ea45e1756047674e9e4db4f775eb9dac.ppt
- Количество слайдов: 49
Learning Disability Awareness
Introductions Housekeeping Ice Breaker
Aims & Objectives Aim To increase awareness of the support needs of people with learning disabilities who access mental health services. Objectives Participants will have a greater awareness of the causes of learning disability and the impact of ‘global impairment’ on functioning. Participants will have gained a better understanding of the support needs of people who have learning disabilities. Participants will have gained a better understanding of the role of community learning disability teams and the services they can offer.
What do you want to get out of the session?
What is a Learning Disability?
Definitions of Learning Disabilities “A condition of arrested or incomplete development of the mind, which is especially characterised by impairment of skills manifested during the developmental period, which contribute to the overall level of intelligence i. e. cognitive, language, motor and social abilities. ” (World Health Organisation 1992)
Definitions of Learning Disabilities Learning disability includes the presence of: A significant reduced ability to understand new or complex information, to learn new skills (impaired intelligence). A reduced ability to cope independently (impaired social functioning), which started before adulthood and has a lasting effect on development. ” (Department of Health 2002)
Causes of learning disability Before birth (Pre-Natal) • Chromosome disorders e. g. Downs Syndrome. • Genetic disorders e. g. Tuberous sclerosis, Phenylketonuria • Congenital abnormalities e. g. Spina Bifida (central nervous system malformation) • Infection – e. g. Rubella, toxoplasmosis • Toxins – alcohol, smoking, drugs • Maternal disease – pre-eclampsia, thyroid, diabetes, physical trauma, radiation
During Birth (Perinatal) • Foetal stress, lack of oxygen e. g. Cerebral Palsy • Trauma, twins, obstructed birth, instrumental birth • Abnormal growth, intrauterine growth, born premature.
After Birth (Post Natal) • • Infections - encephalitis, meningitis Physical - non-accidental injury Environmental - emotional deprivation Toxins - lead, carbon monoxide
Prevalence of Learning Disability 2% of general population have a learning disability (= 985, 000*) There are 828, 000* Adults in England identified as having a learning disability (= 0. 47% of the general adult population). 177, 000* of these adults are known to services. (Do. H, 2004) Valuing People (Do. H, 2000) estimated 65, 000* children & 145, 000* adults Have a severe/profound learning disability. 1. 2 million individuals have a mild to moderate learning disability. *All of the above figures are predicted to rise by up to 3% in 2014 ‘People with Learning Disabilities in England - Ce. DR Research Report 2008: 1 (Emerson. E. , & Hatton. , C. 2008)
The medical model of disability describes different levels of learning disability • Mild Learning Disability • Moderate Learning Disability • Severe and Profound Learning Disability
LEARNING DISABILITY POKER
MILD Learning Disability The majority of people with a mild learning disability: - • • Live independently Many have partners & children In employment Have no need for extra support, except in times of crisis.
Moderate Learning disability People who have a moderate learning disability: - • Carry out everyday living activities with support. • May have difficulty communicating their needs. • Access day, outreach and supported living schemes.
Severe and Profound Learning Disability • Experience significantly increased health risks. • Highest rates of epilepsy. • Very likely to have a sensory impairment. • More likely to have physical disability. • More likely to communicate inappropriately by displaying ‘challenging behaviour’, including selfinjurious behaviour.
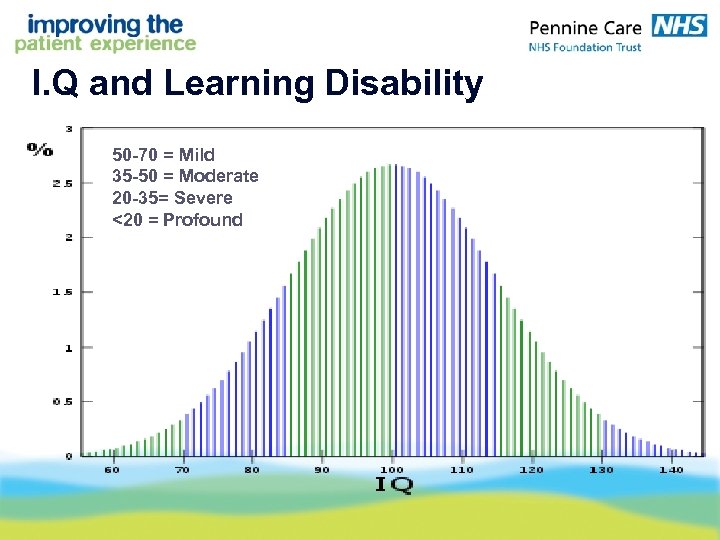
I. Q and Learning Disability 50 -70 = Mild 35 -50 = Moderate 20 -35= Severe <20 = Profound
Common difficulties in functioning • A significantly reduced ability to understand new or complex information, or learn new skills. • Communication difficulties • Difficulties monitoring and maintaining own health • A reduced ability to cope independently • Inability to support self financially • Poor social skills • Difficulty controlling emotions • Inability to occupy time constructively • Inability to identify and manage risks • Difficulty accessing community facilities
A learning disability is NOT • Problems with reading and writing or numeracy only • Emotional difficulties that may have disrupted schooling, influencing achievement • Conditions like Attention Deficit Disorder or hyperactive disorder or other difficulties with learning. • A Learning DIFFICULTY. • Asperger’s Syndrome and some people with ‘high functioning’ autism. • Disability resulting from brain trauma post 18 yrs of age. • Having a chaotic, alternative or culturally different lifestyle.
Mental Health Issues in Learning Disability Depression - 1. 3 – 3. 7% of people with a learning disability will have depression at any one time. (Twice as high as figure for non learning disabled population) General Anxiety Disorder and Bi-polar Disorder - higher in learning disability population. Dementia - prevalence rates in people with Down’s syndrome are significantly higher. Schizophrenia has a prevalence of 3% within the learning disability population. (Only 1% prevalence in non-learning disabled population. )
Recognising mental health problems How can you tell if someone has a mental health problem? • Often can be difficult to detect. • Changes in behaviour and functioning are a key indicator. • We are crucially looking for changes from what is normal for the person.
Could these changes indicate something other than a mental health problem? YES! – Changes in behaviour, functioning and thinking do not necessarily mean that the person has a mental health problem. These changes could be due to other considerations including physical illness.
Do mental health problems look the same in people with different degrees of learning disability? YES! But is dependent on: - 1. Person’s level of functioning 2. How person communicates their thoughts & feelings. 3. In people with a learning disability, aggression, self injury and other forms of challenging behaviour can be an indicator of changes in their mental health state.
Case study exercise Instructions Read through the first part of the case study that describes the ‘build up’ to the individual’s admission to hospital. Questions • Which behaviours do you think are attributed to his learning disability? • How would you support this individual on your ward? • Who would you contact for further advice and support? Read through the second part of the case study that provides important information about the individual’s history, background, diagnosis and general behaviour. Consider How does this additional information alter your initial view in relation to possible causes for his behaviour?
‘Then & Now’ Video (20 mins) (A short film about how attitudes towards people who have learning disabilities have changed fifty years)
‘PLAY YOUR CARDS RIGHT’ (Play your cards right exercise)
What are the barriers to good health?

Barriers to good health: • Communication • Lack of awareness / education • Poor choice around health issues • Access to services • Cost • Reliance on others • Attitudes • Understanding • Inconsistencies in care delivery • High turn over of staffing • Fear of health professionals • Confidentiality
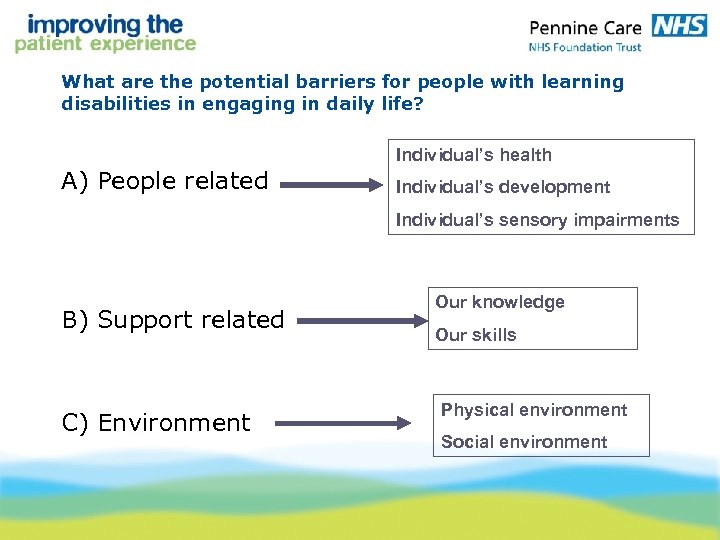
What are the potential barriers for people with learning disabilities in engaging in daily life? Individual’s health A) People related Individual’s development Individual’s sensory impairments B) Support related C) Environment Our knowledge Our skills Physical environment Social environment
How do we overcome some of these barriers? Develop a greater understanding of the individual. Alter our approaches Alter environments Teach the individual new skills Staff development
Overcoming barriers to effective assessment and treatment / intervention. • Make time to reassure person. • Improve Communication Become better at understanding what the person who has Learning Disability is trying to tell us about their condition. • Become better at communicating with the person who has Learning Disability. Explaining clearly: a) Why they are here (e. g. the ward) b) Treatment options (What is going to happen whilst you are here) • Manage anxiety / tolerance levels a) Anxiety over environment and interventions b) Knowing the persons important routines c) Recognise the person’s vulnerability due to their dual diagnosis • Access additional Resources (Human and equipment)
Consent and Mental Capacity • This is a big concern for health professionals. English law states that everyone should be deemed capable of giving consent until an assessment proves otherwise. • If a patient does not, in your opinion, have capacity to agree to or refuse treatment, you are legally obligated to act in their overall best interest. • The Mental Capacity Act 2005 provides the legal framework for assessing a person’s capacity to make decisions.
Consent and Mental Capacity • The health professional carrying out the procedure is ultimately responsible for ensuring that the patient is genuinely consenting to what is being done: it is they who will be responsible in law if this is challenged later. • Parents or carers cannot give consent for an adult who lacks capacity.
Two stage test of capacity 1. Is there an impairment of or disturbance in the functioning of the patients mind or brain? 2. Is the impairment or disturbance sufficient that the person lacks capacity to make that particular decision? • For consent to be valid the person must: a) Have the mental capacity to take the particular decision. b) Have received sufficient information to take it and not be acting under duress.
Assessing Mental Capacity If a patient is thought to have the ‘capacity’ to consent they must be able to: • • Understand the information about the proposed intervention Weigh up the pros and cons Retain the information Communicate their decision A patient is not to be treated as unable to make a decision unless all practicable steps have been taken to help them do so without success.
Best Interest Decisions • If a patient is unable to give consent then you must consider whether the proposed intervention or treatment is in their ‘best interest’ by weighing up the risks and benefits. Also take into consideration: • The person's past and present wishes and feelings • The beliefs and values that would be likely to influence their decision if they had capacity • The other factors that they would be likely to consider if they were able to do so
Considerations relating to ‘Best Interests’ • If it is practicable and appropriate consult with anyone named by the person or anyone engaged in caring for the person or interested in their welfare • Record all capacity assessments and best interest decisions in medical notes
Total Communication W. ords O. bjects S. igns S. ymbols U. nique P. hotographs
Overcoming Communication barriers If you only remember 10 things about communication… • Before you communicate with someone, you must GET THEIR ATTENTION, THEN HOLD IT. • When using words and sentences, DON’T OVERLOAD: Remember to K. I. S. S – KEEP IT SHORT AND SIMPLE. • It doesn’t hurt to REPEAT THINGS.
• Some people need TIME to understand. • Make sure that everything MATCHES – do both your body language (including facial expression) and the tone of your voice match the words that you are using. • QUESTION CAREFULLY – avoid closed questions, don’t lead. • NATURAL GESTURE (and SIGNING, if you know it) are very powerful supports to the words you use. • Use PICTURES, PHOTOS and OBJECTS to support your words – they can also help people make CHOICES (again, don’t overload or overface) • Be aware that some people have very INDIVIDUAL WAYS OF THEIR MESSAGES ACROSS
Managing Anxiety issues relating to investigations and treatment 1. Demonstrate procedure on carer first 2. De-sensitisation 3. Respect routines 4. Be aware of short concentration spans
Traffic Light – Hospital Assessment
The Community Learning Disability Team • The CLDT is a group of professional staff who provide assessment, support, advice and therapeutic interventions to people who have a learning disability • We operate an open referral system. • Criteria for access
CLDT members Can include- • • • • Community Learning Disability Nurses Psychologists Speech & Language Therapist Occupational Therapist Administration staff Social Workers Carer support officer Reviewing Officer Health care support workers Psychiatrist Strategic Health Facilitator Forensic Team Physiotherapist Creative art therapist Dietician
What we offer: • • • Health assessments and health action plans Behavioural assessments and interventions Mental health screening Skills assessments/skills teaching Communication assessments and interventions OT assessments/interventions Psychological therapies Community care assessments Monitoring and reviewing care packages Healthy living, anger management and sexuality and relationships group work • Carers assessments and services • Dementia screening
ANY QUESTIONS?
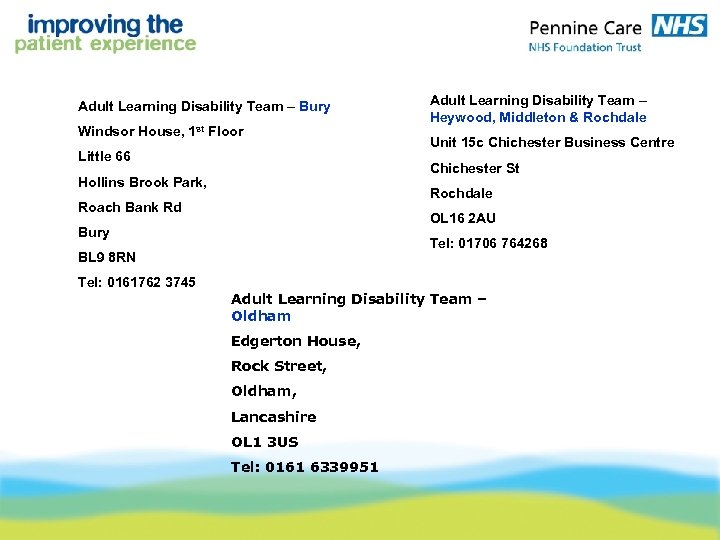
Adult Learning Disability Team – Bury Windsor House, 1 st Floor Little 66 Unit 15 c Chichester Business Centre Chichester St Hollins Brook Park, Rochdale Roach Bank Rd OL 16 2 AU Bury Tel: 01706 764268 BL 9 8 RN Tel: 0161762 3745 Adult Learning Disability Team – Heywood, Middleton & Rochdale Adult Learning Disability Team – Oldham Edgerton House, Rock Street, Oldham, Lancashire OL 1 3 US Tel: 0161 6339951
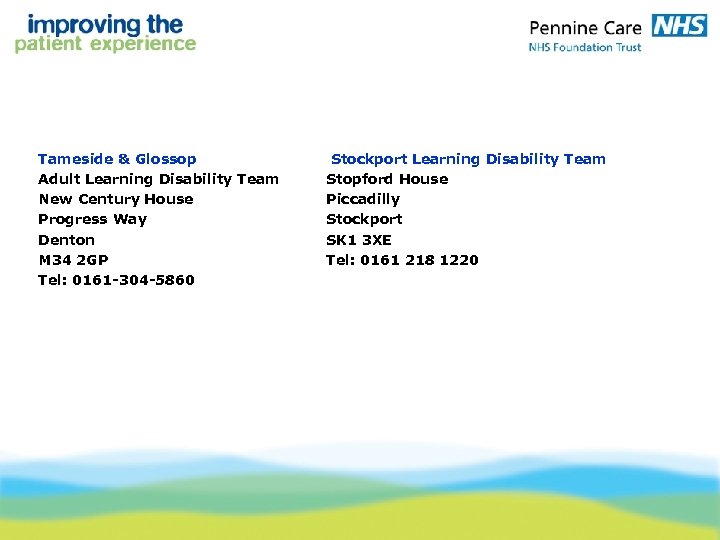
Tameside & Glossop Adult Learning Disability Team New Century House Progress Way Denton M 34 2 GP Tel: 0161 -304 -5860 Stockport Learning Disability Team Stopford House Piccadilly Stockport SK 1 3 XE Tel: 0161 218 1220

Mental Health Champions Karen Ashcroft - Rochdale - Tel: 01706 754371 Particia O’Hara - Oldham - Tel: 0161 627 8032 - Tel: 0161 778 2527 Janet Dale - Stockport - Tel: 0161 716 3727 Clare Diggle - Tameside - Tel: To be confirmed Damian Mc Kenna - Bury
ea45e1756047674e9e4db4f775eb9dac.ppt