ac057dc21ca804b6b59f3369eb3c43ef.ppt
- Количество слайдов: 146
LEARN TO ADAPT “Change is inevitable-except from a vending machine” -Robert C. Gallagher
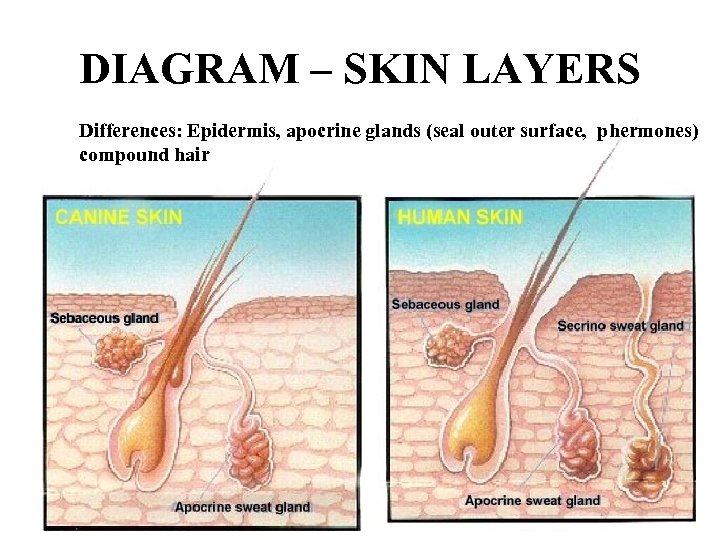
DIAGRAM – SKIN LAYERS Differences: Epidermis, apocrine glands (seal outer surface, phermones) compound hair
Apocrine vs. Sebaceous • Apocrine – ~ Sweat glands • Specialized forms in eyelids, external ear canal – Hair follicle complex – Anal sacs – Sympathetic NS • Sebaceous – Hair follicles – Secrete sebum (oily) – Large glands • Dog: dorsum of tail, Mucocutaneous junction • Cat: dorsum of tail, on lip margins and under chin
Skin • Protects from physical, chemical and microbiological injury • Sensory organ: pain, heat, cold, touch • Storage: Electrolytes, water, proteins, fats and carbohydrates, activates Vit D by sunlight • Epidermis • Dermis • Hypodermis/ subcuticular: Stores fat for insulation and energy
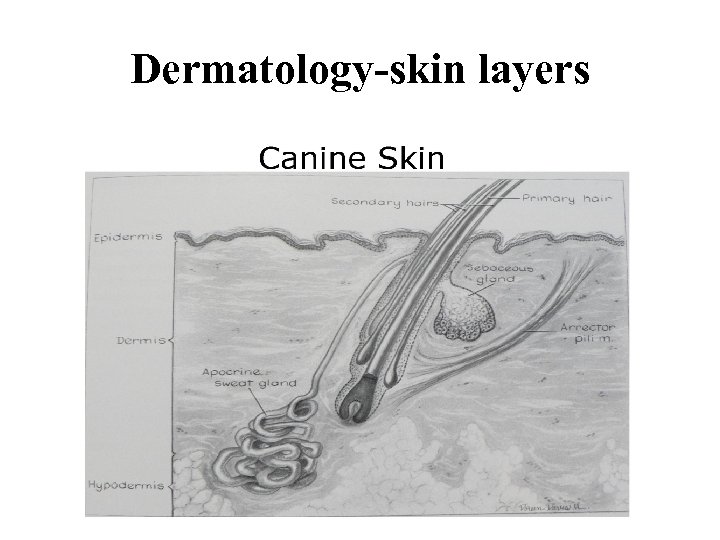
Dermatology-skin layers
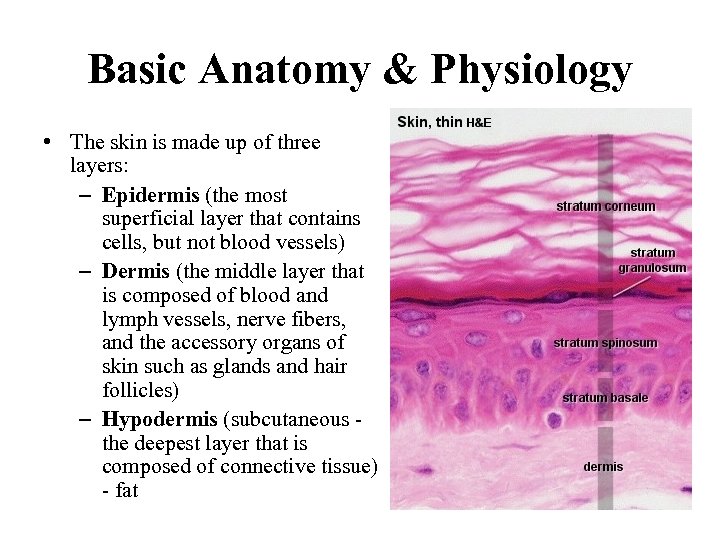
Basic Anatomy & Physiology • The skin is made up of three layers: – Epidermis (the most superficial layer that contains cells, but not blood vessels) – Dermis (the middle layer that is composed of blood and lymph vessels, nerve fibers, and the accessory organs of skin such as glands and hair follicles) – Hypodermis (subcutaneous the deepest layer that is composed of connective tissue) - fat
Skin - Function • • • • Enclosing barrier: Water and electrolyte loss Environment protection Temperature regulation Sensory perception: touch, temp. and pain Motion and shape Antimicrobial and antifungal Blood pressure control: peripheral vascular bed Secretion: apocrine and sebaceous glands Adnexa: hair, nails, hooves, horny layer – epidermis Storage: Electrolyte, H 2 O, Vit. , fat, protein, Carbs and other. . Pigmentation: color and sun protection Excretion: some Sun > activate vit D > normal Ca absorption
Definitions • • Dermatology: study of diseases of the skin Dermatosis: skin disease Alopecia: hairloss Seborrhea: Excessive secretion of sebum (oily secretion of the sebaceous glands composed of fat and epithelial debris) Scale: Flakes of stratum corneum on the skin surface or hair coat; various colors Erythema: increased redness Collarette: circular arrangement of scale with central area of hyperpigmentation Crust: accumulation of dead cells and exudate on skin surface
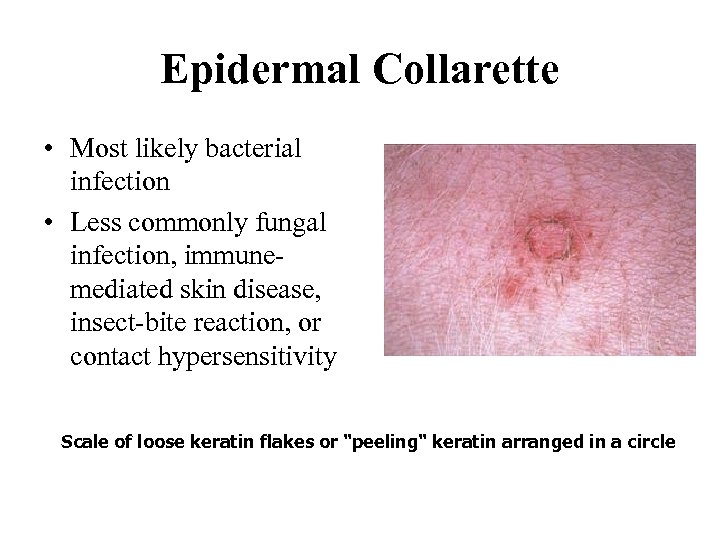
Epidermal Collarette • Most likely bacterial infection • Less commonly fungal infection, immunemediated skin disease, insect-bite reaction, or contact hypersensitivity Scale of loose keratin flakes or "peeling" keratin arranged in a circle
Definitions • • Ectoparasites: external parasites Skin Scraping: method of examining skin for parasites Dermatophyte: fungi that grow on the skin Dermatomycosis: fungal skin infection not involving pathogens below Dermatophytosis (ringworm): a skin infection with keratinophilic fungi (e. g. Microsporum; Trichophyton, Epidermophyton) Pyoderma: Bacterial infection of skin • Superficial • Deep Fungal culture – lab test used to grow dermatophytes for identification Bacterial culture and sensitivity: lab test used to grow and identify bacteria from lesions and determine antibiotic sensitivity
Definitions • Impetigo (not intertigo: skin fold pyoderma): Superficial bacterial skin infection seen in young dogs “puppy pyoderma” (staph) • Acne: Pores clogged with oil forming “blackheads”, esp chin • Lesion: area of altered skin • Rash: wide spread eruption of lesions • Hyperpigmentation: increased pigmentation (melanin) of skin (epidermal/dermal) • Lichenification: Thickening and hardening of skin characterized by exaggerated superficial skin markings. • Cyst: Fluctuant nodule; walled off, fluid filled nodule
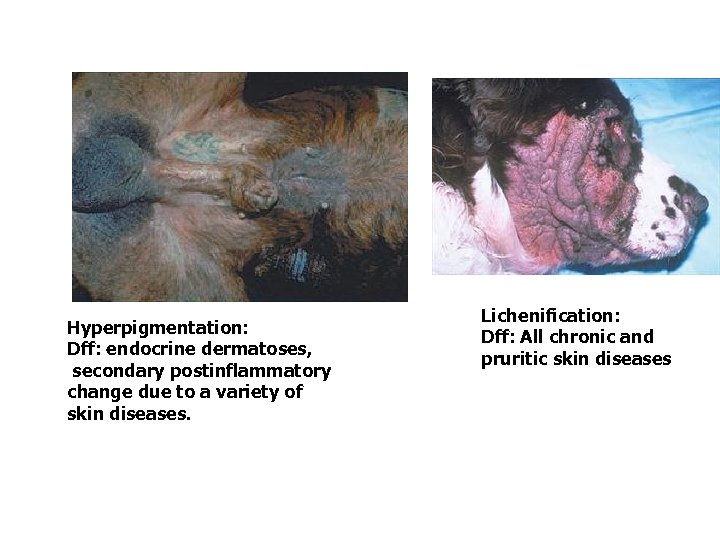
Hyperpigmentation: Dff: endocrine dermatoses, secondary postinflammatory change due to a variety of skin diseases. Lichenification: Dff: All chronic and pruritic skin diseases
Definitions • Macule: A focal, circumscribed, nonpalpable change in color <1 cm (when it is larger, it is termed a patch). • Papule: small, circumscribed, solid elevated lesion of the skin ~ 1 cm • Wheal: A sharply circumscribed, raised, edematous lesion that appears and disappears within minutes to hours • Pustule: a small, elevated, circumscribed, puscontaining lesion of the skin within the epidermis. • Abscess: localized collection of pus; larger than a pustule • Cellulitis: swollen, tender area of skin with bacterial infection; can develop into an abscess

Macule: Vitiligo, discoid lupus erythematosus, uveodermatologic syndrome, mucocutaneous pyoderma. Papule: Bacterial folliculitis, demodicosis, fungal folliculitis, flea-bite and mosquito-bite hypersensitivity, scabies, contact allergy, autoimmune skin disease, drug eruption
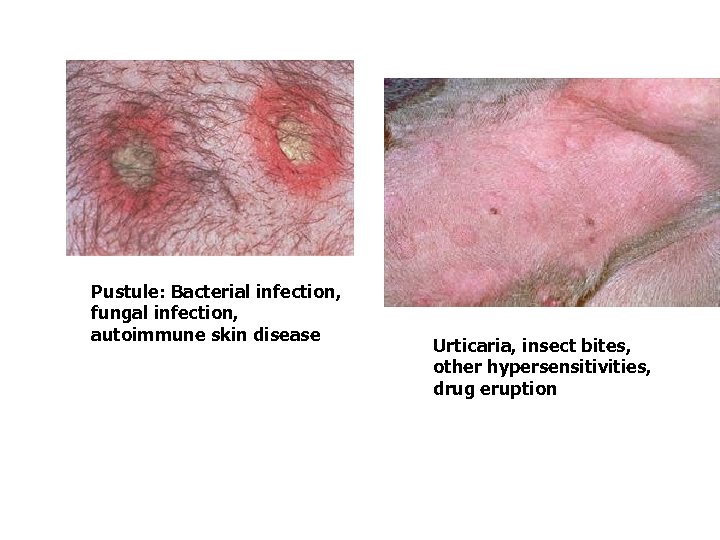
Pustule: Bacterial infection, fungal infection, autoimmune skin disease Urticaria, insect bites, other hypersensitivities, drug eruption
Definitions • Granulation tissue: new tissue in a healing wound; consists of connective tissue and capillaries • Erosion: loss of skin surface; shallow, moist, crusted does not penetrate basement membrane • Ulcer: loss of the epidermis resulting in exposure of dermis • Comedone: dilated hair follicle blocked with sebum and other cellular debris
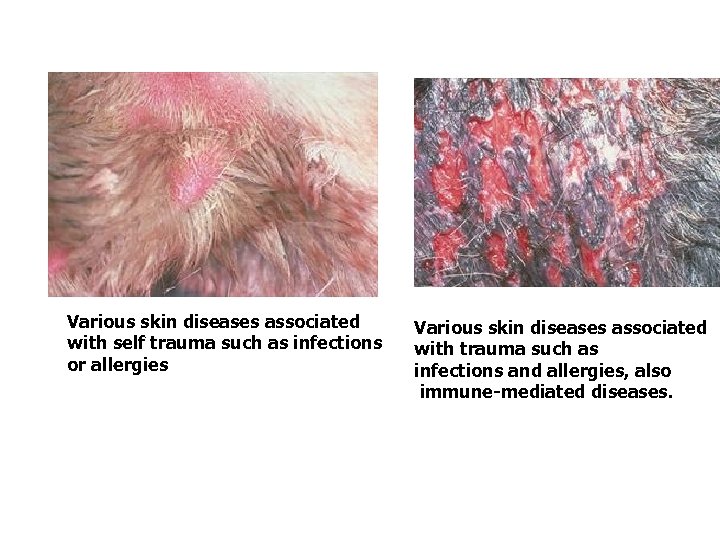
Various skin diseases associated with self trauma such as infections or allergies Various skin diseases associated with trauma such as infections and allergies, also immune-mediated diseases.
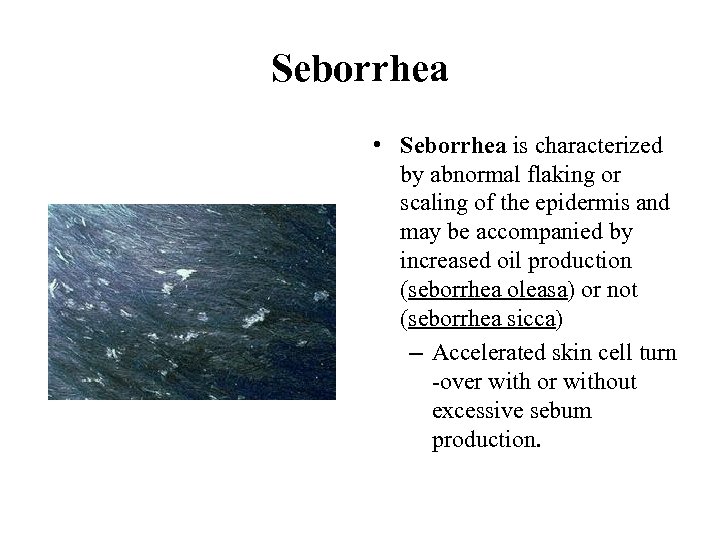
Seborrhea • Seborrhea is characterized by abnormal flaking or scaling of the epidermis and may be accompanied by increased oil production (seborrhea oleasa) or not (seborrhea sicca) – Accelerated skin cell turn -over with or without excessive sebum production.
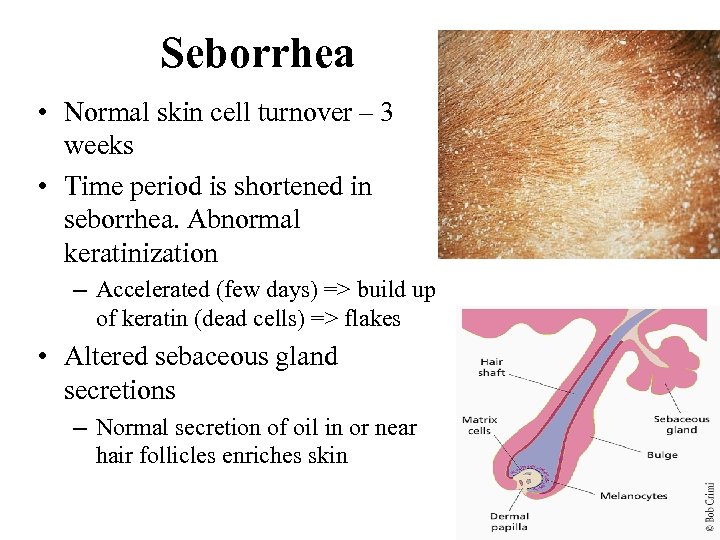
Seborrhea • Normal skin cell turnover – 3 weeks • Time period is shortened in seborrhea. Abnormal keratinization – Accelerated (few days) => build up of keratin (dead cells) => flakes • Altered sebaceous gland secretions – Normal secretion of oil in or near hair follicles enriches skin

Seborrhea
Seborrhea • Causes – Primary: hereditary as in Amer. Cocker Spaniel, Eng. Springer Spaniel, Westies, Basset Hounds – Secondary: disease/injury to skin from other causes • Allergies, parasites, nutritional disorders, immune-mediated, endocrine disorders (hypothyroidism) • Types – Seborrhea sicca: dry, only scaliness – Seborrhea oleosa: oily + scales

Seborrhea sicca DRY and SCALY

Seborrhea oleosa
Keratolytics • Keratolytics are an important group of antiseborrheics – Keratolytics remove excess keratin and promote loosening of the outer layers of the epidermis – Keratolytics break down the protein structure of the keratin layer, permitting easier removal of this material – Found in medicated shampoos to help in treatment of seborrhea

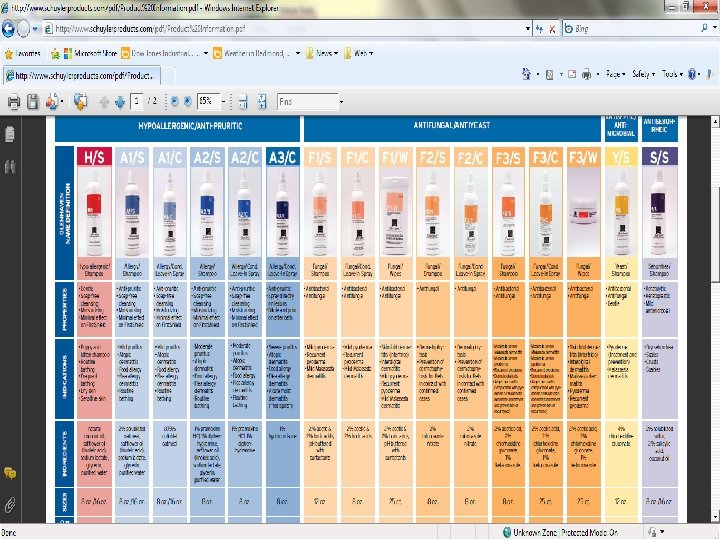
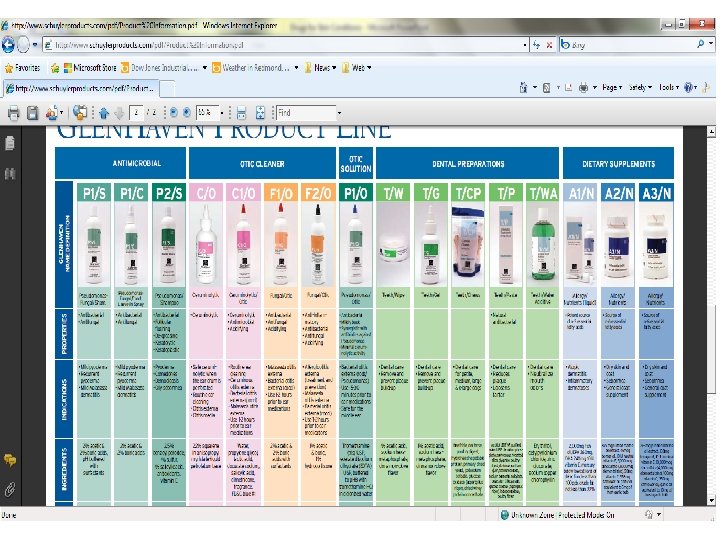
Seborrhea – Treatment • Medicated shampoos – Sicca: Sulfur (keratolytic, antipruritic, antibacterial, antifungal, antiparasitic); Salicyclic acid (KL, AP, AB) – Oleaso: Coal tar: degreaser, KL; BENZOYL PEROXIDE: Also for Moist dermatitis, pyoderma, stud tail – Conditioners

Seborrhea – Treatment • Clip hair so shampoo can penetrate • If secondary, treat underlying cause – Antifungal and/or antibacterial meds • Omega-3 fatty acid supplements – Anti-inflammatory, antipruritic properties
Seborrheic Fungal Dermatitis • Malassezia species • Some commensal on skin (normal) • Cause infection when skin surface altered/abnormal or immunosuppressed • Diagnosed by cytology (stained slides) – Skin impressions: Samples can be obtained via tape prep or impression smear • Tx: – – 2% miconazole/2% chlorhexidine shampoo Selenium sulphide Other Antifungals: ketoconazole, clotrimazole, miconazole Oral ketoconazole x 3+ weeks (not approved in dogs and cats)
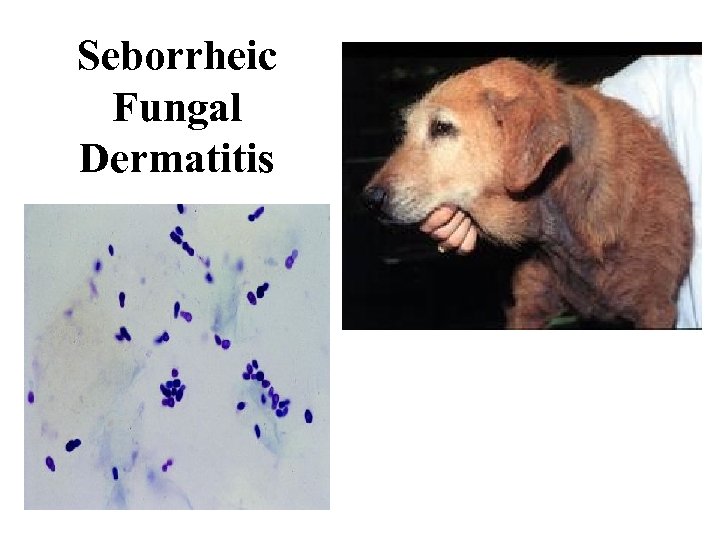
Seborrheic Fungal Dermatitis
Pyodermas • Definition: Bacterial infection of skin, superficial or deep; Primary or secondary - Occurs when: - skin surface broken - skin macerated by chronic exposure to moisture - Normal bacteria altered - Circulation impaired - Immunocompetence impaired (aka immunosuppressed) • Superficial- Lesion usually involve superficial epidermis and heal w/o scarring, short duration, rarely ill
Pyoderma - Causes - Dogs - Staph intermedius - Cats – Pasteurella multocida - Deep pyodermas – gram-negative organisms (E. coli, proteus sp, pseudomonas sp) - Risk factors - Allergies Fungal infections Endocrine diseases Immune incompetence Seborrhea Conformation – ex: skin folds Trauma Foreign body
Pyoderma - Superficial – commonly the trunk - Deep – chin, nose, pressure points, feet, generalized, skin folds - PE may show: papules, pustules, crusts, epidermal collarettes, circular erythematous or hyperpigmented spots, alopecia, scaling, lichenification, abscess, cellulitis, etc. .
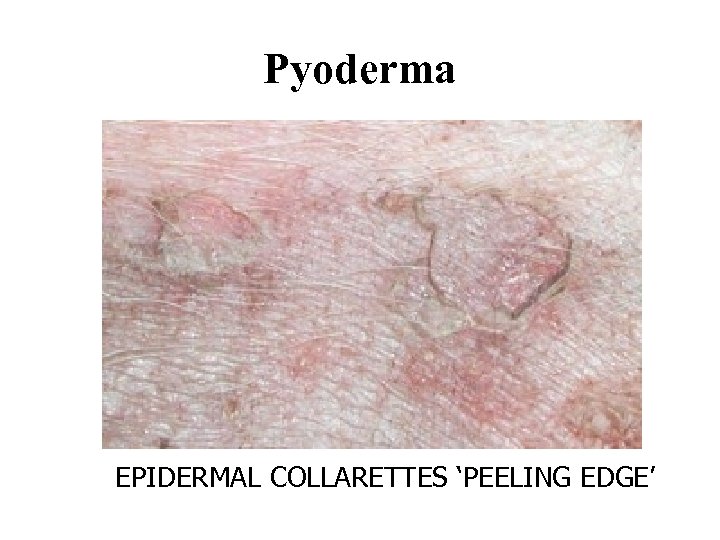
Pyoderma EPIDERMAL COLLARETTES ‘PEELING EDGE’
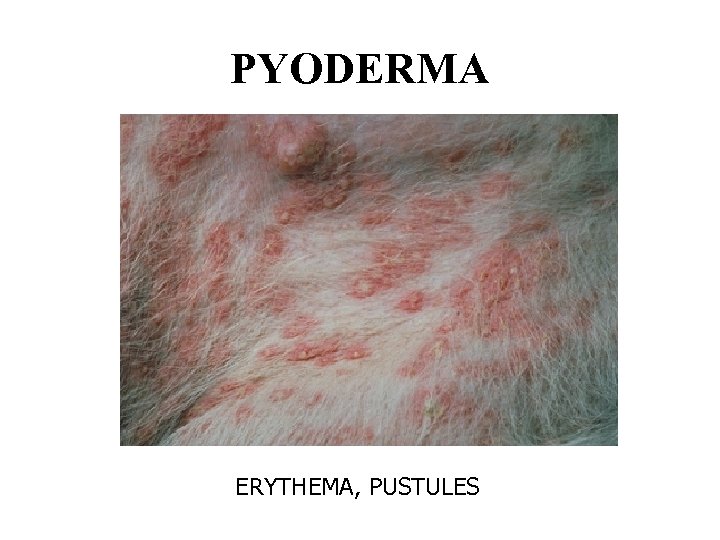
PYODERMA ERYTHEMA, PUSTULES
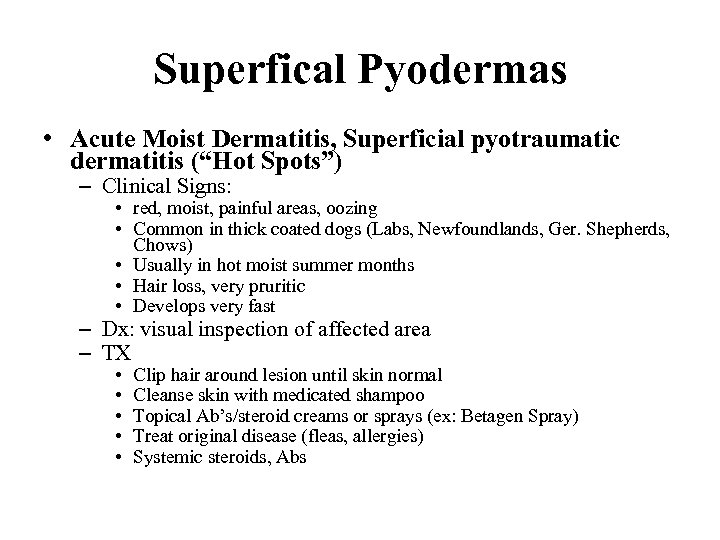
Superfical Pyodermas • Acute Moist Dermatitis, Superficial pyotraumatic dermatitis (“Hot Spots”) – Clinical Signs: • red, moist, painful areas, oozing • Common in thick coated dogs (Labs, Newfoundlands, Ger. Shepherds, Chows) • Usually in hot moist summer months • Hair loss, very pruritic • Develops very fast – Dx: visual inspection of affected area – TX • • • Clip hair around lesion until skin normal Cleanse skin with medicated shampoo Topical Ab’s/steroid creams or sprays (ex: Betagen Spray) Treat original disease (fleas, allergies) Systemic steroids, Abs
Superficial Pyodermas – Client Info • Gentle cleansing BID • Owner should wash hands after treatment • E-collar may be necessary

Superficial Pyoderma: “Hot spot”

Superficial Pyoderma: “Hot Spot”
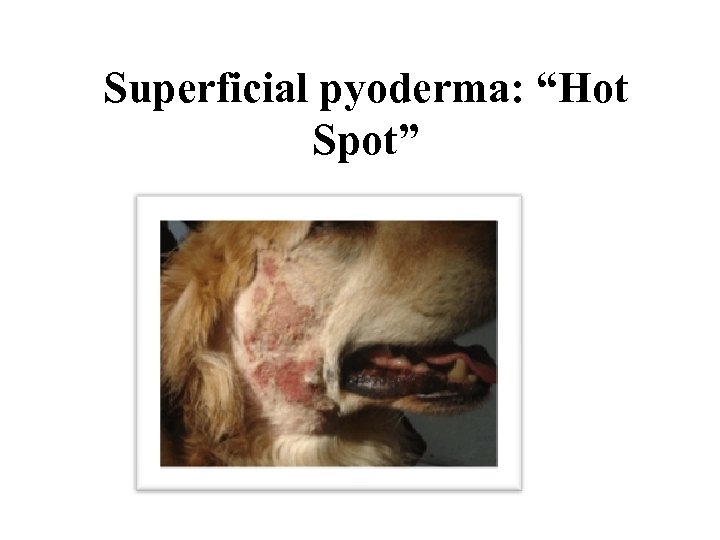
Superficial pyoderma: “Hot Spot”
Superficial Pyodermas • Impetigo (aka superficial pustular dermatitis) – Signalment: young dogs secondary to malnourishment and poor hygiene – Strep and Staph occasionally cultured from lesions – Clinical Signs: non-pruritic, non-painful pustules and papules on abdomen – Dx: Physical signs – Tx: Systemic Ab, Ab shampoo q 2 -3 days, +/- Topical Ab cream – Client Info: Not contagious, usually clears by 6 months
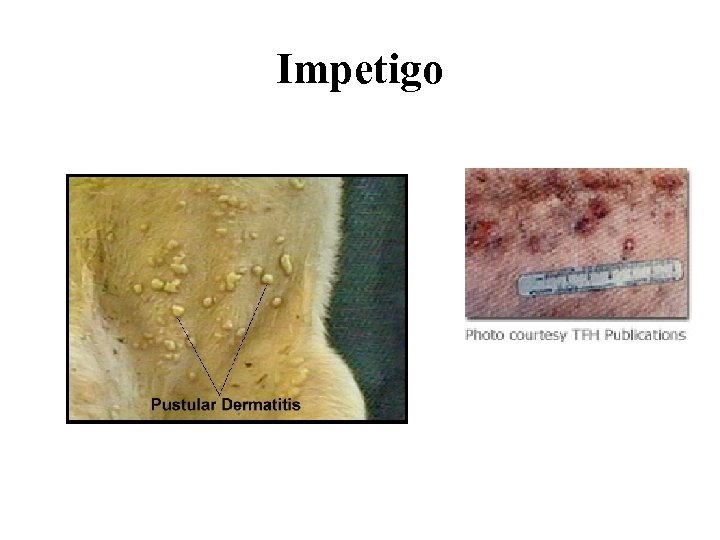
Impetigo
Skin Fold Pyoderma (aka Intertrigo) • Occurs in breeds with abundant skin – Facial folds, vulvar folds, tail folds – Spaniels, Bulldogs, Pekingese, Pugs, Bostons, obese dogs • Folds trap moisture, heat and bacteria • Usually chronic • Dx: Affected area moist, red, ulcerated • Tx: Relieve symptoms by cleaning and drying lesion – – Sx reduction of skin fold may be only permanent solution Weight loss in obese patients Abs, chlorhexidine-containing pledgets Antibacterial and/or benzoyl peroxide shampoos • Client Info – Require long term medical management – Keep area dry and clean – Keep hair/folds away from eyes
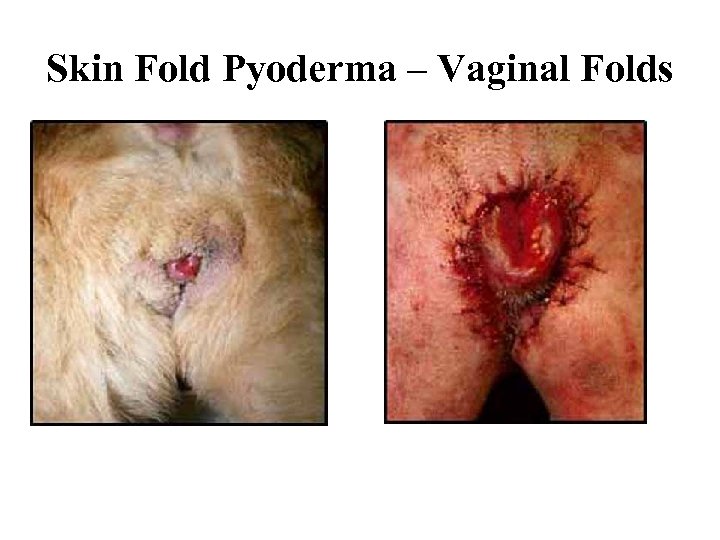
Skin Fold Pyoderma – Vaginal Folds
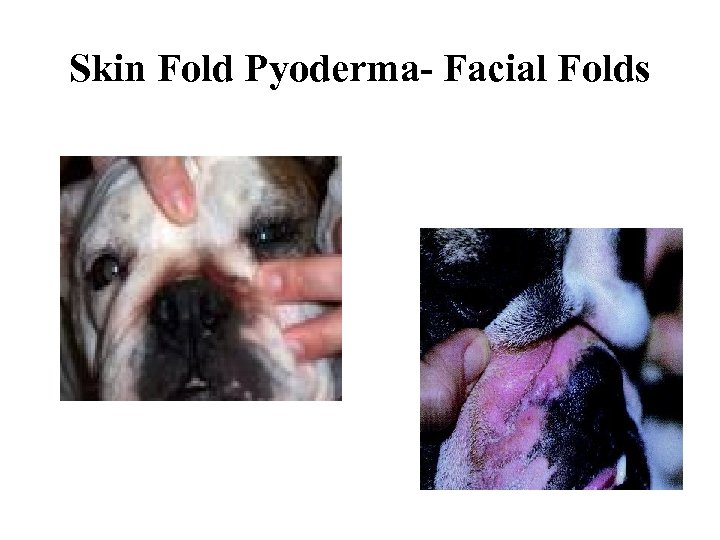
Skin Fold Pyoderma- Facial Folds
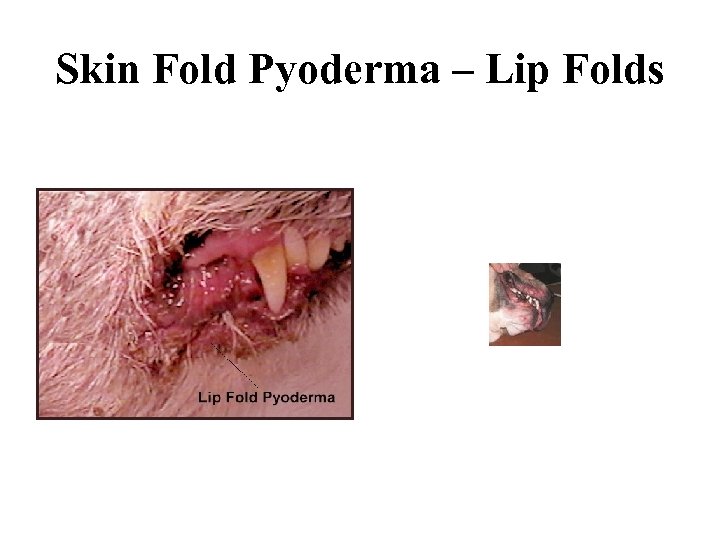
Skin Fold Pyoderma – Lip Folds
Acne • Common in young short-haired dog breeds and cats - can be chronic • Clinical Signs: – Chin swollen and painful to touch, dark spots => black heads (comedones) • Dx: Appearance, r/o bite wounds, abscesses • Rx: – clip hair on chin – clean daily with human acne product (helps with follicular flushing) – benzoyl peroxide – systemic antibiotics – Topical Mupirocin ointment or cream • Client Info: – May become chronic – Daily cleaning of chin – Use only ceramic or stainless steel bowls – NO PLASTIC
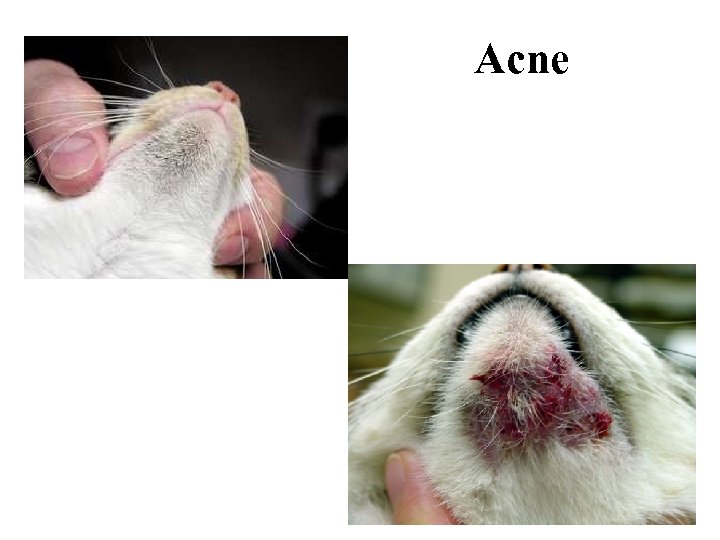
Acne
Deep Pyodermas • More difficult to treat than Superficial Pyodermas • Often chronic • Patients are often resistant to treatment or immunosuppressed • Frequently involves Staph intermedius, Proteus, Pseudomonas, e. Coli
Deep Pyodermas • Clinical Signs – Papules and pustules, – +/- fever – Draining fistulas • Dx: clinical signs • Tx: – Thorough cleaning – Systemic Ab’s (clavamox, baytril, cephalexin) • Client Info – Causative organism often drug resistant – Treatment may be prolonged and expensive in large breed dogs – Some animals will never fully recovery
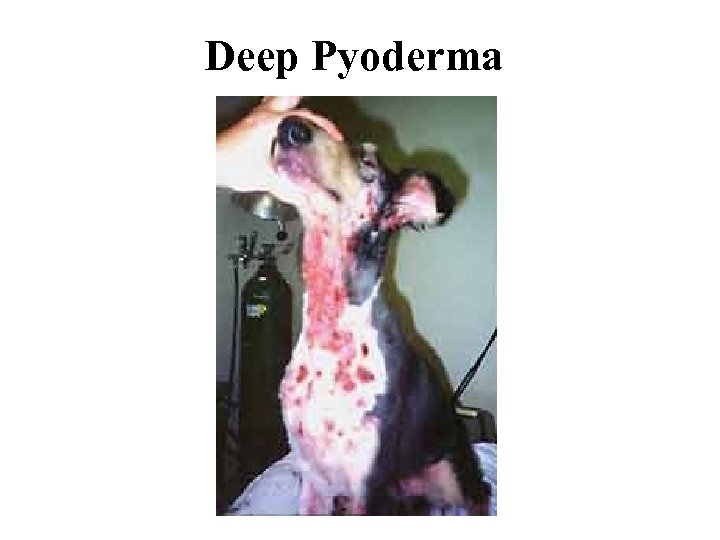
Deep Pyoderma
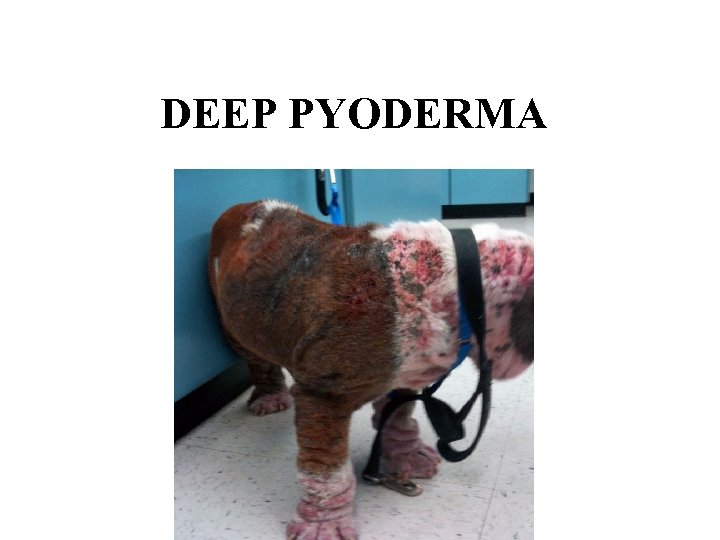
DEEP PYODERMA
Live each moment! “It is only possible to live happily ever after on a day to day basis. ” -Margaret Bonnano
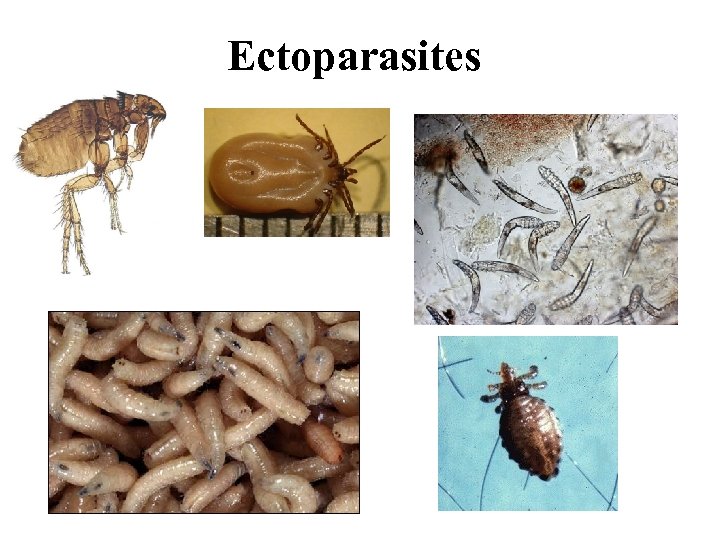
Ectoparasites
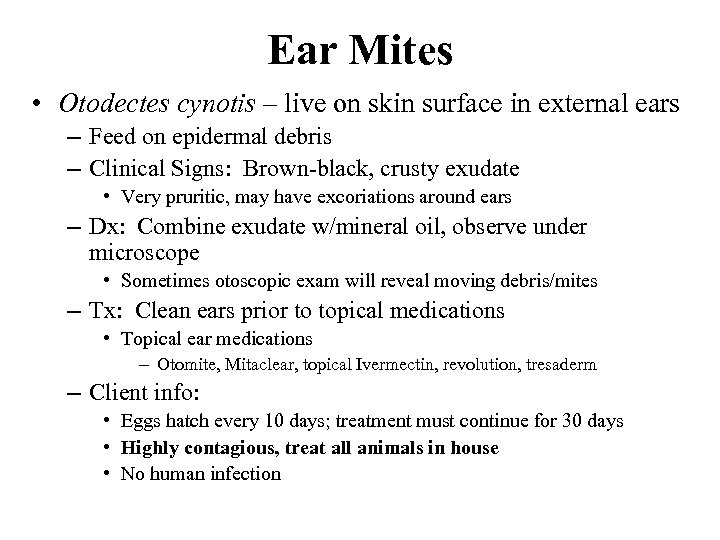
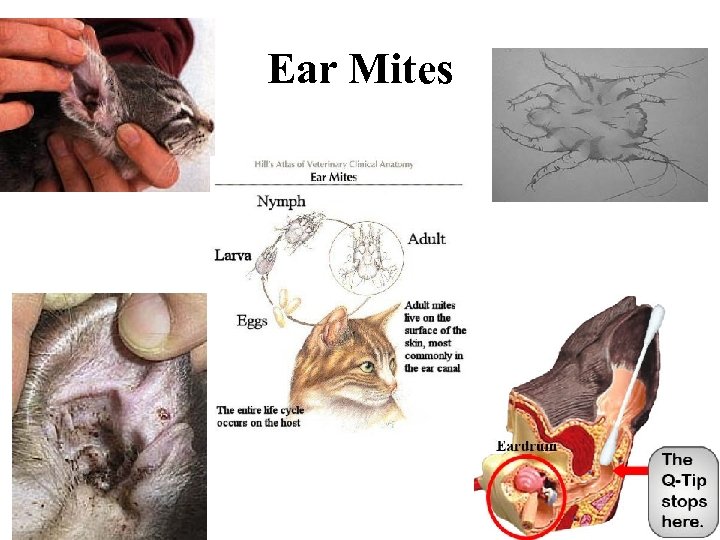
Ear Mites • Otodectes cynotis – live on skin surface in external ears – Feed on epidermal debris – Clinical Signs: Brown-black, crusty exudate • Very pruritic, may have excoriations around ears – Dx: Combine exudate w/mineral oil, observe under microscope • Sometimes otoscopic exam will reveal moving debris/mites – Tx: Clean ears prior to topical medications • Topical ear medications – Otomite, Mitaclear, topical Ivermectin, revolution, tresaderm – Client info: • Eggs hatch every 10 days; treatment must continue for 30 days • Highly contagious, treat all animals in house • No human infection
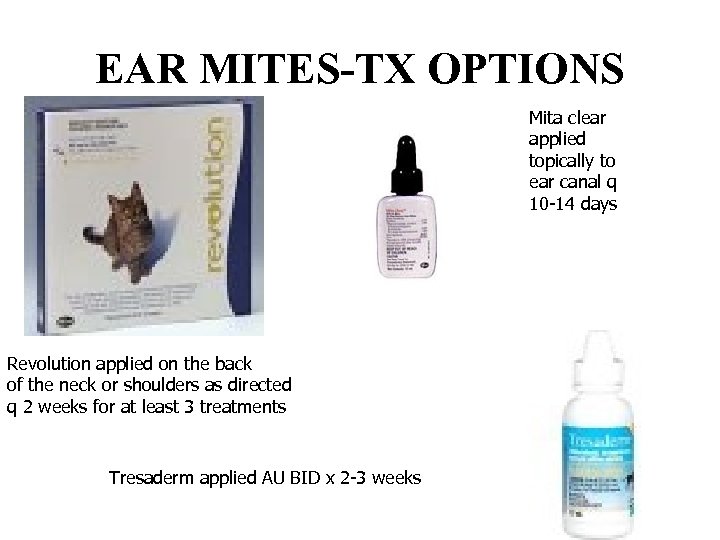
EAR MITES-TX OPTIONS Mita clear applied topically to ear canal q 10 -14 days Revolution applied on the back of the neck or shoulders as directed q 2 weeks for at least 3 treatments Tresaderm applied AU BID x 2 -3 weeks
Ear Mites
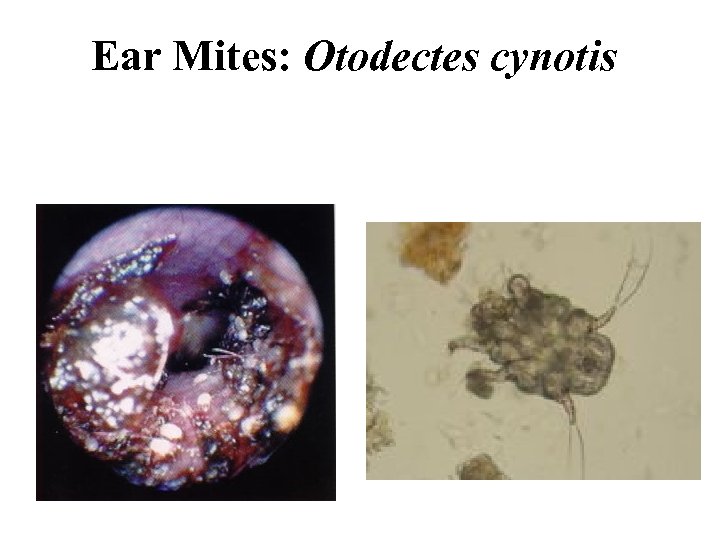
Ear Mites: Otodectes cynotis
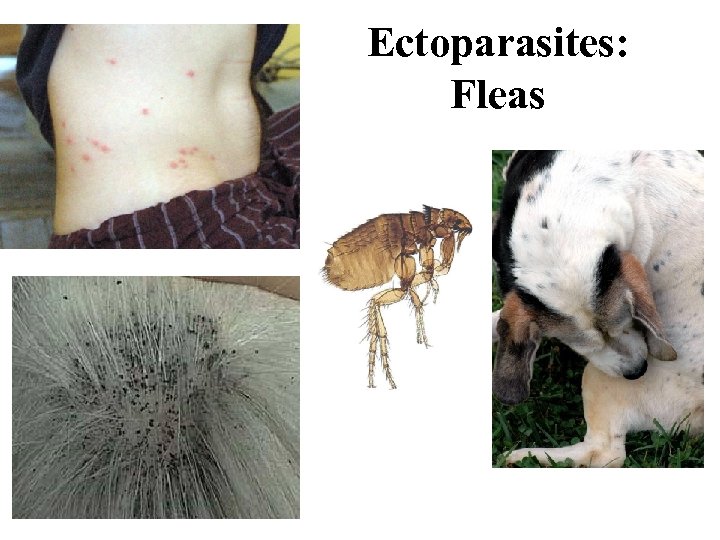
Ectoparasites: Fleas
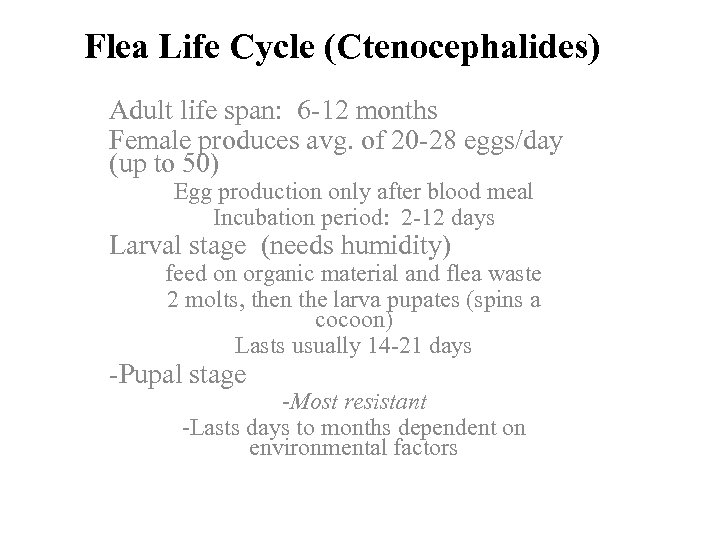
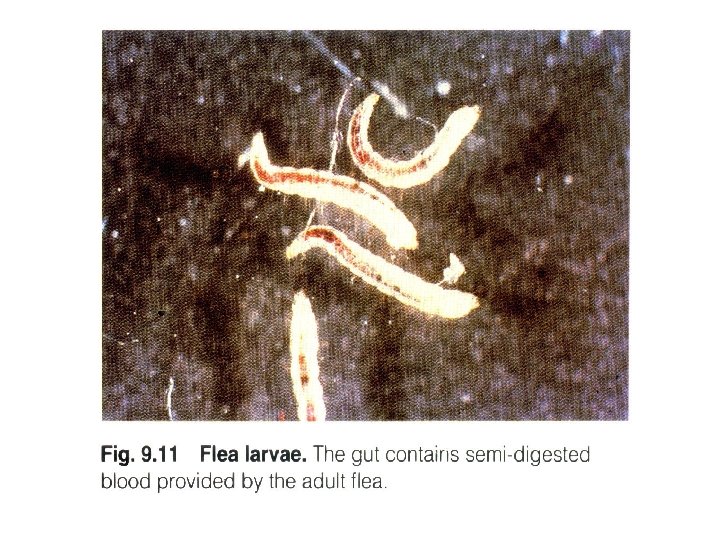
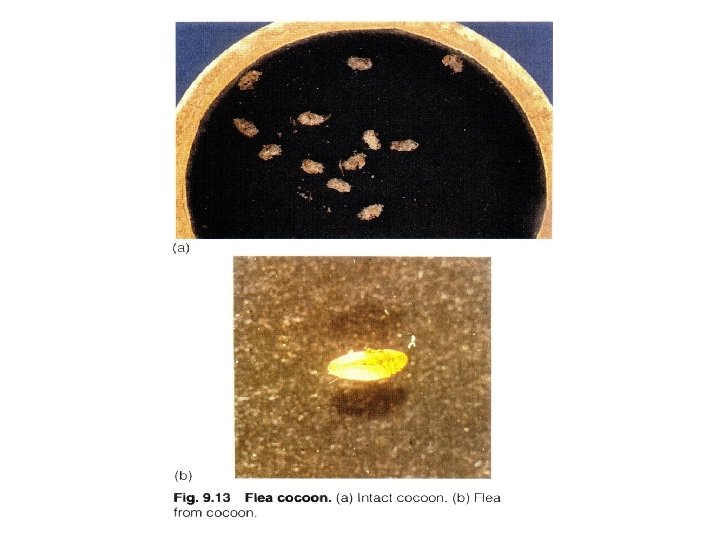
Flea Life Cycle (Ctenocephalides) Adult life span: 6 -12 months Female produces avg. of 20 -28 eggs/day (up to 50) Egg production only after blood meal Incubation period: 2 -12 days Larval stage (needs humidity) feed on organic material and flea waste 2 molts, then the larva pupates (spins a cocoon) Lasts usually 14 -21 days -Pupal stage -Most resistant -Lasts days to months dependent on environmental factors
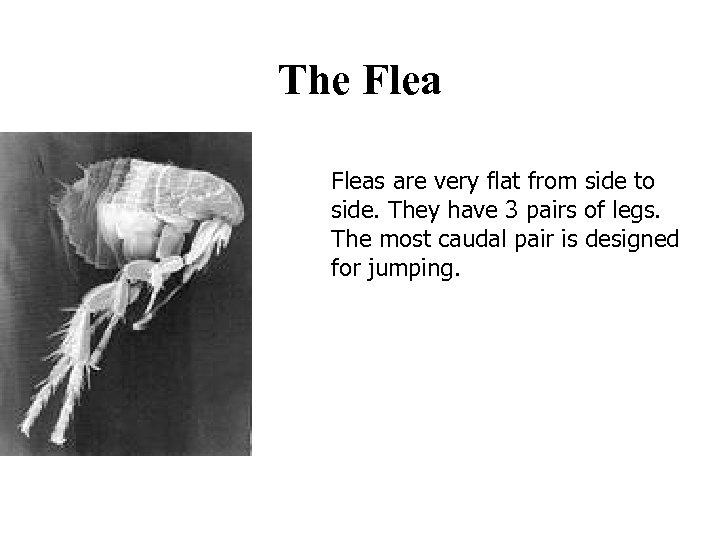
The Fleas are very flat from side to side. They have 3 pairs of legs. The most caudal pair is designed for jumping.
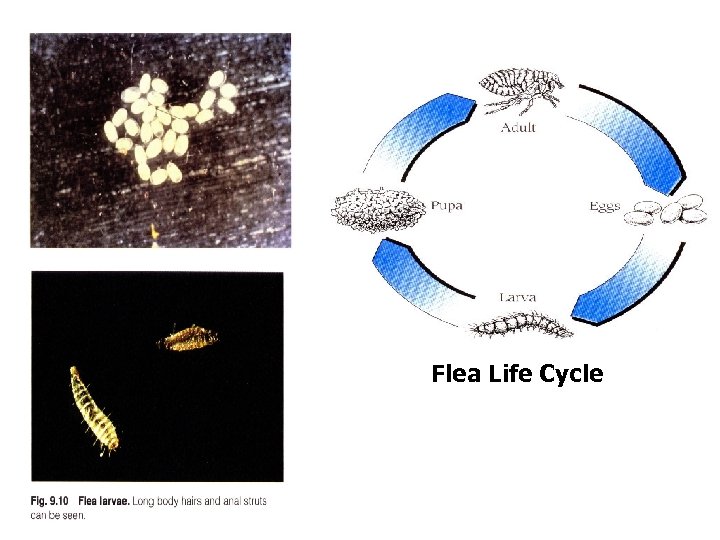
Flea Life Cycle
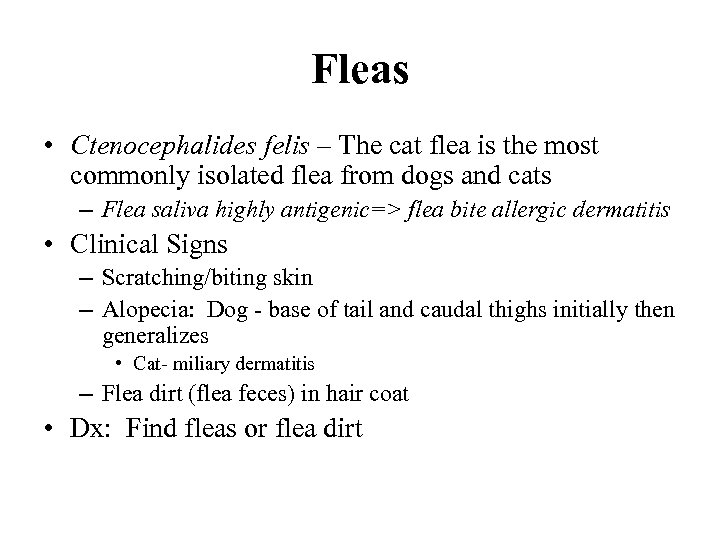
Fleas • Ctenocephalides felis – The cat flea is the most commonly isolated flea from dogs and cats – Flea saliva highly antigenic=> flea bite allergic dermatitis • Clinical Signs – Scratching/biting skin – Alopecia: Dog - base of tail and caudal thighs initially then generalizes • Cat- miliary dermatitis – Flea dirt (flea feces) in hair coat • Dx: Find fleas or flea dirt
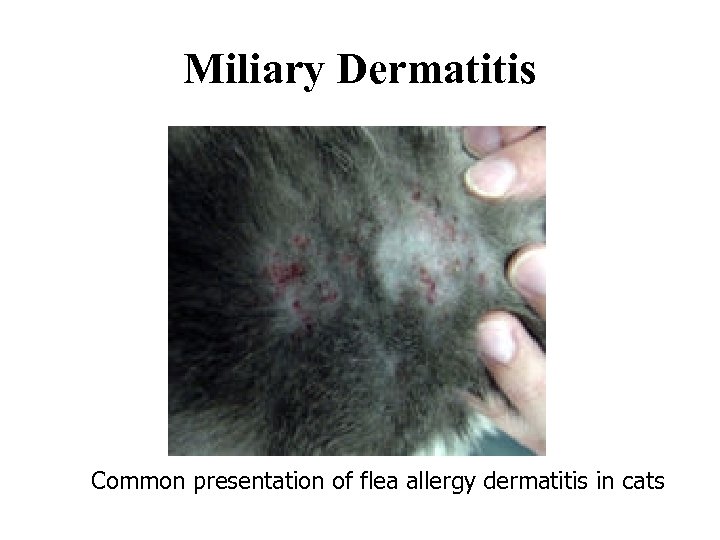
Miliary Dermatitis Common presentation of flea allergy dermatitis in cats
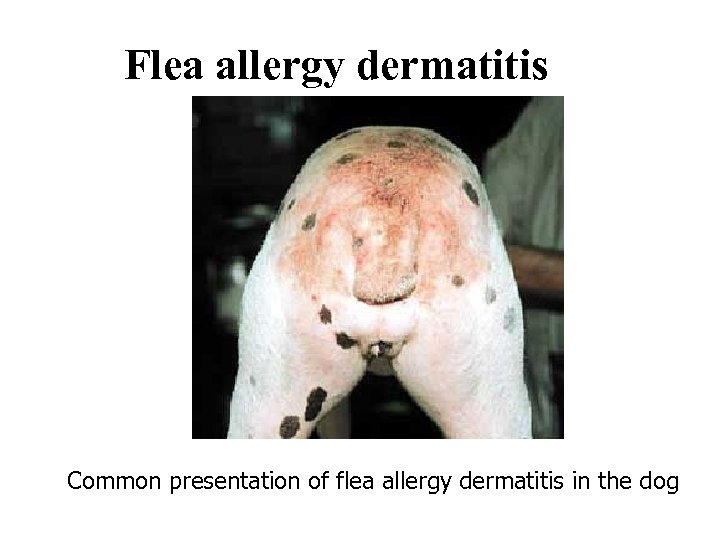
Flea allergy dermatitis Common presentation of flea allergy dermatitis in the dog
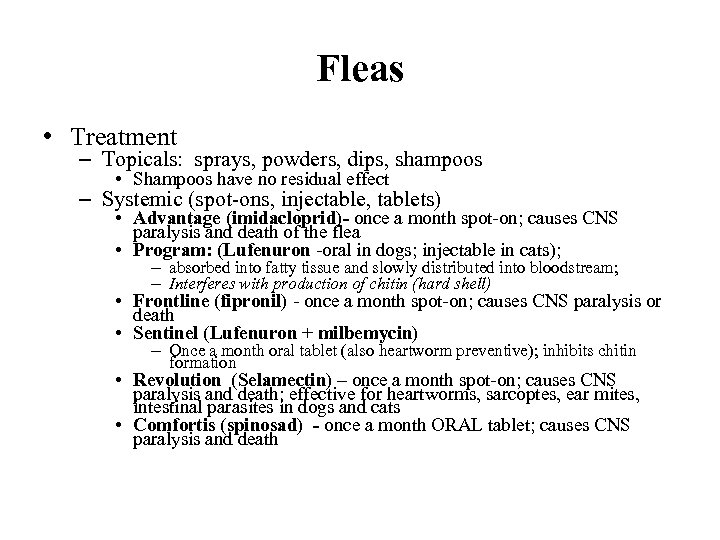
Fleas • Treatment – Topicals: sprays, powders, dips, shampoos • Shampoos have no residual effect – Systemic (spot-ons, injectable, tablets) • Advantage (imidacloprid)- once a month spot-on; causes CNS paralysis and death of the flea • Program: (Lufenuron -oral in dogs; injectable in cats); – absorbed into fatty tissue and slowly distributed into bloodstream; – Interferes with production of chitin (hard shell) • Frontline (fipronil) - once a month spot-on; causes CNS paralysis or death • Sentinel (Lufenuron + milbemycin) – Once a month oral tablet (also heartworm preventive); inhibits chitin formation • Revolution (Selamectin) – once a month spot-on; causes CNS paralysis and death; effective for heartworms, sarcoptes, ear mites, intestinal parasites in dogs and cats • Comfortis (spinosad) - once a month ORAL tablet; causes CNS paralysis and death
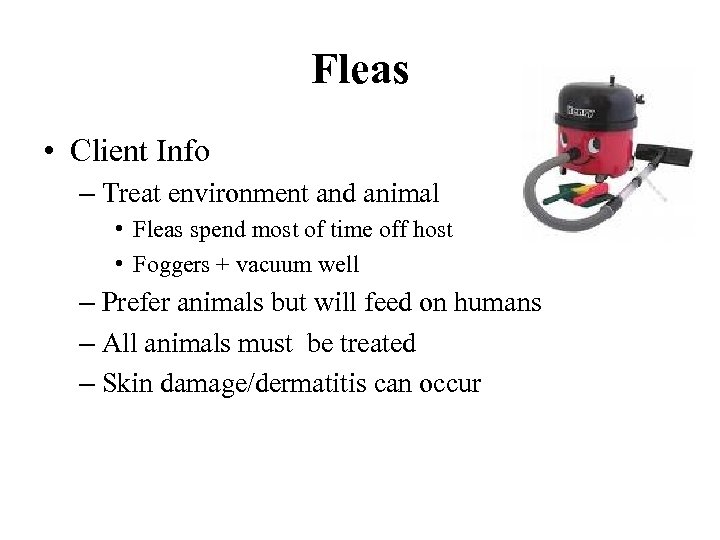
Fleas • Client Info – Treat environment and animal • Fleas spend most of time off host • Foggers + vacuum well – Prefer animals but will feed on humans – All animals must be treated – Skin damage/dermatitis can occur
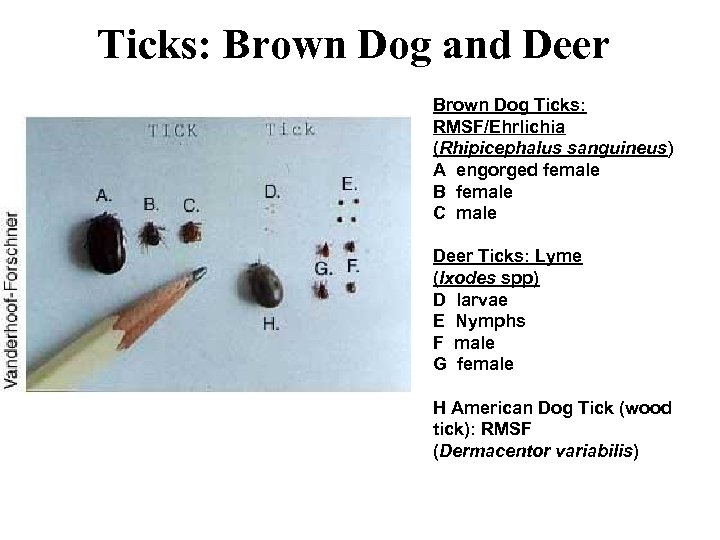
Ticks: Brown Dog and Deer Brown Dog Ticks: RMSF/Ehrlichia (Rhipicephalus sanguineus) A engorged female B female C male Deer Ticks: Lyme (Ixodes spp) D larvae E Nymphs F male G female H American Dog Tick (wood tick): RMSF (Dermacentor variabilis)
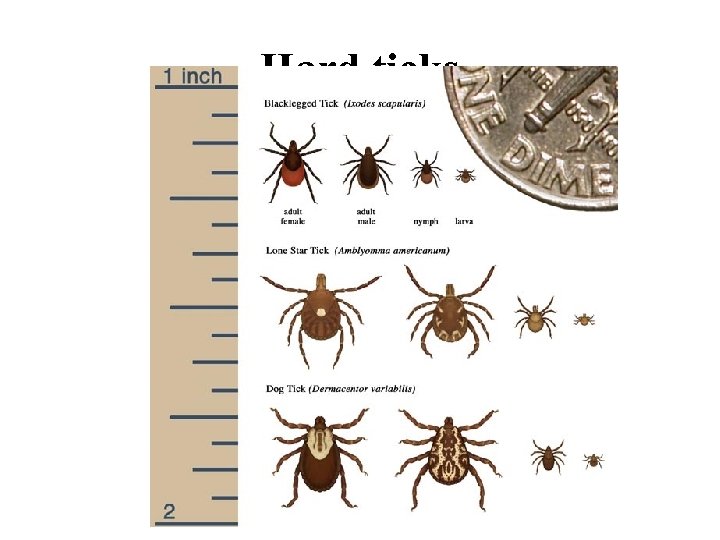
Hard ticks
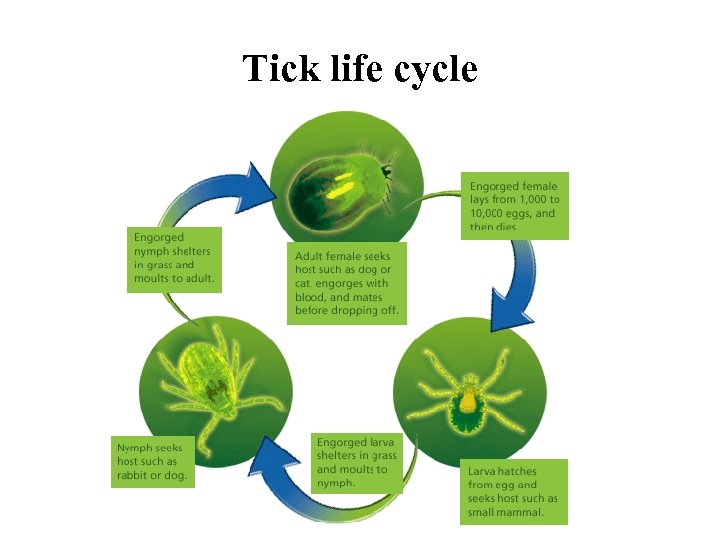
Tick life cycle
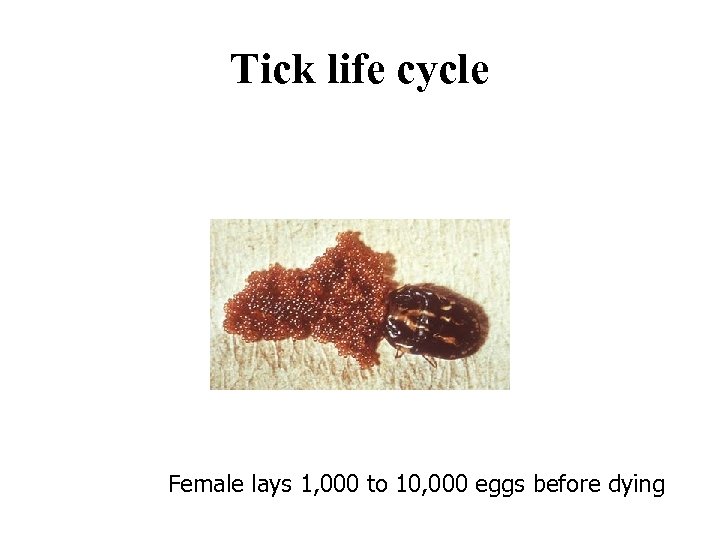
Tick life cycle Female lays 1, 000 to 10, 000 eggs before dying
Ticks – – – Irritation of the bite wound Vector for diseases Neurotoxins in saliva of 12 different species Clinical signs vary with disease Dx: finding tick; hx of exposure to wooded and grassy areas
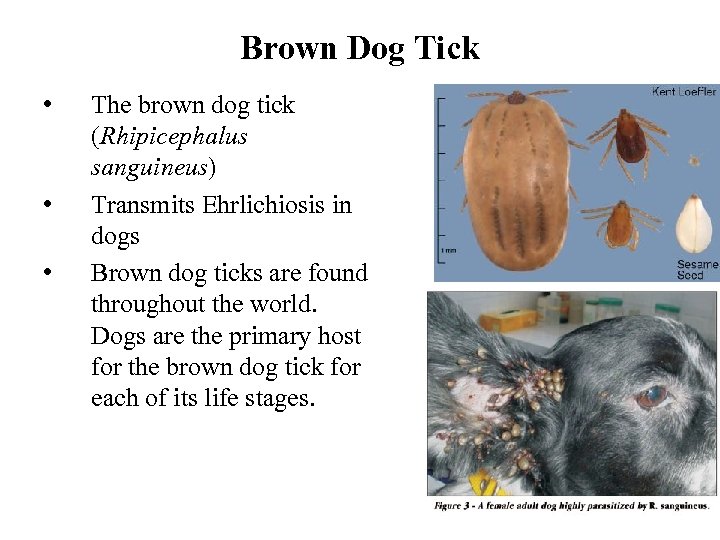
Brown Dog Tick • • • The brown dog tick (Rhipicephalus sanguineus) Transmits Ehrlichiosis in dogs Brown dog ticks are found throughout the world. Dogs are the primary host for the brown dog tick for each of its life stages.
Ticks • Rx: Manually remove ticks – Grasp head parts close to skin with forceps (NOT HANDS) and pull backwards; no gasoline, cigarettes, etc. – Topical treatments (sprays, shampoos, powder, dips) – Collars – Topical systemic products • Client Info – Routinely check pets for ticks, esp after walks in parks, etc – Do not use bare hands to remove and kill ticks – blood may be infectious – Ticks will feed on humans
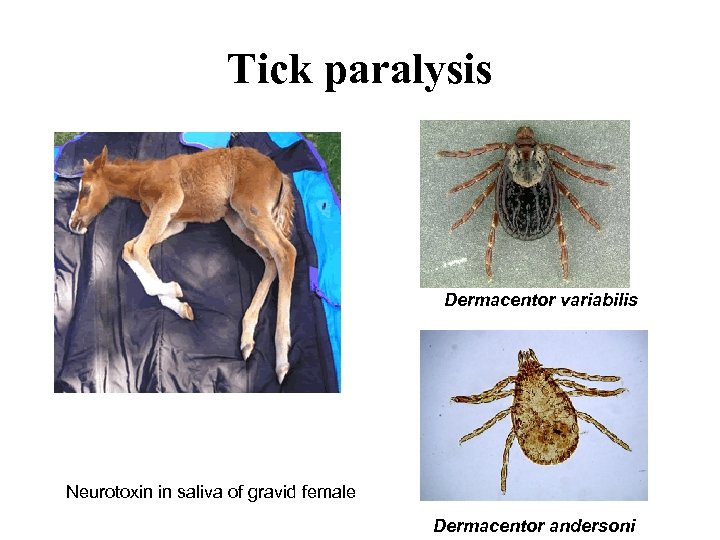
Tick paralysis Dermacentor variabilis Neurotoxin in saliva of gravid female Dermacentor andersoni
The Mites • Large variety of life styles among mites (free living vs parasitic), skin parasites vs respiratory parasites, etc. • Life cycle involves egg, larva (6 legs), nymph and adult (8 legs).
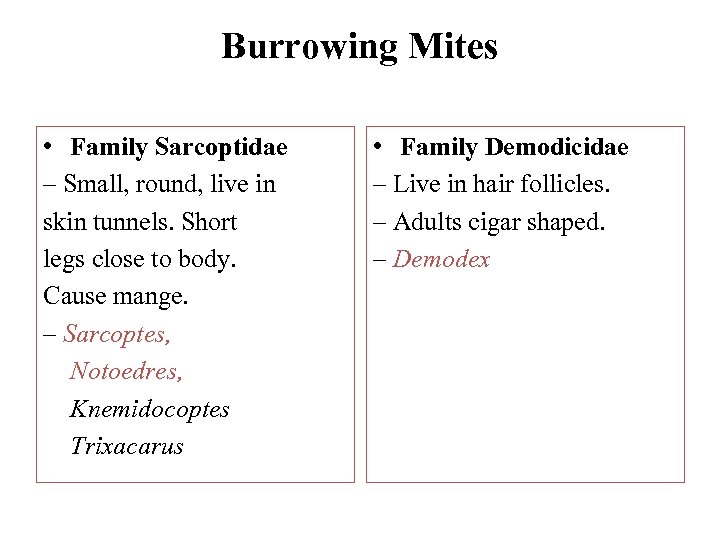
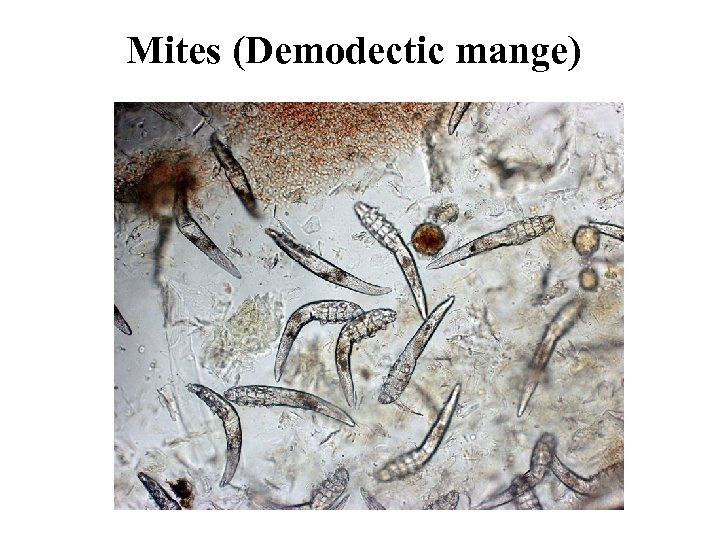
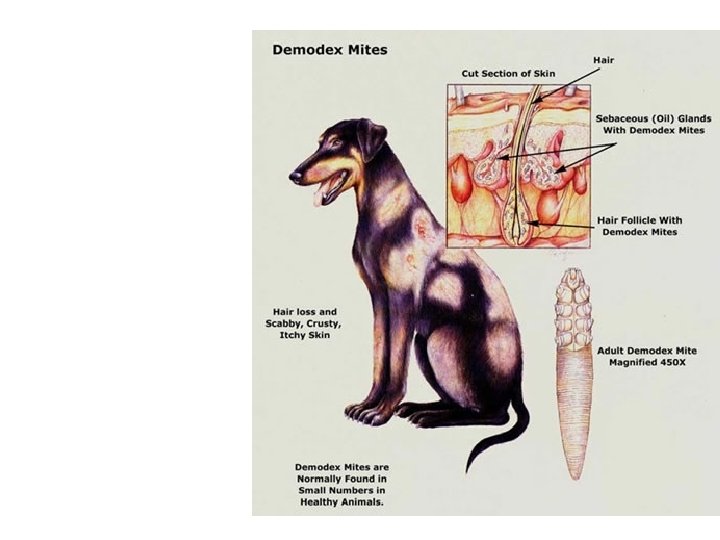
Burrowing Mites • Family Sarcoptidae – Small, round, live in skin tunnels. Short legs close to body. Cause mange. – Sarcoptes, Notoedres, Knemidocoptes Trixacarus • Family Demodicidae – Live in hair follicles. – Adults cigar shaped. – Demodex
Mites (Demodectic mange)
Demodex - Inhabits hair follicles, sebaceous glands or apocrine sweat glands - D. canis - Normal inhabitant in small numbers - Some cats are asymptomatic carriers - Spends entire life cycle on host - Immune system controls infestation - Genetic predisposition - Localized or generalized - Transmission - Have not seen dog-to-dog or dog-to-human transmission
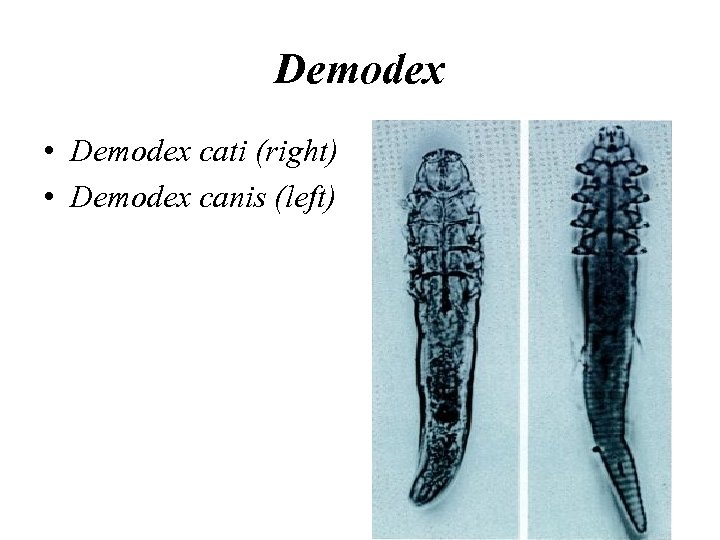
Demodex • Demodex cati (right) • Demodex canis (left)
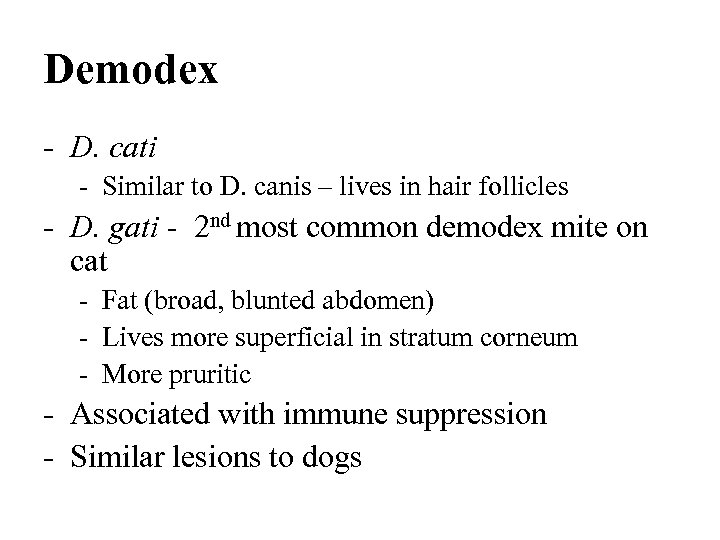
Demodex - D. cati - Similar to D. canis – lives in hair follicles - D. gati - 2 nd most common demodex mite on cat - Fat (broad, blunted abdomen) - Lives more superficial in stratum corneum - More pruritic - Associated with immune suppression - Similar lesions to dogs
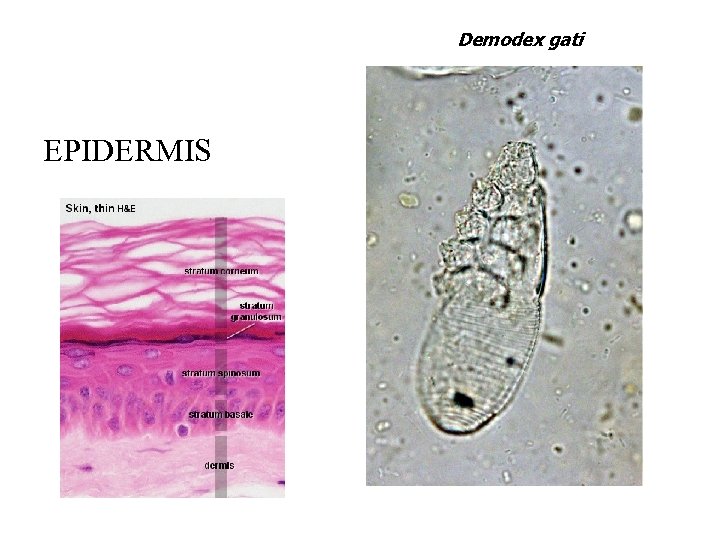
Demodex gati EPIDERMIS
DEMODEX
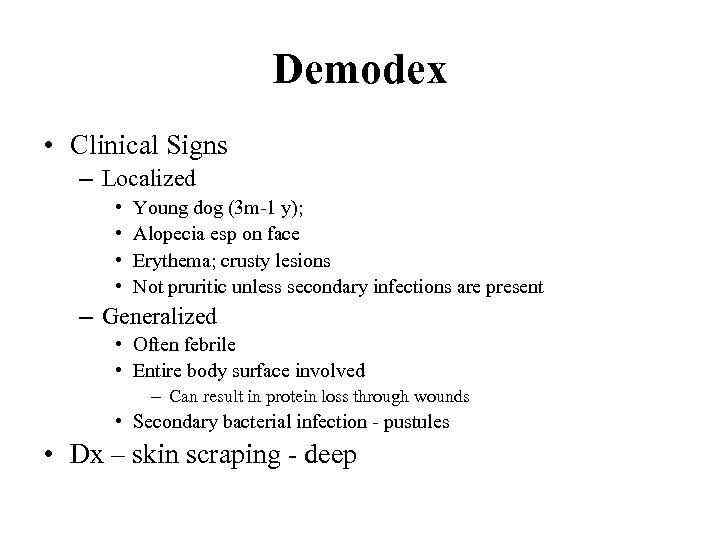
Demodex • Clinical Signs – Localized • • Young dog (3 m-1 y); Alopecia esp on face Erythema; crusty lesions Not pruritic unless secondary infections are present – Generalized • Often febrile • Entire body surface involved – Can result in protein loss through wounds • Secondary bacterial infection - pustules • Dx – skin scraping - deep

Demodex: Localized
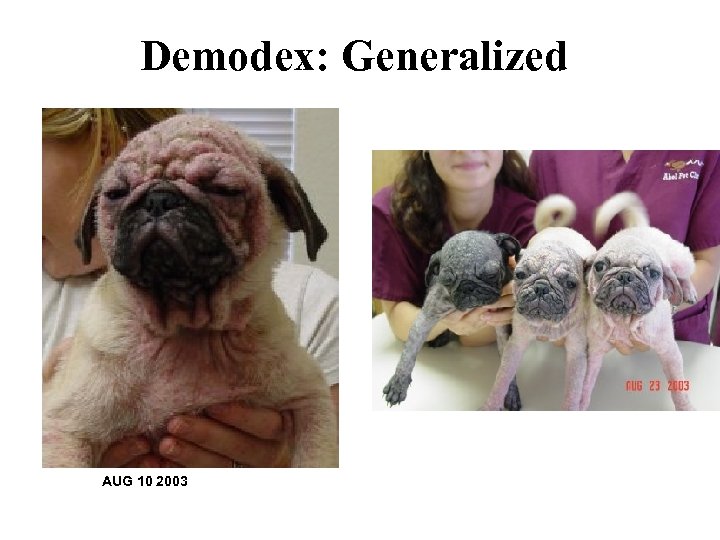
Demodex: Generalized AUG 10 2003
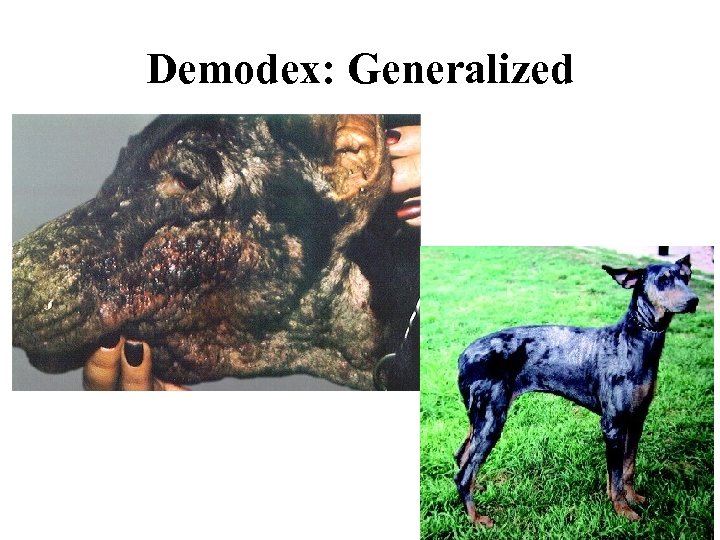
Demodex: Generalized
Demodex • Tx – Localized – Rotenone (Goodwinol) topical daily or mupiricin (Bactroban) – Generalized • Mitaban (amitraz) dips q 7 days x 3 -6 treatments or 2 negative skin scrapings – Side Effects – sedation for 12 -24 hrs (up to 72 hrs) • Ivermectin: 0. 3 mg/kg SQ repeat q 14 days OR PO SID x 60 -90 days extralabel use – client sign a release form – Not herding breeds • Interceptor: 1/mo x 3 mo or more • Oral antibiotics for secondary bacterial infections • Client Info – – Many animals outgrow demodex as they age Not contagious to humans Tx does not completely remove mites If breeding dog, then do not treat and do not breed if does not clear on its own – Strongly recommend OHE with treatment or will relapse with heat cycles – Generalized form can be fatal.
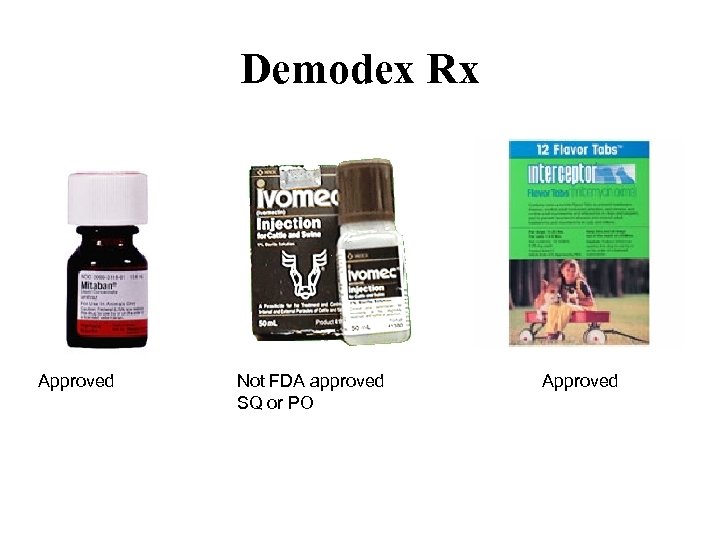
Demodex Rx Approved Not FDA approved SQ or PO Approved
Demodex • Newer drugs and protocols – Ivermectin – lower initial dose due to side effects, then gradually increase dose over several days; 300 -500 µg/kg PO SID x 90 days • SE: ataxia, bradycardia, mydriasis, resp arrest, salivation, stupor and tremors – Milbemycin (Interceptor) – 2 mg/kg PO SID x 30 -45 days • Fewer SE • Expensive for large dogs • Continue for 4 weeks post 2 nd negative skin scraping – may be cost prohibitive – moxidectin + Imidacloprid (Advantage Multi) • Only APPROVED treatments – Amitraz (Mitaban) – Moxidectin + imidacloprid in topical formulation (Advantage Multi) – Milbemycin oxime (Interceptor) orally
![Mites (Sarcoptic mange [Scabies]) Mites (Sarcoptic mange [Scabies])](https://present5.com/presentation/ac057dc21ca804b6b59f3369eb3c43ef/image-93.jpg)
Mites (Sarcoptic mange [Scabies])
Sarcoptic Mange - Species specific - Adults live 4 -5 weeks - Egg-larva-nymph-adult cycle - 17 -21 days - Entire life cycle on skin - Infective in house environment for 24 -36 hrs - Burrows under skin – stratum corneum (epidermis) - Hypersensitivity reaction
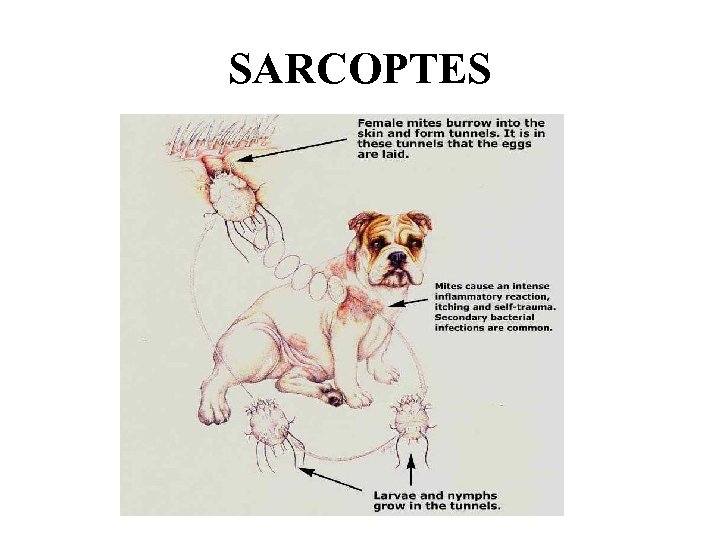
SARCOPTES
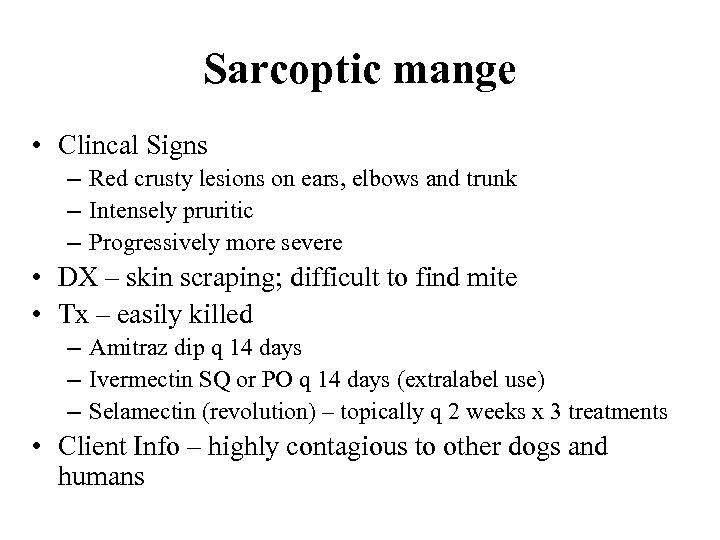
Sarcoptic mange • Clincal Signs – Red crusty lesions on ears, elbows and trunk – Intensely pruritic – Progressively more severe • DX – skin scraping; difficult to find mite • Tx – easily killed – Amitraz dip q 14 days – Ivermectin SQ or PO q 14 days (extralabel use) – Selamectin (revolution) – topically q 2 weeks x 3 treatments • Client Info – highly contagious to other dogs and humans
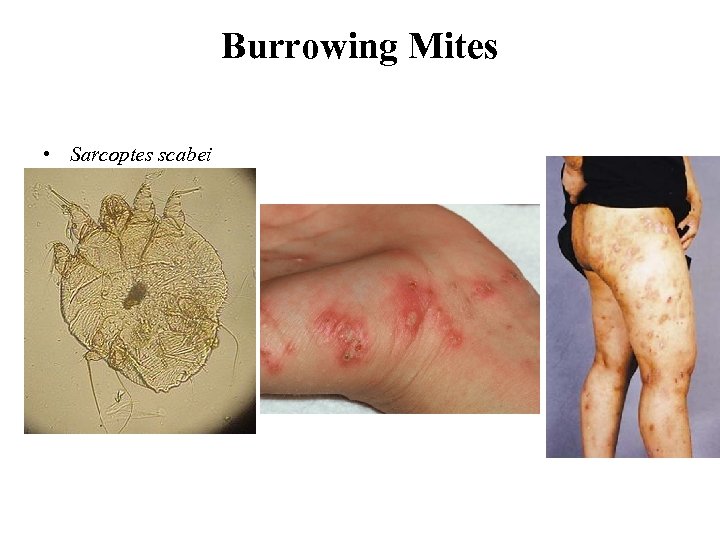
Burrowing Mites • Sarcoptes scabei

Scabies: Clinical signs
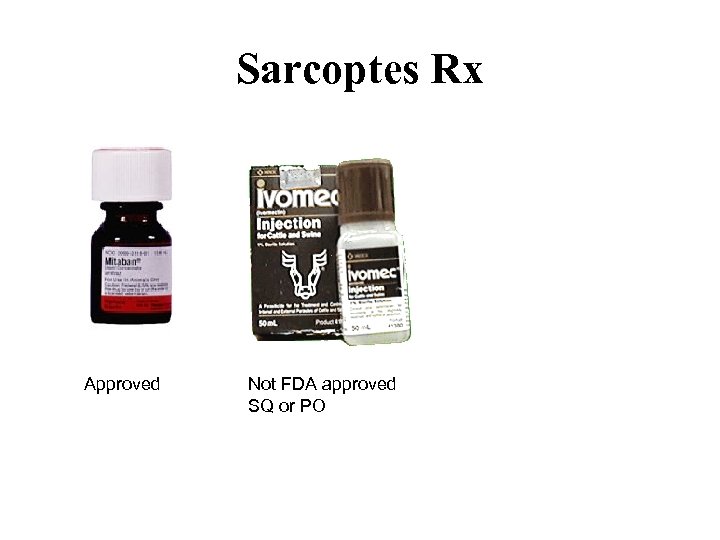
Sarcoptes Rx Approved Not FDA approved SQ or PO
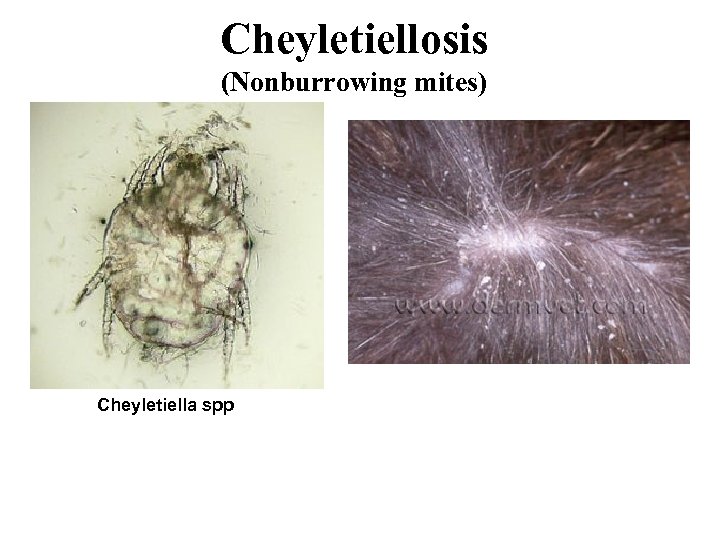
Cheyletiellosis (Nonburrowing mites) Cheyletiella spp
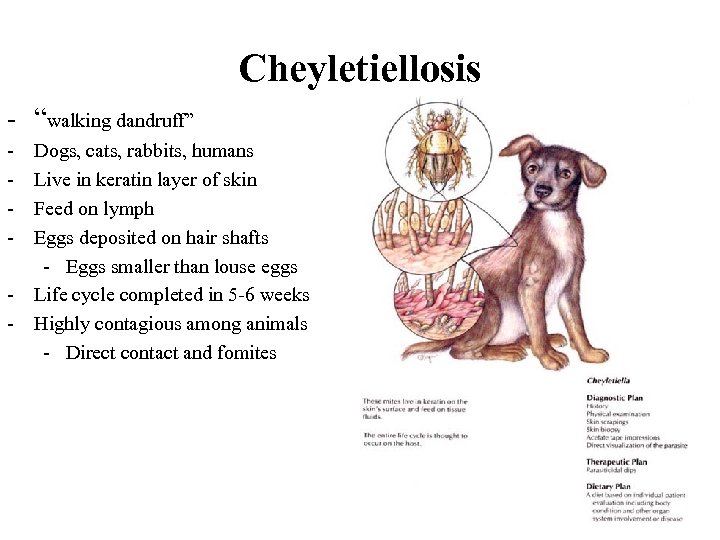
Cheyletiellosis - “walking dandruff” - Dogs, cats, rabbits, humans Live in keratin layer of skin Feed on lymph Eggs deposited on hair shafts - Eggs smaller than louse eggs Life cycle completed in 5 -6 weeks Highly contagious among animals - Direct contact and fomites
Cheyletiellosis • Clinical Signs – Severity of pruritis varies – Dry scales along back => entire body – Patchy hair loss from scratching – Dx: collect scales with clear tape, flea comb, skin scraping and ID with microscope – Rx: Weekly baths with flea control products containing pyrethrins or permethrin and/or lime sulfur dip
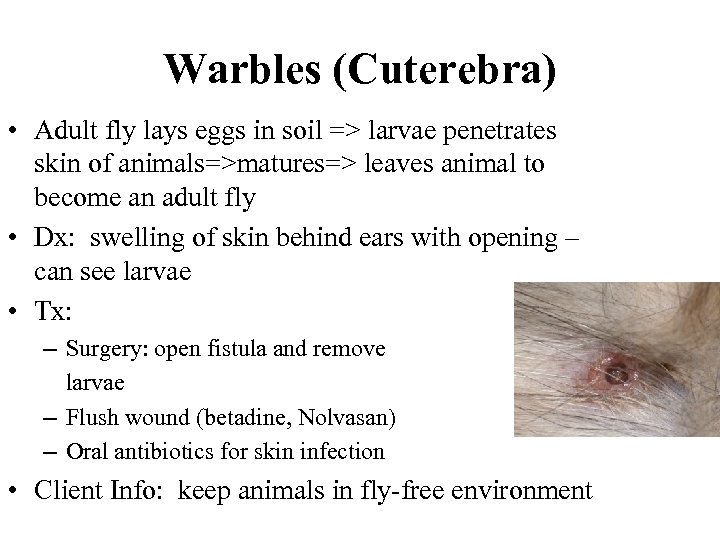
Warbles (Cuterebra) • Adult fly lays eggs in soil => larvae penetrates skin of animals=>matures=> leaves animal to become an adult fly • Dx: swelling of skin behind ears with opening – can see larvae • Tx: – Surgery: open fistula and remove larvae – Flush wound (betadine, Nolvasan) – Oral antibiotics for skin infection • Client Info: keep animals in fly-free environment
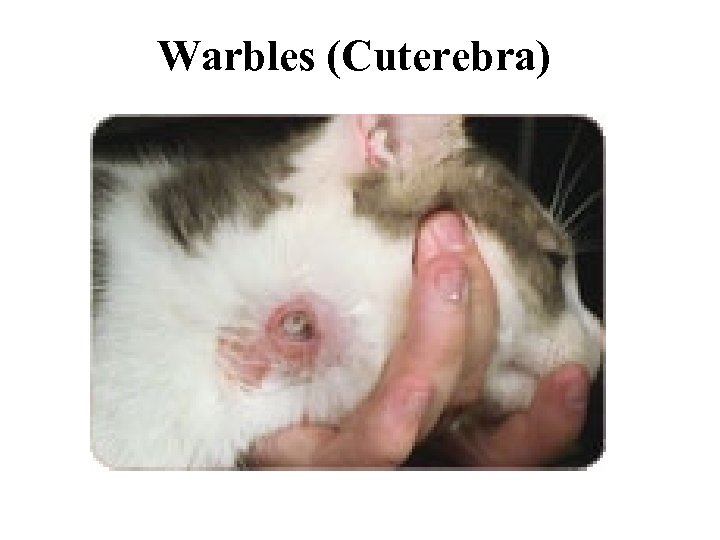
Warbles (Cuterebra)
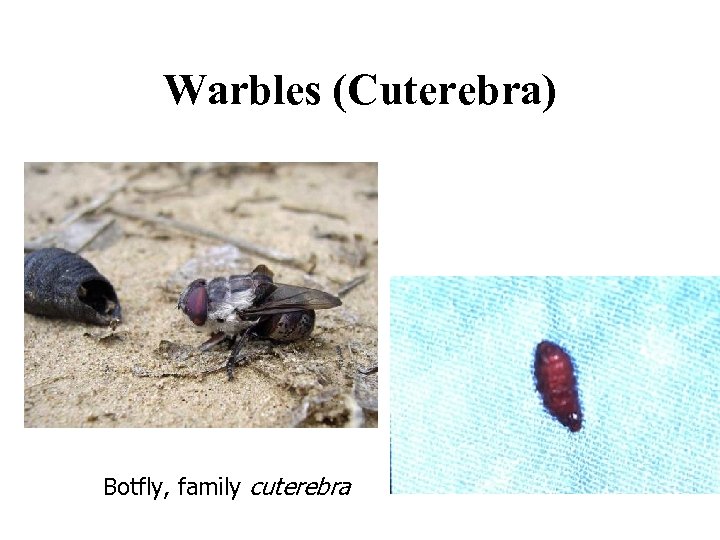
Warbles (Cuterebra) Botfly, family cuterebra
EDUCATION “Education is a progressive discovery of our own ignorance. ” -Will Durant

Myiasis (Fly maggots)
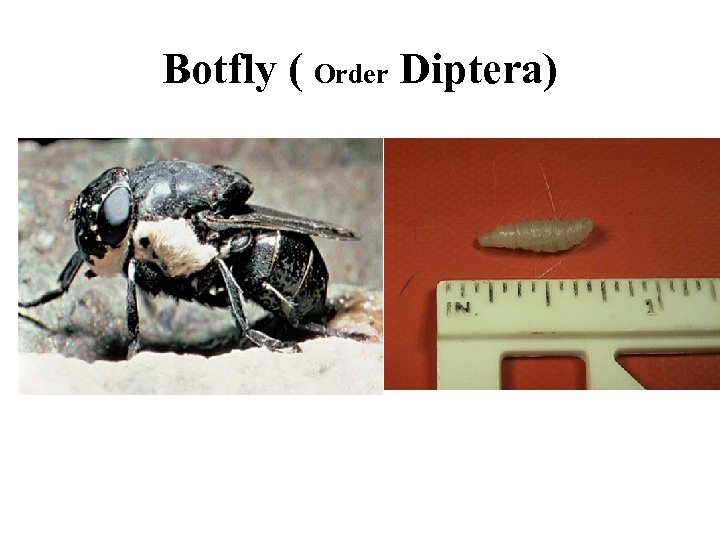
Botfly ( Order Diptera)
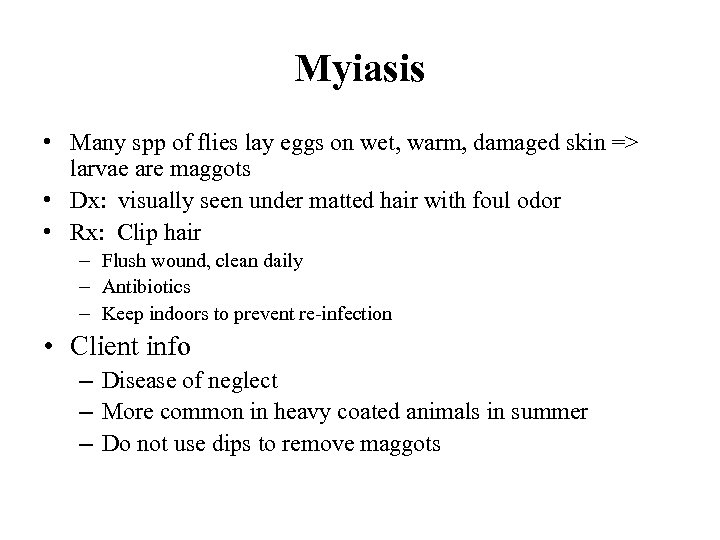
Myiasis • Many spp of flies lay eggs on wet, warm, damaged skin => larvae are maggots • Dx: visually seen under matted hair with foul odor • Rx: Clip hair – Flush wound, clean daily – Antibiotics – Keep indoors to prevent re-infection • Client info – Disease of neglect – More common in heavy coated animals in summer – Do not use dips to remove maggots

Dog Lice (Linognathus setosus)
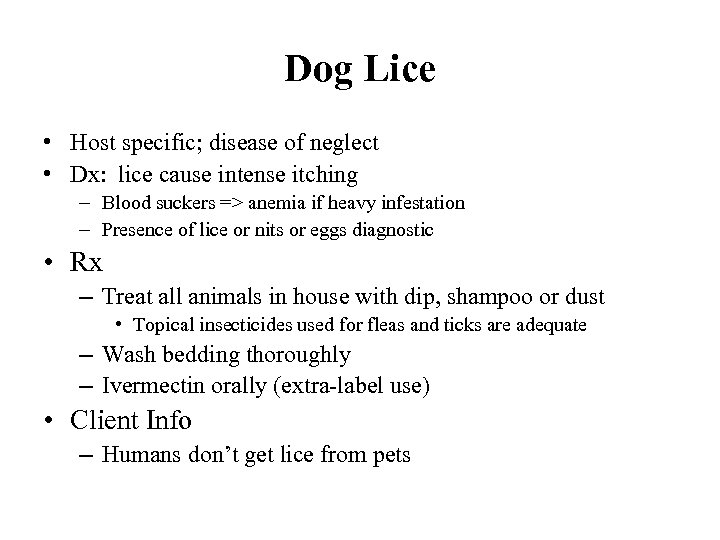
Dog Lice • Host specific; disease of neglect • Dx: lice cause intense itching – Blood suckers => anemia if heavy infestation – Presence of lice or nits or eggs diagnostic • Rx – Treat all animals in house with dip, shampoo or dust • Topical insecticides used for fleas and ticks are adequate – Wash bedding thoroughly – Ivermectin orally (extra-label use) • Client Info – Humans don’t get lice from pets
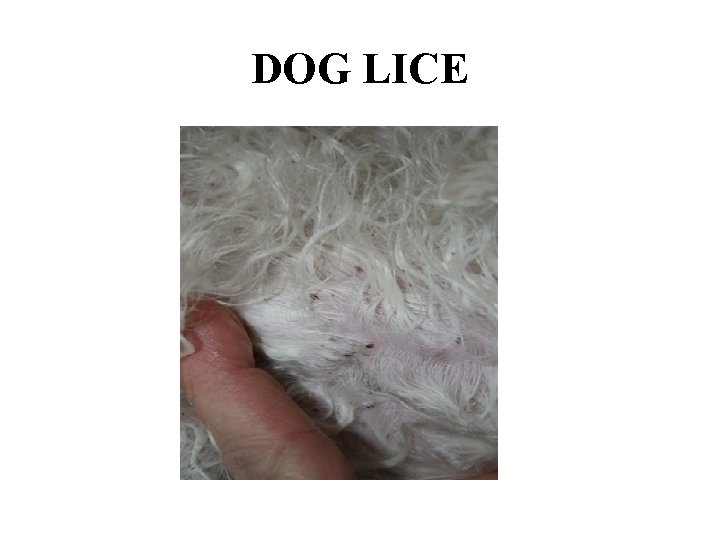
DOG LICE

Dermatophytes Microsporum canis
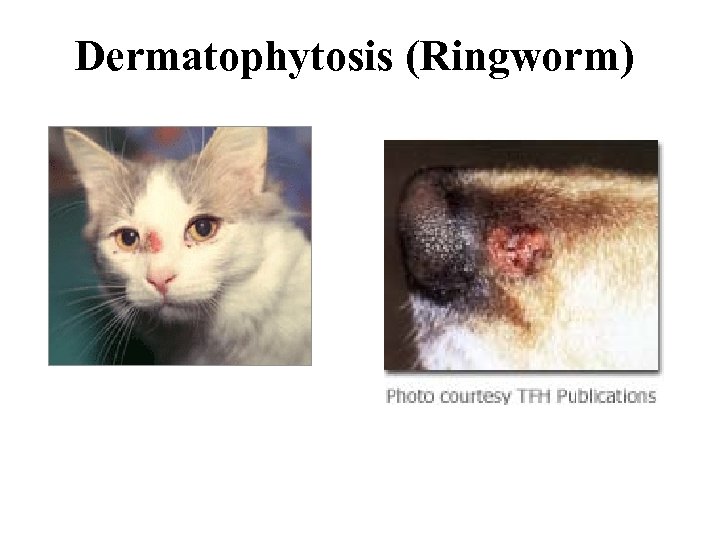
Dermatophytosis (Ringworm)
Dermatophytosis • Superficial cutaneous infection • 3 primary dermatophytes – Microsporum canis – Trichophyton mentagrophytes – Microsporum gypseum • Cat: 90% M. canis; Dog: all 3 • Transmission – Direct contact – Contact with infected hair and scale – Fomites • Spores small and easily aerosolized • Fleas • Infected hairs – infective for up to 18 months – – – Incubation period 1 -3 weeks M. canis – cats Trichophyton – rodents or nests M. gypseum – geophilic (soil) More common in moist, warm environments
Dermatophytosis • Clinical Signs – Hair loss, scaling and crusting – +/- pruritus – Cats • Mimics other skin diseases • Kittens – facial 1 st • Can form ulcerated dermal nodules – Dog • Focal or multifocal areas of hair loss • Papules, scales and crusts • Central area of hyperpigmentation
Dermatophytosis • Dx: – Wood’s Light – UV light • • Quick and easy screen 50% of M. canis fluoresce, rest do not Differentiate from scale, dust, dirt Lamp must warm up for 5 minutes prior to exam.
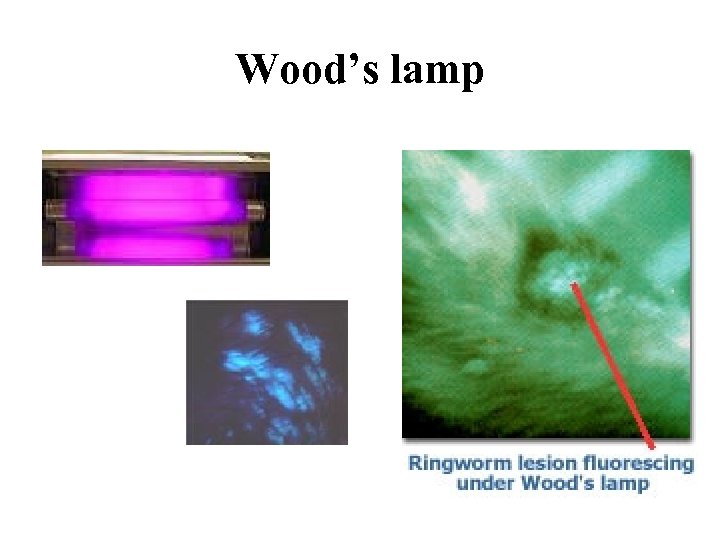
Wood’s lamp
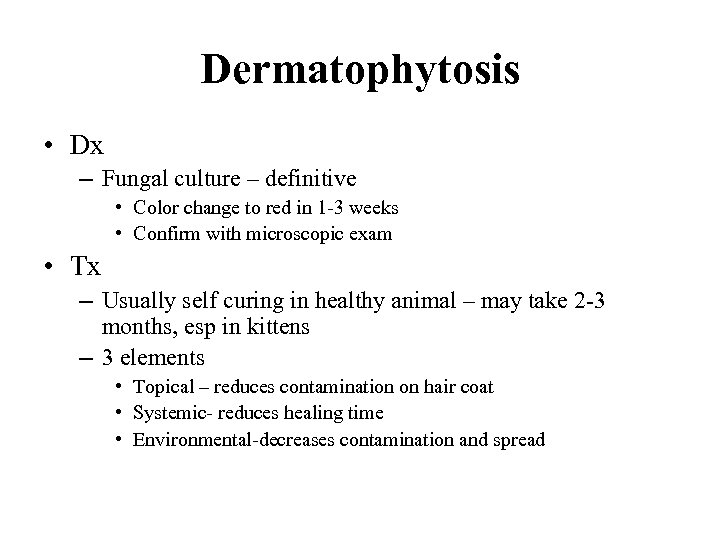
Dermatophytosis • Dx – Fungal culture – definitive • Color change to red in 1 -3 weeks • Confirm with microscopic exam • Tx – Usually self curing in healthy animal – may take 2 -3 months, esp in kittens – 3 elements • Topical – reduces contamination on hair coat • Systemic- reduces healing time • Environmental-decreases contamination and spread

Microsporum canis
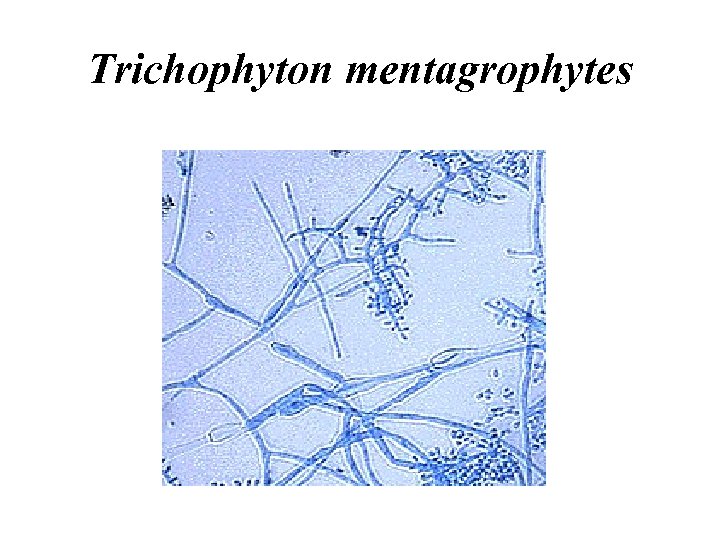
Trichophyton mentagrophytes
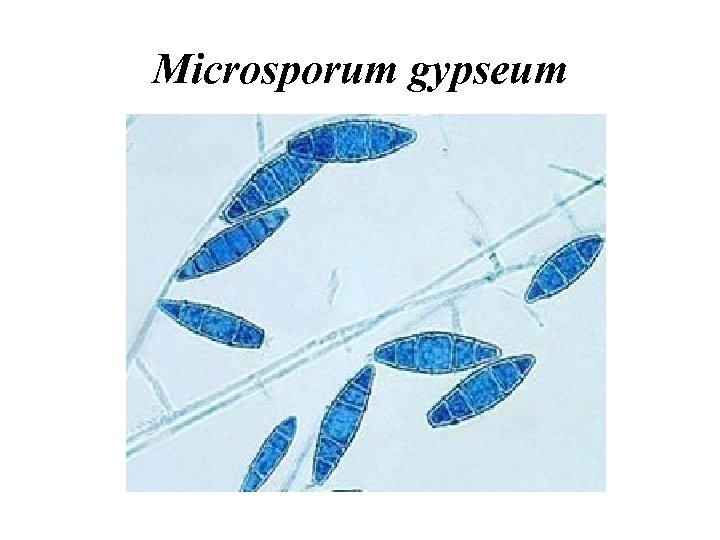
Microsporum gypseum
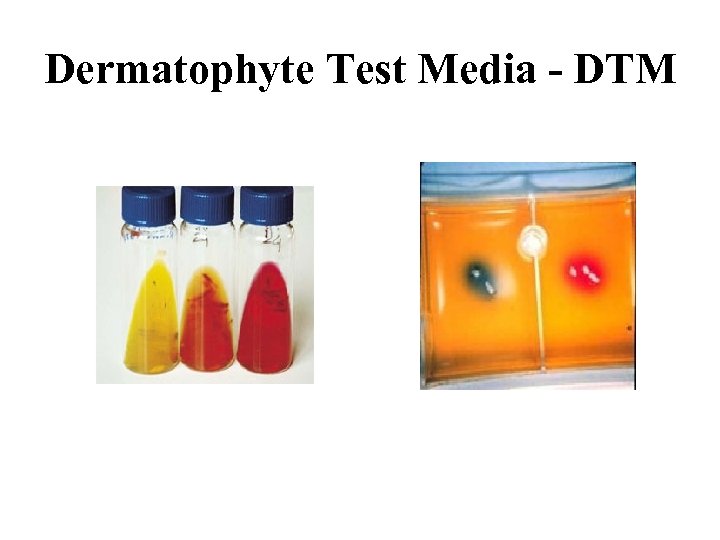
Dermatophyte Test Media - DTM
Dermatophytosis – Treatment • Clip haircoat, particularly long hairs • Topicals – Spot treatment may predispose to subclinical infections – Whole body shampoos, dips, rinses twice weekly • Lime-sulfur at 8 oz/gal (4 oz not effective) • Miconazole containing shampoos
Dermatophytosis-Treatment • Systemic tx – Griseofulvin (don’t use in pregnant animals: teratogenic effects) • GI absorption variable • Adverse effects – Vomiting/diarrhea, anorexia – Bone marrow suppression – Neurologic signs – Ketoconazole (Aplastic anemia in FIV + cats) • Potential liver toxicity – Intraconazole • Less Side effects – Lufenuron – inhibits chitin formation; chitin in outer wall of fungi • Being studied – Tx till resolution of signs and 2 negative cultures
Dermatophytosis – Treatment • Environment – Remove or discard all bedding, brushes, fabric toys, etc – Cheap vacuum to clean with, then discard – Clean all surfaces; use bleach – Vacuum daily – Disinfect weekly – Catteries – strict isolation
Dermatophytosis – Zoonosis • At risk populations: children, immune suppressed adults, older adults • Vaccine – reduces severity but not occurrence of disease – May not be available now • Cats can be carriers w/o clinical signs

Ringworm (human)
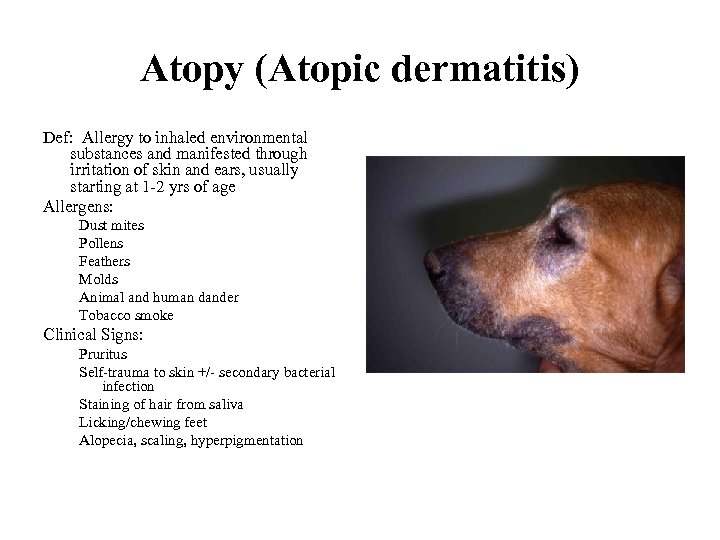
Atopy (Atopic dermatitis) Def: Allergy to inhaled environmental substances and manifested through irritation of skin and ears, usually starting at 1 -2 yrs of age Allergens: Dust mites Pollens Feathers Molds Animal and human dander Tobacco smoke Clinical Signs: Pruritus Self-trauma to skin +/- secondary bacterial infection Staining of hair from saliva Licking/chewing feet Alopecia, scaling, hyperpigmentation
Atopy • Dx – Accurate hx critical • R/o food allergies, flea allergy dermatitis, sarcoptic mange, contact dermatitis BEFORE diagnosis of atopy can be made – Intradermal skin testing – most accurate to identify offending allergen • Tx: No cure – ID and eliminate cause best treatmetn – ATOPICA – contains cyclosporin A (immunosuppressor), Antiinflammatory and antipruritic – Treat any bacterial or fungal infections before using immune suppressive drugs – Medication (steroids, Abs) and allergy shots (desensitization) – Omega 3 fatty acids – Antihistamines-more effective if given before symptoms occur
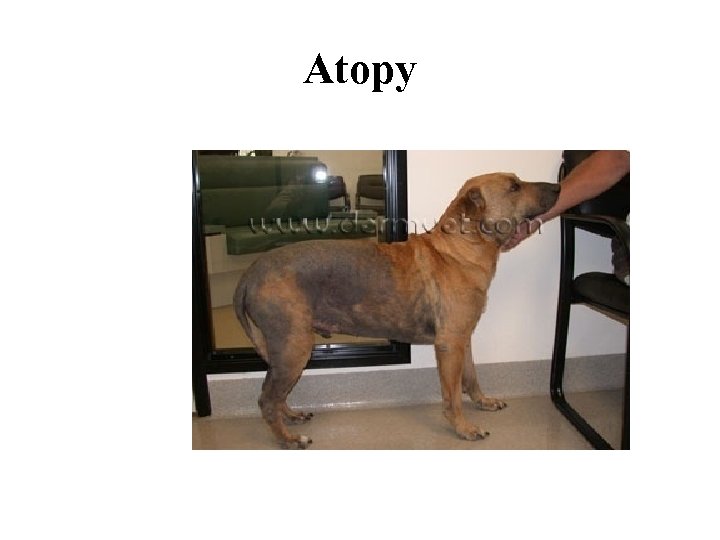
Atopy
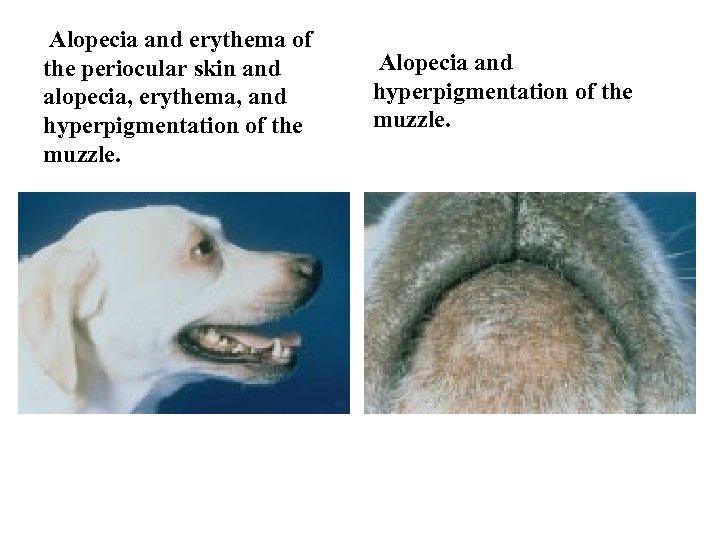
Alopecia and erythema of the periocular skin and alopecia, erythema, and hyperpigmentation of the muzzle. Alopecia and hyperpigmentation of the muzzle.
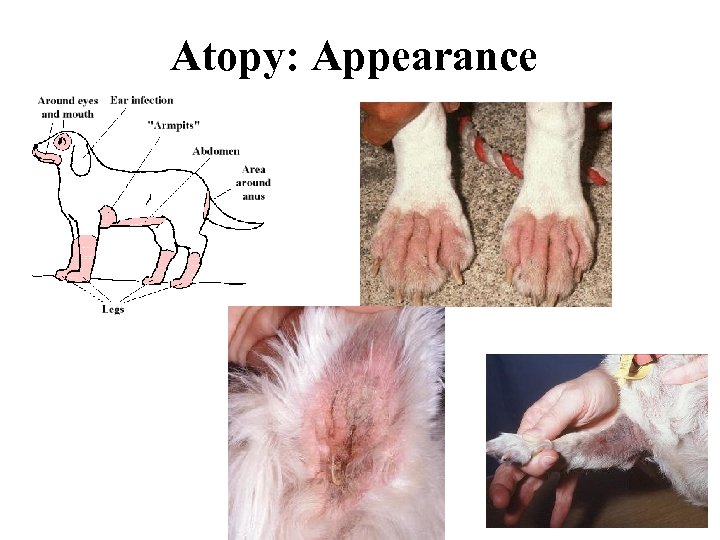
Atopy: Appearance
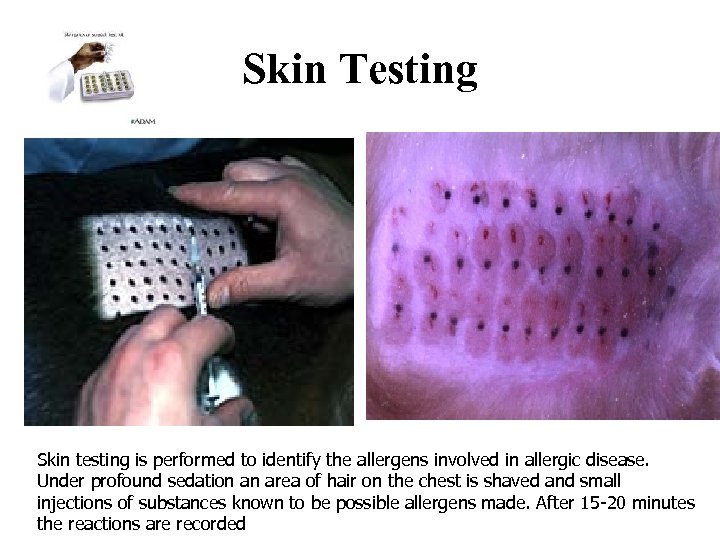
Skin Testing Skin testing is performed to identify the allergens involved in allergic disease. Under profound sedation an area of hair on the chest is shaved and small injections of substances known to be possible allergens made. After 15 -20 minutes the reactions are recorded
Food Allergies • 10% of allergies • Usually starts between 2 -6 yrs • Processed foods increase likelihood of reaction – Fillers, artificial colors, preservatives

Food allergies in dogs
Food Allergies • Dx and Tx – Elimination diets: new source of protein for 3 mo. – If improves, reintroduce original protein to see if symptoms recur – confirmation of dx – Use new diet. – May develop allergies to new diet later
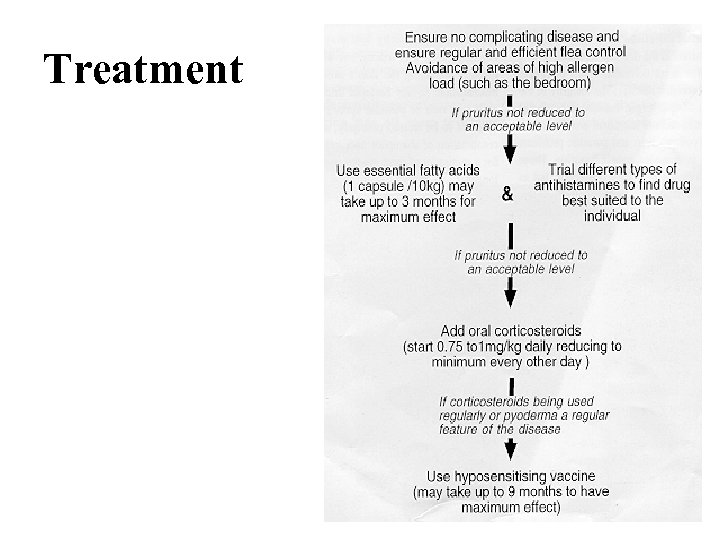
Treatment

Food allergies
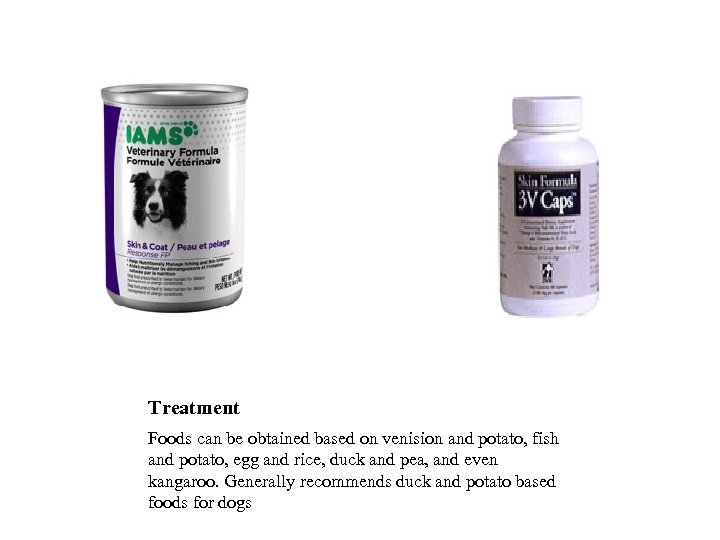
Treatment Foods can be obtained based on venision and potato, fish and potato, egg and rice, duck and pea, and even kangaroo. Generally recommends duck and potato based foods for dogs
How do you diagnose food intolerance (food allergy)? • The patient is fed a hypoallergenic diet for 6090 days. This allows the body to become desensitized to the offending allergens. When the previous diet is fed back to the pet, an acute hypersensitivity reaction may occur. This helps to identify that a food was the source of the allergic signs
Pruritits Algorithm • Dogs • Cats
Evaluating Feline Pruritus • Feline Food Allergy – Year round pruritus – Variable response to steroids – 10 -30% with concurrent GI symptoms • Common offending proteins -Dairy, fish, beef, pork, chicken, rabbit, horse, lamb, eggs, clams, "commercial diets"
Managing Feline Pruritus • • Diagnosing food allergy 10 week food trial Home cooked meat Potato/rice Canned food Innovative Veterinary Diets (IVD) Green pea & duck/rabbit Hills ZD? ? ?
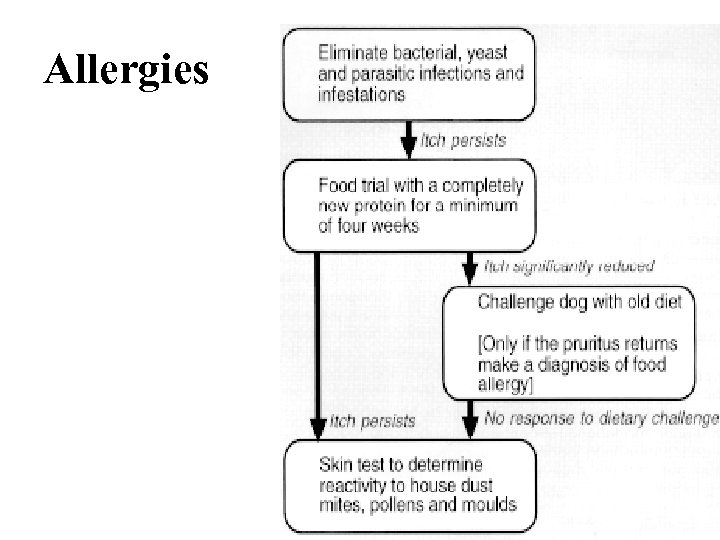
Allergies
References • Alleice Summers, Common Diseases of Companion Animals • Dr. Ralf S. Mueller, Dermatology for the Small Animal Practitioner
ac057dc21ca804b6b59f3369eb3c43ef.ppt