Lecture #5 III course lungs.ppt
- Количество слайдов: 35
 Lecture #5 Theme: Histology of lungs. Features in children.
Lecture #5 Theme: Histology of lungs. Features in children.
 The plan: • • • 1. Lungs. Bronchial arbor. 2. General plan of structure of wall of bronchi. 3. Dependence of structure of wall of bronchi and bronchioles from their caliber. 4. Respiratory section of lung. Acinus. Structure of alveoles, types of alveolocytes. 5. Air-hematic barrier and its significance in gas exchange. 6. Features of lungs in children.
The plan: • • • 1. Lungs. Bronchial arbor. 2. General plan of structure of wall of bronchi. 3. Dependence of structure of wall of bronchi and bronchioles from their caliber. 4. Respiratory section of lung. Acinus. Structure of alveoles, types of alveolocytes. 5. Air-hematic barrier and its significance in gas exchange. 6. Features of lungs in children.
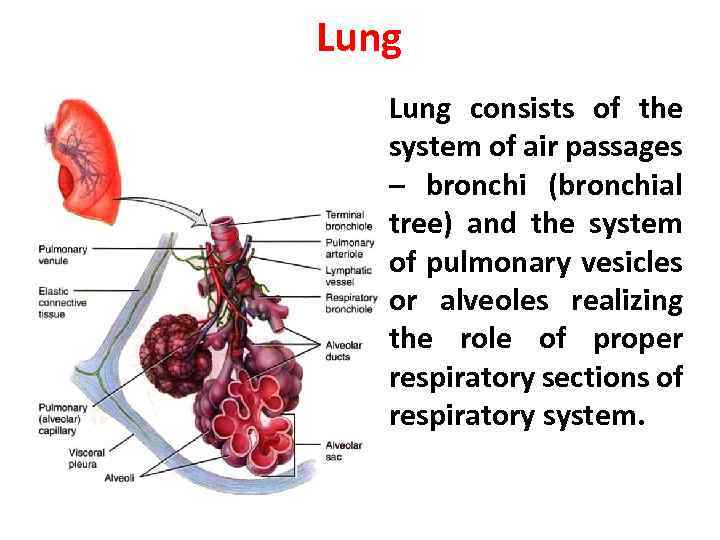 Lung • Lung consists of the system of air passages – bronchi (bronchial tree) and the system of pulmonary vesicles or alveoles realizing the role of proper respiratory sections of respiratory system.
Lung • Lung consists of the system of air passages – bronchi (bronchial tree) and the system of pulmonary vesicles or alveoles realizing the role of proper respiratory sections of respiratory system.
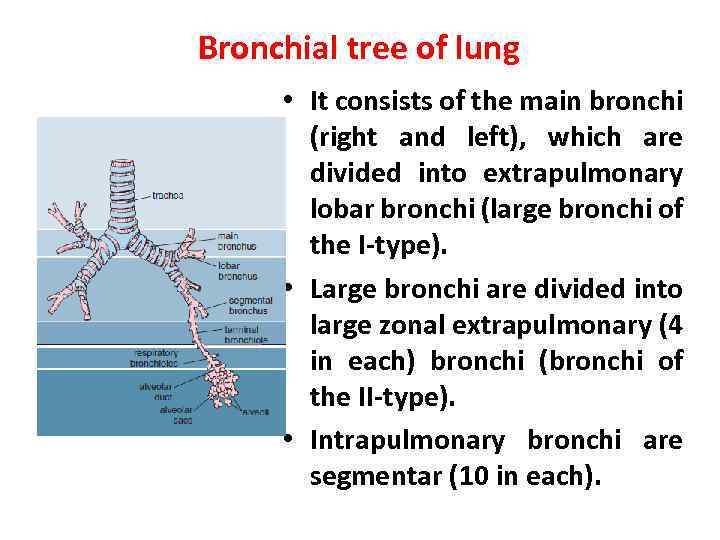 Bronchial tree of lung • It consists of the main bronchi (right and left), which are divided into extrapulmonary lobar bronchi (large bronchi of the I-type). • Large bronchi are divided into large zonal extrapulmonary (4 in each) bronchi (bronchi of the II-type). • Intrapulmonary bronchi are segmentar (10 in each).
Bronchial tree of lung • It consists of the main bronchi (right and left), which are divided into extrapulmonary lobar bronchi (large bronchi of the I-type). • Large bronchi are divided into large zonal extrapulmonary (4 in each) bronchi (bronchi of the II-type). • Intrapulmonary bronchi are segmentar (10 in each).
 Bronchial tree of lung • Intrapulmonary bronchi are divided into bronchi of the III-V-type subsegmentar middle bronchi (2 -5 millimeters). • The middle bronchi are branched into small (1 -2 millimeters in diameter) bronchi and into terminal bronchioles. • Than respiratory sections of lung start, they realize gas-exchange function.
Bronchial tree of lung • Intrapulmonary bronchi are divided into bronchi of the III-V-type subsegmentar middle bronchi (2 -5 millimeters). • The middle bronchi are branched into small (1 -2 millimeters in diameter) bronchi and into terminal bronchioles. • Than respiratory sections of lung start, they realize gas-exchange function.
 Structure of bronchi • • • Bronchus contains the following layers: 1. mucosa, 2. submucosa, 3. fibrous-cartilaginous layer, 4. adventitial layer.
Structure of bronchi • • • Bronchus contains the following layers: 1. mucosa, 2. submucosa, 3. fibrous-cartilaginous layer, 4. adventitial layer.
 Structure of mucosa of bronchi • The internal layer of bronchi – mucosa is lined by pseudostratified ciliated epithelium. • Proper lamina is rich in elastic fibers. • Muscle lamina is well developed in bronchi of small caliber.
Structure of mucosa of bronchi • The internal layer of bronchi – mucosa is lined by pseudostratified ciliated epithelium. • Proper lamina is rich in elastic fibers. • Muscle lamina is well developed in bronchi of small caliber.
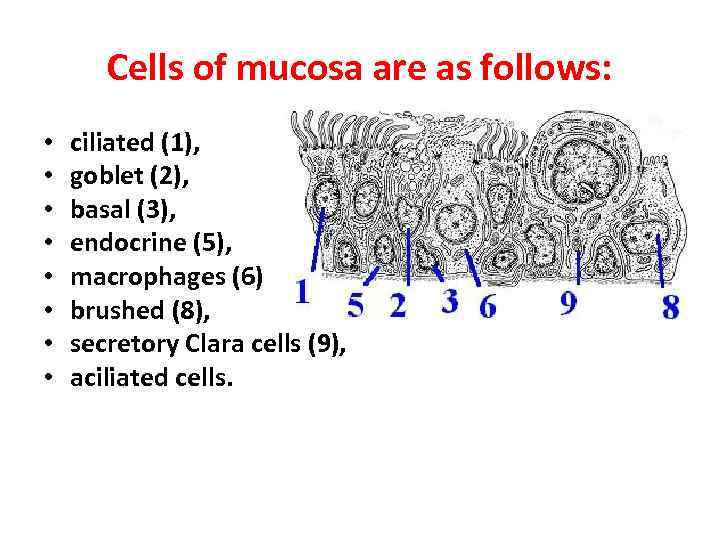 Cells of mucosa are as follows: • • ciliated (1), goblet (2), basal (3), endocrine (5), macrophages (6) brushed (8), secretory Clara cells (9), aciliated cells.
Cells of mucosa are as follows: • • ciliated (1), goblet (2), basal (3), endocrine (5), macrophages (6) brushed (8), secretory Clara cells (9), aciliated cells.
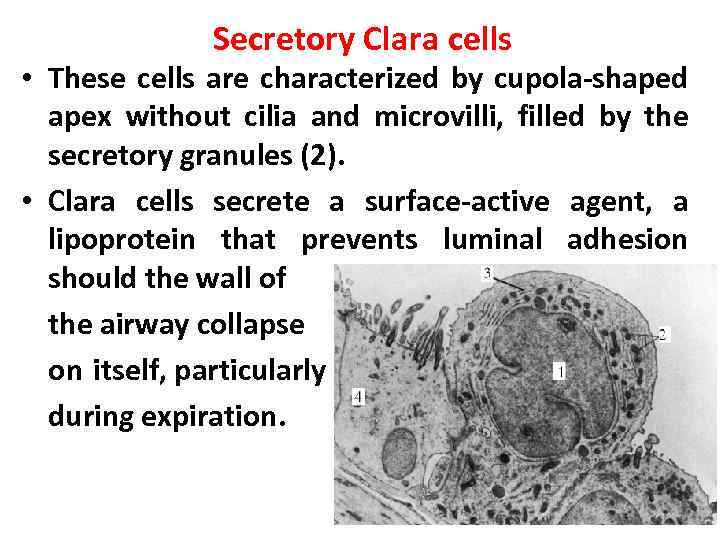 Secretory Clara cells • These cells are characterized by cupola-shaped apex without cilia and microvilli, filled by the secretory granules (2). • Clara cells secrete a surface-active agent, a lipoprotein that prevents luminal adhesion should the wall of the airway collapse on itself, particularly during expiration.
Secretory Clara cells • These cells are characterized by cupola-shaped apex without cilia and microvilli, filled by the secretory granules (2). • Clara cells secrete a surface-active agent, a lipoprotein that prevents luminal adhesion should the wall of the airway collapse on itself, particularly during expiration.
 • In addition, Clara cells produce a 16 -kilodalton protein known as Clara cell secretory protein (CC 16), which is an abundant component of the airway secretion. • Chronic lung diseases such as chronic obstructive pulmonary disease (COPD) and asthma are associated with changes in the abundance of CC 16 in airway fluid and serum. • CC 16 is used as a measurable pulmonary marker in bronchoalveolar lavage fluid and serum. • Secretion of CC 16 into the bronchial tree decreases during lung injury (because of damage to the Clara cells), whereas serum levels of CC 16 may increase because of leakage across the air–blood barrier.
• In addition, Clara cells produce a 16 -kilodalton protein known as Clara cell secretory protein (CC 16), which is an abundant component of the airway secretion. • Chronic lung diseases such as chronic obstructive pulmonary disease (COPD) and asthma are associated with changes in the abundance of CC 16 in airway fluid and serum. • CC 16 is used as a measurable pulmonary marker in bronchoalveolar lavage fluid and serum. • Secretion of CC 16 into the bronchial tree decreases during lung injury (because of damage to the Clara cells), whereas serum levels of CC 16 may increase because of leakage across the air–blood barrier.
 Brushed and aciliated cells of bronchi • Brushed cells contain microvilli. They realize the function of chemoreceptors. • Aciliated cells are prismatic-shaped. Function of these cells is not clear.
Brushed and aciliated cells of bronchi • Brushed cells contain microvilli. They realize the function of chemoreceptors. • Aciliated cells are prismatic-shaped. Function of these cells is not clear.
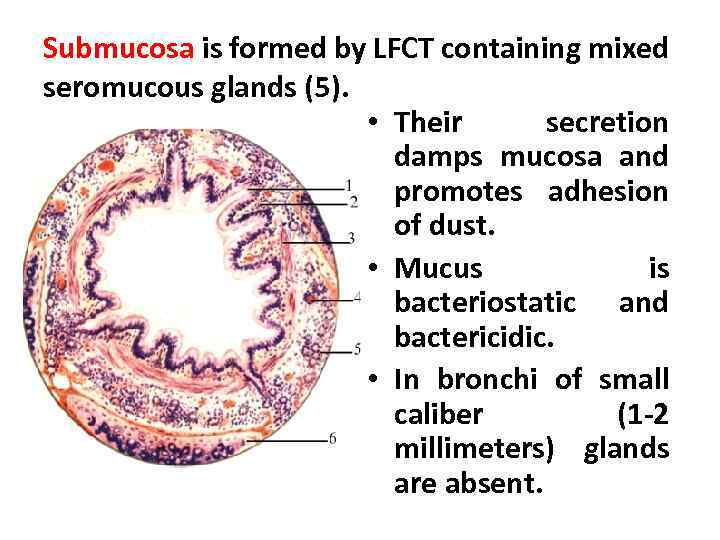 Submucosa is formed by LFCT containing mixed seromucous glands (5). • Their secretion damps mucosa and promotes adhesion of dust. • Mucus is bacteriostatic and bactericidic. • In bronchi of small caliber (1 -2 millimeters) glands are absent.
Submucosa is formed by LFCT containing mixed seromucous glands (5). • Their secretion damps mucosa and promotes adhesion of dust. • Mucus is bacteriostatic and bactericidic. • In bronchi of small caliber (1 -2 millimeters) glands are absent.
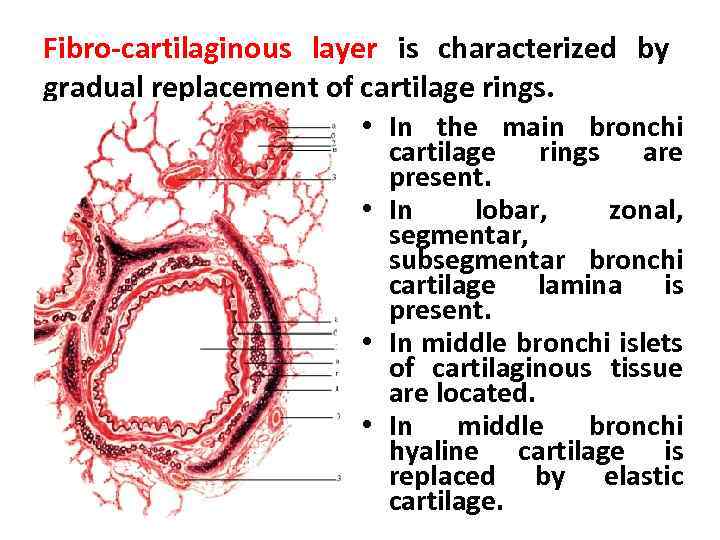 Fibro-cartilaginous layer is characterized by gradual replacement of cartilage rings. • In the main bronchi cartilage rings are present. • In lobar, zonal, segmentar, subsegmentar bronchi cartilage lamina is present. • In middle bronchi islets of cartilaginous tissue are located. • In middle bronchi hyaline cartilage is replaced by elastic cartilage.
Fibro-cartilaginous layer is characterized by gradual replacement of cartilage rings. • In the main bronchi cartilage rings are present. • In lobar, zonal, segmentar, subsegmentar bronchi cartilage lamina is present. • In middle bronchi islets of cartilaginous tissue are located. • In middle bronchi hyaline cartilage is replaced by elastic cartilage.
 Adventitia • External adventitial layer is made up of fibrous connective tissue. • Among connective tissue cells tissue basophils are present. • They take part in regulation of local homeostasis and blood coagulation.
Adventitia • External adventitial layer is made up of fibrous connective tissue. • Among connective tissue cells tissue basophils are present. • They take part in regulation of local homeostasis and blood coagulation.
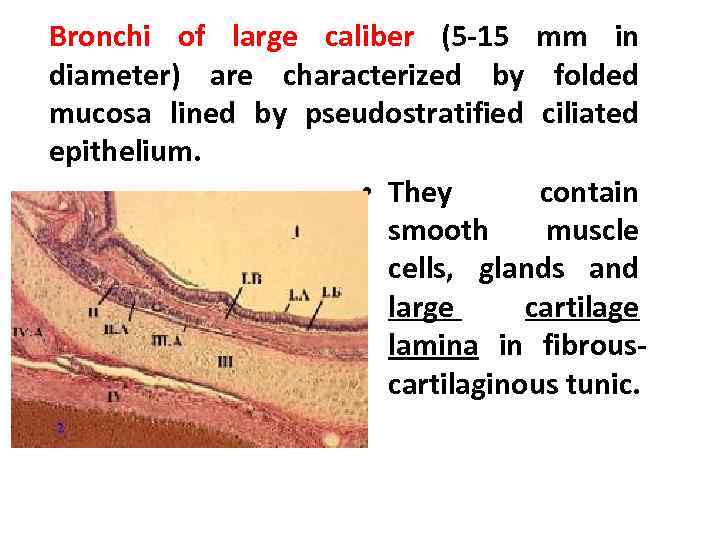 Bronchi of large caliber (5 -15 mm in diameter) are characterized by folded mucosa lined by pseudostratified ciliated epithelium. • They contain smooth muscle cells, glands and large cartilage lamina in fibrouscartilaginous tunic.
Bronchi of large caliber (5 -15 mm in diameter) are characterized by folded mucosa lined by pseudostratified ciliated epithelium. • They contain smooth muscle cells, glands and large cartilage lamina in fibrouscartilaginous tunic.
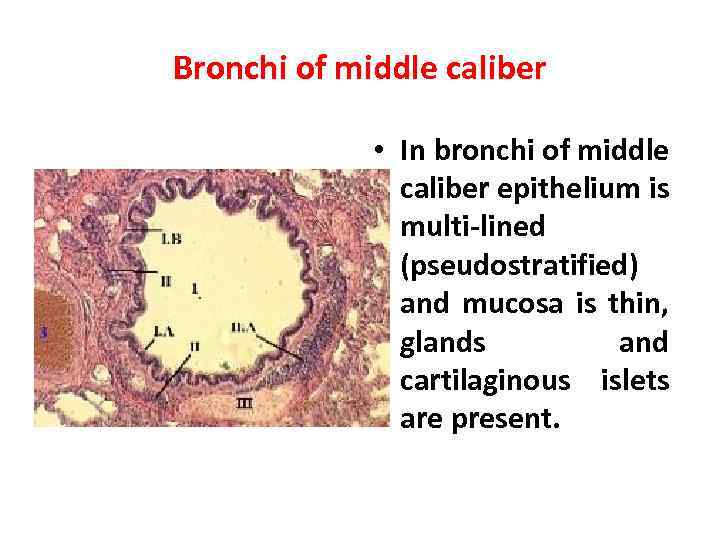 Bronchi of middle caliber • In bronchi of middle caliber epithelium is multi-lined (pseudostratified) and mucosa is thin, glands and cartilaginous islets are present.
Bronchi of middle caliber • In bronchi of middle caliber epithelium is multi-lined (pseudostratified) and mucosa is thin, glands and cartilaginous islets are present.
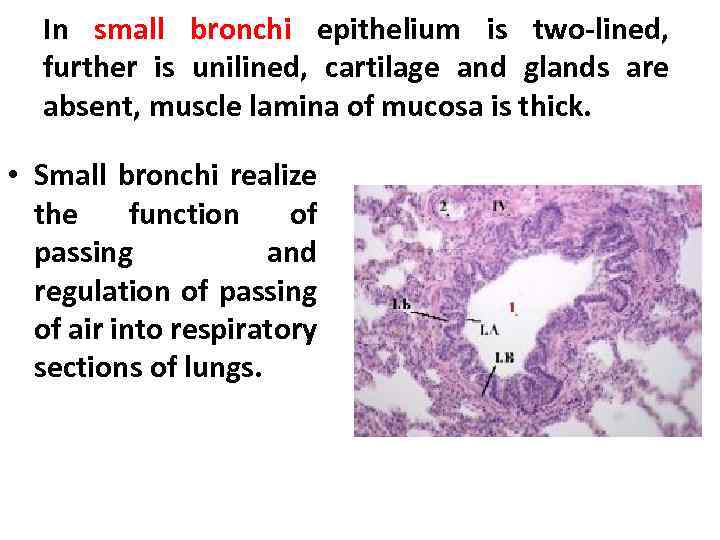 In small bronchi epithelium is two-lined, further is unilined, cartilage and glands are absent, muscle lamina of mucosa is thick. • Small bronchi realize the function of passing and regulation of passing of air into respiratory sections of lungs.
In small bronchi epithelium is two-lined, further is unilined, cartilage and glands are absent, muscle lamina of mucosa is thick. • Small bronchi realize the function of passing and regulation of passing of air into respiratory sections of lungs.
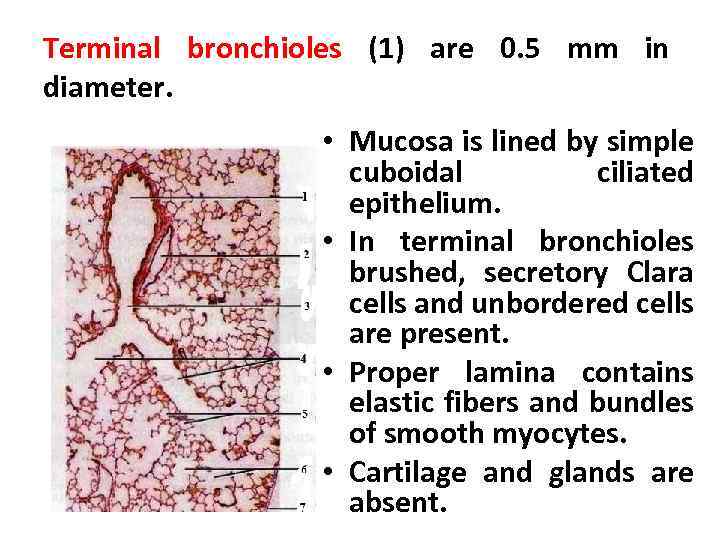 Terminal bronchioles (1) are 0. 5 mm in diameter. • Mucosa is lined by simple cuboidal ciliated epithelium. • In terminal bronchioles brushed, secretory Clara cells and unbordered cells are present. • Proper lamina contains elastic fibers and bundles of smooth myocytes. • Cartilage and glands are absent.
Terminal bronchioles (1) are 0. 5 mm in diameter. • Mucosa is lined by simple cuboidal ciliated epithelium. • In terminal bronchioles brushed, secretory Clara cells and unbordered cells are present. • Proper lamina contains elastic fibers and bundles of smooth myocytes. • Cartilage and glands are absent.
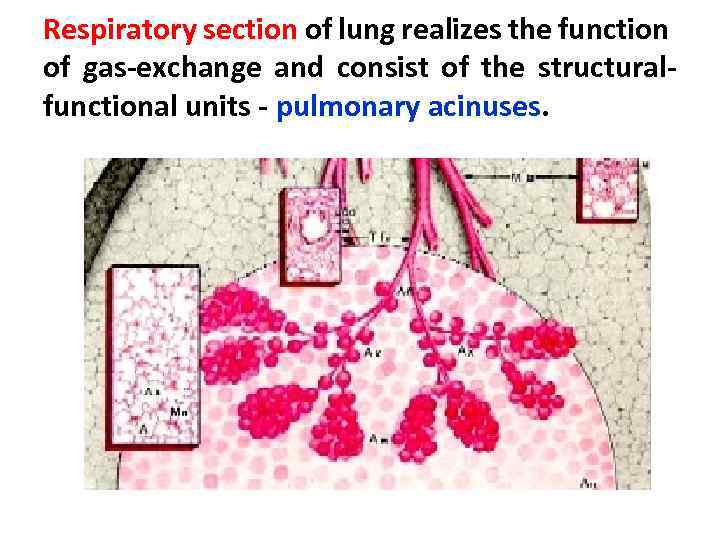 Respiratory section of lung realizes the function of gas-exchange and consist of the structuralfunctional units - pulmonary acinuses.
Respiratory section of lung realizes the function of gas-exchange and consist of the structuralfunctional units - pulmonary acinuses.
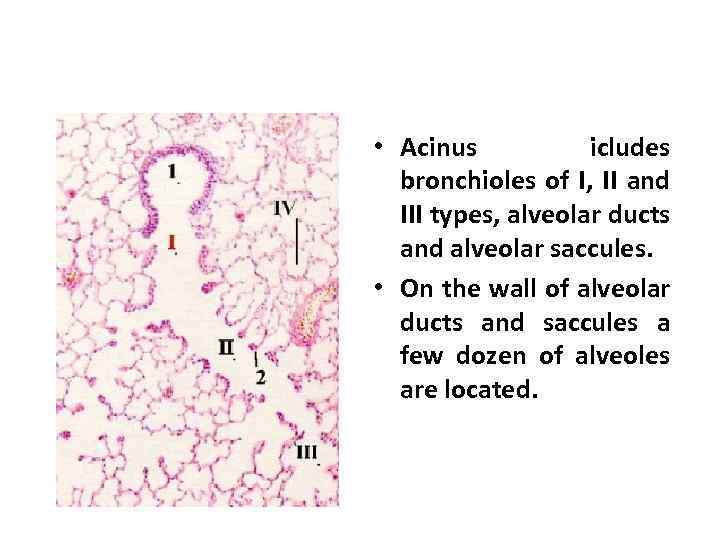 • Acinus icludes bronchioles of I, II and III types, alveolar ducts and alveolar saccules. • On the wall of alveolar ducts and saccules a few dozen of alveoles are located.
• Acinus icludes bronchioles of I, II and III types, alveolar ducts and alveolar saccules. • On the wall of alveolar ducts and saccules a few dozen of alveoles are located.
 Respiratory section • Each respiratory bronchiole of II-type is divided into alveolar ducts. • Each alveolar duct ends by two alveolar saccules. • In the mouth of alveolar ducts bundles of smooth myocytes are present. • Fine connective tissue layers separate acinuses from each other. • 12 -18 acinuses form pulmonary lobule.
Respiratory section • Each respiratory bronchiole of II-type is divided into alveolar ducts. • Each alveolar duct ends by two alveolar saccules. • In the mouth of alveolar ducts bundles of smooth myocytes are present. • Fine connective tissue layers separate acinuses from each other. • 12 -18 acinuses form pulmonary lobule.
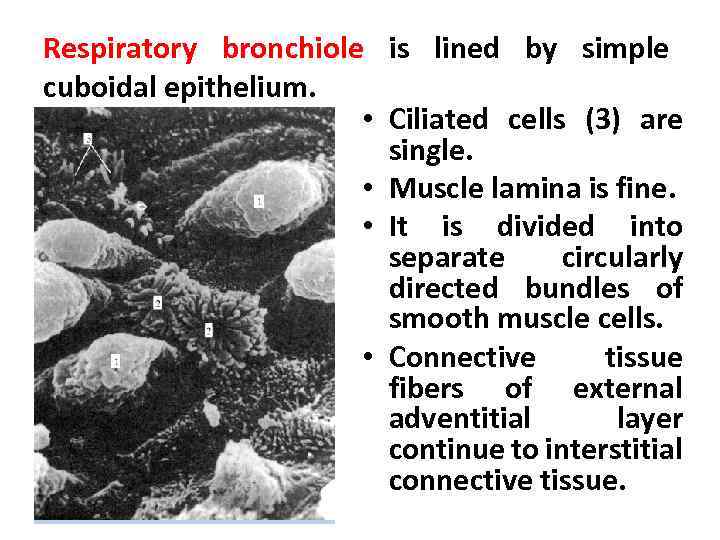 Respiratory bronchiole is lined by simple cuboidal epithelium. • Ciliated cells (3) are single. • Muscle lamina is fine. • It is divided into separate circularly directed bundles of smooth muscle cells. • Connective tissue fibers of external adventitial layer continue to interstitial connective tissue.
Respiratory bronchiole is lined by simple cuboidal epithelium. • Ciliated cells (3) are single. • Muscle lamina is fine. • It is divided into separate circularly directed bundles of smooth muscle cells. • Connective tissue fibers of external adventitial layer continue to interstitial connective tissue.
 Alveoli • Alveoli are the terminal air spaces of the respiratory system and are the actual sites of gas exchange between the air and the blood. • Each alveolus is surrounded by a network of capillaries that brings blood into close proximity to inhaled air inside the alveolus. • About 300 to 400 million alveoli are found in each adult lung; their combined internal surface area is approximately 100 m 2. • Each alveolus is a thin-walled polyhedral chamber approximately 0. 2 mm in diameter that is confluent with an alveolar sac.
Alveoli • Alveoli are the terminal air spaces of the respiratory system and are the actual sites of gas exchange between the air and the blood. • Each alveolus is surrounded by a network of capillaries that brings blood into close proximity to inhaled air inside the alveolus. • About 300 to 400 million alveoli are found in each adult lung; their combined internal surface area is approximately 100 m 2. • Each alveolus is a thin-walled polyhedral chamber approximately 0. 2 mm in diameter that is confluent with an alveolar sac.
 • Alveolar ducts are elongated airways that have almost no walls, only alveoli, as their peripheral boundary. • Rings of smooth muscle are present in the knoblike interalveolar. • Alveolar sacs are spaces surrounded by clusters of alveoli. • The surrounding alveoli open into these spaces. • Alveolar sacs usually occur at the termination of an alveolar duct but may occur anywhere along its length.
• Alveolar ducts are elongated airways that have almost no walls, only alveoli, as their peripheral boundary. • Rings of smooth muscle are present in the knoblike interalveolar. • Alveolar sacs are spaces surrounded by clusters of alveoli. • The surrounding alveoli open into these spaces. • Alveolar sacs usually occur at the termination of an alveolar duct but may occur anywhere along its length.
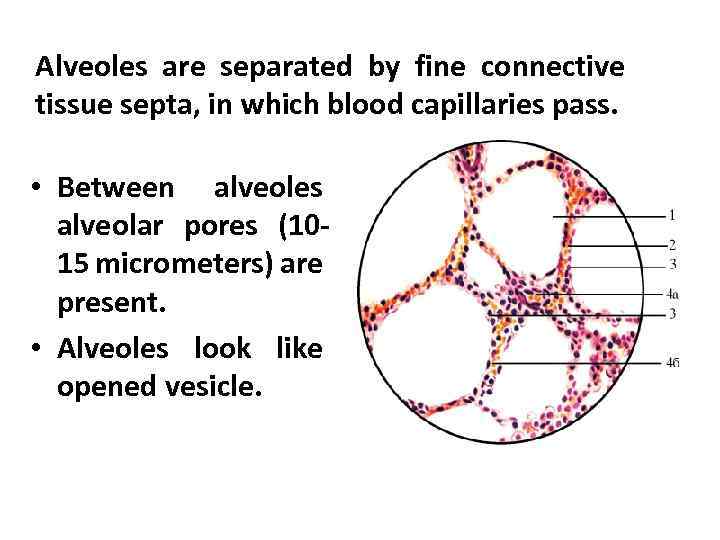 Alveoles are separated by fine connective tissue septa, in which blood capillaries pass. • Between alveoles alveolar pores (1015 micrometers) are present. • Alveoles look like opened vesicle.
Alveoles are separated by fine connective tissue septa, in which blood capillaries pass. • Between alveoles alveolar pores (1015 micrometers) are present. • Alveoles look like opened vesicle.
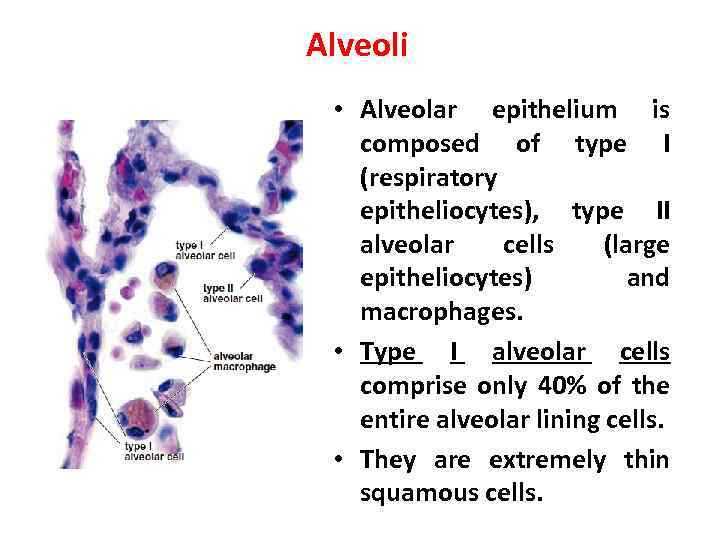 Alveoli • Alveolar epithelium is composed of type I (respiratory epitheliocytes), type II alveolar cells (large epitheliocytes) and macrophages. • Type I alveolar cells comprise only 40% of the entire alveolar lining cells. • They are extremely thin squamous cells.
Alveoli • Alveolar epithelium is composed of type I (respiratory epitheliocytes), type II alveolar cells (large epitheliocytes) and macrophages. • Type I alveolar cells comprise only 40% of the entire alveolar lining cells. • They are extremely thin squamous cells.
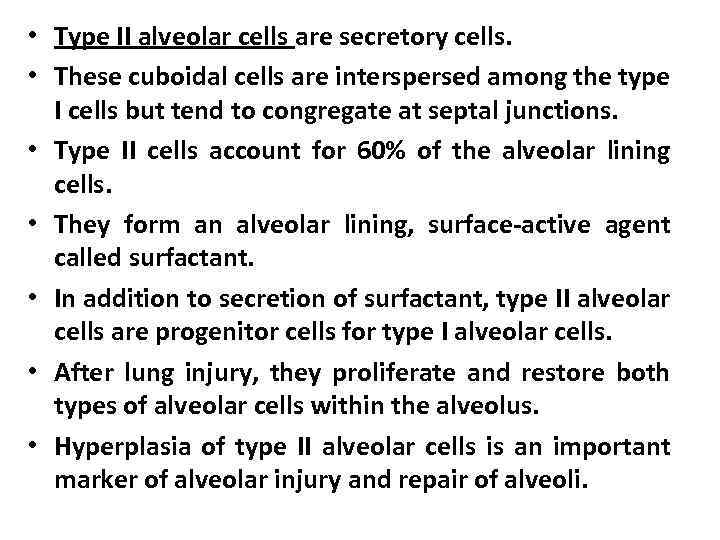 • Type II alveolar cells are secretory cells. • These cuboidal cells are interspersed among the type I cells but tend to congregate at septal junctions. • Type II cells account for 60% of the alveolar lining cells. • They form an alveolar lining, surface-active agent called surfactant. • In addition to secretion of surfactant, type II alveolar cells are progenitor cells for type I alveolar cells. • After lung injury, they proliferate and restore both types of alveolar cells within the alveolus. • Hyperplasia of type II alveolar cells is an important marker of alveolar injury and repair of alveoli.
• Type II alveolar cells are secretory cells. • These cuboidal cells are interspersed among the type I cells but tend to congregate at septal junctions. • Type II cells account for 60% of the alveolar lining cells. • They form an alveolar lining, surface-active agent called surfactant. • In addition to secretion of surfactant, type II alveolar cells are progenitor cells for type I alveolar cells. • After lung injury, they proliferate and restore both types of alveolar cells within the alveolus. • Hyperplasia of type II alveolar cells is an important marker of alveolar injury and repair of alveoli.
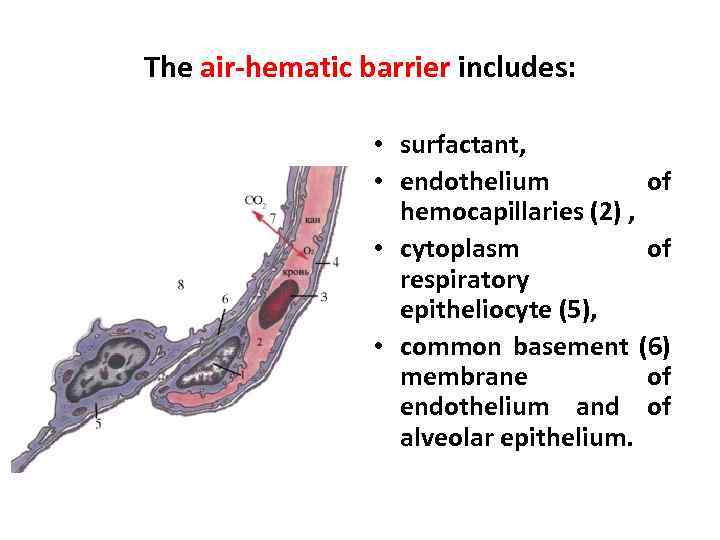 The air-hematic barrier includes: • surfactant, • endothelium of hemocapillaries (2) , • cytoplasm of respiratory epitheliocyte (5), • common basement (6) membrane of endothelium and of alveolar epithelium.
The air-hematic barrier includes: • surfactant, • endothelium of hemocapillaries (2) , • cytoplasm of respiratory epitheliocyte (5), • common basement (6) membrane of endothelium and of alveolar epithelium.
 Air-hematic barrier • The air-hematic barrier plays significant function in prevent of collapse of alveoli during inspiration. • It also prevents them from penetration of microorganisms from inspiration air through. the wall of alveoli, from transudation of fluid from capillaries of interalveolar septa into alveoli.
Air-hematic barrier • The air-hematic barrier plays significant function in prevent of collapse of alveoli during inspiration. • It also prevents them from penetration of microorganisms from inspiration air through. the wall of alveoli, from transudation of fluid from capillaries of interalveolar septa into alveoli.
 Surfactant • Surfactant is substance of glycolipidprotein origin. • It consists of two phases – membranous and fluid (hypophase). .
Surfactant • Surfactant is substance of glycolipidprotein origin. • It consists of two phases – membranous and fluid (hypophase). .
 Surfactant • Phospholipids and proteins form membranous component. • Lipoproteins and glycoproteins are located deeply and form hypophase (fluid component). . • Synthesis of phospholipids occurs in epitheliocytes of II-type or large epitheliocytes.
Surfactant • Phospholipids and proteins form membranous component. • Lipoproteins and glycoproteins are located deeply and form hypophase (fluid component). . • Synthesis of phospholipids occurs in epitheliocytes of II-type or large epitheliocytes.
 Alveolar macrophages • Alveolar macrophages scavenge the surface to remove inhaled particulate matter (e. g. , dust and pollen) and surfactant plenty. • Alveolar macrophages are derived from blood monocytes and belong to the mononuclear phagocytotic system. • They phagocytize red blood cells that may enter the alveoli in heart failure. • Lungs of urban dwellers and smokers usually show many alveolar and septal macrophages filled with carbon particles, anthracotic pigment, and birefringent needle-like particles of silica.
Alveolar macrophages • Alveolar macrophages scavenge the surface to remove inhaled particulate matter (e. g. , dust and pollen) and surfactant plenty. • Alveolar macrophages are derived from blood monocytes and belong to the mononuclear phagocytotic system. • They phagocytize red blood cells that may enter the alveoli in heart failure. • Lungs of urban dwellers and smokers usually show many alveolar and septal macrophages filled with carbon particles, anthracotic pigment, and birefringent needle-like particles of silica.
 Features of lungs in children • The period of differentiation of pulmonary acinus in child age occurs till 2 -years old. • Muscular elements of bronchi develop intensively from 2 till 4 years old. • Child’ s pulmonary acinus looks like adult’s to 7 years. • Number of alveoles in lung reaches the adult’s norm to 8 years.
Features of lungs in children • The period of differentiation of pulmonary acinus in child age occurs till 2 -years old. • Muscular elements of bronchi develop intensively from 2 till 4 years old. • Child’ s pulmonary acinus looks like adult’s to 7 years. • Number of alveoles in lung reaches the adult’s norm to 8 years.
 Control questions: • 1. How is structure of wall of bronchi changed depending of decrease of their caliber? • 2. What is acinus? • 3. Name structural components of acinus.
Control questions: • 1. How is structure of wall of bronchi changed depending of decrease of their caliber? • 2. What is acinus? • 3. Name structural components of acinus.
 Thank you for attention!
Thank you for attention!


