V 5 Motion perception disrupted most with V 5 stimulation up to 30 ms after visual stimulation onset V 1 stimulation also partially disrupts motion perception, but later (60 -70 ms after VS onset). Takes 30 -50 ms for signals to go from V 1 to V 5 Disruption of V 5 causes motion blindness more than V 1 Direct fast route from retina to V 5 via pulvinar bypassing V 1 Slower route to V 5 through V 1
 motion Where/How X Parietal shapes colours objects and faces MT V 5 M-ganglion cells Magno LGN V 1 V 2 P-ganglion cells Parvo LGN V 1 V 2 V 3 V 4 IT cortex What
motion Where/How X Parietal shapes colours objects and faces MT V 5 M-ganglion cells Magno LGN V 1 V 2 P-ganglion cells Parvo LGN V 1 V 2 V 3 V 4 IT cortex What
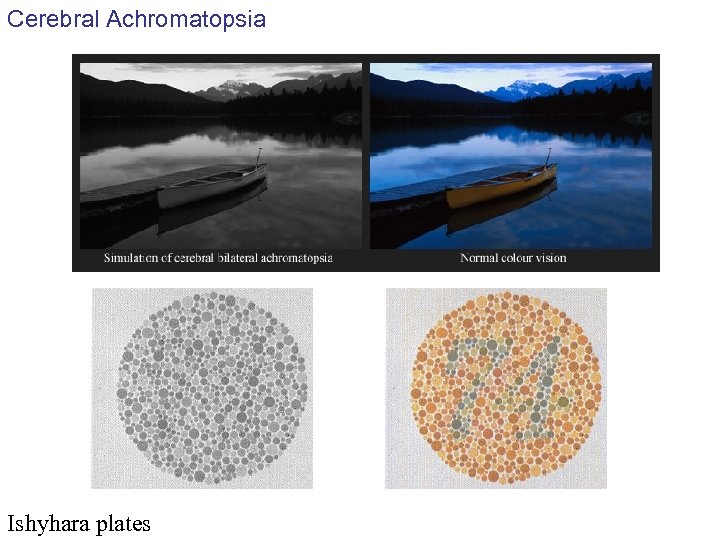 Cerebral Achromatopsia Ishyhara plates
Cerebral Achromatopsia Ishyhara plates
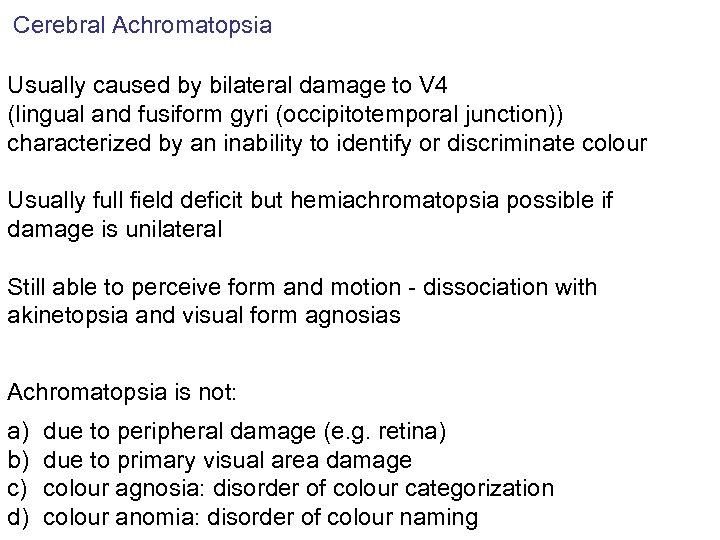 Cerebral Achromatopsia Usually caused by bilateral damage to V 4 (lingual and fusiform gyri (occipitotemporal junction)) characterized by an inability to identify or discriminate colour Usually full field deficit but hemiachromatopsia possible if damage is unilateral Still able to perceive form and motion - dissociation with akinetopsia and visual form agnosias Achromatopsia is not: a) b) c) d) due to peripheral damage (e. g. retina) due to primary visual area damage colour agnosia: disorder of colour categorization colour anomia: disorder of colour naming
Cerebral Achromatopsia Usually caused by bilateral damage to V 4 (lingual and fusiform gyri (occipitotemporal junction)) characterized by an inability to identify or discriminate colour Usually full field deficit but hemiachromatopsia possible if damage is unilateral Still able to perceive form and motion - dissociation with akinetopsia and visual form agnosias Achromatopsia is not: a) b) c) d) due to peripheral damage (e. g. retina) due to primary visual area damage colour agnosia: disorder of colour categorization colour anomia: disorder of colour naming
 Cerebral Achromatopsia - Famous Case The case of the colorblind painter by Oliver Sacks Facts: Auto accident No clear damage (no bleeding) No recollection of accident Alexia for five days. "Driving in a fog" His studio was ". . now utterly gray and void of colour. His canvases, the abstract colour paintings he was known for, were now grayish or black and white. At this point the magnitude of his loss overwhelmed him. " Over time he adapted. "I am completely divorced from colour. "
Cerebral Achromatopsia - Famous Case The case of the colorblind painter by Oliver Sacks Facts: Auto accident No clear damage (no bleeding) No recollection of accident Alexia for five days. "Driving in a fog" His studio was ". . now utterly gray and void of colour. His canvases, the abstract colour paintings he was known for, were now grayish or black and white. At this point the magnitude of his loss overwhelmed him. " Over time he adapted. "I am completely divorced from colour. "
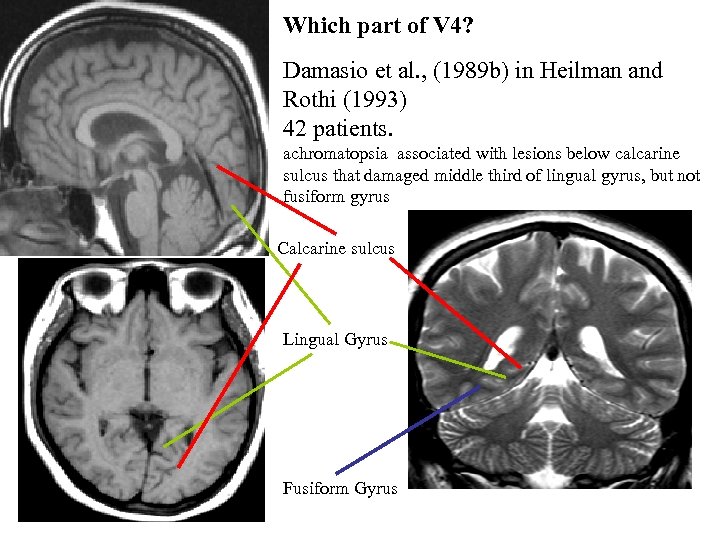 Which part of V 4? Damasio et al. , (1989 b) in Heilman and Rothi (1993) 42 patients. achromatopsia associated with lesions below calcarine sulcus that damaged middle third of lingual gyrus, but not fusiform gyrus Calcarine sulcus Lingual Gyrus Fusiform Gyrus
Which part of V 4? Damasio et al. , (1989 b) in Heilman and Rothi (1993) 42 patients. achromatopsia associated with lesions below calcarine sulcus that damaged middle third of lingual gyrus, but not fusiform gyrus Calcarine sulcus Lingual Gyrus Fusiform Gyrus
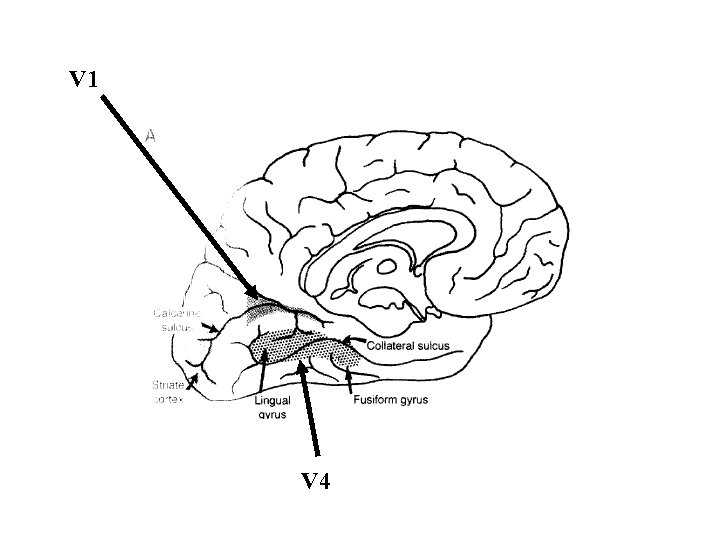 V 1 V 4
V 1 V 4
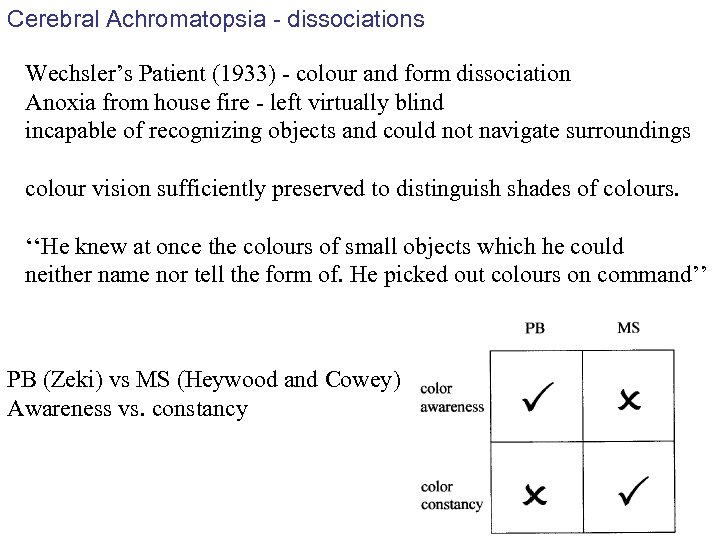 Cerebral Achromatopsia - dissociations Wechsler’s Patient (1933) - colour and form dissociation Anoxia from house fire - left virtually blind incapable of recognizing objects and could not navigate surroundings colour vision sufficiently preserved to distinguish shades of colours. ‘‘He knew at once the colours of small objects which he could neither name nor tell the form of. He picked out colours on command’’ PB (Zeki) vs MS (Heywood and Cowey) Awareness vs. constancy
Cerebral Achromatopsia - dissociations Wechsler’s Patient (1933) - colour and form dissociation Anoxia from house fire - left virtually blind incapable of recognizing objects and could not navigate surroundings colour vision sufficiently preserved to distinguish shades of colours. ‘‘He knew at once the colours of small objects which he could neither name nor tell the form of. He picked out colours on command’’ PB (Zeki) vs MS (Heywood and Cowey) Awareness vs. constancy
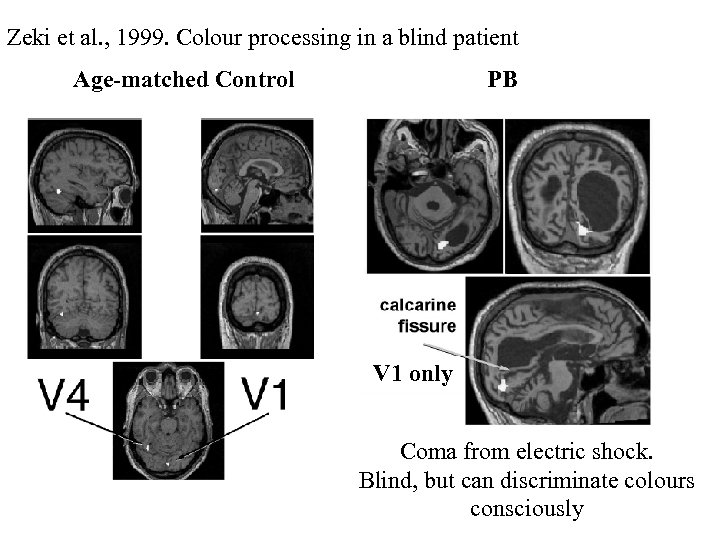 Zeki et al. , 1999. Colour processing in a blind patient Age-matched Control PB V 1 only Coma from electric shock. Blind, but can discriminate colours consciously
Zeki et al. , 1999. Colour processing in a blind patient Age-matched Control PB V 1 only Coma from electric shock. Blind, but can discriminate colours consciously
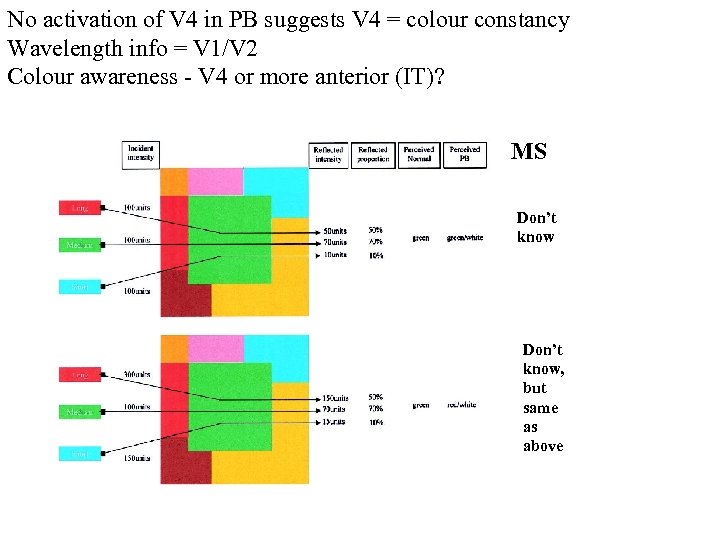 No activation of V 4 in PB suggests V 4 = colour constancy Wavelength info = V 1/V 2 Colour awareness - V 4 or more anterior (IT)? MS Don’t know, but same as above
No activation of V 4 in PB suggests V 4 = colour constancy Wavelength info = V 1/V 2 Colour awareness - V 4 or more anterior (IT)? MS Don’t know, but same as above
 The Agnosias Bauer (1993) In Hielman and Rothi 1993 A failure of recognition that cannot be attributed to: primary sensory defects mental deterioration attentional disturbances aphasic misnaming unfamiliarity with sensorially presented stimuli Originally classified as having two types Lissauer (1889) : Apperceptive and Associative
The Agnosias Bauer (1993) In Hielman and Rothi 1993 A failure of recognition that cannot be attributed to: primary sensory defects mental deterioration attentional disturbances aphasic misnaming unfamiliarity with sensorially presented stimuli Originally classified as having two types Lissauer (1889) : Apperceptive and Associative
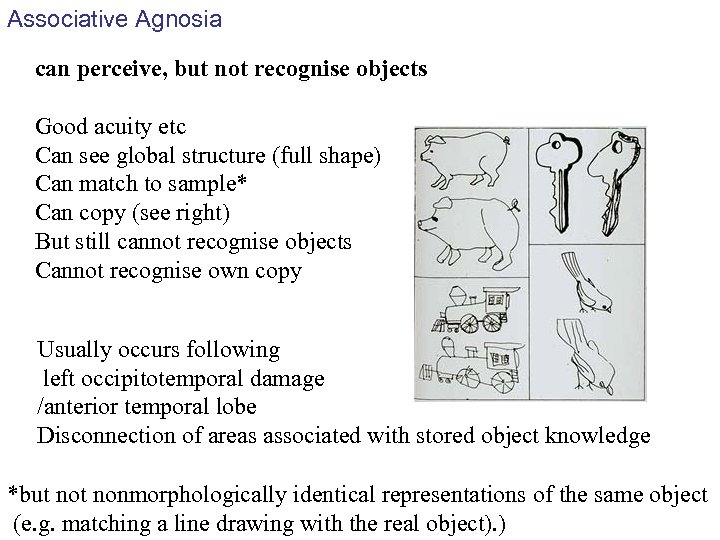 Associative Agnosia can perceive, but not recognise objects Good acuity etc Can see global structure (full shape) Can match to sample* Can copy (see right) But still cannot recognise objects Cannot recognise own copy Usually occurs following left occipitotemporal damage /anterior temporal lobe Disconnection of areas associated with stored object knowledge *but nonmorphologically identical representations of the same object (e. g. matching a line drawing with the real object). )
Associative Agnosia can perceive, but not recognise objects Good acuity etc Can see global structure (full shape) Can match to sample* Can copy (see right) But still cannot recognise objects Cannot recognise own copy Usually occurs following left occipitotemporal damage /anterior temporal lobe Disconnection of areas associated with stored object knowledge *but nonmorphologically identical representations of the same object (e. g. matching a line drawing with the real object). )
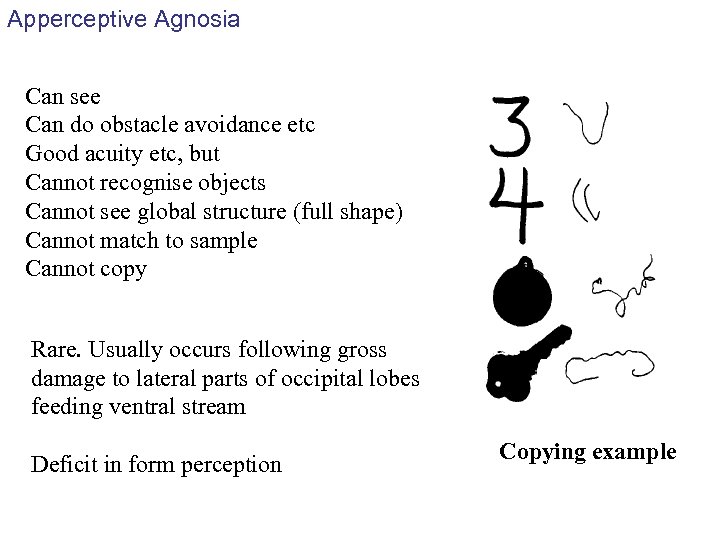 Apperceptive Agnosia Can see Can do obstacle avoidance etc Good acuity etc, but Cannot recognise objects Cannot see global structure (full shape) Cannot match to sample Cannot copy Rare. Usually occurs following gross damage to lateral parts of occipital lobes feeding ventral stream Deficit in form perception Copying example
Apperceptive Agnosia Can see Can do obstacle avoidance etc Good acuity etc, but Cannot recognise objects Cannot see global structure (full shape) Cannot match to sample Cannot copy Rare. Usually occurs following gross damage to lateral parts of occipital lobes feeding ventral stream Deficit in form perception Copying example
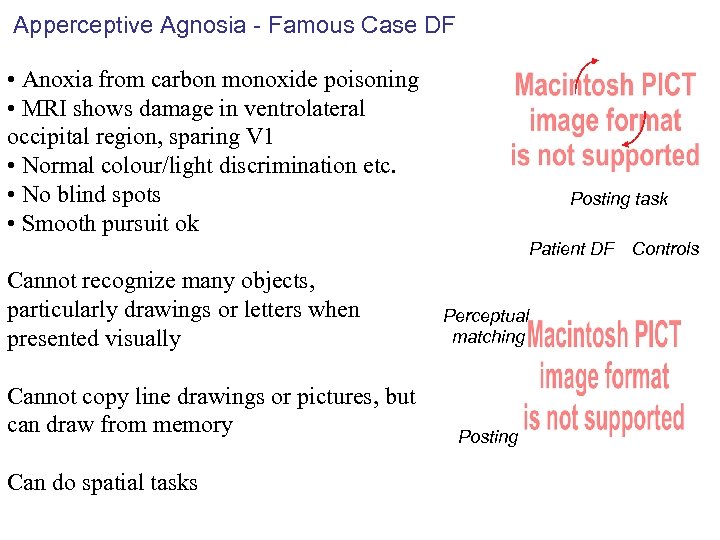 Apperceptive Agnosia - Famous Case DF • Anoxia from carbon monoxide poisoning • MRI shows damage in ventrolateral occipital region, sparing V 1 • Normal colour/light discrimination etc. • No blind spots • Smooth pursuit ok Posting task Patient DF Controls Cannot recognize many objects, particularly drawings or letters when presented visually Cannot copy line drawings or pictures, but can draw from memory Can do spatial tasks Perceptual matching Posting
Apperceptive Agnosia - Famous Case DF • Anoxia from carbon monoxide poisoning • MRI shows damage in ventrolateral occipital region, sparing V 1 • Normal colour/light discrimination etc. • No blind spots • Smooth pursuit ok Posting task Patient DF Controls Cannot recognize many objects, particularly drawings or letters when presented visually Cannot copy line drawings or pictures, but can draw from memory Can do spatial tasks Perceptual matching Posting
 Other Agnosia Alexia - left fusiform/lingual areas Inability to form coherent lexical representations from letters Topographagnosia or topographical agnosia - right lingual gyrus Inability to navigate routes using familiar landmarks - deficit in familiar scene perception Prosopagnosia - Can’t identify faces - even extremely familiar ones (even themselves!) But can identify people by other means And can recognise a face as being a face and Can discriminate between faces. Some P patients (e. g. LF - Bauer) show covert recognition GSR picks up when familiar vs. unfamiliar faces shown. Recognition not lost, awareness of recognition lost.
Other Agnosia Alexia - left fusiform/lingual areas Inability to form coherent lexical representations from letters Topographagnosia or topographical agnosia - right lingual gyrus Inability to navigate routes using familiar landmarks - deficit in familiar scene perception Prosopagnosia - Can’t identify faces - even extremely familiar ones (even themselves!) But can identify people by other means And can recognise a face as being a face and Can discriminate between faces. Some P patients (e. g. LF - Bauer) show covert recognition GSR picks up when familiar vs. unfamiliar faces shown. Recognition not lost, awareness of recognition lost.

 Prosopagnosia - Famous case Dr. P Sacks, 1985 The Man Who Mistook His Wife for a Hat Dr. P. well educated musician and teacher possible degenerative disease or large tumor couldn't recognize faces He recognised people on the basis of their "body music"- their voices and the manner in which they moved Would talk to people-shaped objects expecting a reply Also had agnosia for objects - at times unable to tell the difference between his feet and his slippers Could recognise geometric objects by touch
Prosopagnosia - Famous case Dr. P Sacks, 1985 The Man Who Mistook His Wife for a Hat Dr. P. well educated musician and teacher possible degenerative disease or large tumor couldn't recognize faces He recognised people on the basis of their "body music"- their voices and the manner in which they moved Would talk to people-shaped objects expecting a reply Also had agnosia for objects - at times unable to tell the difference between his feet and his slippers Could recognise geometric objects by touch
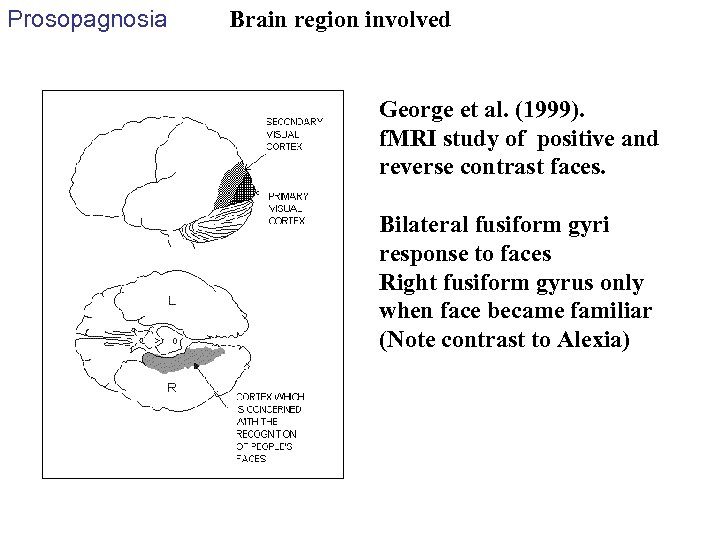 Prosopagnosia Brain region involved George et al. (1999). f. MRI study of positive and reverse contrast faces. Bilateral fusiform gyri response to faces Right fusiform gyrus only when face became familiar (Note contrast to Alexia)
Prosopagnosia Brain region involved George et al. (1999). f. MRI study of positive and reverse contrast faces. Bilateral fusiform gyri response to faces Right fusiform gyrus only when face became familiar (Note contrast to Alexia)
 Prosopagnosia Is prosopagnosia special (i. e. is there a special face processing area in the brain) or just another type of agnosia? Are faces a separate (special) class of objects or are faces just very difficult objects? Are faces just very difficult objects Or are they special because of our level of expertise?
Prosopagnosia Is prosopagnosia special (i. e. is there a special face processing area in the brain) or just another type of agnosia? Are faces a separate (special) class of objects or are faces just very difficult objects? Are faces just very difficult objects Or are they special because of our level of expertise?
 Prosopagnosia often co-occurs with other types of agnosia (anatomical coincidence of separate areas or are faces just objects? ) Are faces just very difficult objects? Assal et al. (1984) patient MX Farmer lost ability to recognise cows Could recognise faces Bruyer et al. , (1983) patient RB Can’t recognise faces Less impaired at cows. If faces just more difficult then shouldn’t have patients more impaired at other objects (i. e. cows).
Prosopagnosia often co-occurs with other types of agnosia (anatomical coincidence of separate areas or are faces just objects? ) Are faces just very difficult objects? Assal et al. (1984) patient MX Farmer lost ability to recognise cows Could recognise faces Bruyer et al. , (1983) patient RB Can’t recognise faces Less impaired at cows. If faces just more difficult then shouldn’t have patients more impaired at other objects (i. e. cows).
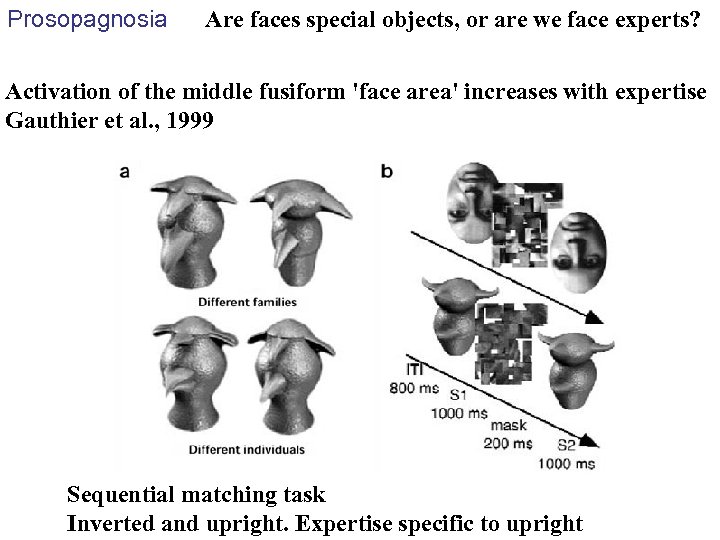 Prosopagnosia Are faces special objects, or are we face experts? Activation of the middle fusiform 'face area' increases with expertise Gauthier et al. , 1999 Sequential matching task Inverted and upright. Expertise specific to upright
Prosopagnosia Are faces special objects, or are we face experts? Activation of the middle fusiform 'face area' increases with expertise Gauthier et al. , 1999 Sequential matching task Inverted and upright. Expertise specific to upright
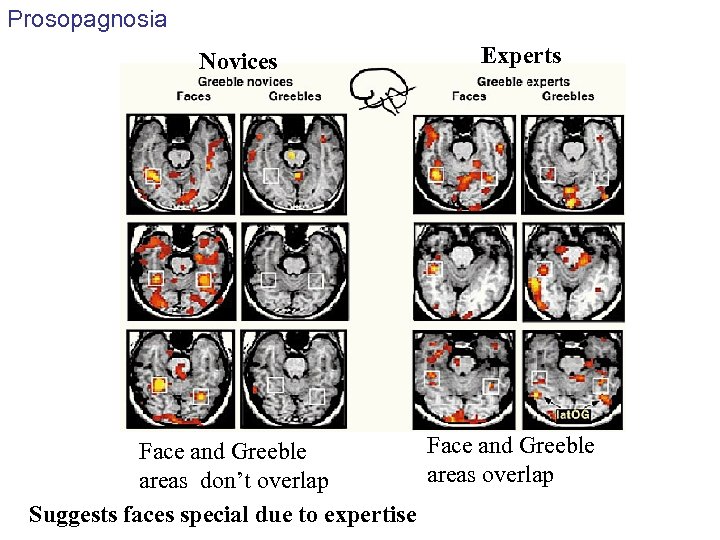 Prosopagnosia Novices Experts Face and Greeble areas overlap areas don’t overlap Suggests faces special due to expertise
Prosopagnosia Novices Experts Face and Greeble areas overlap areas don’t overlap Suggests faces special due to expertise
 Prosopagnosia Conclusions? IS FACE RECOGNITION NOT SO UNIQUE AFTER ALL? Gauthier & Logothetis (2000) COGNITIVE NEUROPSYCHOLOGY, 17 (1/2/3), 125– 142 Faces are not “special” They are the “default special” in the primate recognition system the face-selective area in the middle fusiform gyrus may be most appropriately described as a general substrate for subordinate-level discrimination that can be fine-tuned by experience with any object category. Gauthier et al. 1999.
Prosopagnosia Conclusions? IS FACE RECOGNITION NOT SO UNIQUE AFTER ALL? Gauthier & Logothetis (2000) COGNITIVE NEUROPSYCHOLOGY, 17 (1/2/3), 125– 142 Faces are not “special” They are the “default special” in the primate recognition system the face-selective area in the middle fusiform gyrus may be most appropriately described as a general substrate for subordinate-level discrimination that can be fine-tuned by experience with any object category. Gauthier et al. 1999.
 Prosopagnosia But Gauthier et al. 2004: Greebles not treated like faces CW profound object agnosia. OK on faces, poor on greebles Grill-Spector et al. 2004: FFA is involved in detection and identification of faces, but it has little involvement in within-category identification of non-face objects (including objects of expertise e. g. birds, flowers, houses, guitars, cars etc)
Prosopagnosia But Gauthier et al. 2004: Greebles not treated like faces CW profound object agnosia. OK on faces, poor on greebles Grill-Spector et al. 2004: FFA is involved in detection and identification of faces, but it has little involvement in within-category identification of non-face objects (including objects of expertise e. g. birds, flowers, houses, guitars, cars etc)
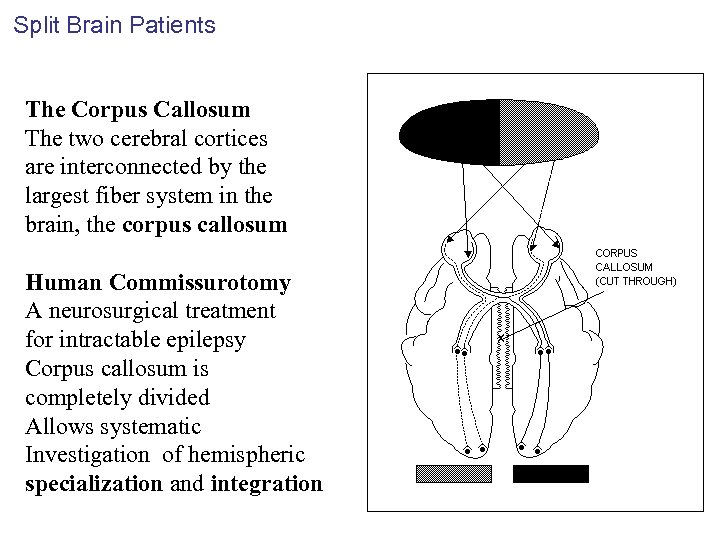 Split Brain Patients The Corpus Callosum The two cerebral cortices are interconnected by the largest fiber system in the brain, the corpus callosum Human Commissurotomy A neurosurgical treatment for intractable epilepsy Corpus callosum is completely divided Allows systematic Investigation of hemispheric specialization and integration
Split Brain Patients The Corpus Callosum The two cerebral cortices are interconnected by the largest fiber system in the brain, the corpus callosum Human Commissurotomy A neurosurgical treatment for intractable epilepsy Corpus callosum is completely divided Allows systematic Investigation of hemispheric specialization and integration
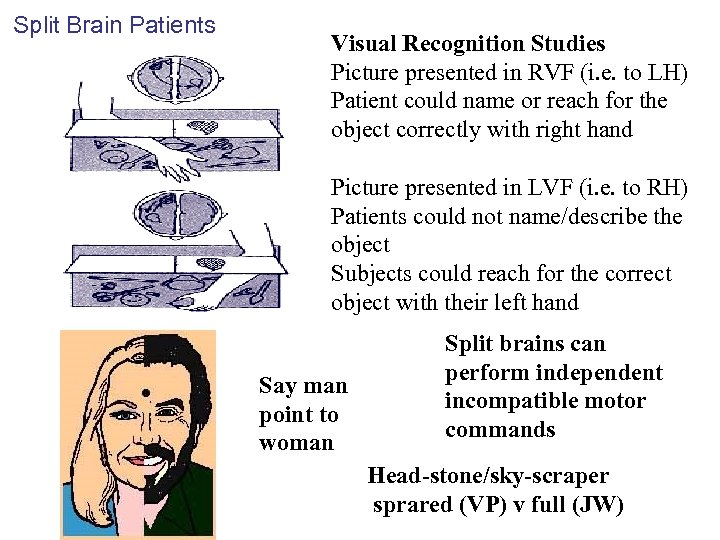 Split Brain Patients Visual Recognition Studies Picture presented in RVF (i. e. to LH) Patient could name or reach for the object correctly with right hand Picture presented in LVF (i. e. to RH) Patients could not name/describe the object Subjects could reach for the correct object with their left hand Say man point to woman Split brains can perform independent incompatible motor commands Head-stone/sky-scraper sprared (VP) v full (JW)
Split Brain Patients Visual Recognition Studies Picture presented in RVF (i. e. to LH) Patient could name or reach for the object correctly with right hand Picture presented in LVF (i. e. to RH) Patients could not name/describe the object Subjects could reach for the correct object with their left hand Say man point to woman Split brains can perform independent incompatible motor commands Head-stone/sky-scraper sprared (VP) v full (JW)
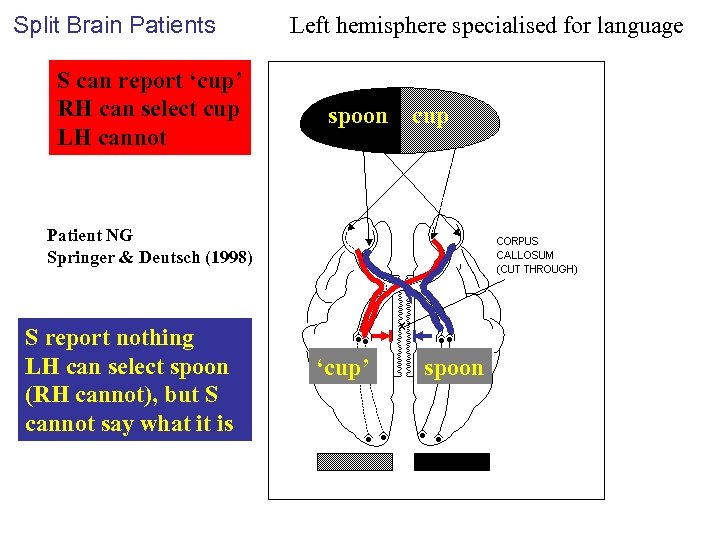 Split Brain Patients S can report ‘cup’ RH can select cup LH cannot Left hemisphere specialised for language spoon cup Patient NG Springer & Deutsch (1998) S report nothing LH can select spoon (RH cannot), but S cannot say what it is ‘cup’ spoon
Split Brain Patients S can report ‘cup’ RH can select cup LH cannot Left hemisphere specialised for language spoon cup Patient NG Springer & Deutsch (1998) S report nothing LH can select spoon (RH cannot), but S cannot say what it is ‘cup’ spoon
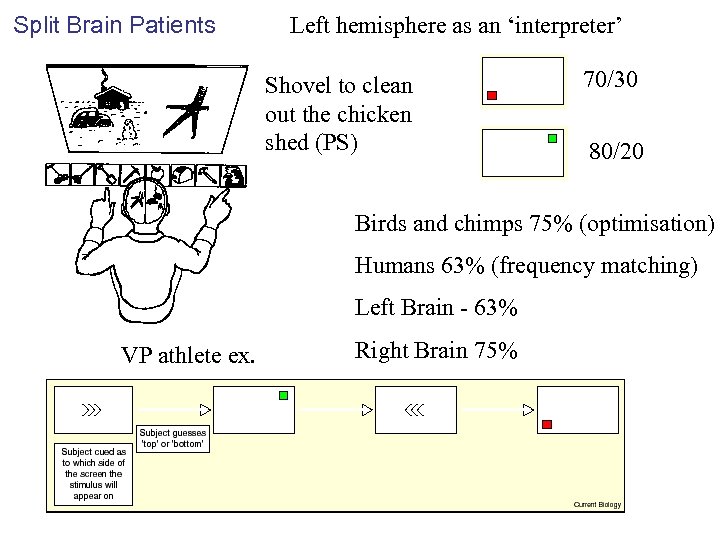 Split Brain Patients Left hemisphere as an ‘interpreter’ Shovel to clean out the chicken shed (PS) 70/30 80/20 Birds and chimps 75% (optimisation) Humans 63% (frequency matching) Left Brain - 63% VP athlete ex. Right Brain 75%
Split Brain Patients Left hemisphere as an ‘interpreter’ Shovel to clean out the chicken shed (PS) 70/30 80/20 Birds and chimps 75% (optimisation) Humans 63% (frequency matching) Left Brain - 63% VP athlete ex. Right Brain 75%
 Next Week Attention
Next Week Attention


